The Management of Common MSDs in the Workplace




- Slides: 45
The Management of Common MSD’s in the Workplace Musculoskeletal Health in the Workplace Conference 14 th November 2018 Presented by Harry Miller

Who are we? Crystal Palace Physio Group Occupational Health: On-site Physiotherapy services Remote Case Management Network Physiotherapy Ergonomic Assessments Office Walk-Throughs Wellbeing events
About me… Corporate Services Operations Manager Account Manager for Barts OH Physiotherapy service Clinical Background in OH Sedentary/Manual Workers Ergonomic Assessment Functional Capacity Evaluation
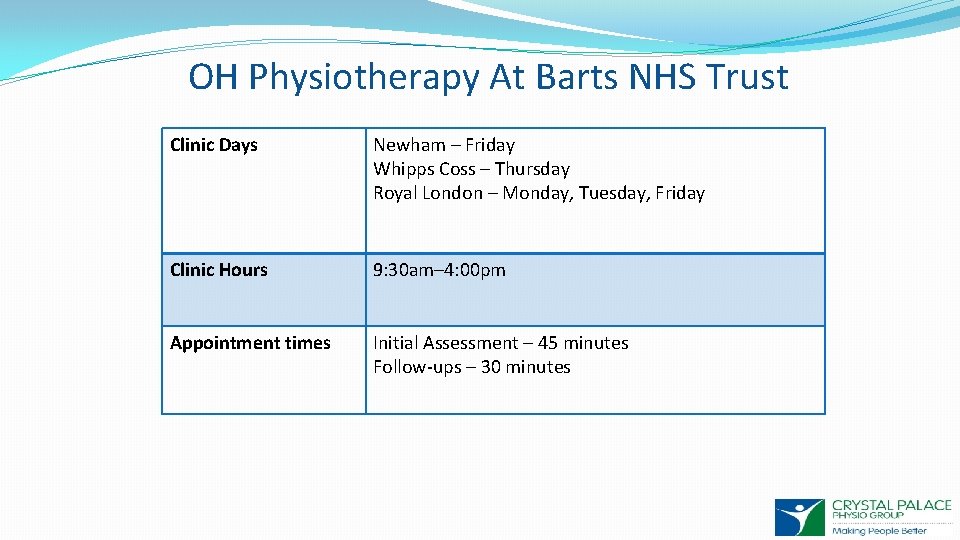
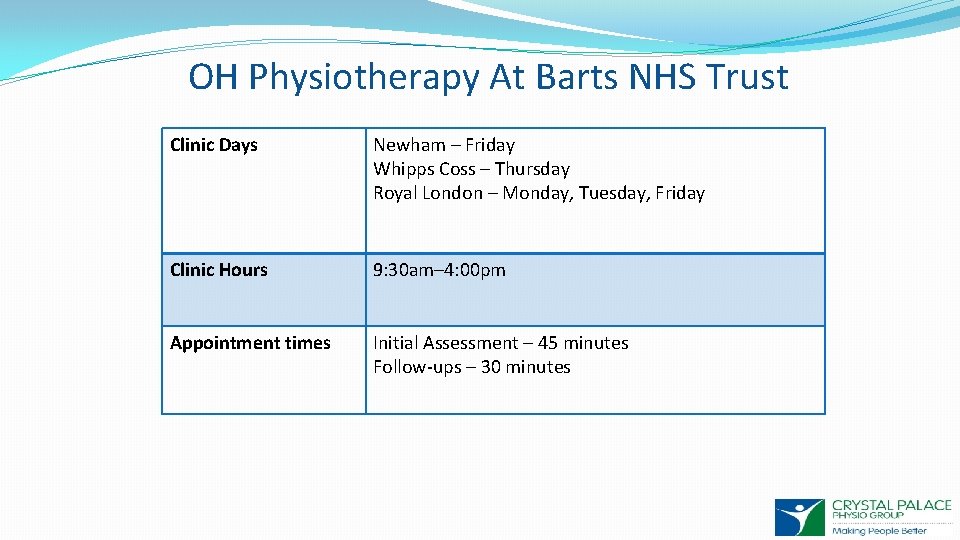
OH Physiotherapy At Barts NHS Trust Clinic Days Newham – Friday Whipps Coss – Thursday Royal London – Monday, Tuesday, Friday Clinic Hours 9: 30 am– 4: 00 pm Appointment times Initial Assessment – 45 minutes Follow-ups – 30 minutes
OH Physiotherapy at Barts Since Dec 2016 Primarily an advisory service Management Referrals consisting of: Job Task Analysis Functional Assessment Assessing Fitness for Work Return to Work Planning On-going Rehabilitation
Criteria For OH Physiotherapy at Barts NHS Trust An injury/condition which was sustained at work or outside of work A injury/condition which is impacting on the employees working capacity Unable to fulfill full duties or is currently on restricted duties due to their symptoms Prolonged sickness absence/multiple bouts of sickness due to musculoskeletal condition Currently not receiving treatment from the NHS or awaiting further intervention/investigation
Referral Process Referral form Submitted by Line Manager Appointment booked by Barts OH team Physiotherapist undertakes Assessment Management report sent back to Line Manager
What is Physiotherapy? “Physiotherapists help people affected by injury, illness or disability through movement and exercise, manual therapy, education and advice. They help patients manage pain and prevent disease. ” – Chartered Society of Physiotherapy What tools are employed by Physiotherapists as part of their treatment to achieve these aims? � Education � Manual therapy � Complementary therapies � Postural Advice � Strengthening/Stretching exercises � Balance/Proprioceptive exercises � Functional Rehabilitation
What is Occupational Health Physiotherapy? OH Physiotherapy is principally concerned with the prevention and management of work-related musculoskeletal disorders. � Aim of retention at work and the limitation of chronicity � Multi-disciplinary team working � Bio-psychosocial approach Aims: � Rehabilitation � Self management � Early return to work; Return to work planning. � Raise awareness of MSK risk factors within the workplace
The Role Of The OH Physiotherapist “Improve the safety, function and performance of the working population. We aim to treat the main condition affecting the employee, improving their ability to work and reducing their sickness absence. It is believed this will help improve productivity and performance of the employee and the workplace as a whole. ” CSP ( 2013); Association of Chartered Physiotherapists in Occupational Health and Ergonomics (2013) This may be achieved by implementing the following: � Structured rehabilitation programmes. � Work place recommendations or Temporary work place restrictions. � Promoting effective self management. � Return to work planning after prolonged sickness absence. � Functional restoration programmes.
Aims of the Service • To provide an accessible service to any employees with a musculoskeletal condition affecting them at work. • To provide the quickest possible access to the service. Triaging the referrals helps to ensure those in greatest need are seen at the earliest possible time. • To focus on self-management of conditions and provide advice on prevention of further injury. • To provide practical work place recommendations to Managers to help them support their staff to remain at work or to return to work after a period of sickness absence
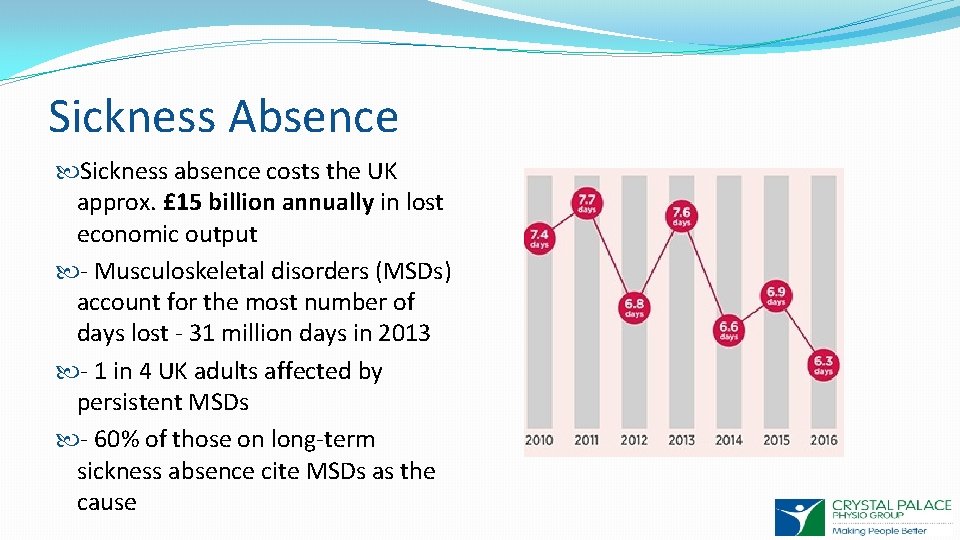
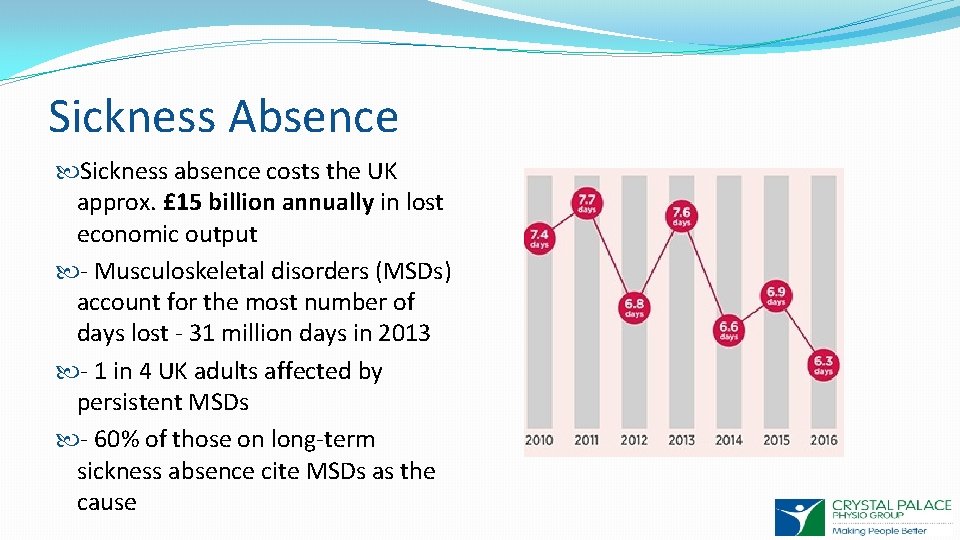
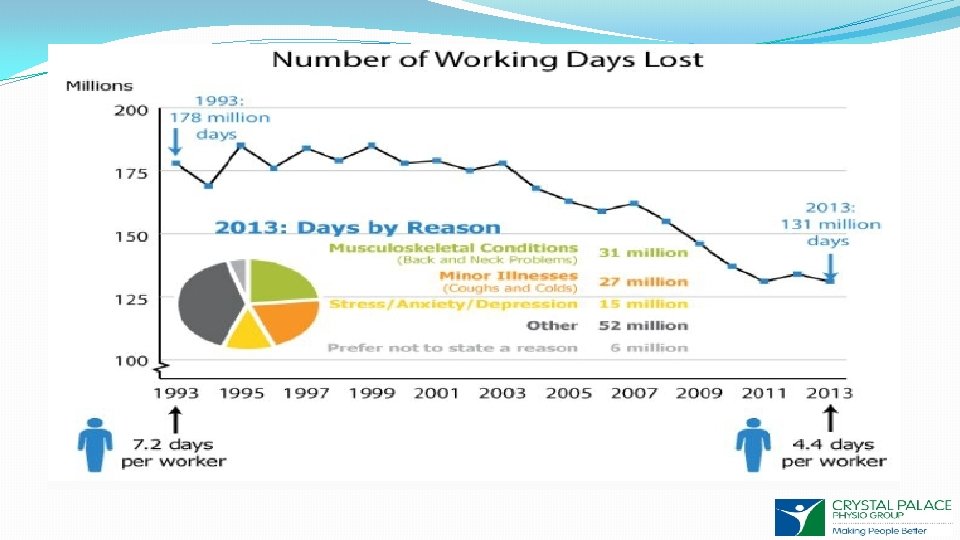
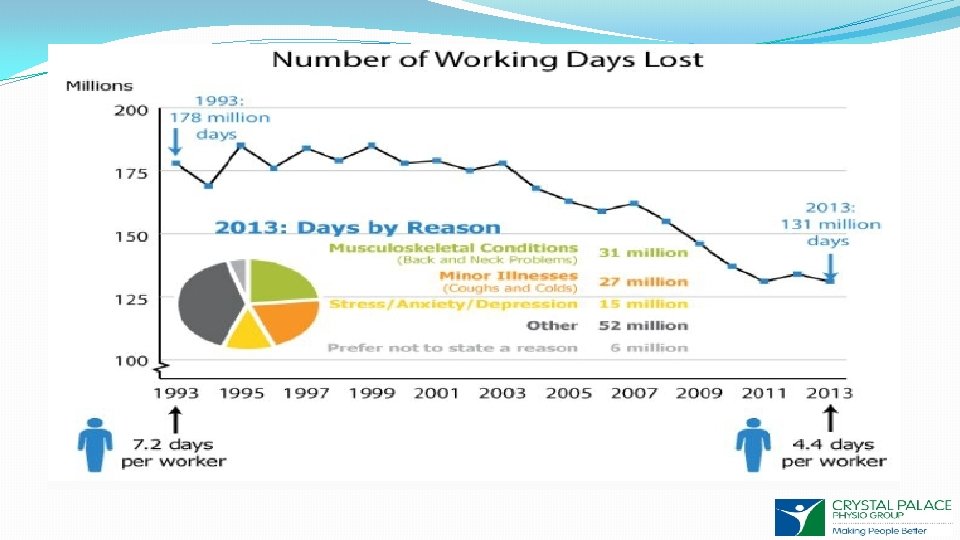
Sickness Absence Sickness absence costs the UK approx. £ 15 billion annually in lost economic output - Musculoskeletal disorders (MSDs) account for the most number of days lost - 31 million days in 2013 - 1 in 4 UK adults affected by persistent MSDs - 60% of those on long-term sickness absence cite MSDs as the cause
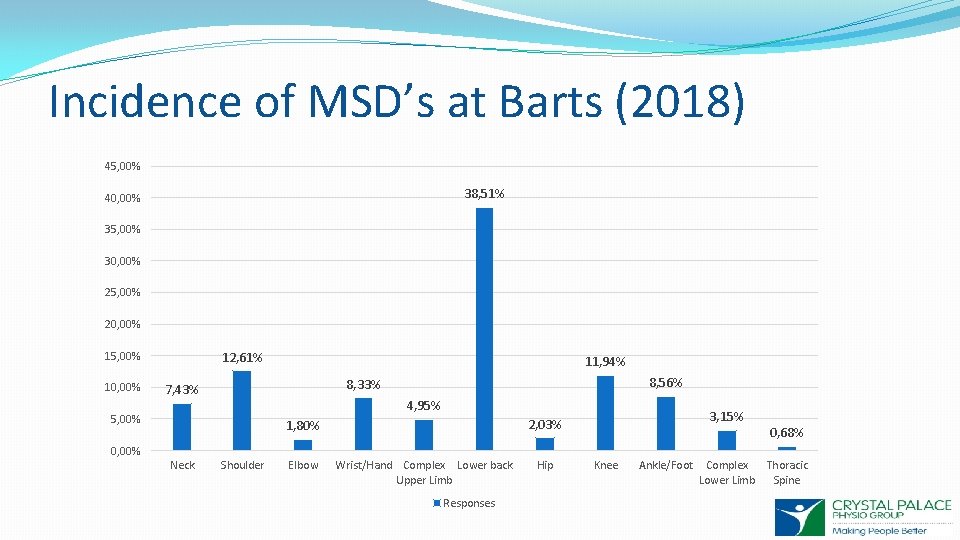
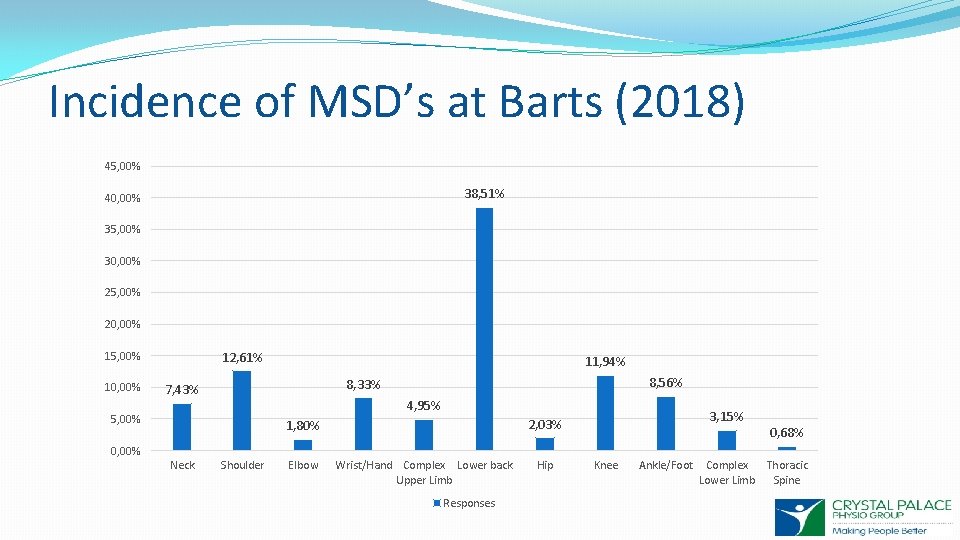
Incidence of MSD’s at Barts (2018) 45, 00% 38, 51% 40, 00% 35, 00% 30, 00% 25, 00% 20, 00% 12, 61% 15, 00% 10, 00% 11, 94% 8, 56% 8, 33% 7, 43% 4, 95% 5, 00% 3, 15% 2, 03% 1, 80% 0, 68% 0, 00% Neck Shoulder Elbow Wrist/Hand Complex Lower back Upper Limb Responses Hip Knee Ankle/Foot Complex Thoracic Lower Limb Spine
Newsflash: Back Pain is common
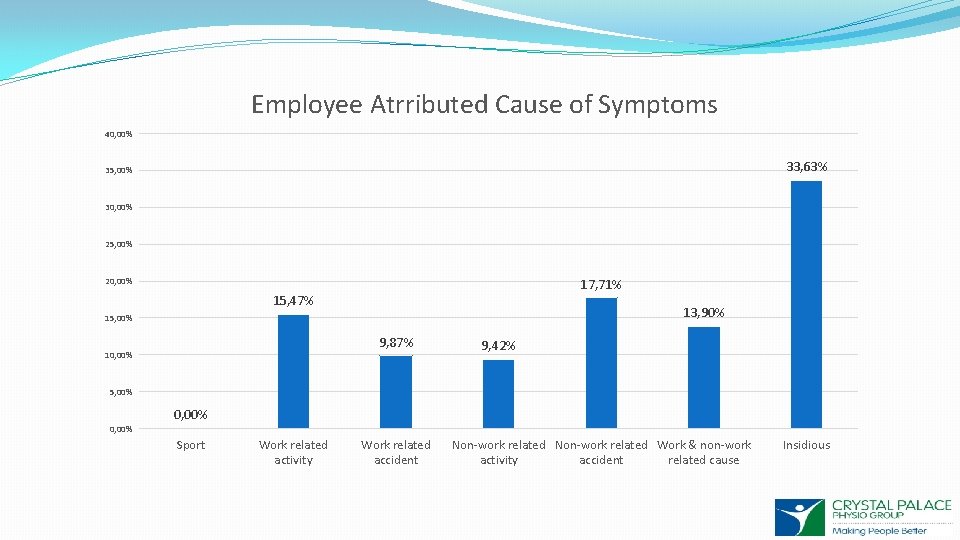
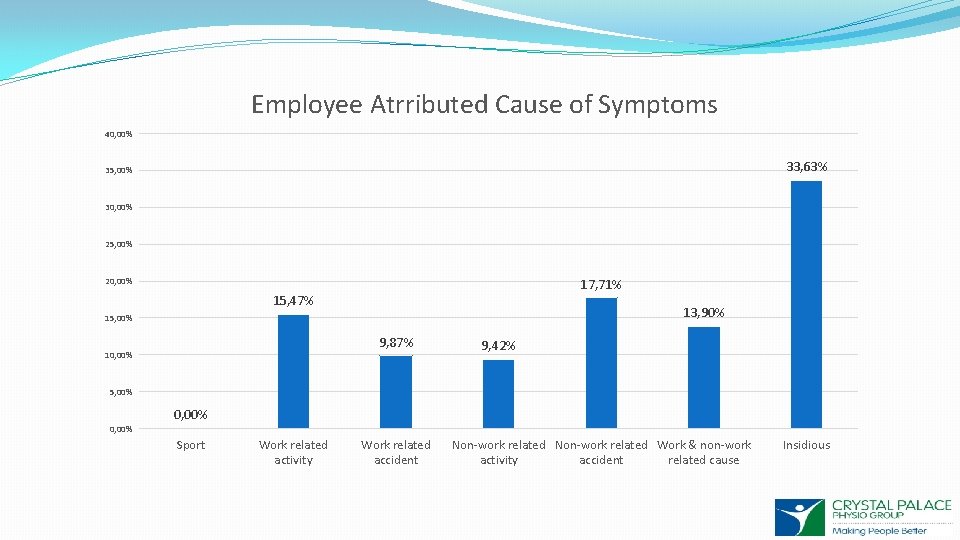
Employee Atrributed Cause of Symptoms 40, 00% 33, 63% 35, 00% 30, 00% 25, 00% 17, 71% 20, 00% 15, 47% 13, 90% 15, 00% 9, 87% 10, 00% 9, 42% 5, 00% 0, 00% Sport Work related activity Work related accident Non-work related Work & non-work activity accident related cause Insidious
HSE’s ‘Improved early pain management for musculoskeletal disorders’ “Latest evidence and current thinking supports the use of biopsychosocial assessment and intervention in close proximity to work for improved early management of musculoskeletal disorders. The employer and employee have the main roles in this and musculoskeletal practitioners are the most accessible qualified health professionals to support them. ”
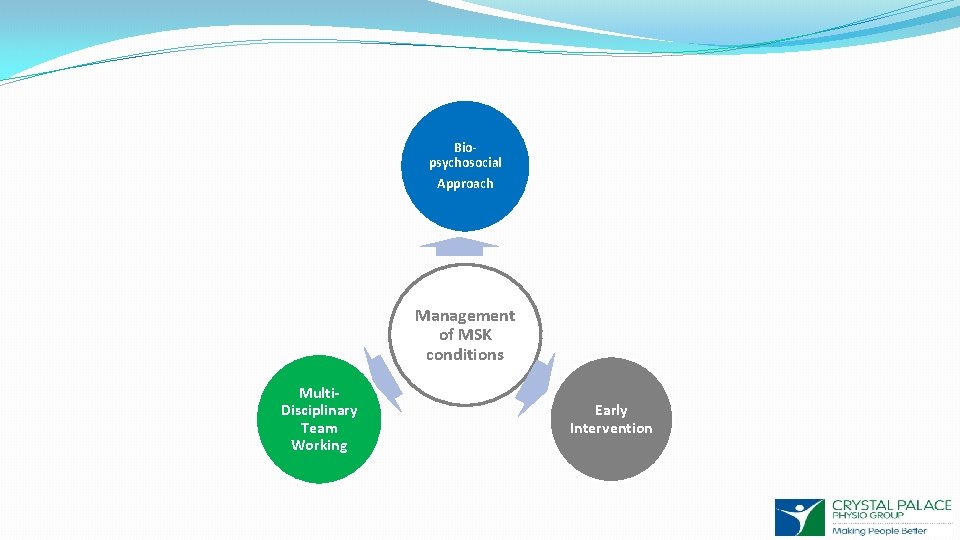
Biopsychosocial Approach Management of MSK conditions Multi. Disciplinary Team Working Early Intervention
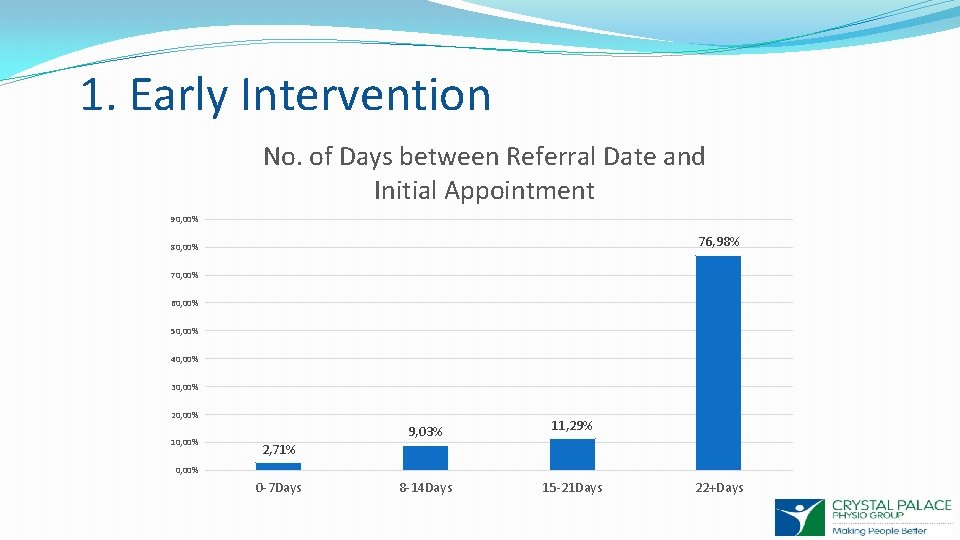
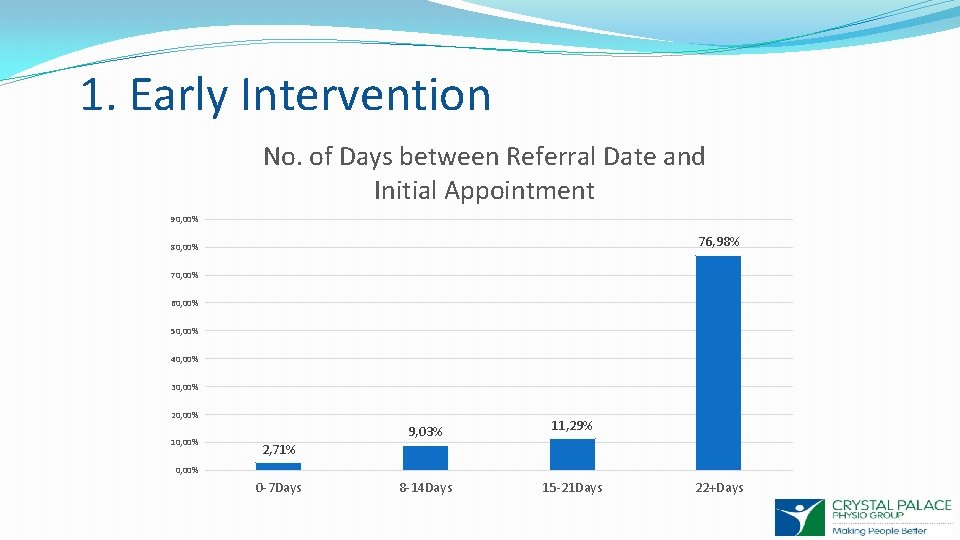
1. Early Intervention No. of Days between Referral Date and Initial Appointment 90, 00% 76, 98% 80, 00% 70, 00% 60, 00% 50, 00% 40, 00% 30, 00% 20, 00% 10, 00% 9, 03% 11, 29% 8 -14 Days 15 -21 Days 2, 71% 0, 00% 0 -7 Days 22+Days
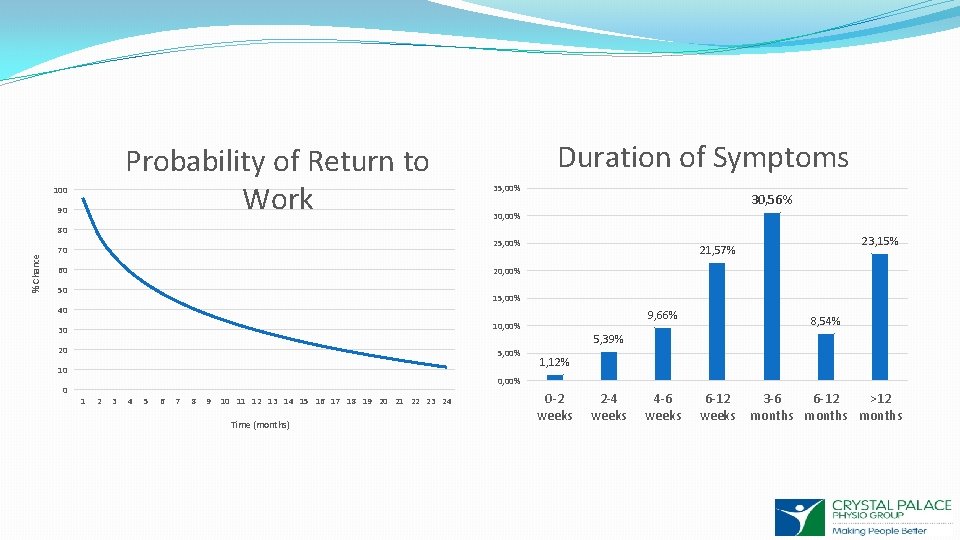
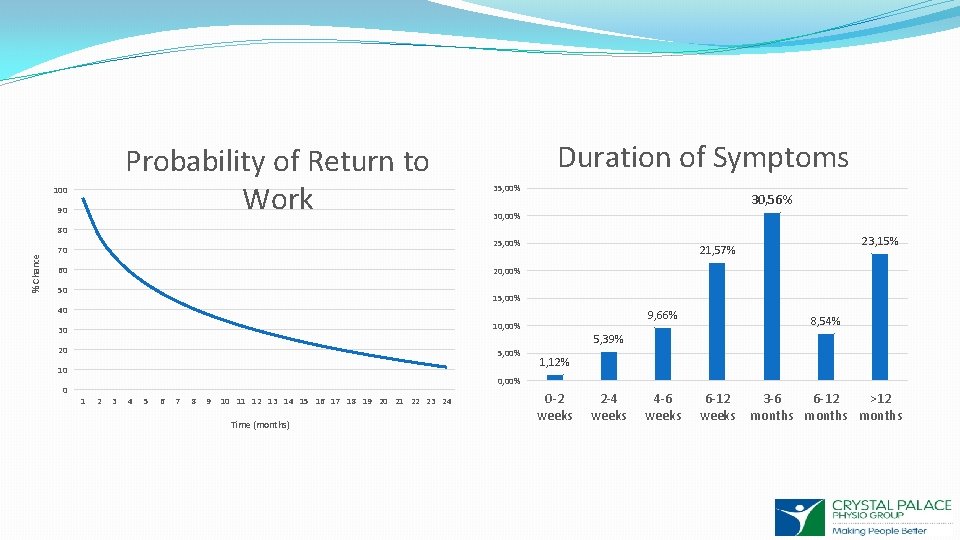
Probability of Return to Work 100 90 Duration of Symptoms 35, 00% 30, 56% 30, 00% % Chance 80 25, 00% 70 60 20, 00% 50 15, 00% 40 30 10, 00% 20 5, 00% 10 0 23, 15% 21, 57% 9, 66% 8, 54% 5, 39% 1, 12% 0, 00% 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Time (months) 0 -2 weeks 2 -4 weeks 4 -6 weeks 6 -12 weeks 3 -6 6 -12 >12 months
“At 6 weeks physiotherapy intervention is more effective than advice on staying active, leading to more rapid improvement in function, mood, quality of life and general health. The timing of intervention affects the progression of psychosocial features. If treatment is provided later, the same psychosocial benefits are not achieved. “ Early intervention for the management of acute low back pain: A single blind randomised controlled trial of biopsychosocial education, manual therapy and exercise (Wand et al, 2004)
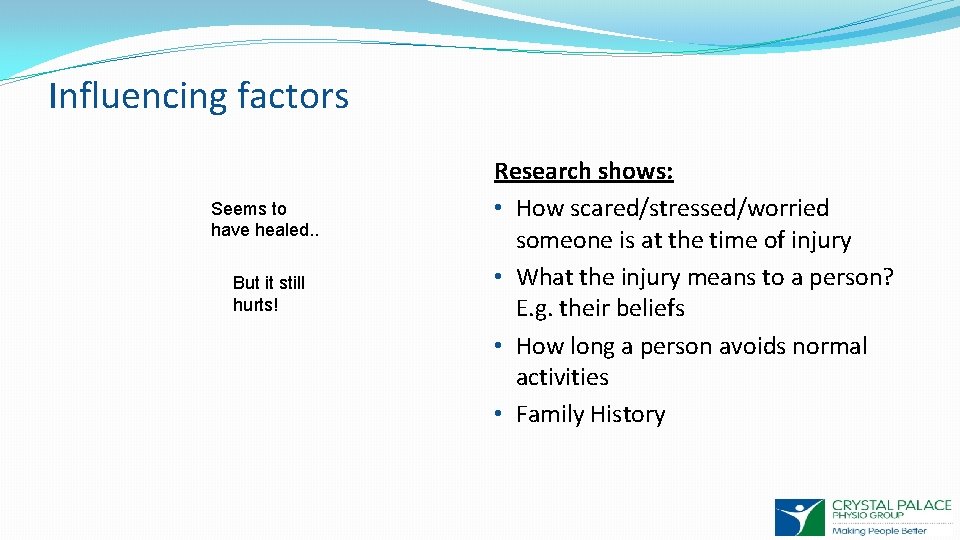
Influencing factors Seems to have healed. . But it still hurts! Research shows: • How scared/stressed/worried someone is at the time of injury • What the injury means to a person? E. g. their beliefs • How long a person avoids normal activities • Family History
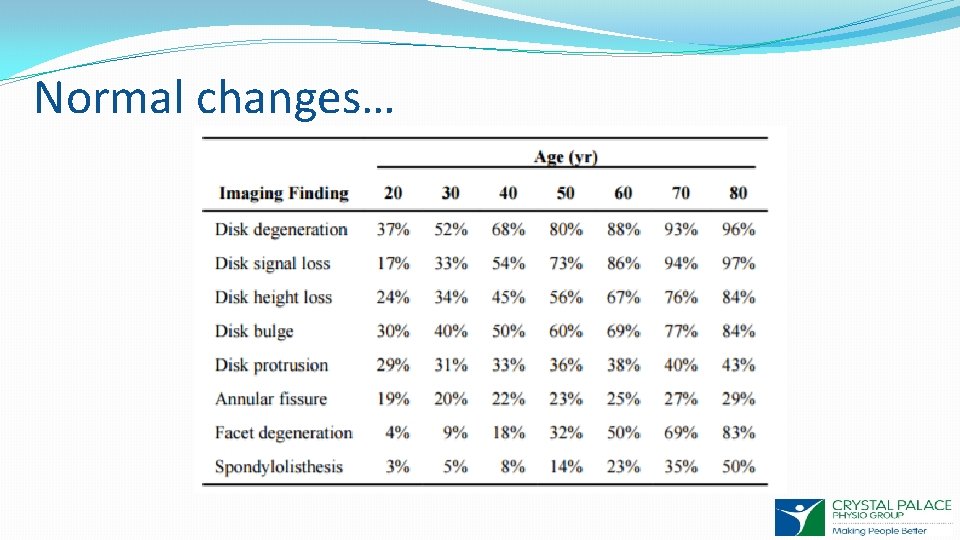
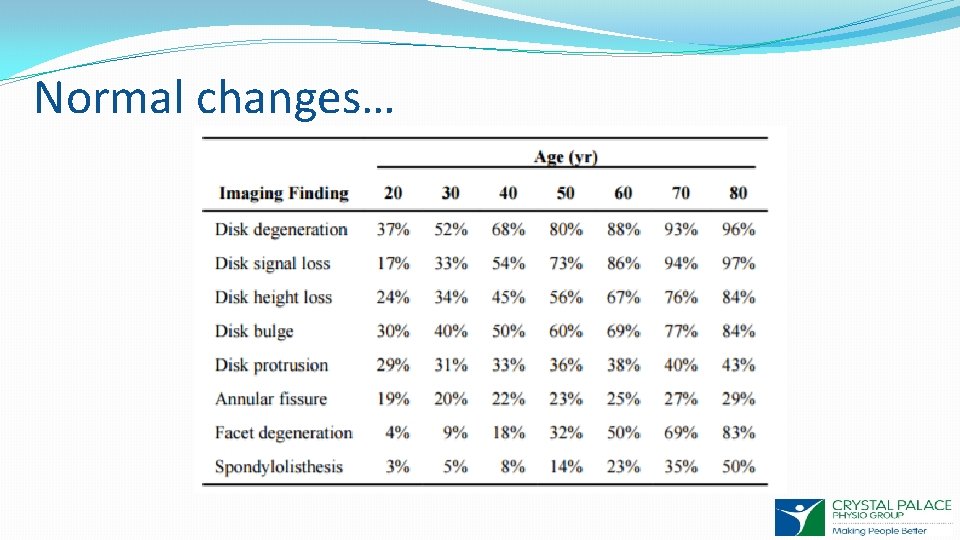
Normal changes…
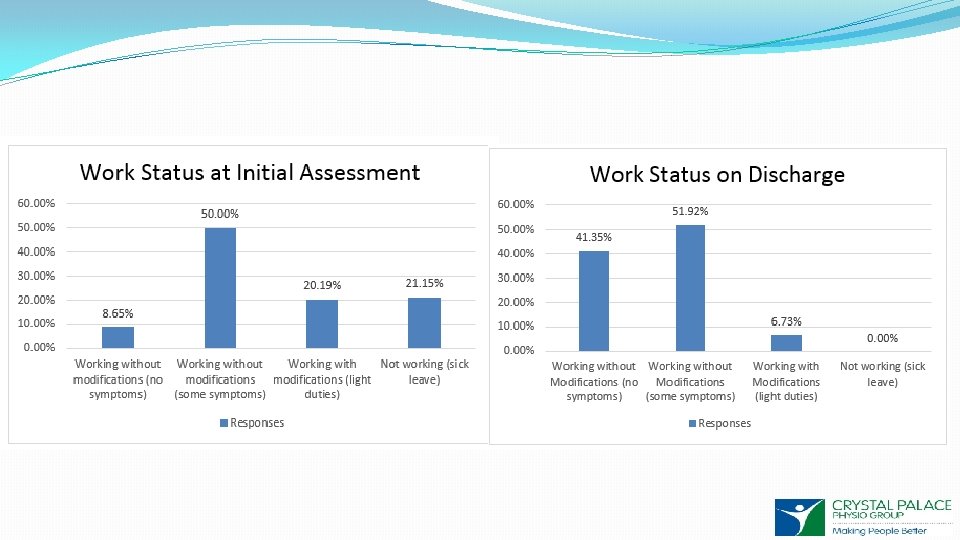
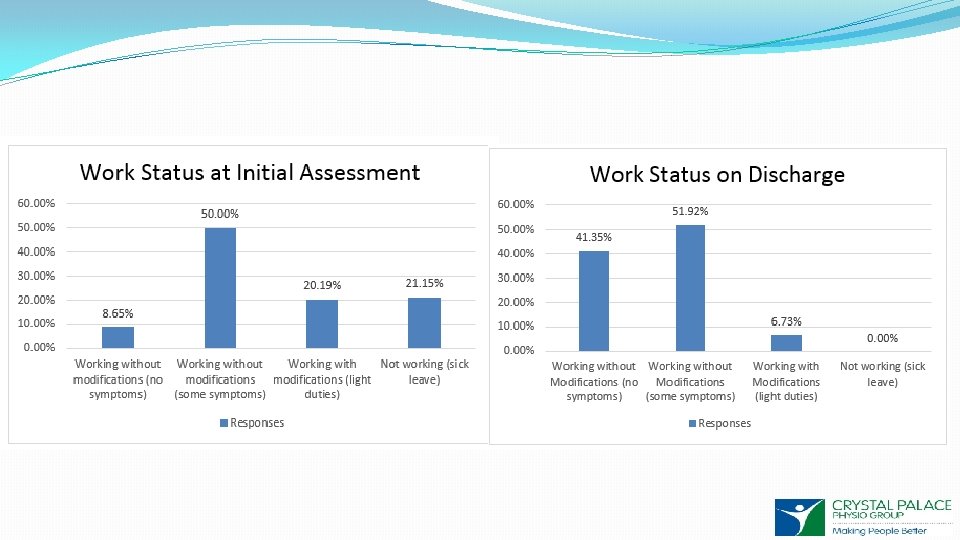
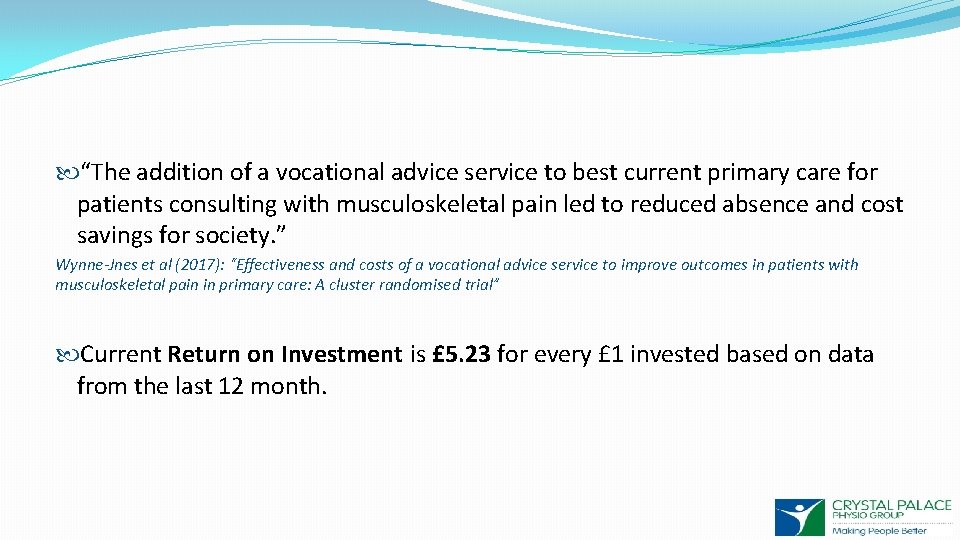
“The addition of a vocational advice service to best current primary care for patients consulting with musculoskeletal pain led to reduced absence and cost savings for society. ” Wynne-Jnes et al (2017): “Effectiveness and costs of a vocational advice service to improve outcomes in patients with musculoskeletal pain in primary care: A cluster randomised trial” Current Return on Investment is £ 5. 23 for every £ 1 invested based on data from the last 12 month.
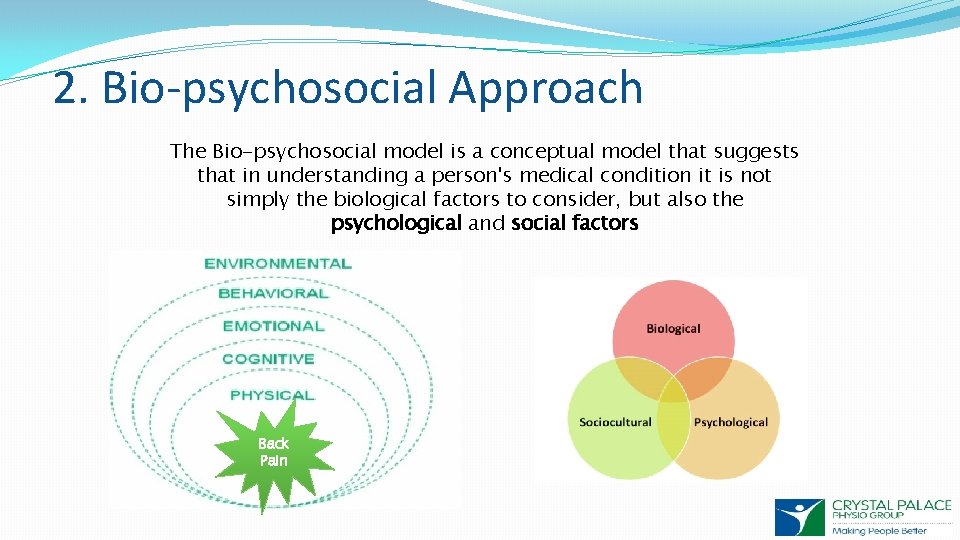
2. Bio-psychosocial Approach The Bio-psychosocial model is a conceptual model that suggests that in understanding a person's medical condition it is not simply the biological factors to consider, but also the psychological and social factors Back Pain
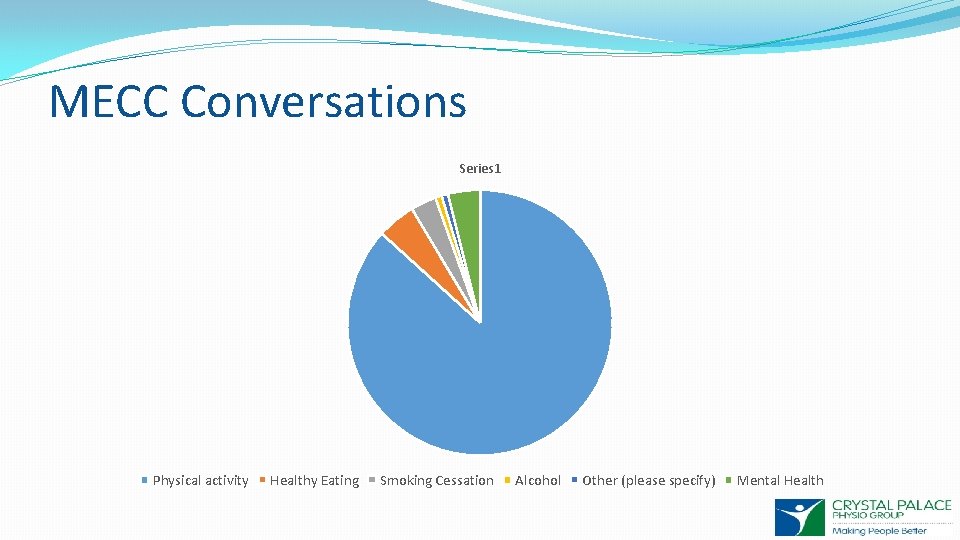
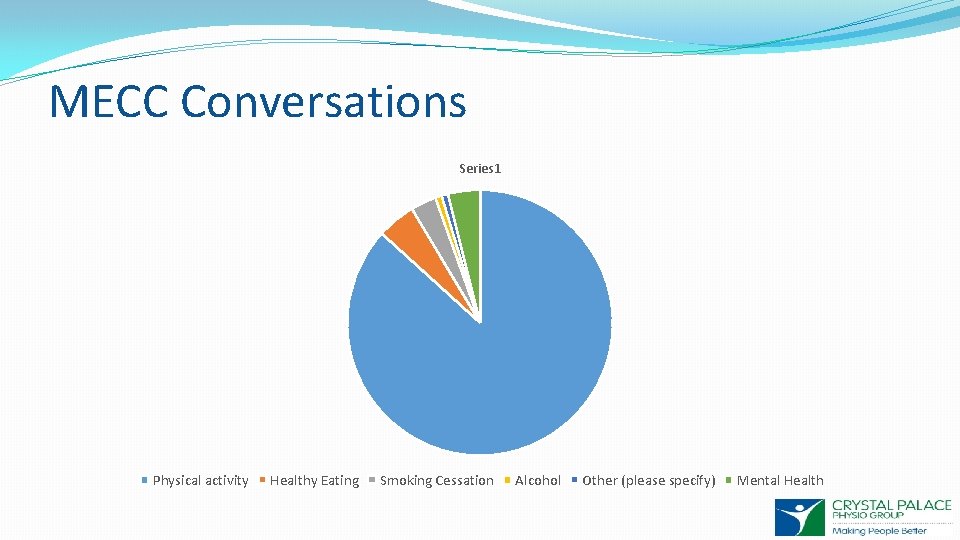
MECC Conversations Series 1 Physical activity Healthy Eating Smoking Cessation Alcohol Other (please specify) Mental Health

Empowering Self-Management Self-management has been described as a model of care whereby patients retain a primary role in management. � Integrated decision-making process � Goal Setting (functional) � Providing the tools to follow the plan � Educating people about pain and its associated behaviours � Pain-management strategies � Self-management strategies vs Passive treatments Emphasis on role and nature of healthcare provider input in a challenging economic context
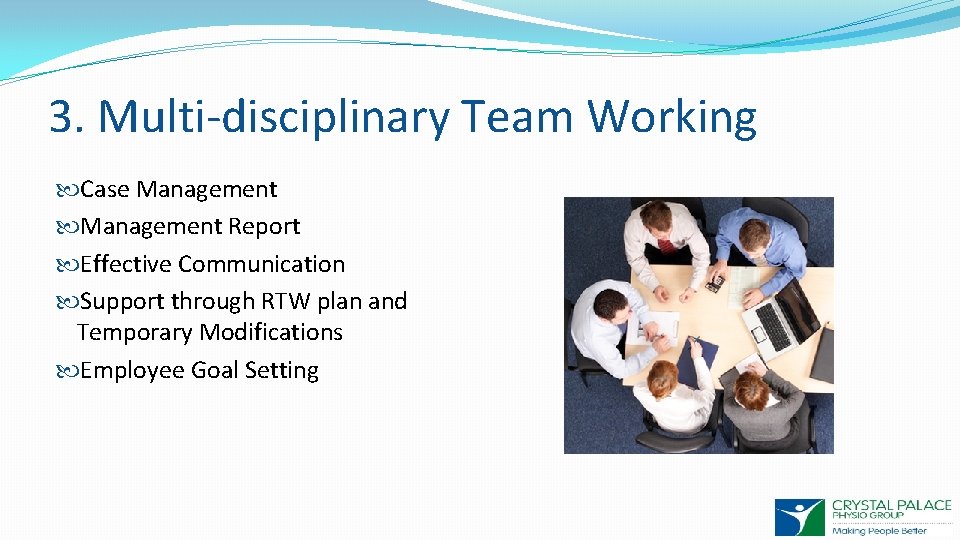
3. Multi-disciplinary Team Working Case Management Report Effective Communication Support through RTW plan and Temporary Modifications Employee Goal Setting
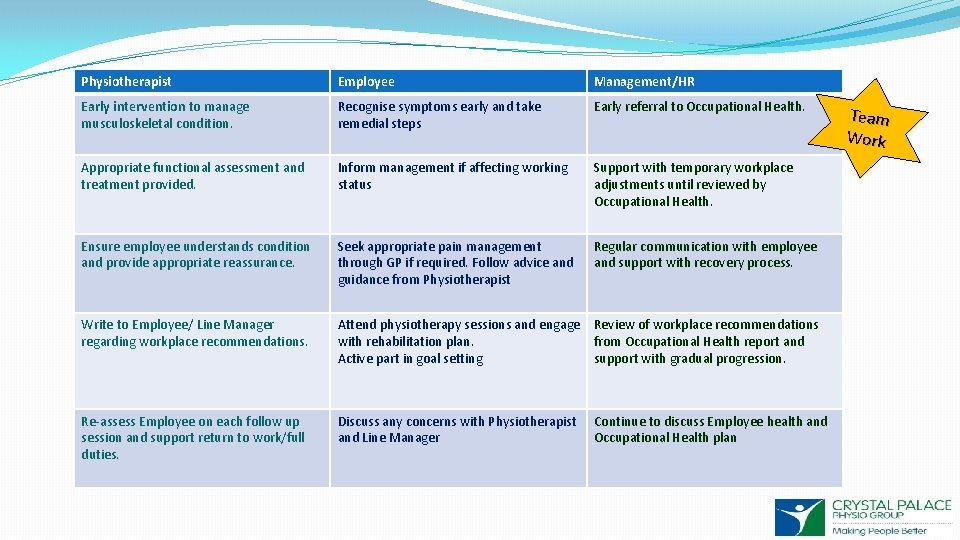
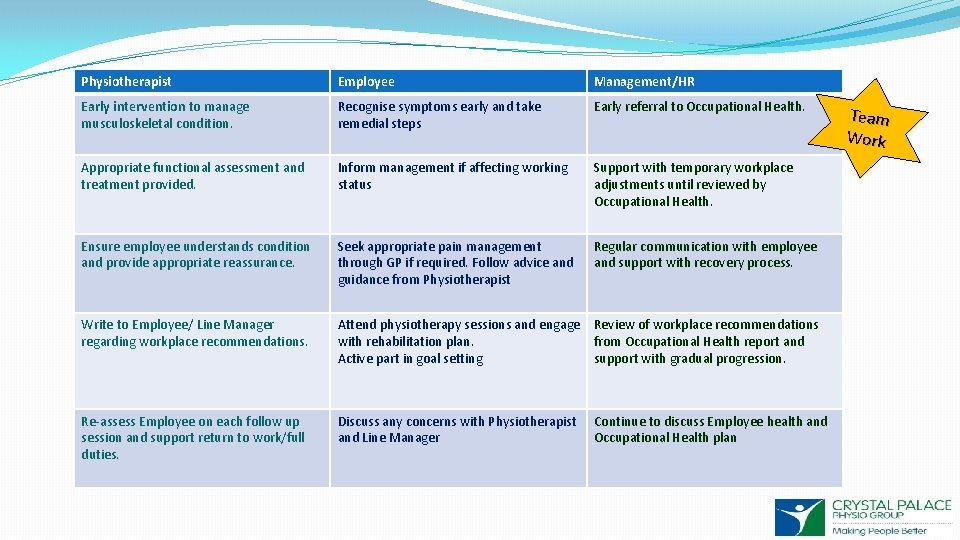
Physiotherapist Employee Management/HR Early intervention to manage musculoskeletal condition. Recognise symptoms early and take remedial steps Early referral to Occupational Health. Appropriate functional assessment and treatment provided. Inform management if affecting working status Support with temporary workplace adjustments until reviewed by Occupational Health. Ensure employee understands condition and provide appropriate reassurance. Seek appropriate pain management through GP if required. Follow advice and guidance from Physiotherapist Regular communication with employee and support with recovery process. Write to Employee/ Line Manager regarding workplace recommendations. Attend physiotherapy sessions and engage Review of workplace recommendations with rehabilitation plan. from Occupational Health report and Active part in goal setting support with gradual progression. Re-assess Employee on each follow up session and support return to work/full duties. Discuss any concerns with Physiotherapist and Line Manager Continue to discuss Employee health and Occupational Health plan Team Work
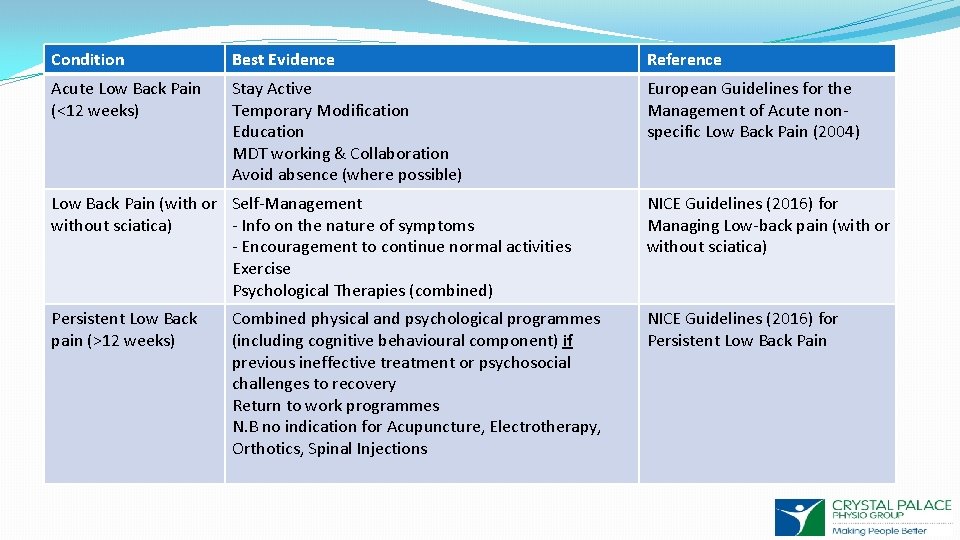
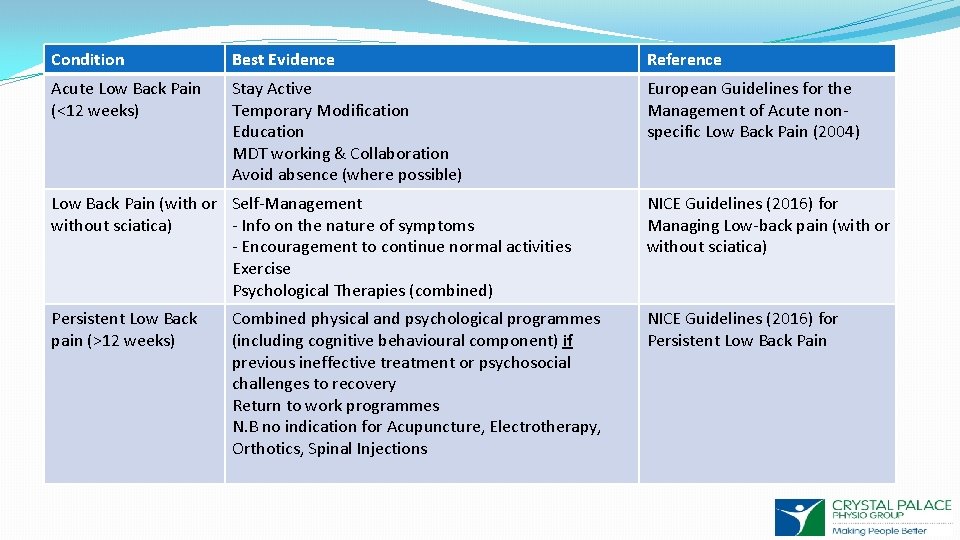
Condition Best Evidence Reference Acute Low Back Pain (<12 weeks) Stay Active Temporary Modification Education MDT working & Collaboration Avoid absence (where possible) European Guidelines for the Management of Acute nonspecific Low Back Pain (2004) Low Back Pain (with or Self-Management without sciatica) - Info on the nature of symptoms - Encouragement to continue normal activities Exercise Psychological Therapies (combined) NICE Guidelines (2016) for Managing Low-back pain (with or without sciatica) Persistent Low Back pain (>12 weeks) NICE Guidelines (2016) for Persistent Low Back Pain Combined physical and psychological programmes (including cognitive behavioural component) if previous ineffective treatment or psychosocial challenges to recovery Return to work programmes N. B no indication for Acupuncture, Electrotherapy, Orthotics, Spinal Injections
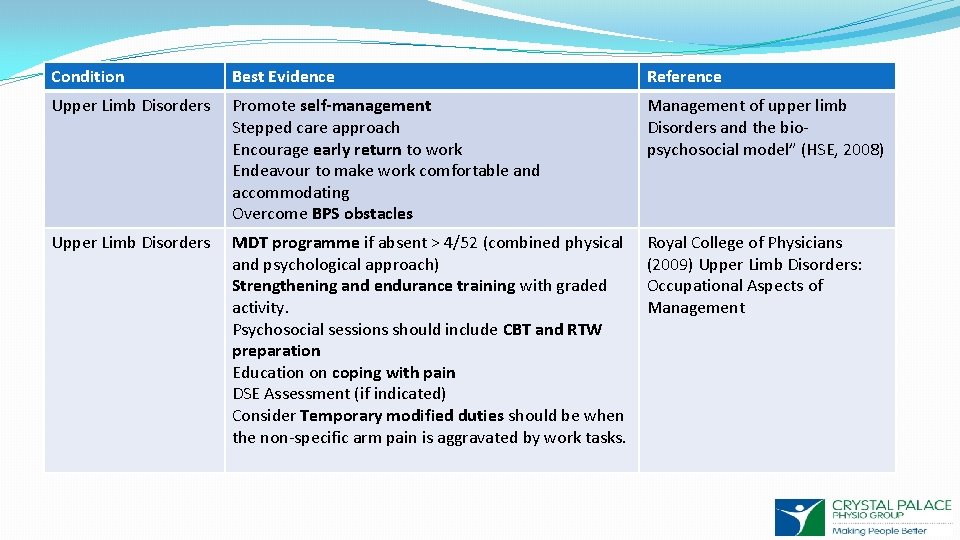
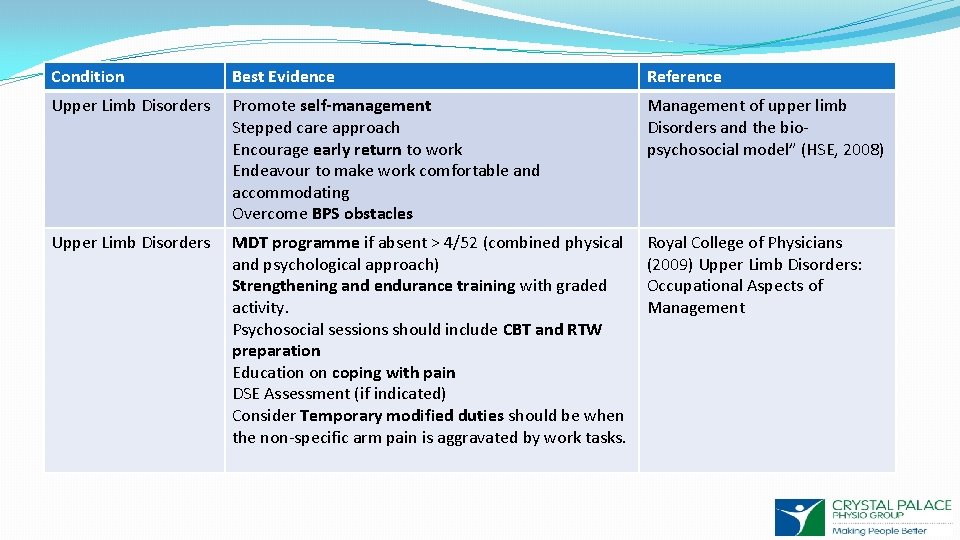
Condition Best Evidence Reference Upper Limb Disorders Promote self-management Stepped care approach Encourage early return to work Endeavour to make work comfortable and accommodating Overcome BPS obstacles Management of upper limb Disorders and the biopsychosocial model” (HSE, 2008) Upper Limb Disorders MDT programme if absent > 4/52 (combined physical and psychological approach) Strengthening and endurance training with graded activity. Psychosocial sessions should include CBT and RTW preparation Education on coping with pain DSE Assessment (if indicated) Consider Temporary modified duties should be when the non-specific arm pain is aggravated by work tasks. Royal College of Physicians (2009) Upper Limb Disorders: Occupational Aspects of Management
So what can we do? ? ?
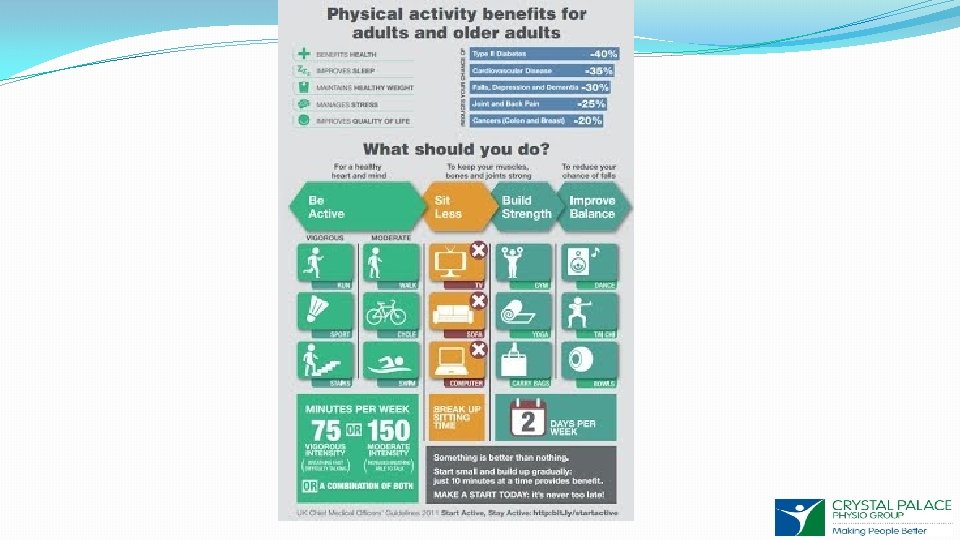
Physical Activity “If exercise could be packaged in a pill, it would be the single most widely prescribed and beneficial medicine in the nation. ” Robert Butler, National Institute on Aging


Healthy Eating https: //www. nhs. uk/oneyou/
…. and Mental Wellbeing
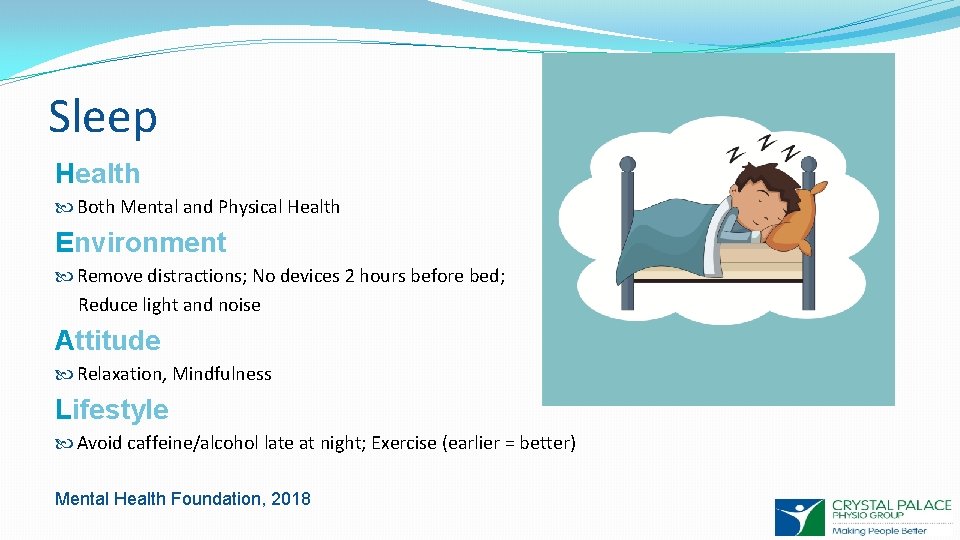
Sleep Health Both Mental and Physical Health Environment Remove distractions; No devices 2 hours before bed; Reduce light and noise Attitude Relaxation, Mindfulness Lifestyle Avoid caffeine/alcohol late at night; Exercise (earlier = better) Mental Health Foundation, 2018
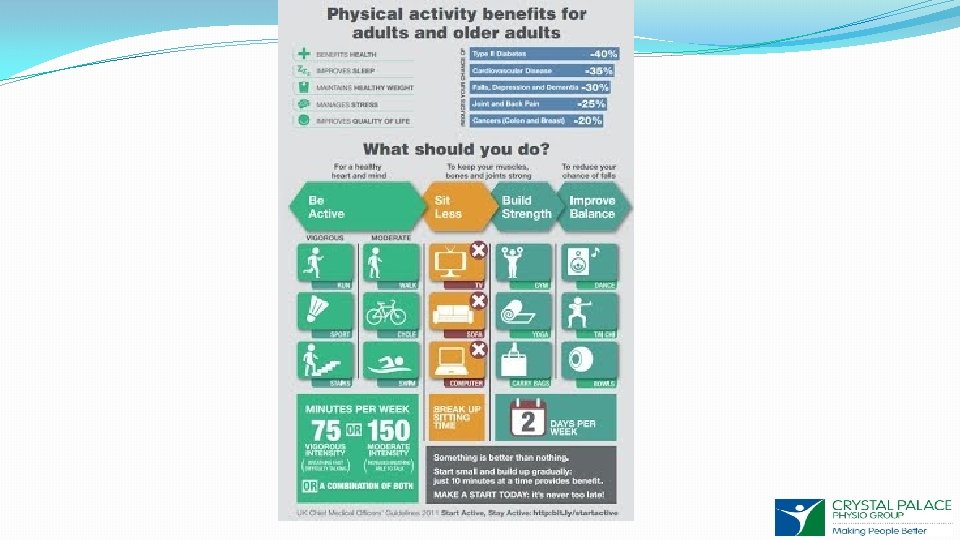
Employee Accountability Take Ownership for your own Health and Wellbeing 2 hours a day of standing/light activity Exercise Take “Microbreaks” Vary your position and posture Avoid prolonged static postures Speak to your Line Manager Seek advice early Public Health England the Active Working Community Interest Company (Buckley et al 2015)
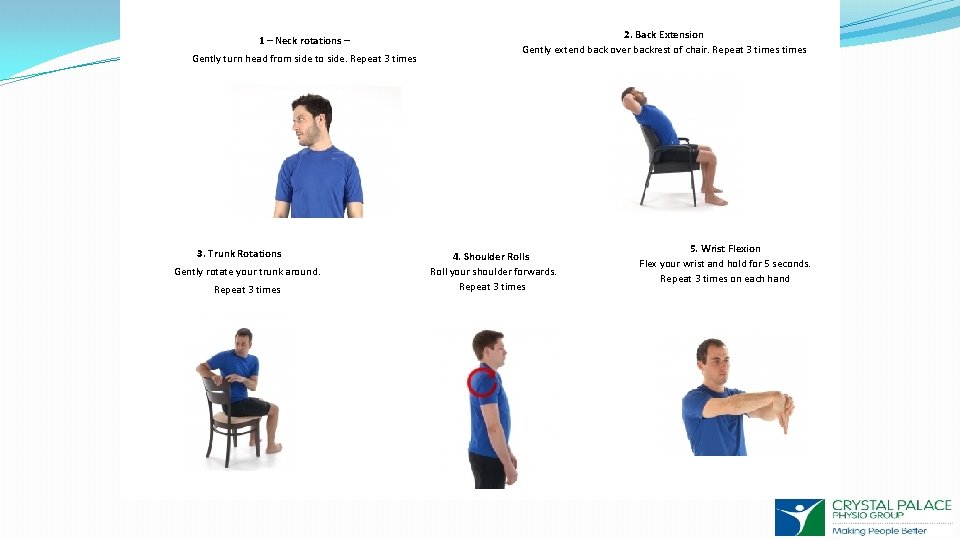
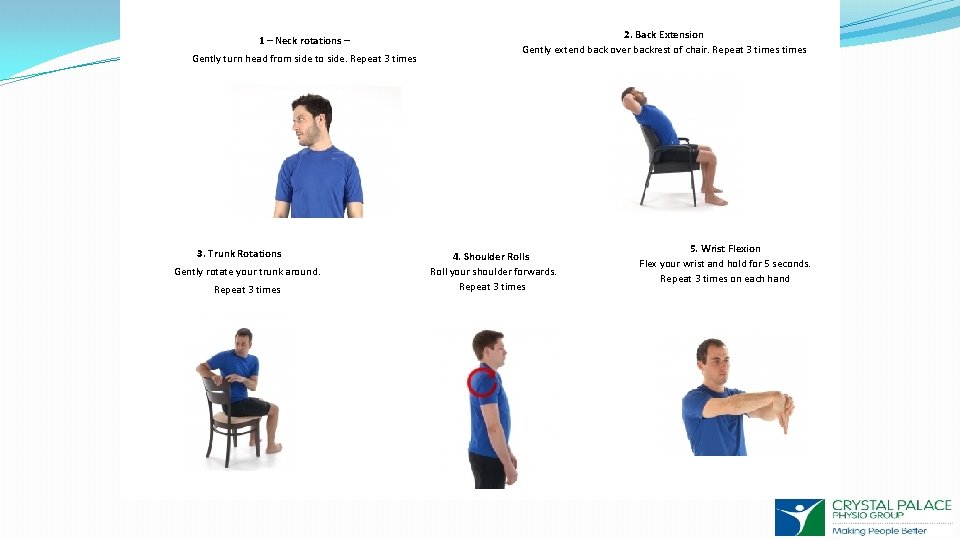
1 – Neck rotations – 2. Back Extension Gently extend back over backrest of chair. Repeat 3 times 4 – An approach to ergonomic assessments Physical Gently turn head from side to side. Repeat 3 times 3. Trunk Rotations Gently rotate your trunk around. Repeat 3 times 5 4. Shoulder Rolls Roll your shoulder forwards. Repeat 3 times 5. Wrist Flexion Flex your wrist and hold for 5 seconds. Repeat 3 times on each hand
Top Tips Incorporate exercise into your working day Walking Meetings Take the stairs Vary your tasks – This will help to avoid cumulative postural stress Break before fatigue (2 -5 minutes per hour) Break Buddy – stretch together (little and often) Stand/Sit whilst on the phone
Summary 1. Exercise (150 minutes moderate; 75 mins vigorous) 2. Take Breaks and regularly changes task/activity 3. Healthy lifestyles 4. Inform your Line Manager about discomfort ASAP
Thanks for listening!