The Neural Control of Breathing CNS 6 2
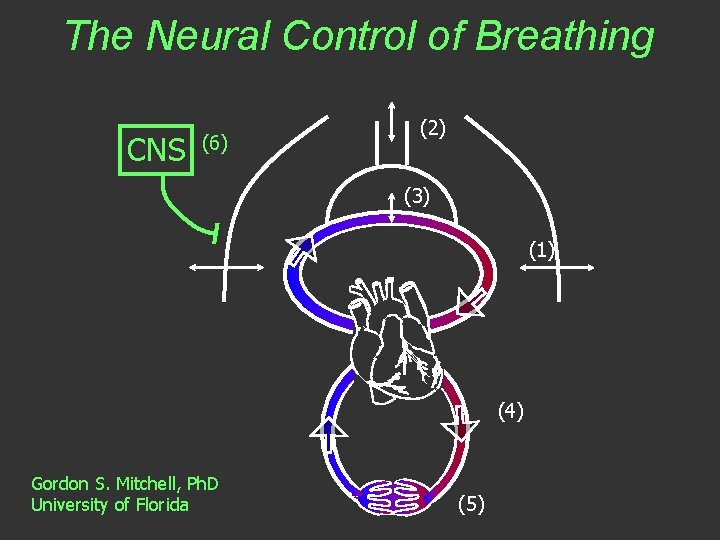
The Neural Control of Breathing CNS (6) (2) (3) (1) (4) Gordon S. Mitchell, Ph. D University of Florida (5)
The brain and breathing: What is the connection? Spinal cord: pump muscles Cranial nerves: upper airway muscles controlling resistance
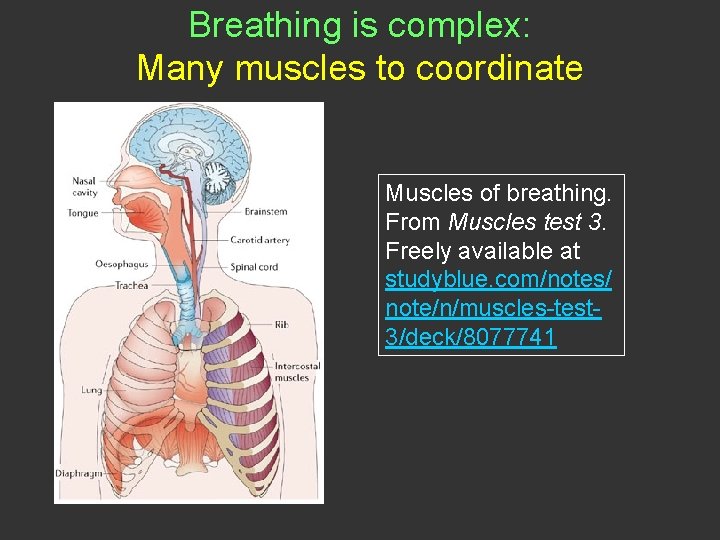
Breathing is complex: Many muscles to coordinate Picture Muscles of breathing. From Muscles test 3. Freely available at studyblue. com/notes/ note/n/muscles-test 3/deck/8077741
visual saccades Motor Behaviors lifting running breathing heart beat
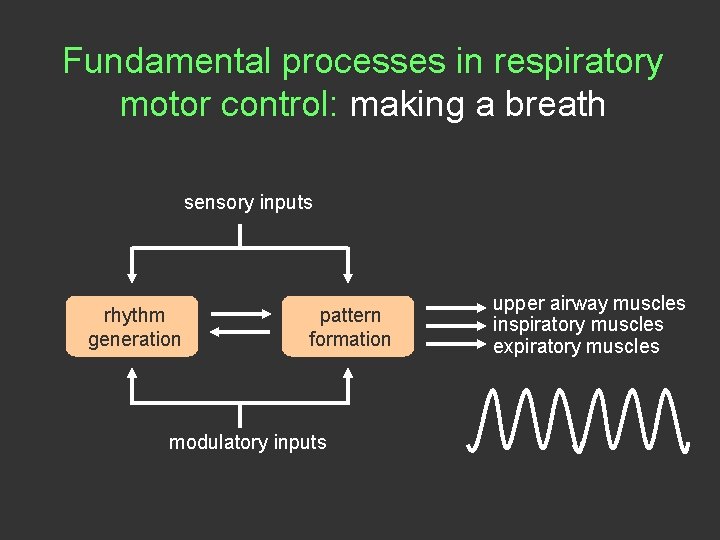
Fundamental processes in respiratory motor control: making a breath sensory inputs rhythm generation pattern formation modulatory inputs upper airway muscles inspiratory muscles expiratory muscles
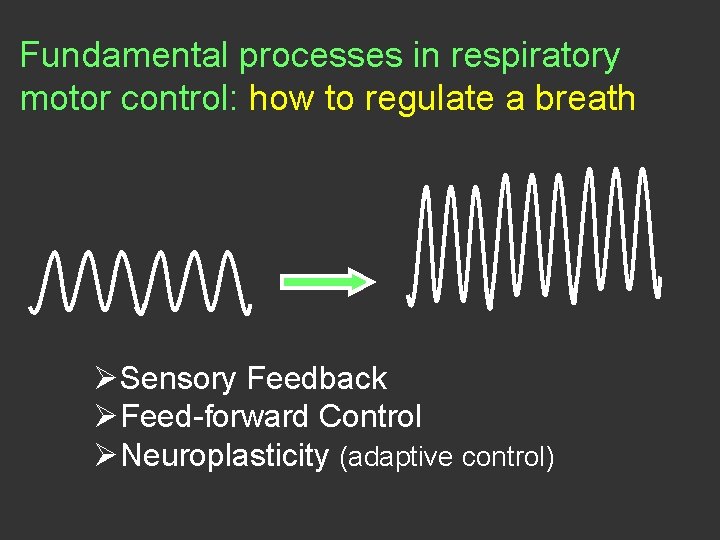
Fundamental processes in respiratory motor control: how to regulate a breath ØSensory Feedback ØFeed-forward Control ØNeuroplasticity (adaptive control)
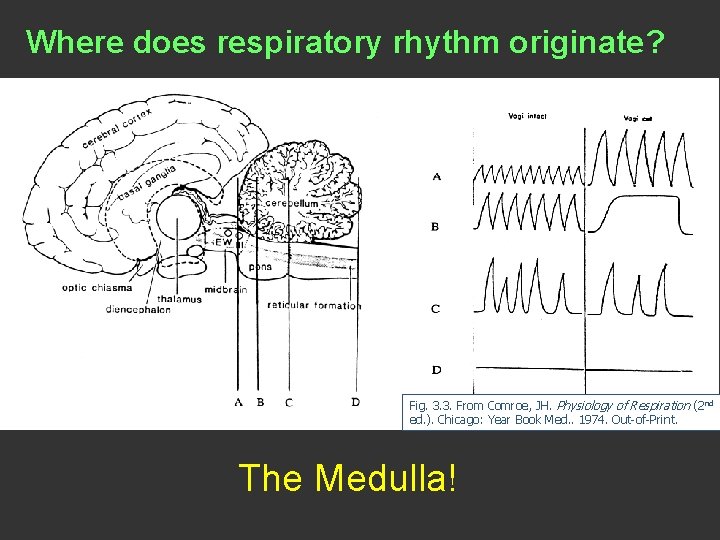
Where does respiratory rhythm originate? Fig. 3. 3. From Comroe, JH. Physiology of Respiration (2 nd ed. ). Chicago: Year Book Med. . 1974. Out-of-Print. The Medulla!
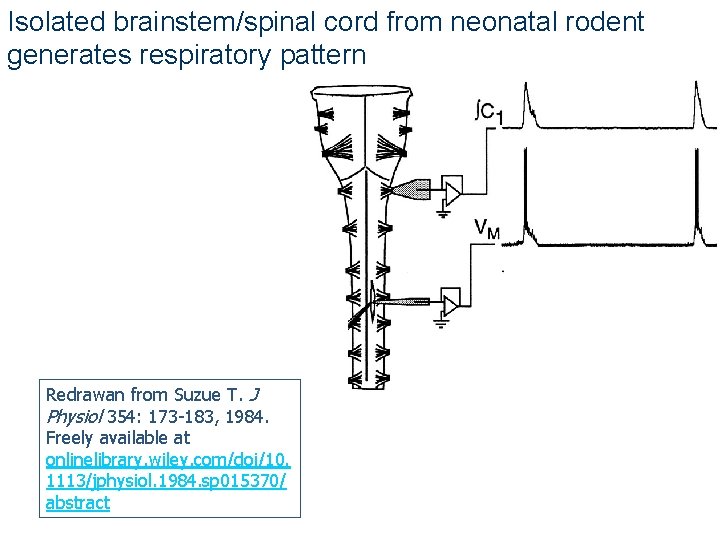
Isolated brainstem/spinal cord from neonatal rodent generates respiratory pattern Redrawan from Suzue T. J Physiol 354: 173 -183, 1984. Freely available at onlinelibrary. wiley. com/doi/10. 1113/jphysiol. 1984. sp 015370/ abstract
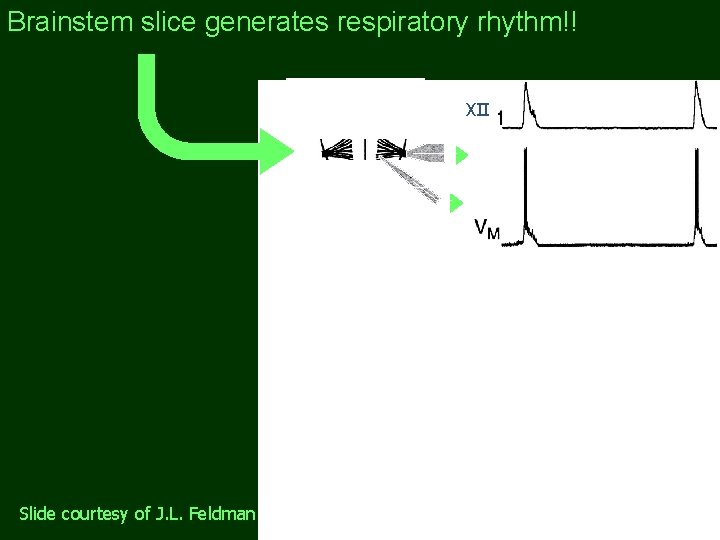
Brainstem slice generates respiratory rhythm!! ∫XII Slide courtesy of J. L. Feldman
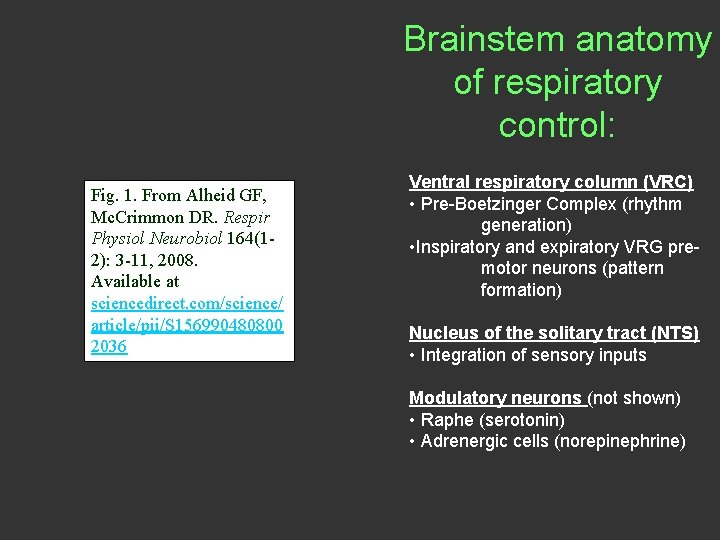
Brainstem anatomy of respiratory control: Fig. 1. From Alheid GF, Mc. Crimmon DR. Respir Physiol Neurobiol 164(12): 3 -11, 2008. Available at sciencedirect. com/science/ article/pii/S 156990480800 2036 Ventral respiratory column (VRC) • Pre-Boetzinger Complex (rhythm generation) • Inspiratory and expiratory VRG premotor neurons (pattern formation) Nucleus of the solitary tract (NTS) • Integration of sensory inputs Modulatory neurons (not shown) • Raphe (serotonin) • Adrenergic cells (norepinephrine)
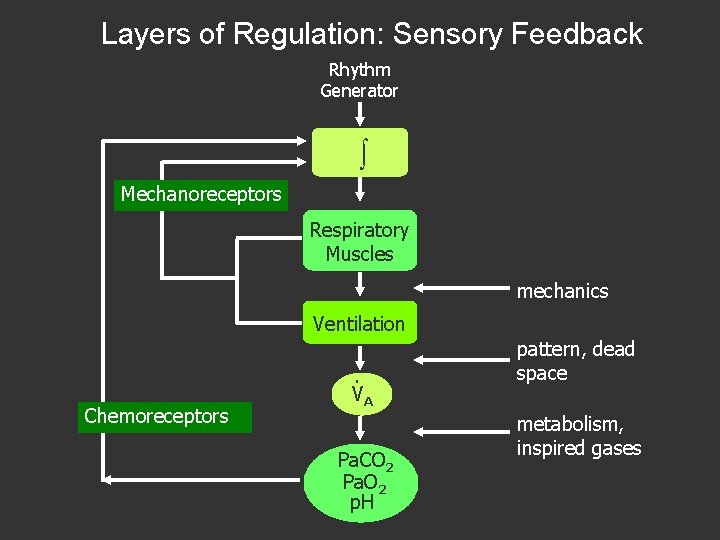
Layers of Regulation: Sensory Feedback Rhythm Generator Mechanoreceptors Respiratory Muscles mechanics Ventilation Chemoreceptors . VA Pa. CO 2 Pa. O 2 p. H pattern, dead space metabolism, inspired gases
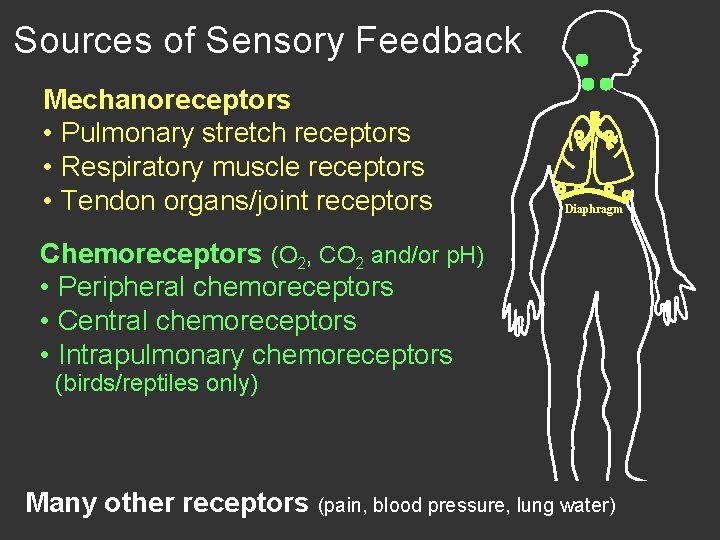
Sources of Sensory Feedback Mechanoreceptors • Pulmonary stretch receptors • Respiratory muscle receptors • Tendon organs/joint receptors Diaphragm Chemoreceptors (O 2, CO 2 and/or p. H) • Peripheral chemoreceptors • Central chemoreceptors • Intrapulmonary chemoreceptors (birds/reptiles only) Many other receptors (pain, blood pressure, lung water)
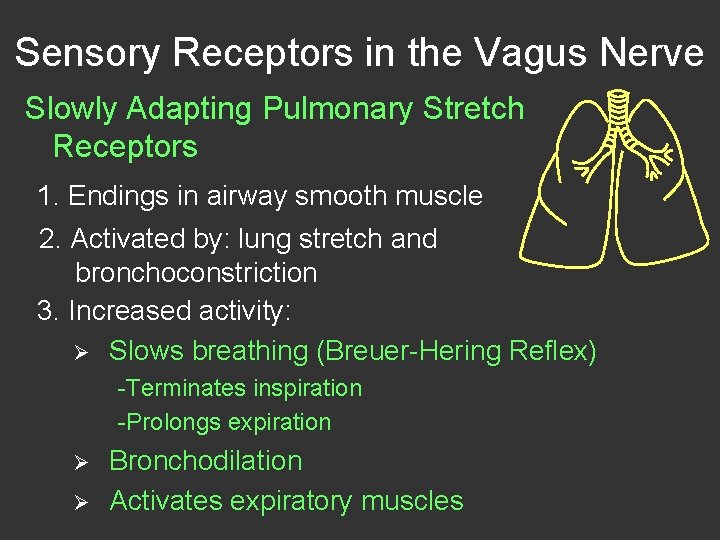
Sensory Receptors in the Vagus Nerve Slowly Adapting Pulmonary Stretch Receptors 1. Endings in airway smooth muscle 2. Activated by: lung stretch and bronchoconstriction 3. Increased activity: Ø Slows breathing (Breuer-Hering Reflex) -Terminates inspiration -Prolongs expiration Ø Ø Bronchodilation Activates expiratory muscles
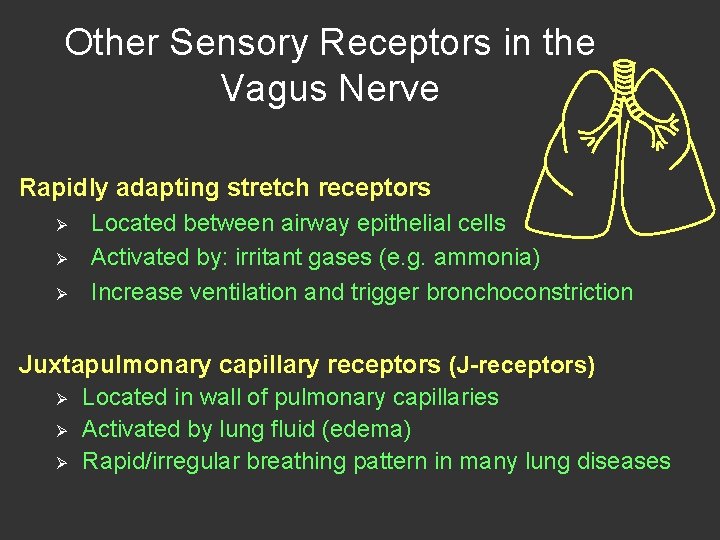
Other Sensory Receptors in the Vagus Nerve Rapidly adapting stretch receptors Ø Located between airway epithelial cells Ø Activated by: irritant gases (e. g. ammonia) Ø Increase ventilation and trigger bronchoconstriction Juxtapulmonary capillary receptors (J-receptors) Ø Located in wall of pulmonary capillaries Ø Activated by lung fluid (edema) Ø Rapid/irregular breathing pattern in many lung diseases
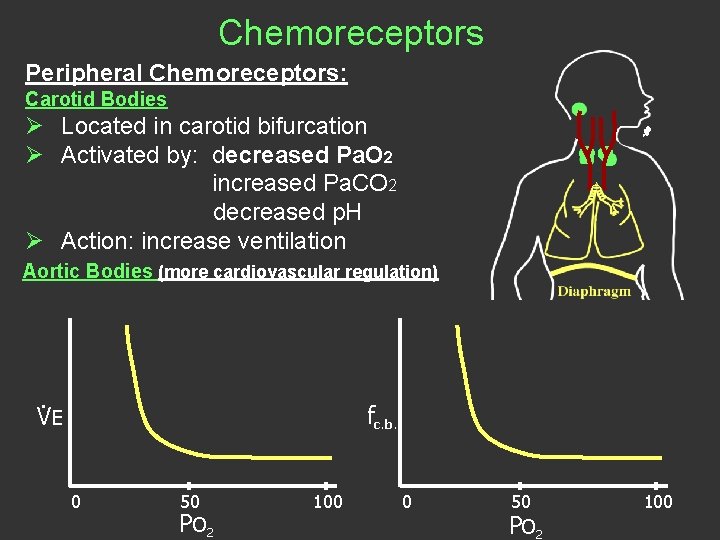
Chemoreceptors Peripheral Chemoreceptors: Carotid Bodies Ø Located in carotid bifurcation Ø Activated by: decreased Pa. O 2 increased Pa. CO 2 decreased p. H Ø Action: increase ventilation Aortic Bodies (more cardiovascular regulation) . fc. b. VE 0 50 PO 2 100
Central (CNS) CO 2 sensitive neurons Ø Multiple sites in brainstem and cerebellum Ø Relative significance of different sites remains controversial Ø Increased CO 2 stimulates breathing Ø The chemoreflex: Fig. 2. From Mitchell GS et al. Respiration. In: Encyclopedia of Neuroscience , edited by LR Squire. 2009. vol. 8, pp. 121130. Oxford: Academic.
CO 2 sensitive Intrapulmonary Chemoreceptors in Birds and Reptiles Fig. 4. From Powell et al. Respir. Physiol. 74: 285 -298, 1988. Available at sciencedirect. com/science/article/pii/ 0034568788900370 Fig. 1. From Milsom et al. Respir. Physiol. 74: 285 -298, 1988. Available at sciencedirect. com/science/article/pii/ S 1569904804002125 CO 2 sensitive chemoreceptor exist in bird and reptile (not mammal) lungs. CO 2 inhibits intrapulmonary chemoreceptors, and they inhibit breathing. Thus, increased lung CO 2 stimulates breathing. They are a well-studied and powerful chemoreceptor in these species.
Integrated Ventilatory Responses Ø Chemoreceptor feedback v CO 2 and O 2 v Interactions among stimuli Ø Feed-forward regulation v Exercise hyperpnea Ø Plasticity v Persistent responses to repetitive/chronic disturbances
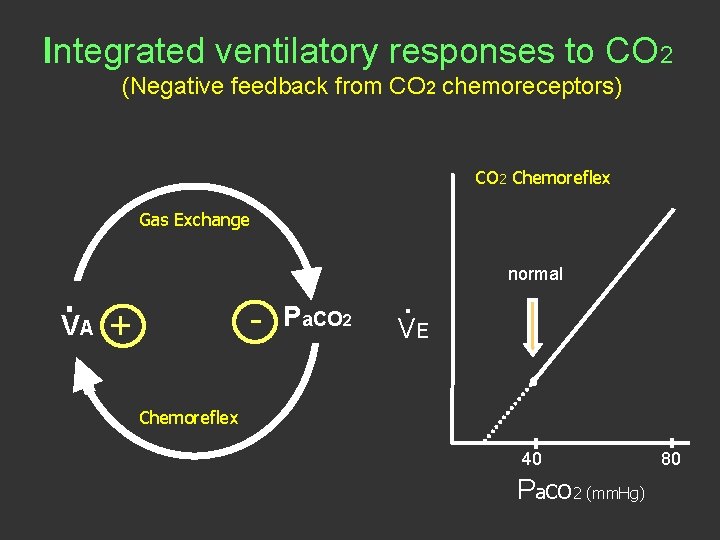
Integrated ventilatory responses to CO 2 (Negative feedback from CO 2 chemoreceptors) CO 2 Chemoreflex Gas Exchange . - VA + Pa. CO 2 . normal VE Chemoreflex 40 Pa. CO 2 (mm. Hg) 80
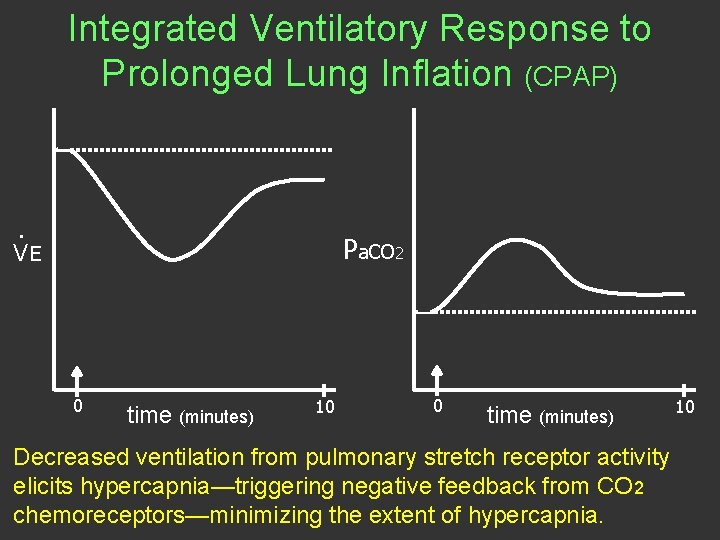
Integrated Ventilatory Response to Prolonged Lung Inflation (CPAP) . Pa. CO 2 VE 0 time (minutes) 10 0 time (minutes) Decreased ventilation from pulmonary stretch receptor activity elicits hypercapnia—triggering negative feedback from CO 2 chemoreceptors—minimizing the extent of hypercapnia. 10
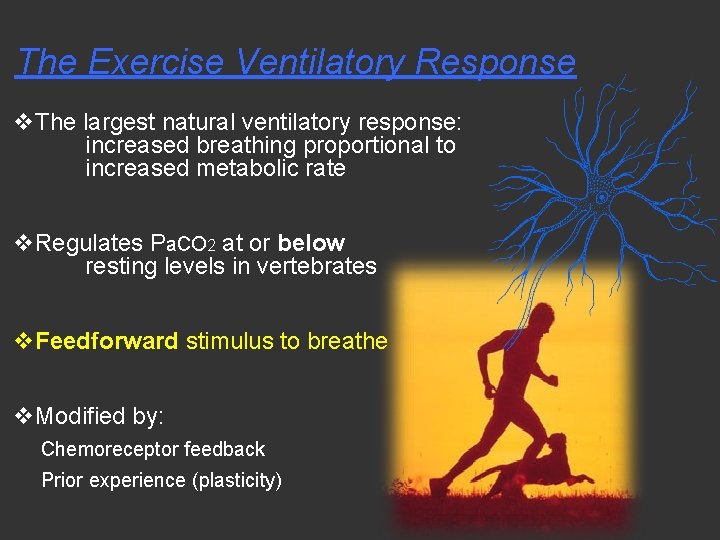
The Exercise Ventilatory Response v. The largest natural ventilatory response: increased breathing proportional to increased metabolic rate v. Regulates Pa. CO 2 at or below resting levels in vertebrates v. Feedforward stimulus to breathe v. Modified by: Chemoreceptor feedback Prior experience (plasticity)
Integrated ventilatory responses to hypoxia and hyperoxia: chemoreceptor feedback and respiratory plasticity ØAcute hypoxia ØAnesthesia ØHypoxia and sleep ØChronic hypoxia (altitude) ØIntermittent hypoxia ØPerinatal hyperoxia
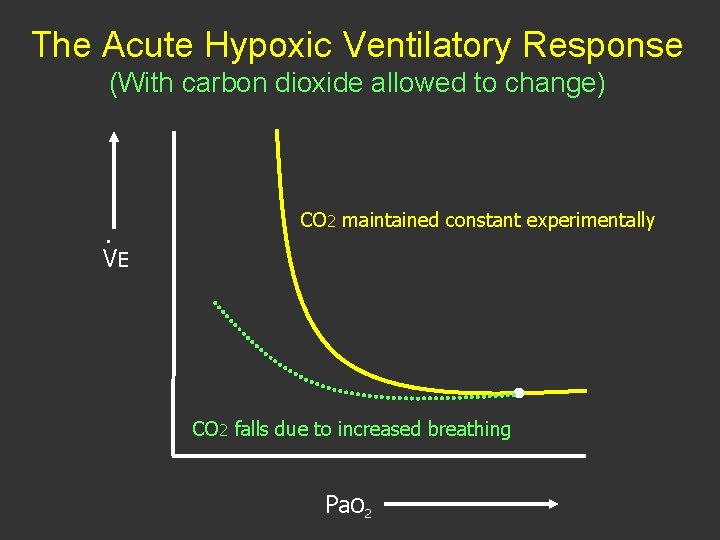
The Acute Hypoxic Ventilatory Response (With carbon dioxide allowed to change) . VE CO 2 maintained constant experimentally CO 2 falls due to increased breathing Pa. O 2
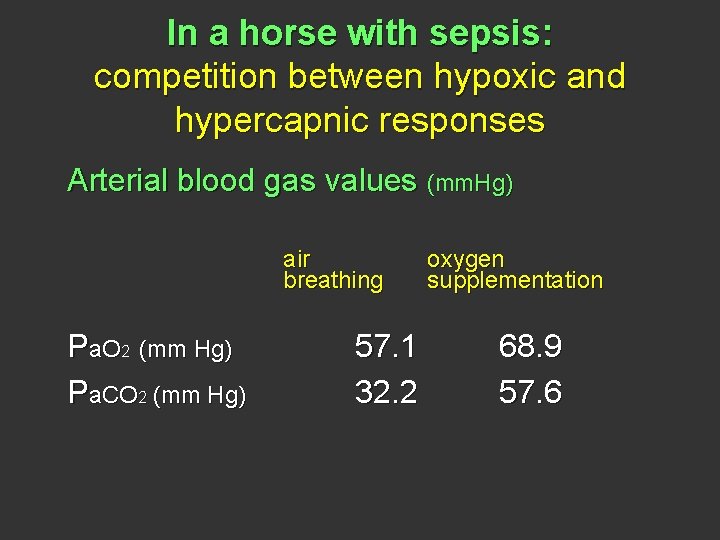
In a horse with sepsis: competition between hypoxic and hypercapnic responses Arterial blood gas values (mm. Hg) air breathing Pa. O 2 (mm Hg) Pa. CO 2 (mm Hg) 57. 1 32. 2 oxygen supplementation 68. 9 57. 6
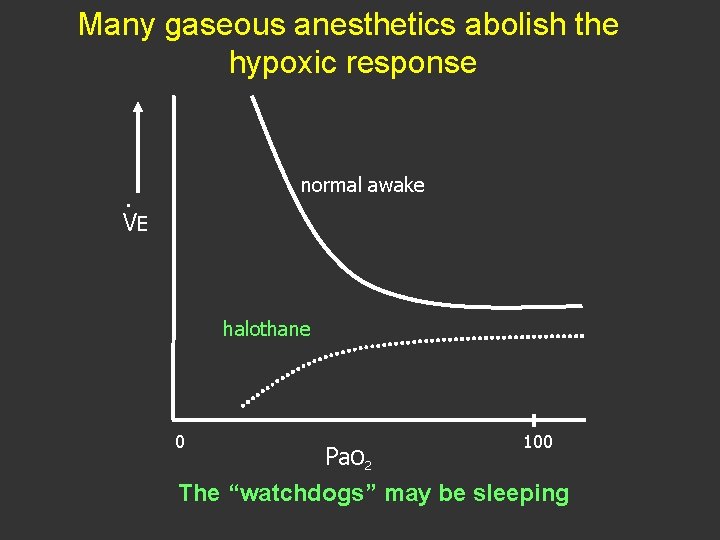
Many gaseous anesthetics abolish the hypoxic response normal awake . VE halothane 0 100 Pa. O 2 The “watchdogs” may be sleeping
Periodic Breathing during sleep at altitude: increased chemosensitivity/CO 2 apneic threshold interaction Fig. 2, top two graphs. Berssenbrugge A et al. J Physiol 343: 507 -524, 1983. Freely available at onlinelibrary. wiley. com/doi/10. 1113/jphysiol. 1983. s p 014906/pdf
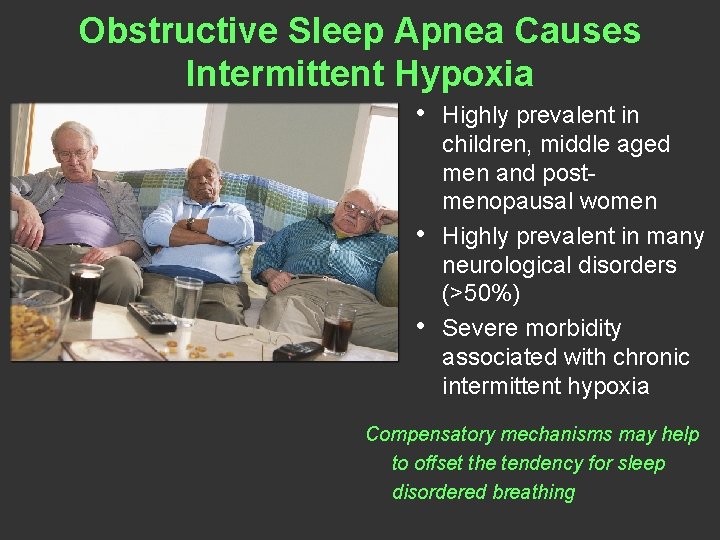
Obstructive Sleep Apnea Causes Intermittent Hypoxia • • • Highly prevalent in children, middle aged men and postmenopausal women Highly prevalent in many neurological disorders (>50%) Severe morbidity associated with chronic intermittent hypoxia Compensatory mechanisms may help to offset the tendency for sleep disordered breathing
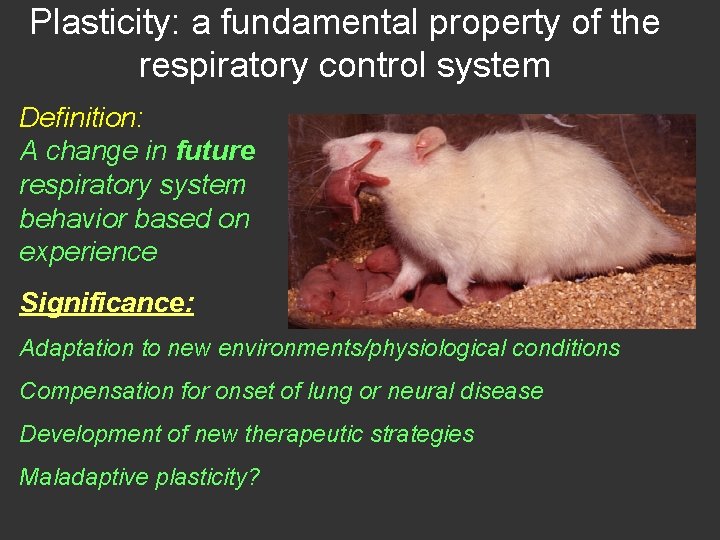
Plasticity: a fundamental property of the respiratory control system Definition: A change in future respiratory system behavior based on experience Significance: Adaptation to new environments/physiological conditions Compensation for onset of lung or neural disease Development of new therapeutic strategies Maladaptive plasticity?
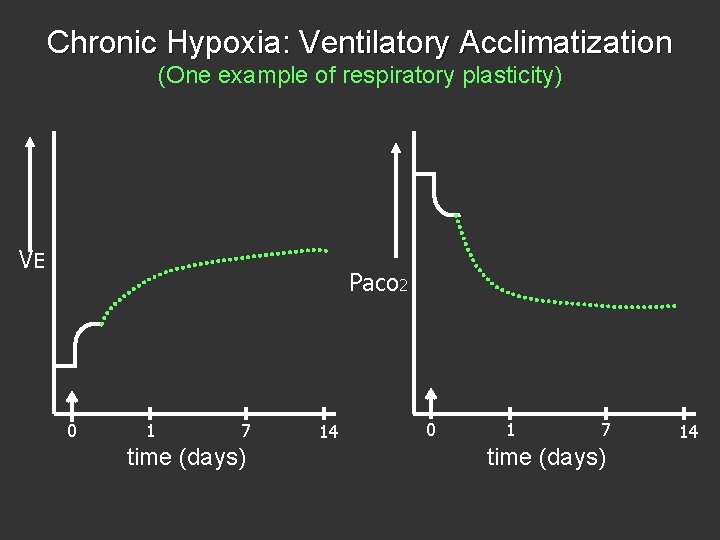
Chronic Hypoxia: Ventilatory Acclimatization (One example of respiratory plasticity) V. E Pa. CO 2 0 1 7 time (days) 14
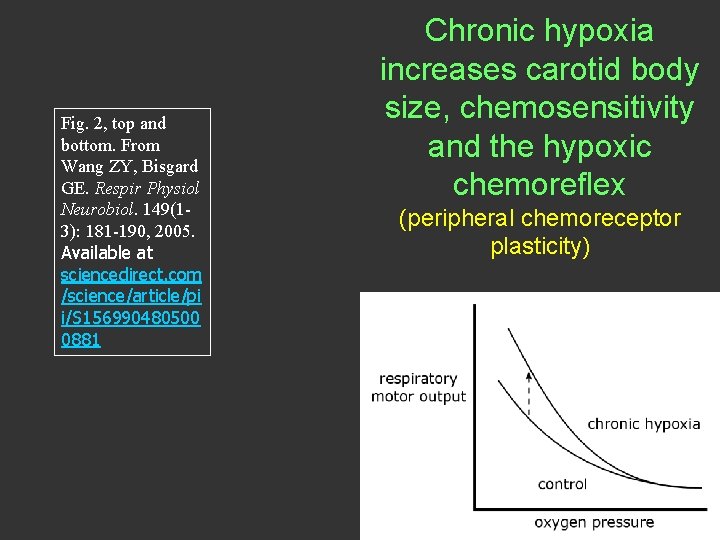
Fig. 2, top and bottom. From Wang ZY, Bisgard GE. Respir Physiol Neurobiol. 149(13): 181 -190, 2005. Available at sciencedirect. com /science/article/pi i/S 156990480500 0881 Chronic hypoxia increases carotid body size, chemosensitivity and the hypoxic chemoreflex (peripheral chemoreceptor plasticity)
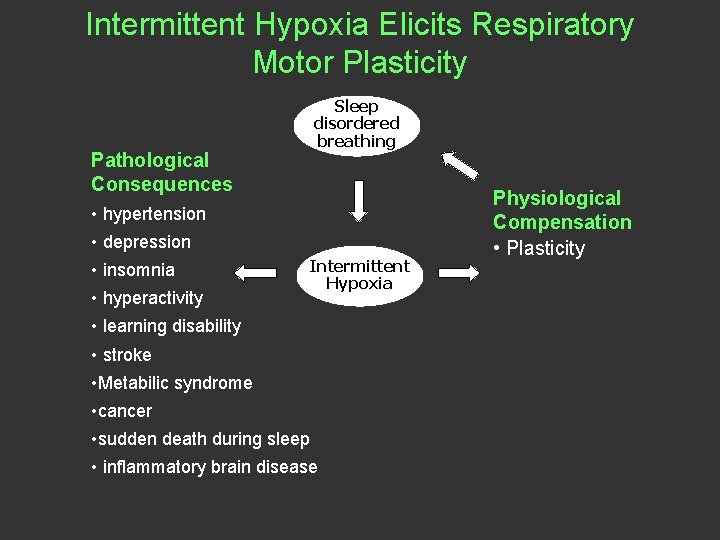
Intermittent Hypoxia Elicits Respiratory Motor Plasticity Sleep disordered breathing Pathological Consequences • hypertension • depression • insomnia • hyperactivity Intermittent Hypoxia • learning disability • stroke • Metabilic syndrome • cancer • sudden death during sleep • inflammatory brain disease Physiological Compensation • Plasticity
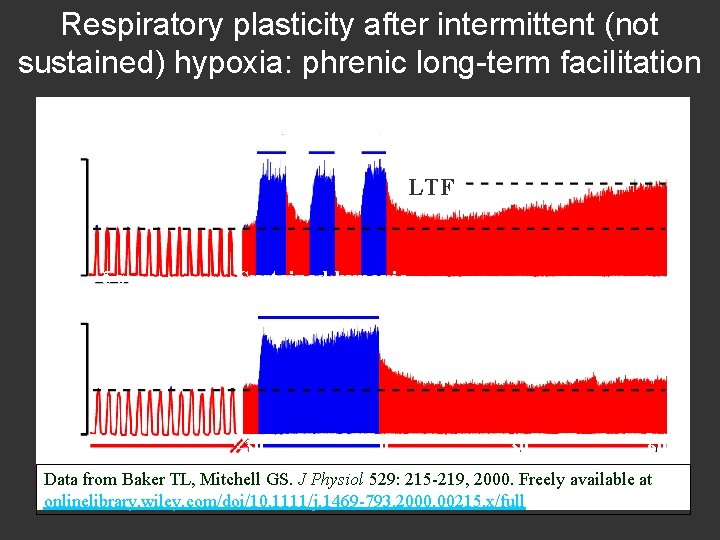
Respiratory plasticity after intermittent (not sustained) hypoxia: phrenic long-term facilitation respiratory motor output Intermittent hypoxia LTF 5 s Sustained hypoxia -30 0 30 60 pre-hypoxia minutes post-hypoxia Data from Baker TL, Mitchell GS. J Physiol 529: 215 -219, 2000. Freely available at onlinelibrary. wiley. com/doi/10. 1111/j. 1469 -793. 2000. 00215. x/full
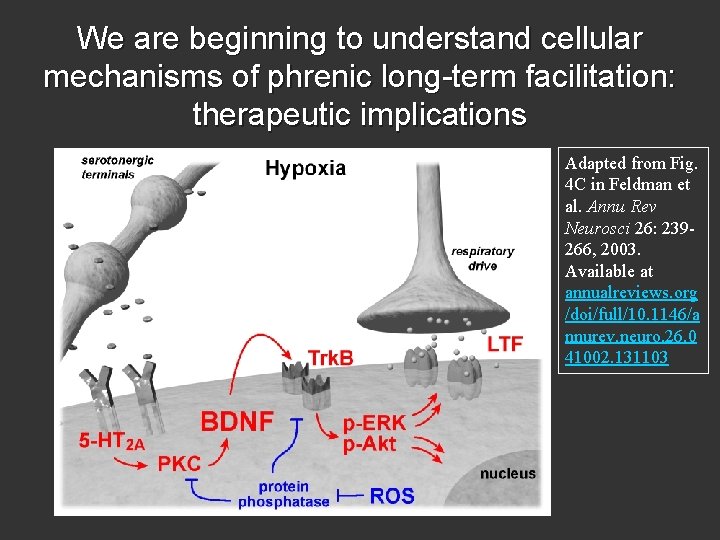
We are beginning to understand cellular mechanisms of phrenic long-term facilitation: therapeutic implications Adapted from Fig. 4 C in Feldman et al. Annu Rev Neurosci 26: 239266, 2003. Available at annualreviews. org /doi/full/10. 1146/a nnurev. neuro. 26. 0 41002. 131103
Developmental Plasticity in Ventilatory Control “A baby’s brain is a work in progress, trillions of neurons waiting to be wired into a mind. The experiences of childhood, pioneering research shows, helps form the brain’s circuits - for music and math, language and emotion. ” -- And Breathing! Newsweek: February 19, 1996
Perinatal hyperoxia (PTR) suppresses carotid body development in neonatal (not adult) rats Fig. 6. From Mitchell GS et al. Respiration. In: Encyclopedia of Neuroscience , edited by LR Squire. 2009. vol. 8, pp. 121130. Oxford: Academic.
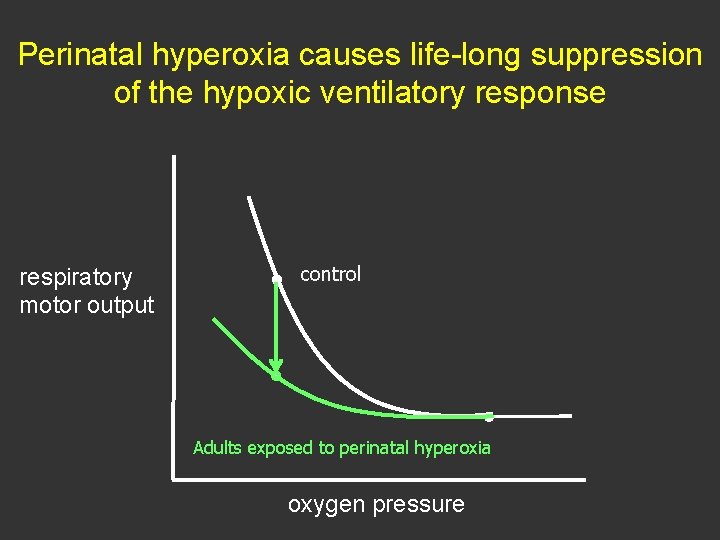
Perinatal hyperoxia causes life-long suppression of the hypoxic ventilatory response respiratory motor output control Adults exposed to perinatal hyperoxia oxygen pressure
Clinical Disorders Challenge Respiratory Control Instability v. Sleep Apnea and/or v. SIDS v. CCHS v. Heart failure v. Apnea of prematurity v. Rhett Syndrome v. Stroke v. Hyperventilation disorders v. Obesity Hypoventilation v. Ventilator Weaning v. Parkinson’s Disease v. Cerebral Palsey Diminished Capacity v. Spinal Cord Injury v. ALS/SMA v. Infectious diseases v. Muscular Dystrophy v. Multiple Sclerosis v. Charcot Marie Tooth v. Pompe Disease v. COPD v. TBI v. Toxins v. Anesthesia/Opiates
Fig. 1. From Mitchell GS. In: Genetic Basis for Respiratory Control Disorders (Gaultier C, ed). 2007. New York: Springer, p. 291 -311. Diverse clinical disorders with similar therapeutic goal: harness respiratory plasticity to restore breathing capacity Major research efforts are needed to enable translation of basic science to treat devastating clinical disorders that compromise breathing, and the quality and duration of life
- Slides: 38