The Lymphatic System Lectures Objectives Understand the origin
The Lymphatic System
Lectures Objectives • Understand the origin and composition of lymph. • Explain the circulation of lymph in the body. • Describe the gross anatomy and histology of the following lymphoid organs: • Spleen, tonsils, thymus, lymph nodes and mucosa associated
Lymphatic System Structure and Function • • Consists of lymph, lymphatic vessels, structures and organs containing lymphatic tissue, red bone marrow Functions of the lymphatic system 1. Drain excess interstitial fluid 2. Transport dietary lipid 3. Carry our immune responses
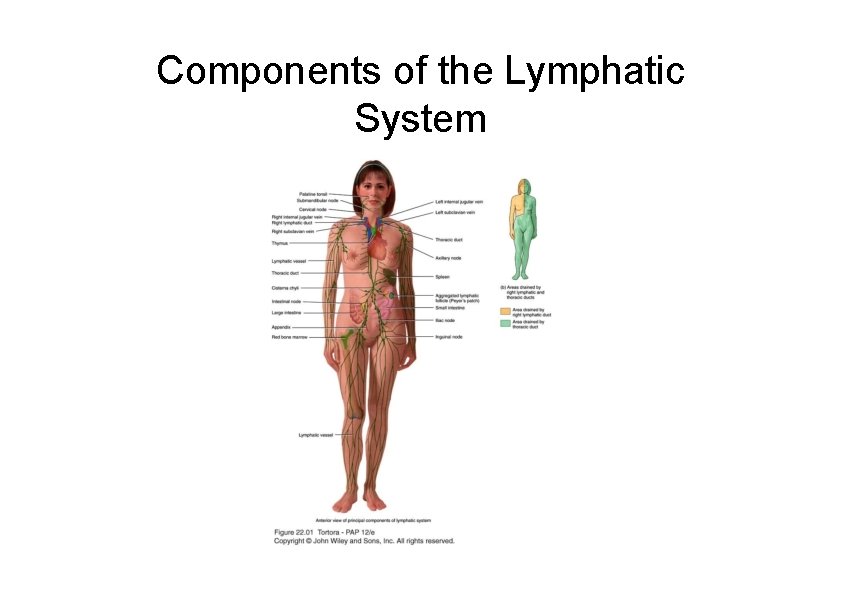
Components of the Lymphatic System
Lymphatic Vessels and Lymph Circulation – Vessels begin as lymphatic capillaries • Closed at one end – Unite to form large lymphatic vessels • Resemble veins in structure but thinner walls and more valves – Passes through lymph nodes • Encapsulated organs with masses and B and T cells
Lymphatic Capillaries – Slightly large diameter than blood capillaries – Unique one-way structure – Permits interstitial fluid to flow in but not out – Anchoring filaments pull openings wider when interstitial fluid accumulates – Found throughout the body except in avascular tissue (cartilage, epidermis & cornea) – Small intestine has lacteal for dietary lipid uptake • Chyle is lymph with lipids
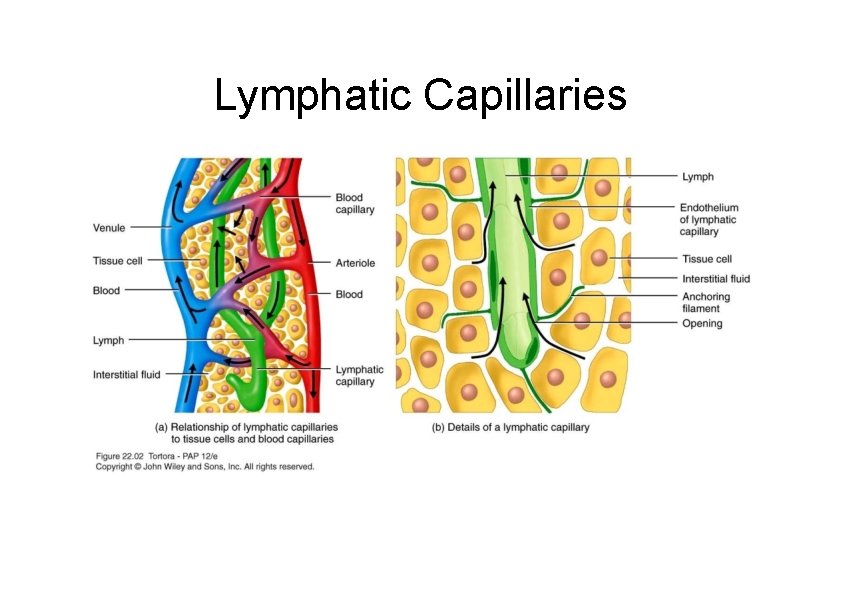
Lymphatic Capillaries
Lymph Trunks and Ducts – Vessels unite to form lymph trunks – Principal trunks are the lumbar, intestinal, bronchomediastinal, subclavian and jugular – Passes from lymph trunks into 2 main channels (thoracic and right lymphatic ducts) before draining into venous blood
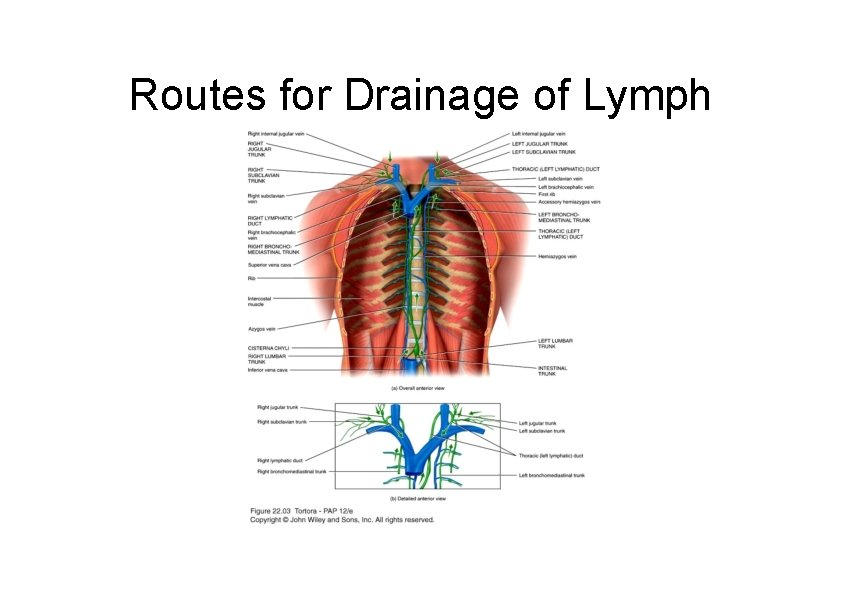
Routes for Drainage of Lymph
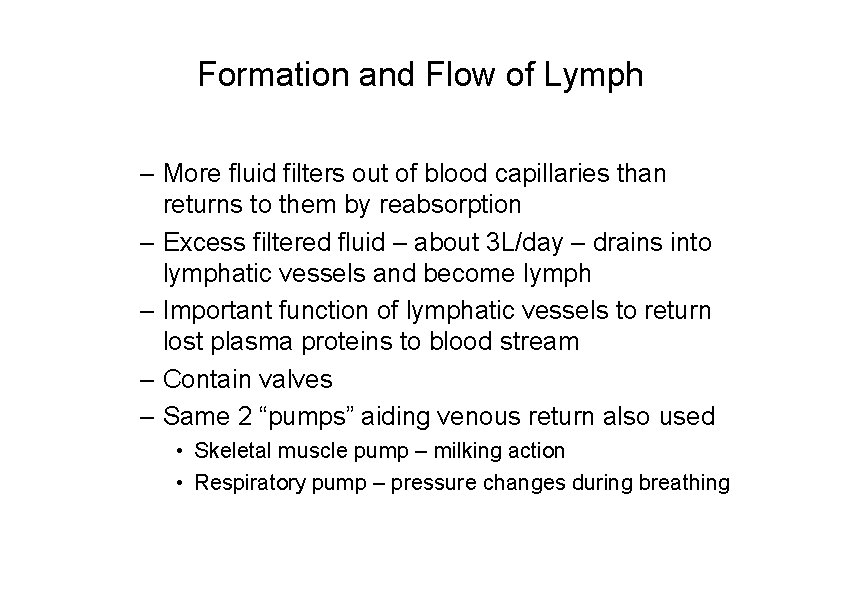
Formation and Flow of Lymph – More fluid filters out of blood capillaries than returns to them by reabsorption – Excess filtered fluid – about 3 L/day – drains into lymphatic vessels and become lymph – Important function of lymphatic vessels to return lost plasma proteins to blood stream – Contain valves – Same 2 “pumps” aiding venous return also used • Skeletal muscle pump – milking action • Respiratory pump – pressure changes during breathing
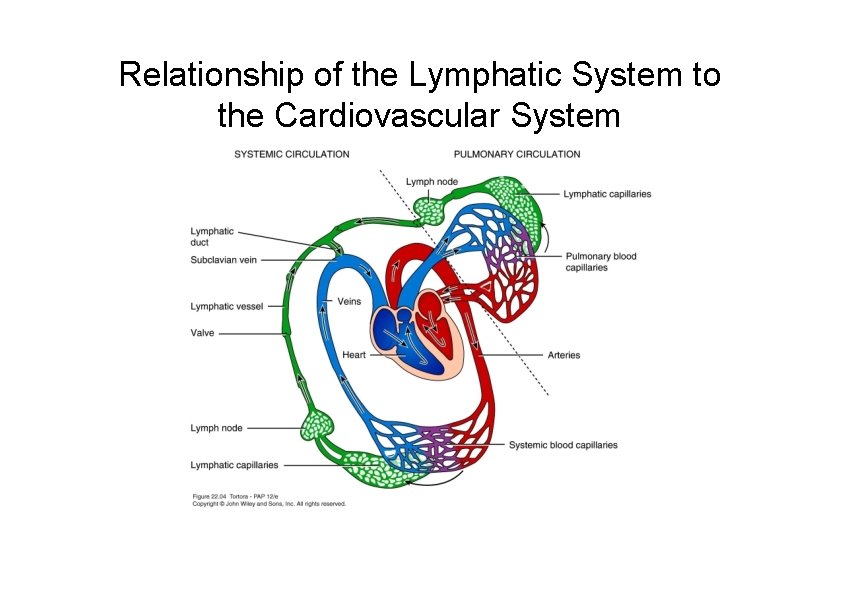
Relationship of the Lymphatic System to the Cardiovascular System
Defense Mechanisms of the Body • Physical barriers to invading organism – – – Secretions-lysozymes, spermine Mucus lining Cilia Epithelial tight junctions Gastric lumen acidic p. H Commensal organisms • Innate, non-adaptive responses – Involve the phagositosis of certain bacteria by granulocytes – These recognition mechanisms are unspecific – Cells involved usually die after completing their attack • Adaptive immune response (lymphatic system)
Adaptive Immune Response • Carried out by the lymphatic system • Responsible for neutralizing many types of infectious agents as well as the organism’s own transformed cells (i. e. , cancer cells) • Immune response must be able to – Recognize the foreign substance or cell – Mount a reaction against it • Carried out by two mechanisms – Humoral immunity – secretion of antibodies by plasma cells – Cell-mediated immunity – secretions of cytokines by T helper cells, action of natural killer cells and cytotoxic T cells • Lymphatic system has three characteristics: – Recognition – Specificity – Memory
Lymphatic Tissues and Organs – 2 groups based on function 1. Primary lymphatic organs • Sites where stem cells divide and become immunocompetent • Red bone marrow and thymus 2. Secondary lymphatic organs • Sites where most immune response occurs • Lymph nodes, spleen, lymphatic nodules
Cells of the Immune System • B-cells/Plasma cells – Differentiate in the bone marrow – Secrete antibodies • T cells – develop in the thymus – Classes of T cells • T helper cells – secrete cytokines which stimulate B cells and other immune cells to elicit an immune response • T cytotoxic cells – destroy host cells that are infected by viruses or are transformed • T suppresser cells – suppresses the immune response • Natural killer cells/Large Granular Lymphocytes (LGLs) – Large lymphocytes with large azurophilic granules – Recognize surface changes that occur on a variety of tumor cells and viral infected cells – Non-phagocytic, they kill by releasing perforins which makes the target cell membrane leaky – There are two classes 1 - null (antibody independent) cells and 2 antibody dependent cells
Cells of the Immune System • Antigen-presenting cells (APCs) – Heterogeneous group of cells such as Langerhans cells in skin, dendritic cells in lymphatic organs and tissues – Express Major Histocompatibility Complex (MHC) molecules on their surface – Phagocytize antigens (any substances that produces an immune response), fragment them into peptides in lysosome, complex the peptide fragments to MHC and present the MHC complex to T helper cells • Macrophages • Reticular cells
Immunoglobulins (Igs, antibodies) • Serum molecules produced by plasma cells (B-cells) • All antibodies have the same basic structure – Fab portion – antigen binding portion; shows diversity – Fc portion – constant region; binds to Fc receptors on the immune cells; determines the Ig class
Immunoglobulins (Igs, antibodies) • Five major classes – Ig. M – first class of antibody produced in a primary response – Ig. A – found in secretions such as milk, saliva, tears, etc. – Ig. D – found on the surface of lymphocytes – Ig. E – found on the surfaces of mast cells and basophils – Ig. G – major Ig of human serum (70 -75% of Ig pool); produced during a secondary response
Immunoglobulins (Igs, antibodies) • Mechanism of immunoglobulin action – Opsonization – binding of antibody to antigen facilitating removal – Complement activation – cascade of reactions of plasma enzymes resulting in increased blood flow, chemotaxis, etc. Activated by Ig. M – Formation of antigen-antibody complex
Lymphocyte Activation • Encountering an antigen – Antigen-presenting cell – Macrophages • Blast transformation • Clonal expansion • Differentiation – Effector cells – Memory cells
Primary Lymphatic Organs
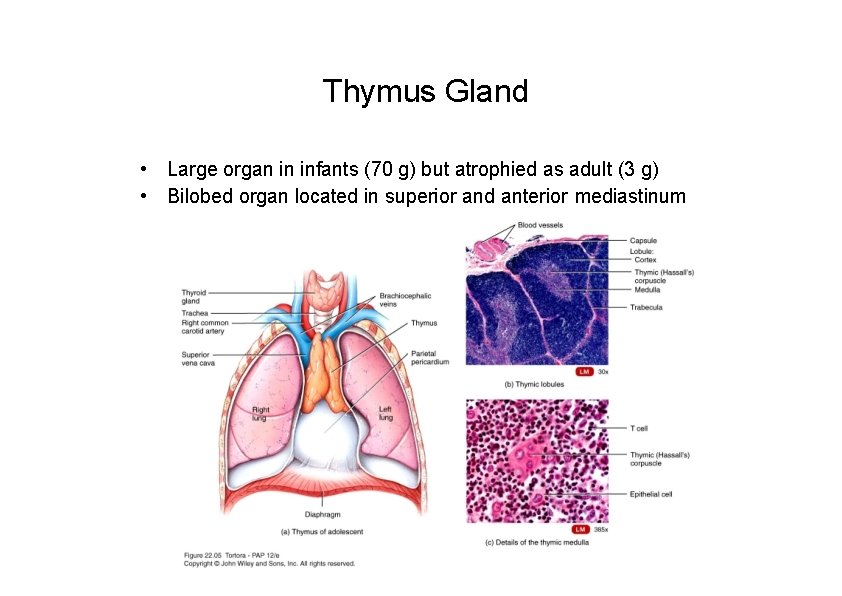
Thymus Gland • Large organ in infants (70 g) but atrophied as adult (3 g) • Bilobed organ located in superior and anterior mediastinum
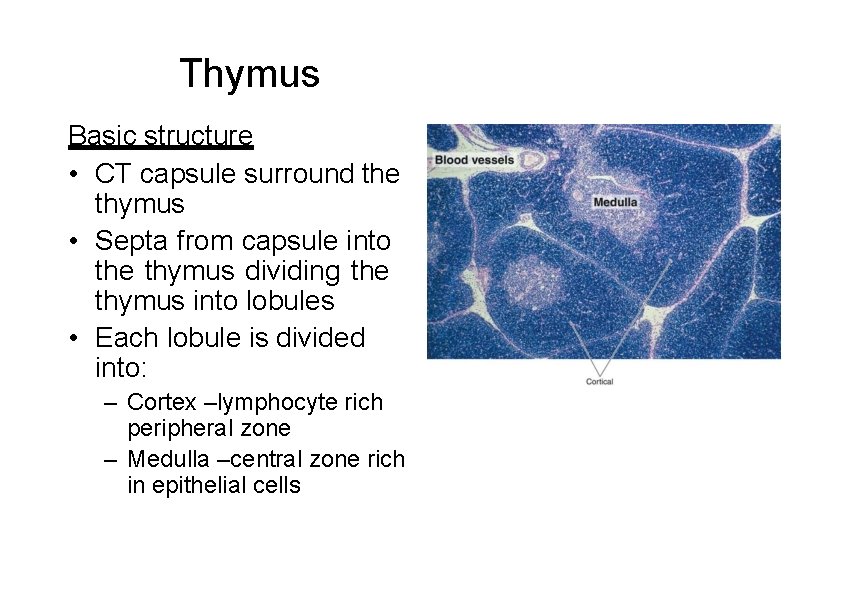
Thymus Basic structure • CT capsule surround the thymus • Septa from capsule into the thymus dividing the thymus into lobules • Each lobule is divided into: – Cortex –lymphocyte rich peripheral zone – Medulla –central zone rich in epithelial cells
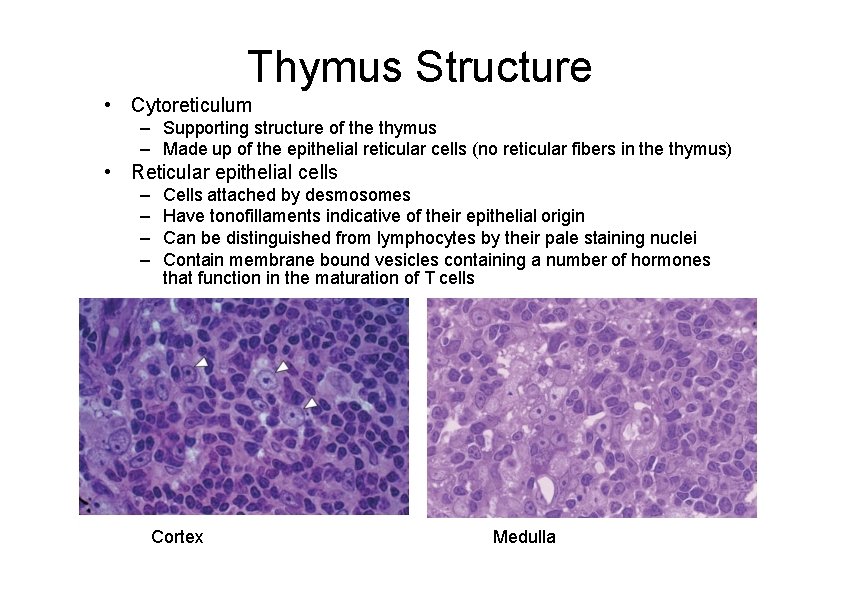
Thymus Structure • Cytoreticulum – Supporting structure of the thymus – Made up of the epithelial reticular cells (no reticular fibers in the thymus) • Reticular epithelial cells – – Cells attached by desmosomes Have tonofillaments indicative of their epithelial origin Can be distinguished from lymphocytes by their pale staining nuclei Contain membrane bound vesicles containing a number of hormones that function in the maturation of T cells Cortex Medulla
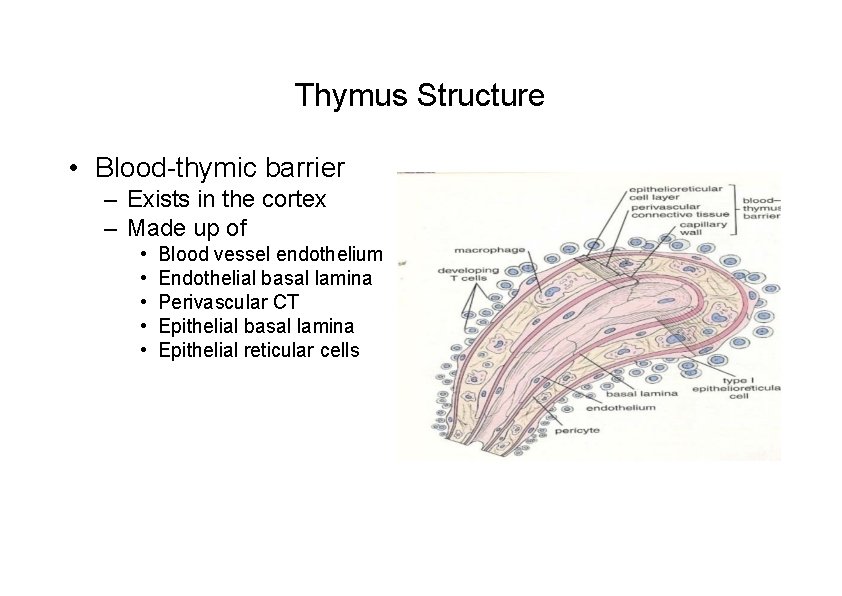
Thymus Structure • Blood-thymic barrier – Exists in the cortex – Made up of • • • Blood vessel endothelium Endothelial basal lamina Perivascular CT Epithelial basal lamina Epithelial reticular cells
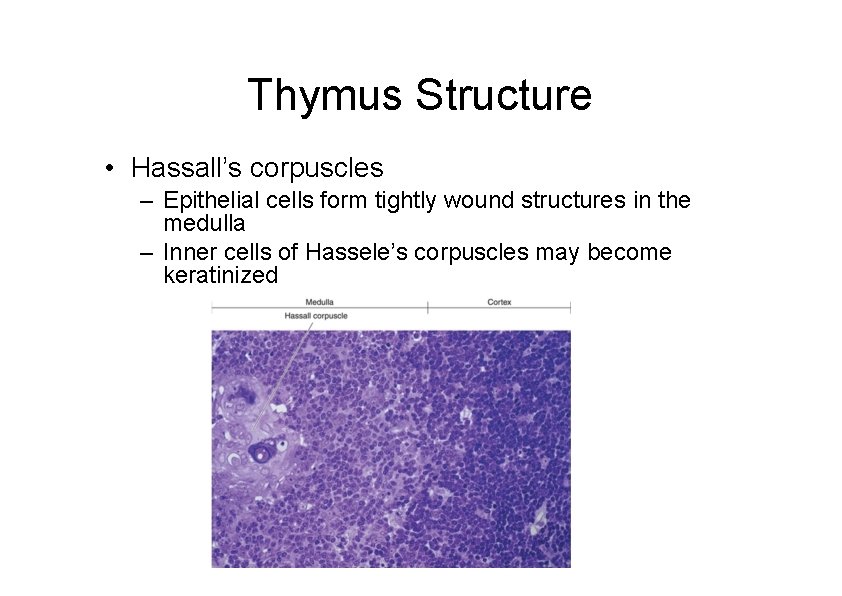
Thymus Structure • Hassall’s corpuscles – Epithelial cells form tightly wound structures in the medulla – Inner cells of Hassele’s corpuscles may become keratinized
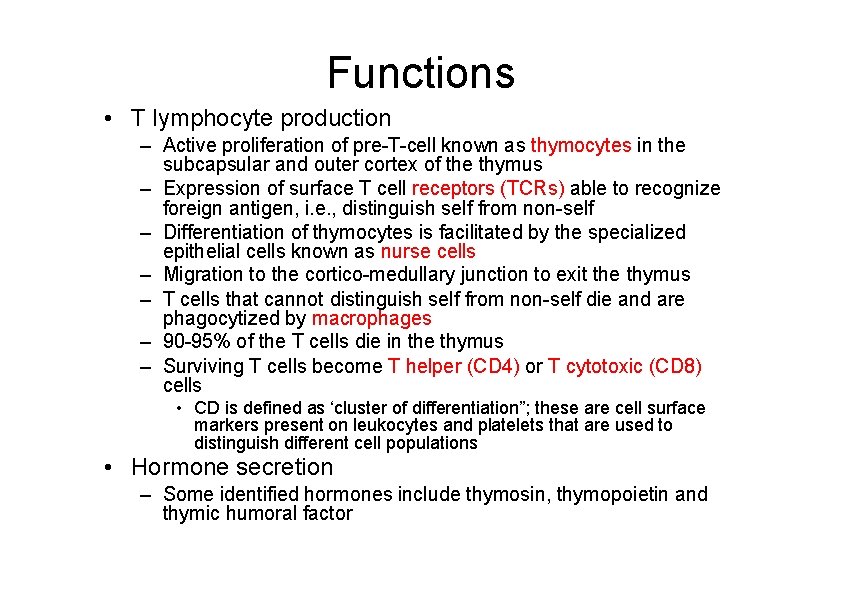
Functions • T lymphocyte production – Active proliferation of pre-T-cell known as thymocytes in the subcapsular and outer cortex of the thymus – Expression of surface T cell receptors (TCRs) able to recognize foreign antigen, i. e. , distinguish self from non-self – Differentiation of thymocytes is facilitated by the specialized epithelial cells known as nurse cells – Migration to the cortico-medullary junction to exit the thymus – T cells that cannot distinguish self from non-self die and are phagocytized by macrophages – 90 -95% of the T cells die in the thymus – Surviving T cells become T helper (CD 4) or T cytotoxic (CD 8) cells • CD is defined as ‘cluster of differentiation”; these are cell surface markers present on leukocytes and platelets that are used to distinguish different cell populations • Hormone secretion – Some identified hormones include thymosin, thymopoietin and thymic humoral factor
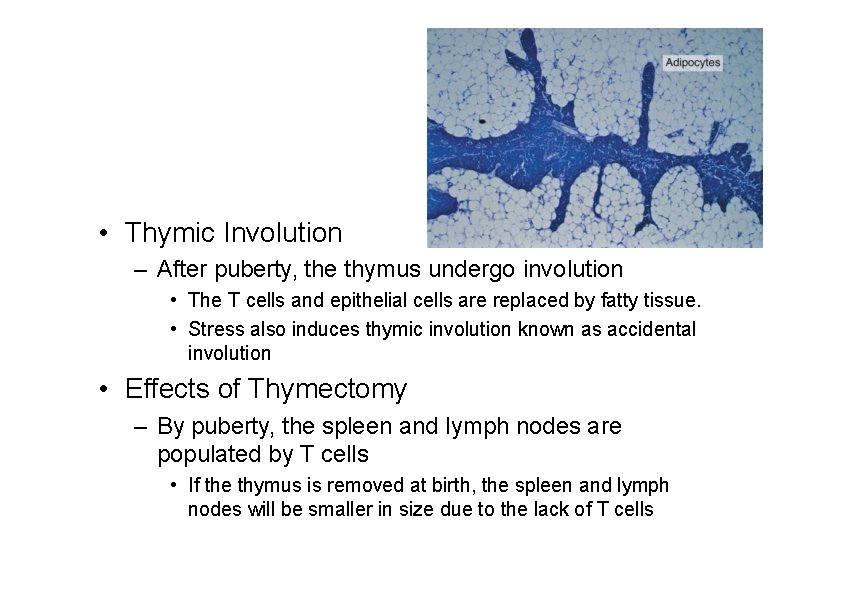
• Thymic Involution – After puberty, the thymus undergo involution • The T cells and epithelial cells are replaced by fatty tissue. • Stress also induces thymic involution known as accidental involution • Effects of Thymectomy – By puberty, the spleen and lymph nodes are populated by T cells • If the thymus is removed at birth, the spleen and lymph nodes will be smaller in size due to the lack of T cells
Secondary Lymphatic Organs
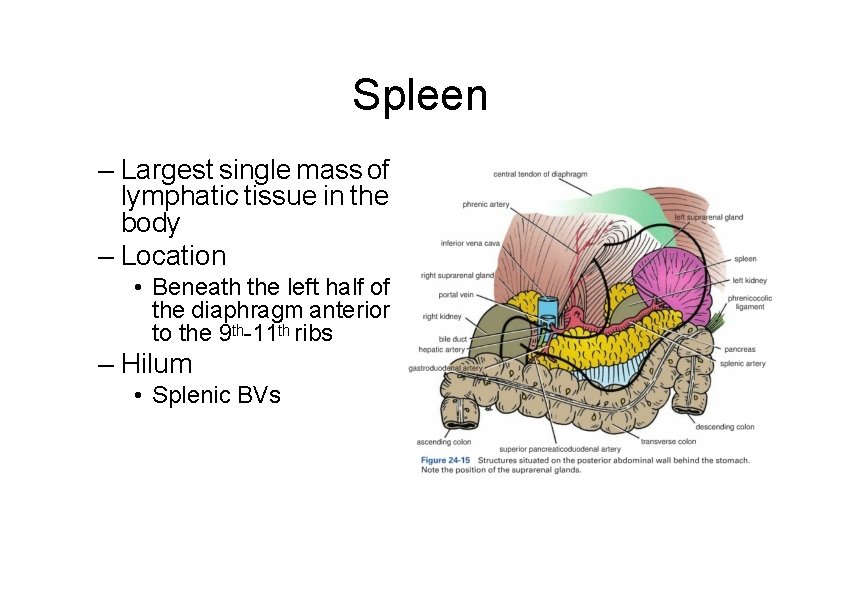
Spleen – Largest single mass of lymphatic tissue in the body – Location • Beneath the left half of the diaphragm anterior to the 9 th-11 th ribs – Hilum • Splenic BVs
Structure of the Spleen
Spleen • Functions of the spleen – Blood filter – Remove of old RBCs – Activation of T and B cells – Antibody production – Blood reservoir – Embryonic hemopoiesis
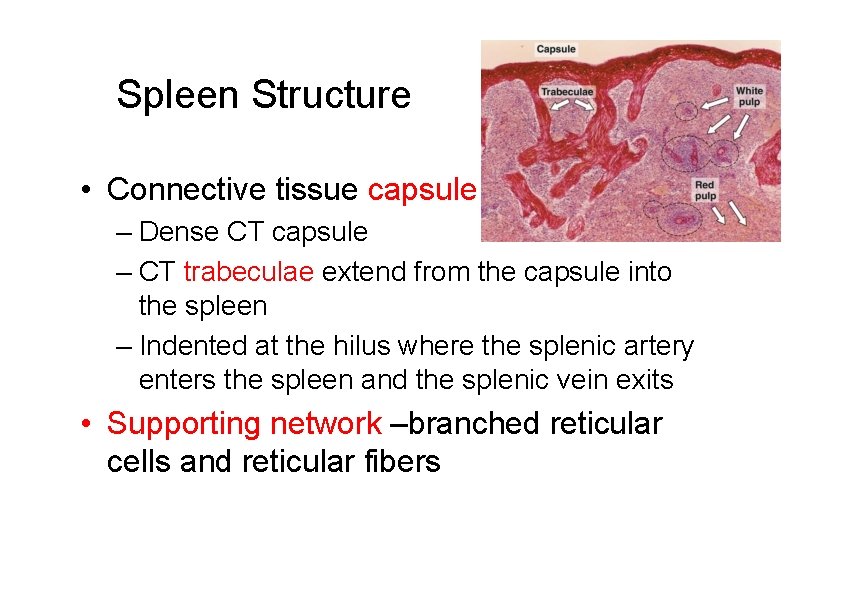
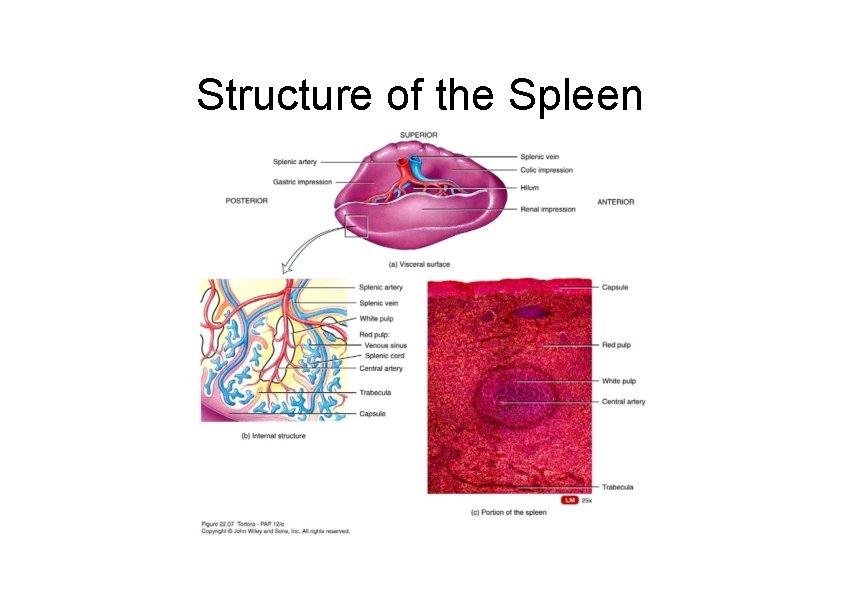
Spleen Structure • Connective tissue capsule – Dense CT capsule – CT trabeculae extend from the capsule into the spleen – Indented at the hilus where the splenic artery enters the spleen and the splenic vein exits • Supporting network –branched reticular cells and reticular fibers
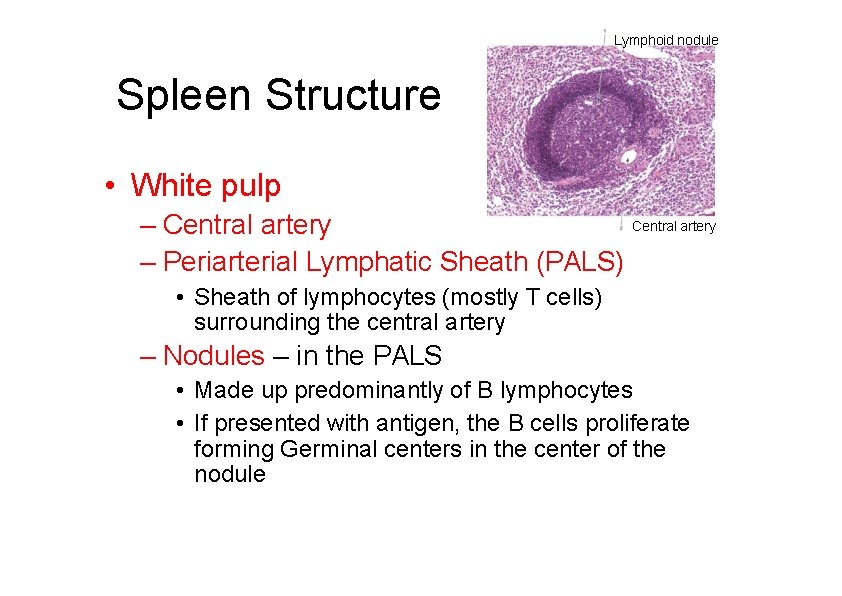
Lymphoid nodule Spleen Structure • White pulp Central artery – Periarterial Lymphatic Sheath (PALS) • Sheath of lymphocytes (mostly T cells) surrounding the central artery – Nodules – in the PALS • Made up predominantly of B lymphocytes • If presented with antigen, the B cells proliferate forming Germinal centers in the center of the nodule
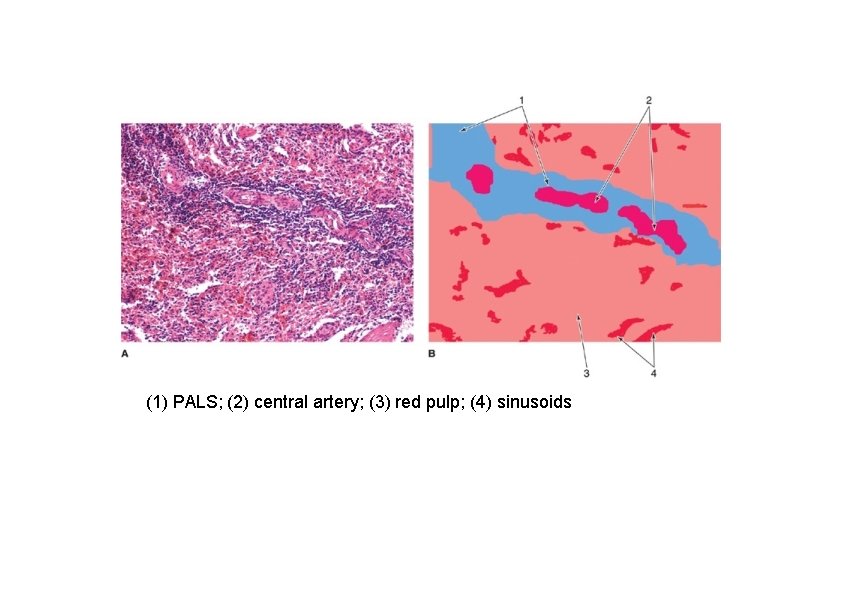
(1) PALS; (2) central artery; (3) red pulp; (4) sinusoids
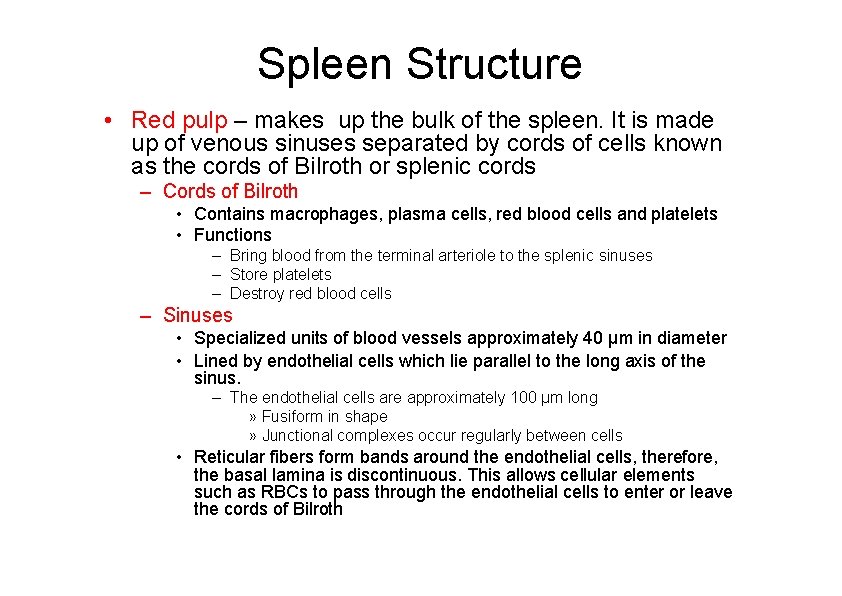
Spleen Structure • Red pulp – makes up the bulk of the spleen. It is made up of venous sinuses separated by cords of cells known as the cords of Bilroth or splenic cords – Cords of Bilroth • Contains macrophages, plasma cells, red blood cells and platelets • Functions – Bring blood from the terminal arteriole to the splenic sinuses – Store platelets – Destroy red blood cells – Sinuses • Specialized units of blood vessels approximately 40 μm in diameter • Lined by endothelial cells which lie parallel to the long axis of the sinus. – The endothelial cells are approximately 100 μm long » Fusiform in shape » Junctional complexes occur regularly between cells • Reticular fibers form bands around the endothelial cells, therefore, the basal lamina is discontinuous. This allows cellular elements such as RBCs to pass through the endothelial cells to enter or leave the cords of Bilroth
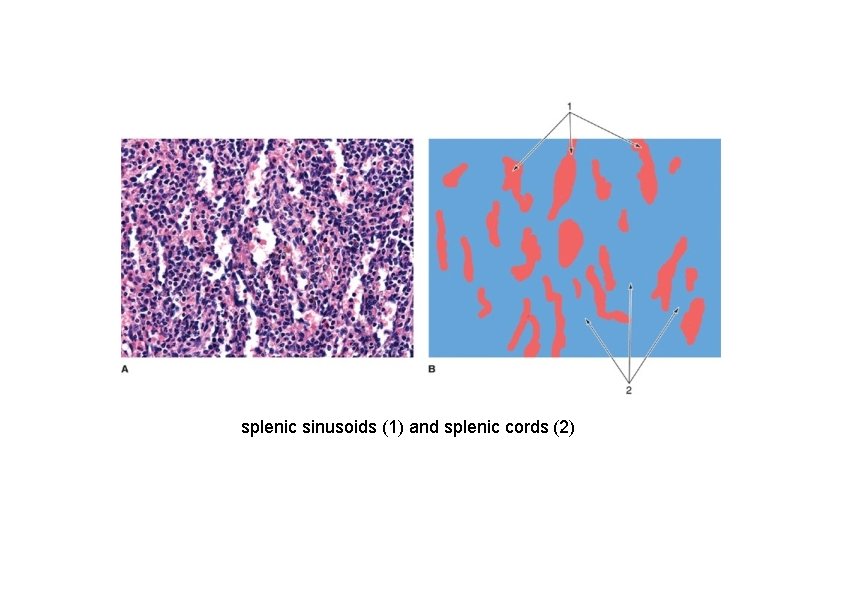
splenic sinusoids (1) and splenic cords (2)
Spleen Structure • Marginal Zone – Concentric layers of reticular cells and fibers at the periphery of the white pulp – Separates white pulp from red pulp – Important because it receives branches from the central artery and much of the blood processing occurs here
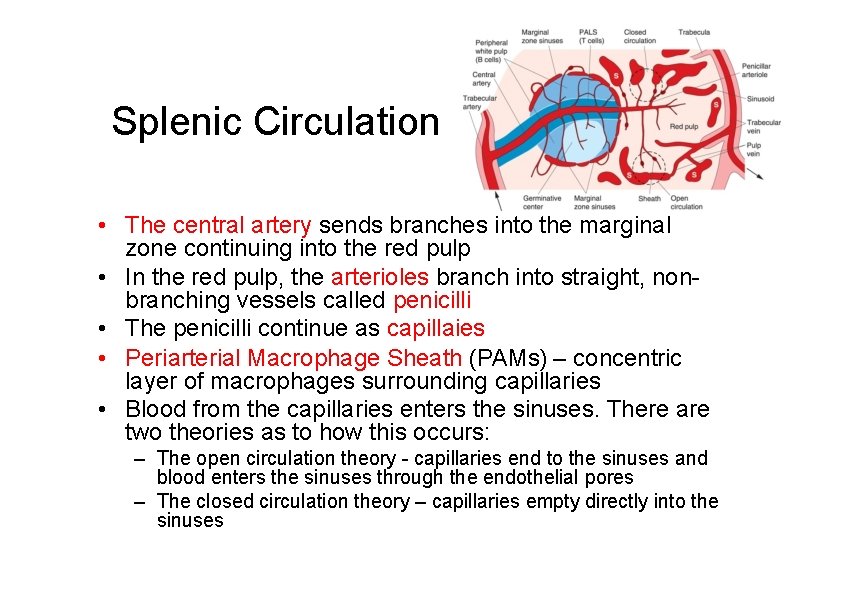
Splenic Circulation • The central artery sends branches into the marginal zone continuing into the red pulp • In the red pulp, the arterioles branch into straight, nonbranching vessels called penicilli • The penicilli continue as capillaies • Periarterial Macrophage Sheath (PAMs) – concentric layer of macrophages surrounding capillaries • Blood from the capillaries enters the sinuses. There are two theories as to how this occurs: – The open circulation theory - capillaries end to the sinuses and blood enters the sinuses through the endothelial pores – The closed circulation theory – capillaries empty directly into the sinuses
Lymph Nodes • Bean-shaped organs, 1 -15 mm diameter • Artery, vein, and efferent lymphatic vessels enter and leave at the hilus • Located along lymphatic vessels • scattered throughout body but concentrated near mammary glands, axillae & groin
Lymph Nodes • Functions – Filtration of lymph • Foreign substances trapped • Destroyed by macrophages or immune response of lymphocytes – Lymphocyte maturation – Immunoglobulin production
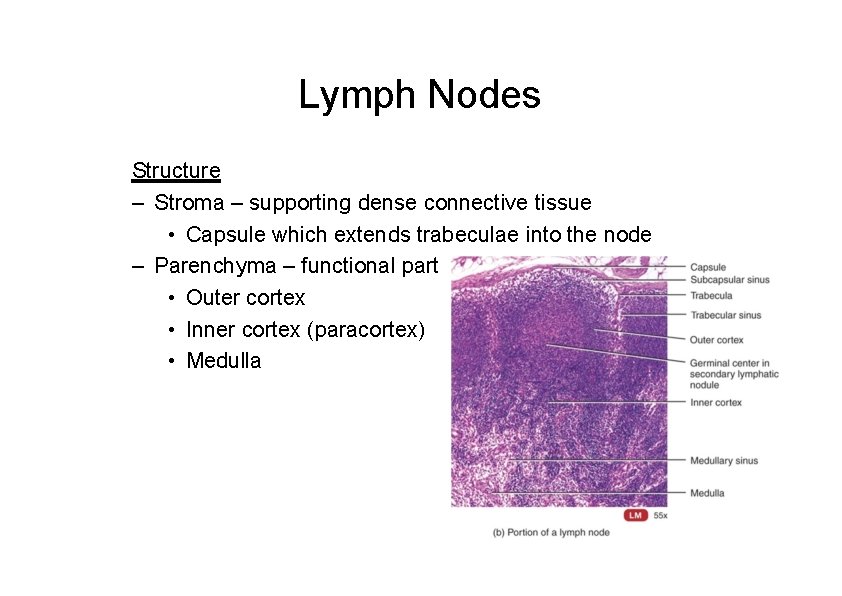
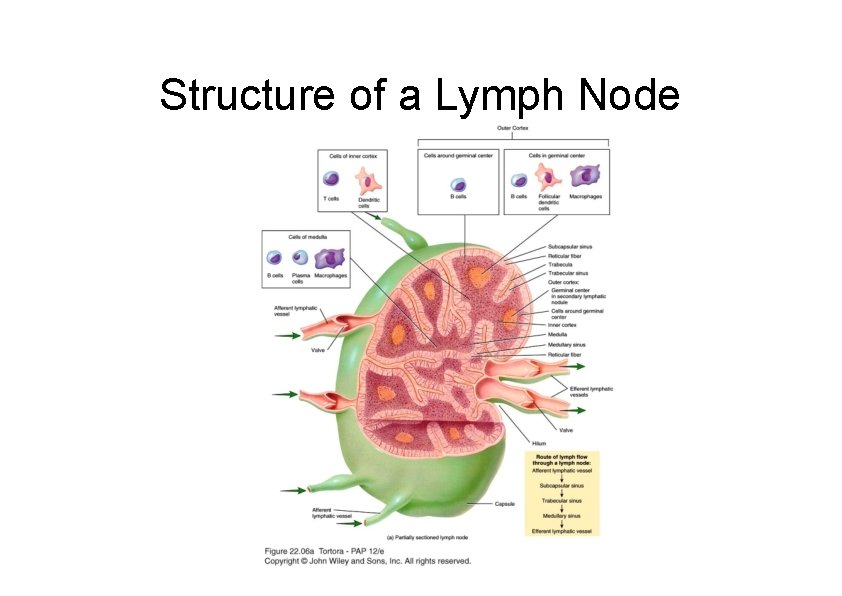
Lymph Nodes Structure – Stroma – supporting dense connective tissue • Capsule which extends trabeculae into the node – Parenchyma – functional part • Outer cortex • Inner cortex (paracortex) • Medulla
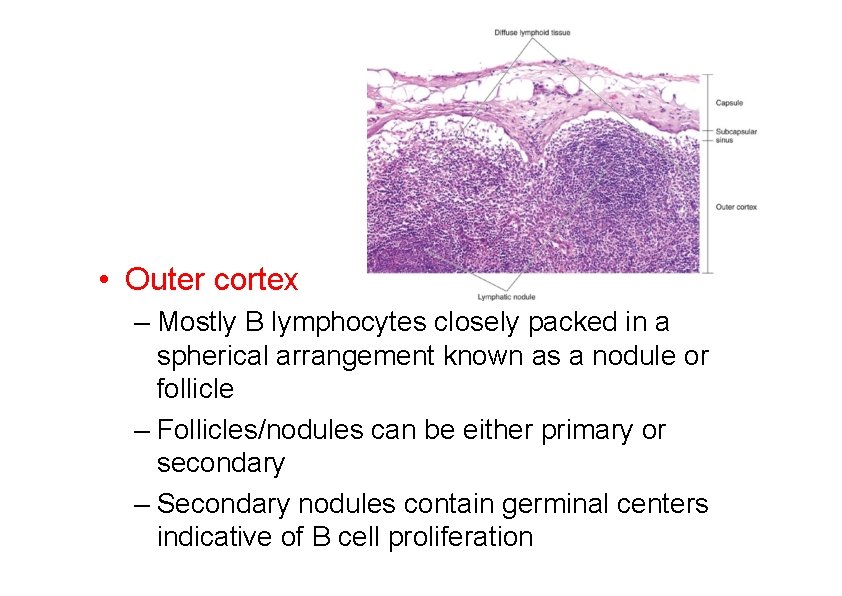
• Outer cortex – Mostly B lymphocytes closely packed in a spherical arrangement known as a nodule or follicle – Follicles/nodules can be either primary or secondary – Secondary nodules contain germinal centers indicative of B cell proliferation
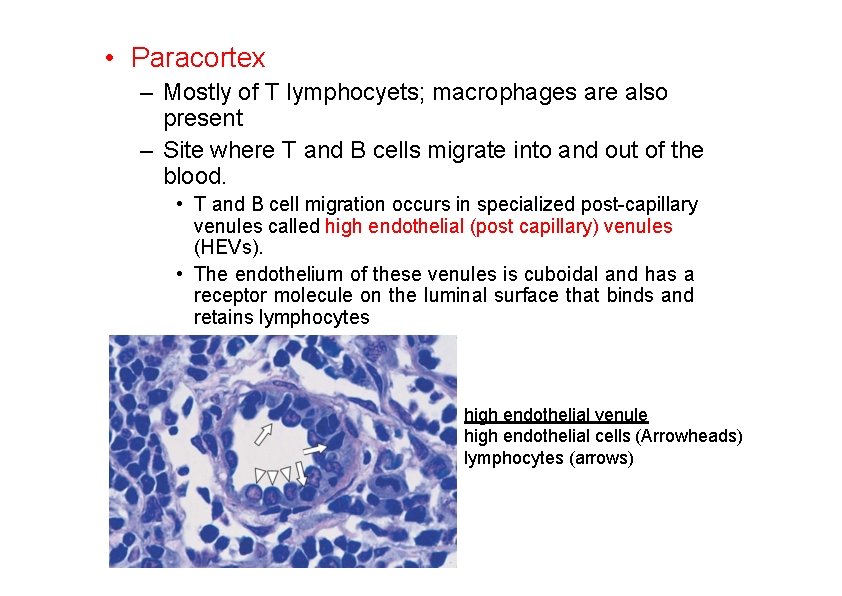
• Paracortex – Mostly of T lymphocyets; macrophages are also present – Site where T and B cells migrate into and out of the blood. • T and B cell migration occurs in specialized post-capillary venules called high endothelial (post capillary) venules (HEVs). • The endothelium of these venules is cuboidal and has a receptor molecule on the luminal surface that binds and retains lymphocytes high endothelial venule high endothelial cells (Arrowheads) lymphocytes (arrows)
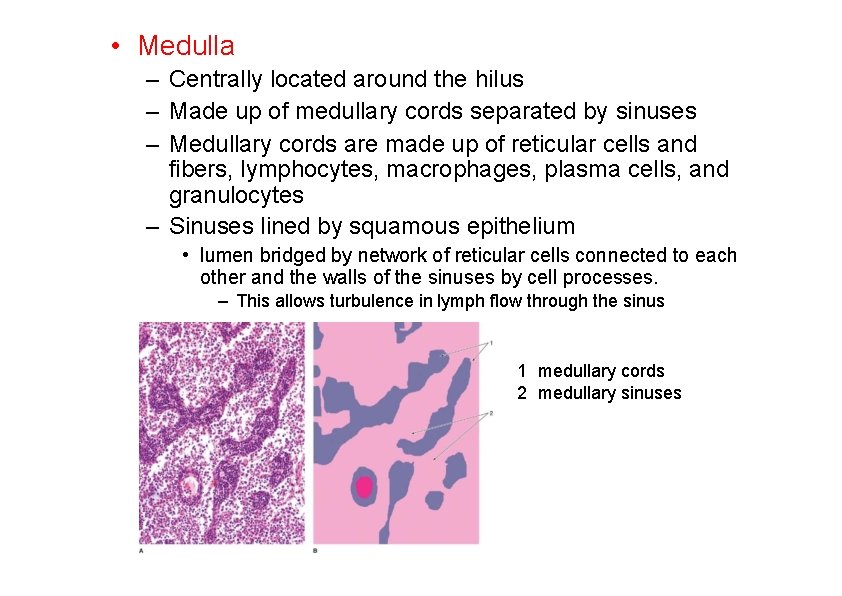
• Medulla – Centrally located around the hilus – Made up of medullary cords separated by sinuses – Medullary cords are made up of reticular cells and fibers, lymphocytes, macrophages, plasma cells, and granulocytes – Sinuses lined by squamous epithelium • lumen bridged by network of reticular cells connected to each other and the walls of the sinuses by cell processes. – This allows turbulence in lymph flow through the sinus 1 medullary cords 2 medullary sinuses
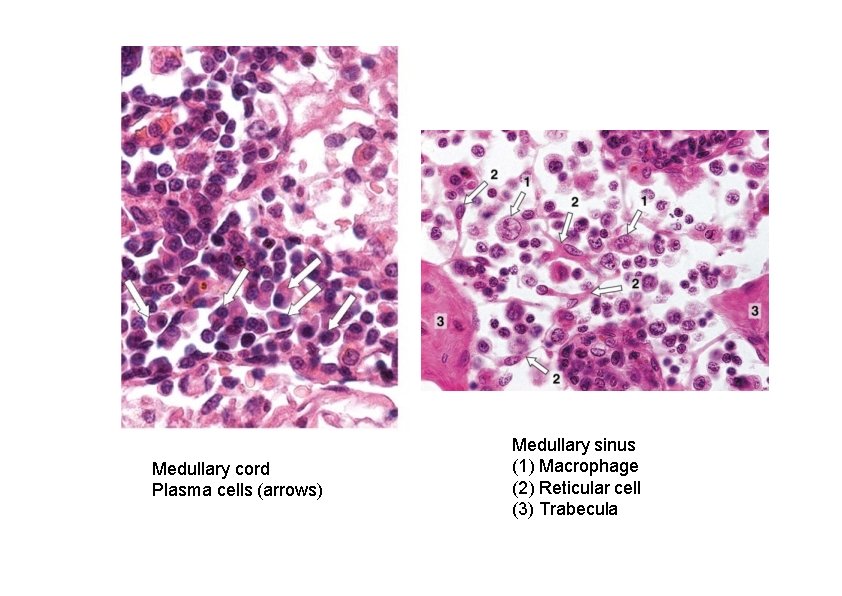
Medullary cord Plasma cells (arrows) Medullary sinus (1) Macrophage (2) Reticular cell (3) Trabecula
Lymph • Lymph flows through a node in 1 direction only – Enters through afferent lymphatic vessels • Directs lymph inward – Lymph enters sinuses (irregular channels) – Into medulla – Medullary sinuses drain into efferent lymphatic vessels – Conveys lymph, antibodies and activated T cells out of the node
Structure of a Lymph Node
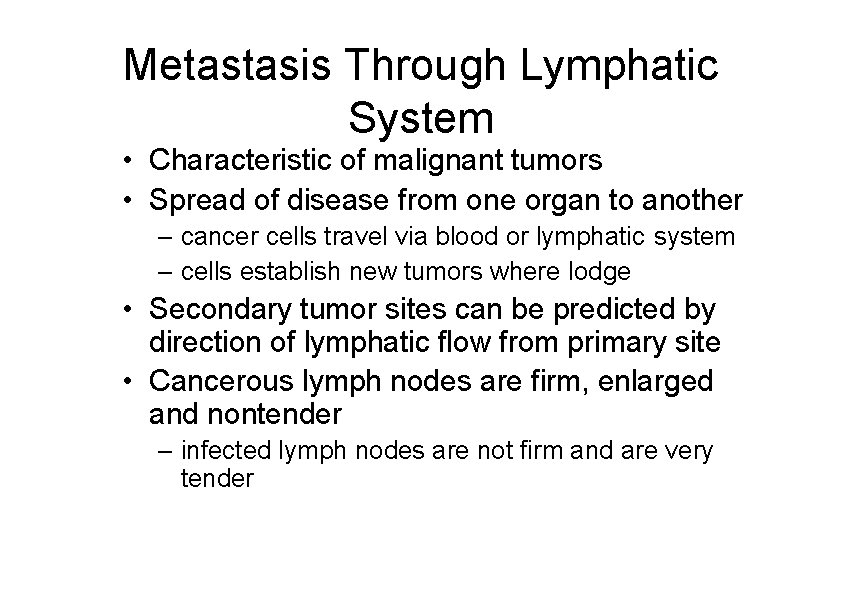
Metastasis Through Lymphatic System • Characteristic of malignant tumors • Spread of disease from one organ to another – cancer cells travel via blood or lymphatic system – cells establish new tumors where lodge • Secondary tumor sites can be predicted by direction of lymphatic flow from primary site • Cancerous lymph nodes are firm, enlarged and nontender – infected lymph nodes are not firm and are very tender
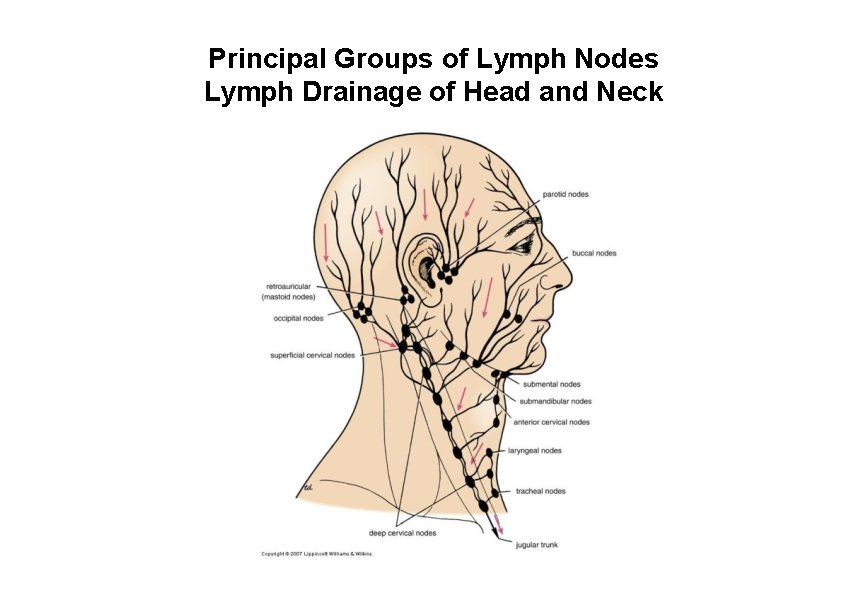
Principal Groups of Lymph Nodes Lymph Drainage of Head and Neck
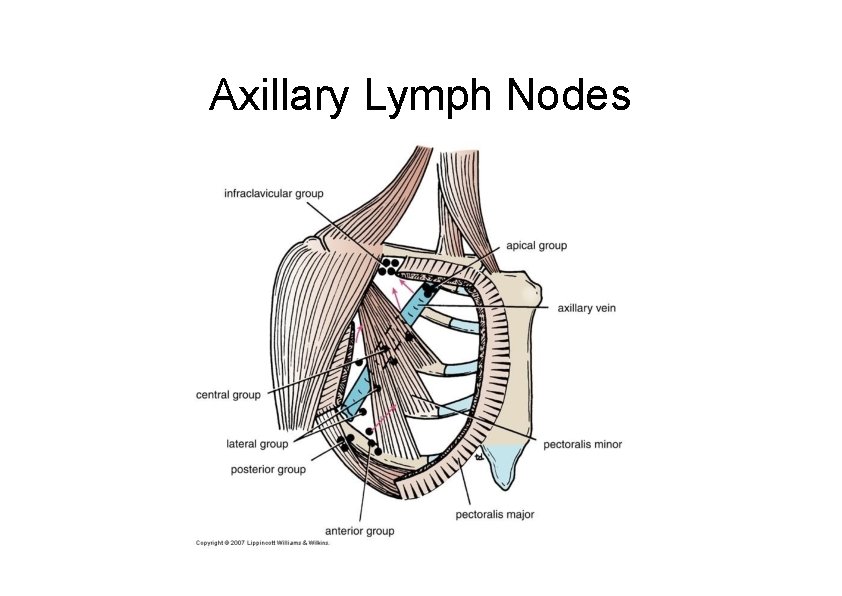
Axillary Lymph Nodes
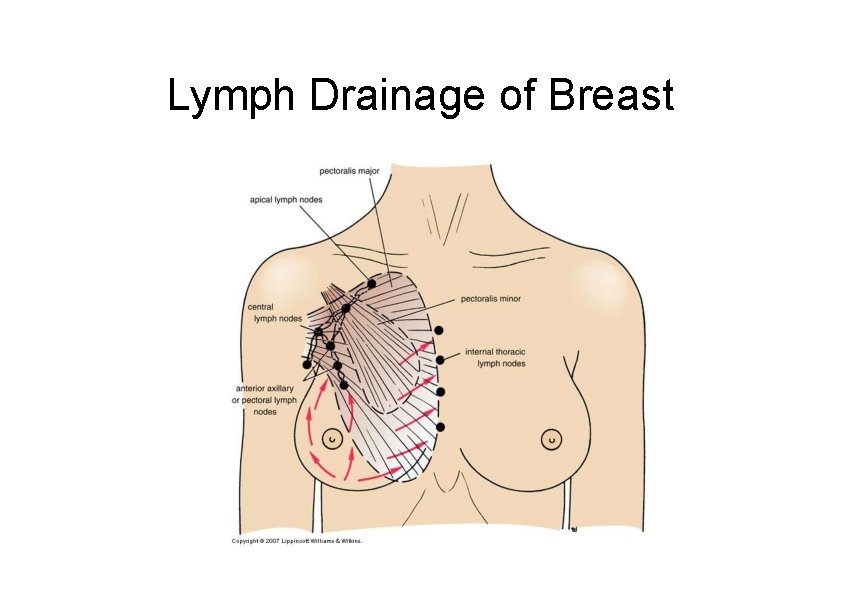
Lymph Drainage of Breast
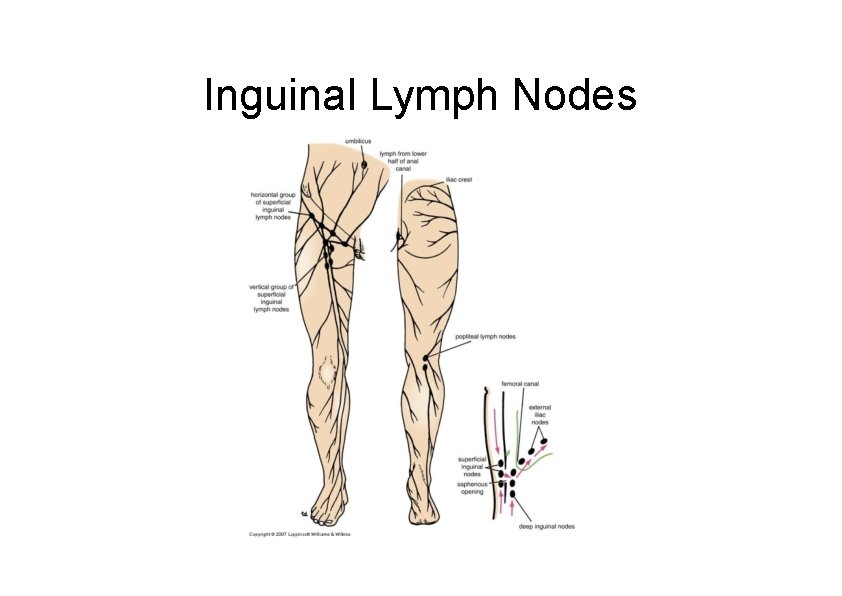
Inguinal Lymph Nodes
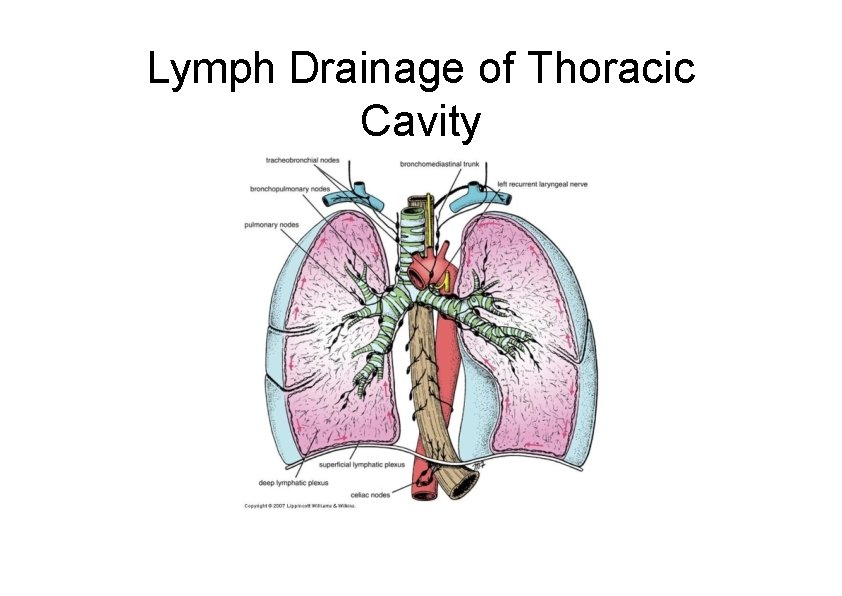
Lymph Drainage of Thoracic Cavity
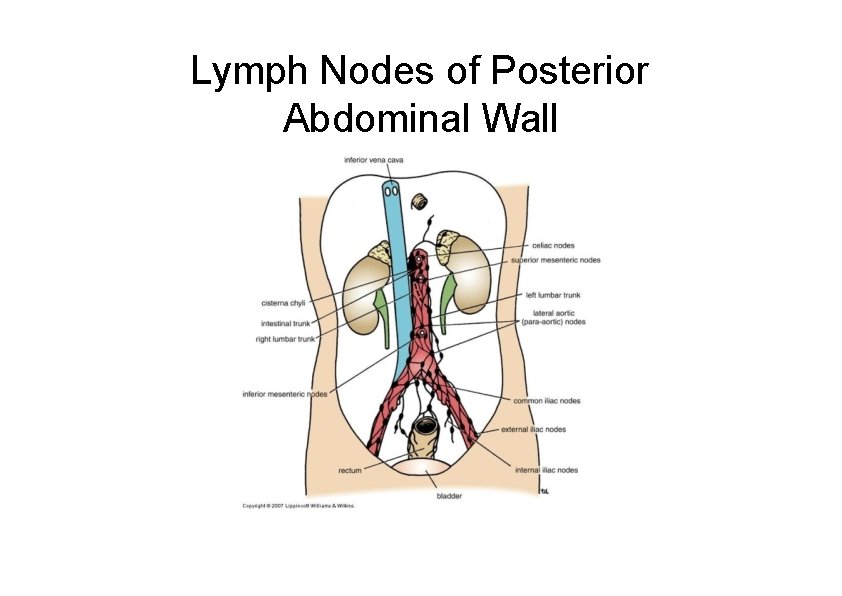
Lymph Nodes of Posterior Abdominal Wall
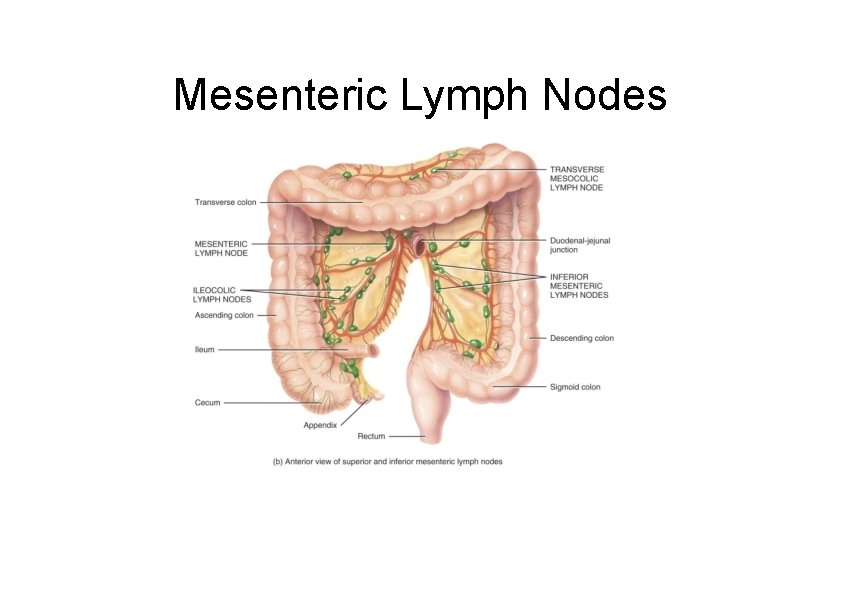
Mesenteric Lymph Nodes
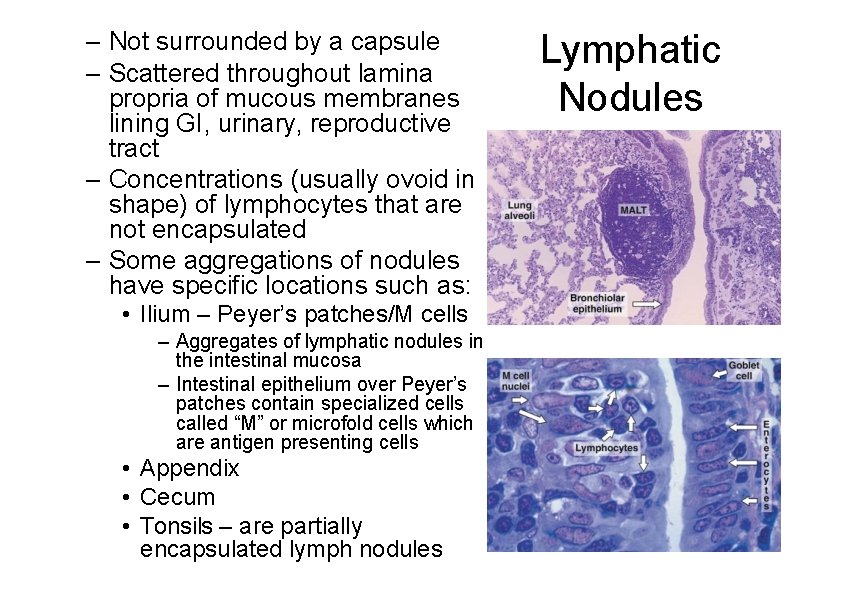
– Not surrounded by a capsule – Scattered throughout lamina propria of mucous membranes lining GI, urinary, reproductive tract – Concentrations (usually ovoid in shape) of lymphocytes that are not encapsulated – Some aggregations of nodules have specific locations such as: • Ilium – Peyer’s patches/M cells – Aggregates of lymphatic nodules in the intestinal mucosa – Intestinal epithelium over Peyer’s patches contain specialized cells called “M” or microfold cells which are antigen presenting cells • Appendix • Cecum • Tonsils – are partially encapsulated lymph nodules Lymphatic Nodules
Tonsils There are three types of tonsils (Waldeyer’s Ring) • Pharyngeal tonsils (adenoids) – Luminal surface lined by stratified squamous or respiratory epithelium – Contains mixed glands in the capsular region • Lingual tonsils – Luminal surface lined by stratified squamous epithelium – Capsular region contains mucous glands and skeletal muscle of the tongue • Palatine tonsil – Luminal surface lined by stratified squamous epithelium – Luminal surface has approximately 20 deep crypts – Capsular region contains mucous glands
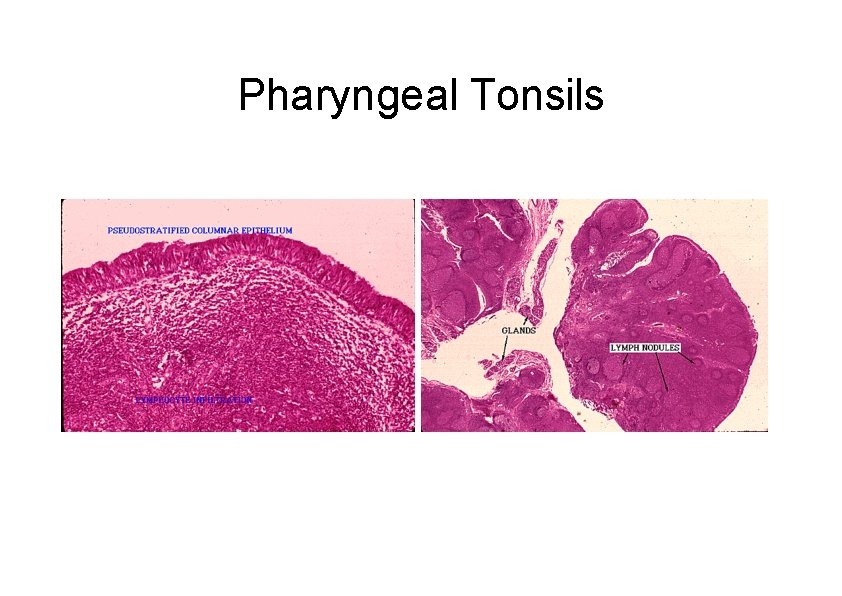
Pharyngeal Tonsils

Lingual Tonsils
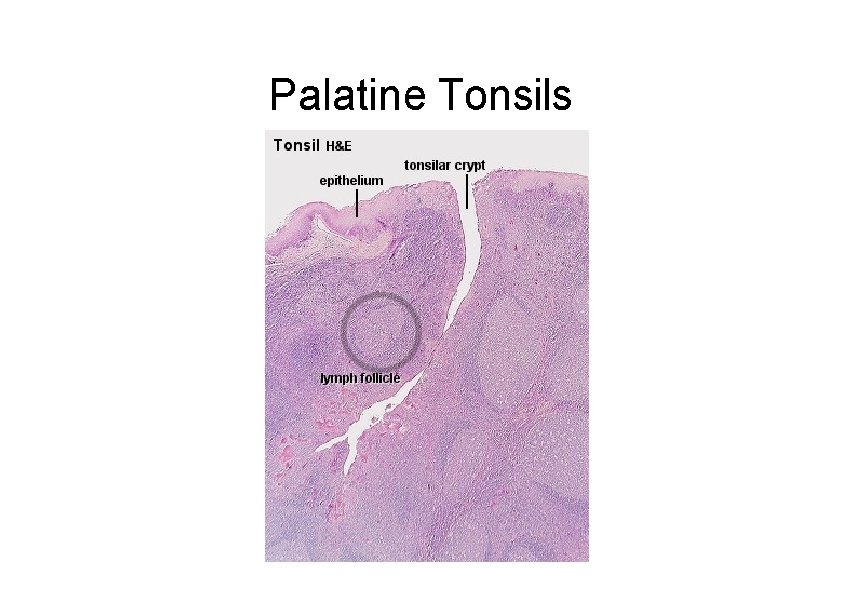
Palatine Tonsils
- Slides: 61