The NUTRIC Score An ICU Nutrition Screening Tool
- Slides: 42
The NUTRIC Score: An ICU Nutrition Screening Tool Rupinder Dhaliwal, RD Nutrition & Rehabilitation Investigator’s Consortium Clinical Evaluation Research Unit Kingston General Hospital
Conflict of interest I have received speaker honoraria and/or I have been paid from grants from the following companies: – Nestlé Canada – Fresenius Kabi AG – Baxter – Abbott Laboratories
Outline ü incidence of underfeeding in the ICU ü nutritional screening tools available for use in ICU ü familiar with the novel approach used to assess the nutritional risk of critically ill patients and implications of this risk assessment for clinical practice.
Health Care Associated Malnutrition “The Skeleton in the Hospital Closet, ” by Charles Butterworth 1974 Does iatrogenic underfeeding exist in the ICU today?
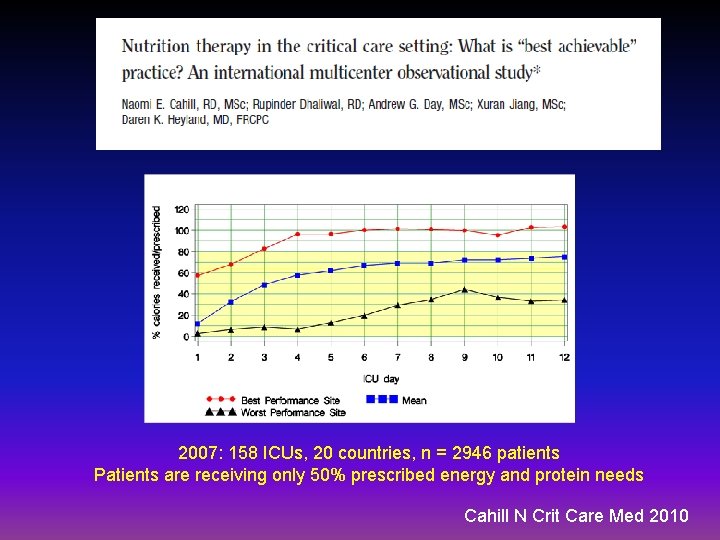
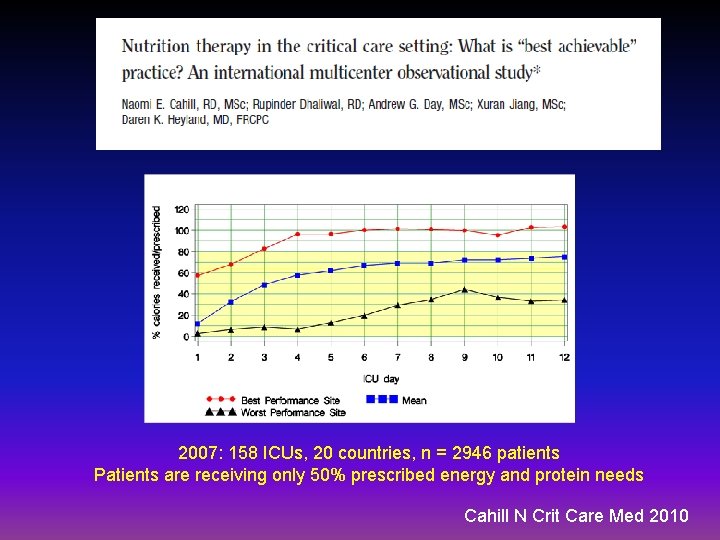
2007: 158 ICUs, 20 countries, n = 2946 patients Patients are receiving only 50% prescribed energy and protein needs Cahill N Crit Care Med 2010
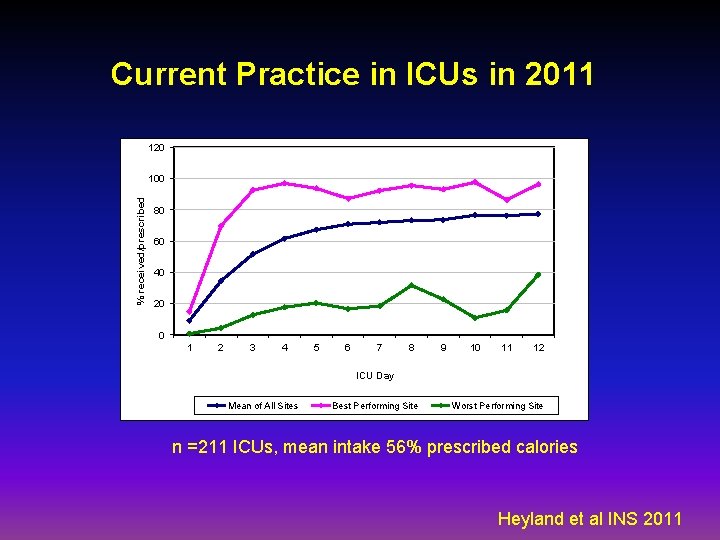
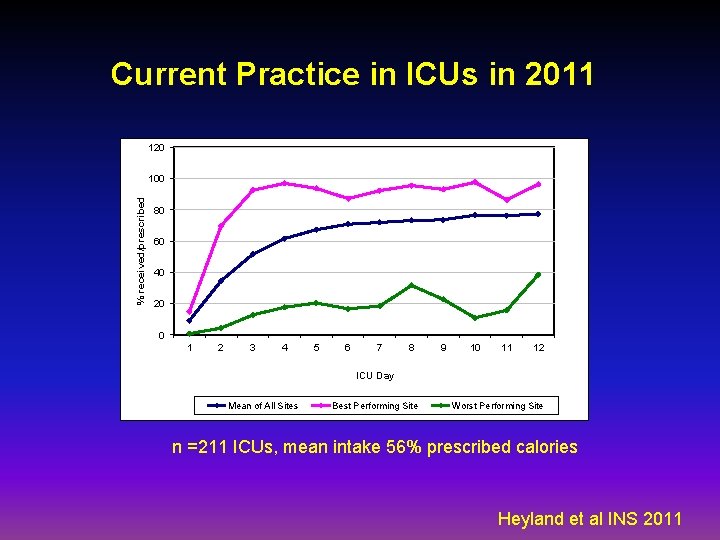
Current Practice in ICUs in 2011 120 % received/prescribed 100 80 60 40 20 0 1 2 3 4 5 6 7 8 9 10 11 12 ICU Day Mean of All Sites Best Performing Site Worst Performing Site n =211 ICUs, mean intake 56% prescribed calories Heyland et al INS 2011
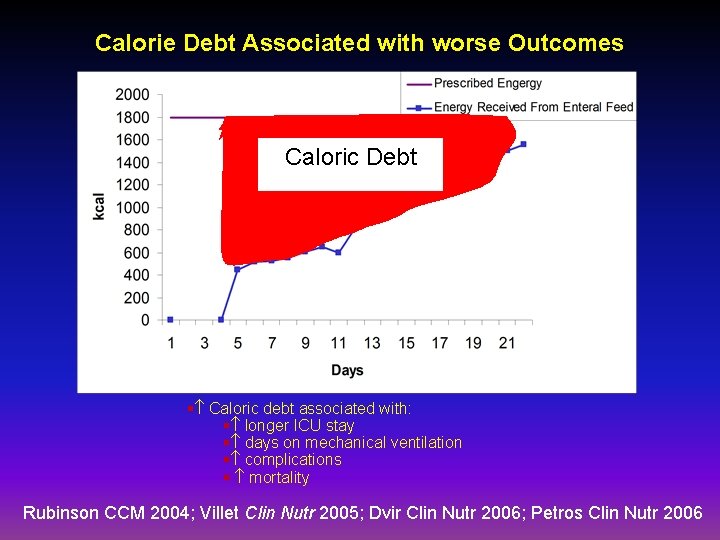
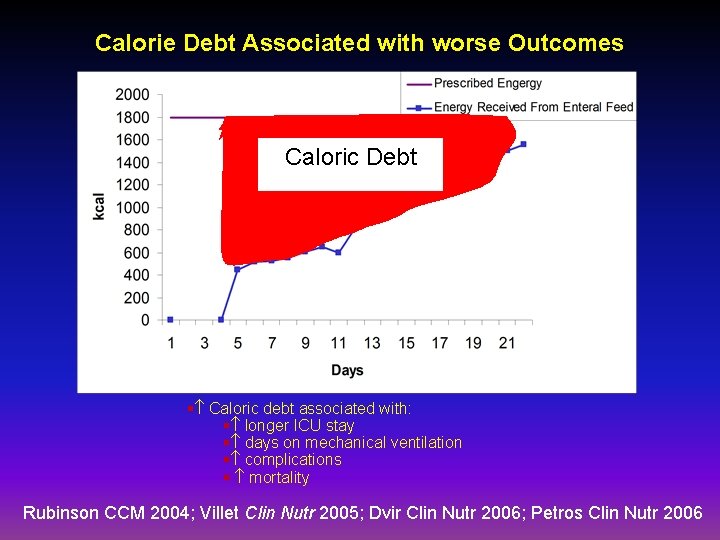
Calorie Debt Associated with worse Outcomes Caloric Debt § Caloric debt associated with: § longer ICU stay § days on mechanical ventilation § complications § mortality Rubinson CCM 2004; Villet Clin Nutr 2005; Dvir Clin Nutr 2006; Petros Clin Nutr 2006
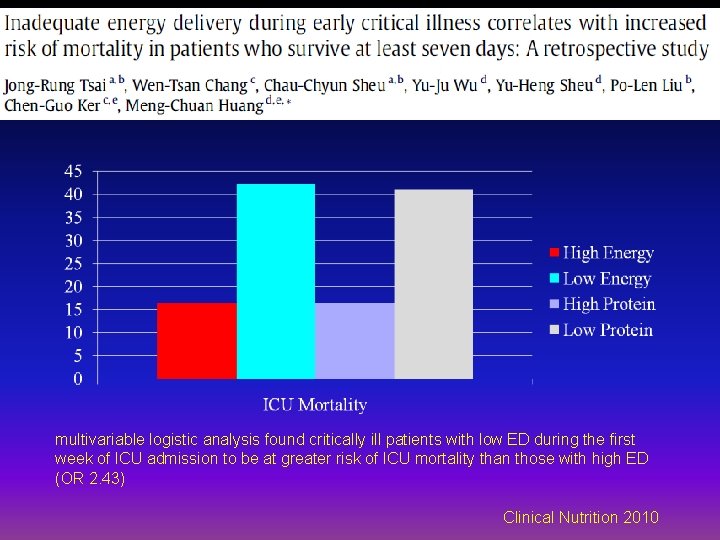
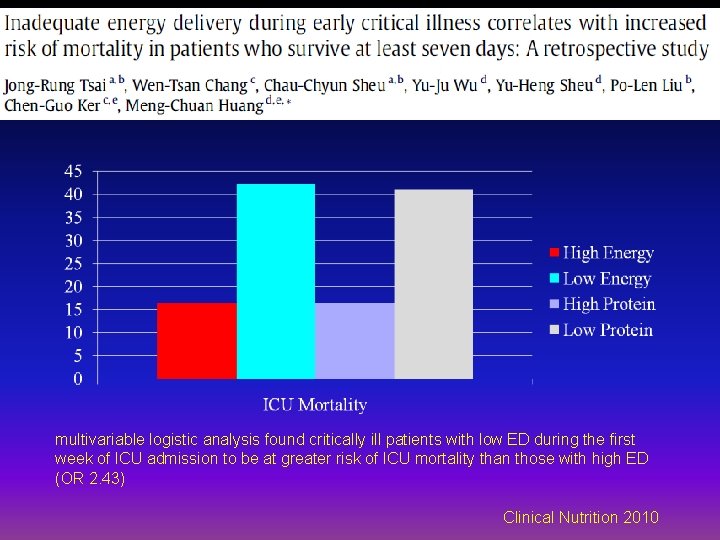
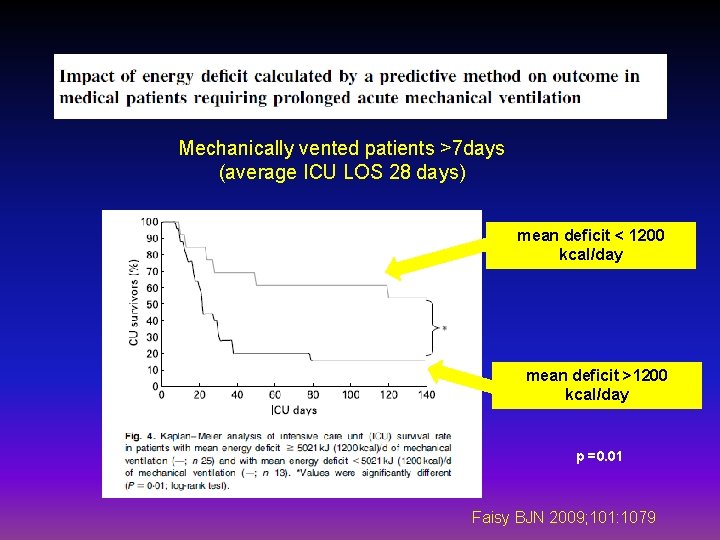
multivariable logistic analysis found critically ill patients with low ED during the first week of ICU admission to be at greater risk of ICU mortality than those with high ED (OR 2. 43) Clinical Nutrition 2010
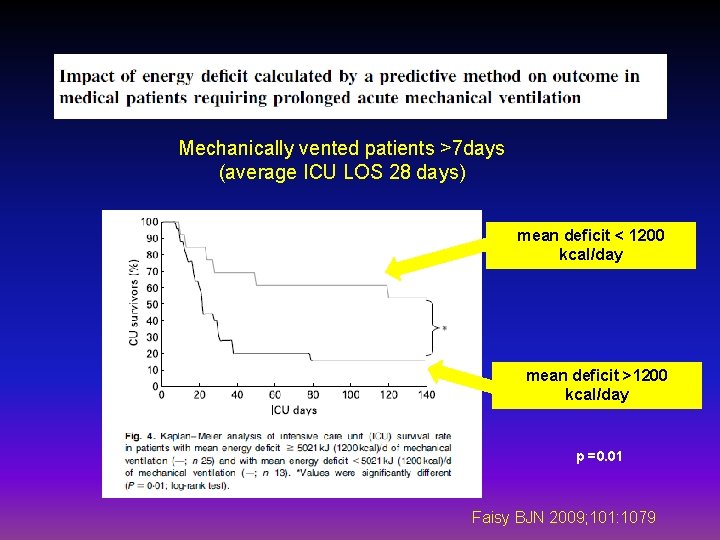
Mechanically vented patients >7 days (average ICU LOS 28 days) mean deficit < 1200 kcal/day mean deficit >1200 kcal/day p =0. 01 Faisy BJN 2009; 101: 1079
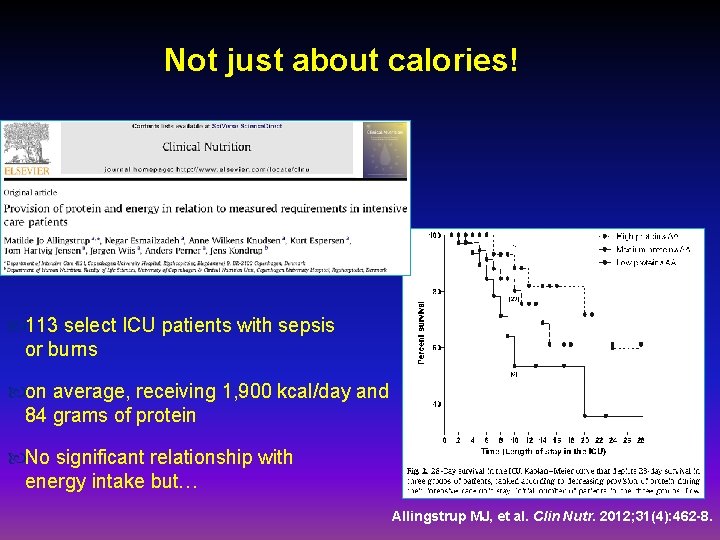
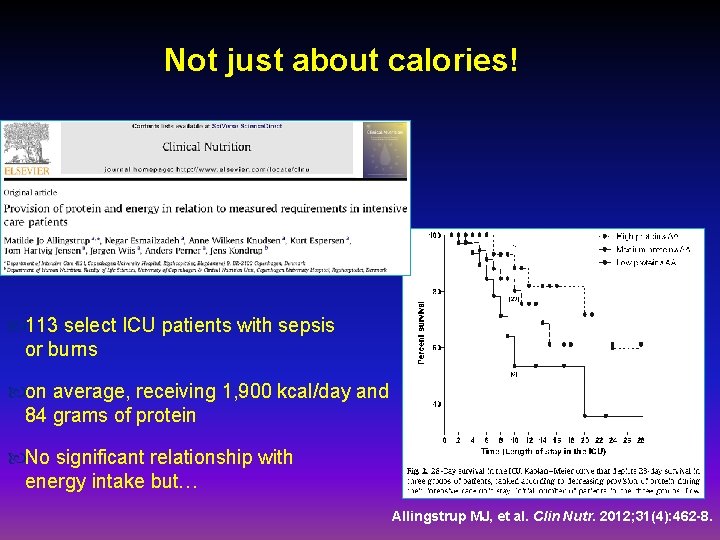
Not just about calories! 113 select ICU patients with sepsis or burns on average, receiving 1, 900 kcal/day and 84 grams of protein No significant relationship with energy intake but… Allingstrup MJ, et al. Clin Nutr. 2012; 31(4): 462 -8.
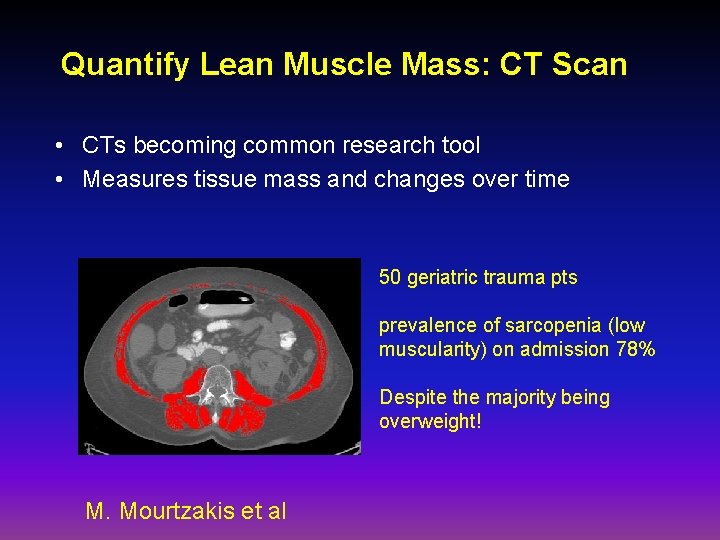
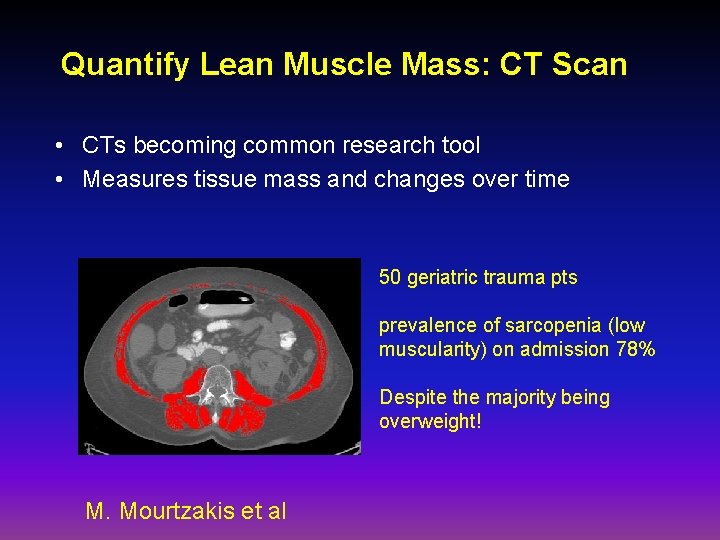
Quantify Lean Muscle Mass: CT Scan • CTs becoming common research tool • Measures tissue mass and changes over time 50 geriatric trauma pts prevalence of sarcopenia (low muscularity) on admission 78% Despite the majority being overweight! M. Mourtzakis et al
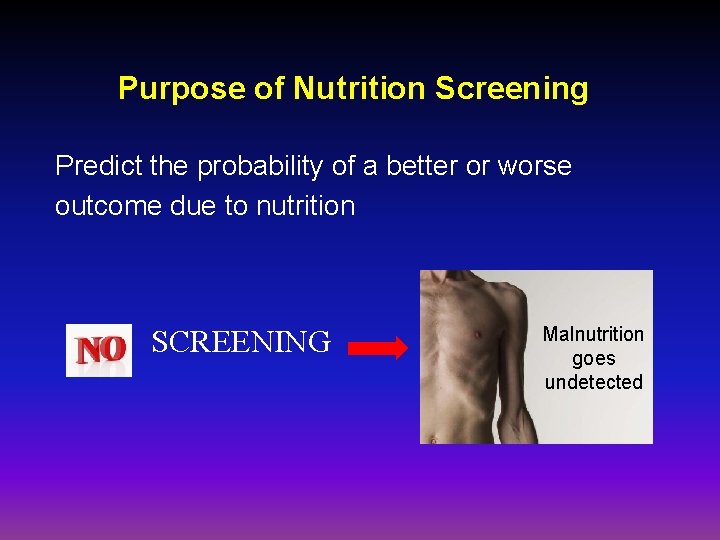
Purpose of Nutrition Screening Predict the probability of a better or worse outcome due to nutrition SCREENING Malnutrition goes undetected
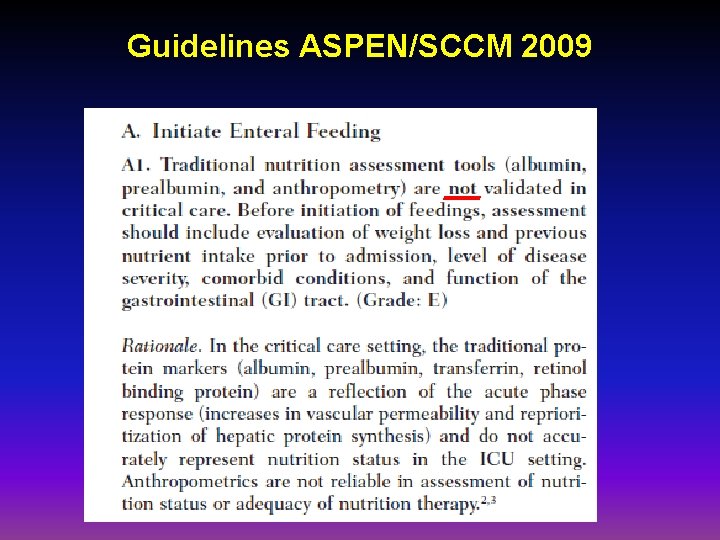
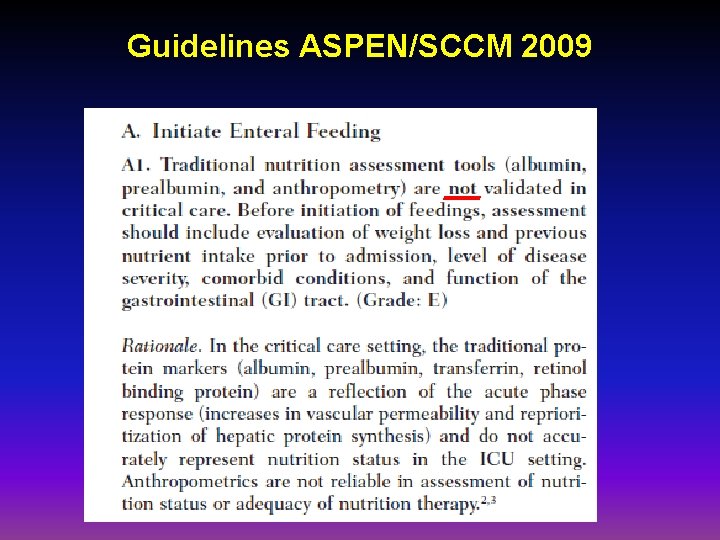
Guidelines ASPEN/SCCM 2009
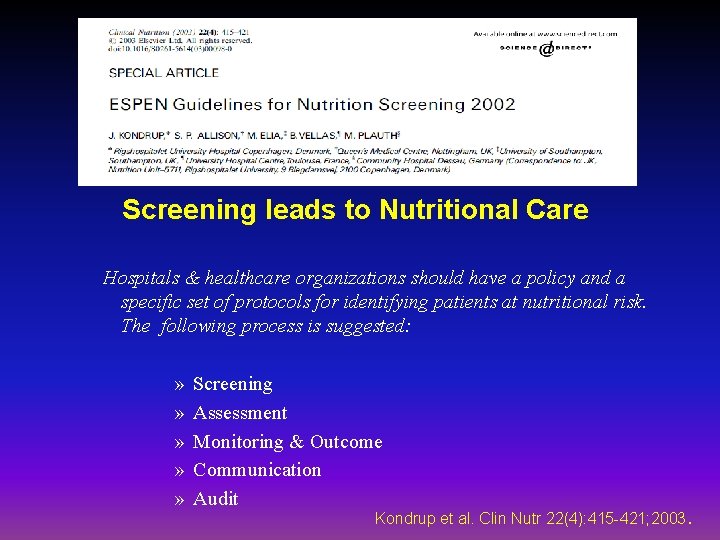
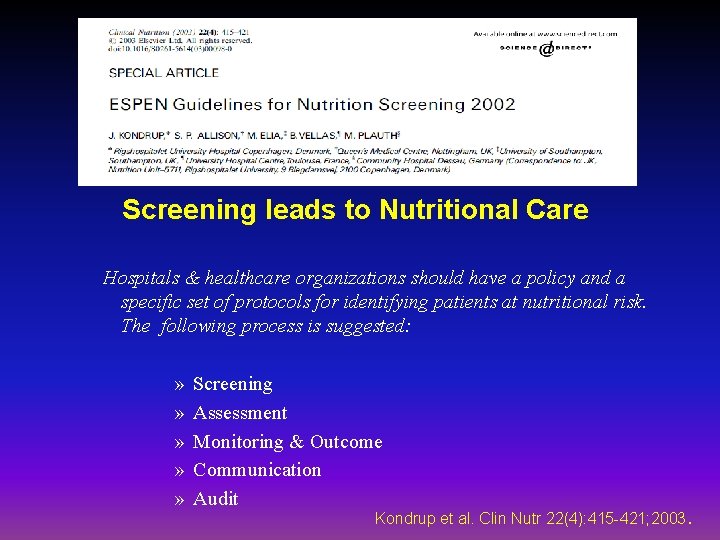
Screening leads to Nutritional Care Hospitals & healthcare organizations should have a policy and a specific set of protocols for identifying patients at nutritional risk. The following process is suggested: » » » Screening Assessment Monitoring & Outcome Communication Audit Kondrup et al. Clin Nutr 22(4): 415 -421; 2003.
ü Underfeeding does occur in ICUs ü Prevalence of sarcopenia • Existing tools for nutrition screening in ICU
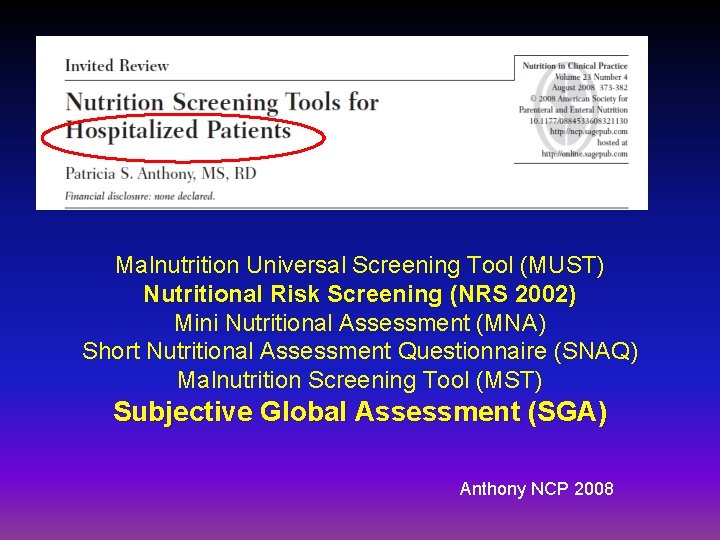
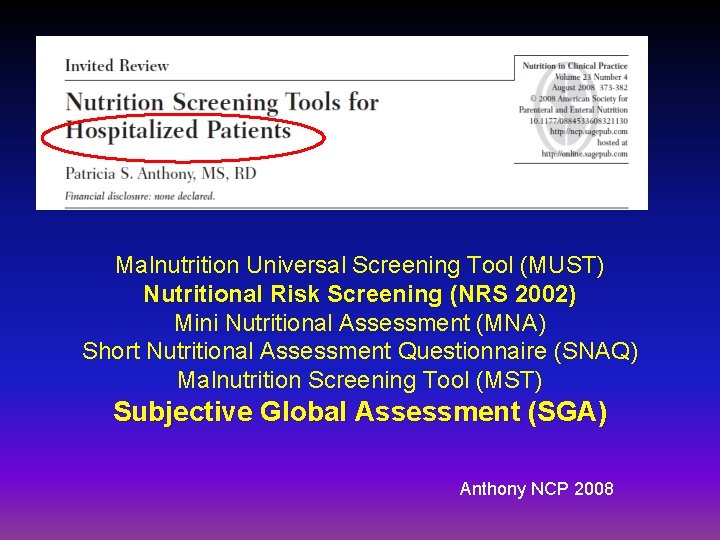
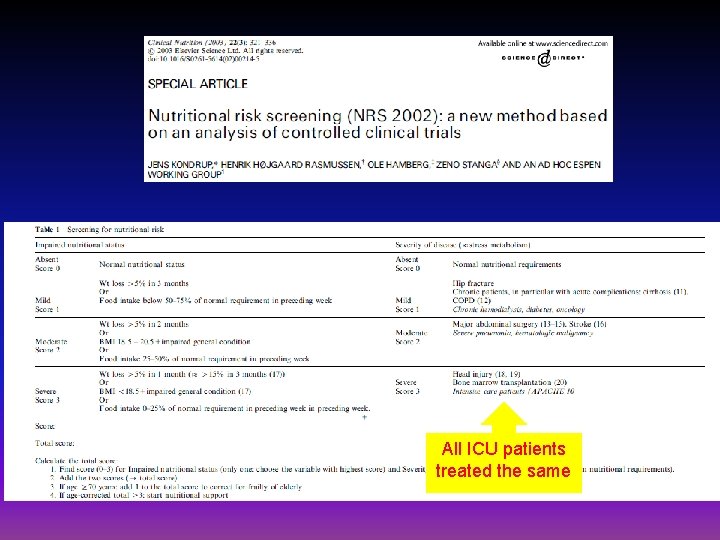
Malnutrition Universal Screening Tool (MUST) Nutritional Risk Screening (NRS 2002) Mini Nutritional Assessment (MNA) Short Nutritional Assessment Questionnaire (SNAQ) Malnutrition Screening Tool (MST) Subjective Global Assessment (SGA) Anthony NCP 2008
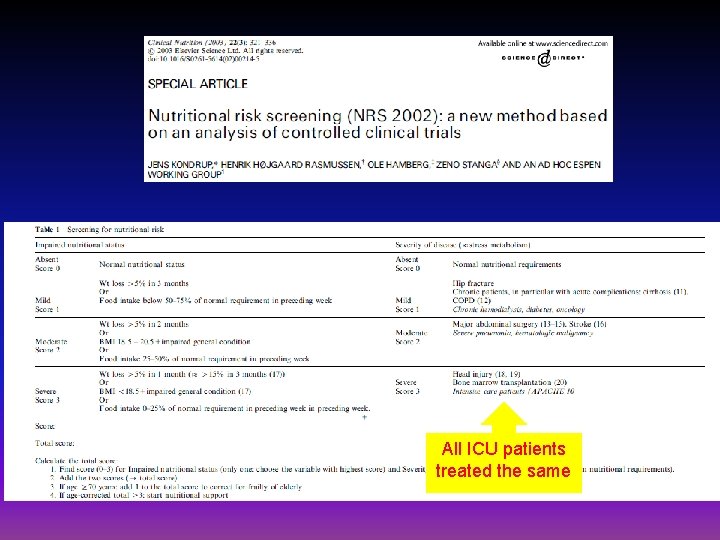
All ICU patients treated the same
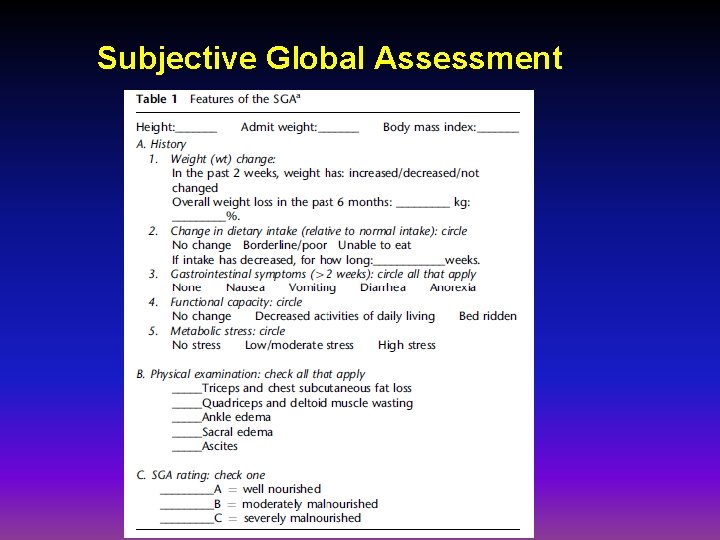
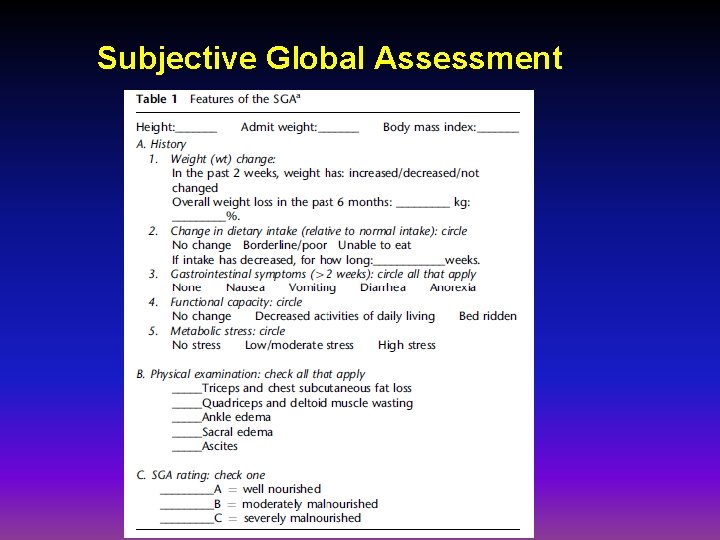
Subjective Global Assessment
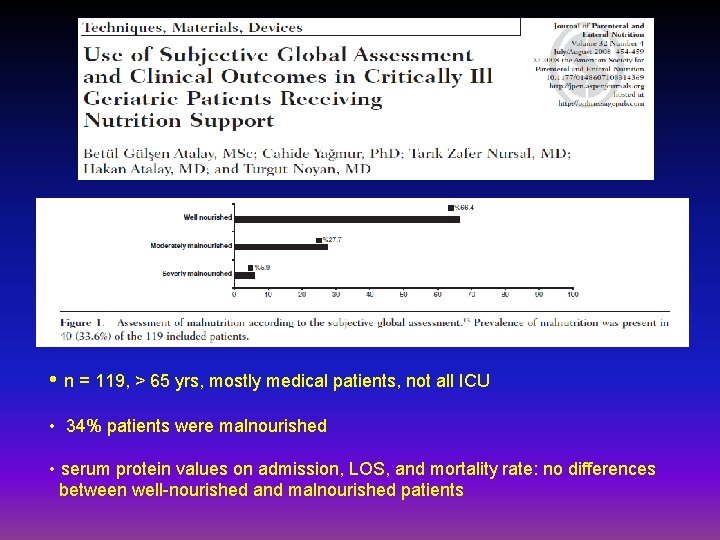
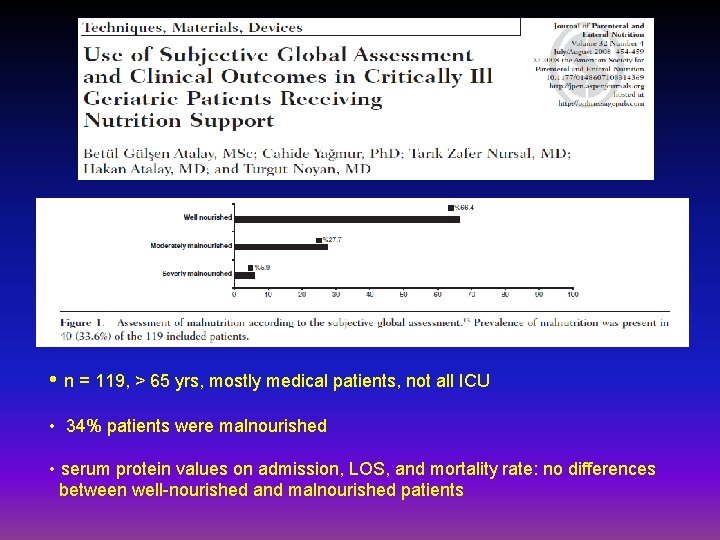
• n = 119, > 65 yrs, mostly medical patients, not all ICU • 34% patients were malnourished • serum protein values on admission, LOS, and mortality rate: no differences between well-nourished and malnourished patients
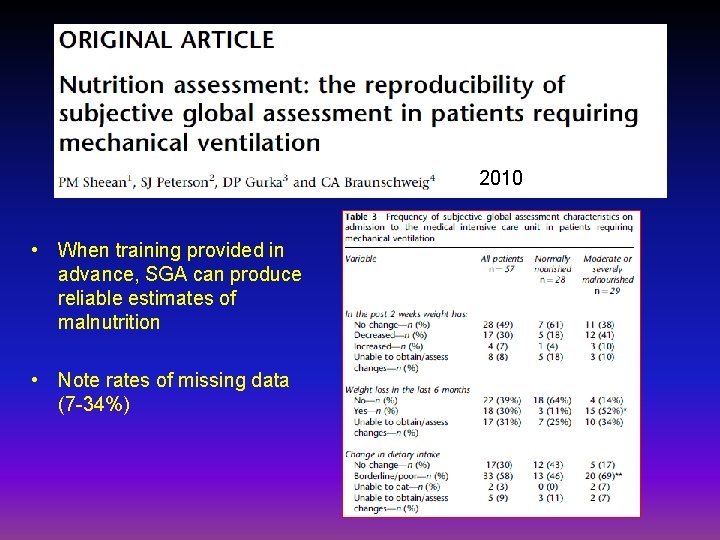
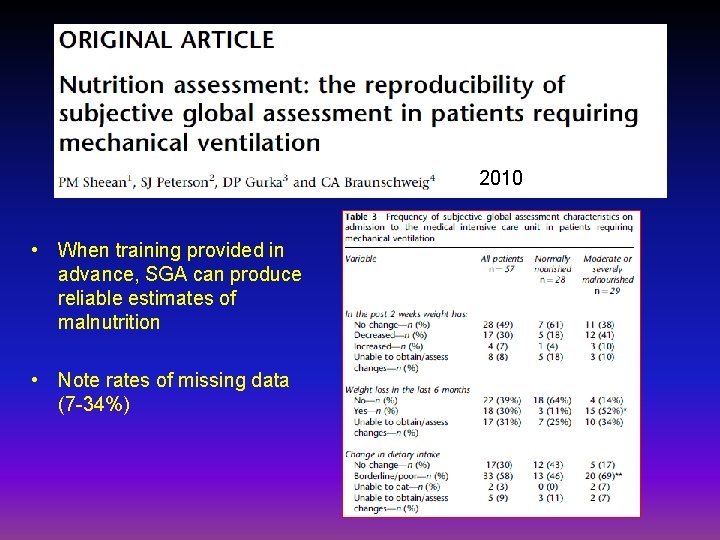
2010 • When training provided in advance, SGA can produce reliable estimates of malnutrition • Note rates of missing data (7 -34%)
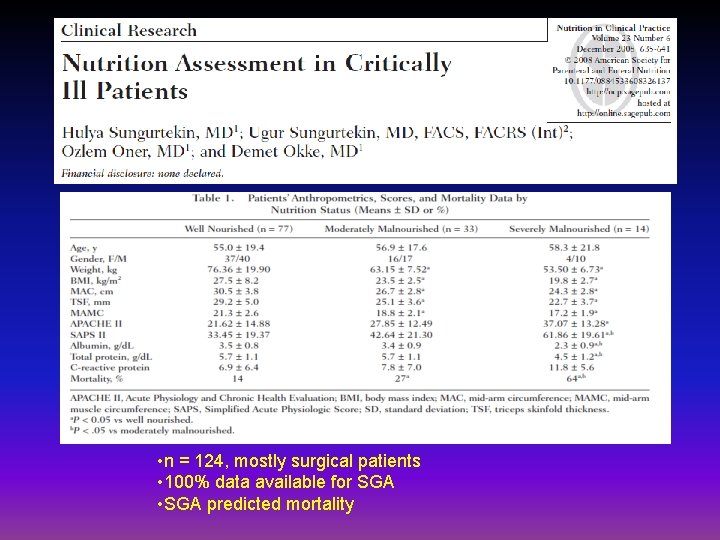
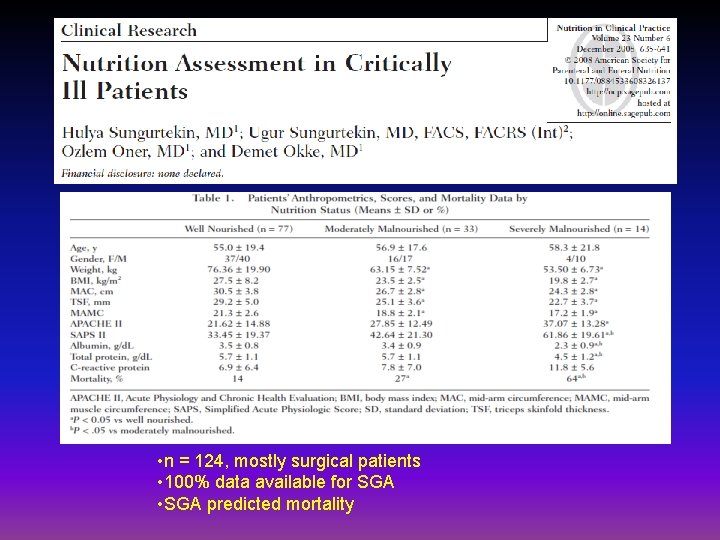
• n = 124, mostly surgical patients • 100% data available for SGA • SGA predicted mortality
ICU patients are not all created equal…should not expect all patients to respond to the same nutrition therapy
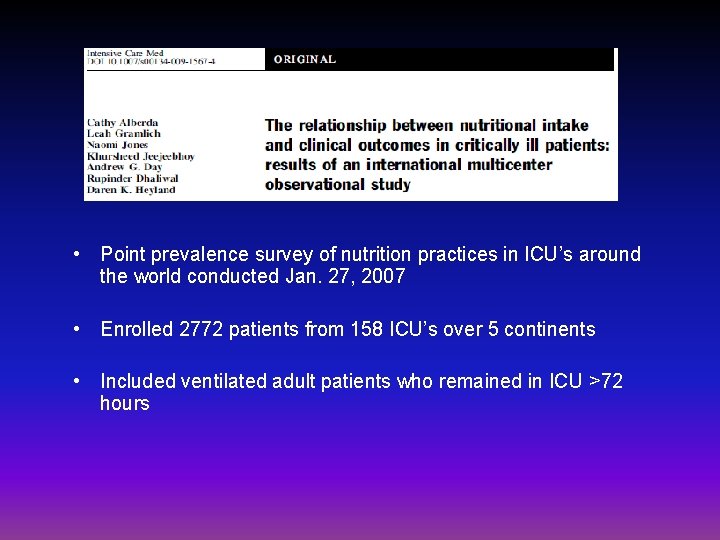
• Point prevalence survey of nutrition practices in ICU’s around the world conducted Jan. 27, 2007 • Enrolled 2772 patients from 158 ICU’s over 5 continents • Included ventilated adult patients who remained in ICU >72 hours
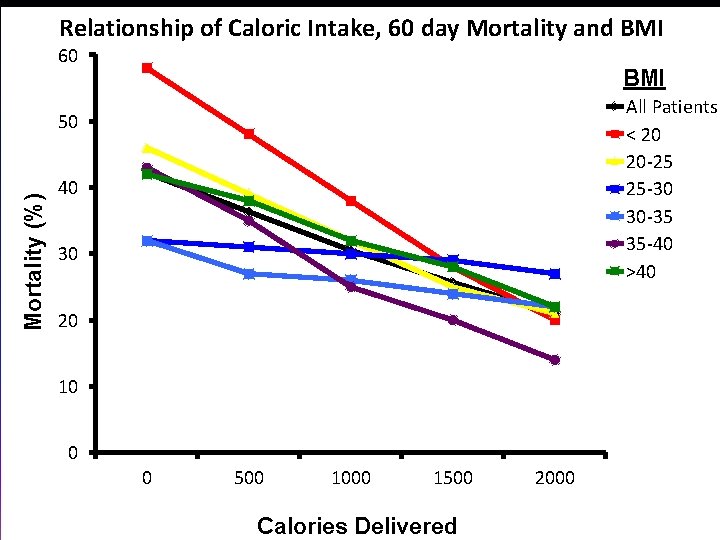
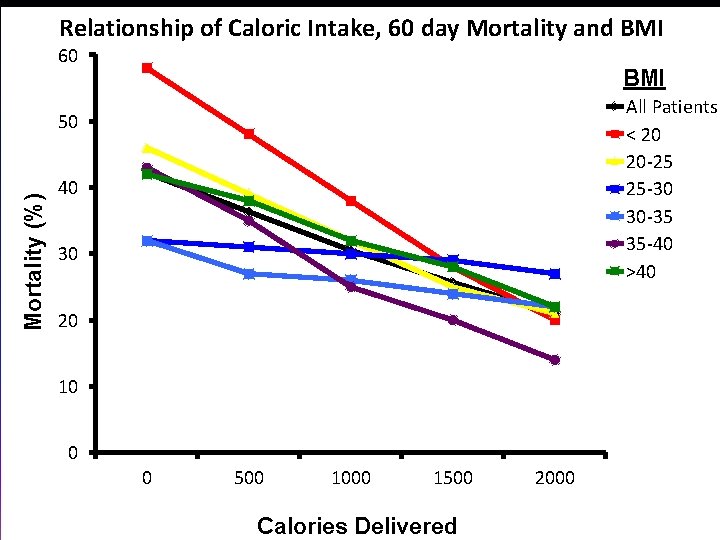
Relationship of Caloric Intake, 60 day Mortality and BMI 60 BMI All Patients < 20 20 -25 25 -30 30 -35 35 -40 >40 Mortality (%) 50 40 30 20 10 0 0 500 1000 1500 Calories Delivered 2000
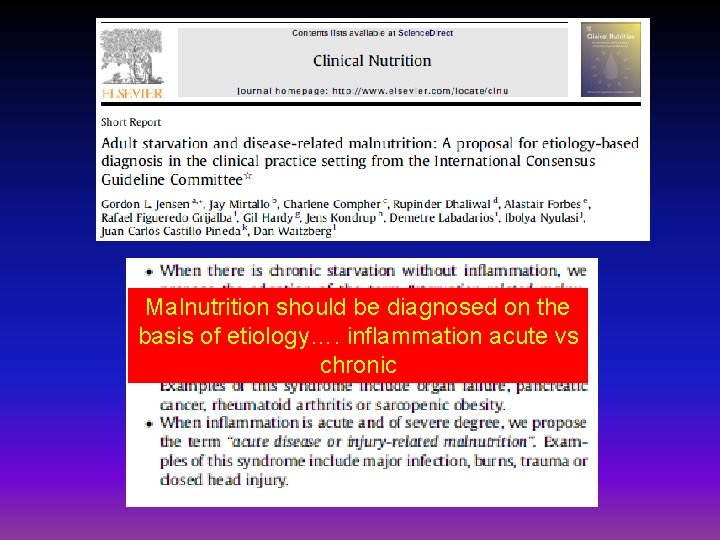
Malnutrition should be diagnosed on the basis of etiology…. inflammation acute vs chronic
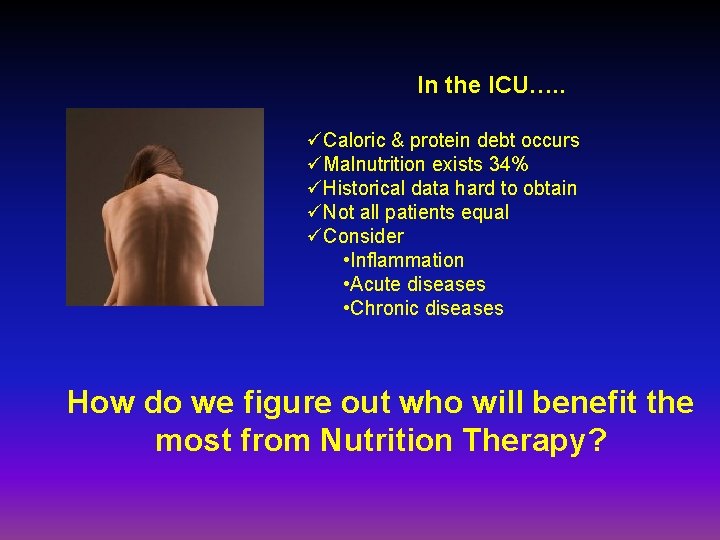
In the ICU…. . üCaloric & protein debt occurs üMalnutrition exists 34% üHistorical data hard to obtain üNot all patients equal üConsider • Inflammation • Acute diseases • Chronic diseases How do we figure out who will benefit the most from Nutrition Therapy?
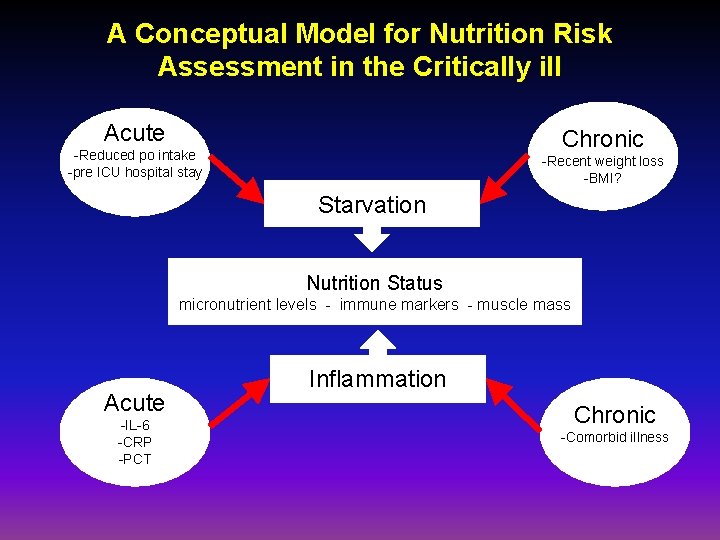
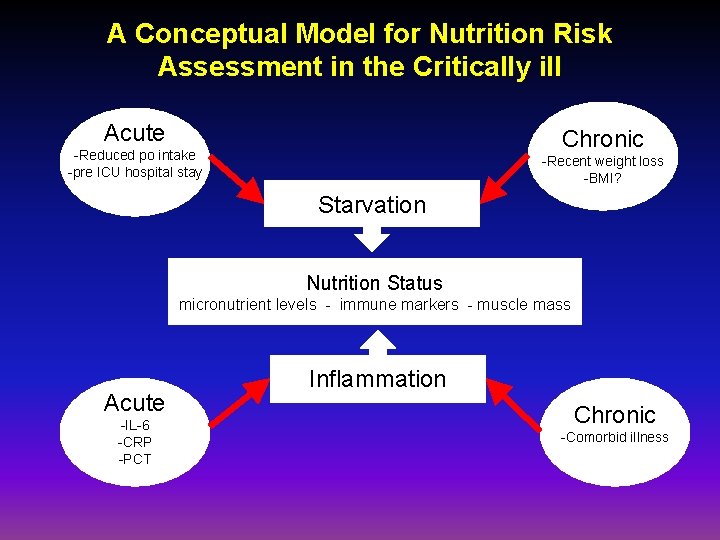
A Conceptual Model for Nutrition Risk Assessment in the Critically ill Acute Chronic -Reduced po intake -pre ICU hospital stay -Recent weight loss -BMI? Starvation Nutrition Status micronutrient levels - immune markers - muscle mass Acute -IL-6 -CRP -PCT Inflammation Chronic -Comorbid illness
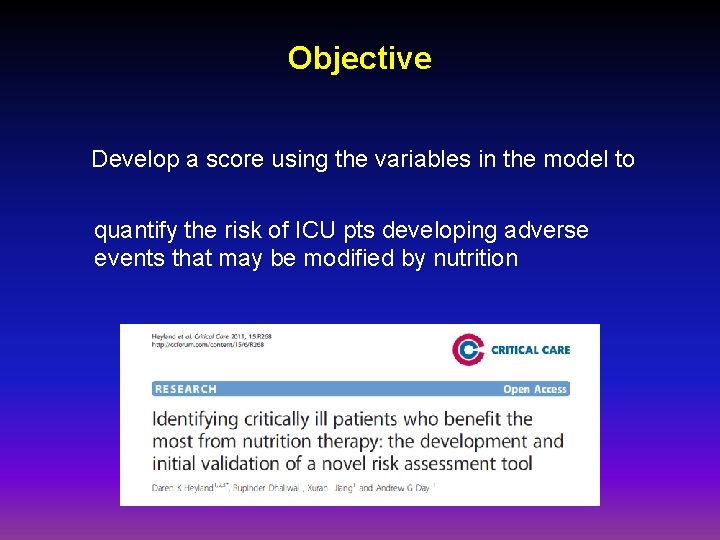
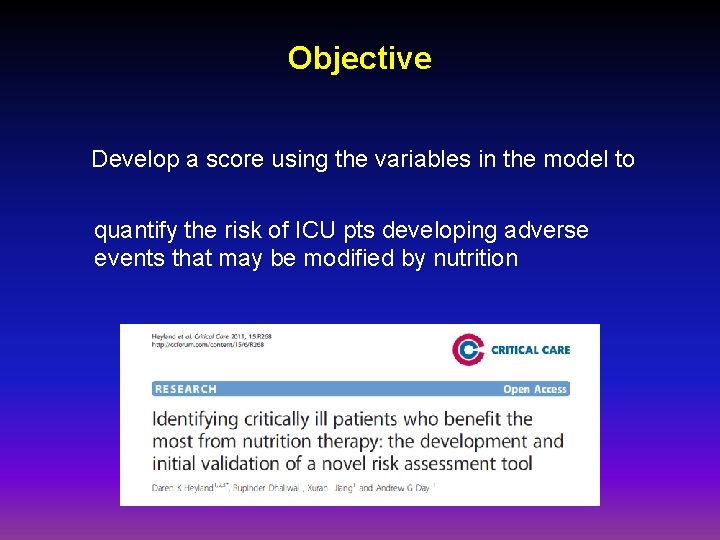
Objective Develop a score using the variables in the model to quantify the risk of ICU pts developing adverse events that may be modified by nutrition
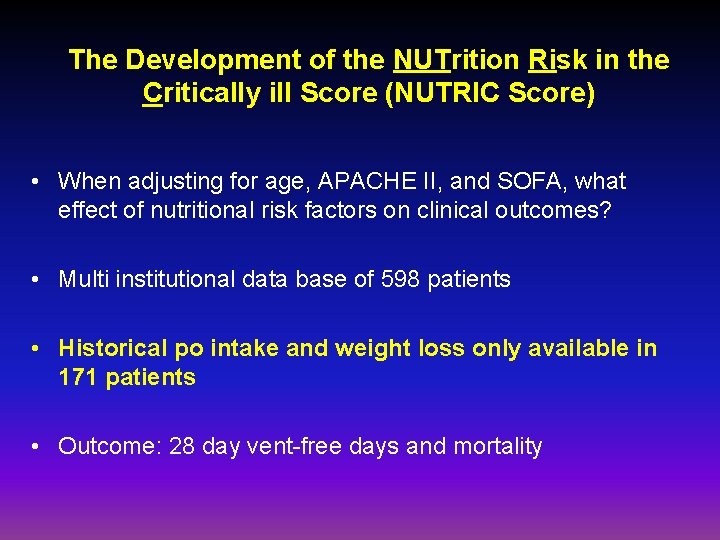
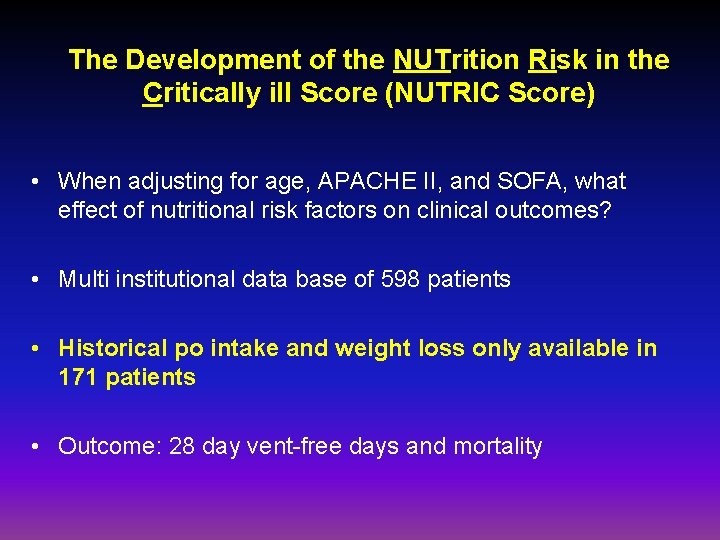
The Development of the NUTrition Risk in the Critically ill Score (NUTRIC Score) • When adjusting for age, APACHE II, and SOFA, what effect of nutritional risk factors on clinical outcomes? • Multi institutional data base of 598 patients • Historical po intake and weight loss only available in 171 patients • Outcome: 28 day vent-free days and mortality
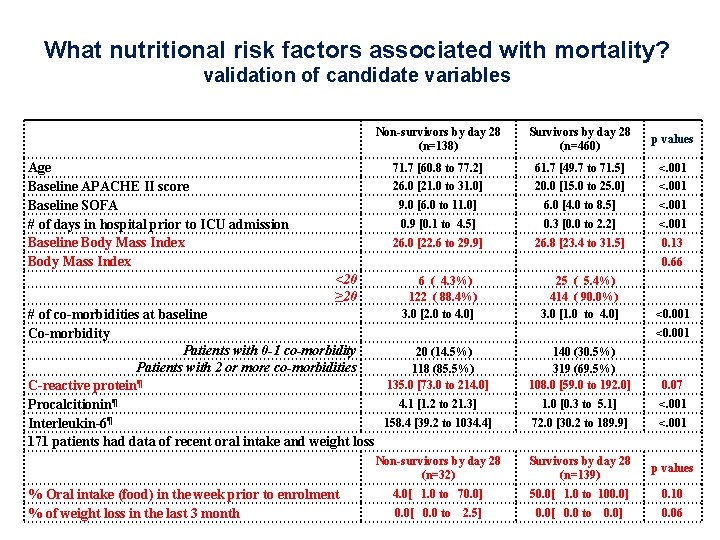
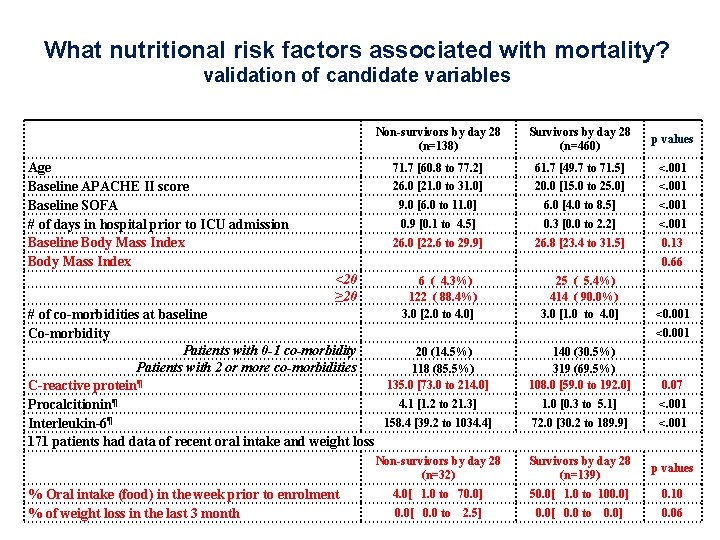
What nutritional risk factors associated with mortality? validation of candidate variables Age Baseline APACHE II score Baseline SOFA # of days in hospital prior to ICU admission Baseline Body Mass Index Non-survivors by day 28 (n=138) Survivors by day 28 (n=460) p values 71. 7 [60. 8 to 77. 2] 61. 7 [49. 7 to 71. 5] <. 001 26. 0 [21. 0 to 31. 0] 20. 0 [15. 0 to 25. 0] <. 001 9. 0 [6. 0 to 11. 0] 6. 0 [4. 0 to 8. 5] <. 001 0. 9 [0. 1 to 4. 5] 0. 3 [0. 0 to 2. 2] <. 001 26. 0 [22. 6 to 29. 9] 26. 8 [23. 4 to 31. 5] 0. 13 0. 66 <20 ≥ 20 6 ( 4. 3%) 122 ( 88. 4%) 3. 0 [2. 0 to 4. 0] # of co-morbidities at baseline Co-morbidity Patients with 0 -1 co-morbidity 20 (14. 5%) Patients with 2 or more co-morbidities 118 (85. 5%) ¶ 135. 0 [73. 0 to 214. 0] C-reactive protein 4. 1 [1. 2 to 21. 3] Procalcitionin¶ ¶ 158. 4 [39. 2 to 1034. 4] Interleukin-6 171 patients had data of recent oral intake and weight loss % Oral intake (food) in the week prior to enrolment % of weight loss in the last 3 month 25 ( 5. 4%) 414 ( 90. 0%) 3. 0 [1. 0 to 4. 0] <0. 001 140 (30. 5%) 319 (69. 5%) 108. 0 [59. 0 to 192. 0] 0. 07 1. 0 [0. 3 to 5. 1] <. 001 72. 0 [30. 2 to 189. 9] <. 001 Non-survivors by day 28 (n=32) Survivors by day 28 (n=139) p values 4. 0[ 1. 0 to 70. 0] 50. 0[ 1. 0 to 100. 0] 0. 10 0. 0[ 0. 0 to 2. 5] 0. 0[ 0. 0 to 0. 0] 0. 06
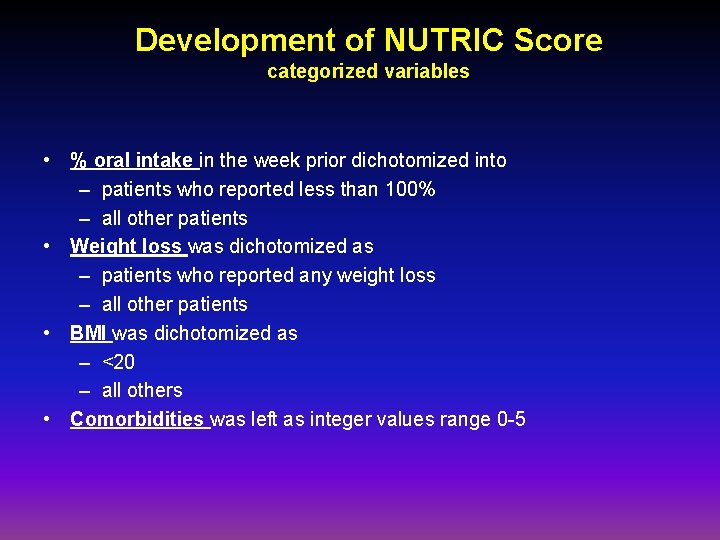
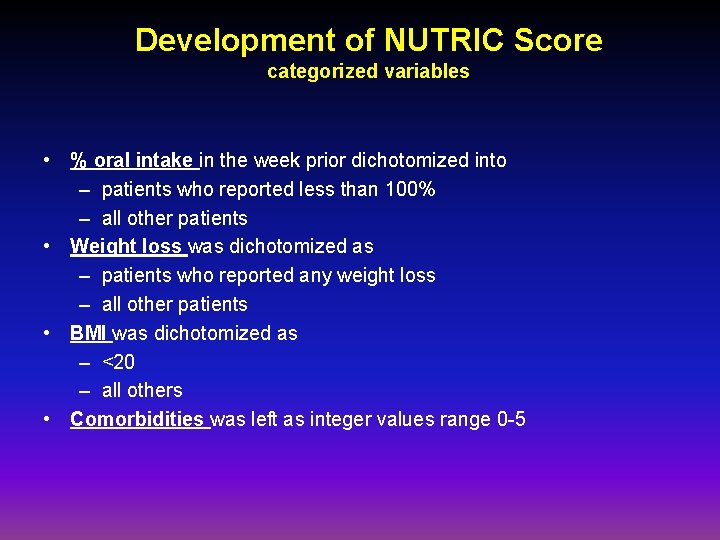
Development of NUTRIC Score categorized variables • % oral intake in the week prior dichotomized into – patients who reported less than 100% – all other patients • Weight loss was dichotomized as – patients who reported any weight loss – all other patients • BMI was dichotomized as – <20 – all others • Comorbidities was left as integer values range 0 -5
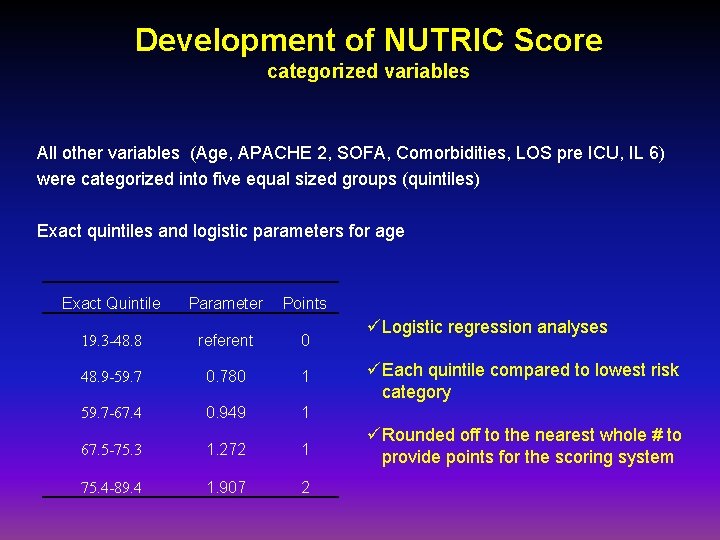
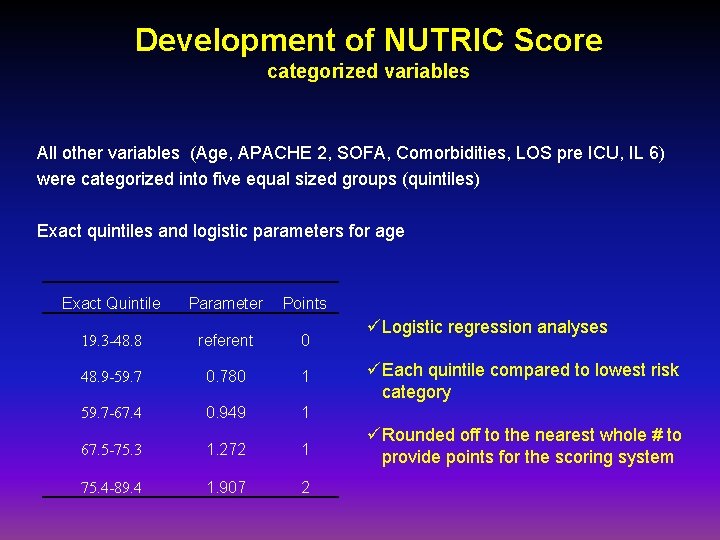
Development of NUTRIC Score categorized variables All other variables (Age, APACHE 2, SOFA, Comorbidities, LOS pre ICU, IL 6) were categorized into five equal sized groups (quintiles) Exact quintiles and logistic parameters for age Exact Quintile Parameter Points 19. 3 -48. 8 referent 0 48. 9 -59. 7 0. 780 1 59. 7 -67. 4 0. 949 1 67. 5 -75. 3 1. 272 1 75. 4 -89. 4 1. 907 2 üLogistic regression analyses üEach quintile compared to lowest risk category üRounded off to the nearest whole # to provide points for the scoring system
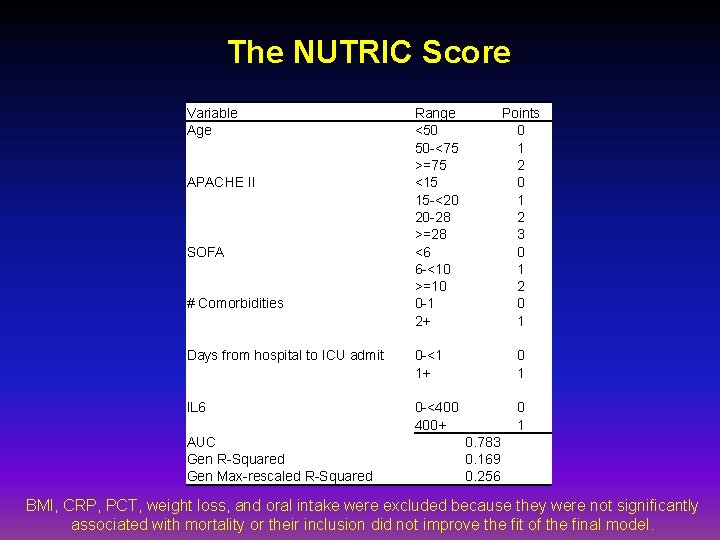
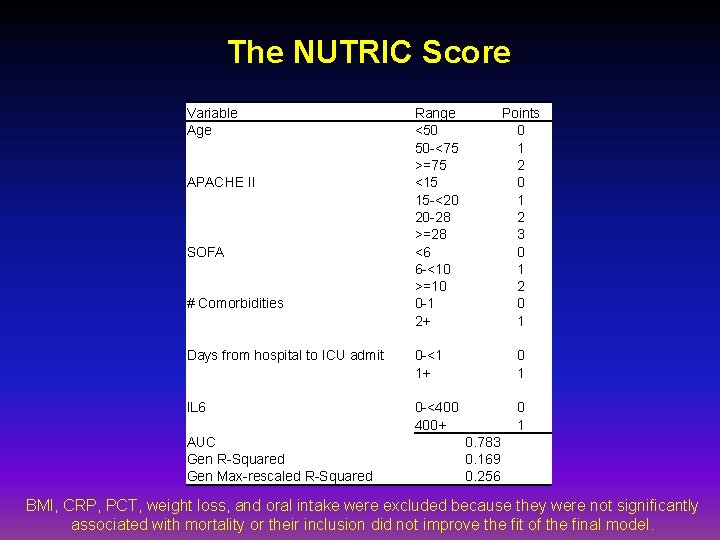
The NUTRIC Score Variable Age APACHE II SOFA # Comorbidities Range <50 50 -<75 >=75 <15 15 -<20 20 -28 >=28 <6 6 -<10 >=10 0 -1 2+ Points 0 1 2 3 0 1 2 0 1 Days from hospital to ICU admit 0 -<1 1+ 0 1 IL 6 0 -<400 400+ 0 1 AUC Gen R-Squared Gen Max-rescaled R-Squared 0. 783 0. 169 0. 256 BMI, CRP, PCT, weight loss, and oral intake were excluded because they were not significantly associated with mortality or their inclusion did not improve the fit of the final model.
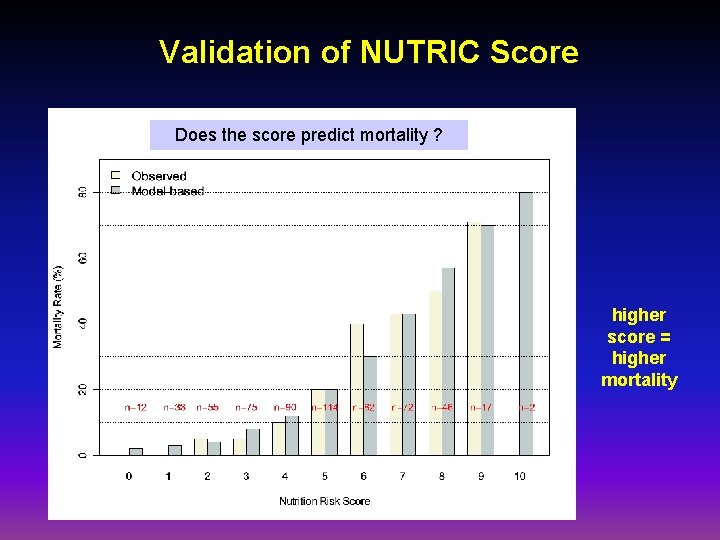
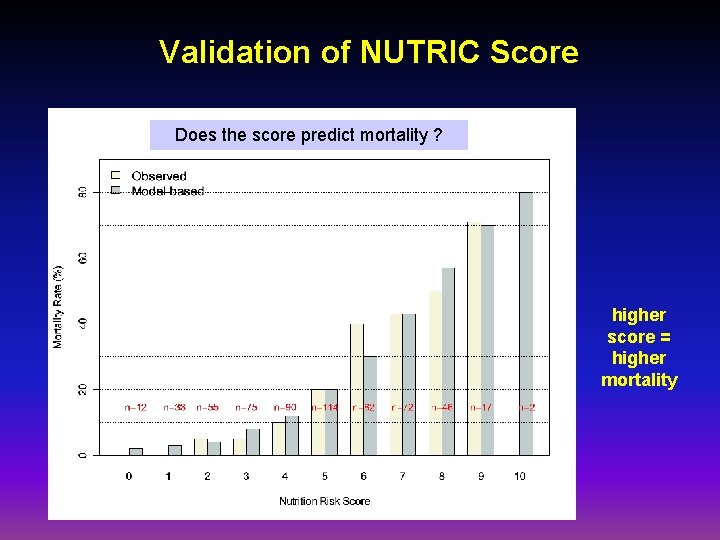
Validation of NUTRIC Score Does the score predict mortality ? higher score = higher mortality
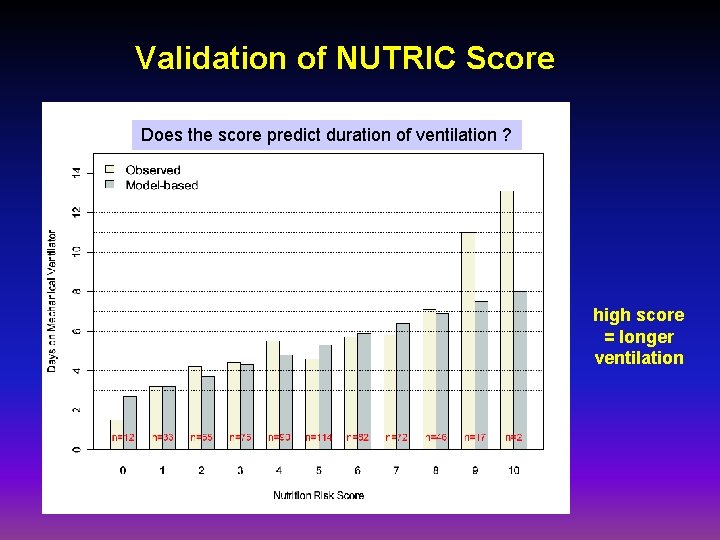
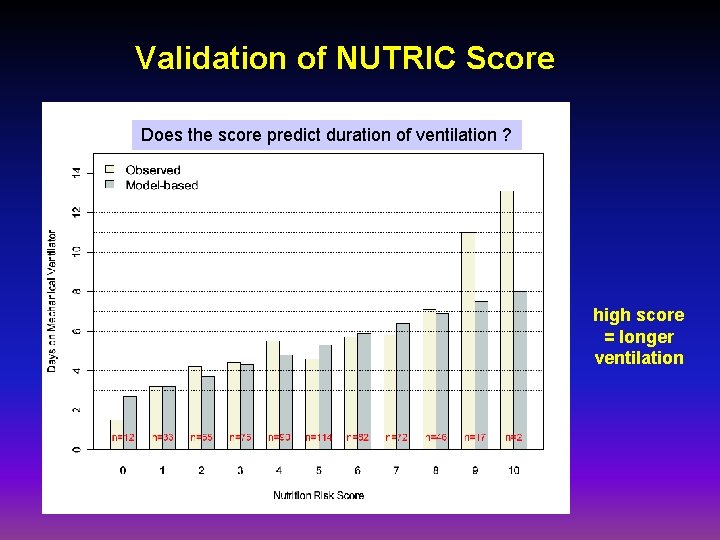
Validation of NUTRIC Score Does the score predict duration of ventilation ? high score = longer ventilation
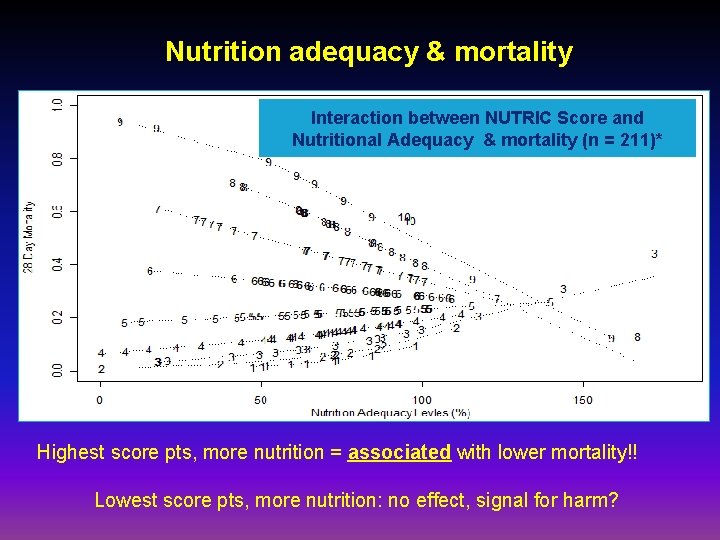
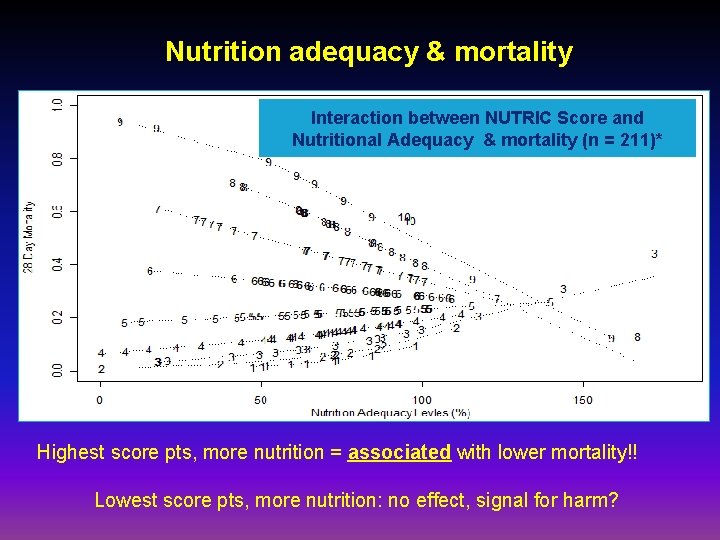
Nutrition adequacy & mortality Can NUTRIC score modify the associationbetween NUTRIC nutritional. Score adequacy Interaction and mortality? Adequacy (n=211) Nutritional & mortality (n = 211)* Highest score pts, more nutrition = associated with lower mortality!! Lowest score pts, more nutrition: no effect, signal for harm?
Summarize: NUTRIC Score • NUTRIC Score (0 -10) based on – – – Age APACHE II SOFA # comorbidities Days in hospital pre ICU IL 6 • High NUTRIC Score associated with worse outcomes (mortality, ventilation) • High NUTRIC Score: benefit the most from nutrition • Low NUTRIC Score : no effect
Applications of NUTRIC Score • Help determine which patients will benefit more from nutrition – Supplemental PN – Aggressive feeding – Small bowel feeding • Design & interpretation of future studies – Negative studies, non high risk, heterogenous patients
Limitations • • • needs to be validated further applies only to macronutrients does not apply to pharmaconutrients nutritional history is suboptimal requires IL-6
Bedside nutrition tool
Conclusion • calorie and protein debt (iatrogenic underfeeding) occurs in ICUs • existing screening tools not helpful in ICU • not all ICU patients are the same in terms of ‘risk’ • NUTRIC Score is one way to quantify that risk and can be used in your ICU • further refinement of this tool will ensure that the right patient gets nutrition
Thanks Dr. Heyland Xuran Jiang Andrew Day