The Nursing Process Practical Nursing Canadian Valley Technology
- Slides: 37
The Nursing Process Practical Nursing Canadian Valley Technology Center Shandy Baggs, RN, BSN, MSN
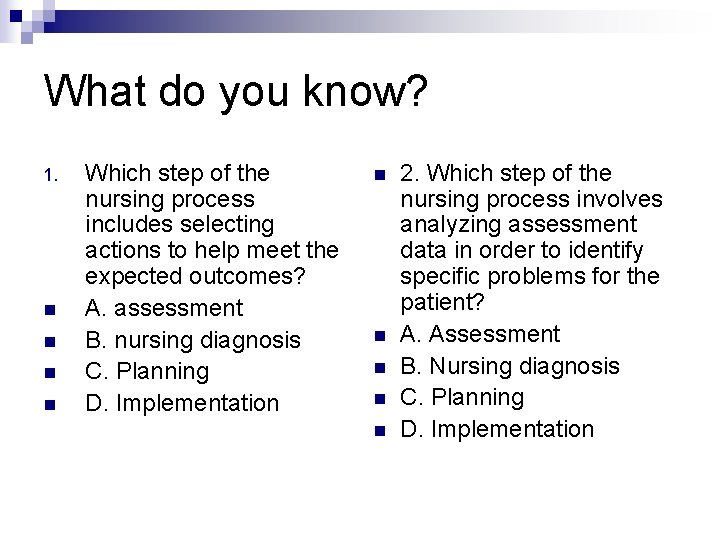
What do you know? 1. n n Which step of the nursing process includes selecting actions to help meet the expected outcomes? A. assessment B. nursing diagnosis C. Planning D. Implementation n n 2. Which step of the nursing process involves analyzing assessment data in order to identify specific problems for the patient? A. Assessment B. Nursing diagnosis C. Planning D. Implementation
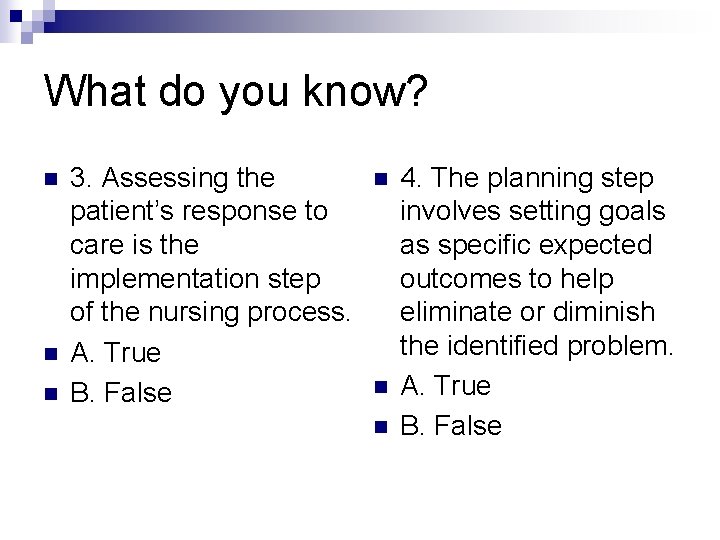
What do you know? n n n 3. Assessing the patient’s response to care is the implementation step of the nursing process. A. True B. False n n n 4. The planning step involves setting goals as specific expected outcomes to help eliminate or diminish the identified problem. A. True B. False
What do you know? n n n #5 Assessment step includes which of the following? A. patient interview B. focused assessment C. chart review D. all of the above n n n #6 The carrying out of actions to help diminish the problem involves which step of the nursing process? A. Assessment B. Nursing Diagnosis C. Planning D. Implementation
Objectives n n n Differentiate between the steps of the nursing process. Discuss the importance of the steps of the nursing process. Prioritize nursing diagnoses according to Maslow’s Hierarchy of Needs. Plan appropriate nursing interventions that are specific and measurable. Evaluate outcome of nursing interventions.
Steps of the Nursing Process Assessment n Nursing Diagnosis n Planning n Implementation n Evaluation n
Assessment Methods of data collection n Subjective data n Objective data n Analyzing data n
Nursing Diagnosis Etiologic factors=causes of the problem. n Signs & Symptoms. n Prioritization of problems according to Maslow’s Hierarchy of Needs. n NANDA nursing diagnoses list. n
Planning Goal- broad idea of what is to be achieved through nursing intervention. n Short-term goal=7 -10 days n Long-term goal=relate to rehabilitation n Expected outcome-specific statement of the goal the patient is expected to achieve as a result of nursing intervention. n
Implementation The carrying out phase n Developing actions to help alleviate the problem. n Utilizing critical thinking. n Identifying the rationale of the intervention. n
Evaluation n n The judgment of the effectiveness of the intervention or plan. Patient’s response to the intervention (good or bad). Determines whether the interventions were effective in helping the patient reach the expected outcome. Is this a continuous process? ?
Prioritizing Nursing Diagnoses n Maslow’s Hierarchy of Needs (physiologic, safety/security, love/belonging, self-esteem, self-actualization) ABC’s n Pain…where does it fit? n Consulting with the patient. n Use of critical thinking and disease process. n
Test your skills at prioritizing problems. n Patient is diagnosed with pneumonia. On O 2 @ 2 L via NC. Sp. O 2 is 85% on room air and 96% on O 2. Assessment reveals crackles auscultated to all lobes. Cap refill sluggish. Respirations 26, shallow, labored, irregular. Productive cough of thick, yellow sputum. Complains of pain upon coughing. Rates 7 on scale 0 -10. Gait unsteady. Tires easily and experiences SOB upon trips to the bathroom. Requires assistance with ADL’s. Has history of CHF, COPD, HTN.
What is your answer? Impaired gas exchange n Ineffective breathing pattern n Pain n Decreased tissue perfusion n Activity Intolerance n Self-care deficit n Risk for falls/injury n
Time to Plan!! What is our goals for this patient? n Are they short-term or long-term? n What are our expected outcomes? n
Implementing Interventions What are interventions needed for this patient? n Look at top priority nursing diagnoses. n Look at goals and expected outcomes. n Will they be effective? n Make them specific and measurable! n
What are interventions for this patient? n Impaired gas exchange 1. 2. 3. 4. Auscultate lung sounds every shift and PRN noting for adventious sounds. Monitor O 2 saturation every 4 hours and PRN throughout the shift noting for levels less than 90%. Teach and enforce to turn, cough, deep breath every 2 hours PRN throughout the shift noting for productive cough and adventitious lung sounds. Teach and enforce incentive spirometer every 1 hour while awake PRN throughout the shift noting for level patient accomplishes.
Interventions continued n Ineffective breathing pattern 1. 2. 3. 4. Assess respiratory rate and effort every 4 hours and PRN throughout the shift noting for rate >24, effort irregular, shallow or deep, and labored. Assess O 2 saturation every 4 hours and PRN throughout the shift noting for levels <90%. Administer O 2 @ 2 L via NC to maintain O 2 sats >90% throughout the shift. Schedule rest periods and cluster care throughout the shift to not tire patient.
Interventions Continued n Pain 1. 2. 3. 4. 5. Instruct patient to notify when pain level is increasing and to not wait for pain to get too intense before intervention can be done. Administer pain med as ordered PRN throughout the shift. Teach guided imagery, relaxation techniques, distraction techniques PRN throughout the shift. Assess pain level using the 0 -10 pain scale every 4 hours and PRN throughout the shift noting for intensity, location, and duration. Instruct use of pillow splint when coughing PRN throughout the shift.
Evaluations n n What was the result? What was the patient’s response? Not to be a restatement of the intervention. Must be specific.
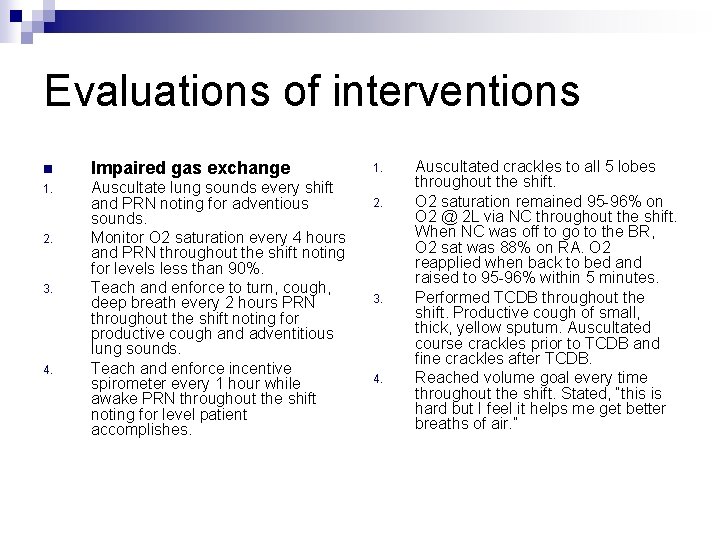
Evaluations of interventions n Impaired gas exchange 1. Auscultate lung sounds every shift and PRN noting for adventious sounds. Monitor O 2 saturation every 4 hours and PRN throughout the shift noting for levels less than 90%. Teach and enforce to turn, cough, deep breath every 2 hours PRN throughout the shift noting for productive cough and adventitious lung sounds. Teach and enforce incentive spirometer every 1 hour while awake PRN throughout the shift noting for level patient accomplishes. 2. 3. 4. 1. 2. 3. 4. Auscultated crackles to all 5 lobes throughout the shift. O 2 saturation remained 95 -96% on O 2 @ 2 L via NC throughout the shift. When NC was off to go to the BR, O 2 sat was 88% on RA. O 2 reapplied when back to bed and raised to 95 -96% within 5 minutes. Performed TCDB throughout the shift. Productive cough of small, thick, yellow sputum. Auscultated course crackles prior to TCDB and fine crackles after TCDB. Reached volume goal every time throughout the shift. Stated, “this is hard but I feel it helps me get better breaths of air. ”
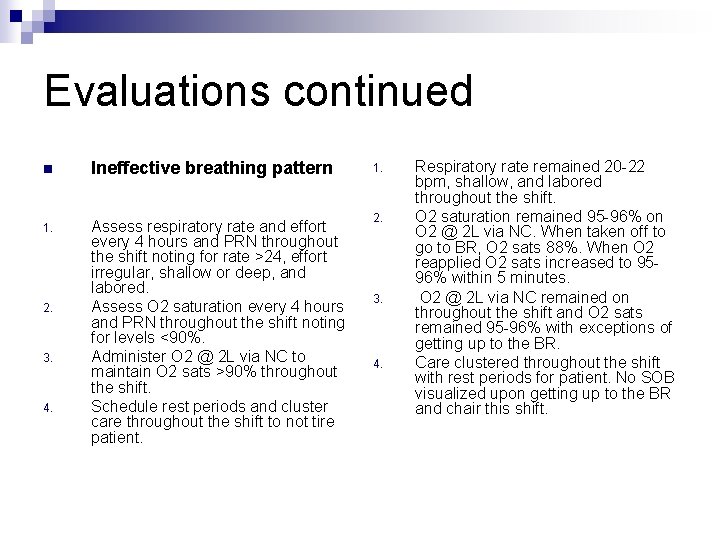
Evaluations continued n Ineffective breathing pattern 1. Assess respiratory rate and effort every 4 hours and PRN throughout the shift noting for rate >24, effort irregular, shallow or deep, and labored. Assess O 2 saturation every 4 hours and PRN throughout the shift noting for levels <90%. Administer O 2 @ 2 L via NC to maintain O 2 sats >90% throughout the shift. Schedule rest periods and cluster care throughout the shift to not tire patient. 2. 3. 4. 1. 2. 3. 4. Respiratory rate remained 20 -22 bpm, shallow, and labored throughout the shift. O 2 saturation remained 95 -96% on O 2 @ 2 L via NC. When taken off to go to BR, O 2 sats 88%. When O 2 reapplied O 2 sats increased to 9596% within 5 minutes. O 2 @ 2 L via NC remained on throughout the shift and O 2 sats remained 95 -96% with exceptions of getting up to the BR. Care clustered throughout the shift with rest periods for patient. No SOB visualized upon getting up to the BR and chair this shift.
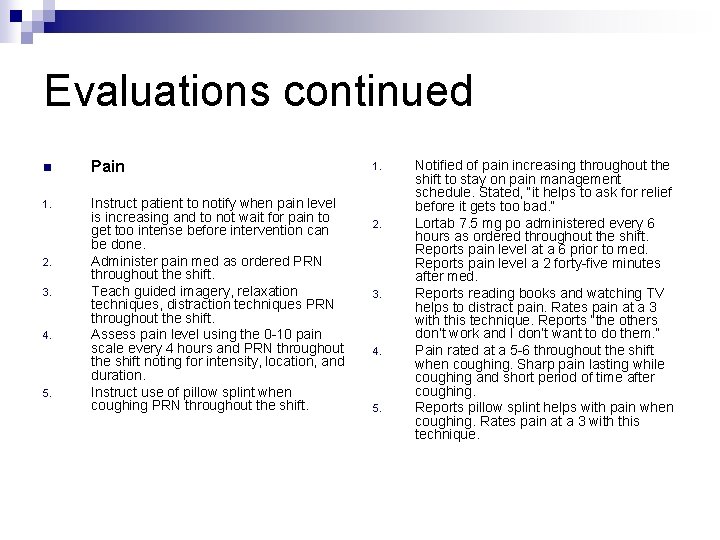
Evaluations continued n Pain 1. Instruct patient to notify when pain level is increasing and to not wait for pain to get too intense before intervention can be done. Administer pain med as ordered PRN throughout the shift. Teach guided imagery, relaxation techniques, distraction techniques PRN throughout the shift. Assess pain level using the 0 -10 pain scale every 4 hours and PRN throughout the shift noting for intensity, location, and duration. Instruct use of pillow splint when coughing PRN throughout the shift. 2. 3. 4. 5. 1. 2. 3. 4. 5. Notified of pain increasing throughout the shift to stay on pain management schedule. Stated, “it helps to ask for relief before it gets too bad. ” Lortab 7. 5 mg po administered every 6 hours as ordered throughout the shift. Reports pain level at a 6 prior to med. Reports pain level a 2 forty-five minutes after med. Reports reading books and watching TV helps to distract pain. Rates pain at a 3 with this technique. Reports “the others don’t work and I don’t want to do them. ” Pain rated at a 5 -6 throughout the shift when coughing. Sharp pain lasting while coughing and short period of time after coughing. Reports pillow splint helps with pain when coughing. Rates pain at a 3 with this technique.
Practice Time n The patient is diagnosed with CHF. The patient is edematous in the extremities, 3+ pitting edema, dyspneic, fatigued, tachycardic, hypertension, sluggish cap refill, crackles and rhonchi auscultated to lungs, SOB with activity. Has O 2 @ 3 L via NC. On strict I & O, and on fluid restriction of 1200 cc/day. Weak peripheral pulses, strong apical pulse. IV heplock to right hand.
Nursing Diagnoses… Number by Priority Decreased Cardiac Output n Impaired Gas Exchange n Fluid Volume Overload n Activity Intolerance n Risk for falls/injury n Risk for skin integrity n
Name those nursing interventions n Decreased cardiac output n Impaired gas exchange n Fluid volume overload
Interventions n Decreased Cardiac Output 1. 2. 3. Assess VS noting for increase or decrease in BP, pulse, and respirations Auscultate apical pulse noting for rate, rhythm, and strength every 4 hours and PRN throughout the shift. Assess peripheral pulses and cap refill noting for rhythm, strength and time to refill every shift and PRN.
Interventions Cont n Impaired gas exchange 1. 2. 3. Assess lung sounds noting for adventious sounds every 4 hours and PRN throughout the shift. Assess respiratory rate, rhythm, and effort noting for increases, struggles every 4 hours and PRN throughout the shift. Assess O 2 sats every 4 hours and PRN throughout the shift.
Interventions Cont. n Fluid volume overload 1. 2. 3. Weight patient daily noting for an excessive weight gain or loss. Monitor and maintain a strict I & O throughout the shift. Educate and maintain fluid restrictions of 600 cc throughout this shift.
Evaluations n 1. 2. 3. Decreased Cardiac output Assess VS noting for increase or decrease in BP, pulse, and respirations Auscultate apical pulse noting for rate, rhythm, and strength every 4 hours and PRN throughout the shift. Assess peripheral pulses and cap refill noting for rhythm, strength and time to refill every shift and PRN. 1. 2. 3. VS @ 0700: BP 136/84, P 100, R 24 1100: BP 130/80, P 96, R 22. VS decreased showing no marked signs of condition worse. AP 100 @0700 AP 96 @1100. Strong, and regular at both times. 2+PPPx 4 extremities and equal and regular bilaterally. Cap refill sluggish throughout the shift.
Evaluations Cont. n 1. 2. 3. Impaired gas exchange Assess lung sounds noting for adventious sounds every 4 hours and PRN throughout the shift. Assess respiratory rate, rhythm, and effort noting for increases, struggles every 4 hours and PRN throughout the shift. Assess O 2 sats every 4 hours and PRN throughout the shift. 1. 2. 3. Crackles heard x 5 lobes throughout the shift. Respirations 24, even regular, shallow @ 0700 and 22, even regular and labored @ 1100. O 2 sats @ 0700, 96% on O 2 @ 3 L. 1100 O 2 sats 97% on O 2 @ 3 L.
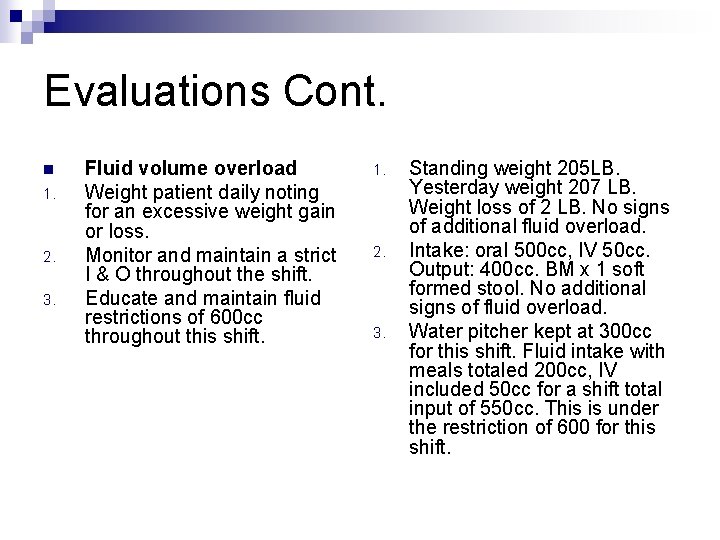
Evaluations Cont. n 1. 2. 3. Fluid volume overload Weight patient daily noting for an excessive weight gain or loss. Monitor and maintain a strict I & O throughout the shift. Educate and maintain fluid restrictions of 600 cc throughout this shift. 1. 2. 3. Standing weight 205 LB. Yesterday weight 207 LB. Weight loss of 2 LB. No signs of additional fluid overload. Intake: oral 500 cc, IV 50 cc. Output: 400 cc. BM x 1 soft formed stool. No additional signs of fluid overload. Water pitcher kept at 300 cc for this shift. Fluid intake with meals totaled 200 cc, IV included 50 cc for a shift total input of 550 cc. This is under the restriction of 600 for this shift.
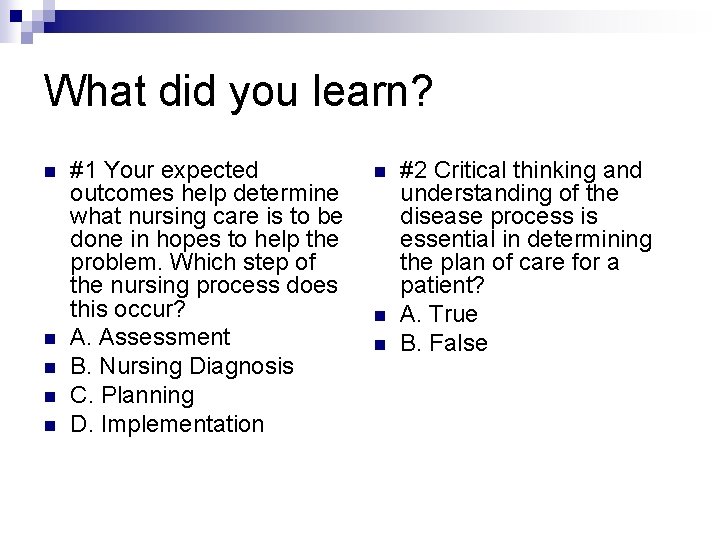
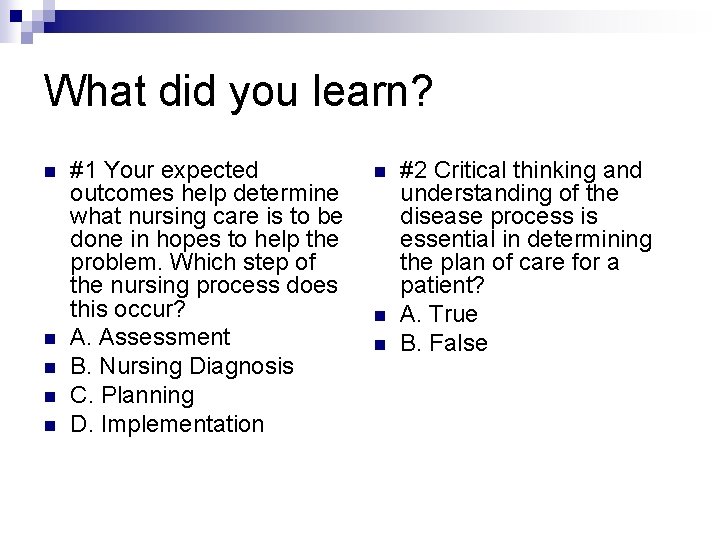
What did you learn? n n n #1 Your expected outcomes help determine what nursing care is to be done in hopes to help the problem. Which step of the nursing process does this occur? A. Assessment B. Nursing Diagnosis C. Planning D. Implementation n #2 Critical thinking and understanding of the disease process is essential in determining the plan of care for a patient? A. True B. False
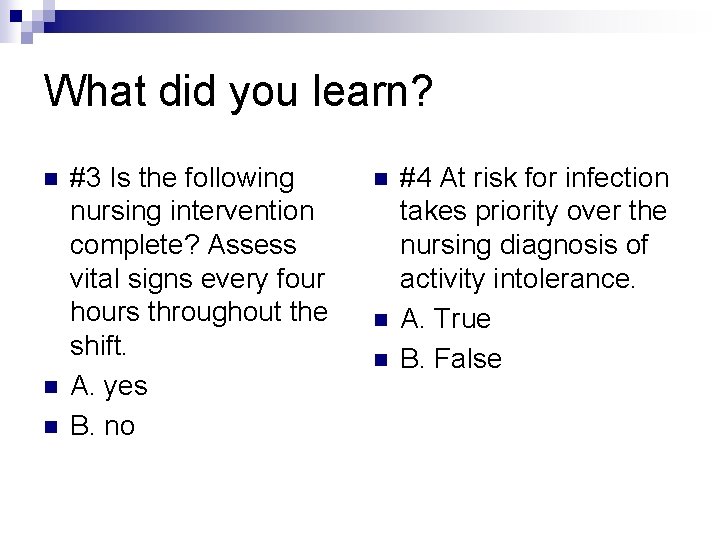
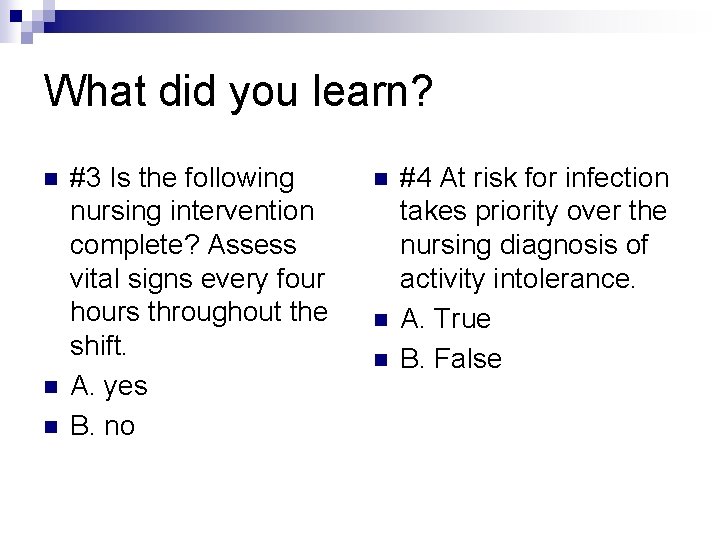
What did you learn? n n n #3 Is the following nursing intervention complete? Assess vital signs every four hours throughout the shift. A. yes B. no n n n #4 At risk for infection takes priority over the nursing diagnosis of activity intolerance. A. True B. False
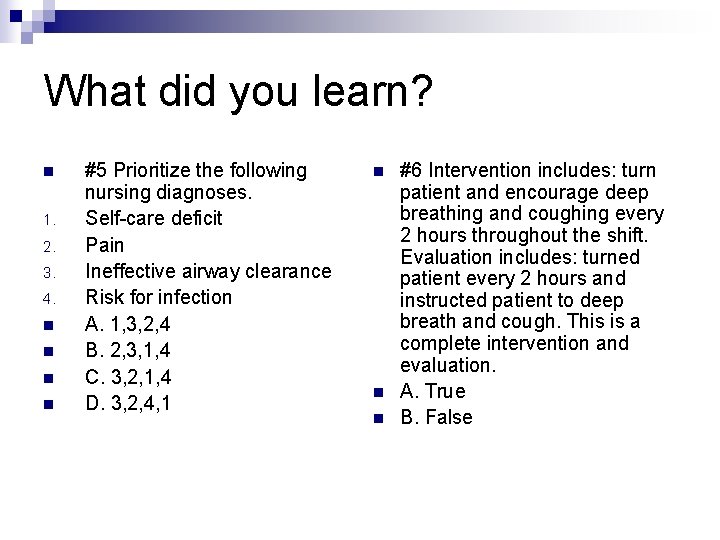
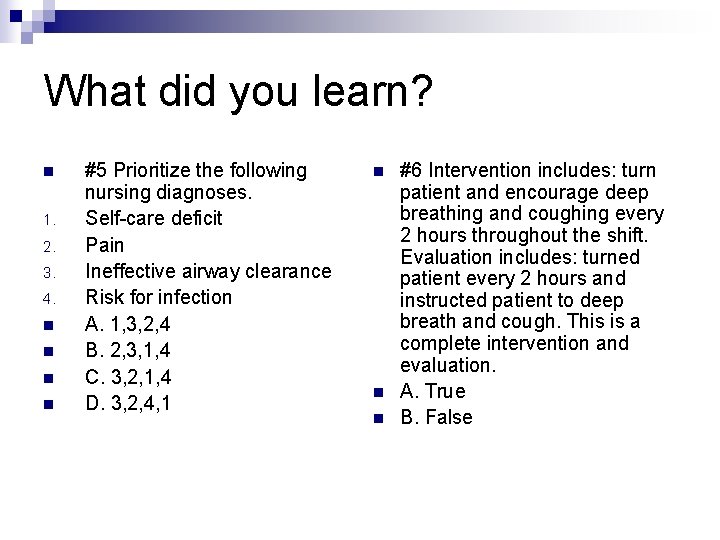
What did you learn? n 1. 2. 3. 4. n n #5 Prioritize the following nursing diagnoses. Self-care deficit Pain Ineffective airway clearance Risk for infection A. 1, 3, 2, 4 B. 2, 3, 1, 4 C. 3, 2, 1, 4 D. 3, 2, 4, 1 n n n #6 Intervention includes: turn patient and encourage deep breathing and coughing every 2 hours throughout the shift. Evaluation includes: turned patient every 2 hours and instructed patient to deep breath and cough. This is a complete intervention and evaluation. A. True B. False
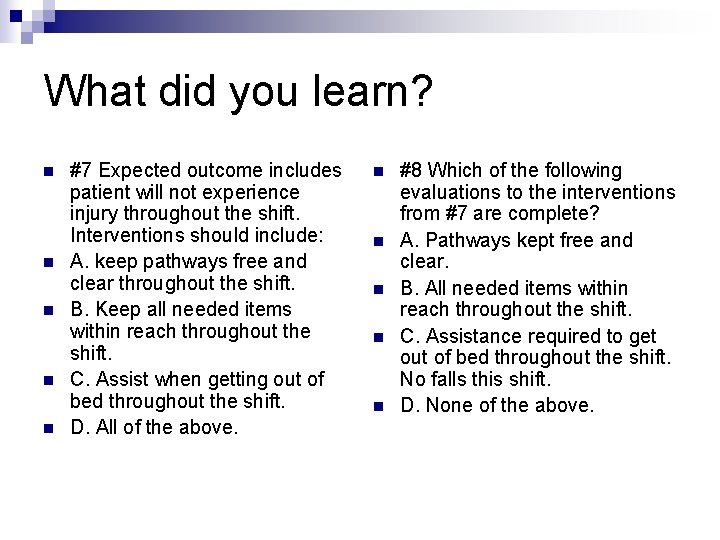
What did you learn? n n n #7 Expected outcome includes patient will not experience injury throughout the shift. Interventions should include: A. keep pathways free and clear throughout the shift. B. Keep all needed items within reach throughout the shift. C. Assist when getting out of bed throughout the shift. D. All of the above. n n n #8 Which of the following evaluations to the interventions from #7 are complete? A. Pathways kept free and clear. B. All needed items within reach throughout the shift. C. Assistance required to get out of bed throughout the shift. No falls this shift. D. None of the above.
What did you learn? n n n #9 Your number 1 nursing diagnosis for your patient yesterday was pain. Today upon assessment, patient rated pain at a 0 throughout the morning. What is your next step to take? A. continue with current plan. B. add another nursing diagnosis to the plan. C. go to your RN and ask her for a nursing diagnosis to follow. D. look at current plan and choose another diagnosis as priority for this patient. n n n #10 Which of the following interventions are complete? A. Weight patient B. Assess VS every 4 hours throughout the shift. C. Assess lung sounds noting for adventious sounds every 4 hours throughout the shift. D. Assess Sp. O 2 noting to keep sats > 95%.