THE MARYLAND EARLY HEARING DETECTION AND INTERVENTION PROGRAM

![Prevention and Health Promotion Administration [Date] 26 Prevention and Health Promotion Administration [Date] 26](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-26.jpg)

![Prevention and Health Promotion Administration [Date] 33 Prevention and Health Promotion Administration [Date] 33](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-33.jpg)
![Prevention and Health Promotion Administration [Date] 34 Prevention and Health Promotion Administration [Date] 34](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-34.jpg)
![Prevention and Health Promotion Administration [Date] 35 Prevention and Health Promotion Administration [Date] 35](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-35.jpg)
![Prevention and Health Promotion Administration [Date] 36 Prevention and Health Promotion Administration [Date] 36](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-36.jpg)
![Prevention and Health Promotion Administration [Date] 37 Prevention and Health Promotion Administration [Date] 37](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-37.jpg)
![Prevention and Health Promotion Administration [Date] 38 Prevention and Health Promotion Administration [Date] 38](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-38.jpg)
![Prevention and Health Promotion Administration [Date] 39 Prevention and Health Promotion Administration [Date] 39](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-39.jpg)
![Prevention and Health Promotion Administration [Date] 40 Prevention and Health Promotion Administration [Date] 40](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-40.jpg)
![Prevention and Health Promotion Administration [Date] 41 Prevention and Health Promotion Administration [Date] 41](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-41.jpg)
![Challenges Prevention and Health Promotion Administration [Date] 44 Challenges Prevention and Health Promotion Administration [Date] 44](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-44.jpg)

- Slides: 56
THE MARYLAND EARLY HEARING DETECTION AND INTERVENTION PROGRAM ”Maryland EHDI Program Update” MAY 16, 2013 Tanya D. Green, M. S. , CCC-A Program Chief, Maryland Infant Hearing Program Maryland Department of Health and Mental Hygiene Prevention and Health Promotion Administration Office for Genetics and People with Special Health Care Needs
MISSION AND VISION of the Prevention and Health Promotion Administration MISSION l The mission of the Prevention and Health Promotion Administration is to protect, promote and improve the health and well-being of all Marylanders and their families through provision of public health leadership and through community-based public health efforts in partnership with local health departments, providers, community based organizations, and public and private sector agencies, giving special attention to at-risk and vulnerable populations. VISION l The Prevention and Health Promotion Administration envisions a future in which all Marylanders and their families enjoy optimal health and wellbeing.
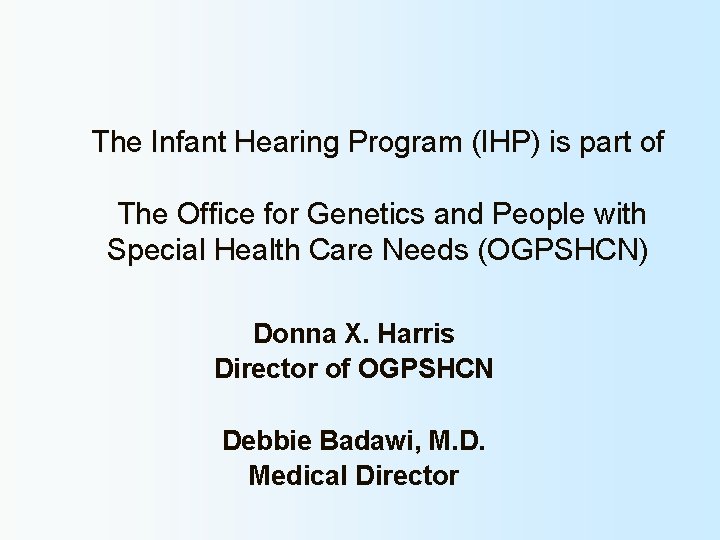
The Infant Hearing Program (IHP) is part of The Office for Genetics and People with Special Health Care Needs (OGPSHCN) Donna X. Harris Director of OGPSHCN Debbie Badawi, M. D. Medical Director
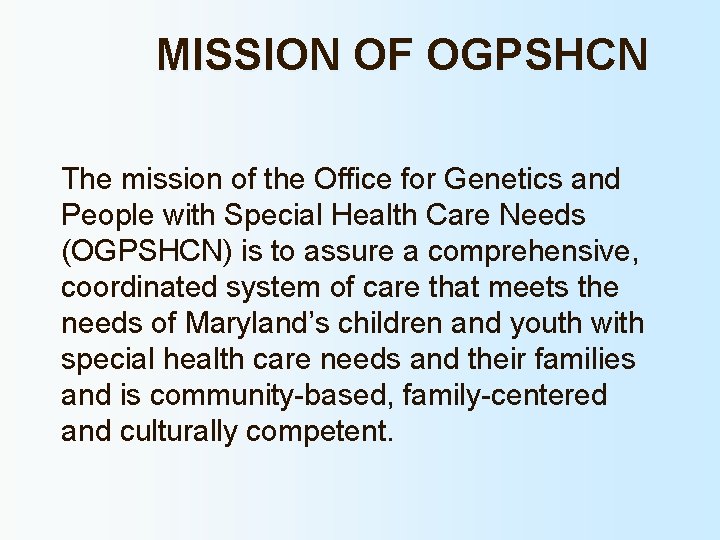
MISSION OF OGPSHCN The mission of the Office for Genetics and People with Special Health Care Needs (OGPSHCN) is to assure a comprehensive, coordinated system of care that meets the needs of Maryland’s children and youth with special health care needs and their families and is community-based, family-centered and culturally competent.
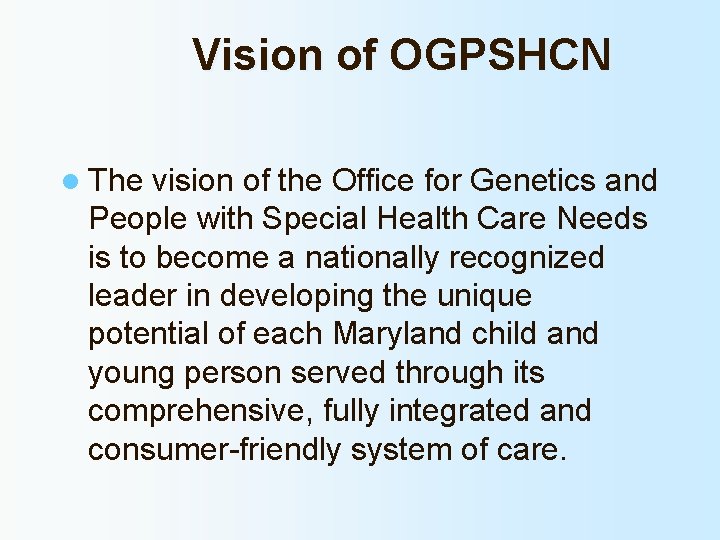
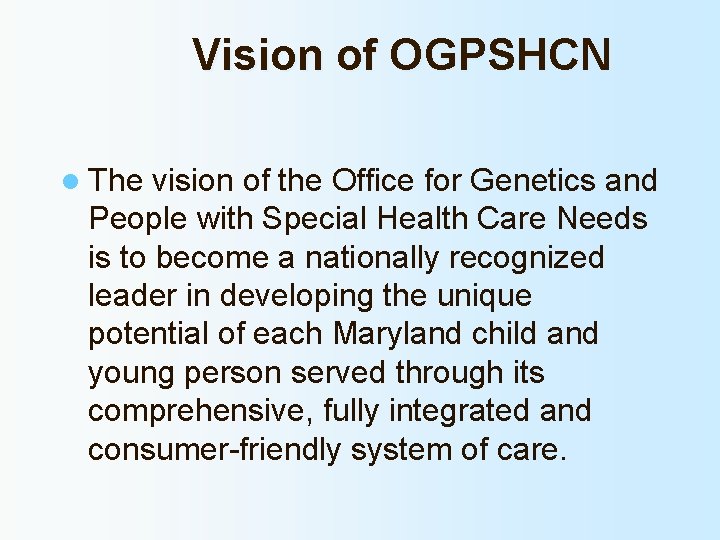
Vision of OGPSHCN l The vision of the Office for Genetics and People with Special Health Care Needs is to become a nationally recognized leader in developing the unique potential of each Maryland child and young person served through its comprehensive, fully integrated and consumer-friendly system of care.
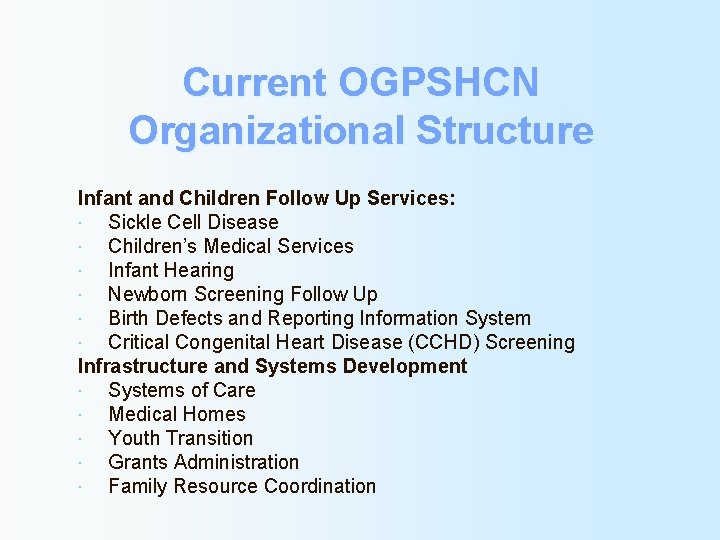
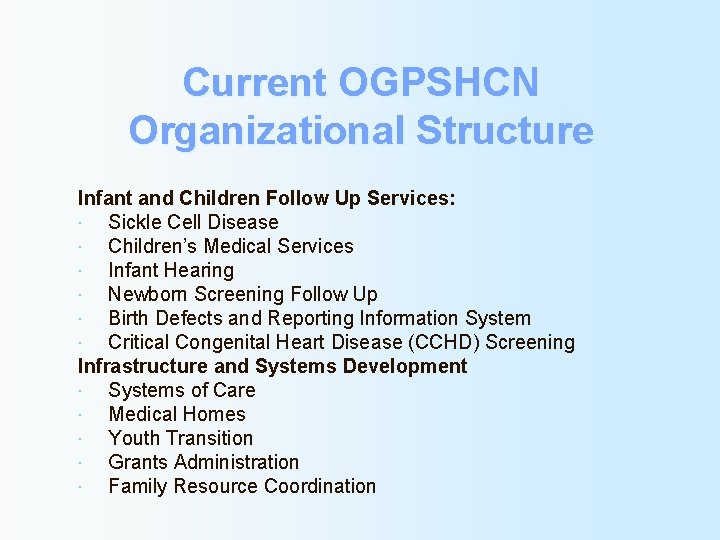
Current OGPSHCN Organizational Structure Infant and Children Follow Up Services: Sickle Cell Disease Children’s Medical Services Infant Hearing Newborn Screening Follow Up Birth Defects and Reporting Information System Critical Congenital Heart Disease (CCHD) Screening Infrastructure and Systems Development Systems of Care Medical Homes Youth Transition Grants Administration Family Resource Coordination
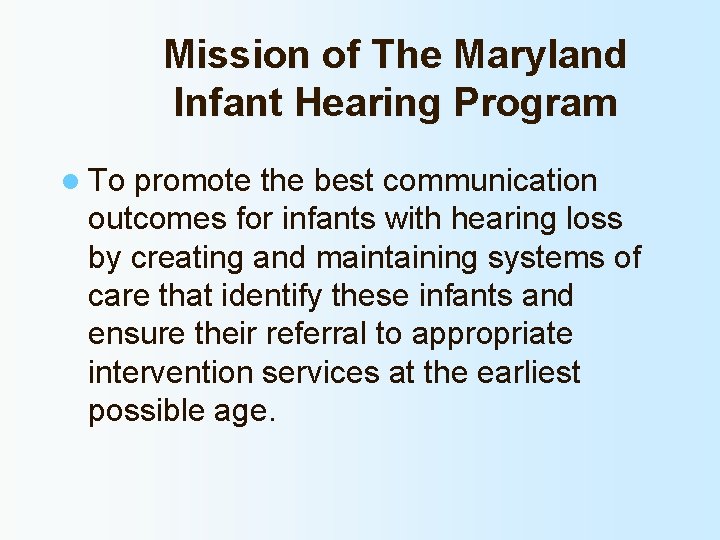
Mission of The Maryland Infant Hearing Program l To promote the best communication outcomes for infants with hearing loss by creating and maintaining systems of care that identify these infants and ensure their referral to appropriate intervention services at the earliest possible age.
The problems of deafness are deeper and more complex if not more important then those of blindness. Deafness is a much worse misfortune for it means the loss of the most vital stimulus – the sound of the voice that brings language, sets thoughts astir, and keeps us in the intellectual company of man. Blindness separates us from things but deafness separates us from people. Helen Keller
MD EHDI PROGRAM OVERVIEW
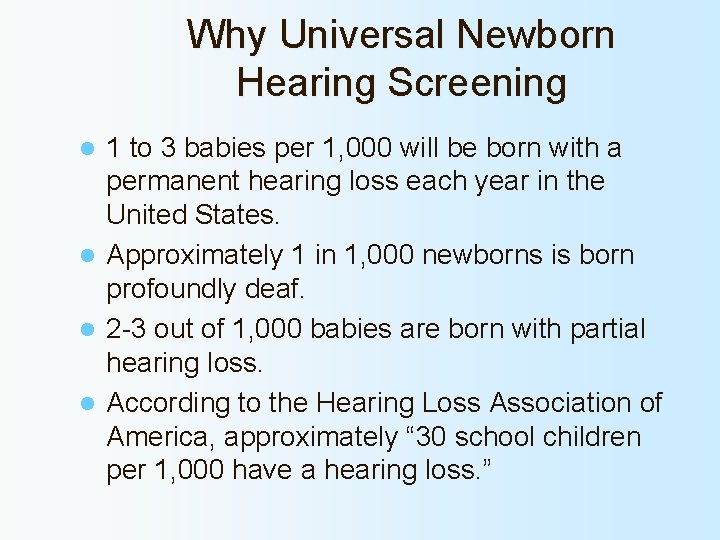
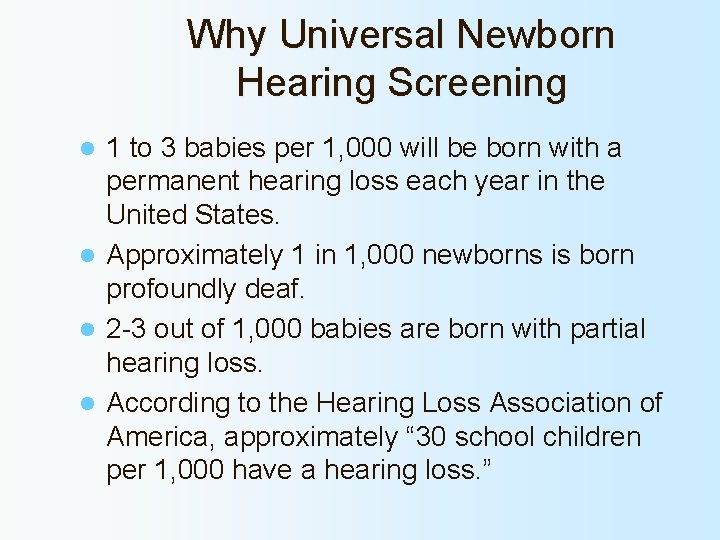
Why Universal Newborn Hearing Screening 1 to 3 babies per 1, 000 will be born with a permanent hearing loss each year in the United States. l Approximately 1 in 1, 000 newborns is born profoundly deaf. l 2 -3 out of 1, 000 babies are born with partial hearing loss. l According to the Hearing Loss Association of America, approximately “ 30 school children per 1, 000 have a hearing loss. ” l
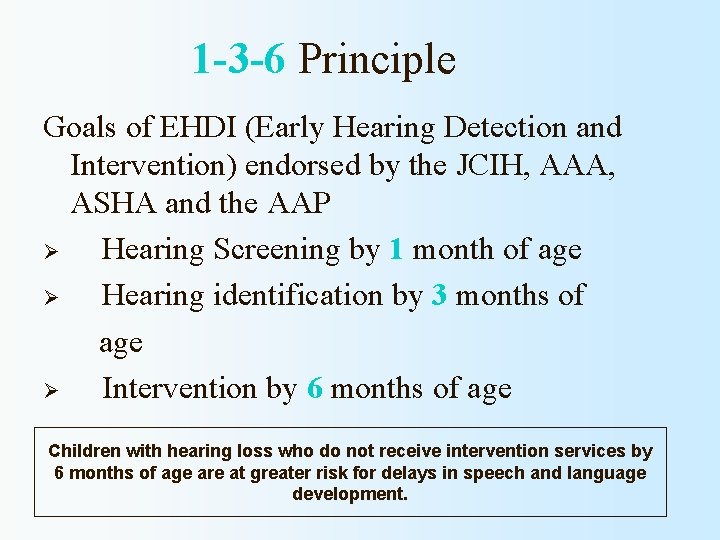
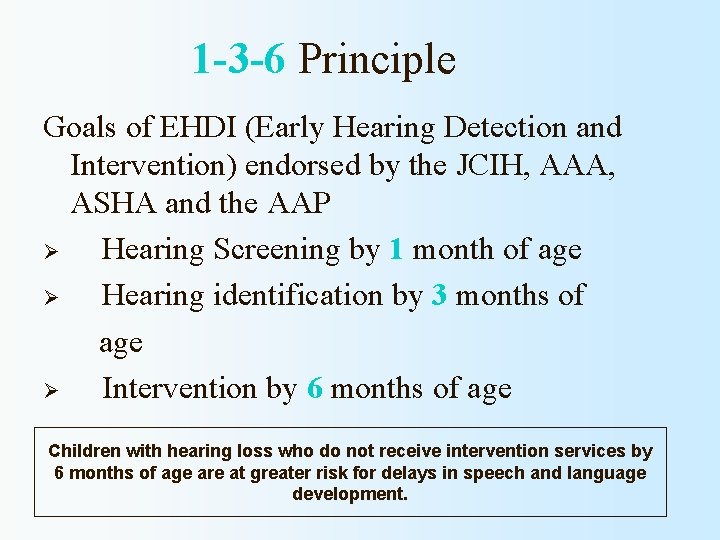
1 -3 -6 Principle Goals of EHDI (Early Hearing Detection and Intervention) endorsed by the JCIH, AAA, ASHA and the AAP Ø Hearing Screening by 1 month of age Ø Hearing identification by 3 months of age Ø Intervention by 6 months of age Children with hearing loss who do not receive intervention services by 6 months of age are at greater risk for delays in speech and language development.

Legislation
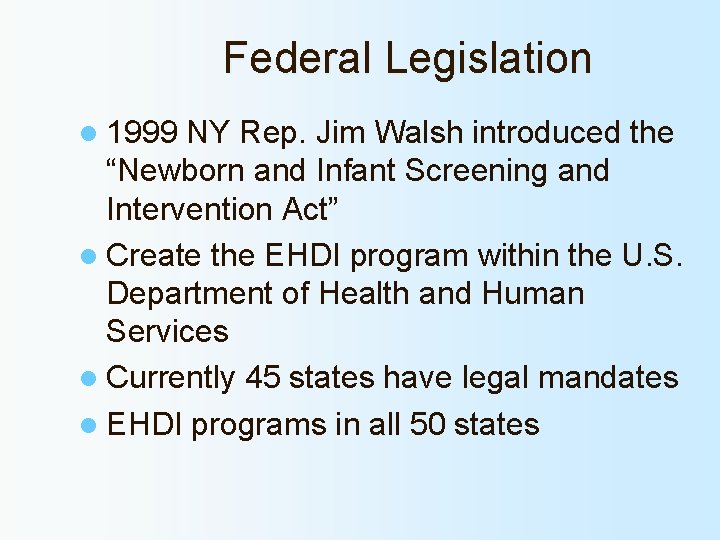
Federal Legislation l 1999 NY Rep. Jim Walsh introduced the “Newborn and Infant Screening and Intervention Act” l Create the EHDI program within the U. S. Department of Health and Human Services l Currently 45 states have legal mandates l EHDI programs in all 50 states
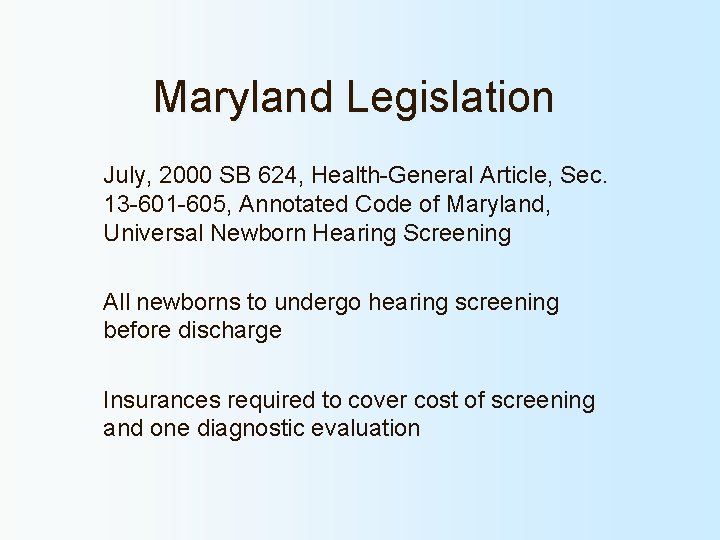
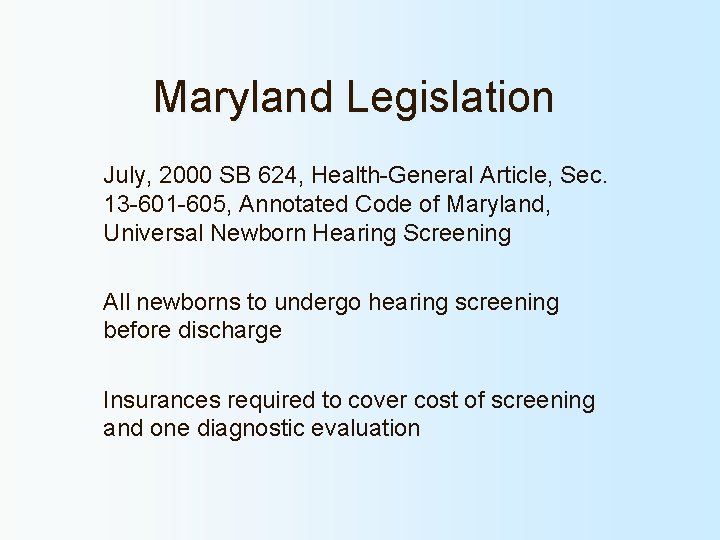
Maryland Legislation July, 2000 SB 624, Health-General Article, Sec. 13 -601 -605, Annotated Code of Maryland, Universal Newborn Hearing Screening All newborns to undergo hearing screening before discharge Insurances required to cover cost of screening and one diagnostic evaluation
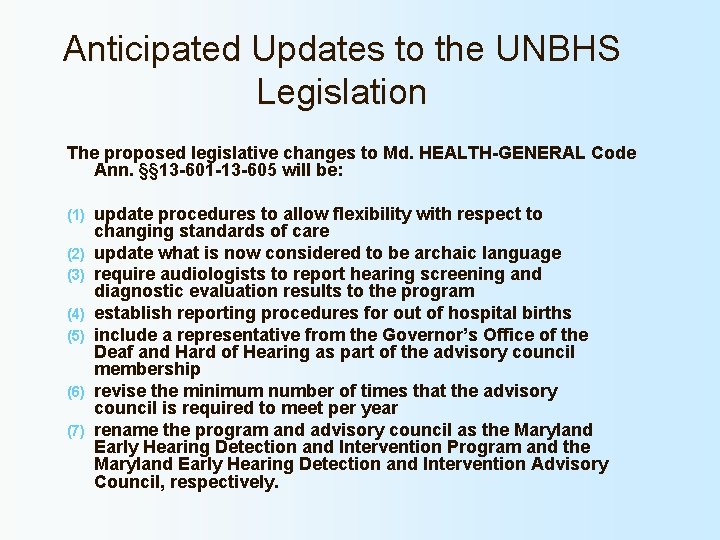
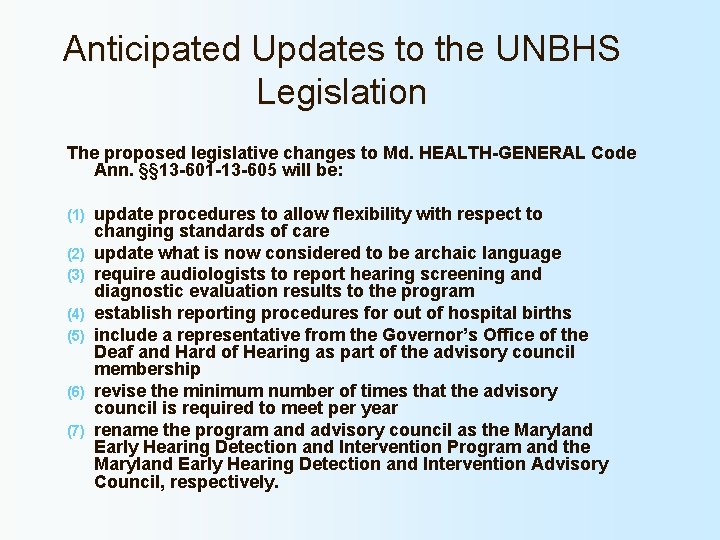
Anticipated Updates to the UNBHS Legislation The proposed legislative changes to Md. HEALTH-GENERAL Code Ann. §§ 13 -601 -13 -605 will be: (1) (2) (3) (4) (5) (6) (7) update procedures to allow flexibility with respect to changing standards of care update what is now considered to be archaic language require audiologists to report hearing screening and diagnostic evaluation results to the program establish reporting procedures for out of hospital births include a representative from the Governor’s Office of the Deaf and Hard of Hearing as part of the advisory council membership revise the minimum number of times that the advisory council is required to meet per year rename the program and advisory council as the Maryland Early Hearing Detection and Intervention Program and the Maryland Early Hearing Detection and Intervention Advisory Council, respectively.
Program Methods
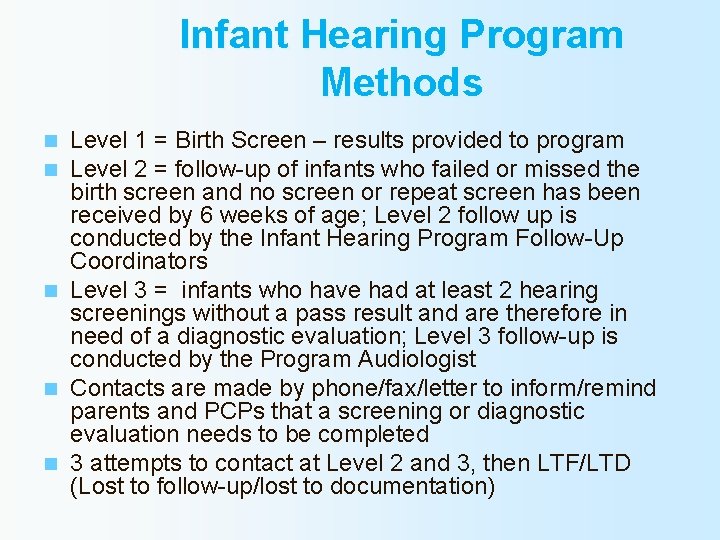
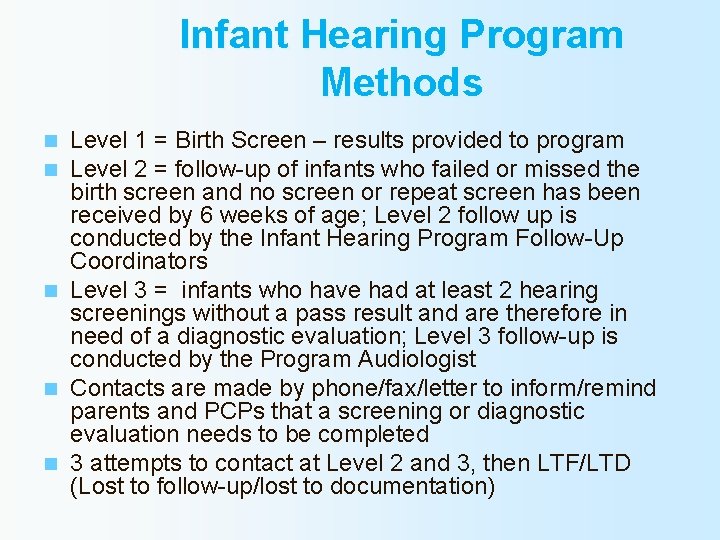
Infant Hearing Program Methods Level 1 = Birth Screen – results provided to program Level 2 = follow-up of infants who failed or missed the birth screen and no screen or repeat screen has been received by 6 weeks of age; Level 2 follow up is conducted by the Infant Hearing Program Follow-Up Coordinators n Level 3 = infants who have had at least 2 hearing screenings without a pass result and are therefore in need of a diagnostic evaluation; Level 3 follow-up is conducted by the Program Audiologist n Contacts are made by phone/fax/letter to inform/remind parents and PCPs that a screening or diagnostic evaluation needs to be completed n 3 attempts to contact at Level 2 and 3, then LTF/LTD (Lost to follow-up/lost to documentation) n n
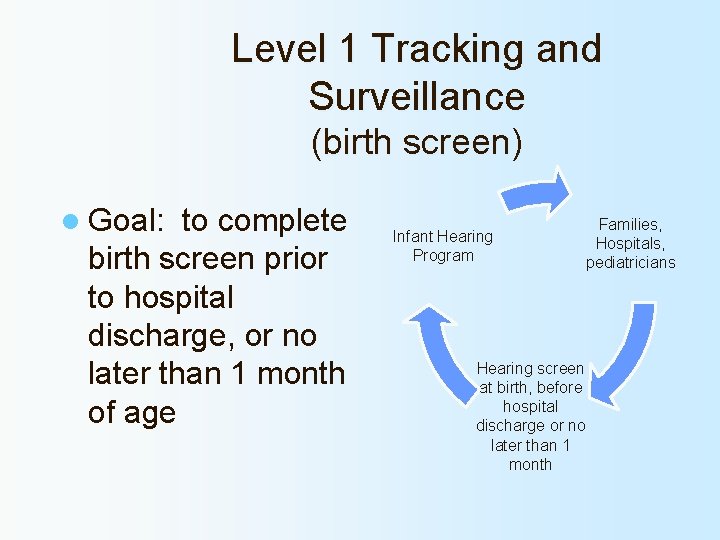
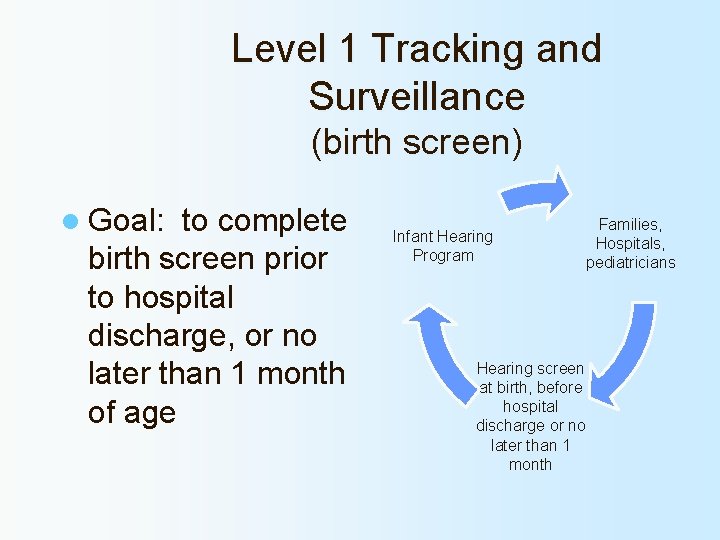
Level 1 Tracking and Surveillance (birth screen) l Goal: to complete birth screen prior to hospital discharge, or no later than 1 month of age Infant Hearing Program Families, Hospitals, pediatricians Hearing screen at birth, before hospital discharge or no later than 1 month
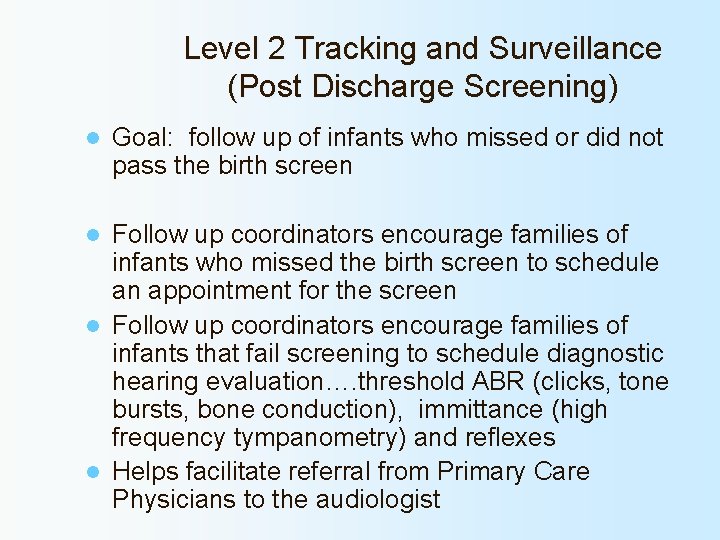
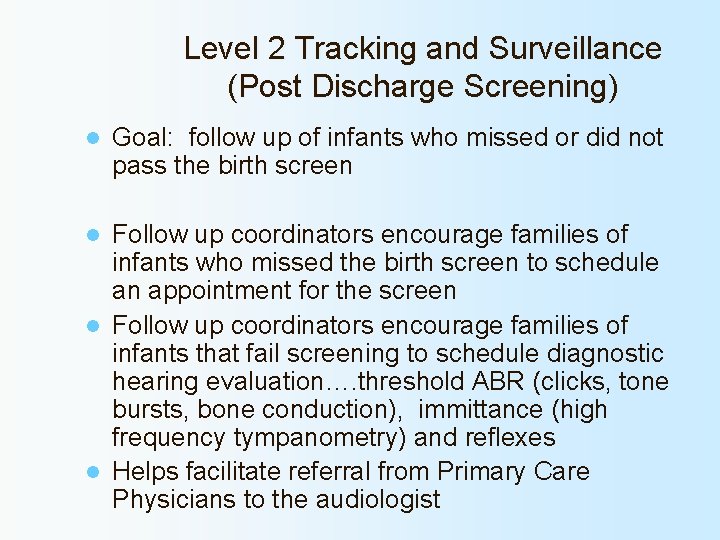
Level 2 Tracking and Surveillance (Post Discharge Screening) l Goal: follow up of infants who missed or did not pass the birth screen Follow up coordinators encourage families of infants who missed the birth screen to schedule an appointment for the screen l Follow up coordinators encourage families of infants that fail screening to schedule diagnostic hearing evaluation…. threshold ABR (clicks, tone bursts, bone conduction), immittance (high frequency tympanometry) and reflexes l Helps facilitate referral from Primary Care Physicians to the audiologist l
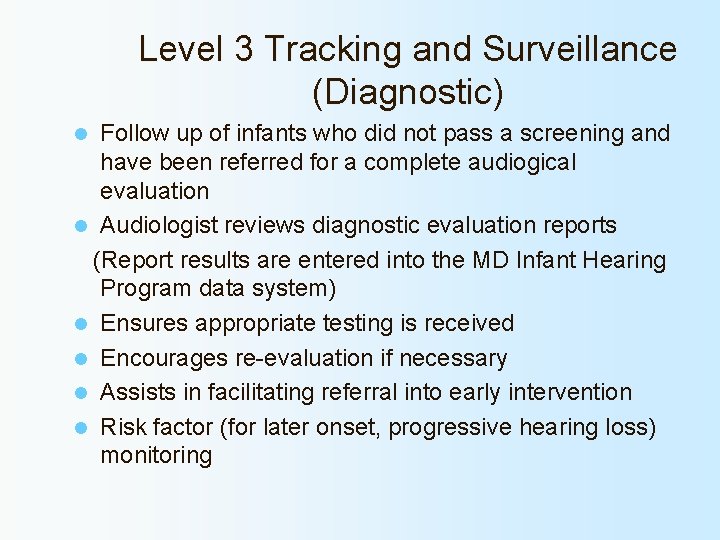
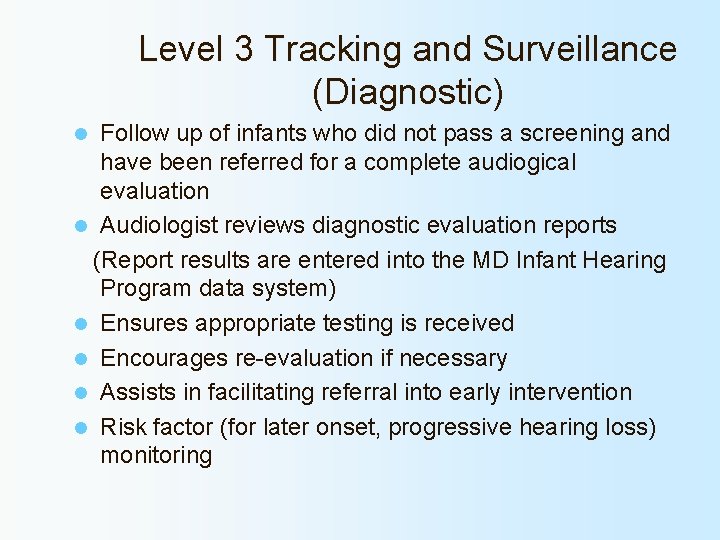
Level 3 Tracking and Surveillance (Diagnostic) Follow up of infants who did not pass a screening and have been referred for a complete audiogical evaluation l Audiologist reviews diagnostic evaluation reports (Report results are entered into the MD Infant Hearing Program data system) l Ensures appropriate testing is received l Encourages re-evaluation if necessary l Assists in facilitating referral into early intervention l Risk factor (for later onset, progressive hearing loss) monitoring l
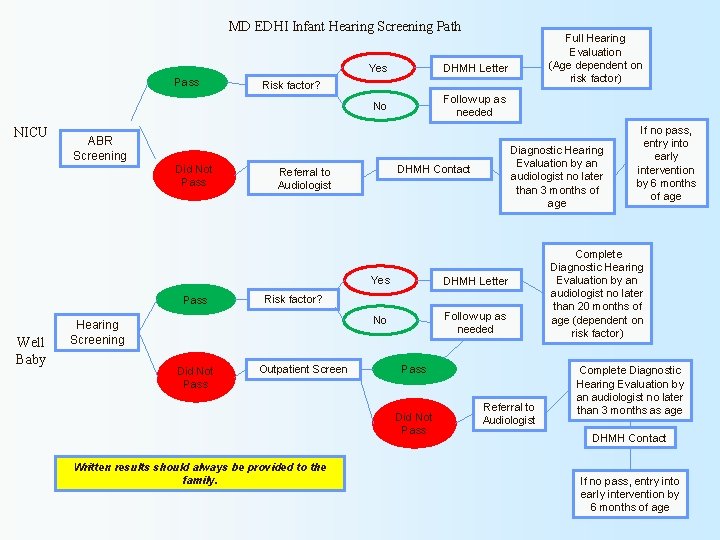
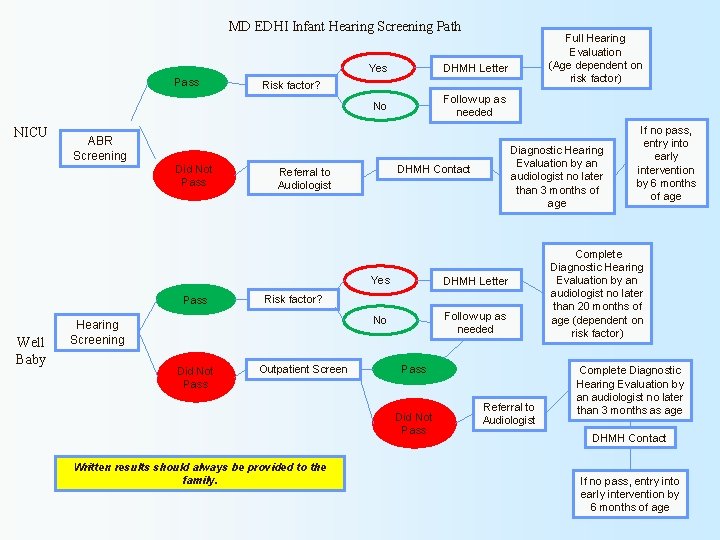
MD EDHI Infant Hearing Screening Path Pass NICU DHMH Letter No Follow up as needed Risk factor? ABR Screening Did Not Pass Well Baby Yes Diagnostic Hearing Evaluation by an audiologist no later than 3 months of age DHMH Contact Referral to Audiologist Yes DHMH Letter No Follow up as needed Risk factor? Hearing Screening Did Not Pass Full Hearing Evaluation (Age dependent on risk factor) Outpatient Screen Pass Did Not Pass Written results should always be provided to the family. Referral to Audiologist If no pass, entry into early intervention by 6 months of age Complete Diagnostic Hearing Evaluation by an audiologist no later than 20 months of age (dependent on risk factor) Complete Diagnostic Hearing Evaluation by an audiologist no later than 3 months as age DHMH Contact If no pass, entry into early intervention by 6 months of age
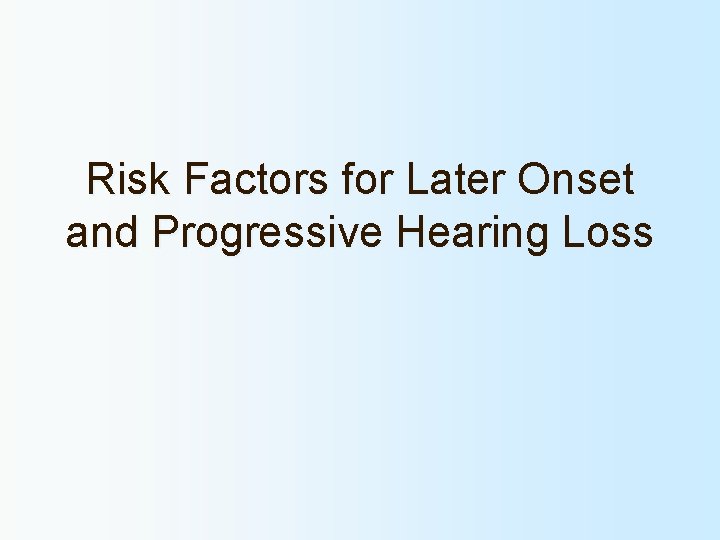
Risk Factors for Later Onset and Progressive Hearing Loss
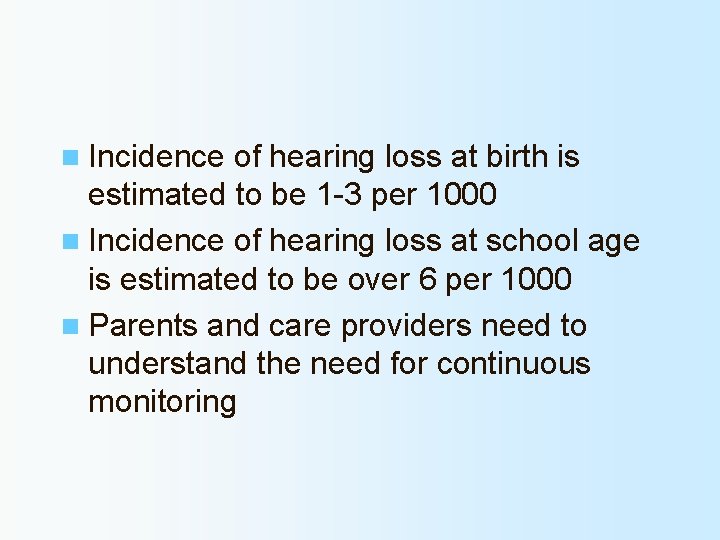
n Incidence of hearing loss at birth is estimated to be 1 -3 per 1000 n Incidence of hearing loss at school age is estimated to be over 6 per 1000 n Parents and care providers need to understand the need for continuous monitoring
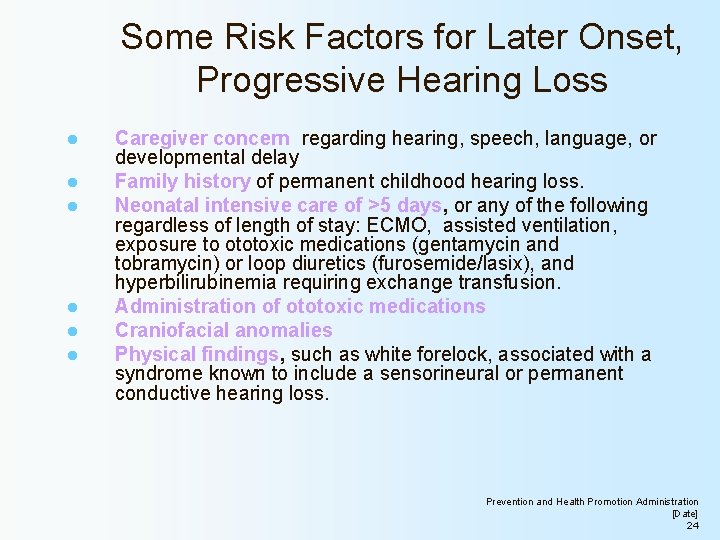
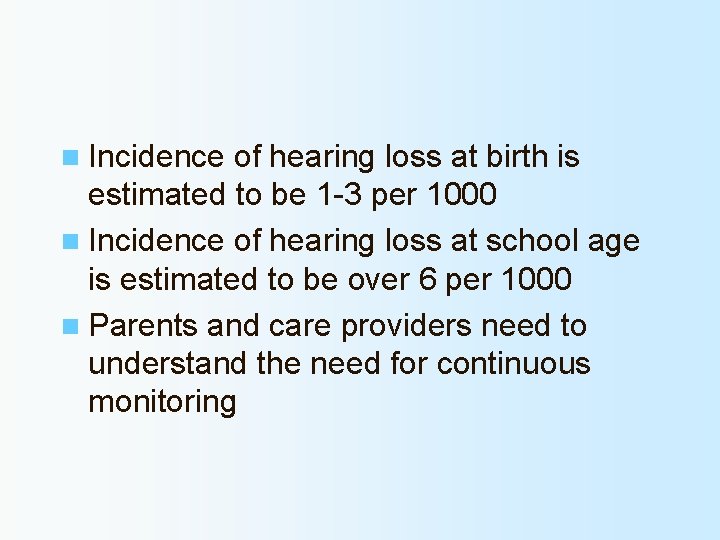
Some Risk Factors for Later Onset, Progressive Hearing Loss l l l Caregiver concern regarding hearing, speech, language, or developmental delay Family history of permanent childhood hearing loss. Neonatal intensive care of >5 days, or any of the following regardless of length of stay: ECMO, assisted ventilation, exposure to ototoxic medications (gentamycin and tobramycin) or loop diuretics (furosemide/lasix), and hyperbilirubinemia requiring exchange transfusion. Administration of ototoxic medications Craniofacial anomalies Physical findings, such as white forelock, associated with a syndrome known to include a sensorineural or permanent conductive hearing loss. Prevention and Health Promotion Administration [Date] 24
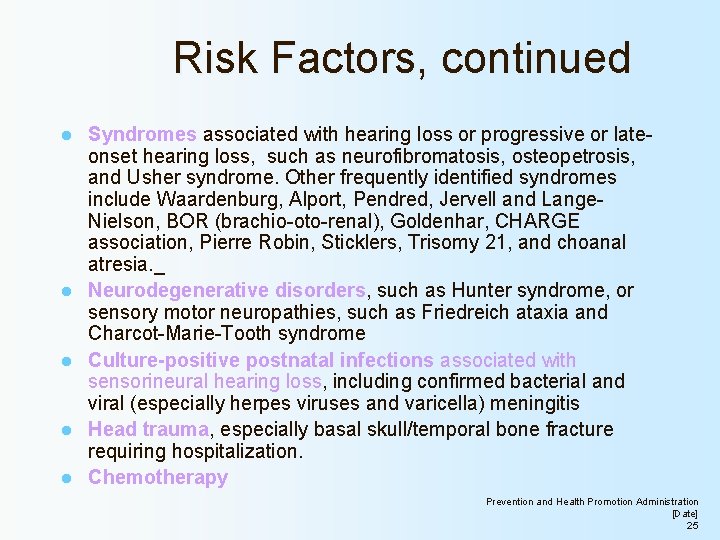
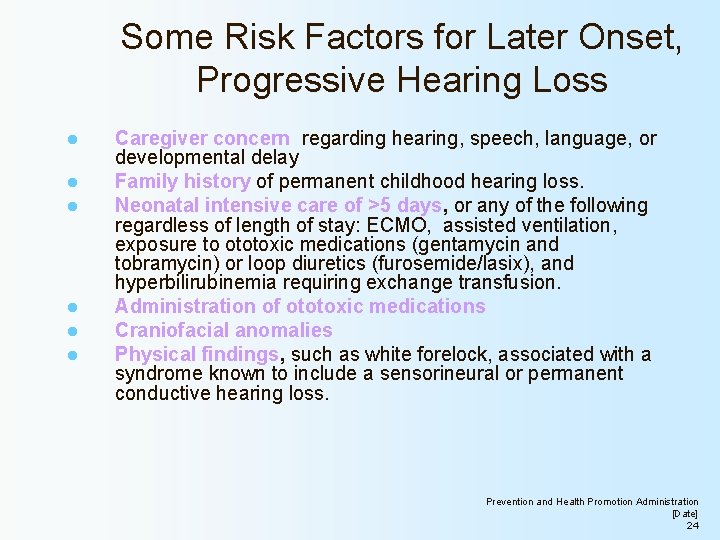
Risk Factors, continued l l l Syndromes associated with hearing loss or progressive or lateonset hearing loss, such as neurofibromatosis, osteopetrosis, and Usher syndrome. Other frequently identified syndromes include Waardenburg, Alport, Pendred, Jervell and Lange. Nielson, BOR (brachio-oto-renal), Goldenhar, CHARGE association, Pierre Robin, Sticklers, Trisomy 21, and choanal atresia. _ Neurodegenerative disorders, such as Hunter syndrome, or sensory motor neuropathies, such as Friedreich ataxia and Charcot-Marie-Tooth syndrome Culture-positive postnatal infections associated with sensorineural hearing loss, including confirmed bacterial and viral (especially herpes viruses and varicella) meningitis Head trauma, especially basal skull/temporal bone fracture requiring hospitalization. Chemotherapy Prevention and Health Promotion Administration [Date] 25
![Prevention and Health Promotion Administration Date 26 Prevention and Health Promotion Administration [Date] 26](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-26.jpg)
Prevention and Health Promotion Administration [Date] 26

Reporting Screening and Diagnostic Test Results to MD EHDI
MD EHDI reporting l Starting June, 2008 l Hearing screening results entered into online data management system : e. SP l Birthing hospitals receive e. SP™ training
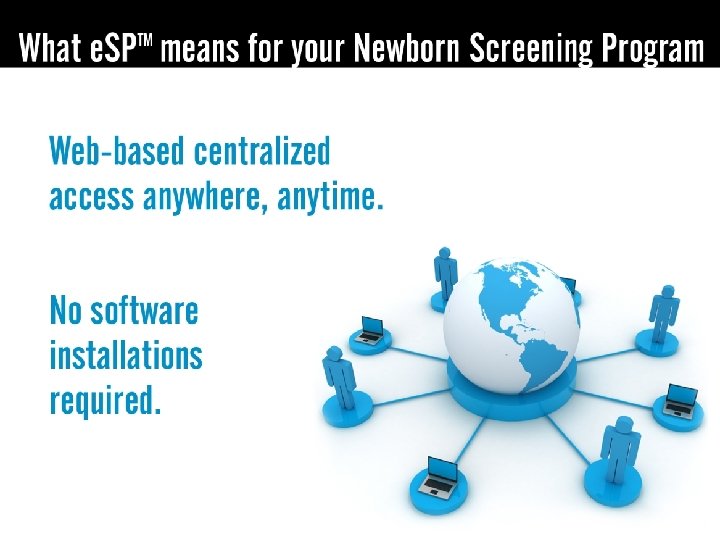
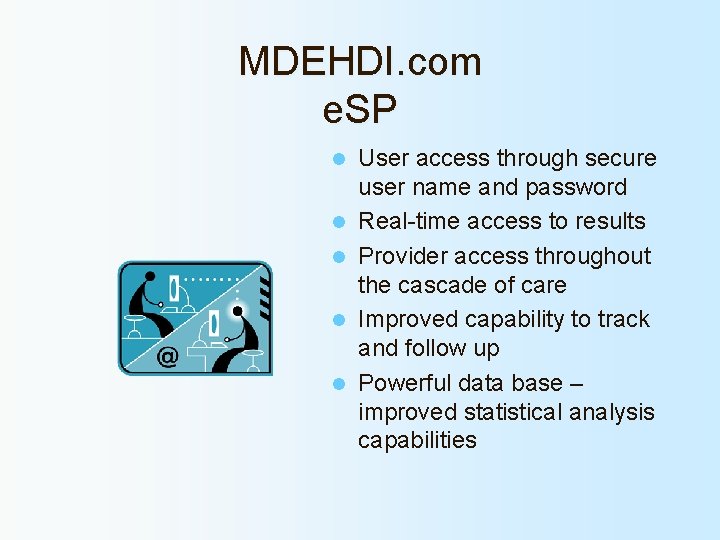
MDEHDI. com e. SP l l l User access through secure user name and password Real-time access to results Provider access throughout the cascade of care Improved capability to track and follow up Powerful data base – improved statistical analysis capabilities
Statistics
![Prevention and Health Promotion Administration Date 33 Prevention and Health Promotion Administration [Date] 33](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-33.jpg)
Prevention and Health Promotion Administration [Date] 33
![Prevention and Health Promotion Administration Date 34 Prevention and Health Promotion Administration [Date] 34](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-34.jpg)
Prevention and Health Promotion Administration [Date] 34
![Prevention and Health Promotion Administration Date 35 Prevention and Health Promotion Administration [Date] 35](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-35.jpg)
Prevention and Health Promotion Administration [Date] 35
![Prevention and Health Promotion Administration Date 36 Prevention and Health Promotion Administration [Date] 36](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-36.jpg)
Prevention and Health Promotion Administration [Date] 36
![Prevention and Health Promotion Administration Date 37 Prevention and Health Promotion Administration [Date] 37](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-37.jpg)
Prevention and Health Promotion Administration [Date] 37
![Prevention and Health Promotion Administration Date 38 Prevention and Health Promotion Administration [Date] 38](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-38.jpg)
Prevention and Health Promotion Administration [Date] 38
![Prevention and Health Promotion Administration Date 39 Prevention and Health Promotion Administration [Date] 39](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-39.jpg)
Prevention and Health Promotion Administration [Date] 39
![Prevention and Health Promotion Administration Date 40 Prevention and Health Promotion Administration [Date] 40](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-40.jpg)
Prevention and Health Promotion Administration [Date] 40
![Prevention and Health Promotion Administration Date 41 Prevention and Health Promotion Administration [Date] 41](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-41.jpg)
Prevention and Health Promotion Administration [Date] 41
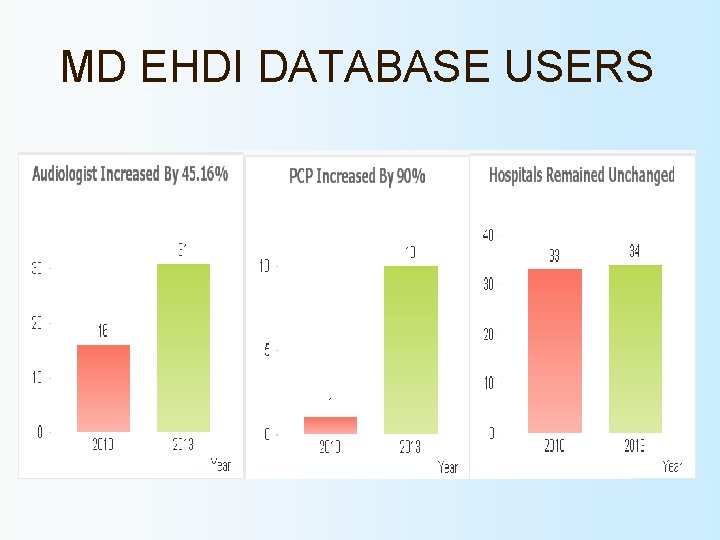
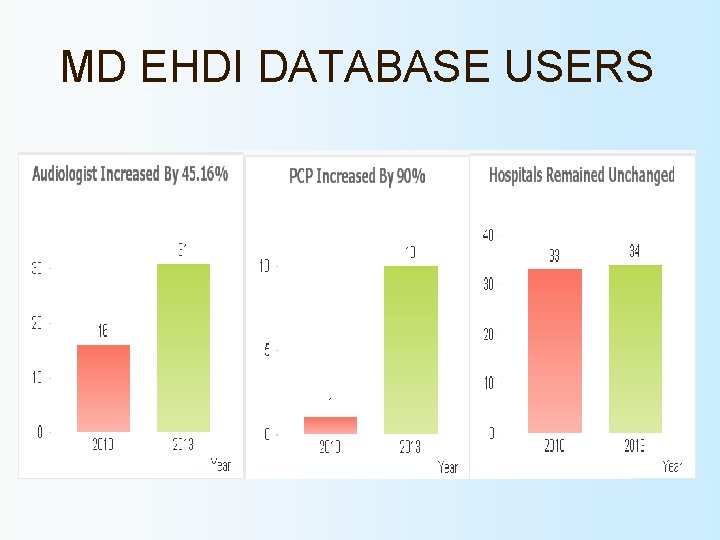
MD EHDI DATABASE USERS
If only it were that easy… Phone calls, faxes, letters! l Parents and physicians who have not yet followed up l Families’ “not at this address”, phone number “has been disconnected and is no longer in service” l
![Challenges Prevention and Health Promotion Administration Date 44 Challenges Prevention and Health Promotion Administration [Date] 44](https://slidetodoc.com/presentation_image_h/e6d7e1ff40e2c8a0d58e1891bb4b80a6/image-44.jpg)
Challenges Prevention and Health Promotion Administration [Date] 44
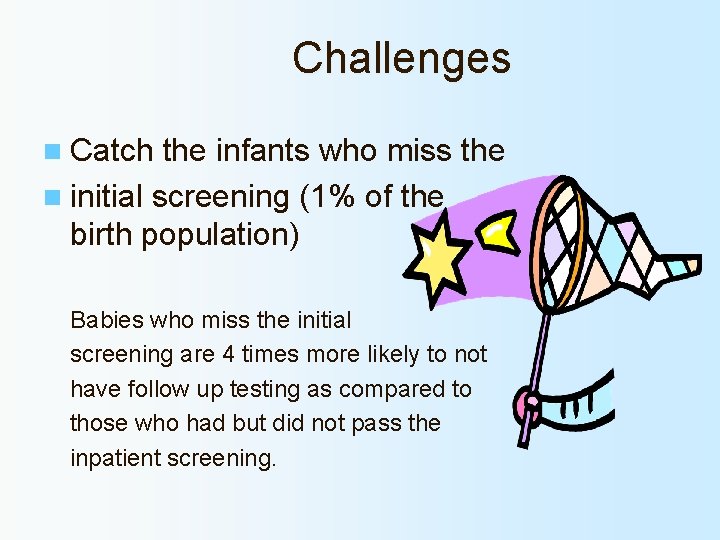
Challenges n Catch the infants who miss the n initial screening (1% of the birth population) Babies who miss the initial screening are 4 times more likely to not have follow up testing as compared to those who had but did not pass the inpatient screening.
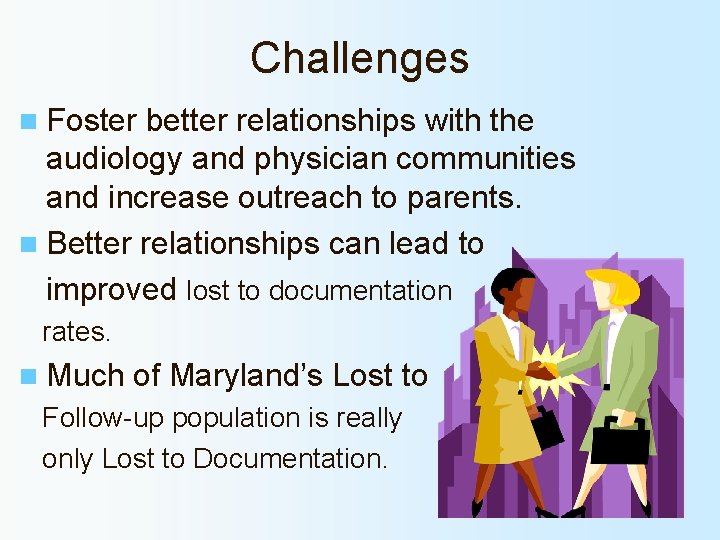
Challenges n Foster better relationships with the audiology and physician communities and increase outreach to parents. n Better relationships can lead to improved lost to documentation rates. n Much of Maryland’s Lost to Follow-up population is really only Lost to Documentation.
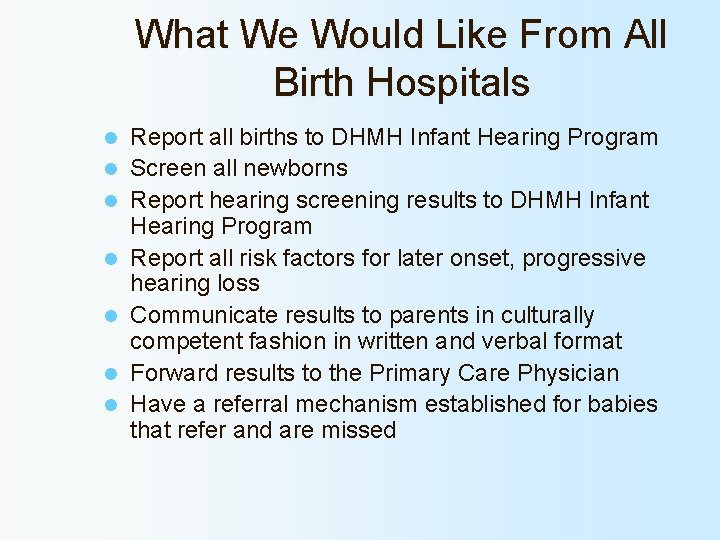
What We Would Like From All Birth Hospitals l l l l Report all births to DHMH Infant Hearing Program Screen all newborns Report hearing screening results to DHMH Infant Hearing Program Report all risk factors for later onset, progressive hearing loss Communicate results to parents in culturally competent fashion in written and verbal format Forward results to the Primary Care Physician Have a referral mechanism established for babies that refer and are missed
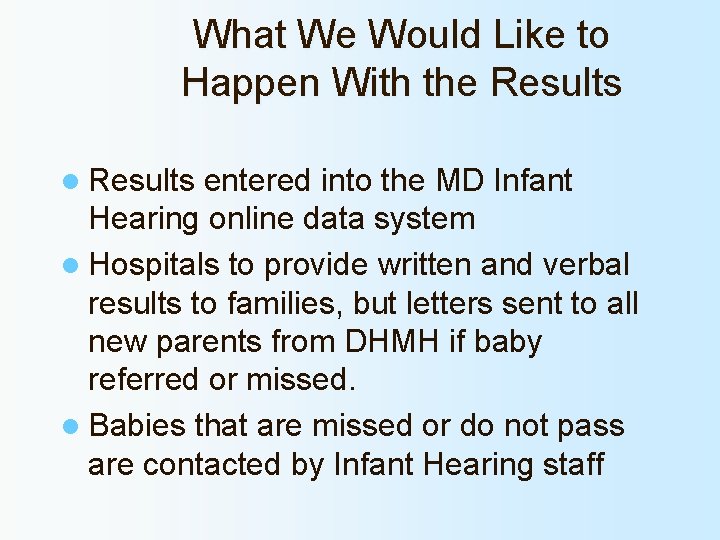
What We Would Like to Happen With the Results l Results entered into the MD Infant Hearing online data system l Hospitals to provide written and verbal results to families, but letters sent to all new parents from DHMH if baby referred or missed. l Babies that are missed or do not pass are contacted by Infant Hearing staff
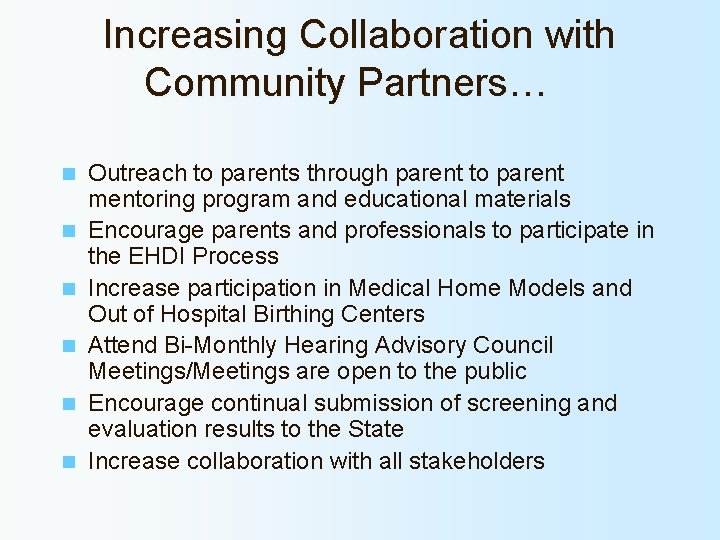
Increasing Collaboration with Community Partners… n n n Outreach to parents through parent to parent mentoring program and educational materials Encourage parents and professionals to participate in the EHDI Process Increase participation in Medical Home Models and Out of Hospital Birthing Centers Attend Bi-Monthly Hearing Advisory Council Meetings/Meetings are open to the public Encourage continual submission of screening and evaluation results to the State Increase collaboration with all stakeholders
MD EHDI Partnerships Parent Connections Mentor Program, through the Parents Place of Maryland AAP EHDI Chapter Champion – Susan Panny, M. D.
Funding Sources: Centers for Disease Control and Prevention (CDC) • Health Resources and Services Administration (HRSA) •
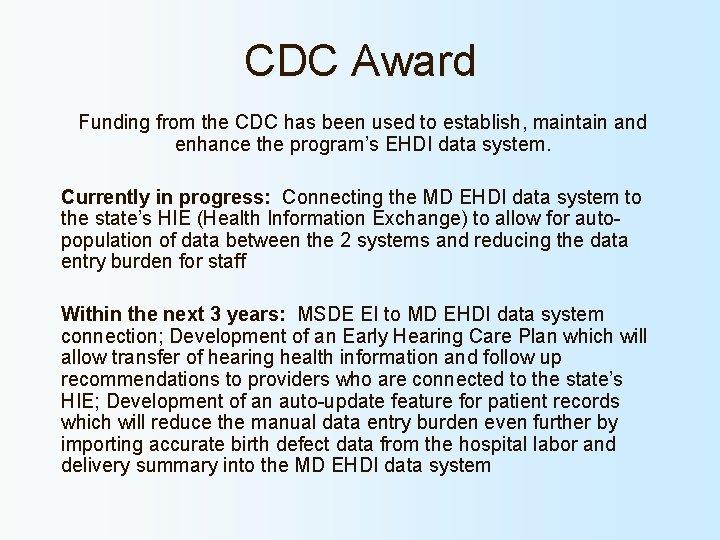
CDC Award Funding from the CDC has been used to establish, maintain and enhance the program’s EHDI data system. Currently in progress: Connecting the MD EHDI data system to the state’s HIE (Health Information Exchange) to allow for autopopulation of data between the 2 systems and reducing the data entry burden for staff Within the next 3 years: MSDE EI to MD EHDI data system connection; Development of an Early Hearing Care Plan which will allow transfer of hearing health information and follow up recommendations to providers who are connected to the state’s HIE; Development of an auto-update feature for patient records which will reduce the manual data entry burden even further by importing accurate birth defect data from the hospital labor and delivery summary into the MD EHDI data system
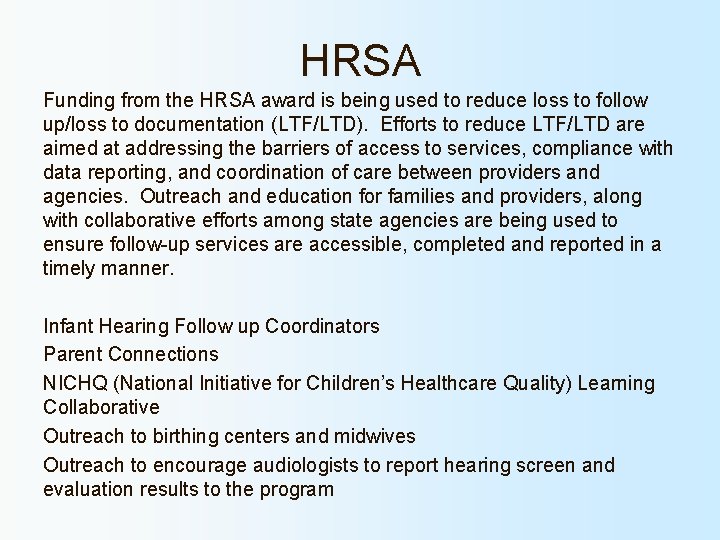
HRSA Funding from the HRSA award is being used to reduce loss to follow up/loss to documentation (LTF/LTD). Efforts to reduce LTF/LTD are aimed at addressing the barriers of access to services, compliance with data reporting, and coordination of care between providers and agencies. Outreach and education for families and providers, along with collaborative efforts among state agencies are being used to ensure follow-up services are accessible, completed and reported in a timely manner. Infant Hearing Follow up Coordinators Parent Connections NICHQ (National Initiative for Children’s Healthcare Quality) Learning Collaborative Outreach to birthing centers and midwives Outreach to encourage audiologists to report hearing screen and evaluation results to the program
Additional Information: EHDI-PALS online database (www. ehdipals. org) Pediatric Audiology Links to Services – web-based link to information, resources and services for children with hearing loss including an audiology facility locator. The Hearing Advisory Council meets bi-monthly on the 3 rd Thursday, beginning in January. Meetings are open to the public and are held at 12: 30 pm at the Hearing and Speech Agency in Baltimore.

Maryland Infant Hearing Program Tanya D Green, Program Chief 410 -767 -6432 tanya. green@maryland. gov Erin Filippone, Program Audiologist 410 -767 -6762 erin. filippone@maryland. gov Theresa Thompson, Follow-up Coordinator 410 -767 -5093 theresa. thompson@maryland. gov Leah Washington, Follow-up Coordinator 410 -767 -6659 leah. washington@maryland. gov
Thank you!! This presentation will be made available on the MD EHDI website. http: //phpa. dhmh. maryland. gov/genetics/sitep ages/inf_hrg. aspx