The Management of SMA Syndrome Dr Chunfai LAU






- Slides: 34
The Management of SMA Syndrome Dr Chun-fai LAU United Christian Hospital Joint Hospital Surgical Grand Round 11 Feb 2012
Case presentation n n Mr. Leung M/63 Diagnosed to have localized CA sigmoid colon in Oct 2011 PMH u u Old CVA Ankylosing spondylitis
Case presentation n Lap converted open sigmoidectomy on 13 Oct 2011 Post-op required ICU care with ventilatory support for aspiration pneumonia Unable to tolerate oral feeding with repeated vomiting
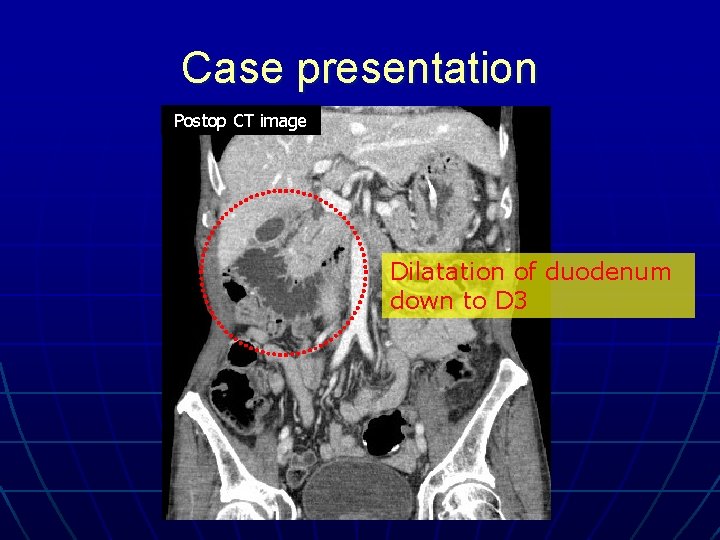
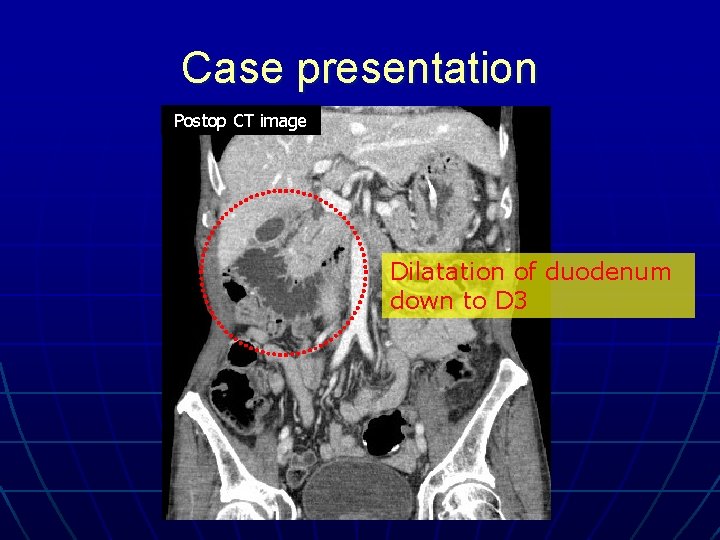
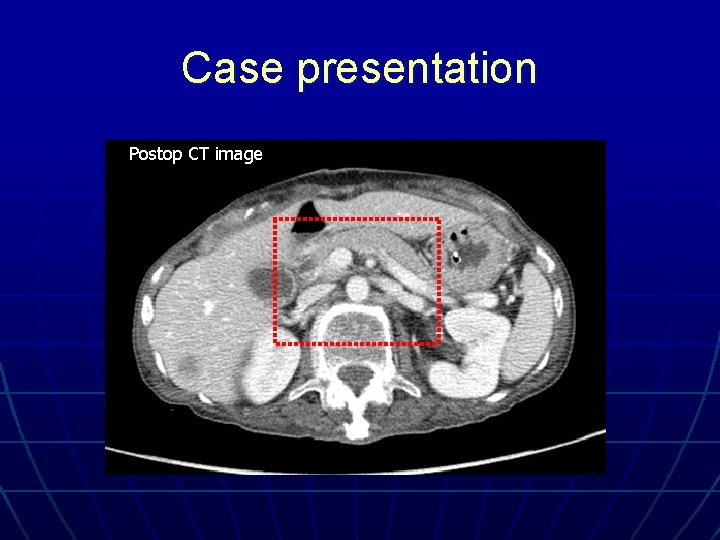
Case presentation Postop CT image Dilatation of duodenum down to D 3
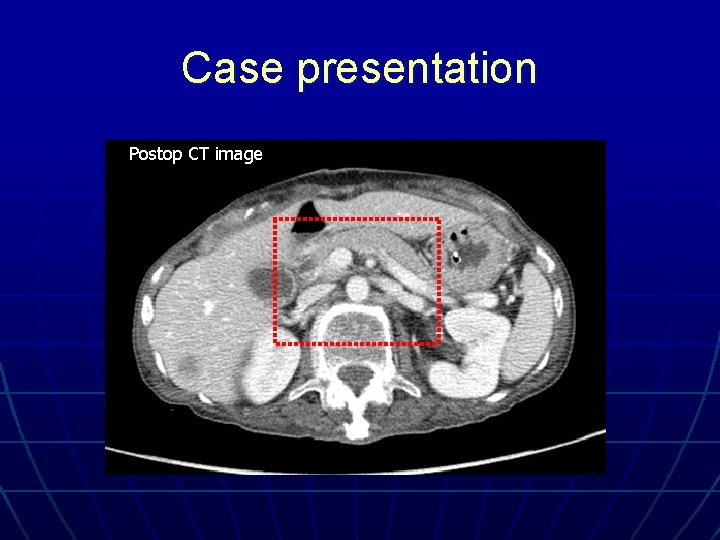
Case presentation Postop CT image
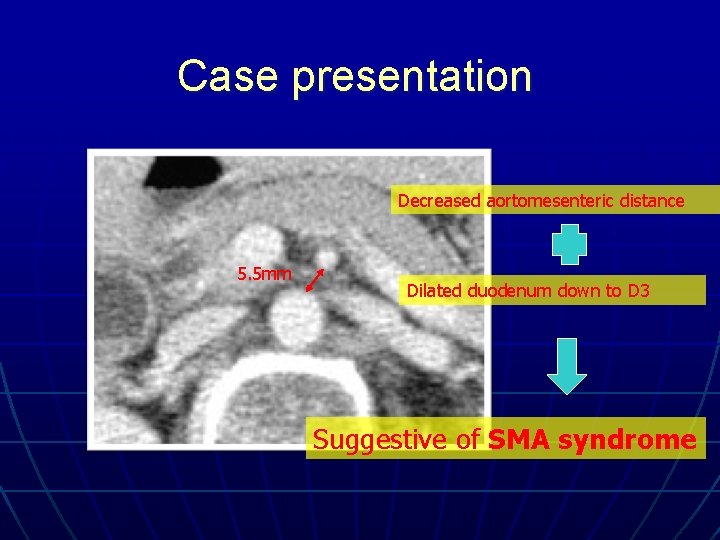
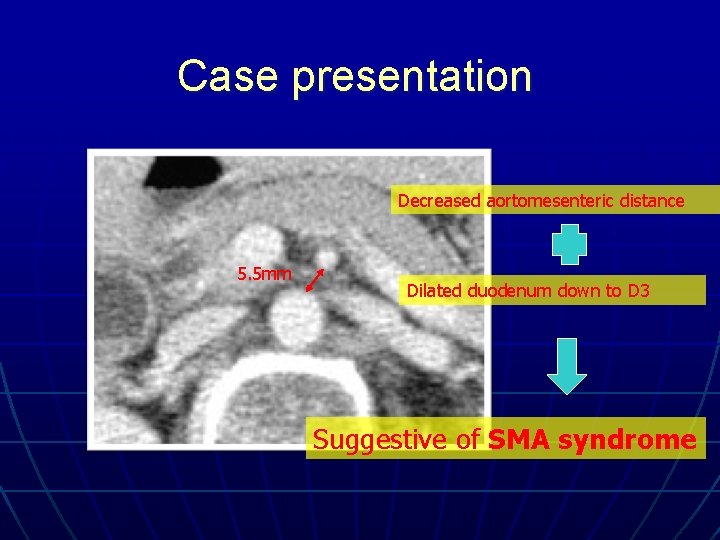
Case presentation Decreased aortomesenteric distance 5. 5 mm Dilated duodenum down to D 3 Suggestive of SMA syndrome
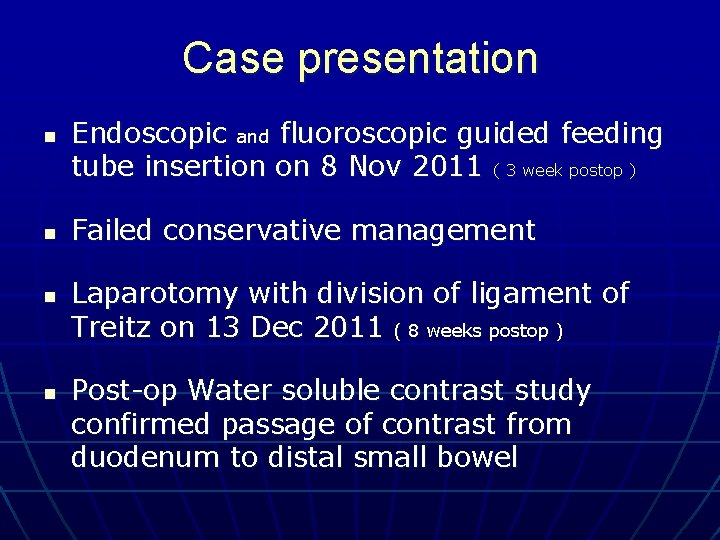
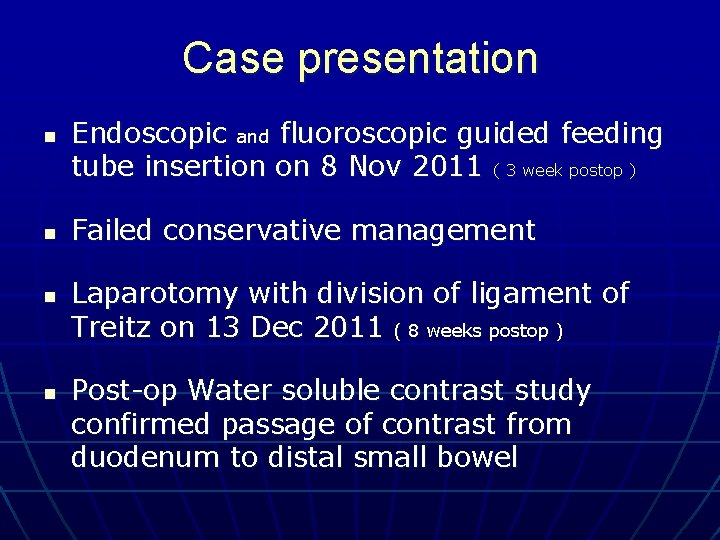
Case presentation n n Endoscopic and fluoroscopic guided feeding tube insertion on 8 Nov 2011 ( 3 week postop ) Failed conservative management Laparotomy with division of ligament of Treitz on 13 Dec 2011 ( 8 weeks postop ) Post-op Water soluble contrast study confirmed passage of contrast from duodenum to distal small bowel
Superior Mesenteric Artery (SMA) Syndrome
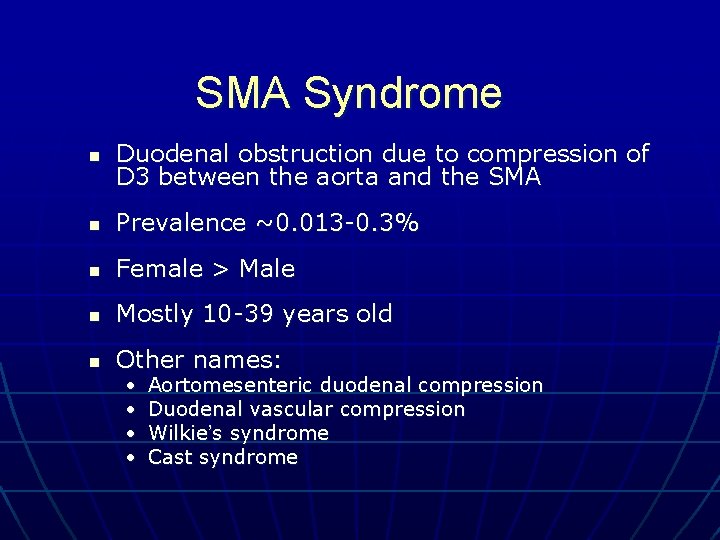
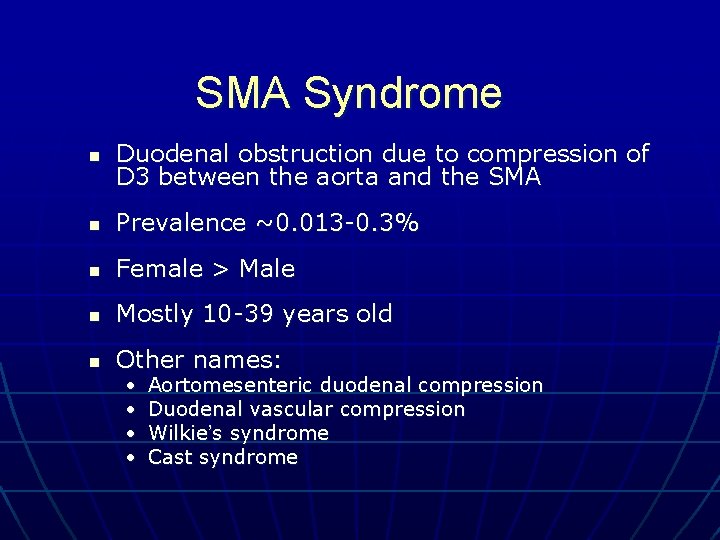
SMA Syndrome n Duodenal obstruction due to compression of D 3 between the aorta and the SMA n Prevalence ~0. 013 -0. 3% n Female > Male n Mostly 10 -39 years old n Other names: • • Aortomesenteric duodenal compression Duodenal vascular compression Wilkie’s syndrome Cast syndrome

History n 1842: 1 st described by the Austrian professor Carl von Rokitansky n 1908: 1 st operative treatment by Stavely (DJ) n 1927: Wilkie published the largest SMA syndrome study based on 75 cases. He concluded that DJ was the treatment of choice n 1995: 1 st laparoscopic treatment performed by Massoud, by dividing the ligament of Treitz n 1998: 1 st laparoscopic DJ performed by Gersin and Heniford
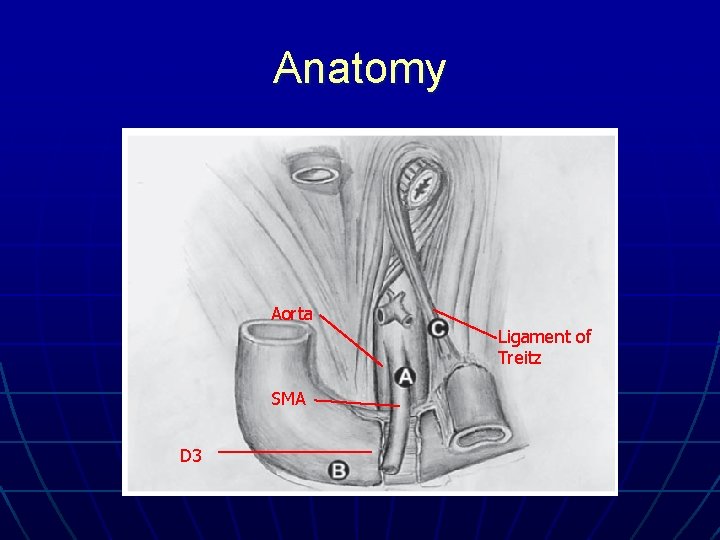
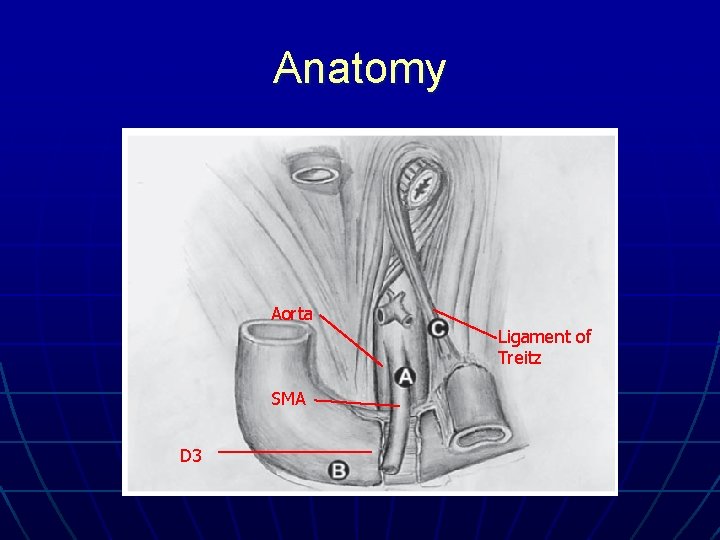
Anatomy Aorta Ligament of Treitz SMA D 3
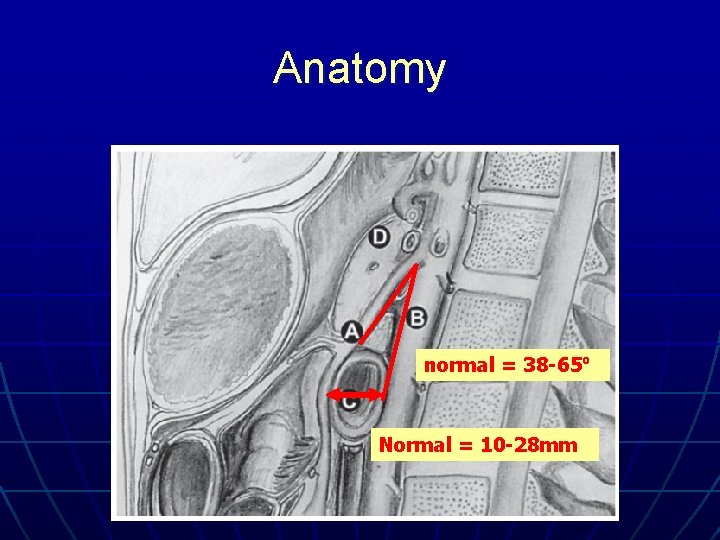
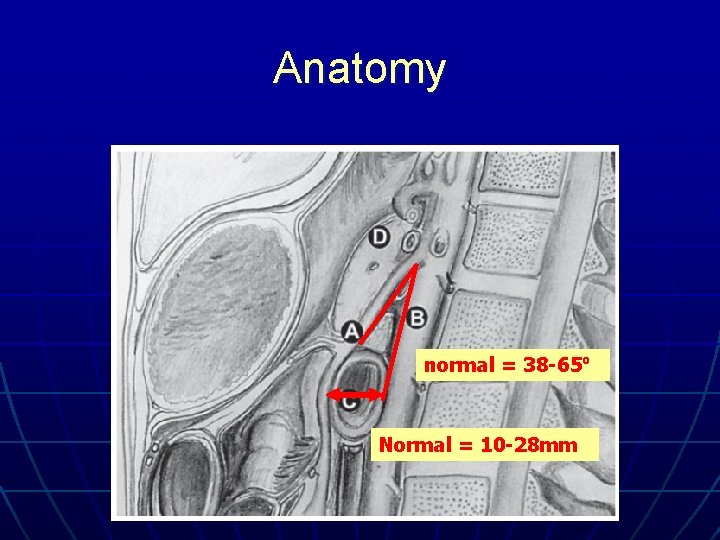
Anatomy normal = 38 -65º Normal = 10 -28 mm
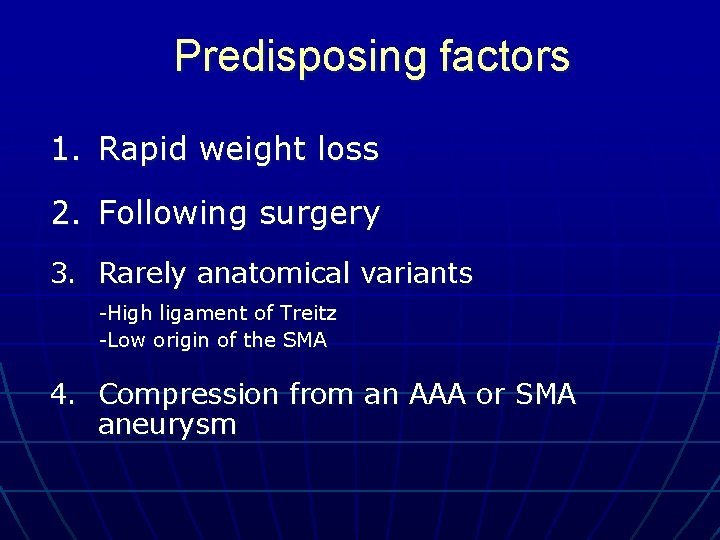
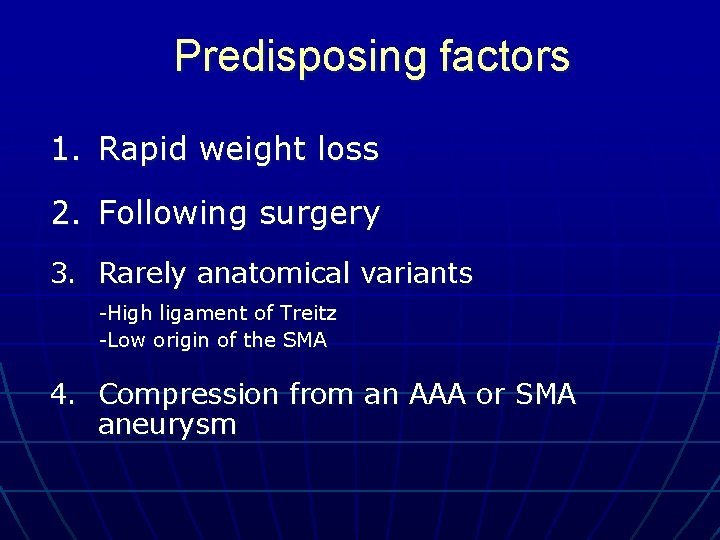
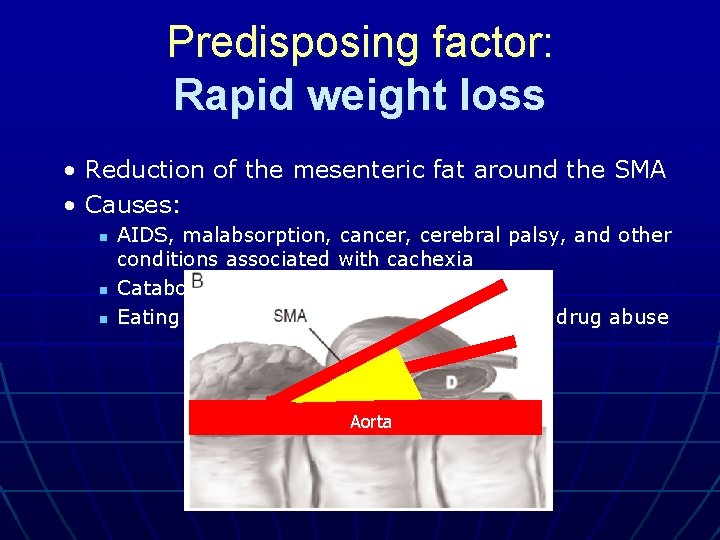
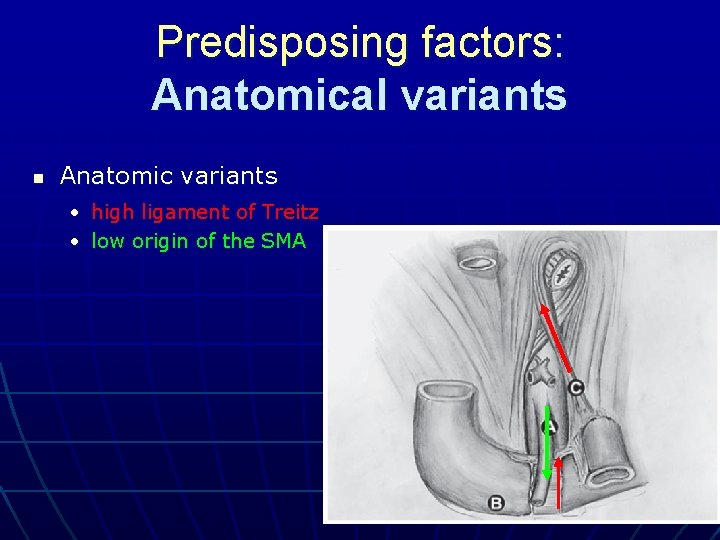
Predisposing factors 1. Rapid weight loss 2. Following surgery 3. Rarely anatomical variants -High ligament of Treitz -Low origin of the SMA 4. Compression from an AAA or SMA aneurysm
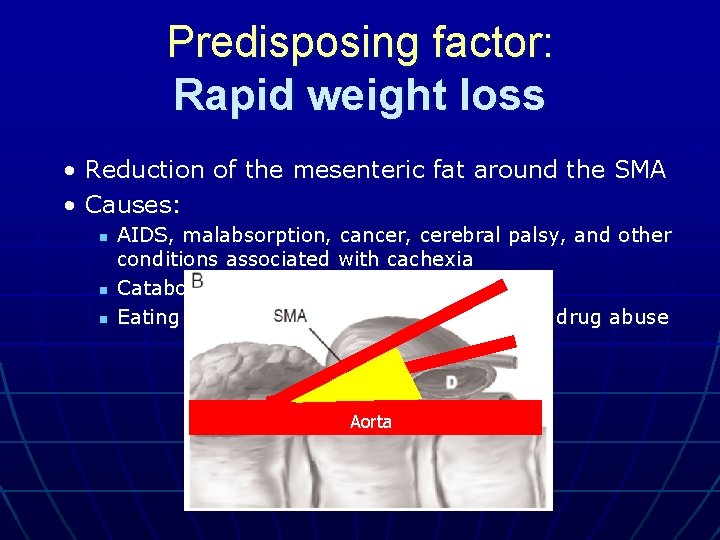
Predisposing factor: Rapid weight loss • Reduction of the mesenteric fat around the SMA • Causes: n n n AIDS, malabsorption, cancer, cerebral palsy, and other conditions associated with cachexia Catabolic conditions e. g. burns Eating disorders e. g. anorexia nervosa and drug abuse Aorta
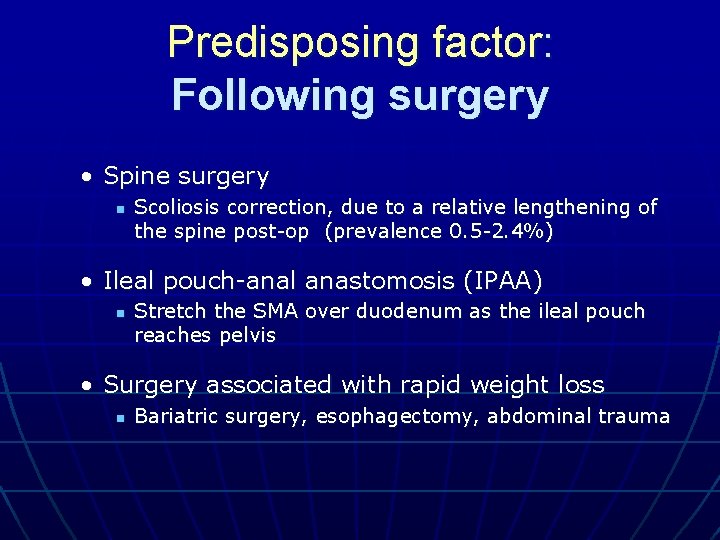
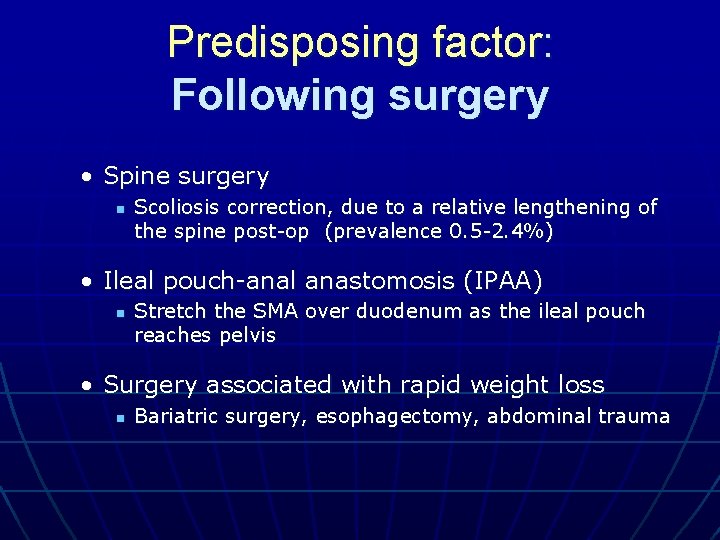
Predisposing factor: Following surgery • Spine surgery n Scoliosis correction, due to a relative lengthening of the spine post-op (prevalence 0. 5 -2. 4%) • Ileal pouch-anal anastomosis (IPAA) n Stretch the SMA over duodenum as the ileal pouch reaches pelvis • Surgery associated with rapid weight loss n Bariatric surgery, esophagectomy, abdominal trauma
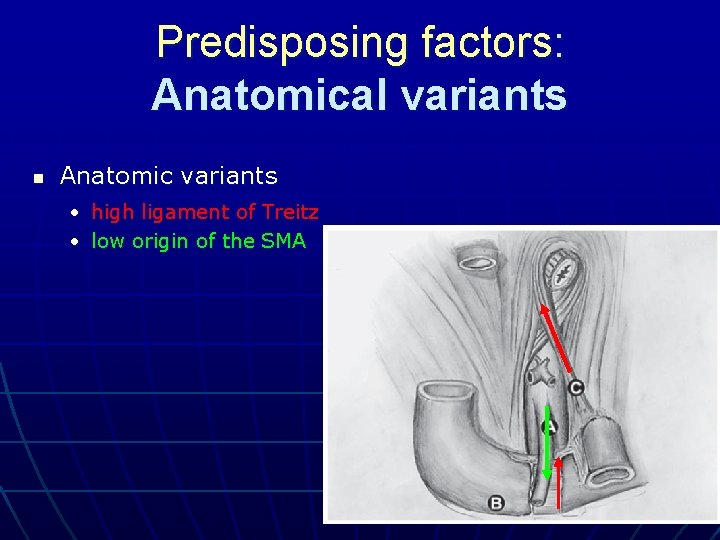
Predisposing factors: Anatomical variants n Anatomic variants • high ligament of Treitz • low origin of the SMA

Symptoms n n Nausea and vomiting Intermittent or post-prandial epigastric pain • relieved by a. VICIOUS prone or knee-chest (open up the aortomesenteric angle) CYCLE n Esophageal reflux n Anorexia n Weight loss

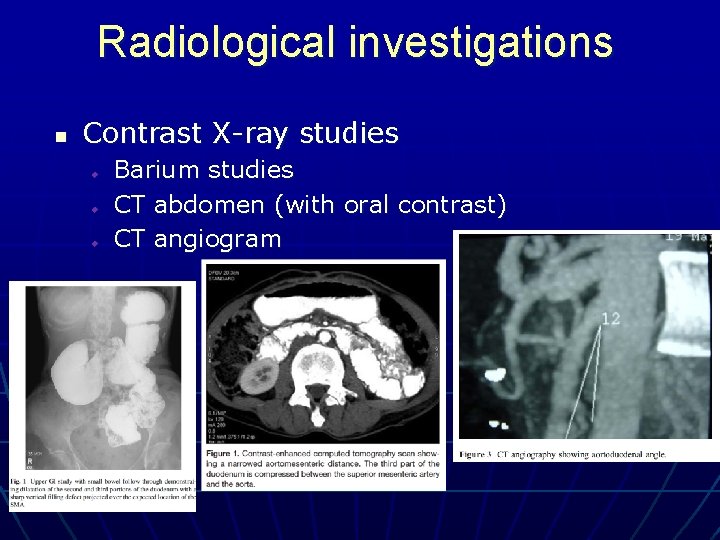
Diagnosis n High index of suspicion n Symptoms n Radiological evidence of D 3 compression by SMA • • • Aorto-mesenteric angle <22º (normal 38 -65º) Aorto-mesenteric distance <8 mm (normal 10 -28 mm) Proximal duodenal dilation with cut-off at D 3
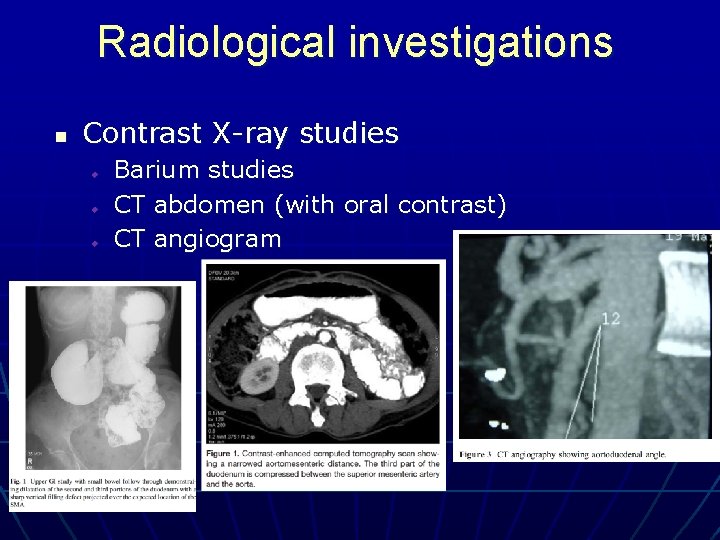
Radiological investigations n Contrast X-ray studies u u u Barium studies CT abdomen (with oral contrast) CT angiogram
Treatment n Conservative management n n In the absence of displacement by an abdominal mass, an aneurysm or another pathologic condition that requires immediate surgical exploration Surgical management n If conservative management fails
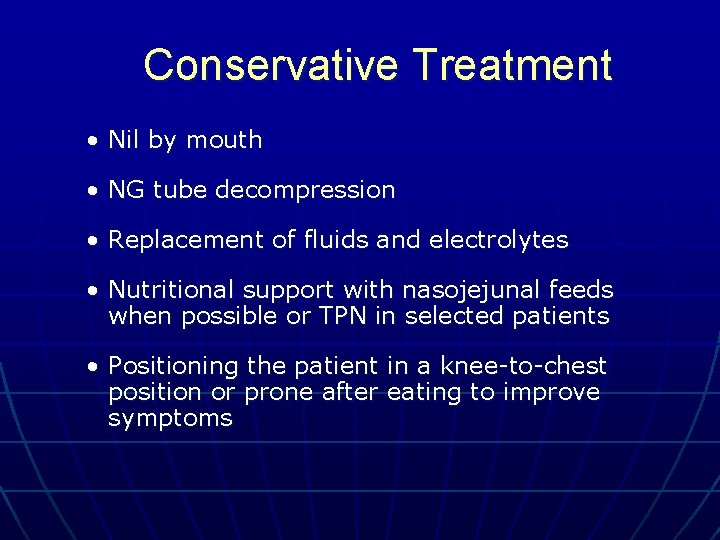
Conservative Treatment • Nil by mouth • NG tube decompression • Replacement of fluids and electrolytes • Nutritional support with nasojejunal feeds when possible or TPN in selected patients • Positioning the patient in a knee-to-chest position or prone after eating to improve symptoms
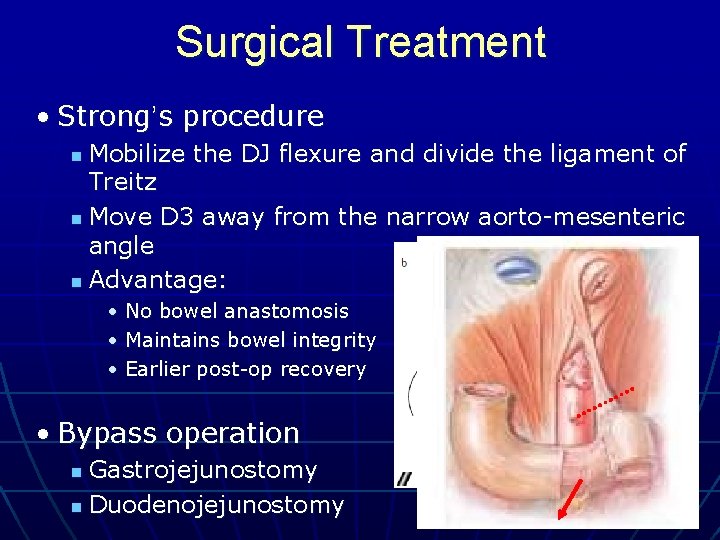
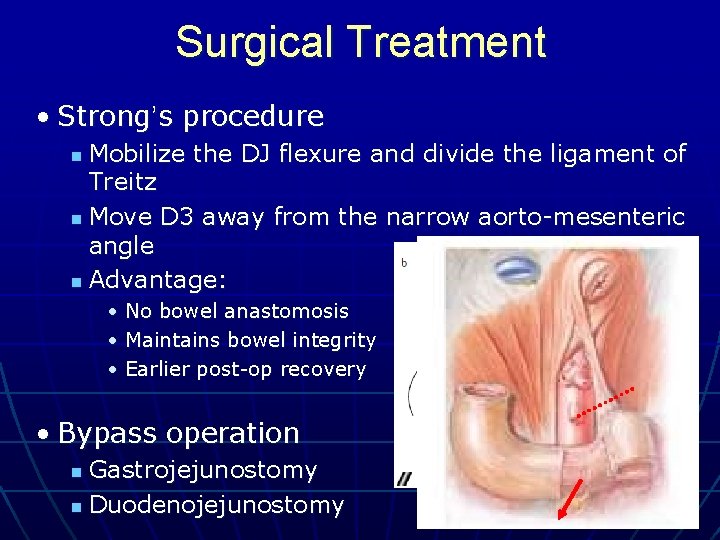
Surgical Treatment • Strong’s procedure Mobilize the DJ flexure and divide the ligament of Treitz n Move D 3 away from the narrow aorto-mesenteric angle n Advantage: n • No bowel anastomosis • Maintains bowel integrity • Earlier post-op recovery • Bypass operation Gastrojejunostomy n Duodenojejunostomy n
Which is better ?
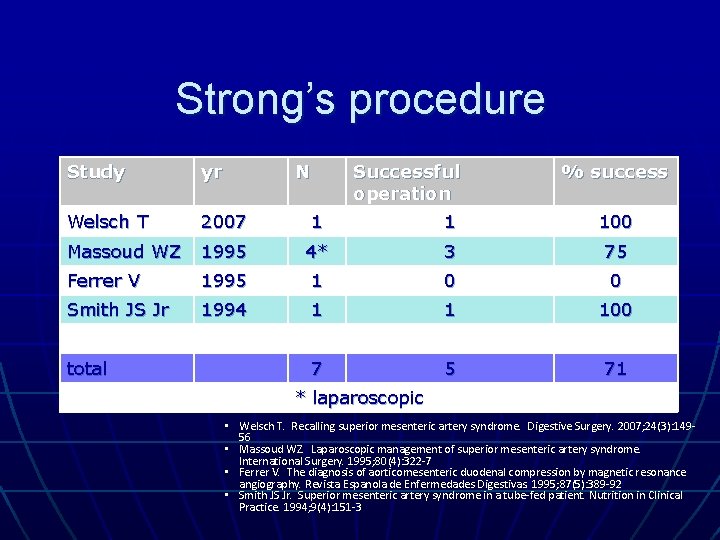
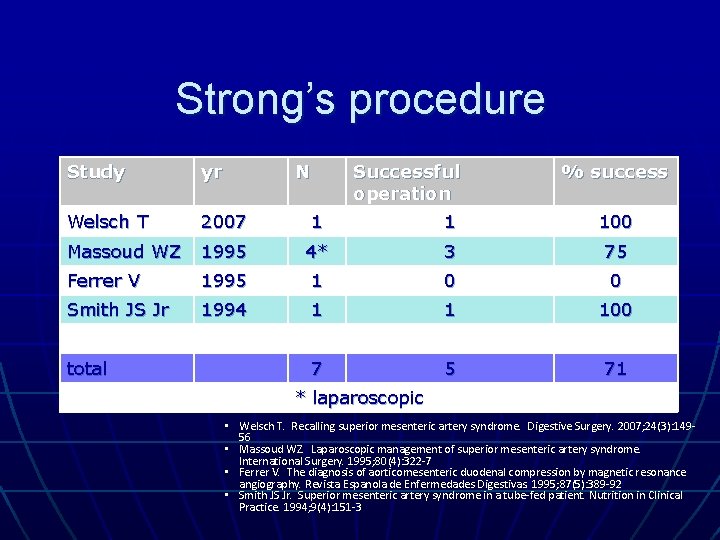
Strong’s procedure Study yr Welsch T 2007 1 1 100 Massoud WZ 1995 4* 3 75 Ferrer V 1995 1 0 0 Smith JS Jr 1994 1 1 100 7 5 71 total N Successful operation % success * laparoscopic • Welsch T. Recalling superior mesenteric artery syndrome. Digestive Surgery. 2007; 24(3): 14956 • Massoud WZ. Laparoscopic management of superior mesenteric artery syndrome. International Surgery. 1995; 80(4): 322 -7 • Ferrer V. The diagnosis of aorticomesenteric duodenal compression by magnetic resonance angiography. Revista Espanola de Enfermedades Digestivas. 1995; 87(5): 389 -92 • Smith JS Jr. Superior mesenteric artery syndrome in a tube-fed patient. Nutrition in Clinical Practice. 1994; 9(4): 151 -3

Gastrojejunostomy Study yr Clapp B 2010 3* 0 0 Yang WL 2008 1 0 0 Pan CH 2007 1 1 100 Tatar G 1996 1 1 100 Octavio de Toledo JM 1993 1 1 100 7 3 43 Total N Successful operation % success * Laparoscopic Roux-en-Y GJ n n n Clapp B. Superior mesenteric artery syndrome after Roux-en-Y gastric bypass. Journal of the Society of Laparoendoscopic Surgeons. 2010; 14(1): 143 -6 Yang WL. Assessment of duodenal circular drainage in treatment of superior mesenteric artery syndrome. World Journal of Gastroenterology. 2008; 14(2): 303 -6 Pan CH. Superior mesenteric artery syndrome complicating staged corrective surgery for scoliosis. Journal of the Formosan Medical Association. 2007; 106(2 Supp): S 37 -45 Tatar G. Superior mesenteric artery syndrome. A case report. Turkish Journal of Pediatrics. 1996; 38(3): 367 -70 Octavio de Toledo JM. Vascular compression of the duodenum related to a plaster cast (the cast syndrome). Revista Espanola de Enfermedades Digestivas. 1993; 83(1): 38 -41
Duodenojejunostomy
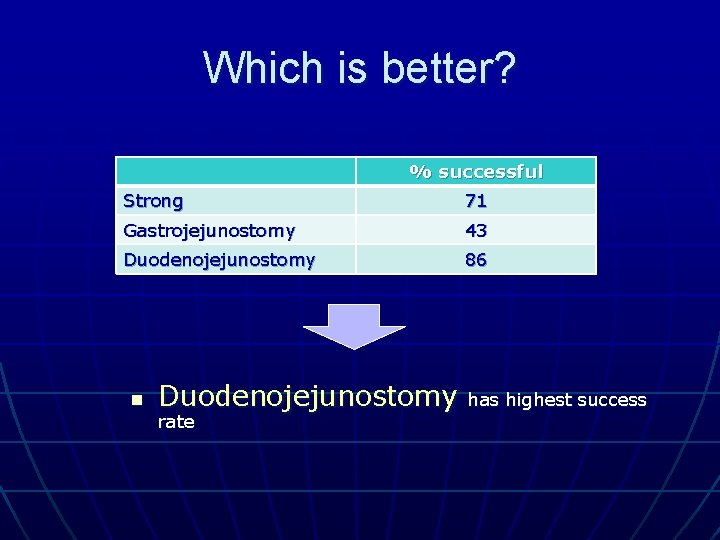
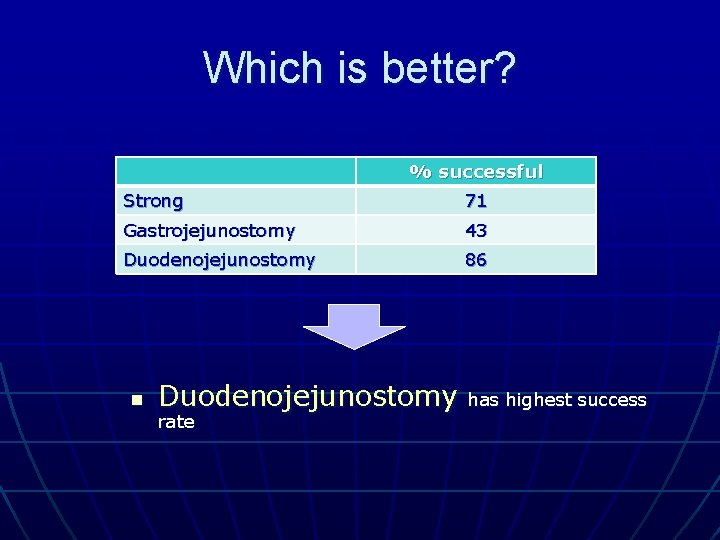
Which is better? % successful Strong 71 Gastrojejunostomy 43 Duodenojejunostomy 86 n Duodenojejunostomy rate has highest success
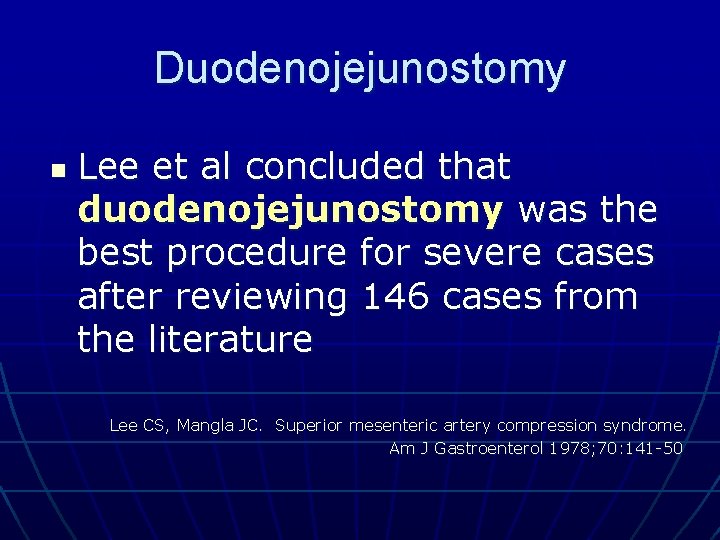
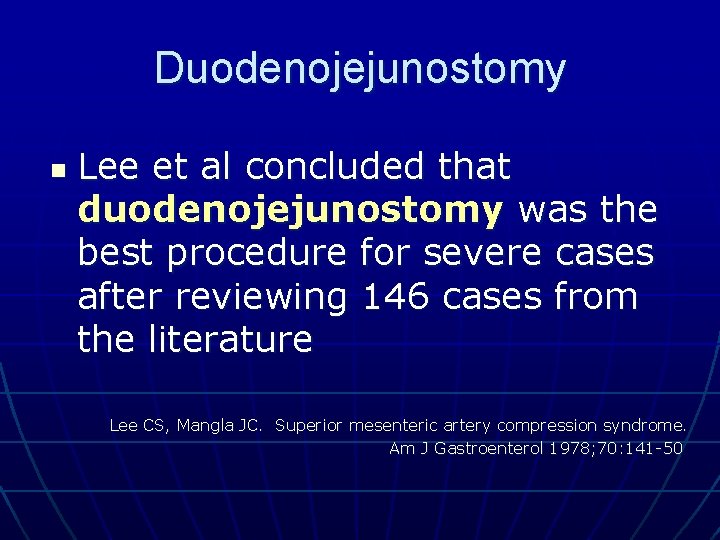
Duodenojejunostomy n Lee et al concluded that duodenojejunostomy was the best procedure for severe cases after reviewing 146 cases from the literature Lee CS, Mangla JC. Superior mesenteric artery compression syndrome. Am J Gastroenterol 1978; 70: 141 -50
Bring Home message n n SMA syndrome is a rare condition Diagnosis requires a high index of suspicion No large scale study comparing the treatment modalities Duodenojejunostomy appears to be superior to gastrojejunostomy or Strong’s operation

Thank you

Strong’s procedure - Reference n n Welsch T. Recalling superior mesenteric artery syndrome. Digestive Surgery. 2007; 24(3): 14956 Massoud WZ. Laparoscopic management of superior mesenteric artery syndrome. International Surgery. 1995; 80(4): 322 -7 Ferrer V. The diagnosis of aorticomesenteric duodenal compression by magnetic resonance angiography. Revista Espanola de Enfermedades Digestivas. 1995; 87(5): 389 -92 Smith JS Jr. Superior mesenteric artery syndrome in a tube-fed patient. Nutrition in Clinical Practice. 1994; 9(4): 151 -3
Gastrojejunostomy - Reference n n n Clapp B. Superior mesenteric artery syndrome after Roux-en-Y gastric bypass. Journal of the Society of Laparoendoscopic Surgeons. 2010; 14(1): 143 -6 Yang WL. Assessment of duodenal circular drainage in treatment of superior mesenteric artery syndrome. World Journal of Gastroenterology. 2008; 14(2): 303 -6 Pan CH. Superior mesenteric artery syndrome complicating staged corrective surgery for scoliosis. Journal of the Formosan Medical Association. 2007; 106(2 Supp): S 37 -45 Tatar G. Superior mesenteric artery syndrome. A case report. Turkish Journal of Pediatrics. 1996; 38(3): 367 -70 Octavio de Toledo JM. Vascular compression of the duodenum related to a plaster cast (the cast syndrome). Revista Espanola de Enfermedades Digestivas. 1993; 83(1): 38 -41
End of Reference