THE LUNG AND THE IMMUNOCOMPROMISED HOST Steve Renshaw


- Slides: 43
THE LUNG AND THE IMMUNOCOMPROMISED HOST Steve Renshaw Reader in Respiratory Medicine Consultant Respiratory Physician University of Sheffield
Aims and Objectives � � � To discuss causes of immunocompromised host To discuss common infections causing problems in such patients To discuss diagnosis and management of these conditions
At the end of this lecture you should be able to; � � Understand how the lung is protected against infection Appreciate that the lung is vulnerable to infection particularly in those who are immunocompromised To appreciate that the presentation of these conditions may not be obvious To understand how prompt investigation and treatment can improve the outcome
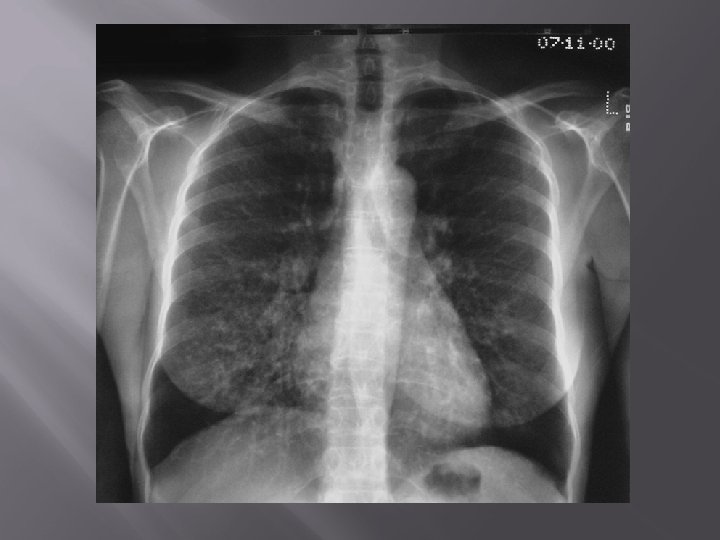
Case History � � � Nov 2000 76 y. o. Man presented via GP with SOB Hx: 12/12 progressive increase SOB Retired steelworker, wife and family all well o/e: O 2 sats 90% on air Bibasal fine end insp. crackles
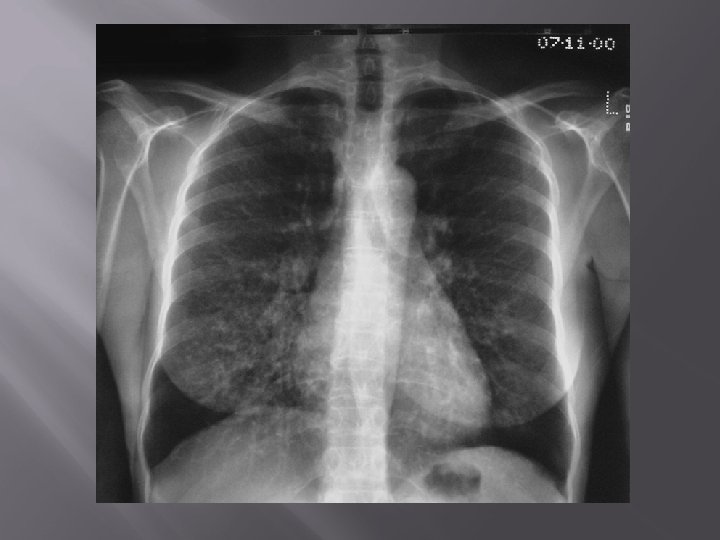
Case History- continued � � Diagnosed Cryptogenic Fibrosing Alveolitis (CFA= Idiopathic Pulmonary Fibrosis) +/infection Treated with po antibiotics Deteriorated gradually over 3 -4 days Referred to respiratory medicine
Seen by me… � � History revisited: Although more SOB over 12/12 was running on a treadmill 6/52 prior to admission, noticed rapid deterioration since Also dry cough On direct questioning, admitted longstanding same sex relationship
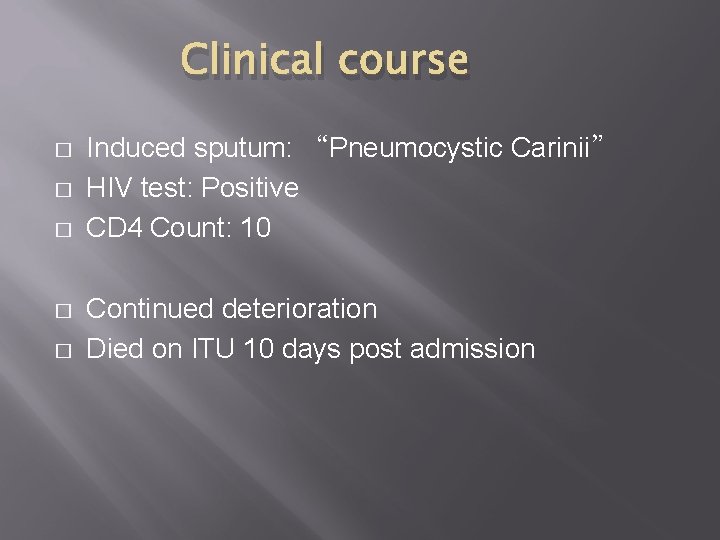
Clinical course � � � Induced sputum: “Pneumocystic Carinii” HIV test: Positive CD 4 Count: 10 Continued deterioration Died on ITU 10 days post admission
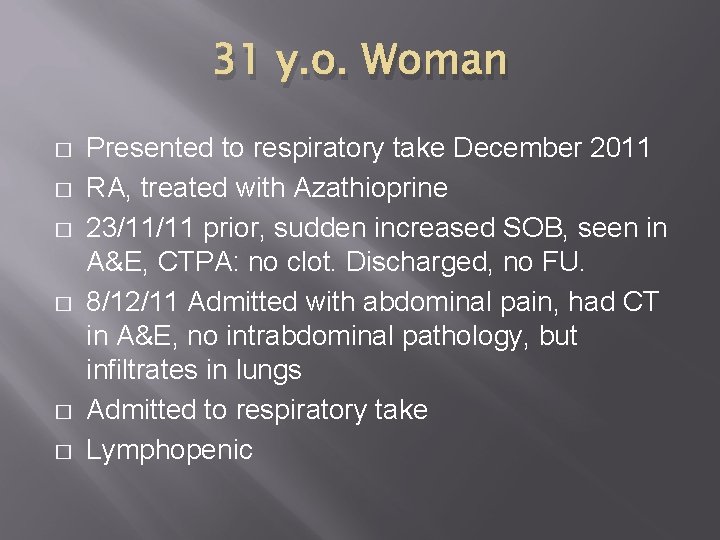
31 y. o. Woman � � � Presented to respiratory take December 2011 RA, treated with Azathioprine 23/11/11 prior, sudden increased SOB, seen in A&E, CTPA: no clot. Discharged, no FU. 8/12/11 Admitted with abdominal pain, had CT in A&E, no intrabdominal pathology, but infiltrates in lungs Admitted to respiratory take Lymphopenic
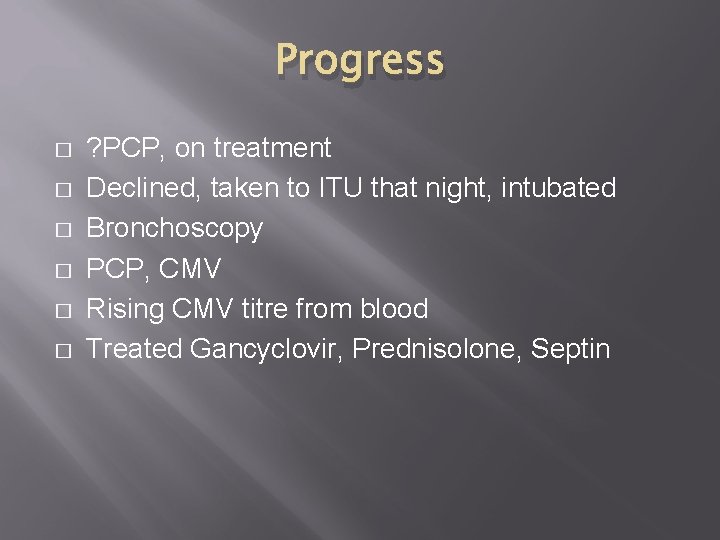
Progress � � � ? PCP, on treatment Declined, taken to ITU that night, intubated Bronchoscopy PCP, CMV Rising CMV titre from blood Treated Gancyclovir, Prednisolone, Septin
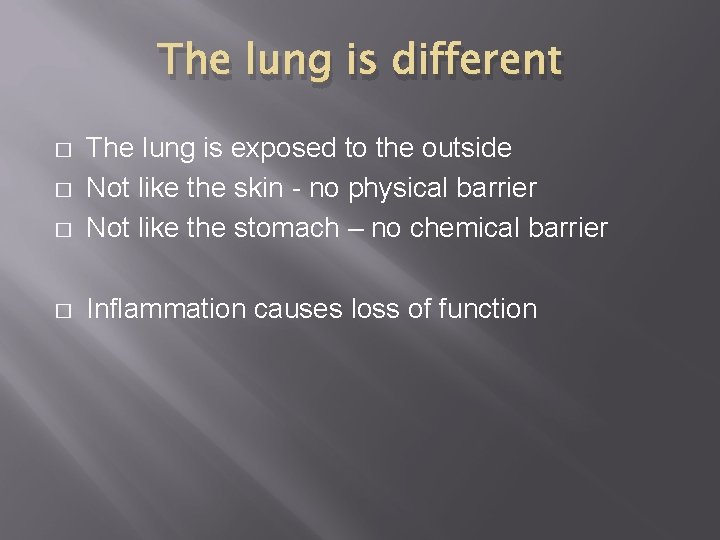
The lung is different � The lung is exposed to the outside Not like the skin - no physical barrier Not like the stomach – no chemical barrier � Inflammation causes loss of function � �
Lung immunity needs to be different � � More robust – tackle all invading pathogens Yet gentler – cannot afford lung injury
Immune compromise � Congenital � X-linked agammaglobulinaemia (XLA) � Chronic granulomatous disease (CGD) � Immunosuppressant treatment � Transplant recipients � Inflammatory disease � Vasculitits � � Cancer chemotherapy Haematological malignancy HIV infection (rare in HAART era) Non-specific – malnutrition, co-existing illness, alcohol
Respiratory immunity � Innate Immune defenses � Mucosal defenses � Complement � Innate cellular defenses Macrophages Neutrophils � Adaptive immune defenses � B-cell mediated Antibodies � T-cell mediated Cytotoxicity
Mucosal Defenses � � Surface secretions Mucosal barrier Respiratory cilia Coughing and sneezing
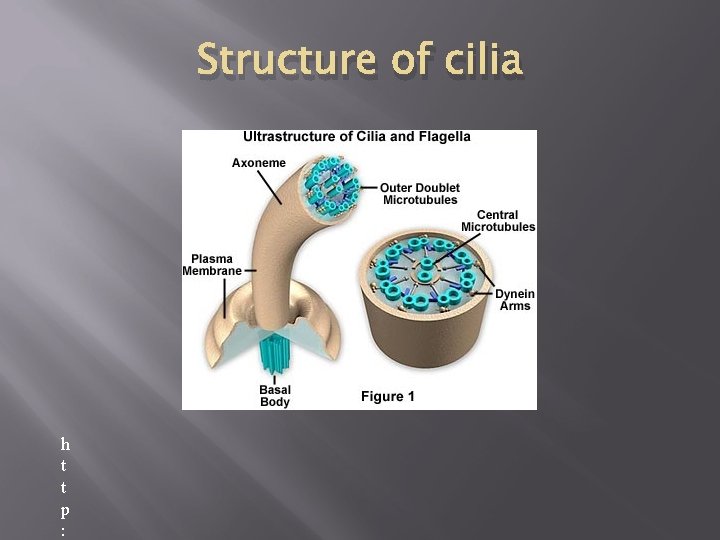
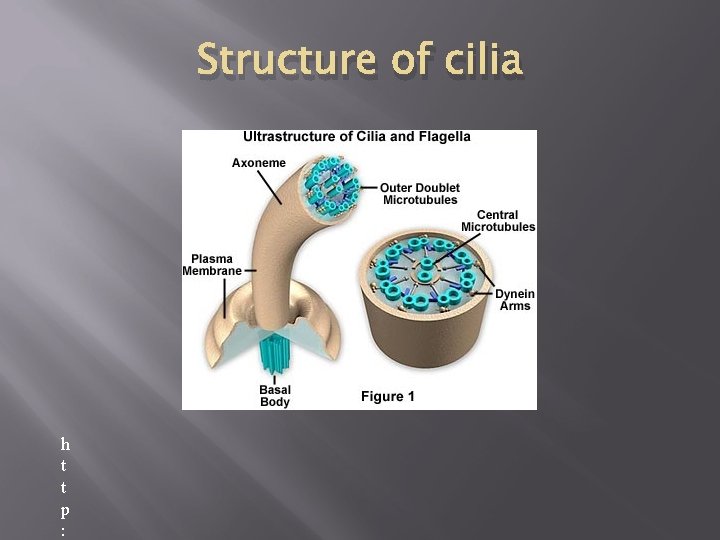
Structure of cilia h t t p :
http: //www. youtube. com/watch? v =NSXbb 5 KZl_I
Mucosal Defense - deficiency � � � Surface secretions – specific defects Mucosal barrier – cystic fibrosis Respiratory cilia – Ciliary Dyskinesias � (Kartagner’s � Syndrome) Coughing and sneezing – Sedation/Ventilation
Innate Cellular Defenses � Neutrophils � “Foot � Soldiers” First cells recruited, fastest migrating Heavily armoured Short-lifespan Phagocytotic Macrophages � Tissue Resident – alveolar macrophages � Recruited from Blood monocytes � Phagocytic � Orchestrate immune response
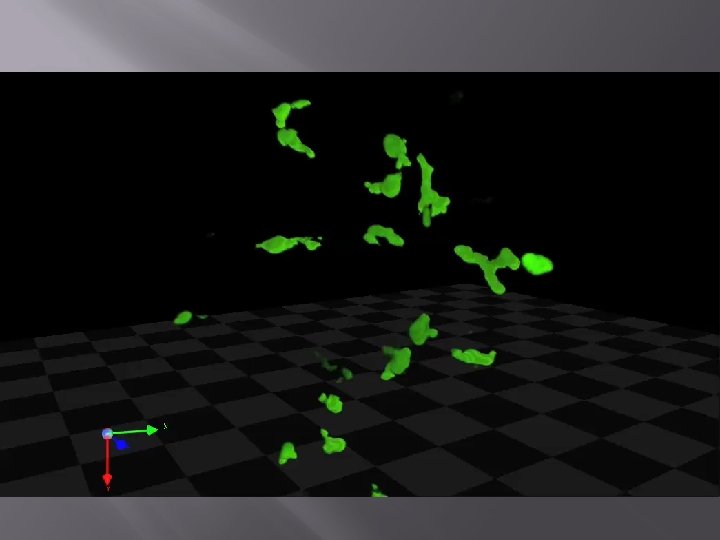

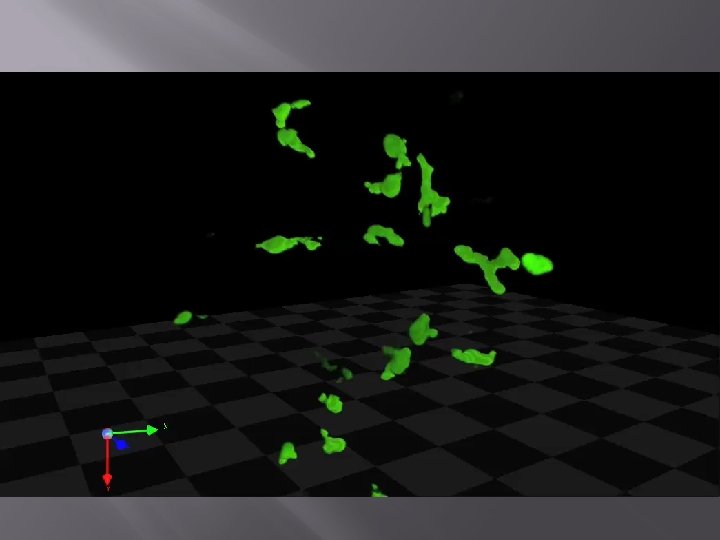
Green = neutrophils Red = zymosan (yeast cell wall particles) © The University of Sheffield

http: //www. youtube. com/watch? v =e. VLO 6 j 6 Ho 64
Defects in Innate Cellular Defenses � Neutrophils � Neutropenia Congenital Iatrogenic � Diseases of neutrophil function �Chronic granulomatous disease � Macrophages
Adaptive immune responses � B-cell � Antibodies � T-cell � Cell mediated cytotoxicity
Defects in adaptive immune responses � B-cell � Antibodies X-linked agammaglobulinaemia Multiple Myeloma Iatrogenic (anti-CD 20, Rituximab) � T-cell � Cell mediated cytotoxicity Iatrogenic Haematological malignancy HIV infection (rare in HAART era)
Iatrogenic immunosuppression � � � Corticosteroid therapy (predominantly T-cell function) Cytotoxic chemotherapy (Neutrophils>Lymph>others) Immune suppression – eg solid organ transplantation, inflammatory disease etc. (T -cells predominantly)
Non-specific immunosuppression � � � Malnutrition Co-existing illness Sepsis Alcohol Trauma Endurance sports
Presentation of pulmonary infection in the immunocompromised � � Pyrexia Respiratory symptoms (Cough, SOB) Pulmonary infiltrates on CXR or CT Hypoxia � at rest � Exertional
Clinical syndromes: � Can divide types of immunosuppression into 2 categories: � Granulocyte/humoral � T-cell defect
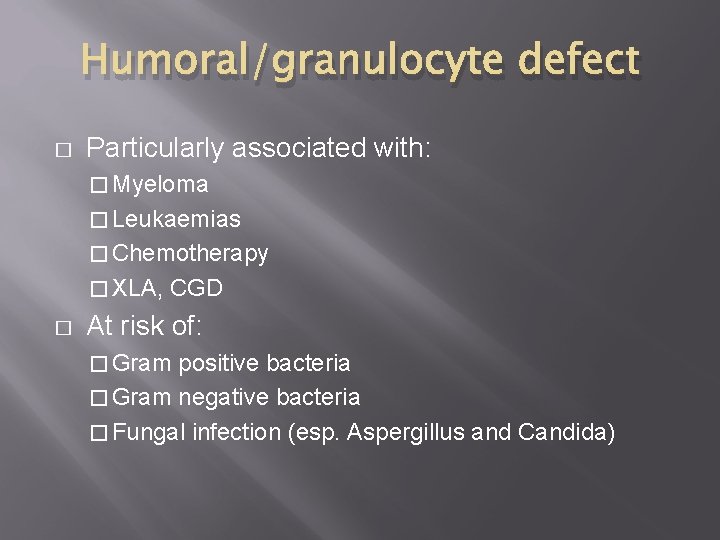
Humoral/granulocyte defect � Particularly associated with: � Myeloma � Leukaemias � Chemotherapy � XLA, � CGD At risk of: � Gram positive bacteria � Gram negative bacteria � Fungal infection (esp. Aspergillus and Candida)
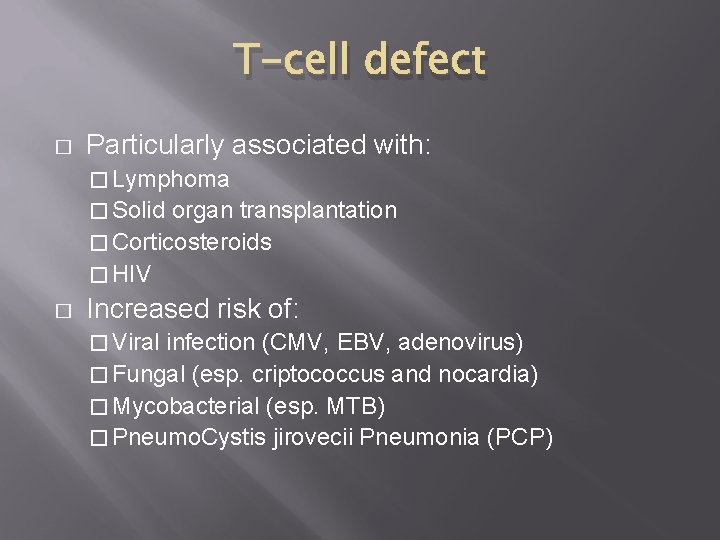
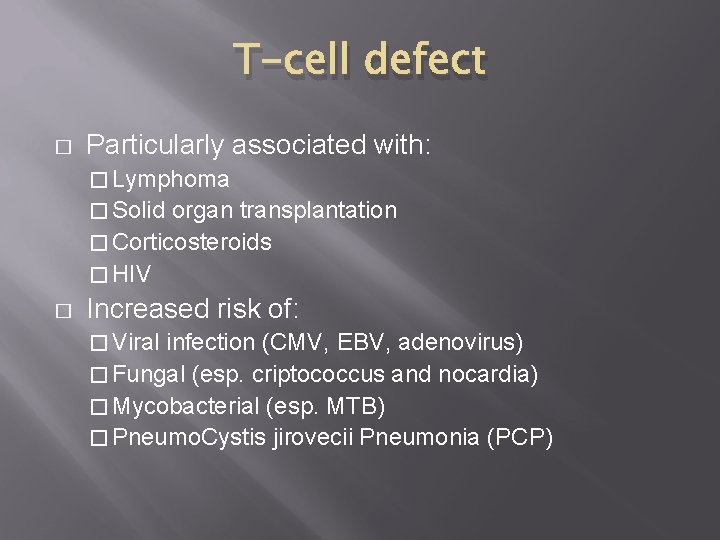
T-cell defect � Particularly associated with: � Lymphoma � Solid organ transplantation � Corticosteroids � HIV � Increased risk of: � Viral infection (CMV, EBV, adenovirus) � Fungal (esp. criptococcus and nocardia) � Mycobacterial (esp. MTB) � Pneumo. Cystis jirovecii Pneumonia (PCP)
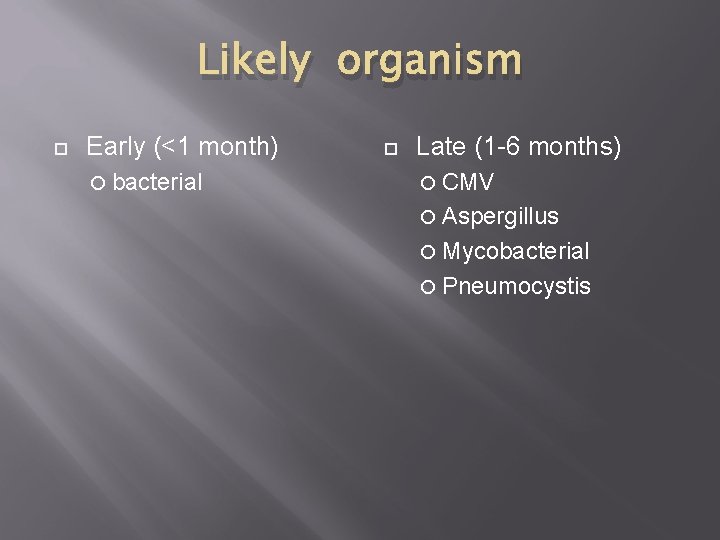
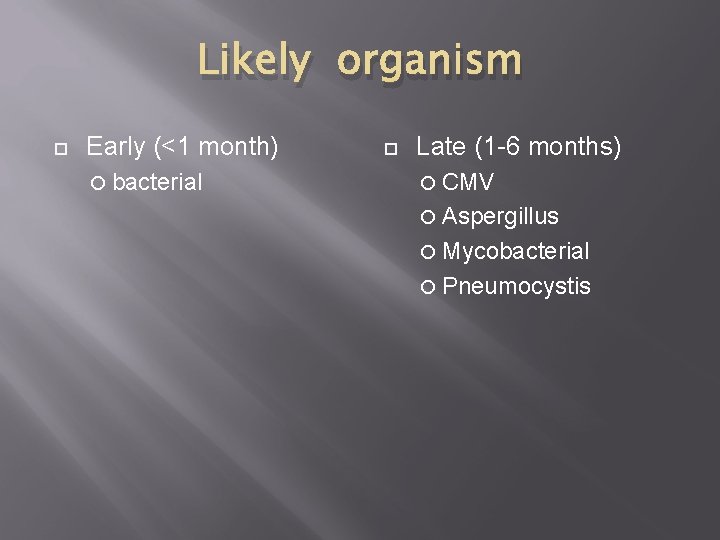
Likely organism Early (<1 month) bacterial Late (1 -6 months) CMV Aspergillus Mycobacterial Pneumocystis
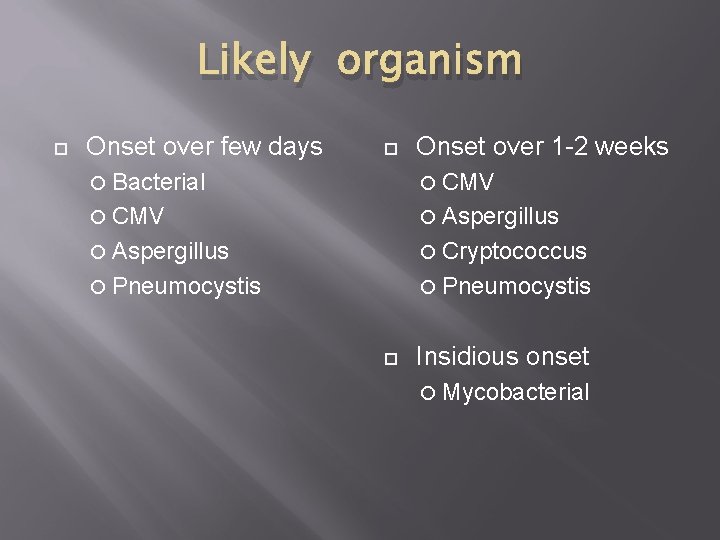
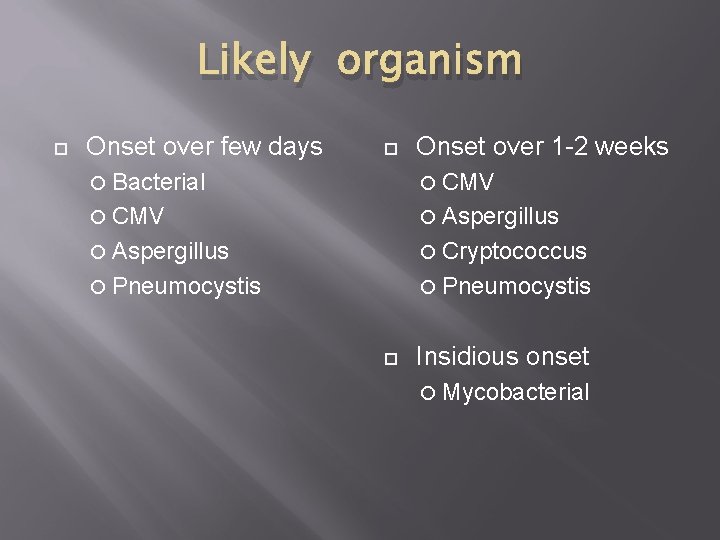
Likely organism Onset over few days Onset over 1 -2 weeks Bacterial CMV Aspergillus Cryptococcus Pneumocystis Insidious onset Mycobacterial
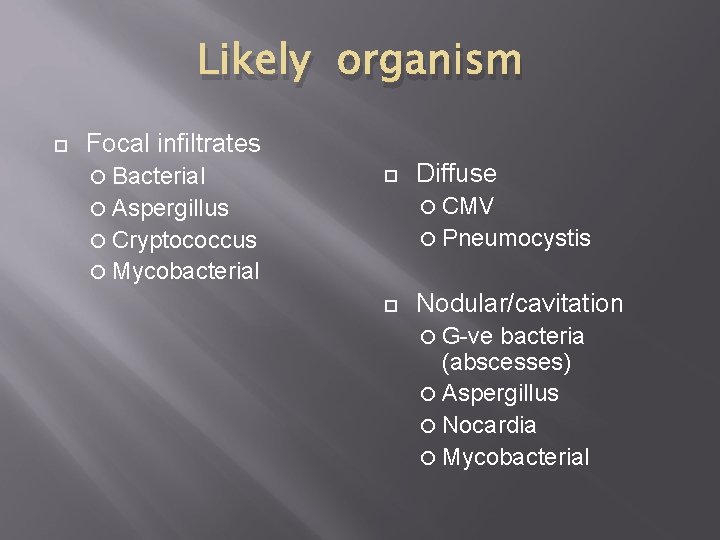
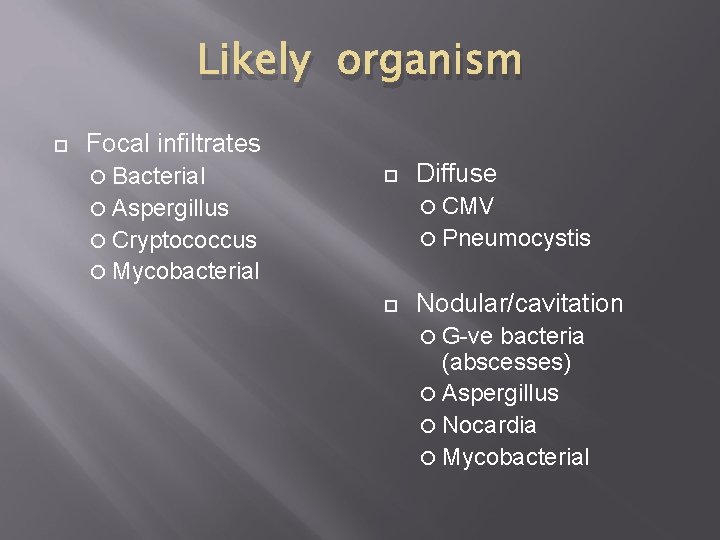
Likely organism Focal infiltrates Bacterial Diffuse Aspergillus CMV Cryptococcus Pneumocystis Mycobacterial Nodular/cavitation G-ve bacteria (abscesses) Aspergillus Nocardia Mycobacterial
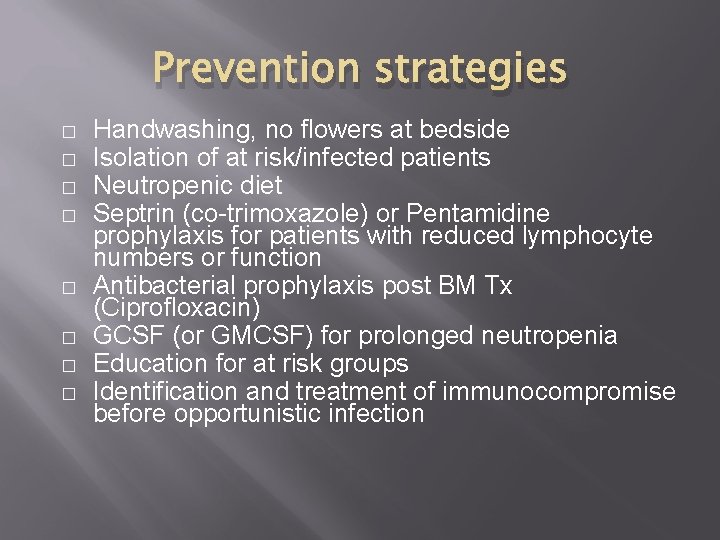
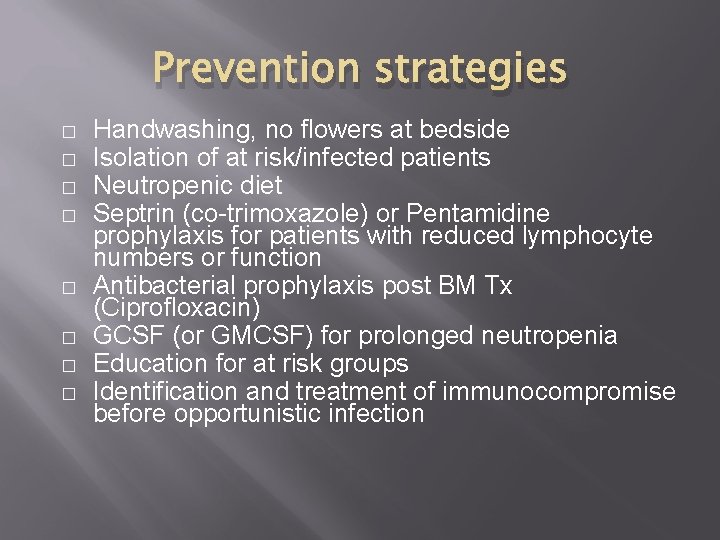
Prevention strategies � � � � Handwashing, no flowers at bedside Isolation of at risk/infected patients Neutropenic diet Septrin (co-trimoxazole) or Pentamidine prophylaxis for patients with reduced lymphocyte numbers or function Antibacterial prophylaxis post BM Tx (Ciprofloxacin) GCSF (or GMCSF) for prolonged neutropenia Education for at risk groups Identification and treatment of immunocompromise before opportunistic infection
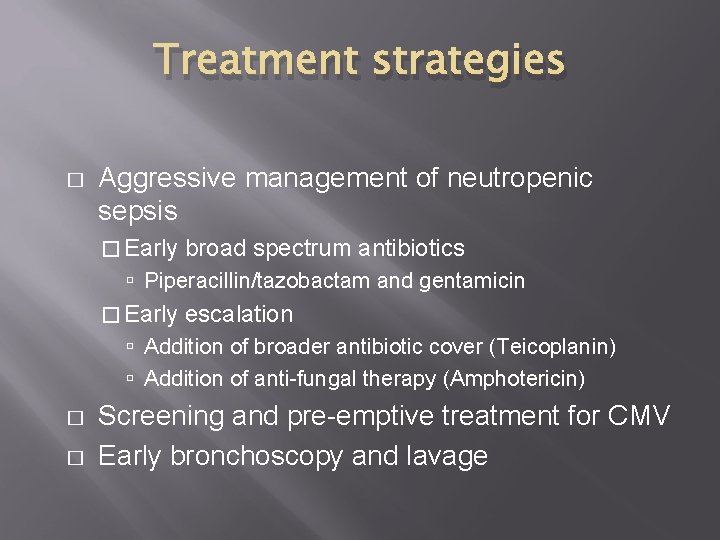
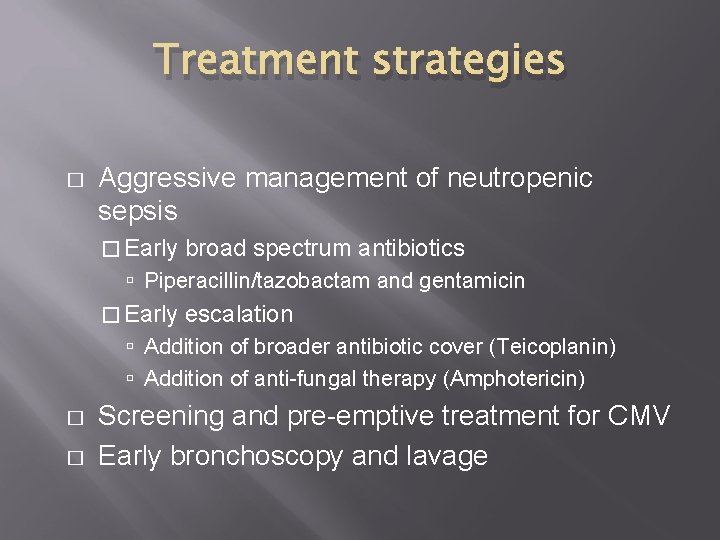
Treatment strategies � Aggressive management of neutropenic sepsis � Early broad spectrum antibiotics Piperacillin/tazobactam and gentamicin � Early escalation Addition of broader antibiotic cover (Teicoplanin) Addition of anti-fungal therapy (Amphotericin) � � Screening and pre-emptive treatment for CMV Early bronchoscopy and lavage
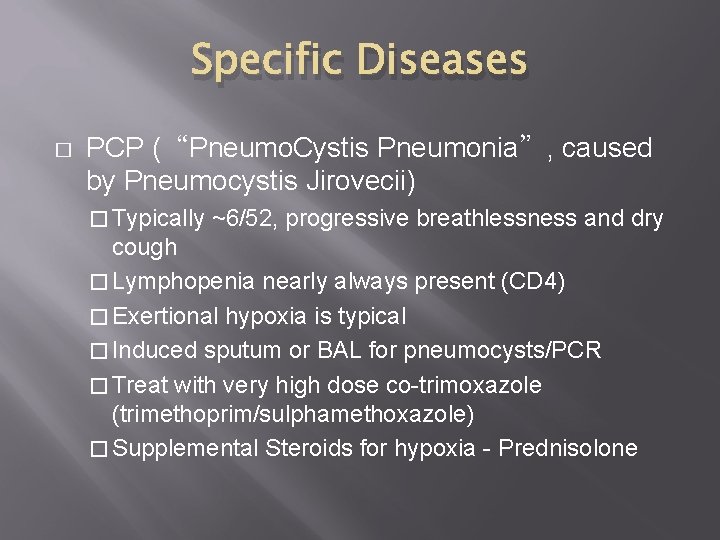
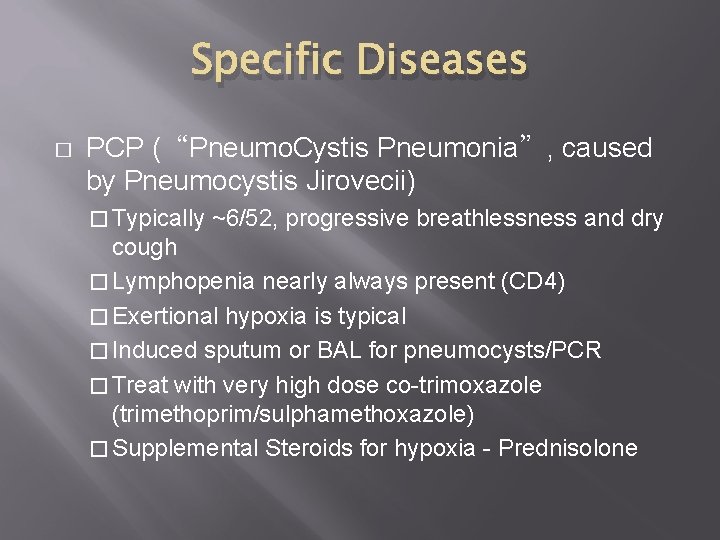
Specific Diseases � PCP (“Pneumo. Cystis Pneumonia”, caused by Pneumocystis Jirovecii) � Typically ~6/52, progressive breathlessness and dry cough � Lymphopenia nearly always present (CD 4) � Exertional hypoxia is typical � Induced sputum or BAL for pneumocysts/PCR � Treat with very high dose co-trimoxazole (trimethoprim/sulphamethoxazole) � Supplemental Steroids for hypoxia - Prednisolone
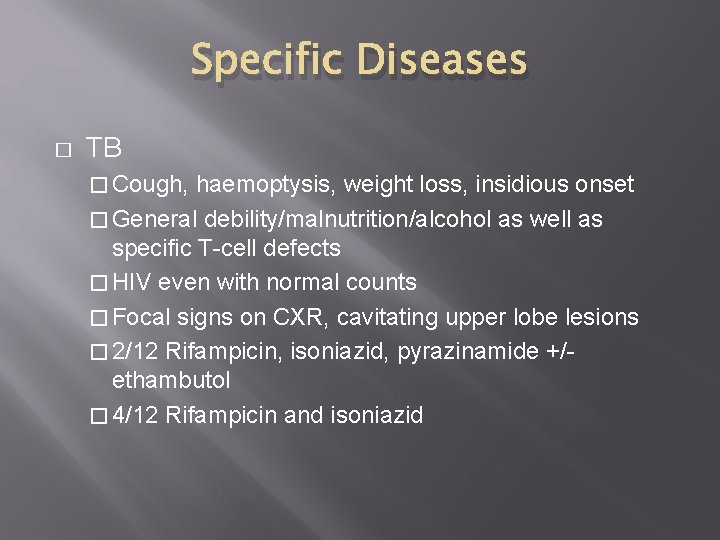
Specific Diseases � TB � Cough, haemoptysis, weight loss, insidious onset � General debility/malnutrition/alcohol as well as specific T-cell defects � HIV even with normal counts � Focal signs on CXR, cavitating upper lobe lesions � 2/12 Rifampicin, isoniazid, pyrazinamide +/ethambutol � 4/12 Rifampicin and isoniazid
Specific Diseases � Invasive Aspergillosis � Fever in neutropenic patient, usually on broad spectrum antibiotics � Multiple pulmonary nodules or infiltrates � Characteristic appearance on CT � Rx Amphotericin (Renal toxicity) Caspofungin Liposomal Amphotericin
Management � � � Culture – blood, urine, sputum Serology – CMV, legionella Imaging � CXR, diffuse vs focal infiltrates � High resolution CT scan � Identification of pathogen � Induced sputum – nebulised hypertonic saline � Bronchoscopy and lavage
Fibreoptic Bronchoscopy
Specific Treatments � � � PCP – high dose iv Septrin (Co-trimoxazole), +/ - Prednisolone Bacterial – broad spectrum, guided by laboratory sensitivity Fungal infection � Amphotericin, � caspofungin, Voriconazole Viral infection � CMV - ganciclovir or foscarnet � RSV – ribovirin � HSV – acyclovir, valcyclovir � VZV – acyclovir, valcyclovir
Summary � � Pulmonary infection is a life threatening complication of immunocompromise of any cause Early identification of the pathogen is important in reducing unnecessary treatment, identifying resistant organisms, and is associated with improved outcomes