The MIME DIME Projects Serving high risk mothers
- Slides: 18
The MIME & DIME Projects: Serving high risk mothers of very low birthweight infants Juanita Graham MSN RN Health Services Chief Nurse MS State Dept of Health
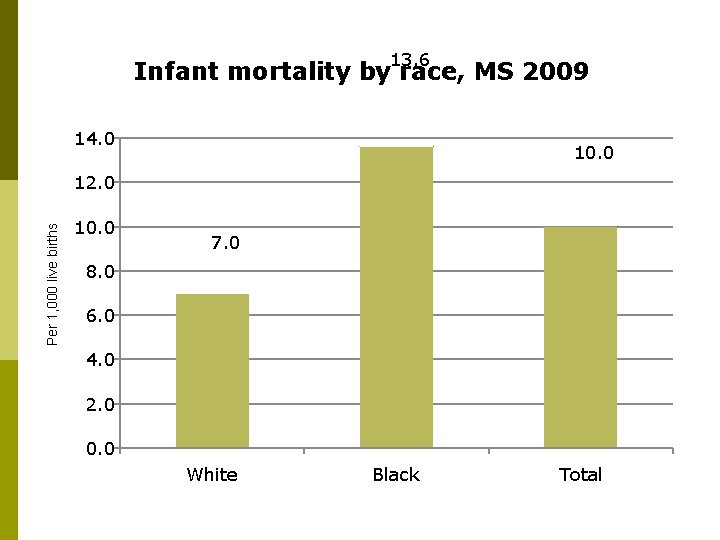
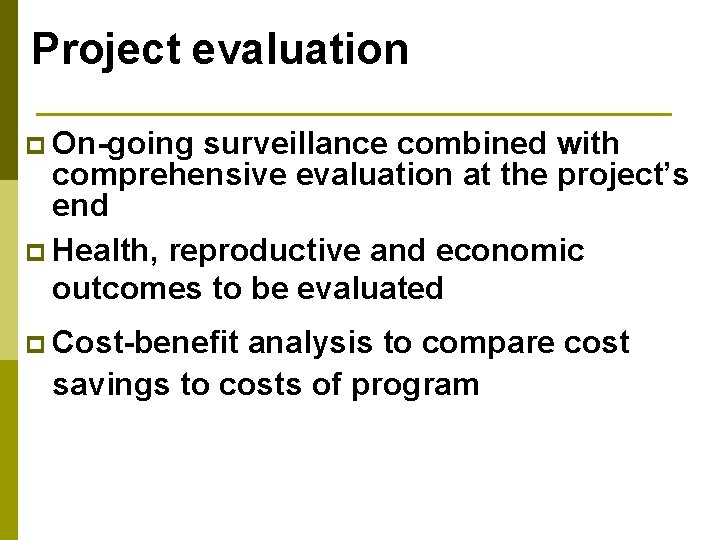
13. 6 Infant mortality by race, MS 2009 14. 0 10. 0 Per 1, 000 live births 12. 0 10. 0 7. 0 8. 0 6. 0 4. 0 2. 0 0. 0 White Black Total
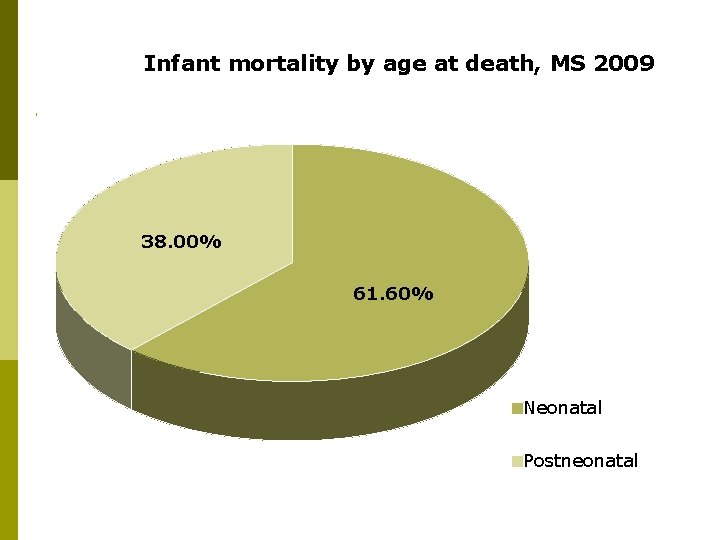
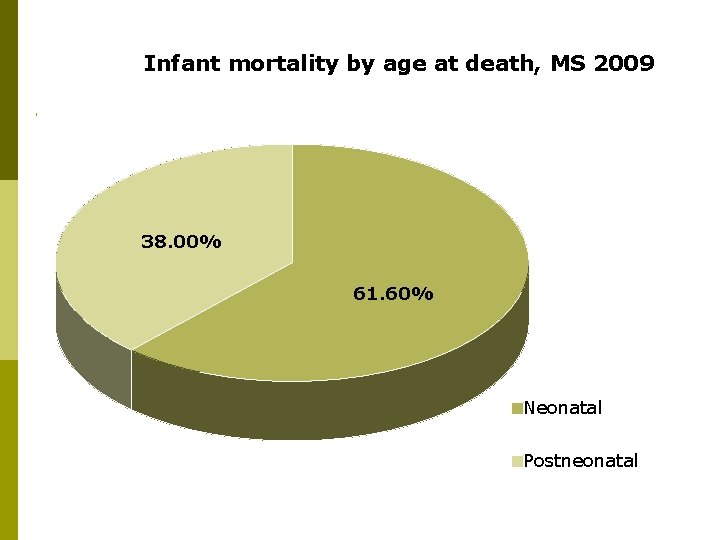
Infant mortality by age at death, MS 2009 38. 00% 61. 60% Neonatal Postneonatal
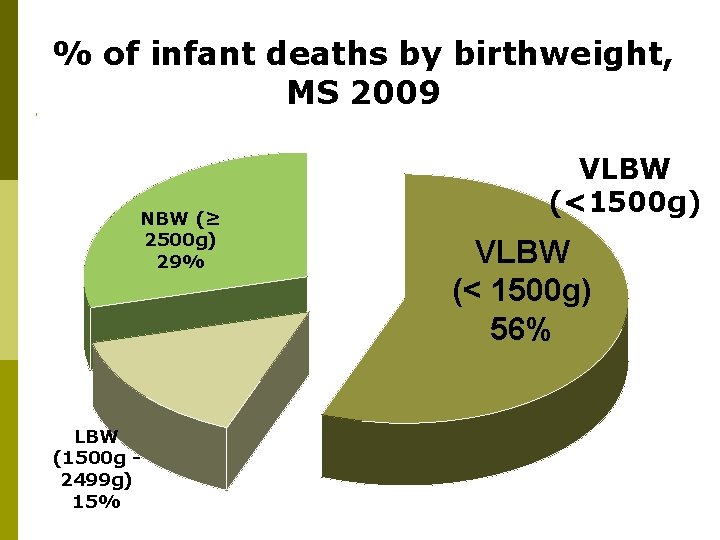
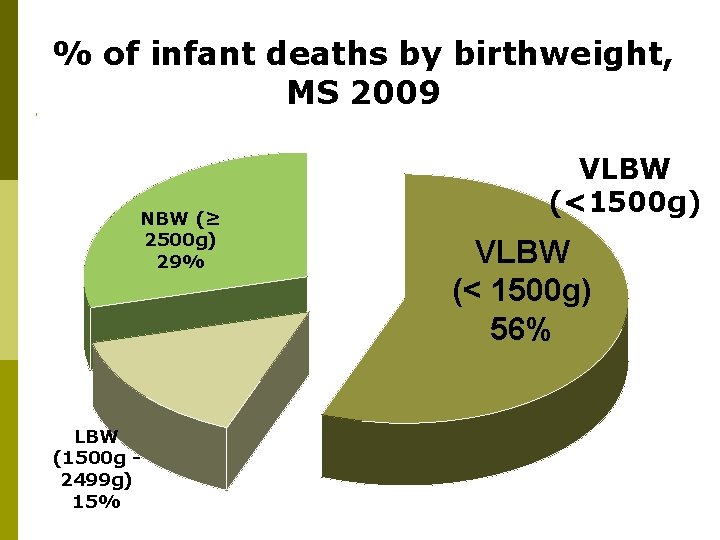
% of infant deaths by birthweight, MS 2009 NBW (≥ 2500 g) 29% LBW (1500 g 2499 g) 15% VLBW (<1500 g) VLBW (< 1500 g) 56%
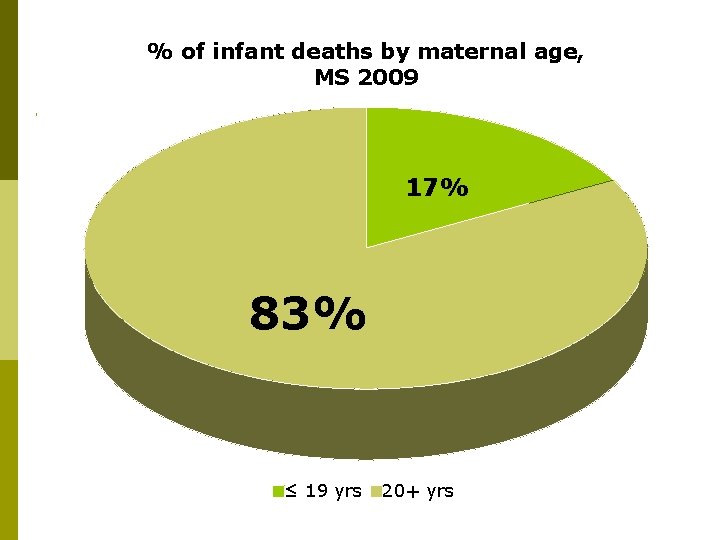
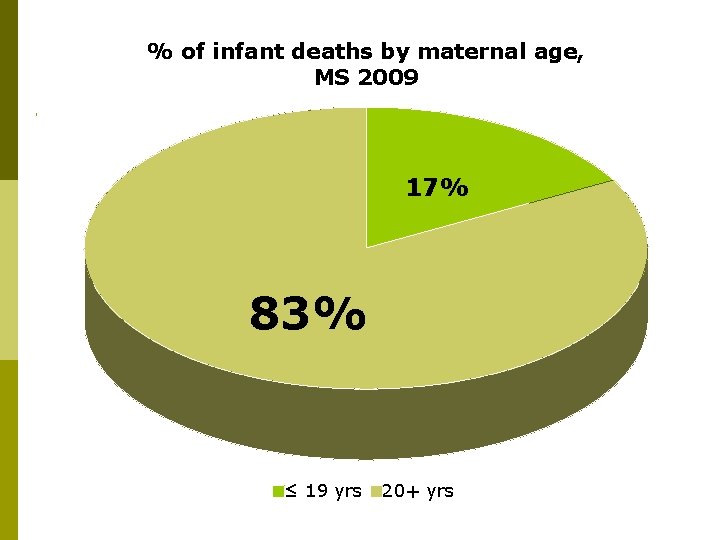
% of infant deaths by maternal age, MS 2009 17% 83% ≤ 19 yrs 20+ yrs
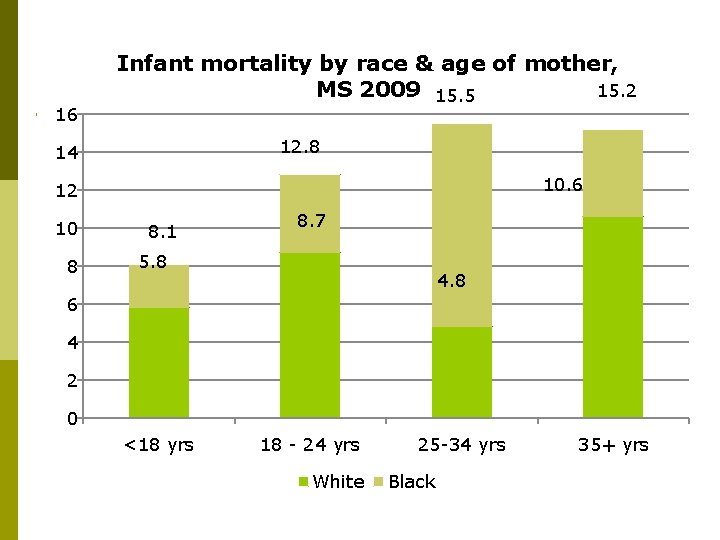
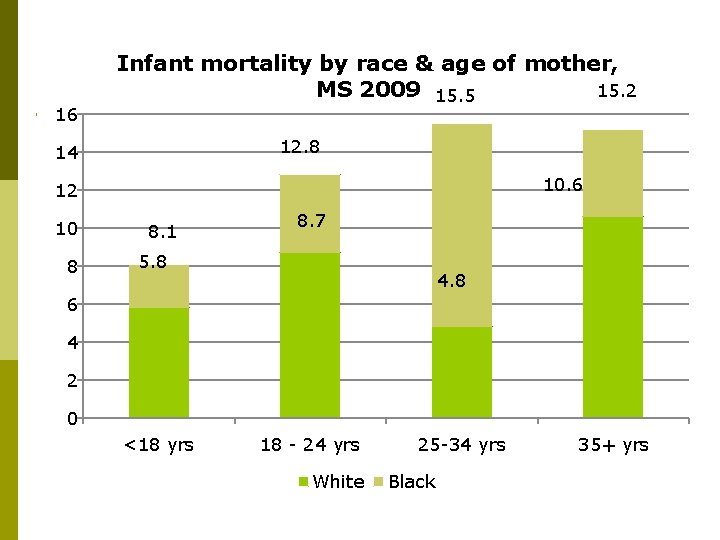
16 Infant mortality by race & age of mother, 15. 2 MS 2009 15. 5 12. 8 14 10. 6 12 10 8 8. 1 8. 7 5. 8 4. 8 6 4 2 0 <18 yrs 18 - 24 yrs White 25 -34 yrs Black 35+ yrs
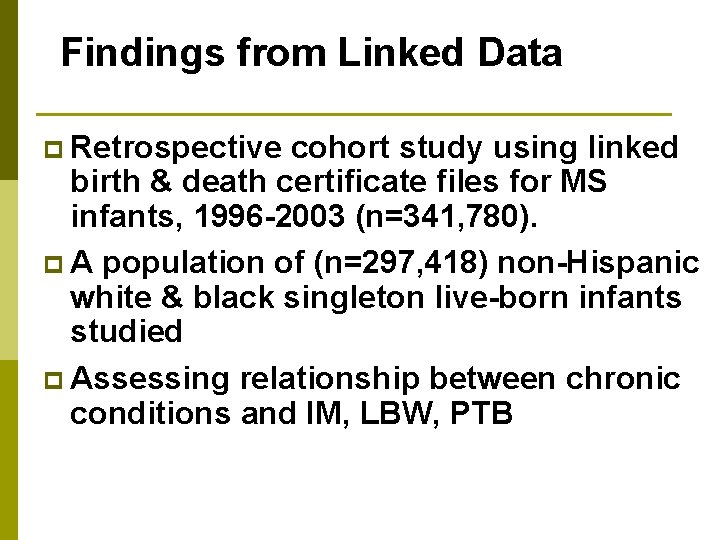
Findings from Linked Data p Retrospective cohort study using linked birth & death certificate files for MS infants, 1996 -2003 (n=341, 780). p A population of (n=297, 418) non-Hispanic white & black singleton live-born infants studied p Assessing relationship between chronic conditions and IM, LBW, PTB
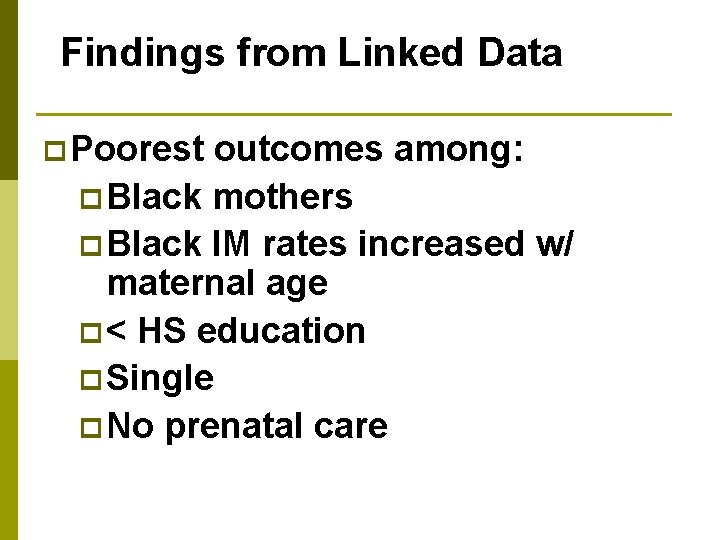
Findings from Linked Data p Poorest outcomes among: p Black mothers p Black IM rates increased w/ maternal age p < HS education p Single p No prenatal care
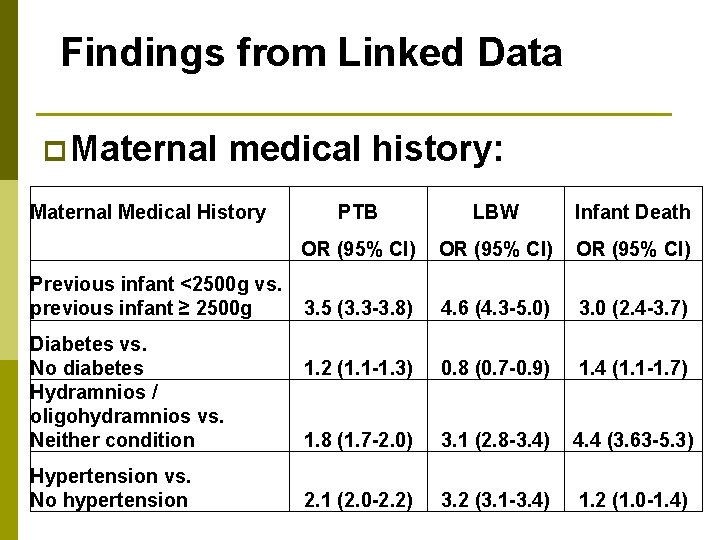
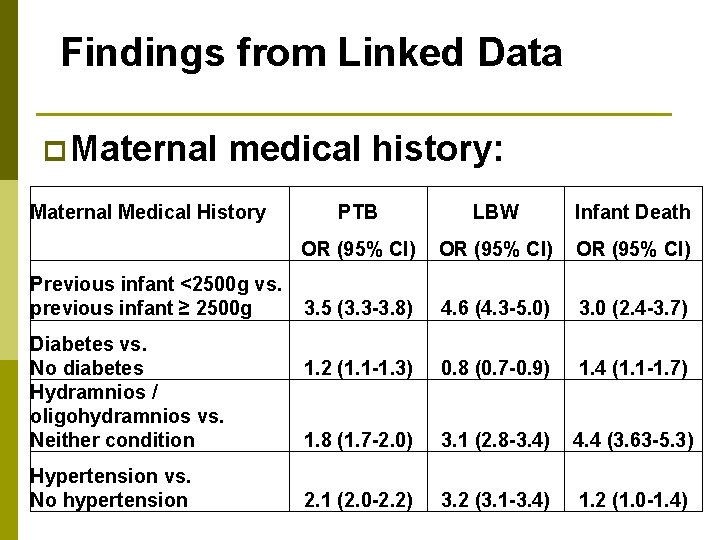
Findings from Linked Data p Maternal medical history: Maternal Medical History PTB LBW Infant Death OR (95% CI) Previous infant <2500 g vs. previous infant ≥ 2500 g 3. 5 (3. 3 -3. 8) 4. 6 (4. 3 -5. 0) 3. 0 (2. 4 -3. 7) 1. 2 (1. 1 -1. 3) 0. 8 (0. 7 -0. 9) 1. 4 (1. 1 -1. 7) 1. 8 (1. 7 -2. 0) 3. 1 (2. 8 -3. 4) 4. 4 (3. 63 -5. 3) 2. 1 (2. 0 -2. 2) 3. 2 (3. 1 -3. 4) 1. 2 (1. 0 -1. 4) Diabetes vs. No diabetes Hydramnios / oligohydramnios vs. Neither condition Hypertension vs. No hypertension
What to do? Problem: Many Mississippi babies die very small & very young despite prenatal care Hypothesis: Mississippi women are not healthy enough to achieve a full term, normal weight delivery Solution: Intervention PRIOR to conception Method: IPC for small population with highest risk for poor delivery outcomes
MIME & DIME p Preconception / interconception care pilot programs p Rural vs. Urban communities p Delta Infant Mortality Elimination p Metro Infant Mortality Elimination
Partnering organizations p Mississippi State Department of Health – lead agency p University of MS Medical Center – principal recruitment site & service provider. p Healthy Linkages – referral service for identification of medical homes. p Division of Medicaid – data source.
Partnering organizations p Federally qualified community health centers – primary care medical homes. p World Health Organization Collaborating Center for Reproductive Health – technical assistance.
IPC intervention package p p Individualized interpregnancy care plan based on assessments of medical/ social risks for subsequent poor pregnancy outcomes Provision of primary health care & dental services in accordance with care plan for 24 months
IPC intervention package p p Assistance in achieving woman’s desire for subsequent pregnancies & need for optimum child spacing (ideally 18 -20 months); Provision of appropriate social services & community outreach in each woman’s community.
Problems & lessons learned p Expansive, rural geographical area p Transportation p Limited resources p Limited funding
Project evaluation p On-going surveillance combined with comprehensive evaluation at the project’s end p Health, reproductive and economic outcomes to be evaluated p Cost-benefit analysis to compare cost savings to costs of program
Goal p Goal: Funding to support statewide expansion of program p Format: Medicaid waiver; other internal options include focusing on increased enrollment and participation in reimbursable programs that could sustain the program