The Nottingham liver disease stratification pathway Dr Neil
- Slides: 30
The Nottingham liver disease stratification pathway Dr Neil Guha and Dr Emilie Wilkes 27/11/2020
Outline of session • LFTS in primary care • Why the need for change and aims of the pathway • Walk through the pathway using examples
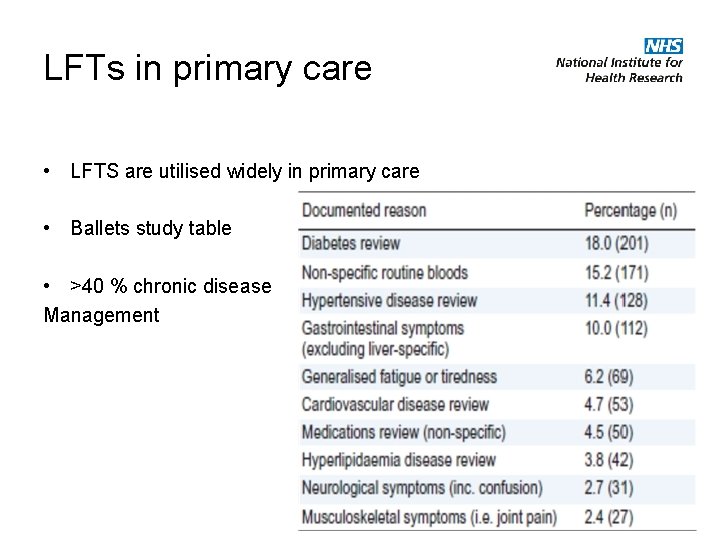
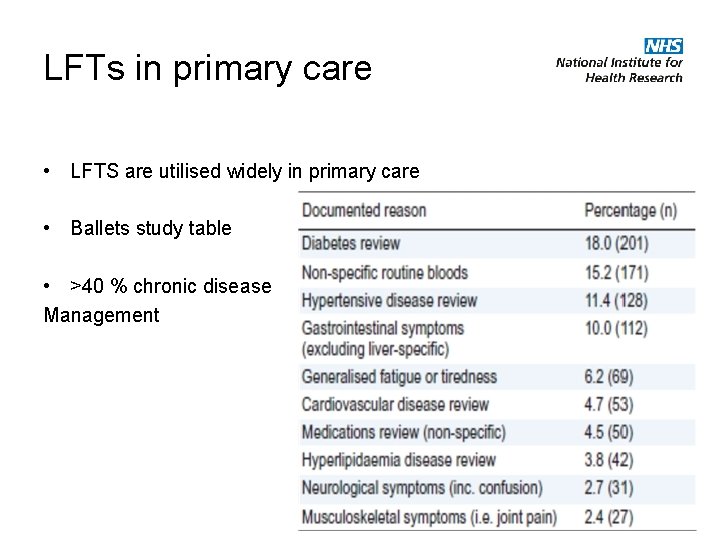
LFTs in primary care • LFTS are utilised widely in primary care • Ballets study table • >40 % chronic disease Management
Three perspectives What we currently do with abnormal LFTS • Primary care • Ignore as not requested for liver (anxiety) • Repeat (might go away) • Refer to secondary care (expense and futility) • Patient • Is my liver damaged, why and what can be done? • Abnormal Liver tests = alcohol • Secondary care • Non-significant disease in new referrals. • LFTS unhelpful in identifying patients at high risk of liver mortality (e. g. cirrhosis)
The rationale for detecting significant liver disease Patient perspective • Have I got something seriously wrong with my liver now? • Will I die from this, if so when and from what ? • Are things getting worse or better with or treatment/observation ? Healthcare perspective • Can we pick this up at a stage where it is serious enough to intervene but not too late to be palliative and/or expensive • Can we intervene with liver specific interventions ( e. g. Pioglitazone in NAFLD and cirrhosis strategies) • Can we organise care in an effective manner (outcomes and costs) • Can we “nudge” behaviour in a positive way for lifestyle aetiologies • Can we select appropriate patients for emerging and/or expensive treatments
How do we assess liver disease
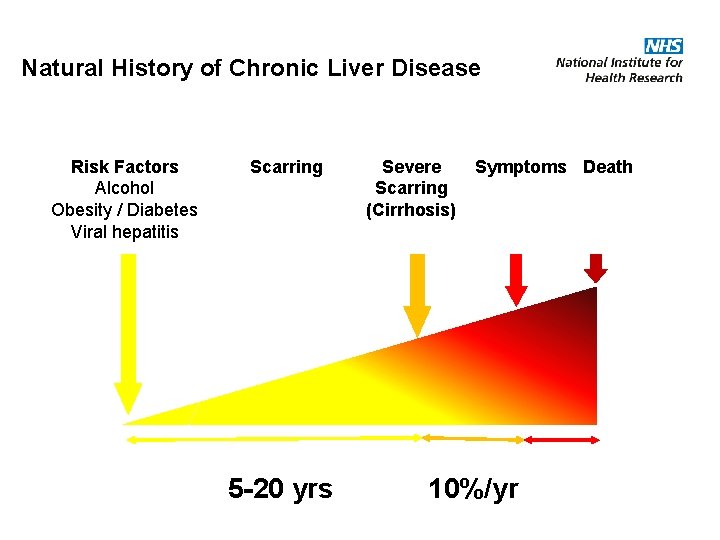
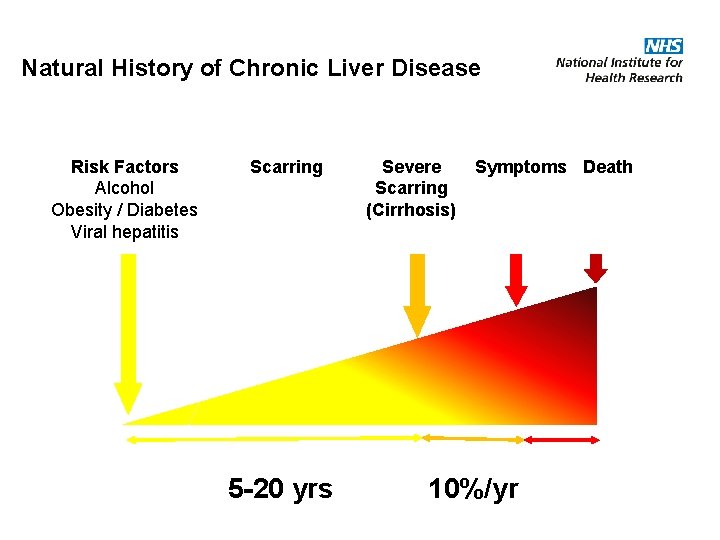
Natural History of Chronic Liver Disease Risk Factors Alcohol Obesity / Diabetes Viral hepatitis Scarring 5 -20 yrs Severe Scarring (Cirrhosis) Symptoms Death 10%/yr
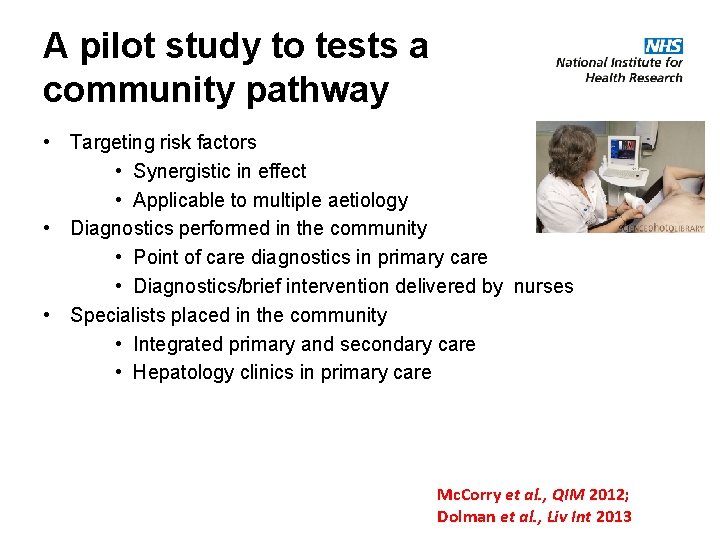
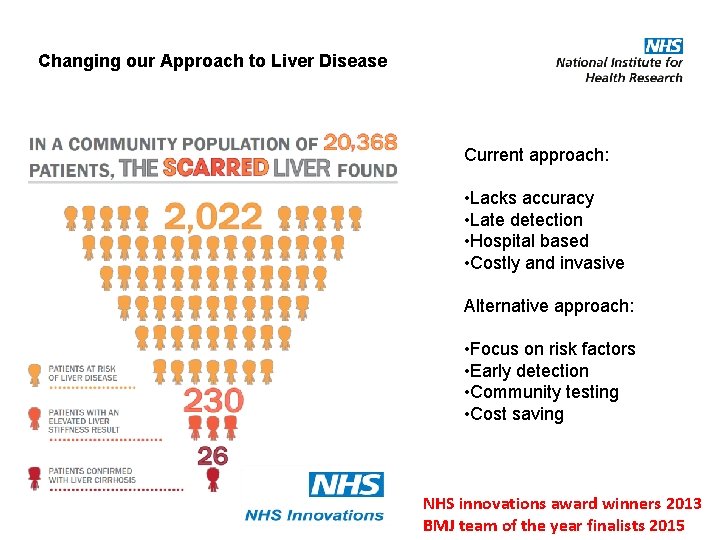
A pilot study to tests a community pathway • Targeting risk factors • Synergistic in effect • Applicable to multiple aetiology • Diagnostics performed in the community • Point of care diagnostics in primary care • Diagnostics/brief intervention delivered by nurses • Specialists placed in the community • Integrated primary and secondary care • Hepatology clinics in primary care Mc. Corry et al. , QIM 2012; Dolman et al. , Liv Int 2013
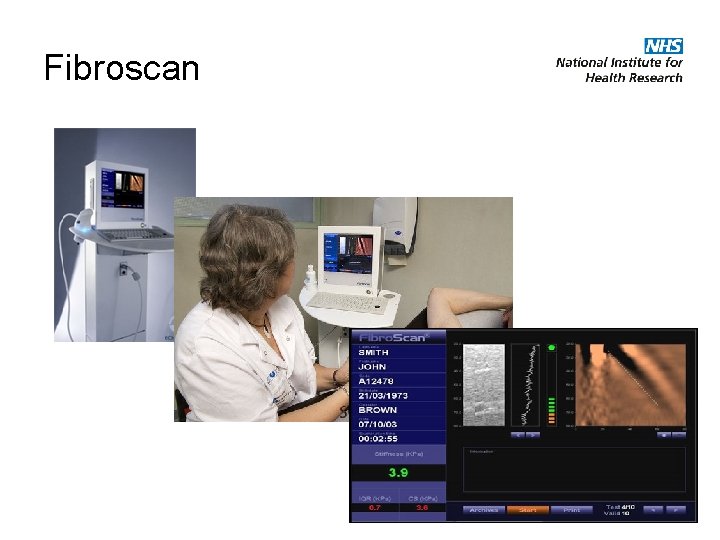
Fibroscan
Fibroscan • Results affected by: – Obesity – Narrow Rib spaces – Liver inflammation • May not be possible to obtain reliable reading • Operator dependent • Contraindicated in pregnancy, intracardiac devices • Metaanalysis – >90% NPV and PPV for cirrhosis
Outcomes • Liver disease – Increased detection of significant liver disease (25 % of those having a community scan) including cirrhosis (3 fold increase) – 68. 3% of patients with elevated liver stiffness had normal liver function enzymes – 73. 1% of patients with proven cirrhosis had normal liver function enzymes • Patient experience (n=349; 378 forms distributed) – 93. 7% of patients would definitely recommend service to friends and family – 95. 9% felt that the appointment was important or very important for their health – 94. 3% felt they were given enough information • Engagement with pathway – 95 % of investigations were performed in the community setting – Attendance rate for community Fibroscan appointment was 95 % • Cost effective – ICER for NAFLD and ALD are £ 2, 000 and £ 6, 000 respectively
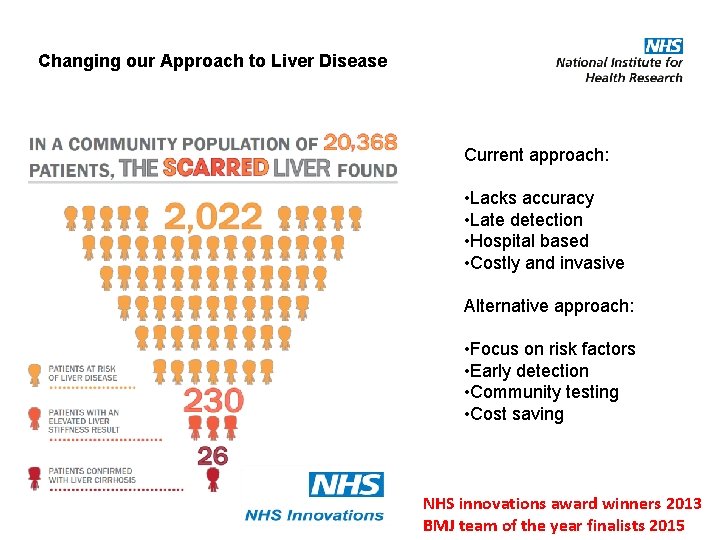
Changing our Approach to Liver Disease Current approach: • Lacks accuracy • Late detection • Hospital based • Costly and invasive Alternative approach: • Focus on risk factors • Early detection • Community testing • Cost saving NHS innovations award winners 2013 BMJ team of the year finalists 2015
NICE guidelines 2016 on NAFLD and cirrhosis • Awareness that NAFLD is common in type 2 diabetes/met syndrome • Detection of NAFLD. FLI index was most cost effective – not a definitive recommendation • Detection of advanced fibrosis in NAFLD ( serum markers of liver fibrosis – ELF score) • Confirmation of cirrhosis using Fibroscan ( hazardous alcohol and advanced fibrosis in NAFLD) • Statins should not be stopped (unless liver enzymes double within 3/12) • Pioglitazone recommended for advanced fibrosis in NAFLD • Cirrhosis surveillance recommended for varices (OGD) and HCC (U/S)
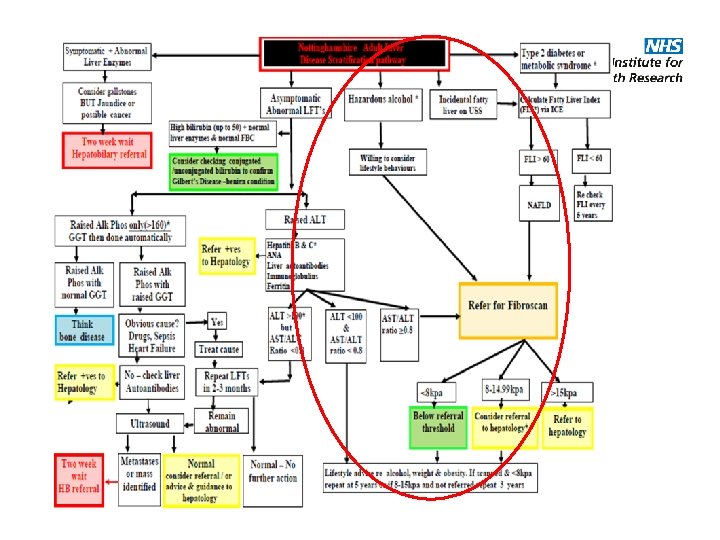
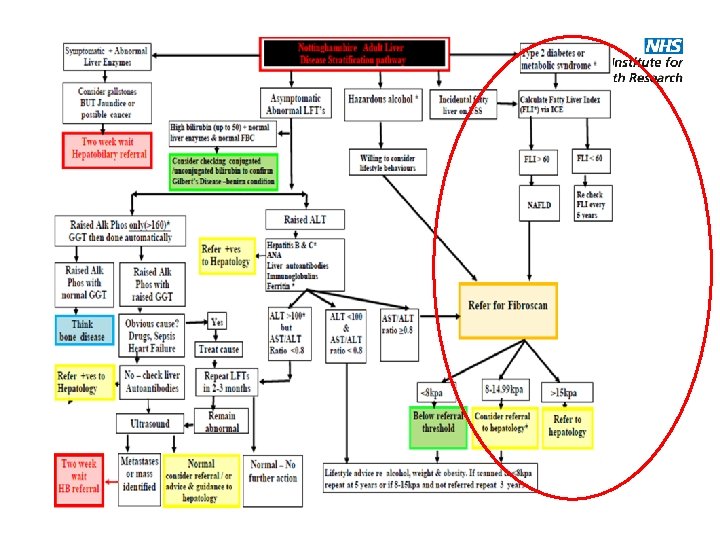
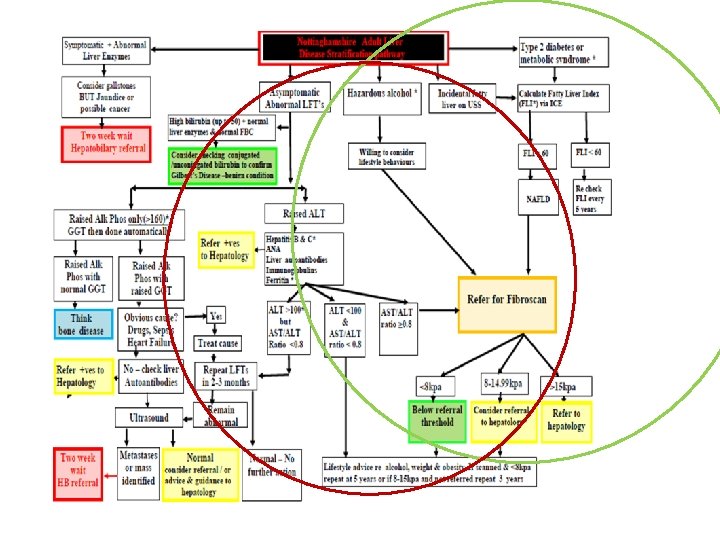
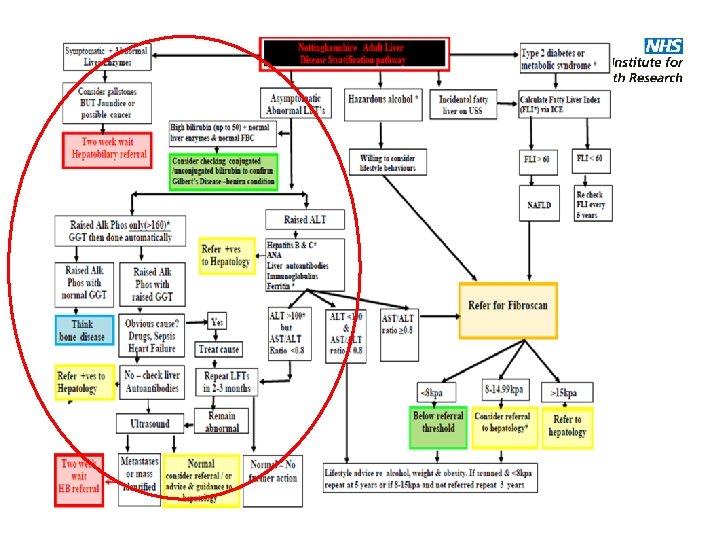
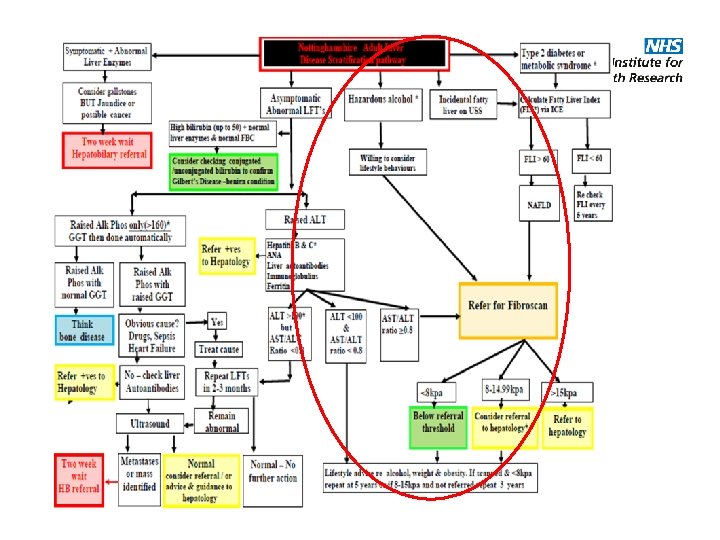
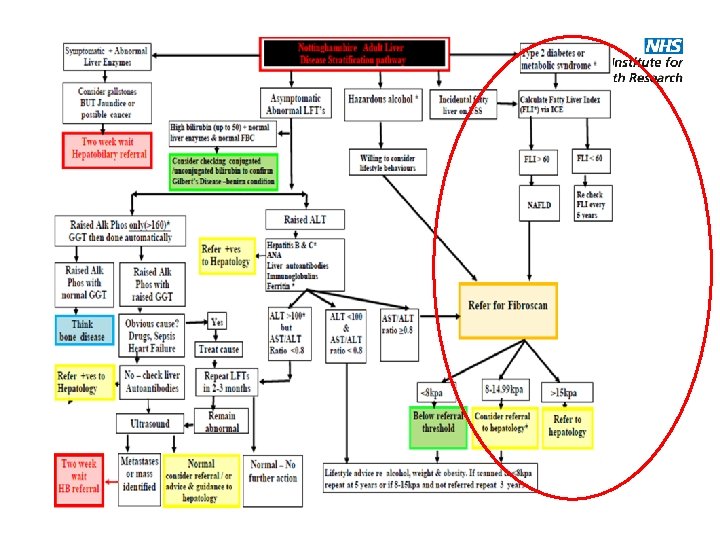
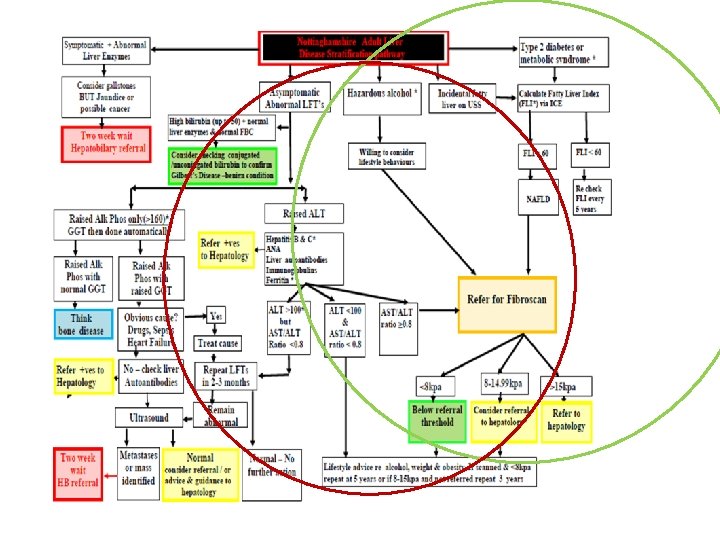
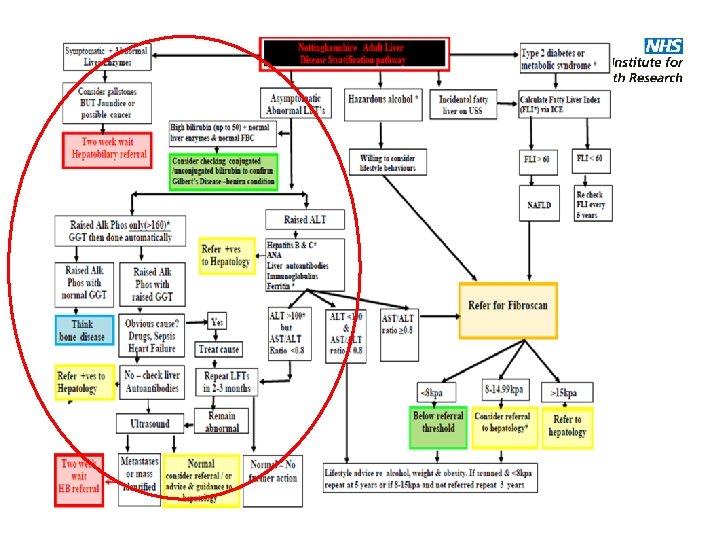
Concepts of the Nottinghamshire Adult Liver Disease Stratification pathway • Focussed on risk factors in addition to LFTS • Compromise between the views of the CCG, hepatology and NICE guidance • Stratification of liver risk rather than a definitive diagnostic test • Highlighting the need to link in with community services that deal with the underlying issues driving the risk factors including alcohol and weight loss
Acknowledging the following • Complex to follow ! • The ICE interface is currently far from ideal and the need to take on feedback form users to improve this • Fatty Liver Index uses variables that may not be easy to access ( e. g. waist circumference and GGT) • The pathway is not didactic in some aspects – both an advantage and disadvantage • The pathway will be evaluated and iterated
Case 1 • 56 y/o female. Teacher • Only significant medical history was asthma • Hazardous alcohol intake for many years ( 30 units/week) but increase in last 18 months following work issues ( 50 units/week). Normal LFTs. BMI 30. • Monthly visits to GP with different symptoms over 9 months. Found to be hypertensive. Advised to reduce alcohol intake. Declined alcohol services. “Not an alcoholic”. • Invited to participate in the community study.
Case 1 • Fibroscan reading elevated at 25 Kp. A • Review with hepatology and cirrhosis confirmed • OGD – showed early varices • Diagnosis was a “shock” ; cirrhosis was a diagnosis for people who “drank on park benches”. • Engaged with last orders, now abstinent for 2 years , off antihypertensive meds and has also lost 2 stones in weight. • Varices have disappeared on follow up endoscopy
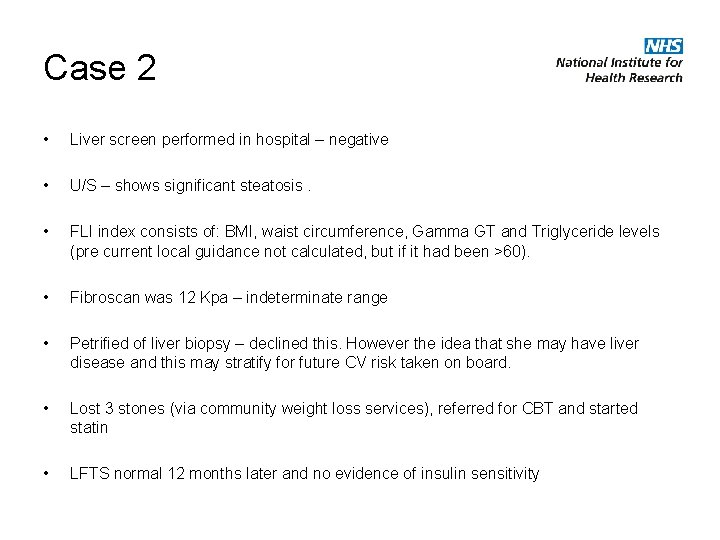
Case 2 • 38 y/o shop assistant • History of anxiety – uses alcohol as anxiolytic (20 units per week) • Fluctuating weight with BMI of 30 to 35; borderline diabetes; raised cholesterol of 7 • Strong FH of IHD and hyperlipidaemia • GP had offered statin but declined • ALT 67 but AST/ALT ratio normal • Referred to secondary care
Case 2 • Liver screen performed in hospital – negative • U/S – shows significant steatosis. • FLI index consists of: BMI, waist circumference, Gamma GT and Triglyceride levels (pre current local guidance not calculated, but if it had been >60). • Fibroscan was 12 Kpa – indeterminate range • Petrified of liver biopsy – declined this. However the idea that she may have liver disease and this may stratify for future CV risk taken on board. • Lost 3 stones (via community weight loss services), referred for CBT and started statin • LFTS normal 12 months later and no evidence of insulin sensitivity
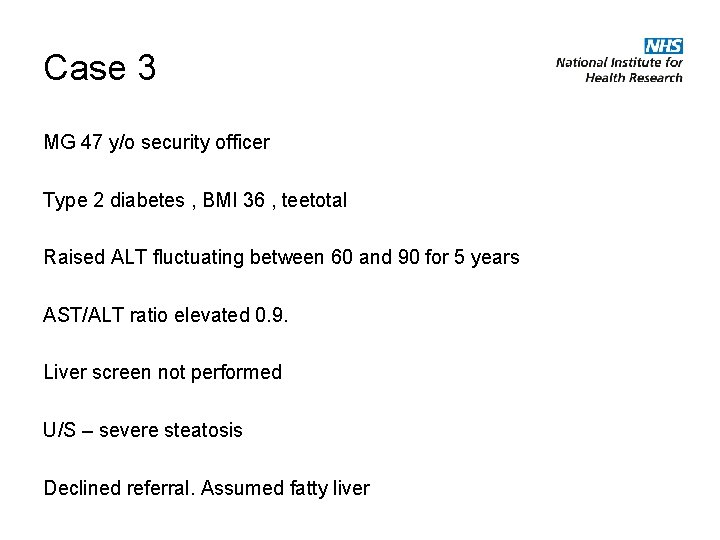
Case 3 MG 47 y/o security officer Type 2 diabetes , BMI 36 , teetotal Raised ALT fluctuating between 60 and 90 for 5 years AST/ALT ratio elevated 0. 9. Liver screen not performed U/S – severe steatosis Declined referral. Assumed fatty liver
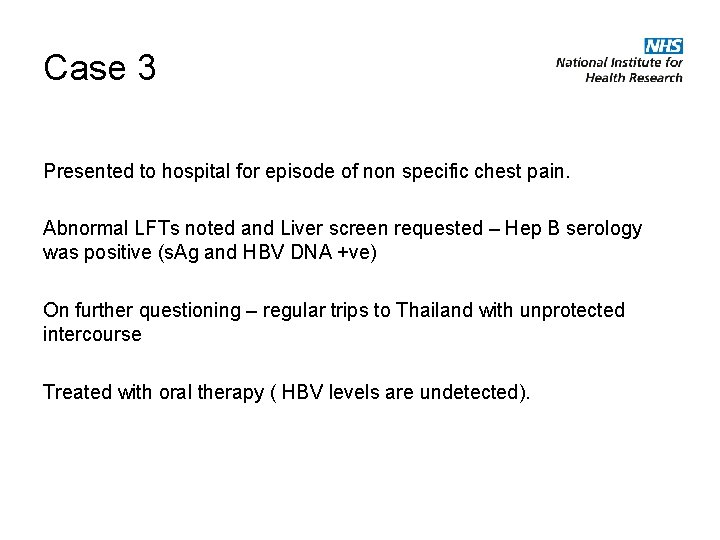
Case 3 Presented to hospital for episode of non specific chest pain. Abnormal LFTs noted and Liver screen requested – Hep B serology was positive (s. Ag and HBV DNA +ve) On further questioning – regular trips to Thailand with unprotected intercourse Treated with oral therapy ( HBV levels are undetected).
Case 4 • 52 y/o house wife • Presents with “tired all the time” symptoms • Overweight BMI 30; Hypertension and hyperlipidaemia • Strong FH of type 2 DM • ALT 50, AST/ALT 0. 9, ALP 456 • Community U/S – shows steatosis, gall stones in GB. • Referred to secondary care
Case 4 • Liver screen performed in hospital – positive Anti-mitochondrial Antibody and Ig. M raised • Liver biopsy – discussed and agreed. • Diagnosis of Primary Biliary Cholangitis (Stage 3 disease – Advanced fibrosis, not cirrhosis), some steatosis present. • LFTs normal after 12 months of Ursodeoxycholic acid. • Fatigue symptoms persist but participates in local PBC support group and has developed coping strategies.
Feedback: e Healthscope Issues Log
The Scarred Liver Project Team • • • Guru Aithal Dave Harman Becky Harris Neil Guha Tim Card Steve Ryder Martin James Emilie Wilkes Aquiline Chivinge AHSN – Nick Hamilton – Lucy Sitton-Kent Primary Care – Matt Jelpke – Sean Ottey – Ken Brown – Marcia Chamberlain