The Need For Intermittent Pneumatic Compression Among Medical

- Slides: 17
The Need For Intermittent Pneumatic Compression Among Medical And Surgical Patients Joseph A. Caprini, M. D. , M. S. , FACS, RVT, DFSVS Senior Clinician Educator University of Chicago Pritzker School of Medicine Chicago, IL Emeritus Physician Evanston Northwestern Healthcare, Evanston, IL
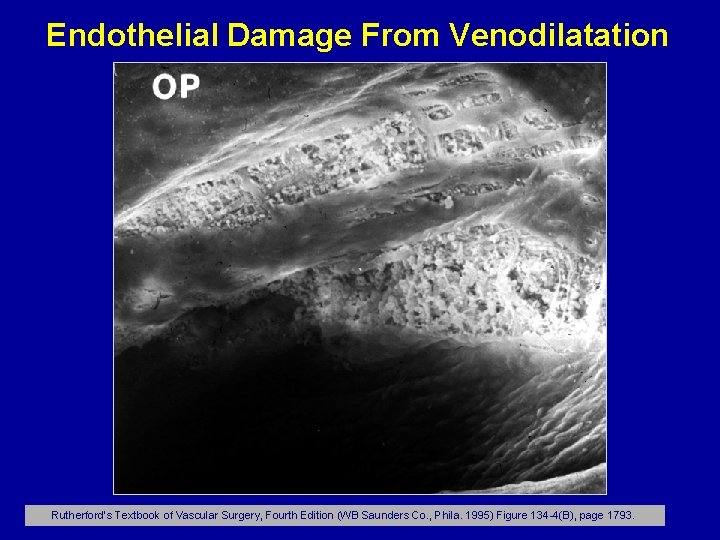
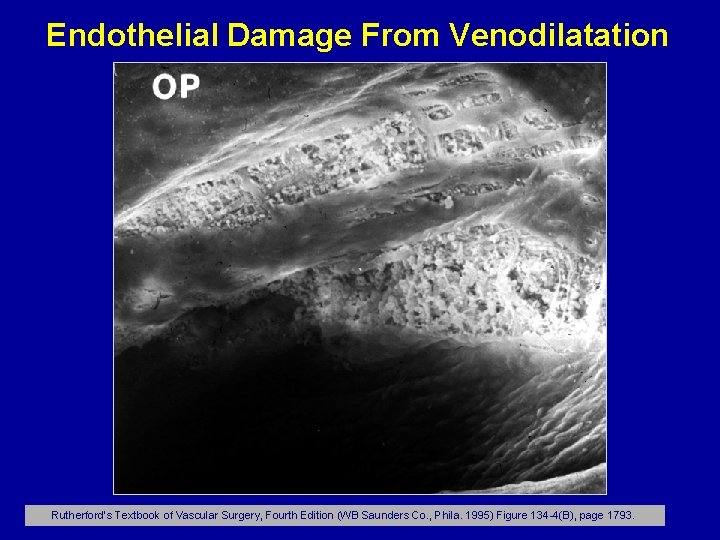
Endothelial Damage From Venodilatation Rutherford’s Textbook of Vascular Surgery, Fourth Edition (WB Saunders Co. , Phila. 1995) Figure 134 -4(B), page 1793.
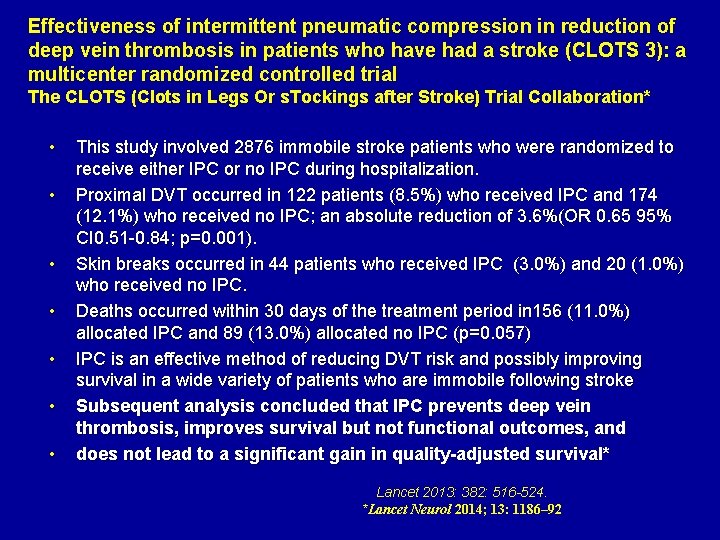
Effectiveness of intermittent pneumatic compression in reduction of deep vein thrombosis in patients who have had a stroke (CLOTS 3): a multicenter randomized controlled trial The CLOTS (Clots in Legs Or s. Tockings after Stroke) Trial Collaboration* • • This study involved 2876 immobile stroke patients who were randomized to receive either IPC or no IPC during hospitalization. Proximal DVT occurred in 122 patients (8. 5%) who received IPC and 174 (12. 1%) who received no IPC; an absolute reduction of 3. 6%(OR 0. 65 95% CI 0. 51 -0. 84; p=0. 001). Skin breaks occurred in 44 patients who received IPC (3. 0%) and 20 (1. 0%) who received no IPC. Deaths occurred within 30 days of the treatment period in 156 (11. 0%) allocated IPC and 89 (13. 0%) allocated no IPC (p=0. 057) IPC is an effective method of reducing DVT risk and possibly improving survival in a wide variety of patients who are immobile following stroke Subsequent analysis concluded that IPC prevents deep vein thrombosis, improves survival but not functional outcomes, and does not lead to a significant gain in quality-adjusted survival* Lancet 2013: 382: 516 -524. *Lancet Neurol 2014; 13: 1186– 92
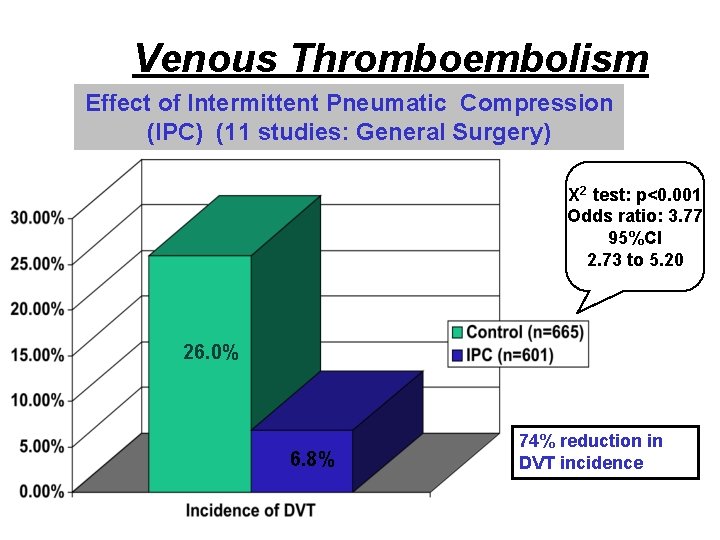
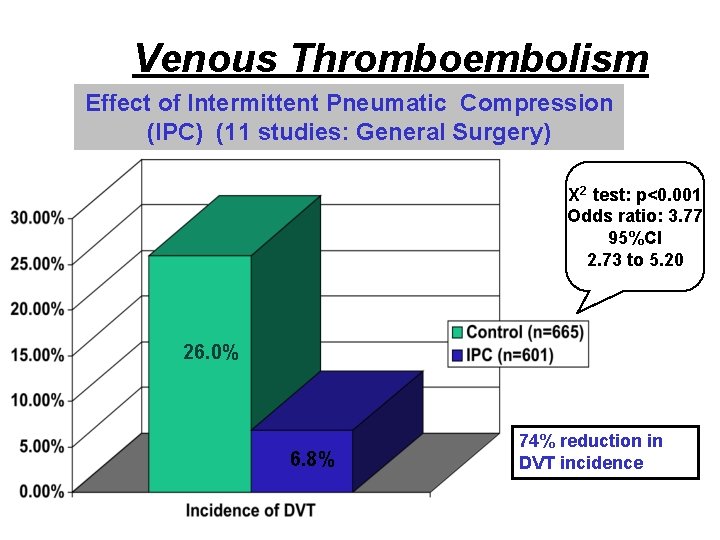
Venous Thromboembolism Effect of Intermittent Pneumatic Compression (IPC) (11 studies: General Surgery) X 2 test: p<0. 001 Odds ratio: 3. 77 95%CI 2. 73 to 5. 20 26. 0% 6. 8% 74% reduction in DVT incidence
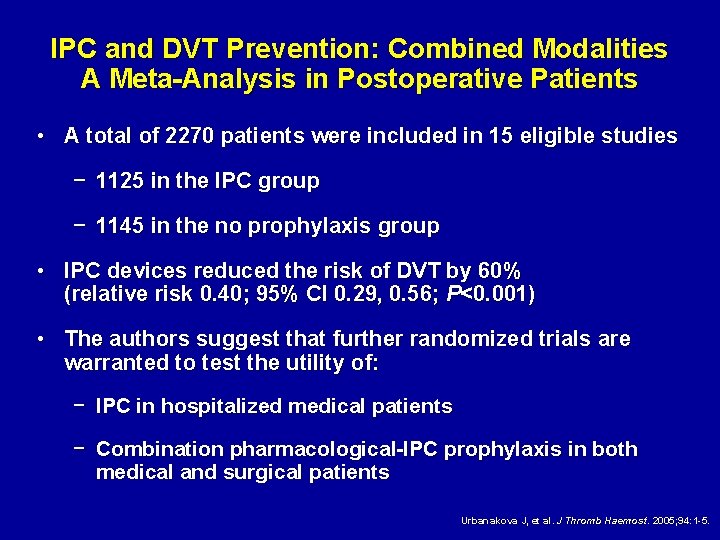
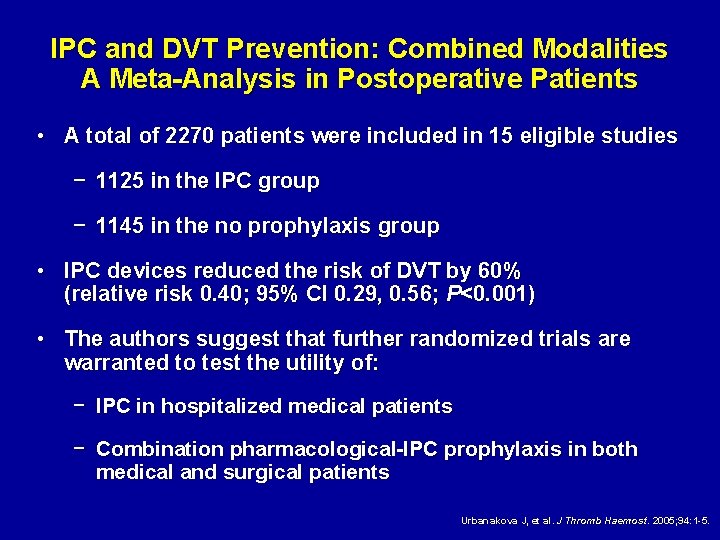
IPC and DVT Prevention: Combined Modalities A Meta-Analysis in Postoperative Patients • A total of 2270 patients were included in 15 eligible studies − 1125 in the IPC group − 1145 in the no prophylaxis group • IPC devices reduced the risk of DVT by 60% (relative risk 0. 40; 95% CI 0. 29, 0. 56; P<0. 001) • The authors suggest that further randomized trials are warranted to test the utility of: − IPC in hospitalized medical patients − Combination pharmacological-IPC prophylaxis in both medical and surgical patients Urbanakova J, et al. J Thromb Haemost. 2005; 94: 1 -5.

Primary efficacy analysis VTE reduction with fondaparinux Odds reduction = 25. 8% % of VTE 7 6 (95% CI : 49. 7; -9. 5) p = 0. 14 5 6. 1% 4 3 2 4. 6% 62/1021 47/1027 1 0 Fondaparinux Dalteparin Agnelli G et al. B J Surg 2005; in press
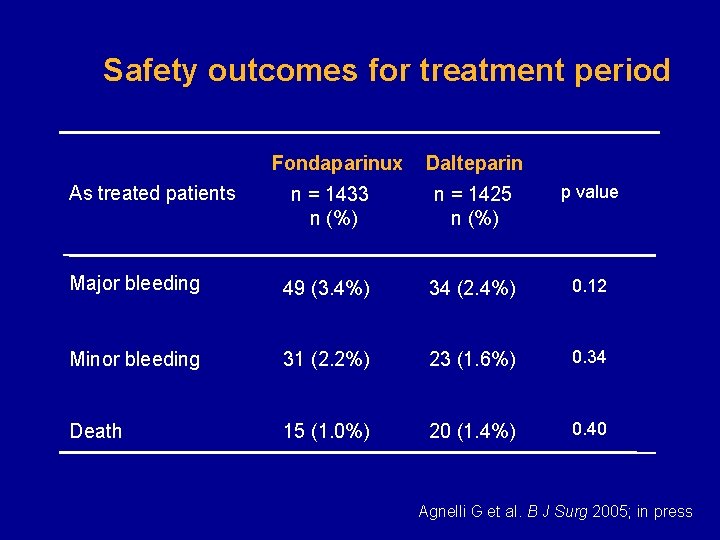
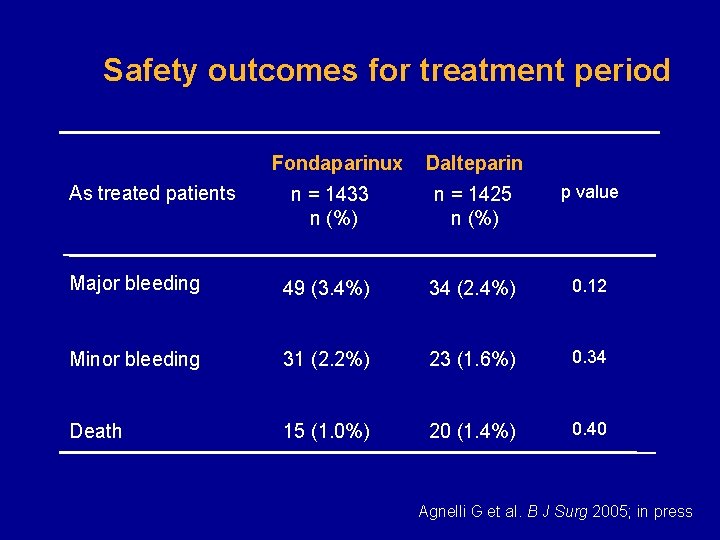
Safety outcomes for treatment period Fondaparinux Dalteparin n = 1433 n (%) n = 1425 n (%) p value Major bleeding 49 (3. 4%) 34 (2. 4%) 0. 12 Minor bleeding 31 (2. 2%) 23 (1. 6%) 0. 34 Death 15 (1. 0%) 20 (1. 4%) 0. 40 As treated patients Agnelli G et al. B J Surg 2005; in press
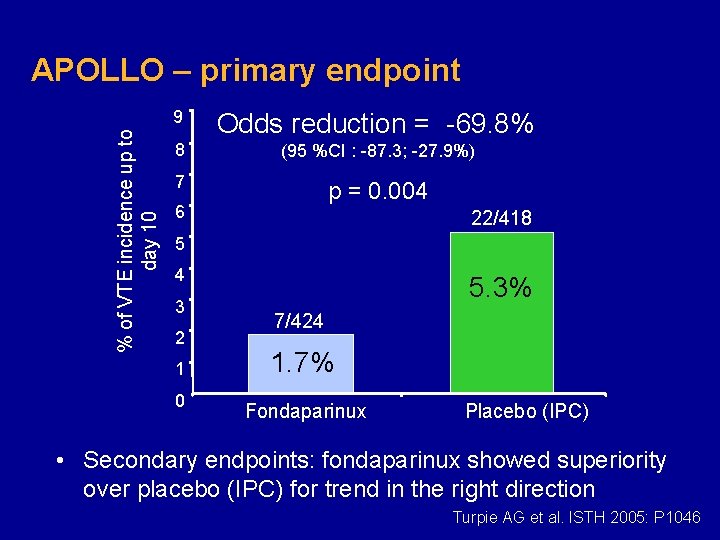
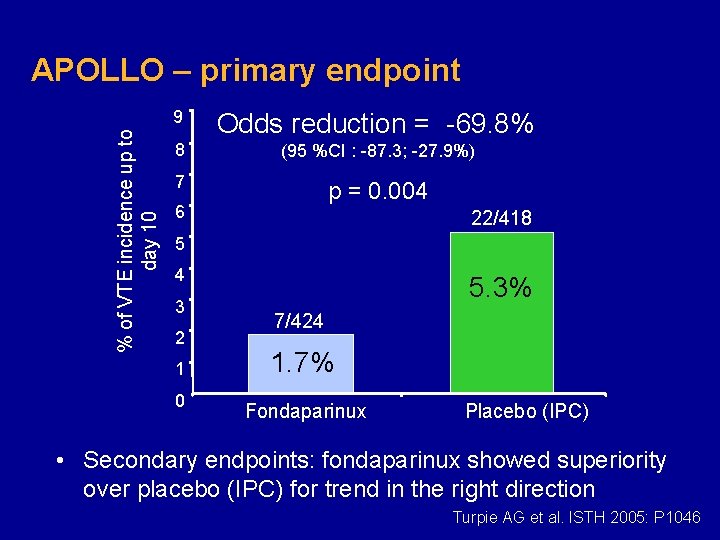
% of VTE incidence up to day 10 APOLLO – primary endpoint 9 Odds reduction = -69. 8% 8 (95 %CI : -87. 3; -27. 9%) 7 p = 0. 004 6 22/418 5 4 3 2 1 0 5. 3% 7/424 1. 7% Fondaparinux Placebo (IPC) • Secondary endpoints: fondaparinux showed superiority over placebo (IPC) for trend in the right direction Turpie AG et al. ISTH 2005: P 1046
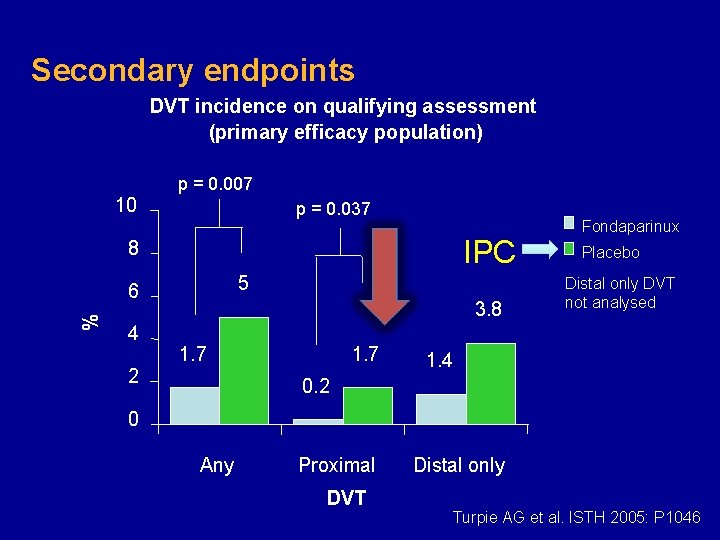
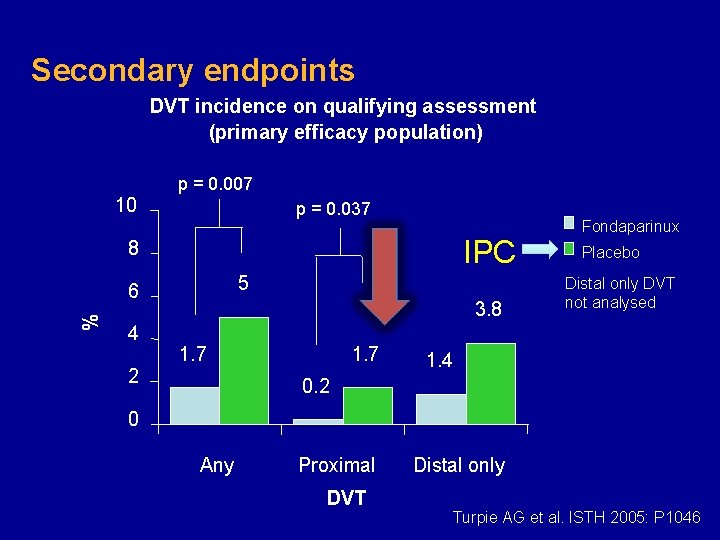
Secondary endpoints DVT incidence on qualifying assessment (primary efficacy population) p = 0. 007 10 p = 0. 037 IPC 8 5 % 6 4 2 3. 8 1. 7 Fondaparinux Placebo Distal only DVT not analysed 1. 4 0. 2 0 Any Proximal DVT Distal only Turpie AG et al. ISTH 2005: P 1046
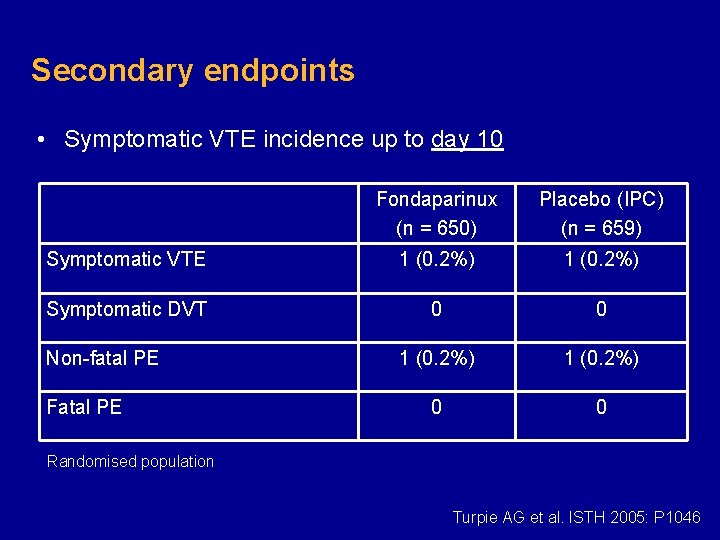
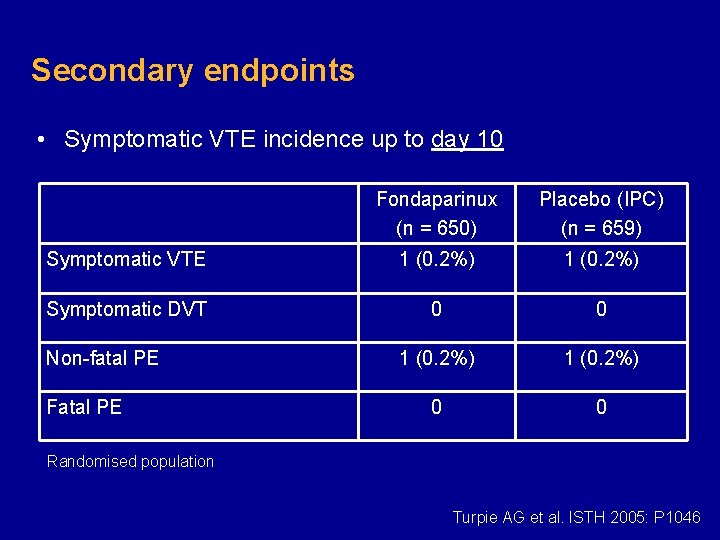
Secondary endpoints • Symptomatic VTE incidence up to day 10 Fondaparinux (n = 650) Placebo (IPC) (n = 659) Symptomatic VTE 1 (0. 2%) Symptomatic DVT 0 0 1 (0. 2%) 0 0 Non-fatal PE Fatal PE Randomised population Turpie AG et al. ISTH 2005: P 1046
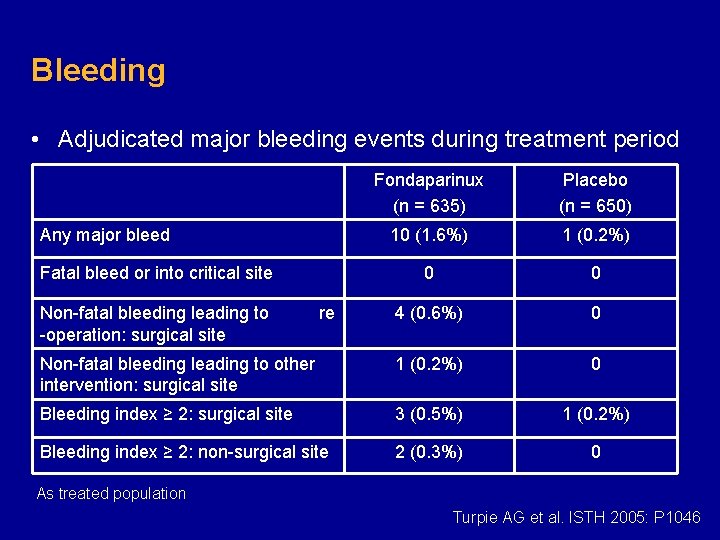
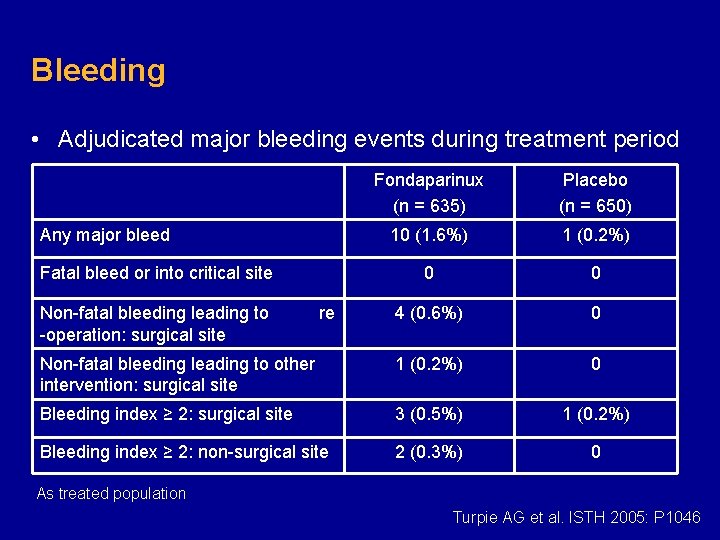
Bleeding • Adjudicated major bleeding events during treatment period Fondaparinux (n = 635) Placebo (n = 650) 10 (1. 6%) 1 (0. 2%) 0 0 4 (0. 6%) 0 Non-fatal bleeding leading to other intervention: surgical site 1 (0. 2%) 0 Bleeding index ≥ 2: surgical site 3 (0. 5%) 1 (0. 2%) Bleeding index ≥ 2: non-surgical site 2 (0. 3%) 0 Any major bleed Fatal bleed or into critical site Non-fatal bleeding leading to -operation: surgical site re As treated population Turpie AG et al. ISTH 2005: P 1046
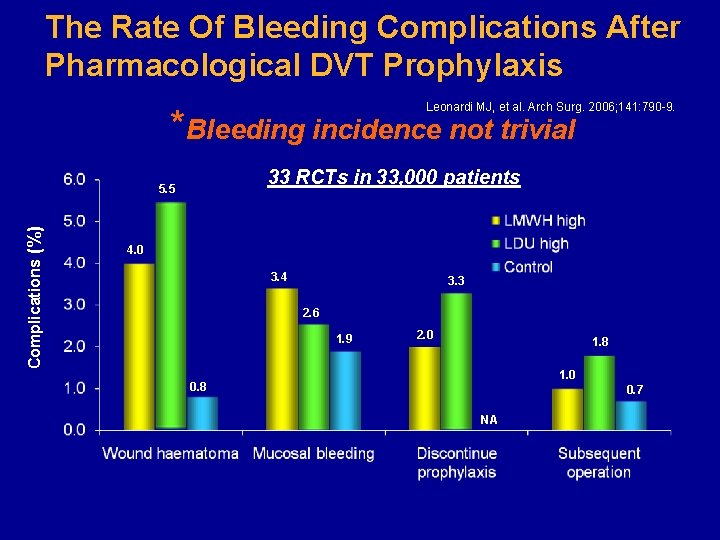
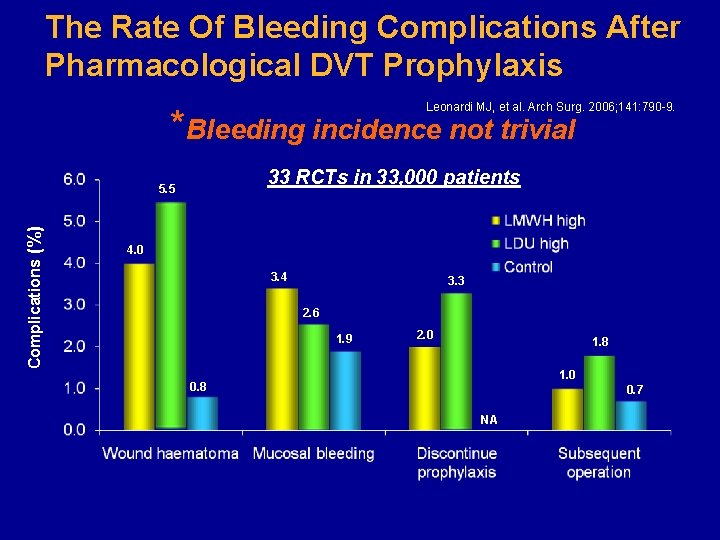
The Rate Of Bleeding Complications After Pharmacological DVT Prophylaxis Leonardi MJ, et al. Arch Surg. 2006; 141: 790 -9. *Bleeding incidence not trivial 33 RCTs in 33, 000 patients Complications (%) 5. 5 4. 0 3. 4 3. 3 2. 6 1. 9 2. 0 1. 8 1. 0 0. 8 0. 7 NA
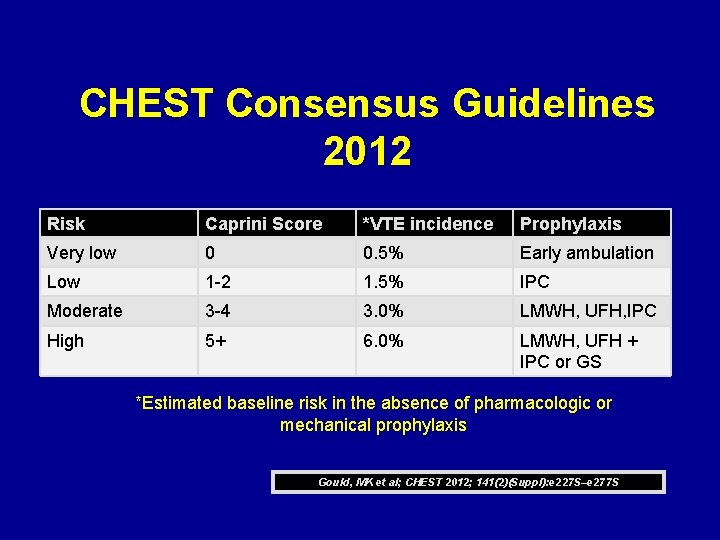
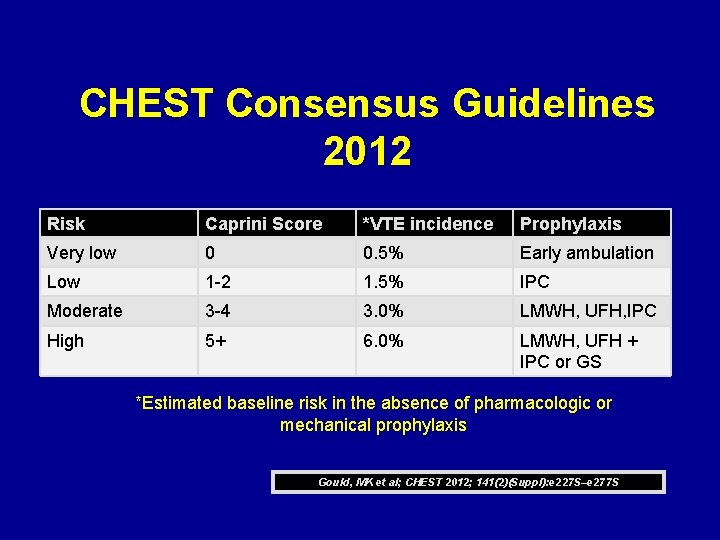
CHEST Consensus Guidelines 2012 Risk Caprini Score *VTE incidence Prophylaxis Very low 0 0. 5% Early ambulation Low 1 -2 1. 5% IPC Moderate 3 -4 3. 0% LMWH, UFH, IPC High 5+ 6. 0% LMWH, UFH + IPC or GS *Estimated baseline risk in the absence of pharmacologic or mechanical prophylaxis Gould, MK et al; CHEST 2012; 141(2)(Suppl): e 227 S–e 277 S
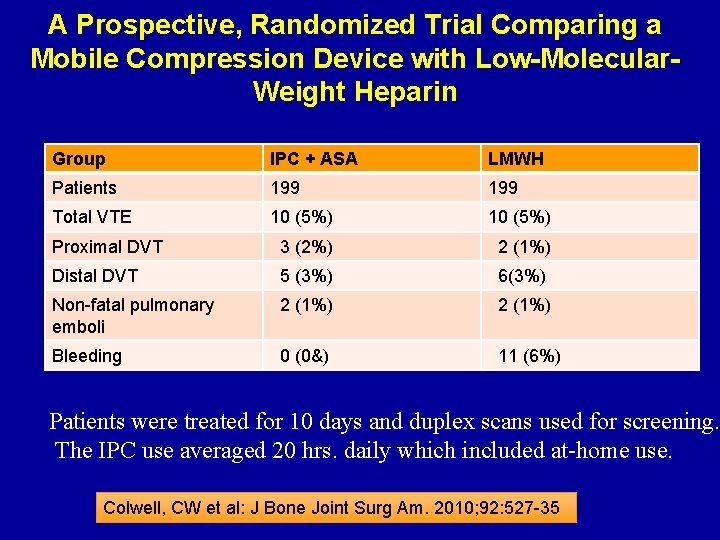
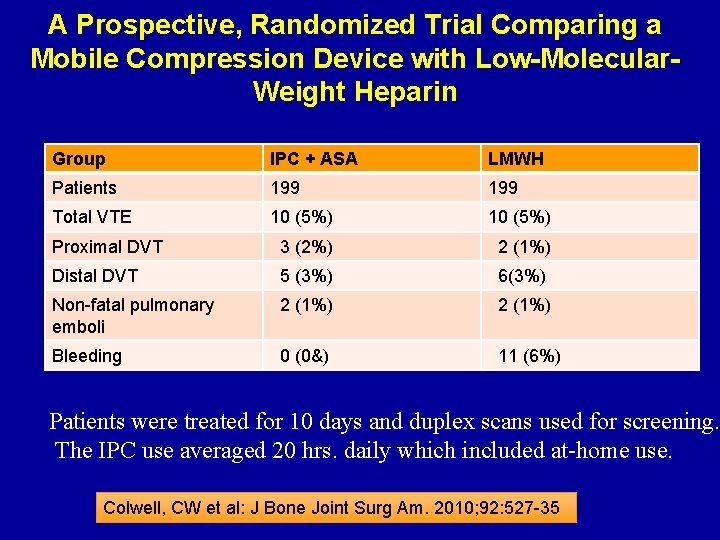
A Prospective, Randomized Trial Comparing a Mobile Compression Device with Low-Molecular. Weight Heparin Group IPC + ASA LMWH Patients 199 Total VTE 10 (5%) Proximal DVT 3 (2%) 2 (1%) Distal DVT 5 (3%) 6(3%) Non-fatal pulmonary emboli 2 (1%) Bleeding 0 (0&) 11 (6%) Patients were treated for 10 days and duplex scans used for screening. The IPC use averaged 20 hrs. daily which included at-home use. Colwell, CW et al: J Bone Joint Surg Am. 2010; 92: 527 -35
A Prospective, Randomized Trial Comparing a Mobile Compression Device with Low-Molecular. Weight Heparin • This study demonstrated that the portable compression device was safer than LMWH with respect to major bleeding after total hip arthroplasty. – Major bleeding occurred in 6%(eleven) of the patients in the heparin group and in none of the patients in the compression group (p = 0. 0004). • Equivalency not established – A study to demonstrate equivalency, noninferiority, or superiority in efficacy would require a minimum of 1480 patients per group due to the low VTE rate using LMWH. Colwell, CW et al: J Bone Joint Surg Am. 2010; 92: 527 -35
Conclusions • The shortcomings of GCS in practice limit its effectiveness for thrombosis prophylaxis • IPC is effective in reducing DVT in stroke patients and may improve overall survival • The use of IPC alone is appropriate for many surgical patients with caprini scores less than 5 since the risk of VTE is less than the risk of bleeding using anticoagulation • Combined IPC and pharmacologic methods appropriate for the highest-risk patients
The End