The Opioid Epidemic and Medication Assisted Treatment Timothy






















- Slides: 57

The Opioid Epidemic and Medication Assisted Treatment Timothy W. Fong MD UCLA Addiction Psychiatry Southern California Collaborative Court Regional Training April 16, 2016
Financial Disclosures Speaker Bureau Indivior Research Support Constellation Friday Night Live Onward, Inc.

Overview • Opioid Dependence – Opioid Use Disorder • Screening and Assessment • Treatment – Focus on Buprenorphine
Opioid Use Disorder (DSM-5) • Now, known as Opioid Use Disorder • Combines Opioid Abuse and Opioid Dependence • Aka Opioid Addiction • 2 out of 11 diagnostic criteria
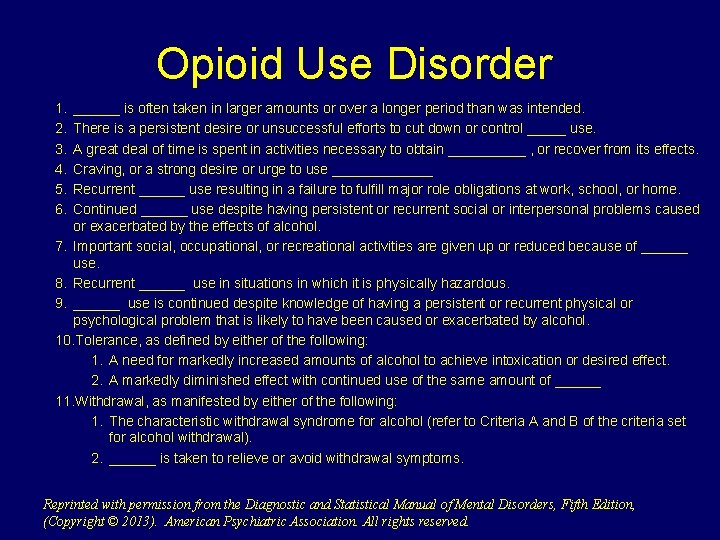
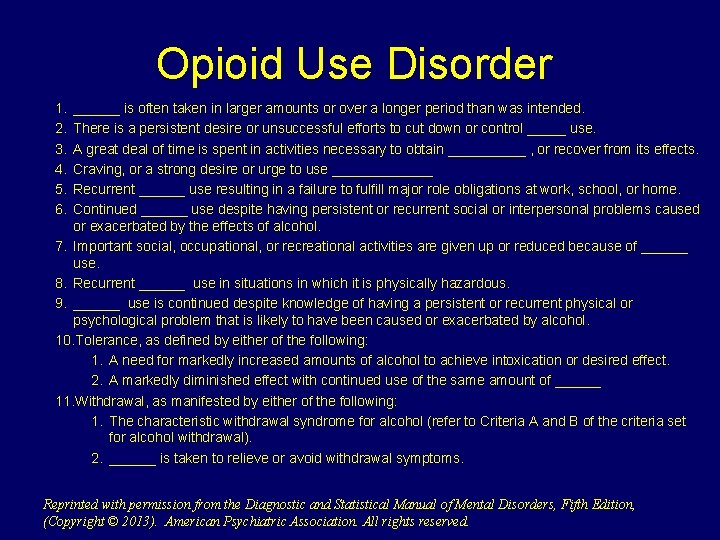
Opioid Use Disorder 1. 2. 3. 4. 5. 6. ______ is often taken in larger amounts or over a longer period than was intended. There is a persistent desire or unsuccessful efforts to cut down or control _____ use. A great deal of time is spent in activities necessary to obtain _____ , or recover from its effects. Craving, or a strong desire or urge to use _______ Recurrent ______ use resulting in a failure to fulfill major role obligations at work, school, or home. Continued ______ use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol. 7. Important social, occupational, or recreational activities are given up or reduced because of ______ use. 8. Recurrent ______ use in situations in which it is physically hazardous. 9. ______ use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol. 10. Tolerance, as defined by either of the following: 1. A need for markedly increased amounts of alcohol to achieve intoxication or desired effect. 2. A markedly diminished effect with continued use of the same amount of ______ 11. Withdrawal, as manifested by either of the following: 1. The characteristic withdrawal syndrome for alcohol (refer to Criteria A and B of the criteria set for alcohol withdrawal). 2. ______ is taken to relieve or avoid withdrawal symptoms. Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, (Copyright © 2013). American Psychiatric Association. All rights reserved.
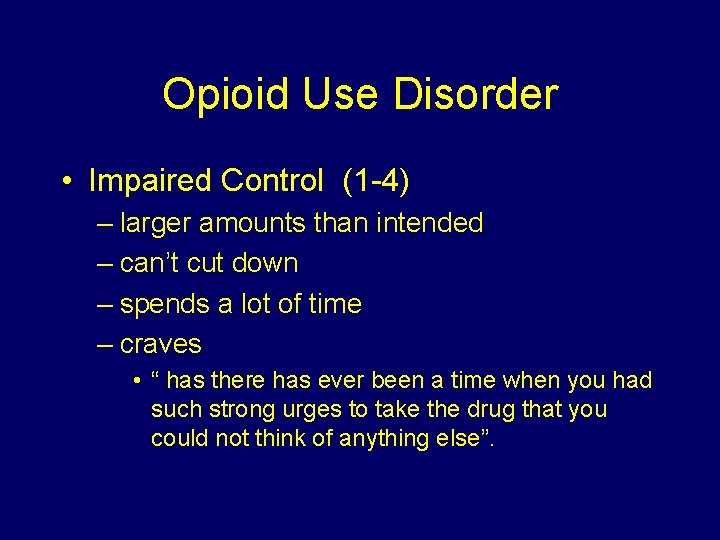
Opioid Use Disorder • Impaired Control (1 -4) – larger amounts than intended – can’t cut down – spends a lot of time – craves • “ has there has ever been a time when you had such strong urges to take the drug that you could not think of anything else”.

Opioid Use Disorder • Social Impairment (5 -7) – Failure to fulfill life obligations – Activities given up or reduced – Social problems
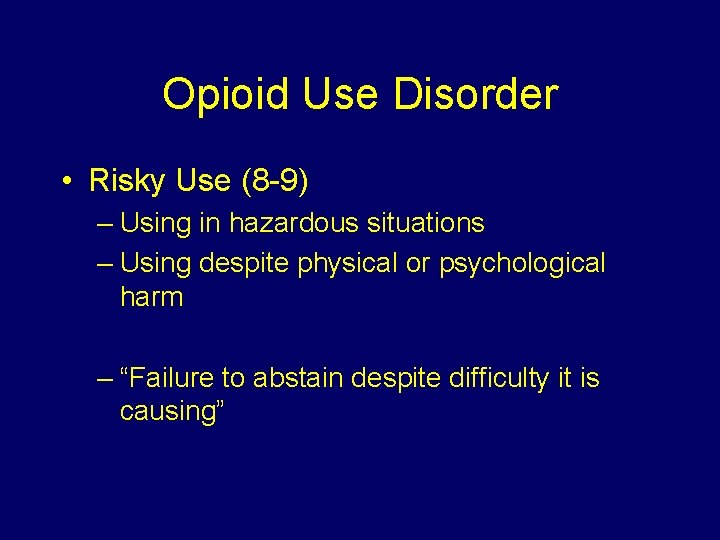
Opioid Use Disorder • Risky Use (8 -9) – Using in hazardous situations – Using despite physical or psychological harm – “Failure to abstain despite difficulty it is causing”
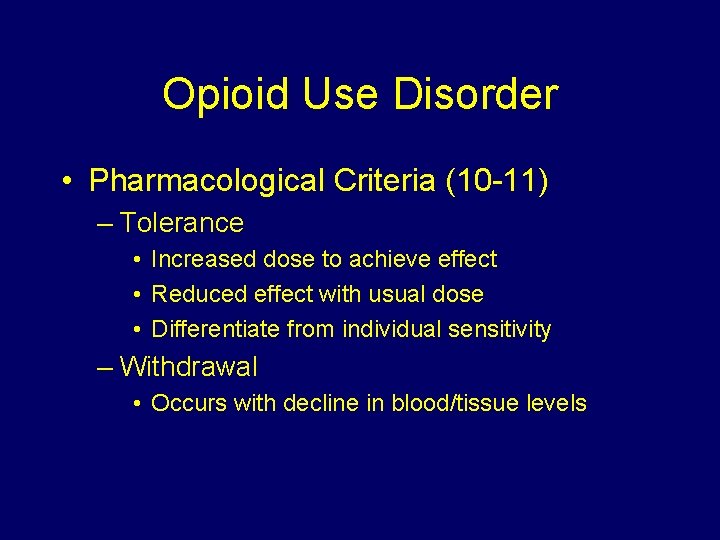
Opioid Use Disorder • Pharmacological Criteria (10 -11) – Tolerance • Increased dose to achieve effect • Reduced effect with usual dose • Differentiate from individual sensitivity – Withdrawal • Occurs with decline in blood/tissue levels
The Opioid Epidemic
Signs of the Opioid Epidemic: More Deaths • Since 1999, the rate of overdose deaths involving opioids (prescription opioids and heroin have quadrupled • More deaths than MVAs • > 30, 000 per year • ~78 opioid overdoses per day • ~4500 deaths in California / year
Signs of the Opioid Epidemic: Increased Heroin Use • Past month heroin use, past year heroin use, and heroin addiction have all since increased among 18 -25 year olds since 2000 • More heroin available on the street • 80% of heroin initiates used prescription opiates previously
Signs of the Opioid Epidemic: Rise of Prescription Opioids • 2014, ~2 million Americans were dependent on prescription opioids. • 1 in 4 people who receive prescription opioids long term for non-cancer pain in primary care settings struggles SUD • Daily, >1, 000 people are treated in emergency departments for misusing prescription opioids


Obama Administration Announces Additional Actions to Address the Prescription Opioid Abuse and Heroin Epidemic March 28, 2016
Action List • • • Expand access to treatment Create MH/SUD Taskforce Prevent Overdose Deaths (naloxone) SUD Treatment Parity Implement Syringe Services Programs Medical Schools – Mandated Prescriber Education
Abused Opiates Prescription Pills Heroin
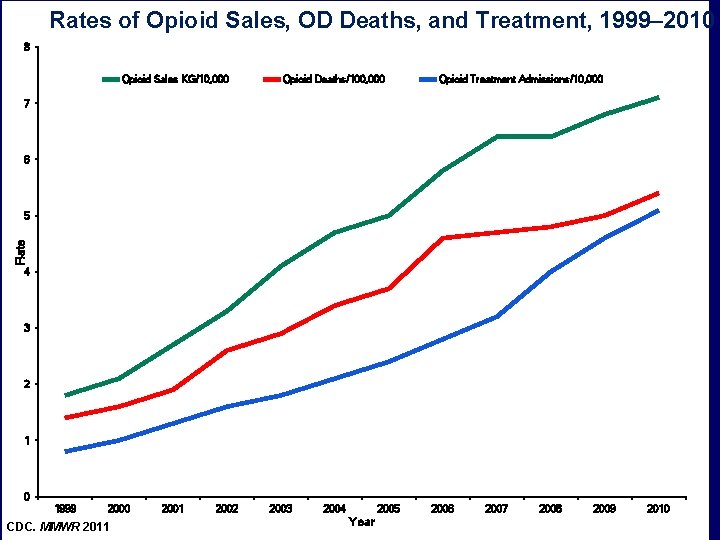
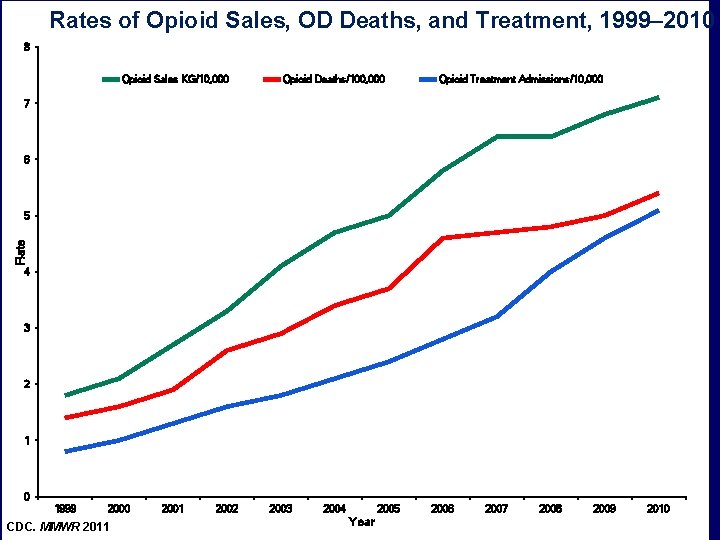
Rates of Opioid Sales, OD Deaths, and Treatment, 1999– 2010 8 Opioid Sales KG/10, 000 Opioid Deaths/100, 000 Opioid Treatment Admissions/10, 000 7 6 Rate 5 4 3 2 1 0 1999 2000 CDC. MMWR 2011 2002 2003 2004 2005 Year 2006 2007 2008 2009 2010


Screening for Opioid Use Disorders
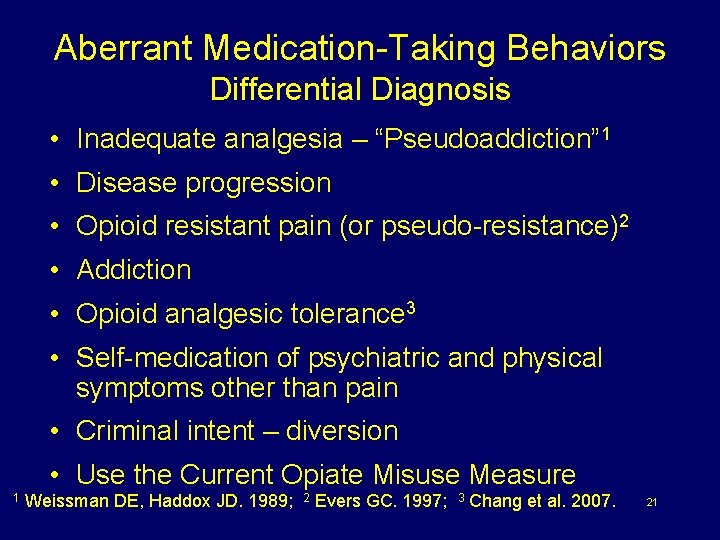
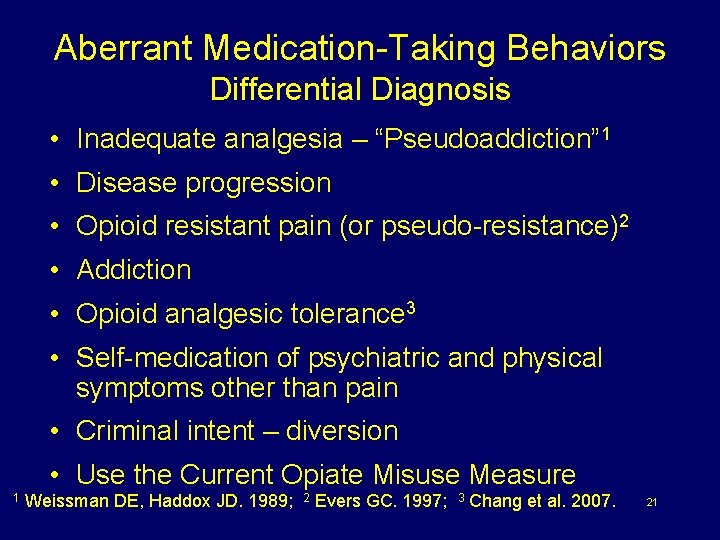
Aberrant Medication-Taking Behaviors Differential Diagnosis • Inadequate analgesia – “Pseudoaddiction” 1 • Disease progression • Opioid resistant pain (or pseudo-resistance)2 • Addiction • Opioid analgesic tolerance 3 • Self-medication of psychiatric and physical symptoms other than pain • Criminal intent – diversion • Use the Current Opiate Misuse Measure 1 Weissman DE, Haddox JD. 1989; 2 Evers GC. 1997; 3 Chang et al. 2007. 21

Assessing Signs and Symptoms of Withdrawal • Ways to assess withdrawal – Written scales (eg, COWS) – Clinical experience • Signs and symptoms (eg, sweating, pupil size, runny nose, gooseflesh) The National Alliance of Advocates for Buprenorphine Treatment. http: //www. naabt. org/documents/NAABT_Precip. WD. pdf. Accessed June 24, 2011.

Pharmacotherapy for Opioid Use Disorder

Opioid Use Disorder Treatment Goals • • • Treat withdrawal Reduce cravings Block euphoria from opiates Improve quality of life Engage in treatment
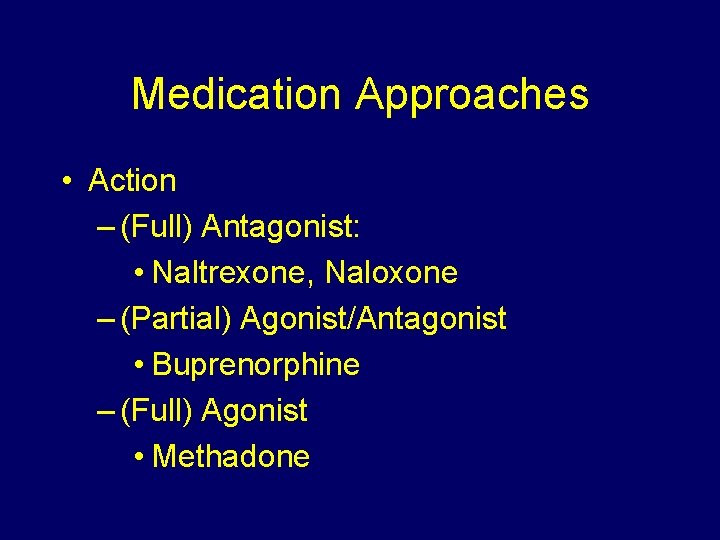
Medication Approaches • Action – (Full) Antagonist: • Naltrexone, Naloxone – (Partial) Agonist/Antagonist • Buprenorphine – (Full) Agonist • Methadone

FDA-Approved Medications Drug of Abuse Brand Name Generic Opiates Buprenorphine/ Naloxone Subutex Methadone Revia Naltrexone Vivitrol Naltrexone
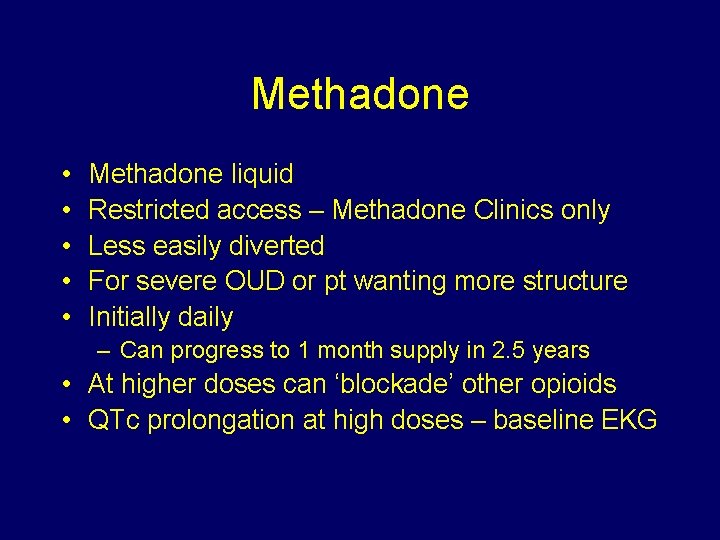
Methadone • • • Methadone liquid Restricted access – Methadone Clinics only Less easily diverted For severe OUD or pt wanting more structure Initially daily – Can progress to 1 month supply in 2. 5 years • At higher doses can ‘blockade’ other opioids • QTc prolongation at high doses – baseline EKG
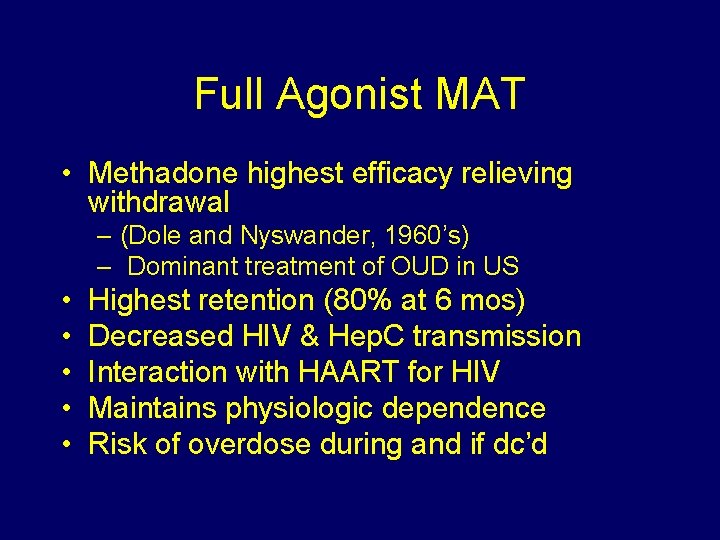
Full Agonist MAT • Methadone highest efficacy relieving withdrawal – (Dole and Nyswander, 1960’s) – Dominant treatment of OUD in US • • • Highest retention (80% at 6 mos) Decreased HIV & Hep. C transmission Interaction with HAART for HIV Maintains physiologic dependence Risk of overdose during and if dc’d
Methadone Effects last 24 hours that allow functioning Withdrawal symptoms are slower and milder Advantages: Cannot be injected Longer duration than Heroin Controlled dispensing Federal – Opioid Treatment Program

Typical Clinic

Methadone Maintenance Therapy “MMT” The patient remains physically dependent on an opioid but is freed from the uncontrolled, compulsive & disruptive behavior. - Improved subjects health - Decreased criminal activity - Increased employment

Opioid Antagonist: Naltrexone Opioid Blockade FDA Approved for Alcohol Prevents relapse Strong Anti-Craving Minimized overdose risk; especially after detox Highly Motivated Does not want agonist therapy
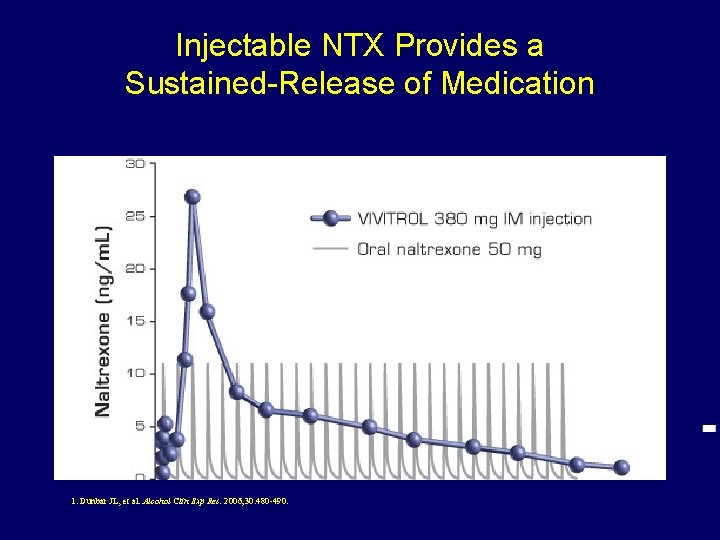
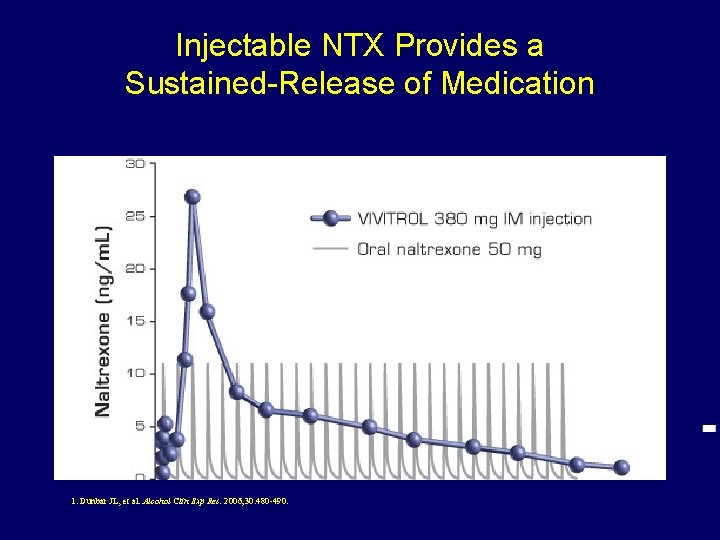
Injectable NTX Provides a Sustained-Release of Medication 1. Dunbar JL, et al. Alcohol Clin Exp Res. 2006; 30: 480 -490. 33

IM Naltrexone Eliminates Daily Adherence Decisions 1 • Naltrexone utilizes a delivery system that – Provides a month of medication in a single dose • Adherence to any treatment program is essential for successful outcomes • Administration by a healthcare provider ensures that the patient receives the medication as directed “…addressing patient adherence systematically will 2 maximize the effectiveness of these medications. ” 1. Dean RL. Front Biosci. 2005; 10: 643 -655. 2. NIAAA. 2007. NIH publication 07 -3769. –Updated NIAAA Clinician’s Guide 34

Buprenorphine (2002)
Overview • Office-based treatment • Physicians prescribing must have certification from DEA (30 -100 pt. Limit) • Manages withdrawal • Used as a maintenance therapy • Limited abuse potential
Pharmacology • Semi-synthetic morphine alkaloid • Partial agonist at mu receptor – Ceiling effects • Antagonist at kappa receptor • Schedule III • Over 20 years of research

Pharmacology • High affinity – Competes with other opioids • Slow dissociation – Prolonged effect • Poor oral bioavailability (1 st pass) • 50 -70% SL bioavailbility • Duration of action – Onset 30 -60 min – Peak 1 -4 hours – Half-life: >30 hours
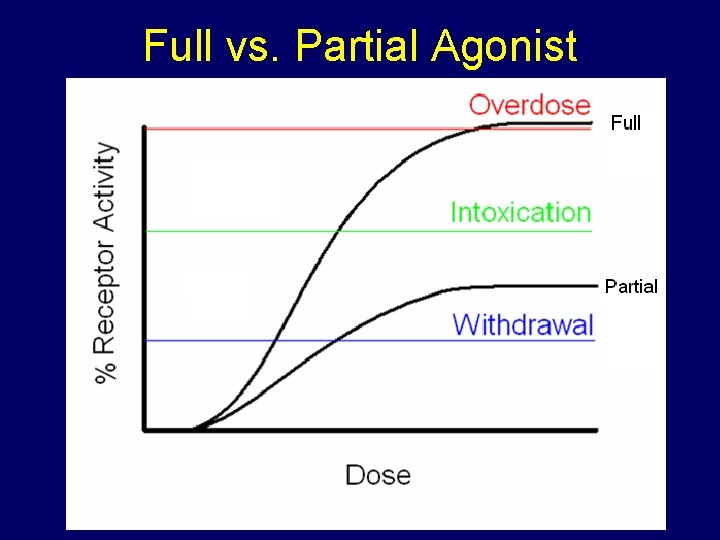
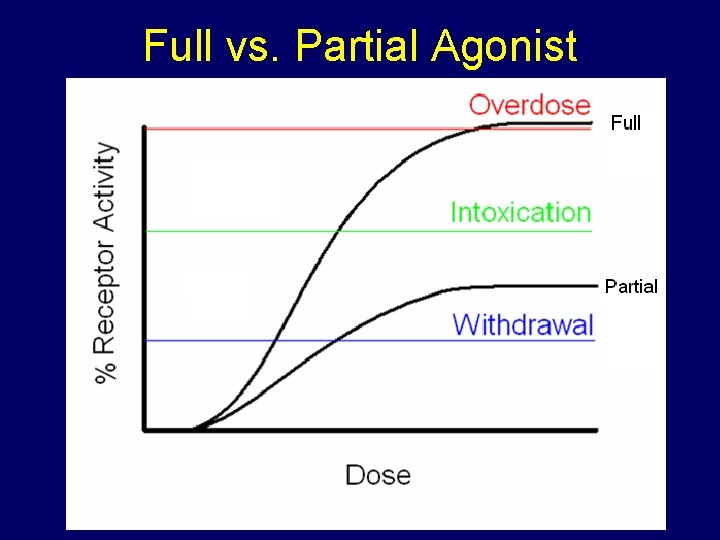
Full vs. Partial Agonist
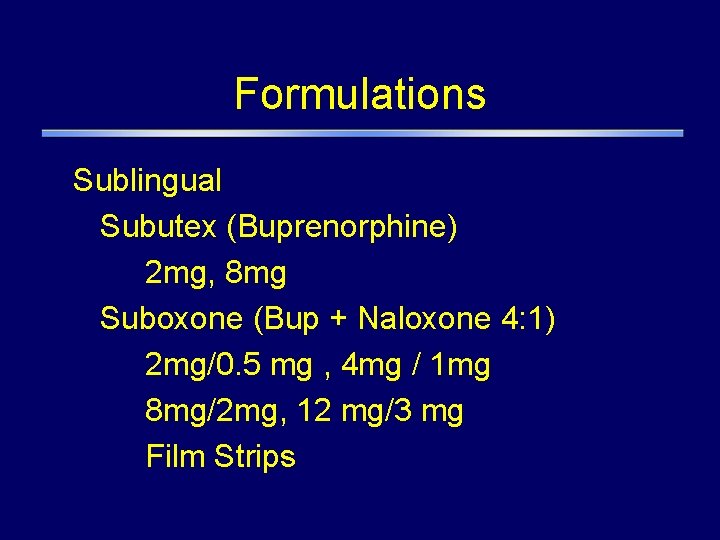
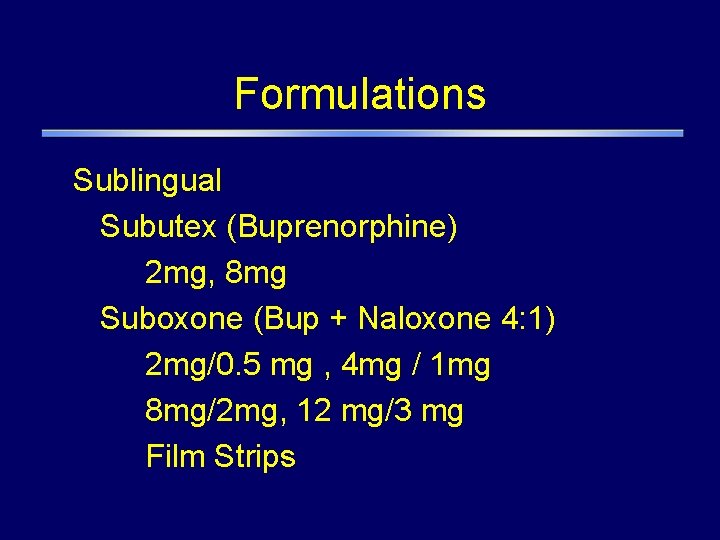
Formulations Sublingual Subutex (Buprenorphine) 2 mg, 8 mg Suboxone (Bup + Naloxone 4: 1) 2 mg/0. 5 mg , 4 mg / 1 mg 8 mg/2 mg, 12 mg/3 mg Film Strips

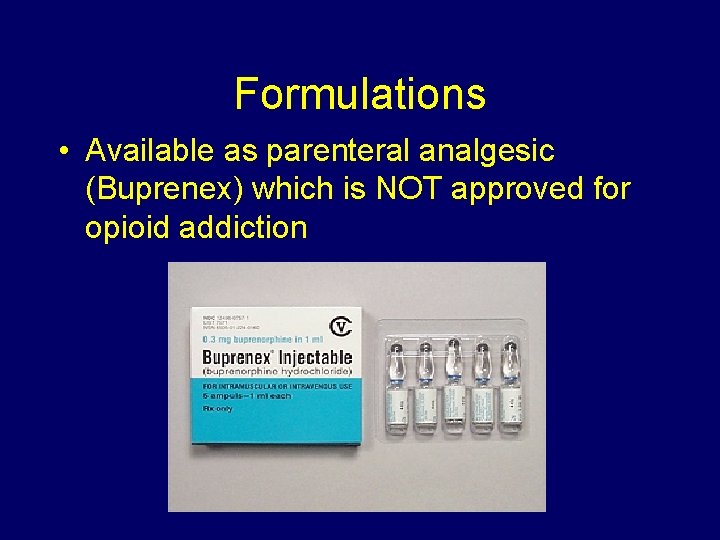
Formulations • Available as parenteral analgesic (Buprenex) which is NOT approved for opioid addiction
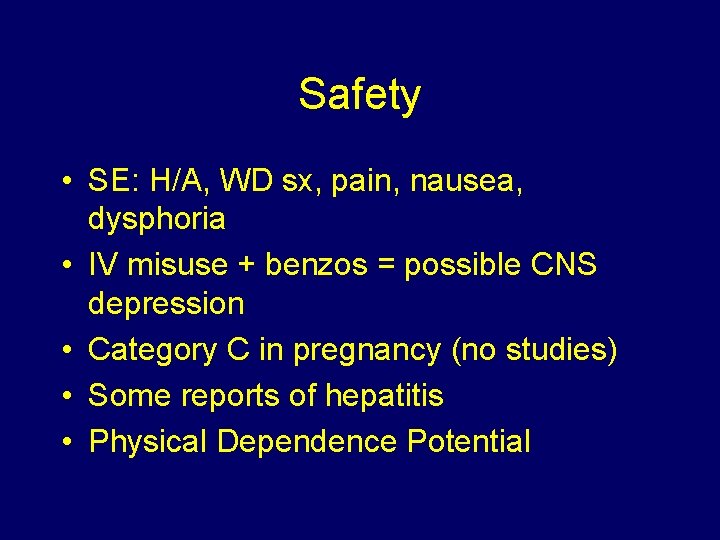
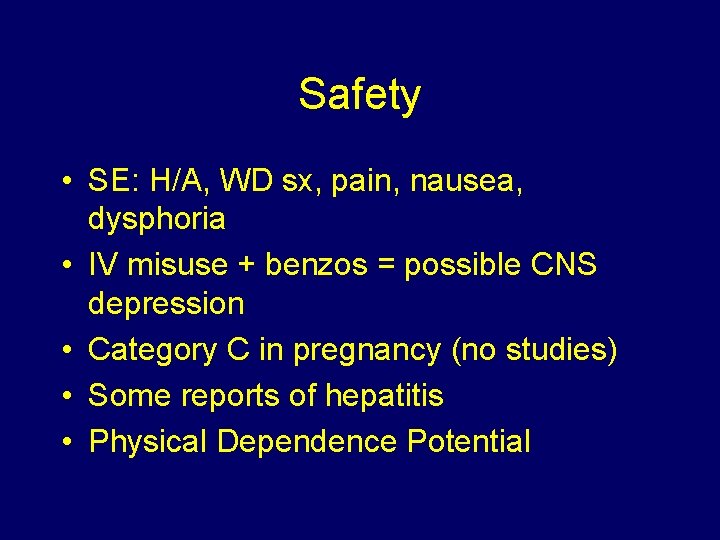
Safety • SE: H/A, WD sx, pain, nausea, dysphoria • IV misuse + benzos = possible CNS depression • Category C in pregnancy (no studies) • Some reports of hepatitis • Physical Dependence Potential
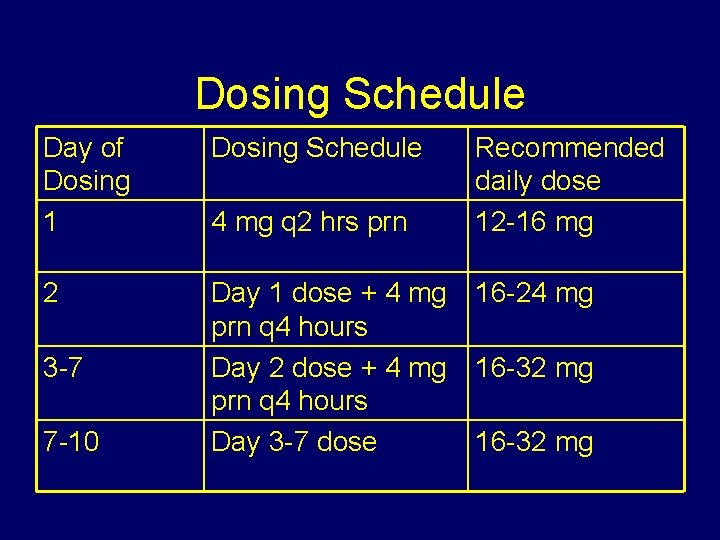
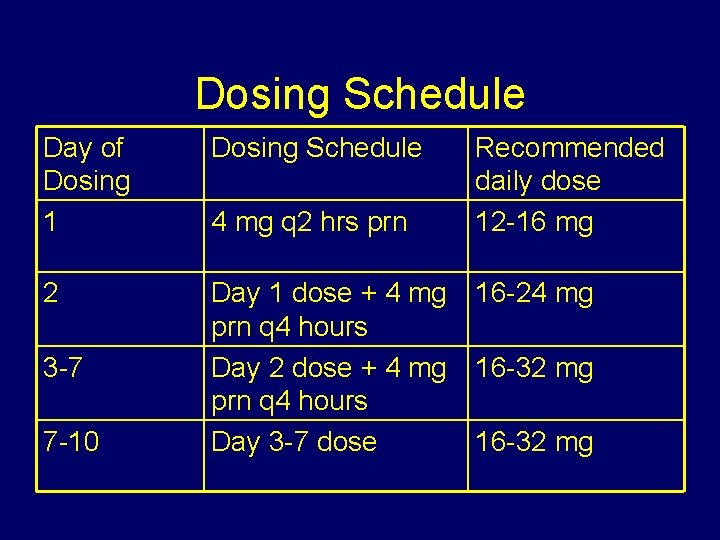
Dosing Schedule Day of Dosing 1 Dosing Schedule 2 Day 1 dose + 4 mg prn q 4 hours Day 2 dose + 4 mg prn q 4 hours Day 3 -7 dose 3 -7 7 -10 4 mg q 2 hrs prn Recommended daily dose 12 -16 mg 16 -24 mg 16 -32 mg
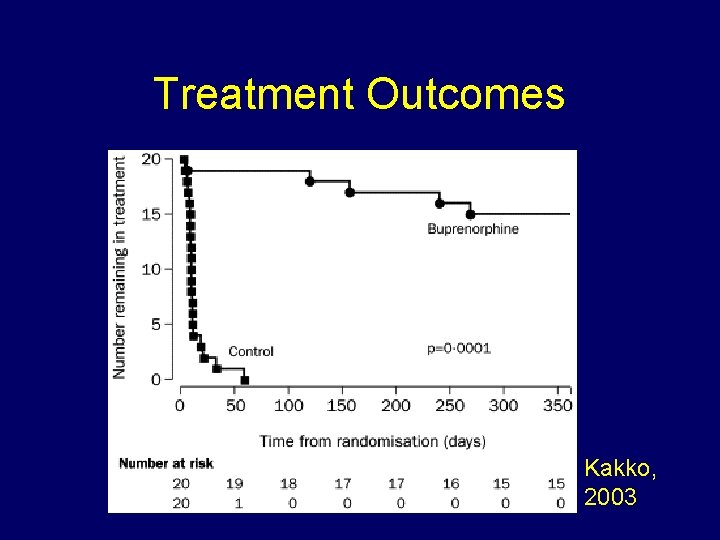
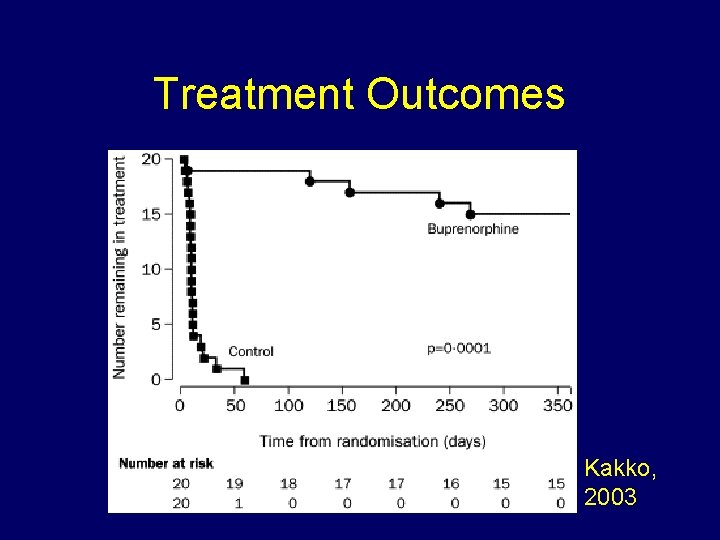
Treatment Outcomes Kakko, 2003
Positive Impact of Medication. Assisted Treatment • ~ 2 million Americans are dependent on opioid prescription painkillers or heroin • Over 900, 000 patients were treated with buprenorphine/naloxone in 2010 • Buprenorphine/naloxone is safe and an effective treatment for opioid dependence • Treatment – is cost-effective – can improve functioning across several psychosocial parameters
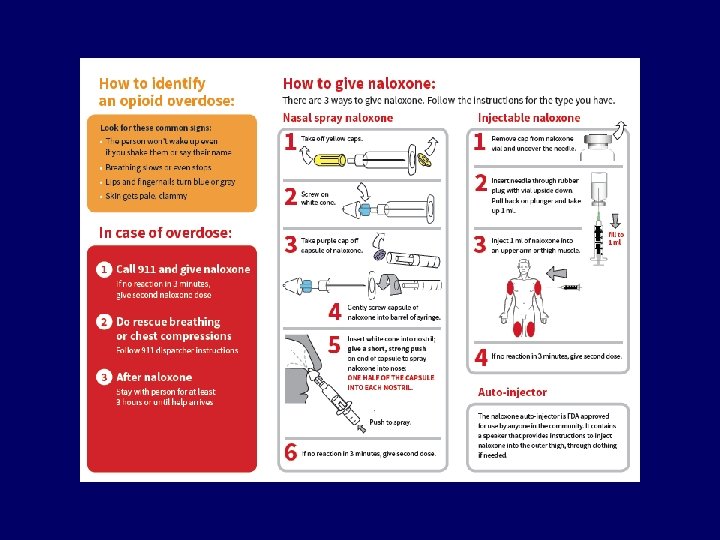
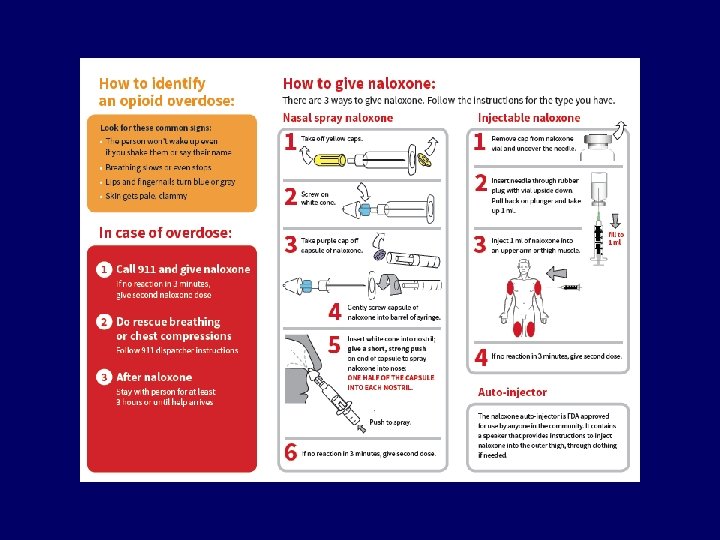
Opioid Overdose • Naloxone – Short acting – Reverses respiratory suppression > opioid analgesia – May require redosing in cases of massive opioid OD – VERY SAFE – non-toxic even at doses multiple x usual dose • No effect if no opioids are present
Overdose Education and Naloxone Distribution (OEND) • Naloxone (injectable and nasal spray) – Reverses opiate overdoses • In early 2015, California law allows pharmacists to distribute naloxone directly to patients
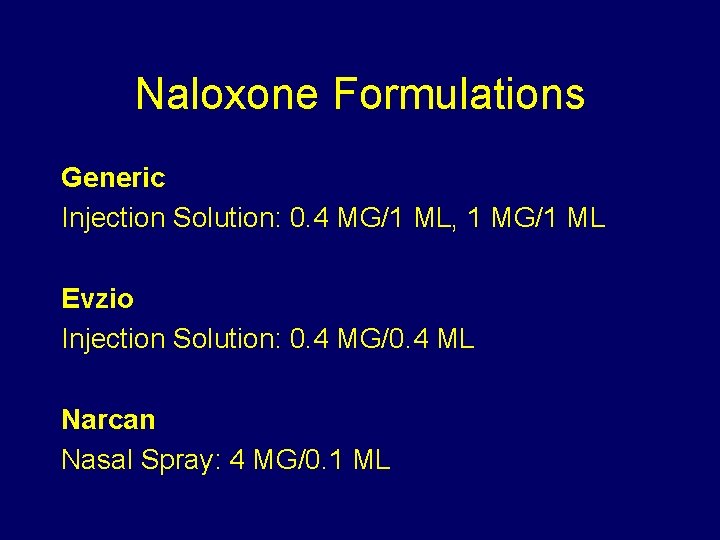
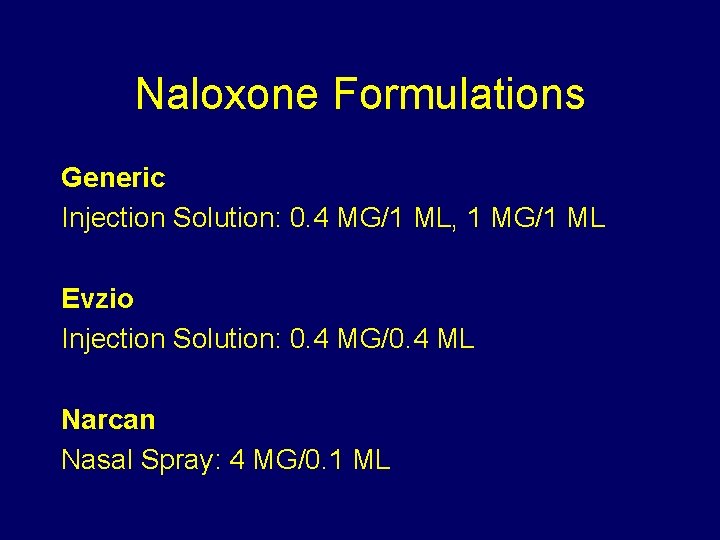
Naloxone Formulations Generic Injection Solution: 0. 4 MG/1 ML, 1 MG/1 ML Evzio Injection Solution: 0. 4 MG/0. 4 ML Narcan Nasal Spray: 4 MG/0. 1 ML
Provider Toolbox

Controlled Substance Utilization Review and Evaluation System (CURES)

Proper Drug Disposal (DEA/FDA) 1. Medicine Take Back Programs 2. Transfer to DEA-authorized collection sites 3. Dispose in Trash Mix with unpalatable substance, seal, throw, de-identify 4. FLUSH Controlled Substances!
CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016

Treatment Referrals • SAMHSA Treatment Locator – http: //findtreatment. samhsa. gov – 1 -800 -662 -HELP • NIDA Clinical Trials Network – www. drugabuse. gov • American Academy of Addiction Psychiatry • American Society of Addiction Medicine
Further Reading • National Institute on Drug Abuse – www. nida. nih. gov • American Academy of Addiction Psychiatry – www. aaap. org • Substance Abuse and Mental Health Service Administration – www. samhsa. gov

Contact Information Timothy Fong MD UCLA Addiction Medicine Clinic 310 -825 -9989 (appts) 310 -825 -1479 (office) tfong@mednet. ucla. edu uclagamblingprogram. org
 Medication assisted treatment colorado
Medication assisted treatment colorado Epidemic broadcast trees
Epidemic broadcast trees Toxinq
Toxinq Gondhli millet
Gondhli millet Doctors attributed the epidemic to the rampant
Doctors attributed the epidemic to the rampant Endemic epidemic
Endemic epidemic Aids epidemic
Aids epidemic Endemic epidemic
Endemic epidemic Epidemiological transition model
Epidemiological transition model Rass vs poss
Rass vs poss Aldolan
Aldolan Opiate tabelle
Opiate tabelle Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Types of pain
Types of pain Mechanism of action of opioid analgesics
Mechanism of action of opioid analgesics Elisha peterson md
Elisha peterson md Opioid receptors location
Opioid receptors location Brian erickson md
Brian erickson md Equianalgesia
Equianalgesia Non-opioid
Non-opioid Kentucky opioid response effort
Kentucky opioid response effort Chapter 27 nutritional therapy and assisted feeding
Chapter 27 nutritional therapy and assisted feeding Disadvantages of russian service
Disadvantages of russian service What is call computer assisted language learning
What is call computer assisted language learning Hidden costs of assisted living
Hidden costs of assisted living Robot assisted surgery
Robot assisted surgery Microwave assisted extraction
Microwave assisted extraction Laser assisted bonding
Laser assisted bonding Models of ltm - frames
Models of ltm - frames Floridahealthfinder.gov facility locator tool
Floridahealthfinder.gov facility locator tool Oedmodo
Oedmodo Contoh computer assisted instruction
Contoh computer assisted instruction Assisted picking
Assisted picking Manual assisted cough
Manual assisted cough What part
What part Park place seattle assisted living
Park place seattle assisted living Information reproduced from memory can be assisted by cues.
Information reproduced from memory can be assisted by cues. Assisted referral tool
Assisted referral tool Virtualization techniques in cloud computing
Virtualization techniques in cloud computing Eno pointe assisted living reviews
Eno pointe assisted living reviews Static exercises definition
Static exercises definition Computer assisted passenger prescreening system
Computer assisted passenger prescreening system Thanks for the rescue
Thanks for the rescue Laser-assisted uvulopalatoplasty
Laser-assisted uvulopalatoplasty Computer assisted guidance systems
Computer assisted guidance systems Peer assisted
Peer assisted Online proctored exams candidate guidelines peoplecert
Online proctored exams candidate guidelines peoplecert Computer assisted audit techniques slideshare
Computer assisted audit techniques slideshare Georgia assisted living association
Georgia assisted living association Florida health finder.gov
Florida health finder.gov Hydrogen assisted cracking
Hydrogen assisted cracking Computer aided teaching
Computer aided teaching Protea senior living
Protea senior living Base case system evaluation
Base case system evaluation Field assisted sintering technology
Field assisted sintering technology Assisted suicide
Assisted suicide