The Mental Health and Poverty Project Mental health
- Slides: 1
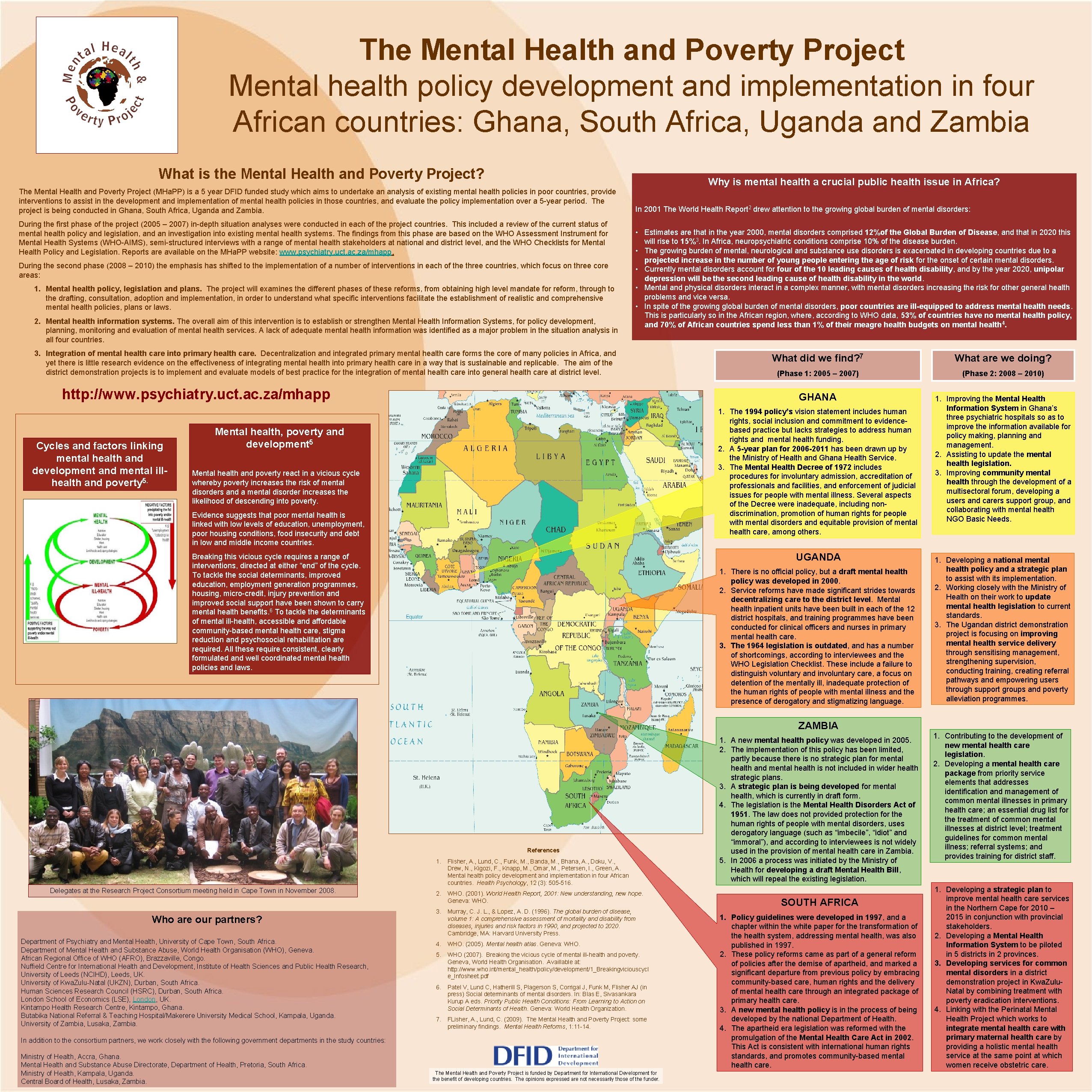
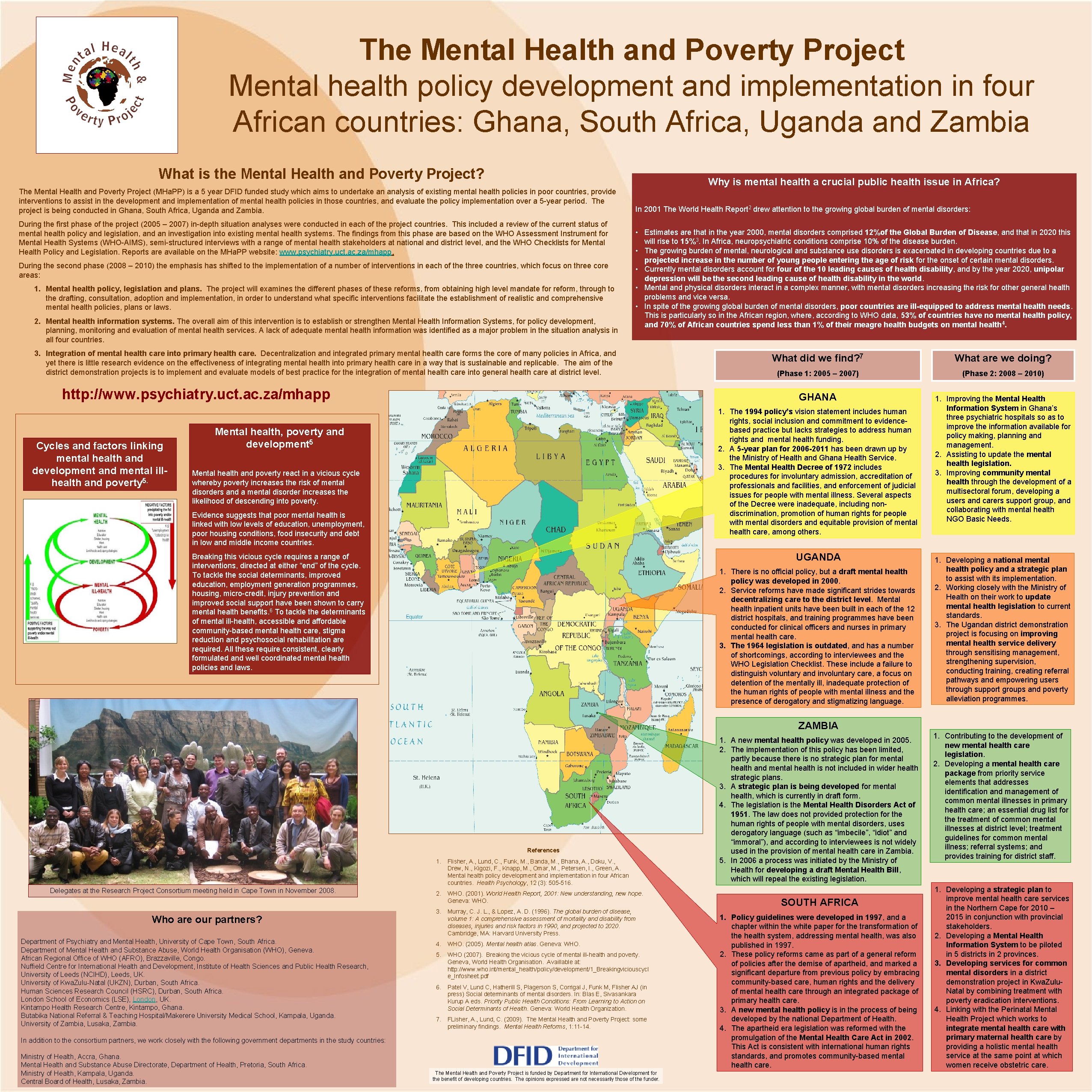
The Mental Health and Poverty Project Mental health policy development and implementation in four African countries: Ghana, South Africa, Uganda and Zambia What is the Mental Health and Poverty Project? Why is mental health a crucial public health issue in Africa? The Mental Health and Poverty Project (MHa. PP) is a 5 year DFID funded study which aims to undertake an analysis of existing mental health policies in poor countries, provide interventions to assist in the development and implementation of mental health policies in those countries, and evaluate the policy implementation over a 5 -year period. The project is being conducted in Ghana, South Africa, Uganda and Zambia. During the first phase of the project (2005 – 2007) in-depth situation analyses were conducted in each of the project countries. This included a review of the current status of mental health policy and legislation, and an investigation into existing mental health systems. The findings from this phase are based on the WHO Assessment Instrument for Mental Health Systems (WHO-AIMS), semi-structured interviews with a range of mental health stakeholders at national and district level, and the WHO Checklists for Mental Health Policy and Legislation. Reports are available on the MHa. PP website: www. psychiatry. uct. ac. za/mhapp. During the second phase (2008 – 2010) the emphasis has shifted to the implementation of a number of interventions in each of the three countries, which focus on three core areas: 1. Mental health policy, legislation and plans. The project will examines the different phases of these reforms, from obtaining high level mandate for reform, through to the drafting, consultation, adoption and implementation, in order to understand what specific interventions facilitate the establishment of realistic and comprehensive mental health policies, plans or laws. 2. Mental health information systems. The overall aim of this intervention is to establish or strengthen Mental Health Information Systems, for policy development, planning, monitoring and evaluation of mental health services. A lack of adequate mental health information was identified as a major problem in the situation analysis in all four countries. In 2001 The World Health Report 2 drew attention to the growing global burden of mental disorders: • Estimates are that in the year 2000, mental disorders comprised 12%of the Global Burden of Disease, and that in 2020 this will rise to 15%3. In Africa, neuropsychiatric conditions comprise 10% of the disease burden. • The growing burden of mental, neurological and substance use disorders is exacerbated in developing countries due to a projected increase in the number of young people entering the age of risk for the onset of certain mental disorders. • Currently mental disorders account for four of the 10 leading causes of health disability, and by the year 2020, unipolar depression will be the second leading cause of health disability in the world. • Mental and physical disorders interact in a complex manner, with mental disorders increasing the risk for other general health problems and vice versa. • In spite of the growing global burden of mental disorders, poor countries are ill-equipped to address mental health needs. This is particularly so in the African region, where, according to WHO data, 53% of countries have no mental health policy, and 70% of African countries spend less than 1% of their meagre health budgets on mental health 4. 3. Integration of mental health care into primary health care. Decentralization and integrated primary mental health care forms the core of many policies in Africa, and yet there is little research evidence on the effectiveness of integrating mental health into primary health care in a way that is sustainable and replicable. The aim of the district demonstration projects is to implement and evaluate models of best practice for the integration of mental health care into general health care at district level. http: //www. psychiatry. uct. ac. za/mhapp Cycles and factors linking mental health and development and mental illhealth and poverty 5. What did we find? 7 What are we doing? (Phase 1: 2005 – 2007) (Phase 2: 2008 – 2010) GHANA 1. Improving the Mental Health Information System in Ghana’s three psychiatric hospitals so as to improve the information available for policy making, planning and management. 2. Assisting to update the mental health legislation. 3. Improving community mental health through the development of a multisectoral forum, developing a users and carers support group, and collaborating with mental health NGO Basic Needs. 1. The 1994 policy’s vision statement includes human rights, social inclusion and commitment to evidencebased practice but lacks strategies to address human rights and mental health funding. 2. A 5 -year plan for 2006 -2011 has been drawn up by the Ministry of Health and Ghana Health Service. 3. The Mental Health Decree of 1972 includes procedures for involuntary admission, accreditation of professionals and facilities, and enforcement of judicial issues for people with mental illness. Several aspects of the Decree were inadequate, including nondiscrimination, promotion of human rights for people with mental disorders and equitable provision of mental health care, among others. Mental health, poverty and development 5 Mental health and poverty react in a vicious cycle whereby poverty increases the risk of mental disorders and a mental disorder increases the likelihood of descending into poverty. Evidence suggests that poor mental health is linked with low levels of education, unemployment, poor housing conditions, food insecurity and debt in low and middle income countries. UGANDA Breaking this vicious cycle requires a range of interventions, directed at either “end” of the cycle. To tackle the social determinants, improved education, employment generation programmes, housing, micro-credit, injury prevention and improved social support have been shown to carry mental health benefits. 6 To tackle the determinants of mental ill-health, accessible and affordable community-based mental health care, stigma reduction and psychosocial rehabilitation are required. All these require consistent, clearly formulated and well coordinated mental health policies and laws. 1. There is no official policy, but a draft mental health policy was developed in 2000. 2. Service reforms have made significant strides towards decentralizing care to the district level. Mental health inpatient units have been built in each of the 12 district hospitals, and training programmes have been conducted for clinical officers and nurses in primary mental health care. 3. The 1964 legislation is outdated, and has a number of shortcomings, according to interviewees and the WHO Legislation Checklist. These include a failure to distinguish voluntary and involuntary care, a focus on detention of the mentally ill, inadequate protection of the human rights of people with mental illness and the presence of derogatory and stigmatizing language. 1. Developing a national mental health policy and a strategic plan to assist with its implementation. 2. Working closely with the Ministry of Health on their work to update mental health legislation to current standards. 3. The Ugandan district demonstration project is focusing on improving mental health service delivery through sensitising management, strengthening supervision, conducting training, creating referral pathways and empowering users through support groups and poverty alleviation programmes. ZAMBIA References Delegates at the Research Project Consortium meeting held in Cape Town in November 2008. Who are our partners? Department of Psychiatry and Mental Health, University of Cape Town, South Africa. Department of Mental Health and Substance Abuse, World Health Organisation (WHO), Geneva. African Regional Office of WHO (AFRO), Brazzaville, Congo. Nuffield Centre for International Health and Development, Institute of Health Sciences and Public Health Research, University of Leeds (NCIHD), Leeds, UK. University of Kwa. Zulu-Natal (UKZN), Durban, South Africa. Human Sciences Research Council (HSRC), Durban, South Africa. London School of Economics (LSE), London, UK. Kintampo Health Research Centre, Kintampo, Ghana. Butabika National Referral & Teaching Hospital/Makerere University Medical School, Kampala, Uganda. University of Zambia, Lusaka, Zambia. 1. Flisher, A. , Lund, C. , Funk, M. , Banda, M. , Bhana, A. , Doku, V. , Drew, N. , Kigozi, F. , Knapp, M. , Omar, M. , Petersen, I. , Green, A. Mental health policy development and implementation in four African countries. Health Psychology, 12 (3): 505 -516. 2. WHO. (2001). World Health Report, 2001: New understanding, new hope. Geneva: WHO. 3. Murray, C. J. L. , & Lopez, A. D. (1996). The global burden of disease, volume 1: A comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990, and projected to 2020. Cambridge, MA: Harvard University Press. 4. WHO. (2005). Mental health atlas. Geneva: WHO. 5. WHO (2007). Breaking the vicious cycle of mental ill-health and poverty. Geneva, World Health Organisation. Availlable at: http: //www. who. int/mental_health/policy/development/1_Breakingviciouscycl e_Infosheet. pdf 6. Patel V, Lund C, Hatherill S, Plagerson S, Corrigal J, Funk M, Flisher AJ (in press) Social determinants of mental disorders. In: Blas E, Sivasankara Kurup A eds. Priority Public Health Conditions: From Learning to Action on Social Determinants of Health. Geneva: World Health Organization. 7. FLisher, A. , Lund, C. (2009). The Mental Health and Poverty Project: some preliminary findings. Mental Health Reforms, 1: 11 -14. In addition to the consortium partners, we work closely with the following government departments in the study countries: Ministry of Health, Accra, Ghana. Mental Health and Substance Abuse Directorate, Department of Health, Pretoria, South Africa. Ministry of Health, Kampala, Uganda. Central Board of Health, Lusaka, Zambia. The Mental Health and Poverty Project is funded by Department for International Development for the benefit of developing countries. The opinions expressed are not necessarily those of the funder. 1. A new mental health policy was developed in 2005. 2. The implementation of this policy has been limited, partly because there is no strategic plan for mental health and mental health is not included in wider health strategic plans. 3. A strategic plan is being developed for mental health, which is currently in draft form. 4. The legislation is the Mental Health Disorders Act of 1951. The law does not provided protection for the human rights of people with mental disorders, uses derogatory language (such as “imbecile”, “idiot” and “immoral”), and according to interviewees is not widely used in the provision of mental health care in Zambia. 5. In 2006 a process was initiated by the Ministry of Health for developing a draft Mental Health Bill, which will repeal the existing legislation. SOUTH AFRICA 1. Policy guidelines were developed in 1997, and a chapter within the white paper for the transformation of the health system, addressing mental health, was also published in 1997. 2. These policy reforms came as part of a general reform of policies after the demise of apartheid, and marked a significant departure from previous policy by embracing community-based care, human rights and the delivery of mental health care through an integrated package of primary health care. 3. A new mental health policy is in the process of being developed by the national Department of Health. 4. The apartheid era legislation was reformed with the promulgation of the Mental Health Care Act in 2002. This Act is consistent with international human rights standards, and promotes community-based mental health care. 1. Contributing to the development of new mental health care legislation. 2. Developing a mental health care package from priority service elements that addresses identification and management of common mental illnesses in primary health care; an essential drug list for the treatment of common mental illnesses at district level; treatment guidelines for common mental illness; referral systems; and provides training for district staff. 1. Developing a strategic plan to improve mental health care services in the Northern Cape for 2010 – 2015 in conjunction with provincial stakeholders. 2. Developing a Mental Health Information System to be piloted in 5 districts in 2 provinces. 3. Developing services for common mental disorders in a district demonstration project in Kwa. Zulu. Natal by combining treatment with poverty eradication interventions. 4. Linking with the Perinatal Mental Health Project which works to integrate mental health care with primary maternal health care by providing a holistic mental health service at the same point at which women receive obstetric care.