The Normal Newborn ASSESSMENT AND CARE Three transition
The Normal Newborn ASSESSMENT AND CARE

Three transition phases Phase One: the first hour Phase Two: from one to three hours Phase Three: from two to 12 hours
Priorities in first hour Cardiovascular assessment and support Thermoregulation Assessment and support of blood glucose Identification Observing urinary/meconium passage Observing for major anomalies and for apparent gestational age concerns
APGAR ASSESSMENT One and five minutes Meant to identify the need for neonatal resucitation
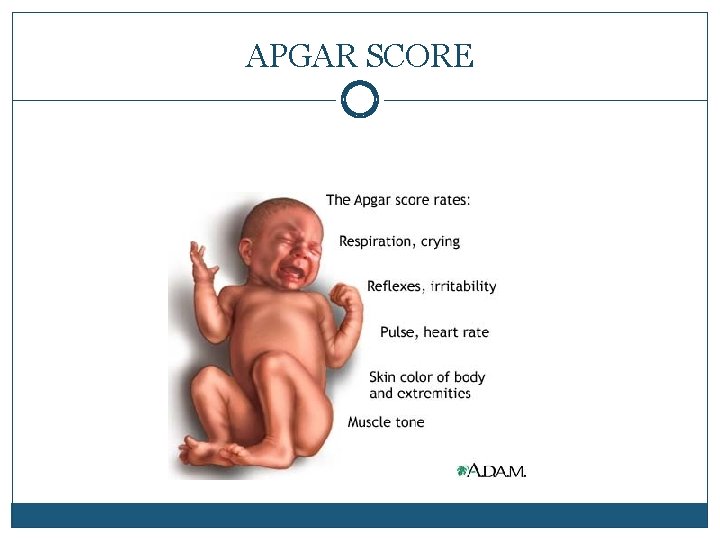
APGAR SCORE
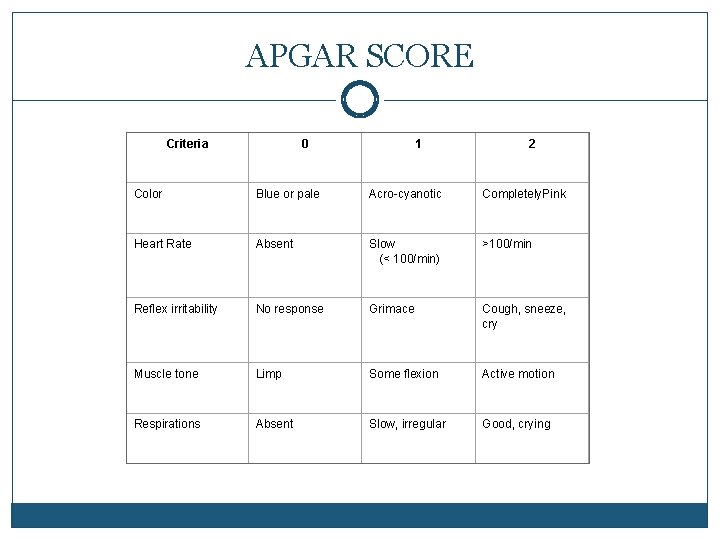
APGAR SCORE Criteria 0 1 2 Color Blue or pale Acro-cyanotic Completely. Pink Heart Rate Absent Slow (< 100/min) >100/min Reflex irritability No response Grimace Cough, sneeze, cry Muscle tone Limp Some flexion Active motion Respirations Absent Slow, irregular Good, crying
Additional signs of respiratory distress Persistant cyanosis Grunting respirations Flaring of the nostrils Retractions Respiratory rate >60 Heart rate >160 or <110
Maintaining thermoregulation Referred to as maintaining a neutral thermal environment Heat loss is minimal Oxygen consumption needs are at their lowest Hypothermia can cause Hypoglycemia Increased oxygen needs
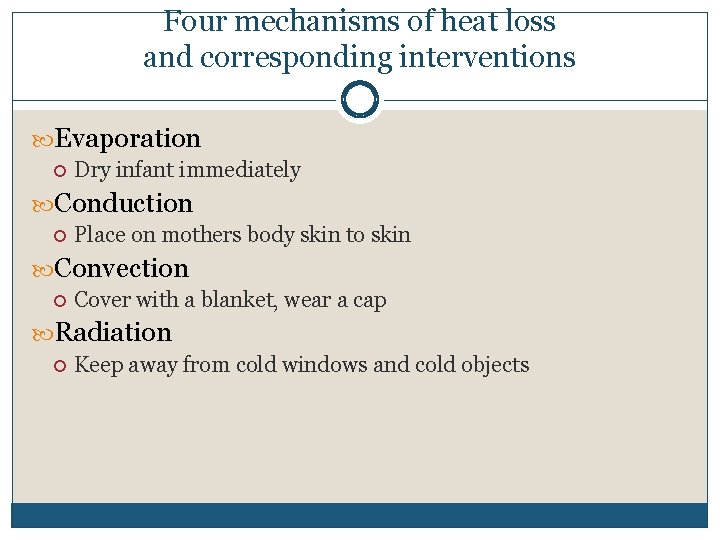
Four mechanisms of heat loss and corresponding interventions Evaporation Dry infant immediately Conduction Place on mothers body skin to skin Convection Cover with a blanket, wear a cap Radiation Keep away from cold windows and cold objects
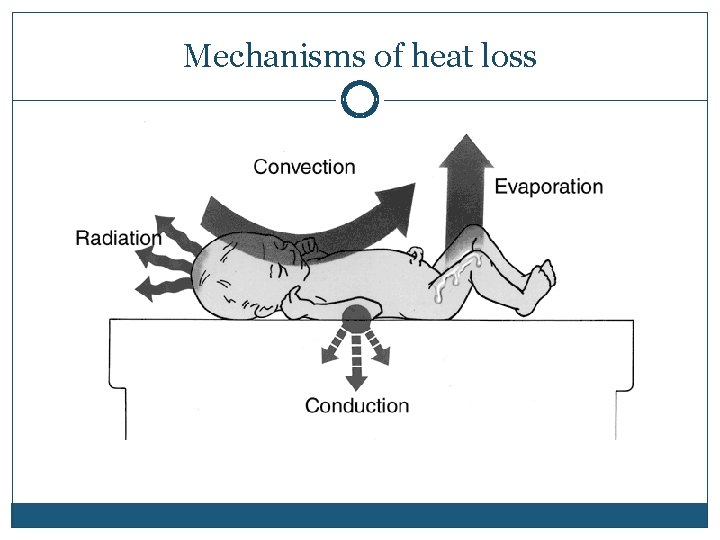
Mechanisms of heat loss
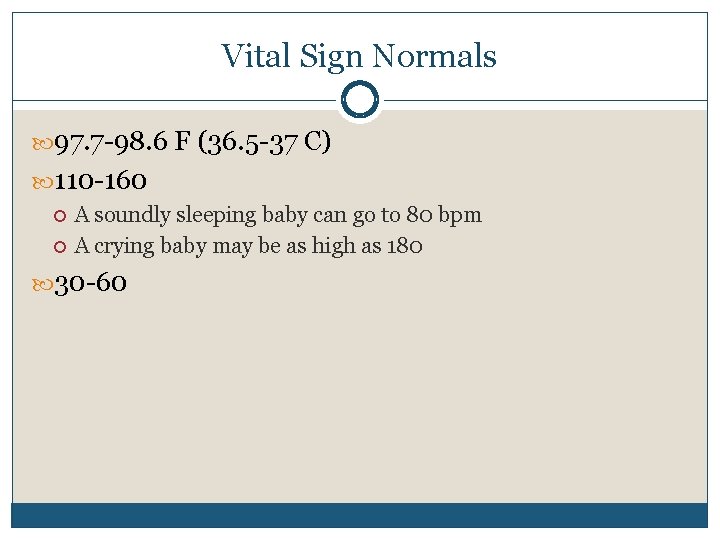
Vital Sign Normals 97. 7 -98. 6 F (36. 5 -37 C) 110 -160 A soundly sleeping baby can go to 80 bpm A crying baby may be as high as 180 30 -60
Voids and Stools Document from the moment of birth Urination sometimes missed in early minutes Generally expect both within the first 24 hours One really wet diaper day of age until milk is fully in.
Observation for Gestational Age Thorough assessment with Ballard Scale done later A quick assessment is done in the delivery room This enables infants earlier admission to the nursery and anticipatory intervention to the problems of pre and post term infants
Quick Assessment of Gestational Age Skin Vernix Hair Ears Breast tissue Genitalia Sole Creases Resting Posture

Cracked Skin

Abundant Lanugo
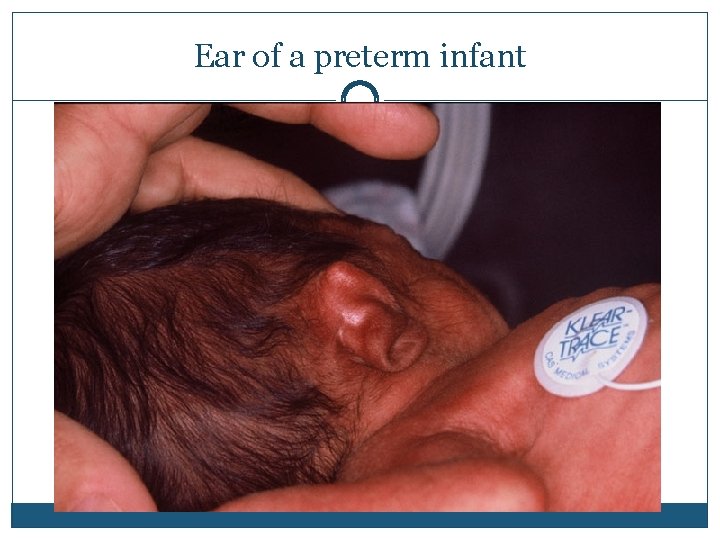
Ear of a preterm infant
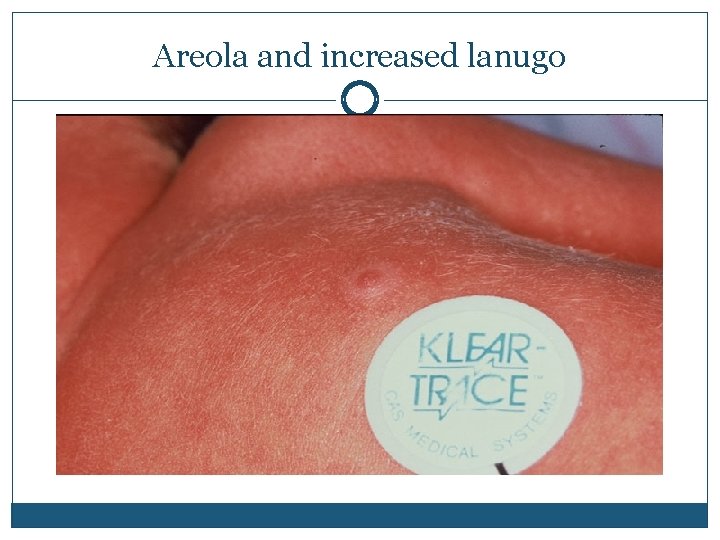
Areola and increased lanugo
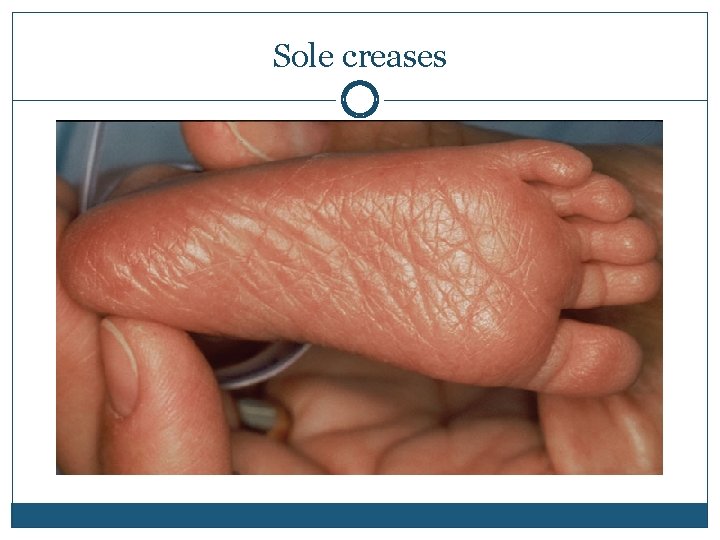
Sole creases
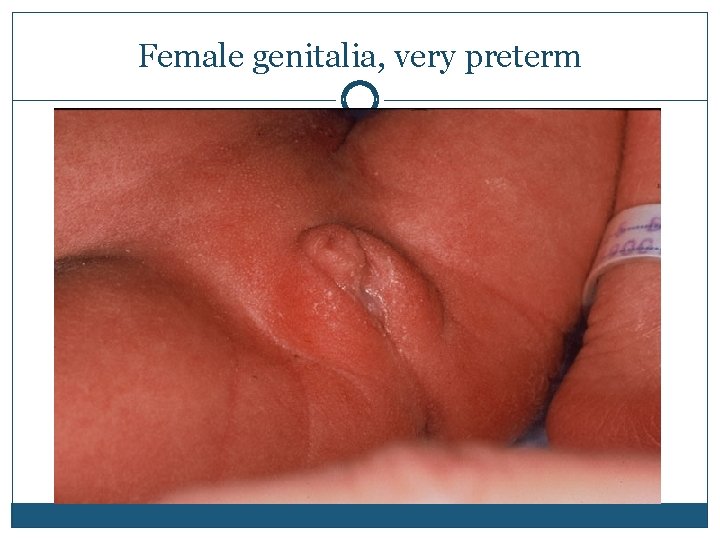
Female genitalia, very preterm
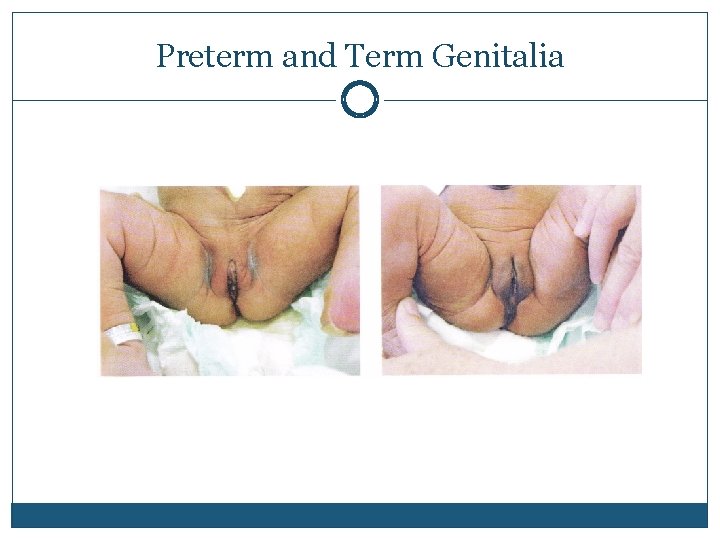
Preterm and Term Genitalia
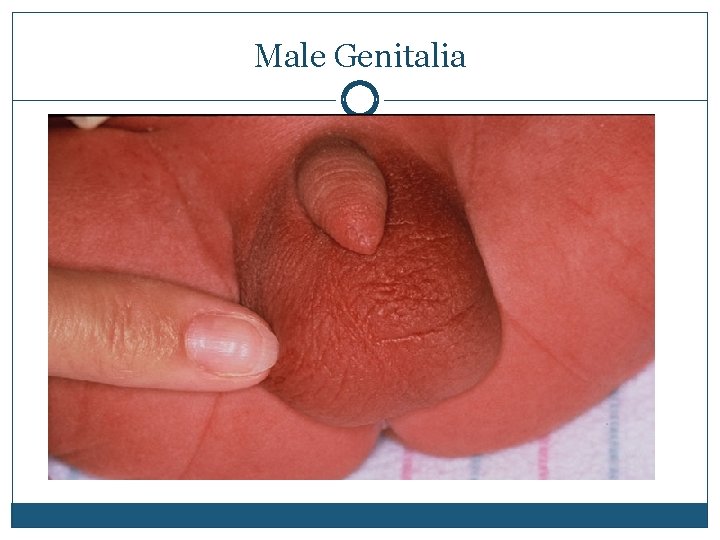
Male Genitalia
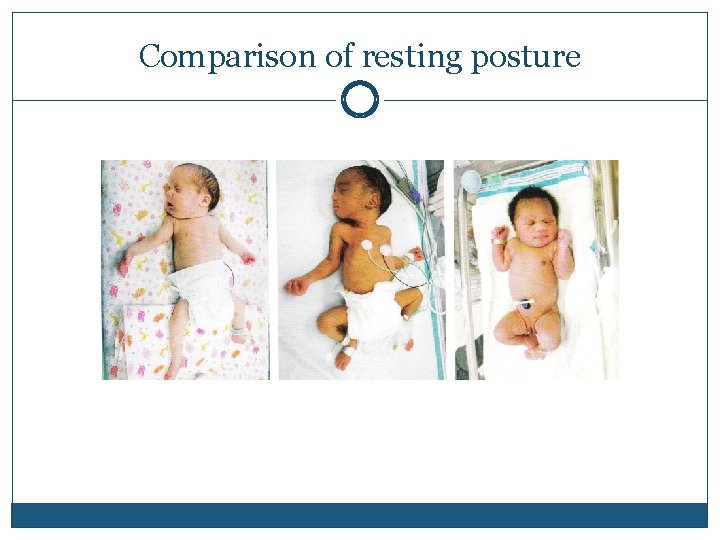
Comparison of resting posture
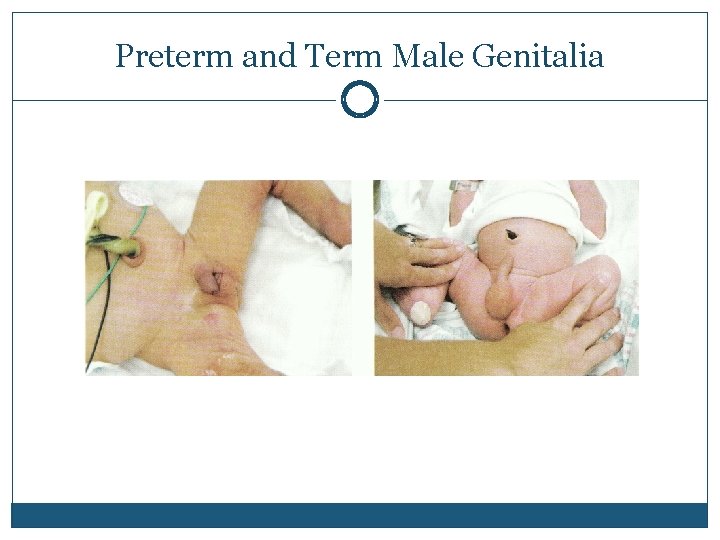
Preterm and Term Male Genitalia
Hypoglycemia Criteria vary from source to source LPN book says <40 RN book says <36 but a threapuetic objective of 45 mg/dl or greater The brain is dependent on a steady supply of glucose for its metabolism
Infants at Increased Risk for Hypoglycemia Preterm/postterm Infants of diabetic mothers Large for gestational age Small for gestational age Infants with Intrauterine growth retardation Asphyxiated infants Infants who are cold stressed Infants whose Moms took ritodrine or tgerbutaline to stop preterm labor
Symptoms of Hypoglycemia Jitteriness Poor suck Poor muscle tone Feeding difficulties Sweating High pitched cry Respiratory difficulty Weak cry Apnea Lethargy Low temperature Seizures
Hypoglycemia protocol Low risk infants have a serum glucose drawn only if symptomatic High risk infants will have one per a hospital protocol Protocol typically at birth and q 1 hour x 3
Routine Medications Erythromycin Eye Ointment Aquamephyton (vitamin K) First Hepatitis B vaccine HBIG if Mother is Hep B surface antigen positive
Physical Characteristics DURING PHASES TWO AND THREE
Nervous System: Reflexes Head lag Rooting reflex Moro reflex Suck Rooting Hand foot grasp Tonic Neck reflex Babinski Dancing reflex Trunk incurvation Magnet reflex Observe for symmetry
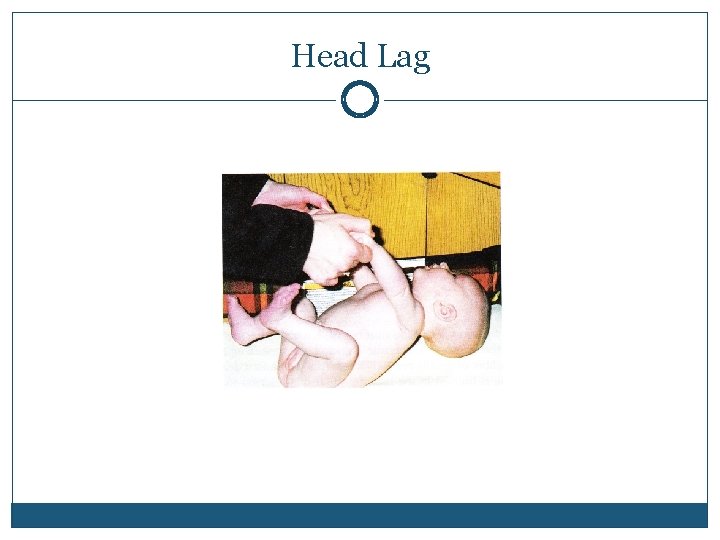
Head Lag
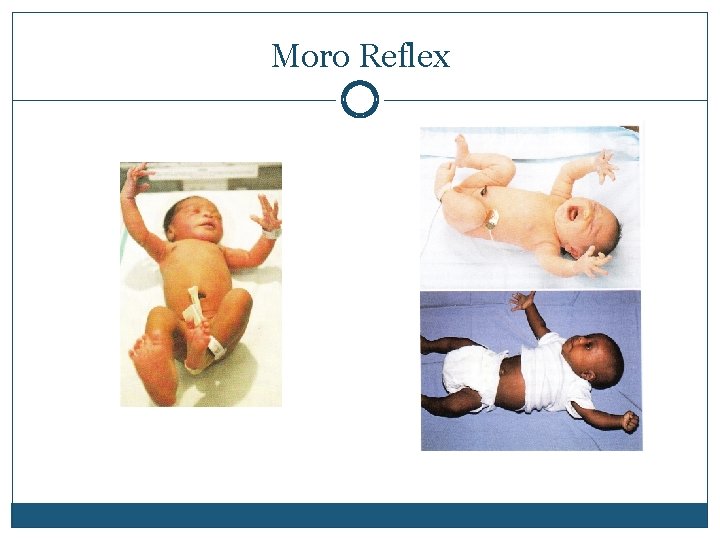
Moro Reflex
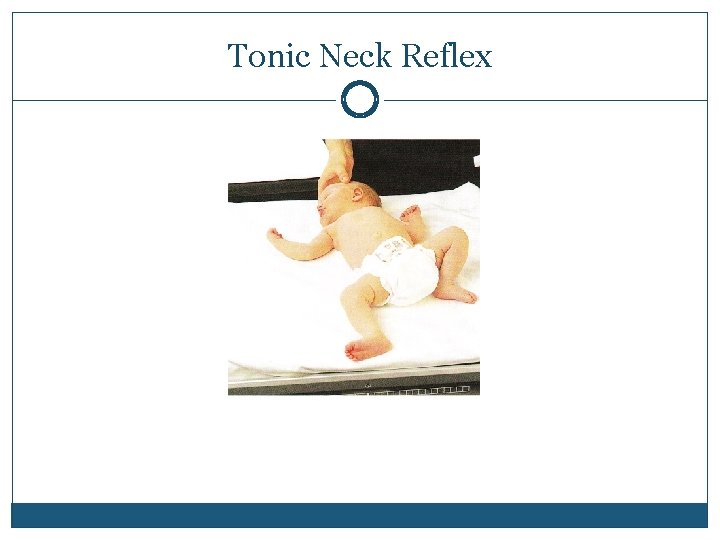
Tonic Neck Reflex
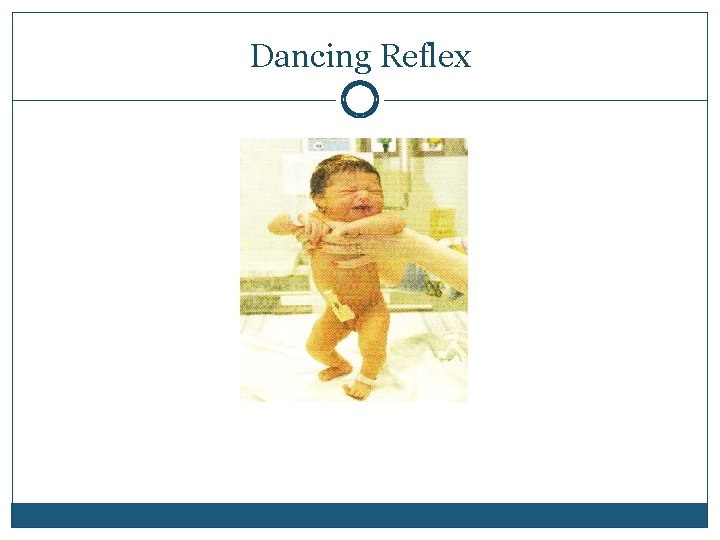
Dancing Reflex
Suck Reflex
Hand Grasp
Foot Grasp
Head circumference Molding Caput succedaneum Cephalohematoma Fontanelles Anterior closes between 12 -18 months Posterior closes by the end of the 2 nd month
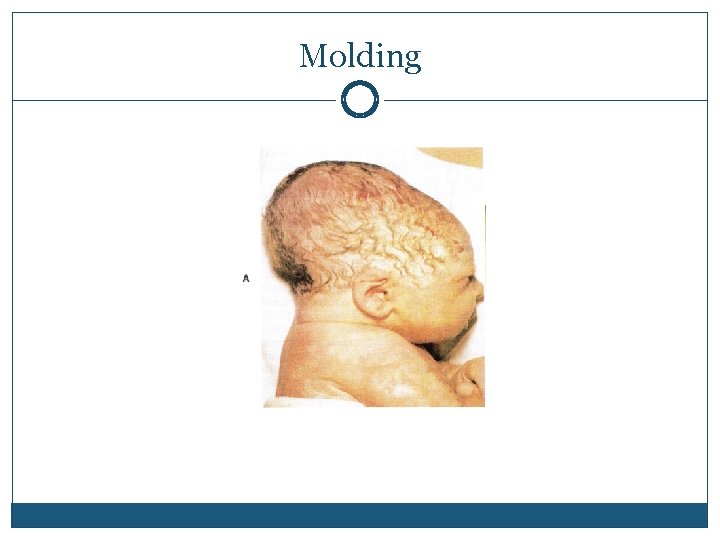
Molding
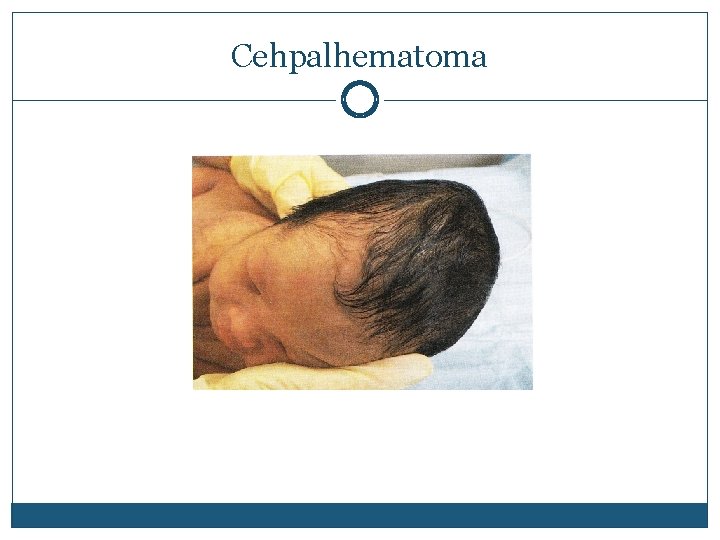
Cehpalhematoma
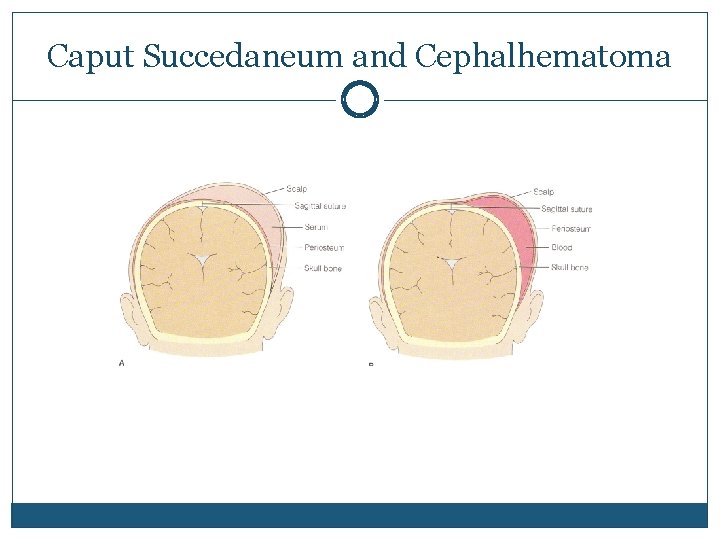
Caput Succedaneum and Cephalhematoma
Eyes Eye placement Epicanthal folds Blink reflex Discharge Pupil reaction Follows to midline
Hearing Check overall response to sudden sound Moro reflex Check for placement of ears Low set ears may indicate a congenital anomaly Most infants receive hearing screening within the first week of life

Respiratory and Cardiovascular Ongoing assessment of cardio respiratory status that has occurred since birth More thorough heart assessment Murmur may be present until fetal openings have completely closed however they must be carefully verified by pediatrician Femoral and brachial pulses Abdominal breathing; nose breathers
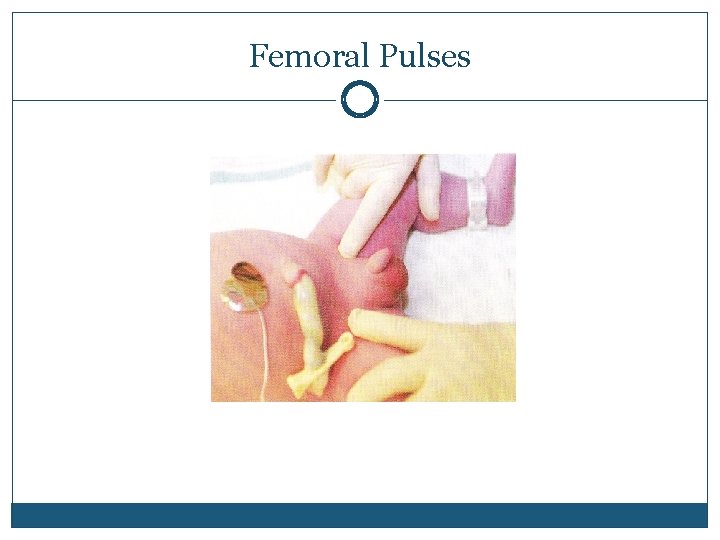
Femoral Pulses
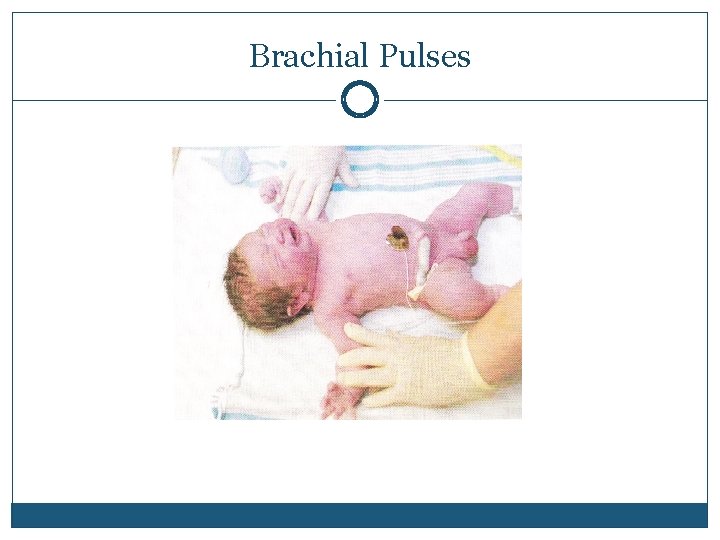
Brachial Pulses
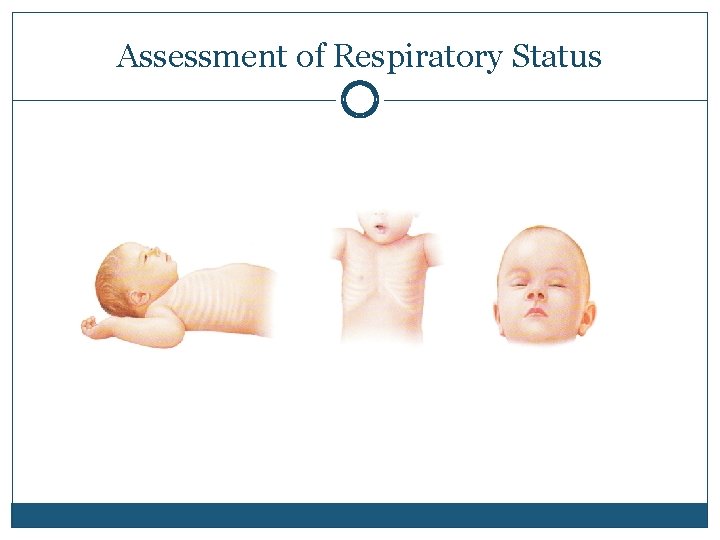
Assessment of Respiratory Status
Musculoskeletal Symmetry!! Five finger and five toes!!! Clavicles Movement of arms Hips for developmental hip dysplasia Lower legs/feet for “club foot” Back: curvatures, cysts or dimples
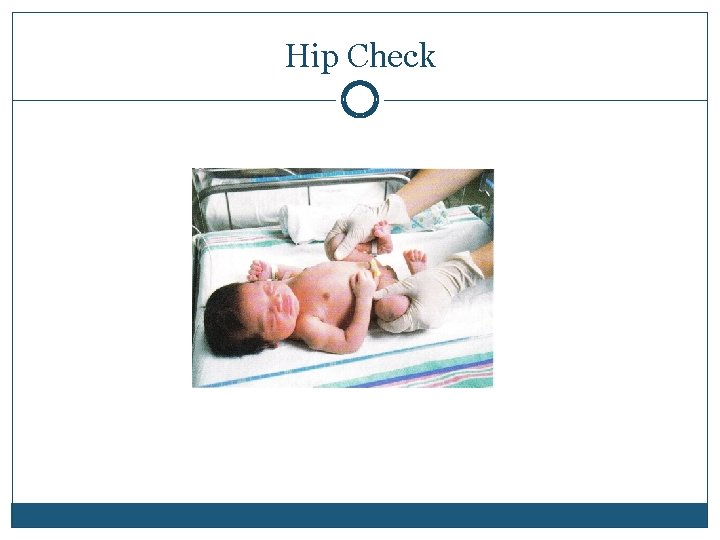
Hip Check

Hip Check Skin Folds
Genito. Urinary Male or female Male Testes descended Proper placement of meatus Female Teach parents about pseudomenstruation Always watch for and record voids!!!
Gastrointestinal Passage of meconium Placement and patency of anus Abdomen should be soft and non tender Round but not distended Bowel sounds are present after first hour of birth Umbilical cord inspection
Skin, many normal findings Acrocyanosis Desquamation Epstein’s Pearls Erythema toxicum Harlequin Color Milia Mongolian Spots Port Wine Stains *
The Normal Newborn CARE MEASURES FOR THE NORMAL NEWBORN PLUS A LITTLE MORE.

Jaundice Yellow coloring of an infants skin Common and is caused by the natural breakdown of RBCs in the infant after birth Is never considered normal in the first 24 hours.
Physiologic Jaundice Most jaundice in newborns is physiologic It peaks between 48 -72 hours Usually disappears within a week Usually benign Can become elevated to a point of concern for the baby
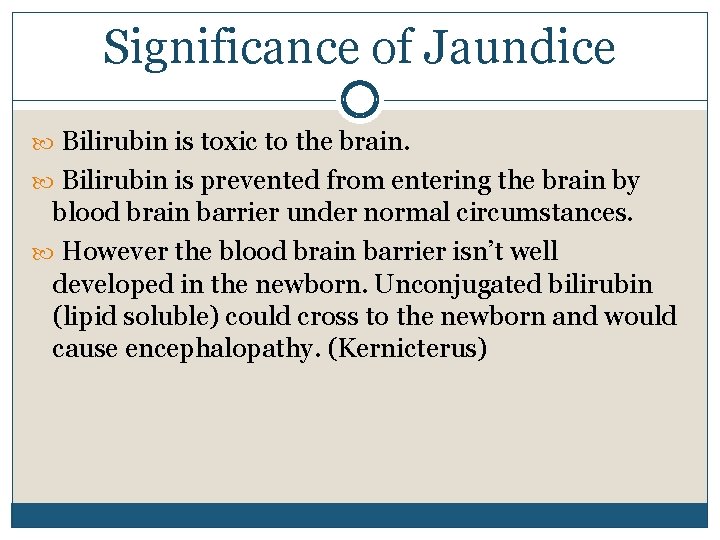
Significance of Jaundice Bilirubin is toxic to the brain. Bilirubin is prevented from entering the brain by blood brain barrier under normal circumstances. However the blood brain barrier isn’t well developed in the newborn. Unconjugated bilirubin (lipid soluble) could cross to the newborn and would cause encephalopathy. (Kernicterus)
Physiologic Jaundice Infants have extra RBCs due to fetal life They need to be broken down by the body Bilirubin is a component of the degradation of the RBCs. The liver is immature and does not conjugate and get rid of the bilirubin fast enough.
More data on Physiologic Jaundice RBC/Hgb level is higher than required Neonatal RBC: 4. 8 -7. 1 Infant: 4. 2 -5. 2 Neonatal Hbg 14 -24 Infant 11 -17 Cells containing fetal hemoglobin have a shorter life span
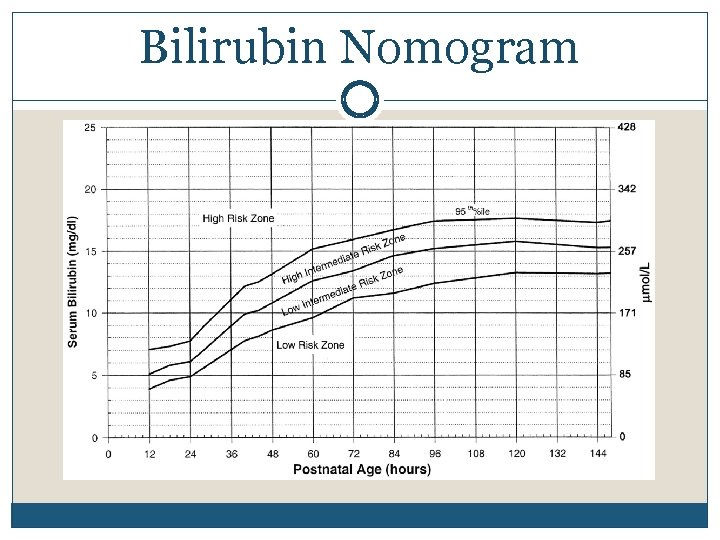
Bilirubin Nomogram
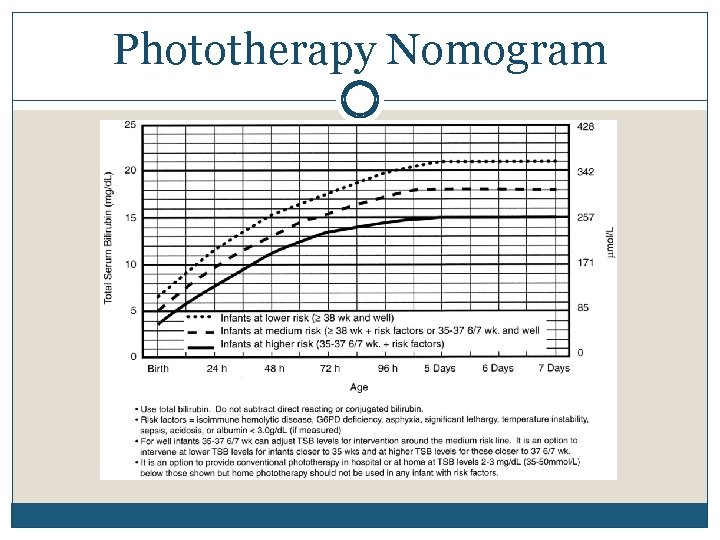
Phototherapy Nomogram
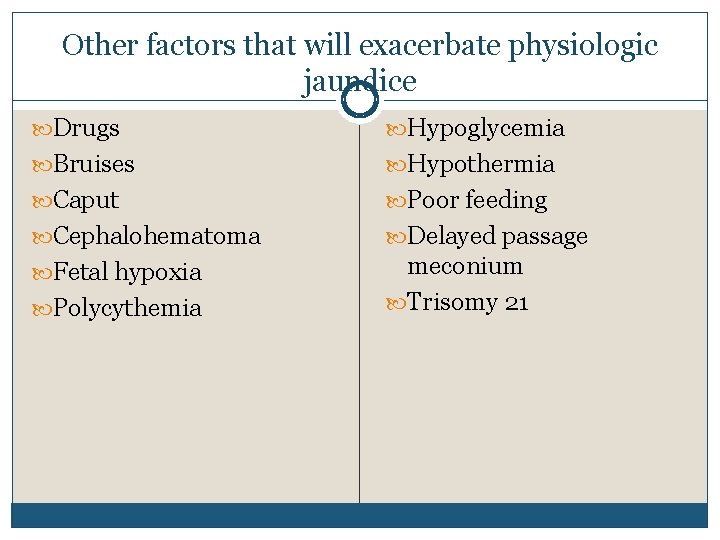
Other factors that will exacerbate physiologic jaundice Drugs Hypoglycemia Bruises Hypothermia Caput Poor feeding Cephalohematoma Delayed passage Fetal hypoxia meconium Trisomy 21 Polycythemia
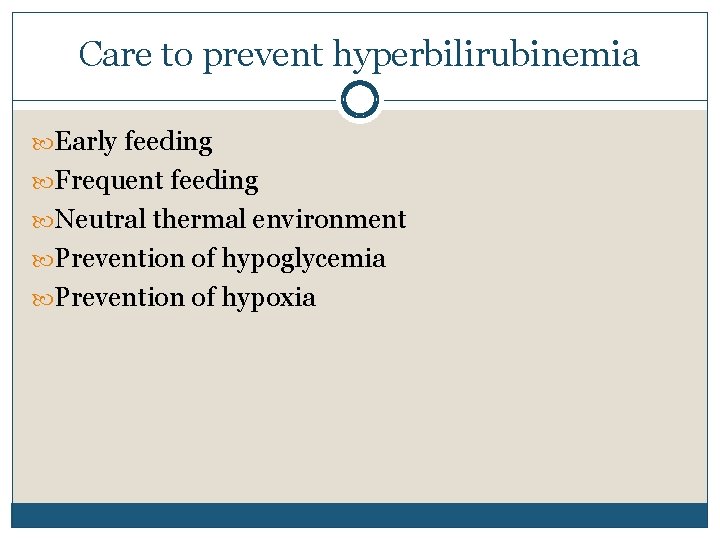
Care to prevent hyperbilirubinemia Early feeding Frequent feeding Neutral thermal environment Prevention of hypoglycemia Prevention of hypoxia
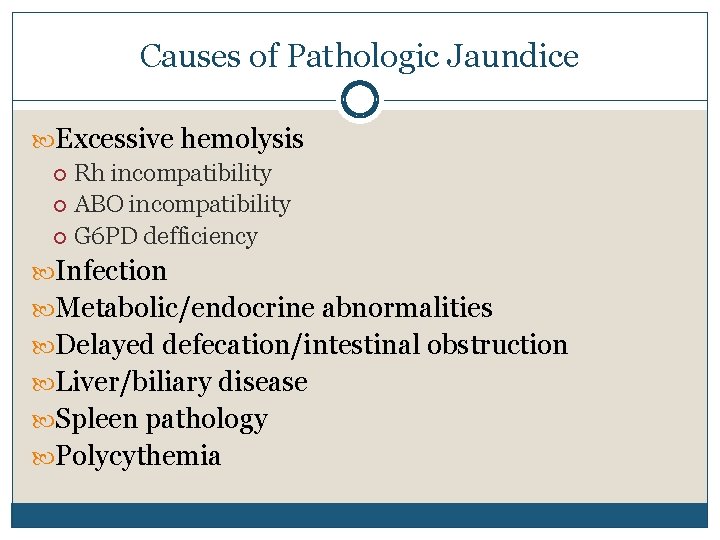
Causes of Pathologic Jaundice Excessive hemolysis Rh incompatibility ABO incompatibility G 6 PD defficiency Infection Metabolic/endocrine abnormalities Delayed defecation/intestinal obstruction Liver/biliary disease Spleen pathology Polycythemia

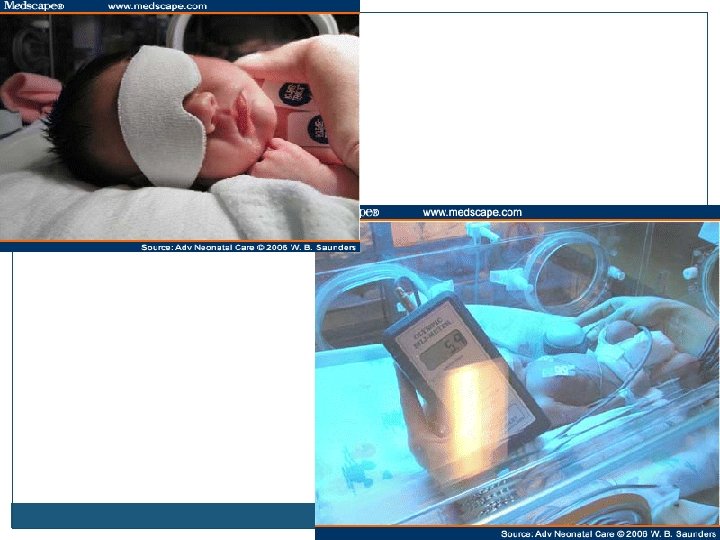
PHOTOTHERAPY
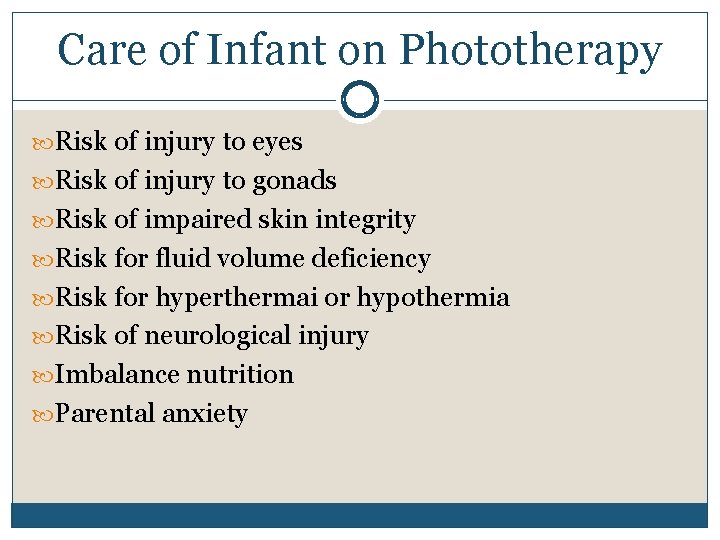
Care of Infant on Phototherapy Risk of injury to eyes Risk of injury to gonads Risk of impaired skin integrity Risk for fluid volume deficiency Risk for hyperthermai or hypothermia Risk of neurological injury Imbalance nutrition Parental anxiety
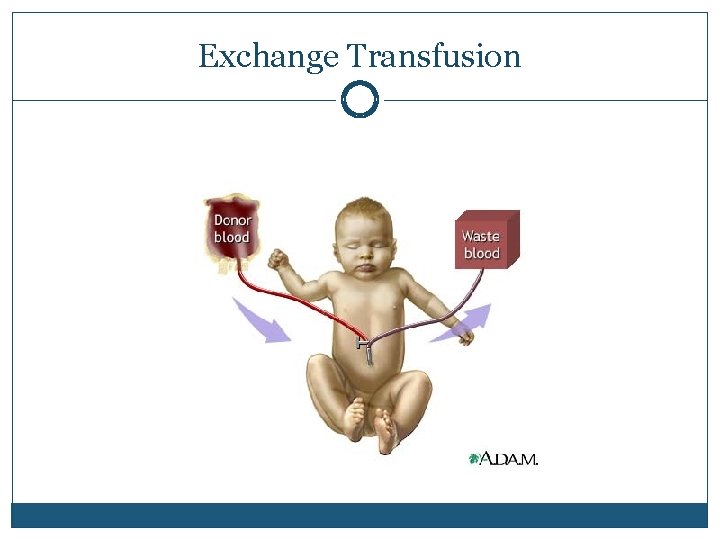
Exchange Transfusion
Isn’t he lovely?
Other Newborn Care issues Bulb suctioning: RN 731 LPN 286 Umb cord care: RN 733 LPN 219 Heel Sticks: RN 741 -43 LPN 219 Circumcision: RN 755 See patient teaching page 757 LPN 290
- Slides: 71