The Language of Fractures How to describe that
The Language of Fractures How to describe that fracture! JOEL L. RUSH, D. O. Clinical Professor Orthopedics Nova Southeastern University Kiran C. Patel College of Osteopathic Medicine Program Director Broward Health Medical Center Orthopaedic Residency 1
Disclosures I have no disclosures 2
The Language of Fractures 3

How do I even think to describe this? ? ?
When looking at an x-ray of a fracture, to be able to describe what you see to, you need to create a brief, clear, concise sentence. Think of describing a scene or a place to someone who has never been there. Give them the opportunity to create a good mental image. 5

“I have a closed distal third displaced, comminuted fracture of a right tibia and fibula with 350 lateral and posterior angulation” So what are all these terms? 6
BASIC FRACTURE DESCRIPTION 7
What is a Fracture? Complete or incomplete break in the continuity of bone or cartilage When a fracture occurs into a joint, the overlying cartilage will also break. 8
A Fracture Can Be: Closed Open 9
Closed Fracture Skin and soft tissue overlying the fracture are intact there is no communication from the fracture to the outside world You may have a laceration of the skin over or near where the fracture is, but if there is no pathway though the underlying soft tissue to the fracture, it is not open. 10

Open Fracture The fracture site communicates with the outside environment This may be from a small pin hole to massive skin loss It is not always easy to determine if the fracture is open or not if there is just a small opening. Those are the times you may need to probe the opening with something sterile and feel if the opening tracks to the bone. 11

Open: Open From Within Bone pushes from inside out Some are easy to determine. 12
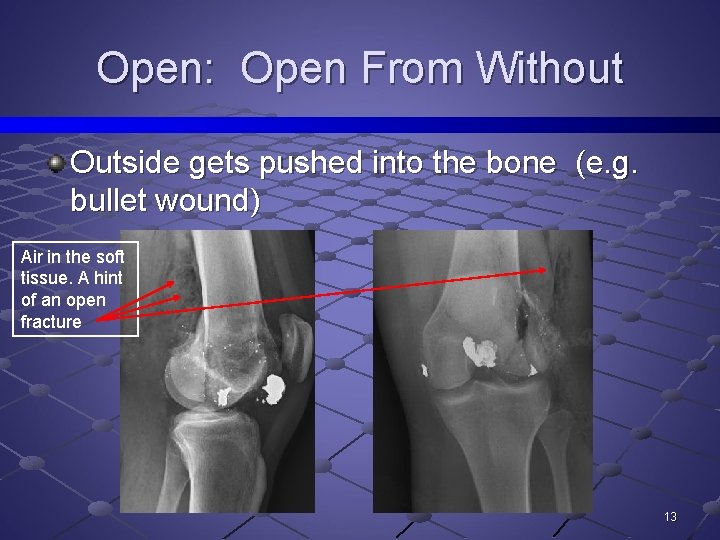
Open: Open From Without Outside gets pushed into the bone (e. g. bullet wound) Air in the soft tissue. A hint of an open fracture 13
Note: Once the skin is broken, any fracture that is exposed to the outside environment is an open fracture. The determination of an open versus closed fracture becomes important in the timing of treatment. An open fracture will need to go to the operating room to irrigate and debride the open fracture area to lessen the risk of infection. A closed fracture may only need to be closed reduced and splinted and not need to be brought to the operating room to do so. 14
Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990
A Fracture Can Be: Complete Incomplete 16
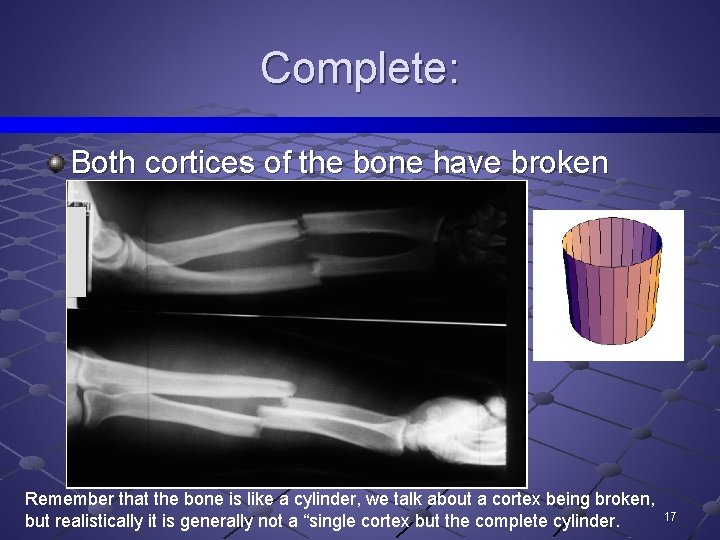
Complete: Both cortices of the bone have broken Remember that the bone is like a cylinder, we talk about a cortex being broken, but realistically it is generally not a “single cortex but the complete cylinder. 17
Incomplete: Only one cortex has been broken Two types 1. Greenstick 2. Torus In children, it is possible for only one cortex to be broken. In adults, a stress fracture (discussed later) can appear as an incomplete fracture. 18
Incomplete: Greenstick Incomplete fracture causing bowing of bone Break occurs on the outer convex (tension) side of fracture Think of a stick from a young tree. The stick has a higher water content. When you try to break that young greenstick, it bends more than breaks. . 19
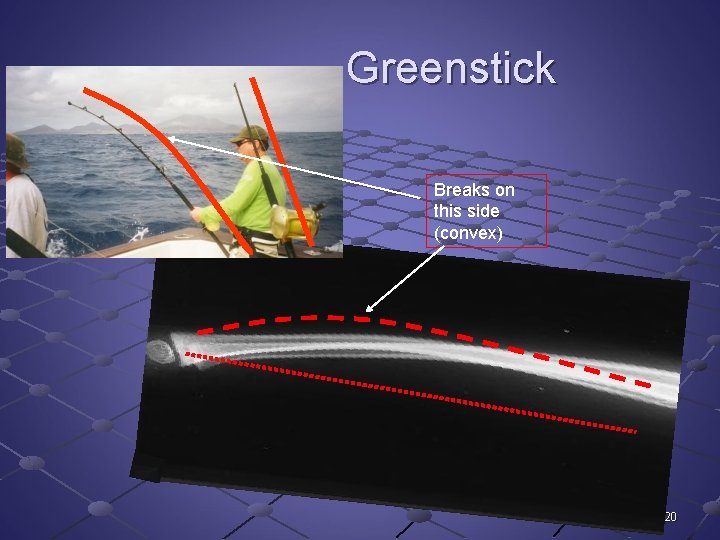
Greenstick Breaks on this side (convex) 20
Incomplete: Torus Incomplete fracture with buckling of cortex Caused by compression forces Think of an earthquake causing the earth to push up and make the mountains. 21
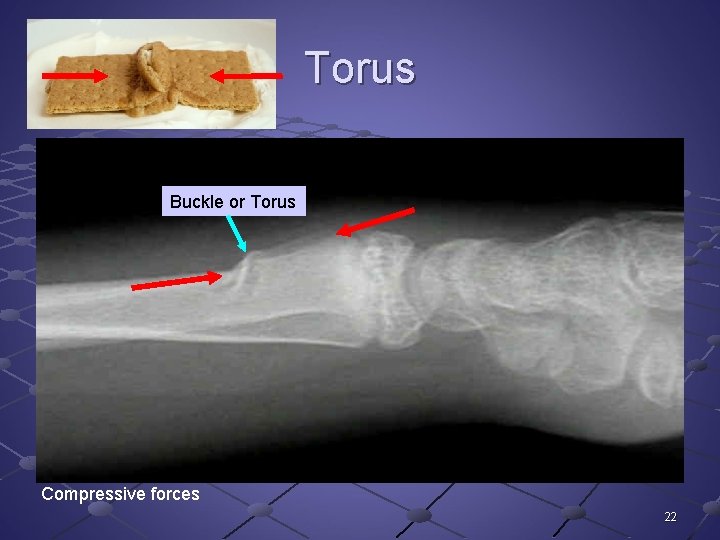
Torus Buckle or Torus Compressive forces 22
Incomplete: Greenstick & torus fractures occur in children due to their “softer” more woven bone versus more “dense” lamellar bone. 23
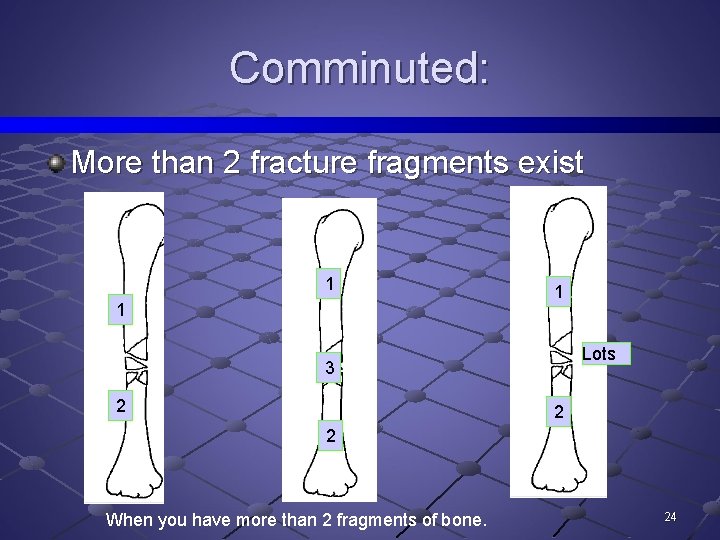
Comminuted: More than 2 fracture fragments exist 1 1 1 Lots 3 2 2 2 When you have more than 2 fragments of bone. 24
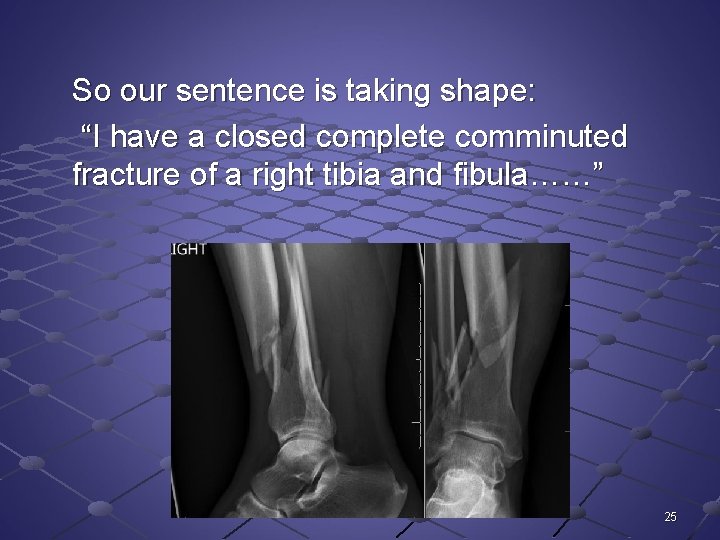
So our sentence is taking shape: “I have a closed complete comminuted fracture of a right tibia and fibula……” 25
What else can help us describe what we are seeing? How about the direction of the fracture lines? 26
Direction of Fracture Lines: Transverse Oblique Spiral Comminuted 27
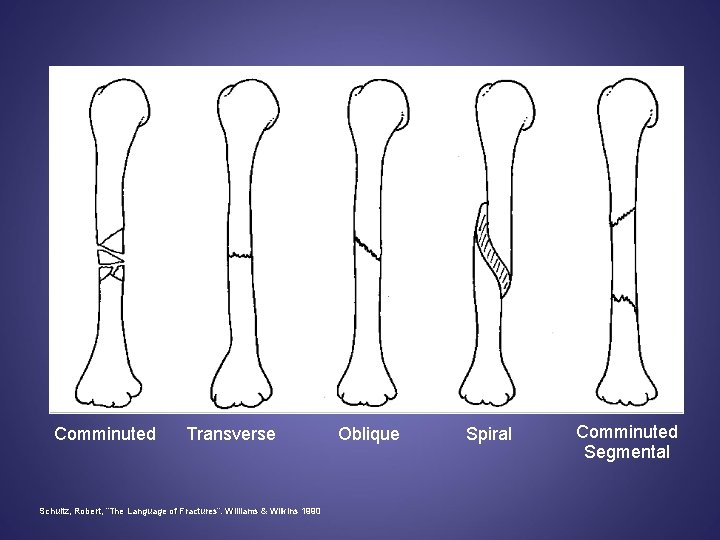
Comminuted Transverse Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990 Oblique Spiral Comminuted Segmental
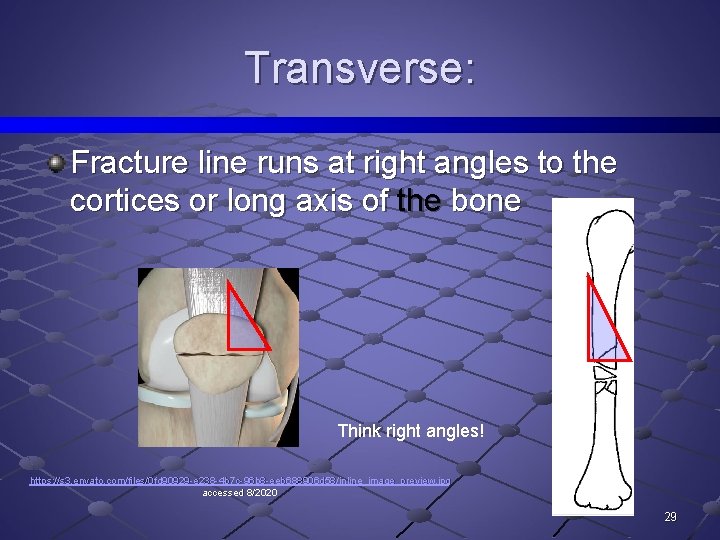
Transverse: Fracture line runs at right angles to the cortices or long axis of the bone Think right angles! https: //s 3. envato. com/files/0 fd 90929 -e 238 -4 b 7 c-96 b 8 -eeb 688906 d 58/inline_image_preview. jpg accessed 8/2020 29

Oblique: Fracture line runs obliquely (at an angle) to long axis of the bone 31
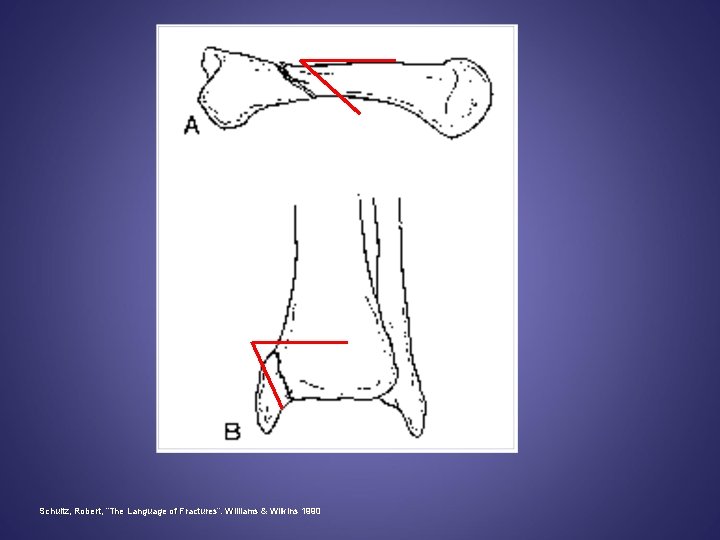
Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990
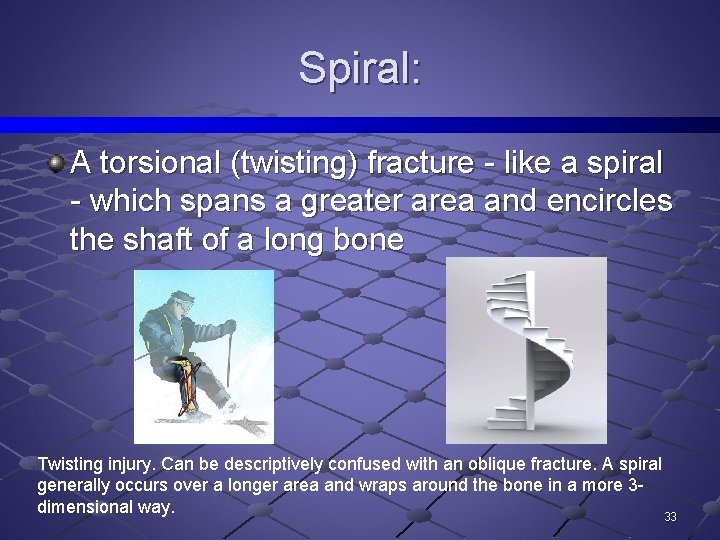
Spiral: A torsional (twisting) fracture - like a spiral - which spans a greater area and encircles the shaft of a long bone Twisting injury. Can be descriptively confused with an oblique fracture. A spiral generally occurs over a longer area and wraps around the bone in a more 3 dimensional way. 33
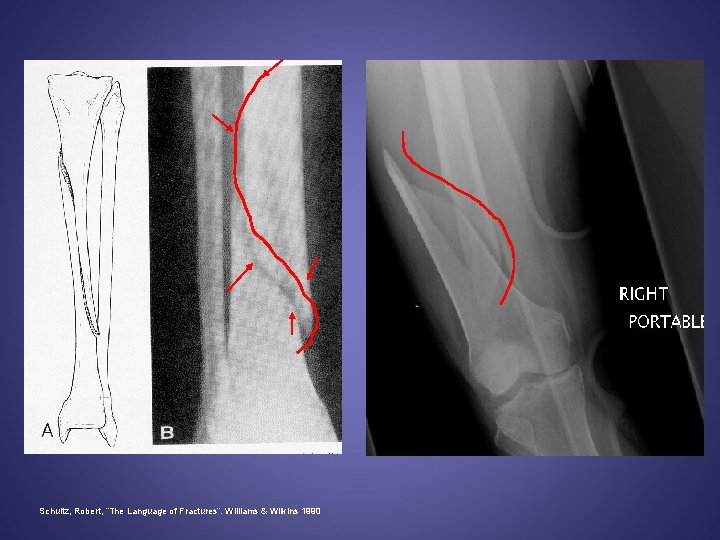
Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990
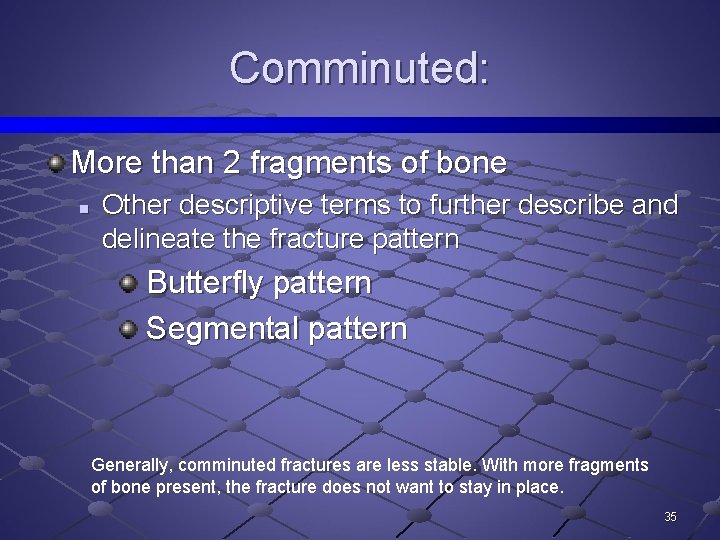
Comminuted: More than 2 fragments of bone n Other descriptive terms to further describe and delineate the fracture pattern Butterfly pattern Segmental pattern Generally, comminuted fractures are less stable. With more fragments of bone present, the fracture does not want to stay in place. 35
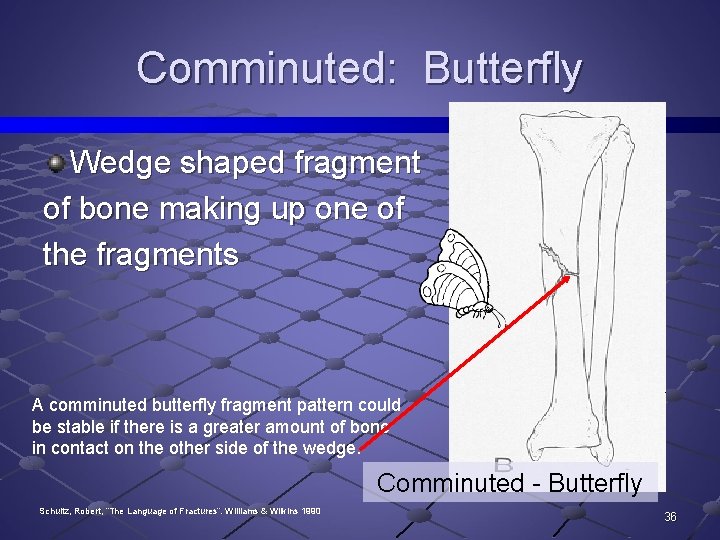
Comminuted: Butterfly Wedge shaped fragment of bone making up one of the fragments A comminuted butterfly fragment pattern could be stable if there is a greater amount of bone in contact on the other side of the wedge. Comminuted - Butterfly Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990 36
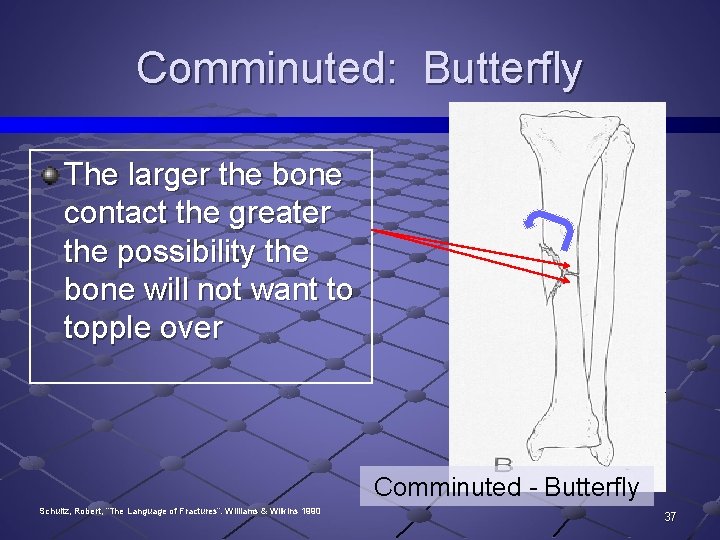
Comminuted: Butterfly The larger the bone contact the greater the possibility the bone will not want to topple over Comminuted - Butterfly Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990 37
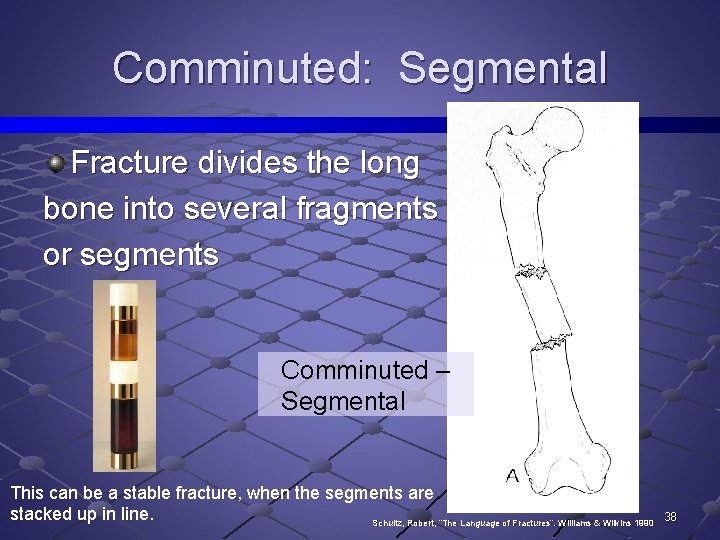
Comminuted: Segmental Fracture divides the long bone into several fragments or segments Comminuted – Segmental This can be a stable fracture, when the segments are stacked up in line. Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990 38
So our sentence is getting a bit longer: “I have a closed, complete, comminuted, spiral fracture of a right tibia and fibula……” 39
What Is Else Is Occurring At The Fracture? 40
What Else Is Occurring at the Fracture: Intraarticular Distraction Impaction Avulsion Depression Compression 41
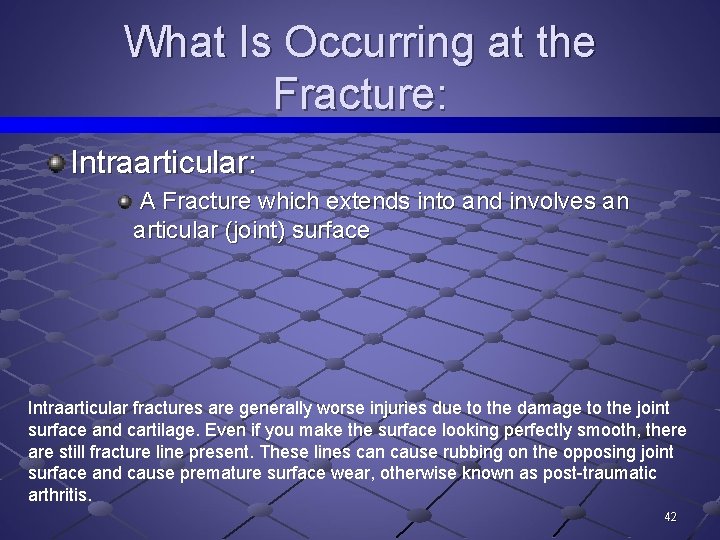
What Is Occurring at the Fracture: Intraarticular: A Fracture which extends into and involves an articular (joint) surface Intraarticular fractures are generally worse injuries due to the damage to the joint surface and cartilage. Even if you make the surface looking perfectly smooth, there are still fracture line present. These lines can cause rubbing on the opposing joint surface and cause premature surface wear, otherwise known as post-traumatic arthritis. 42
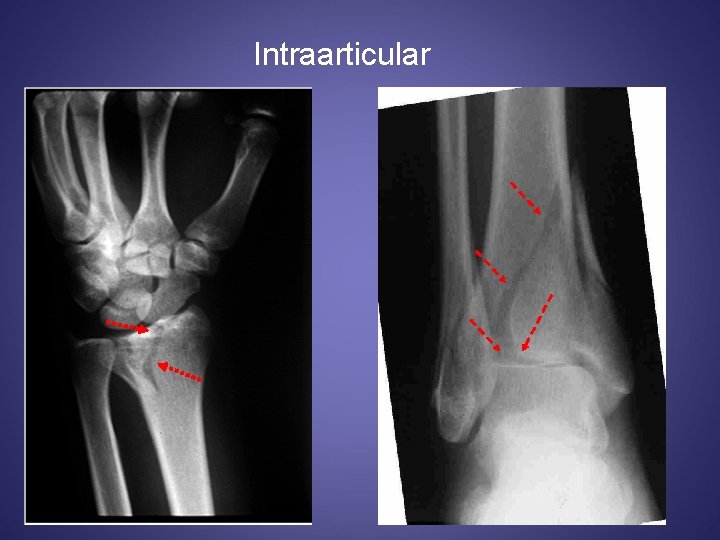
Intraarticular
What Else Is Occurring at the Fracture: Distraction: When opposing ends of the fracture fragments are kept apart from each other resulting from muscle pull, excessive traction on the fracture, or due to interposed tissue 44
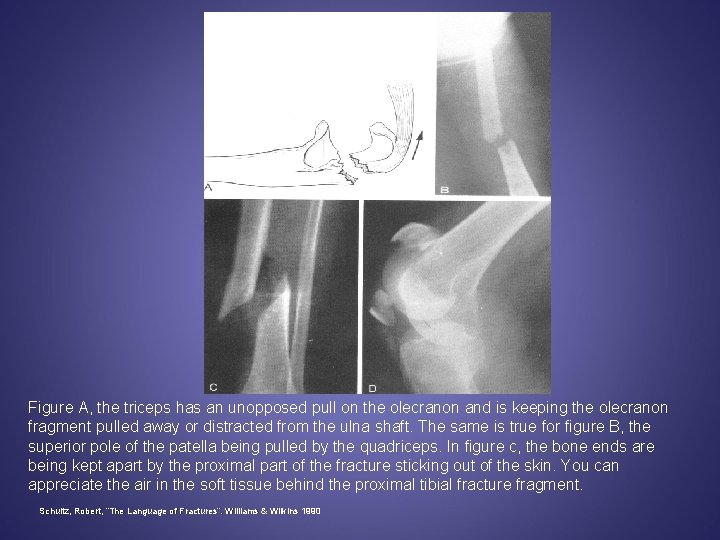
Figure A, the triceps has an unopposed pull on the olecranon and is keeping the olecranon fragment pulled away or distracted from the ulna shaft. The same is true for figure B, the superior pole of the patella being pulled by the quadriceps. In figure c, the bone ends are being kept apart by the proximal part of the fracture sticking out of the skin. You can appreciate the air in the soft tissue behind the proximal tibial fracture fragment. Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990
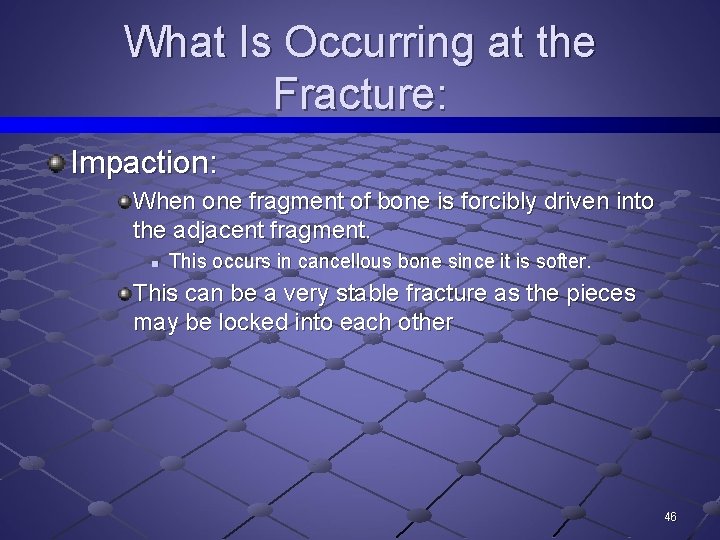
What Is Occurring at the Fracture: Impaction: When one fragment of bone is forcibly driven into the adjacent fragment. n This occurs in cancellous bone since it is softer. This can be a very stable fracture as the pieces may be locked into each other 46

Impaction: Note: Fractures are impacted NOT compacted Garbage is compacted 47
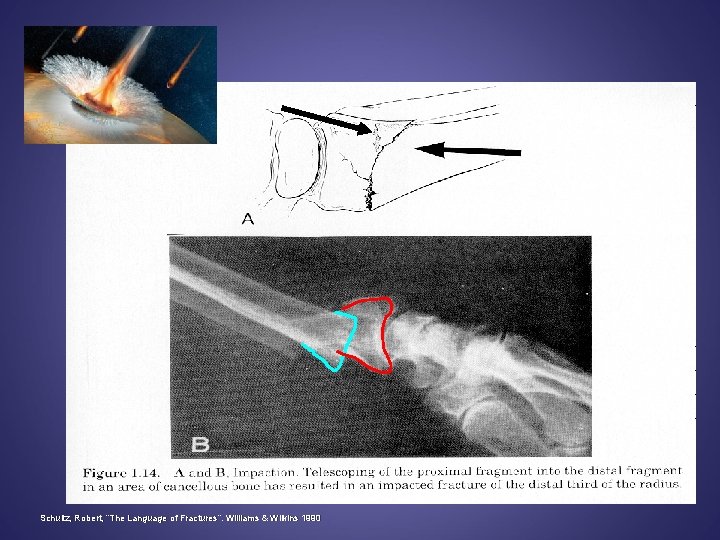
Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990
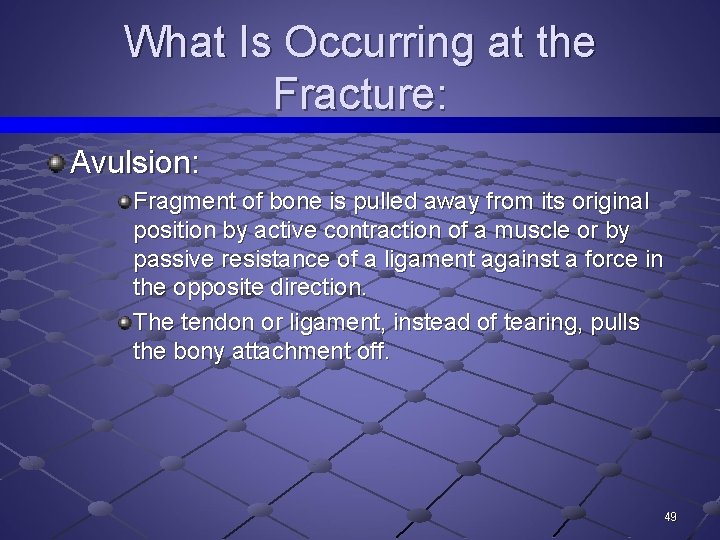
What Is Occurring at the Fracture: Avulsion: Fragment of bone is pulled away from its original position by active contraction of a muscle or by passive resistance of a ligament against a force in the opposite direction. The tendon or ligament, instead of tearing, pulls the bony attachment off. 49
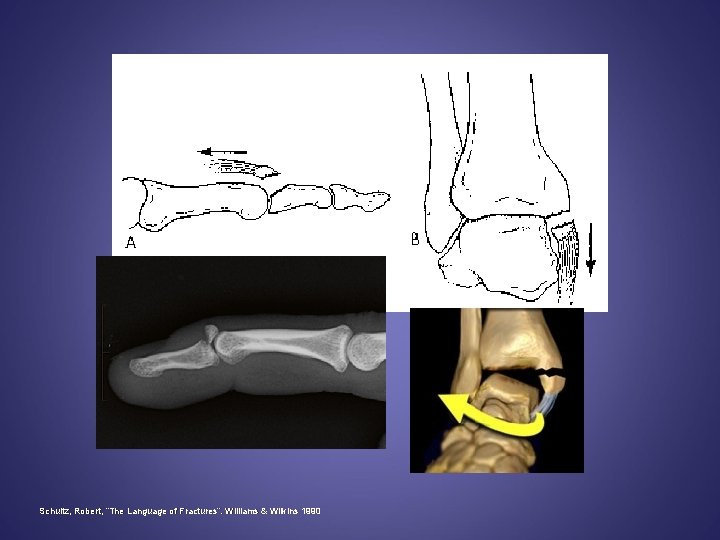
Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990
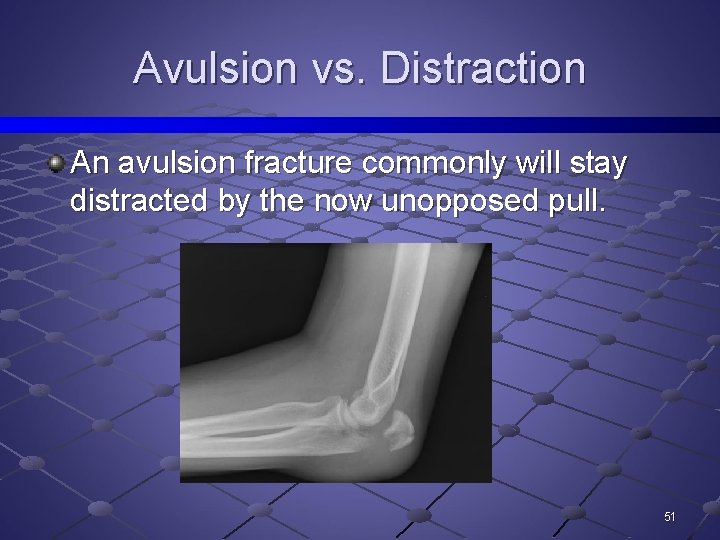
Avulsion vs. Distraction An avulsion fracture commonly will stay distracted by the now unopposed pull. 51
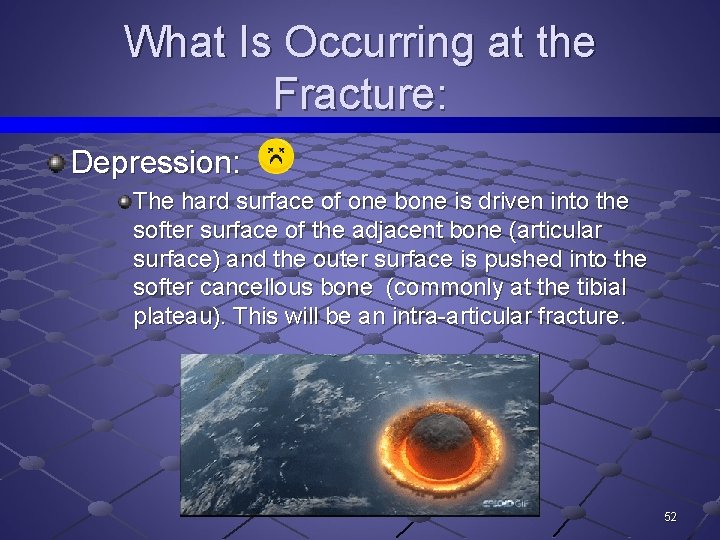
What Is Occurring at the Fracture: Depression: The hard surface of one bone is driven into the softer surface of the adjacent bone (articular surface) and the outer surface is pushed into the softer cancellous bone (commonly at the tibial plateau). This will be an intra-articular fracture. 52
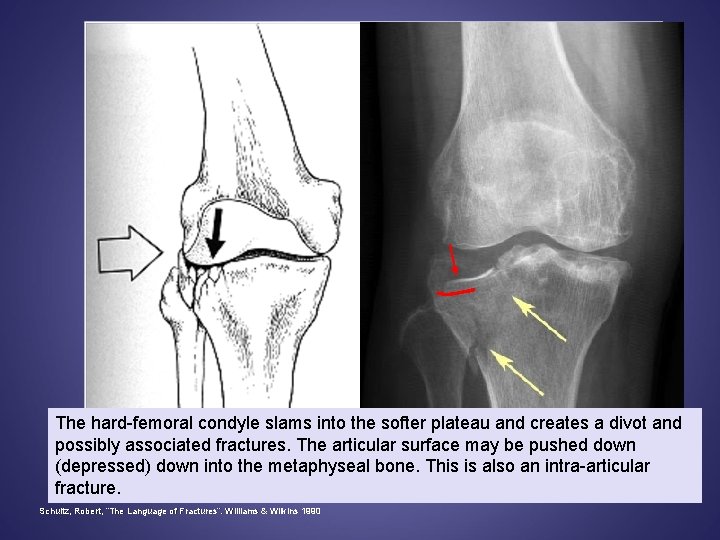
The hard-femoral condyle slams into the softer plateau and creates a divot and possibly associated fractures. The articular surface may be pushed down (depressed) down into the metaphyseal bone. This is also an intra-articular fracture. Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990
What Is Occurring at the Fracture: Compression: In vertebral bodies where the superior and inferior surfaces are driven toward each other producing a wedge shape of varying degrees and extent of compression is described in terms of percent of loss of height as compared to adjacent vertebrae. 54
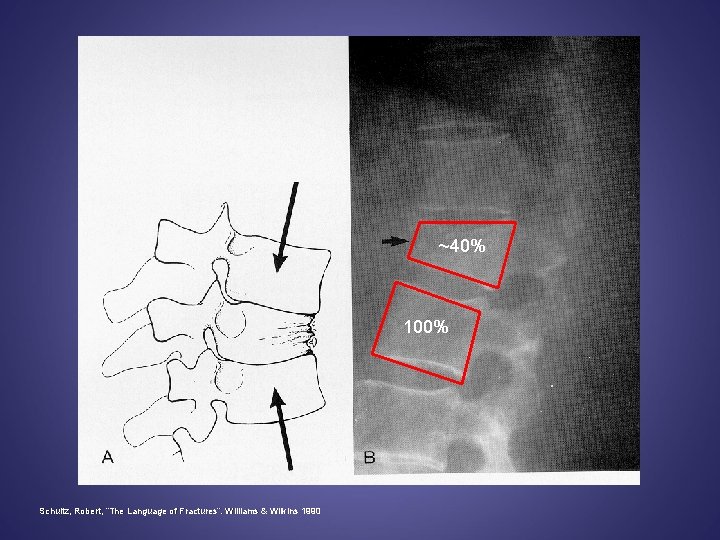
~40% 100% Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990
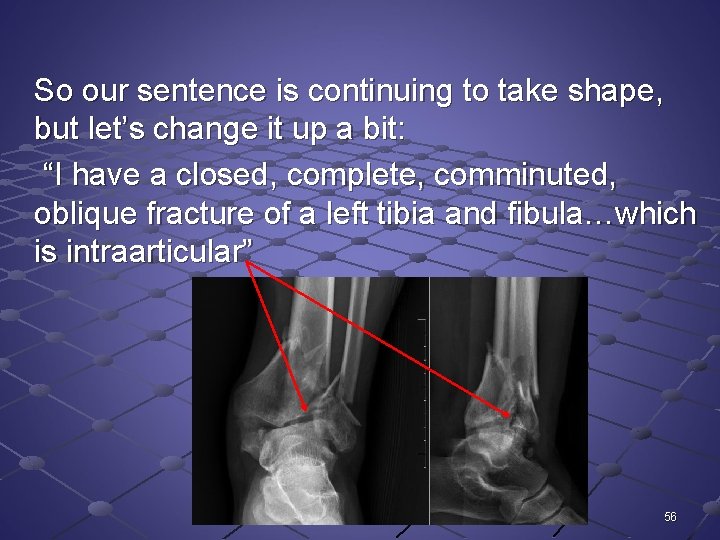
So our sentence is continuing to take shape, but let’s change it up a bit: “I have a closed, complete, comminuted, oblique fracture of a left tibia and fibula…which is intraarticular” 56
Location Of Fracture 57
Location of Fracture: Reference points must be established to be able to give a location. Where in the bone is the fracture occurring. 58
Location of Fracture: A long bone is divided into THIRDS: proximal, middle, and distal If the fracture occurs at junction points or points of overlap, the area then becomes described as "junction of mid to distal third" or "junction of proximal to mid third. " 59
Location of Fracture: If the fracture occurs in the middle it is referred to as "midshaft. " 60
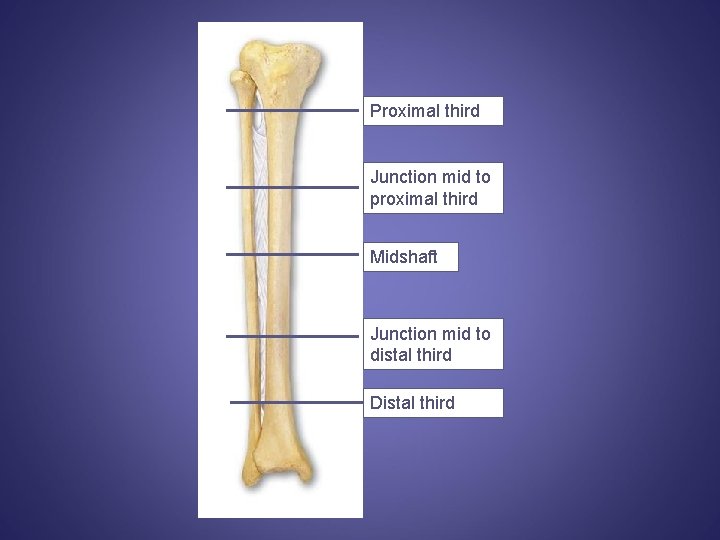
Proximal third Junction mid to proximal third Midshaft Junction mid to distal third Distal third
Location of Fracture: Specific bones or areas can be described by their specific locations: n E. G. Medial malleolus, femoral neck, intertrochanteric, superior or inferior pubic ramus 62
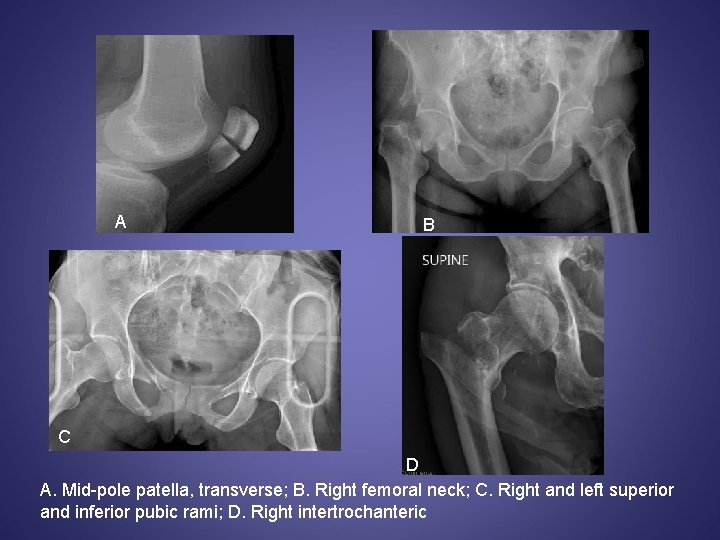
A B C D A. Mid-pole patella, transverse; B. Right femoral neck; C. Right and left superior and inferior pubic rami; D. Right intertrochanteric
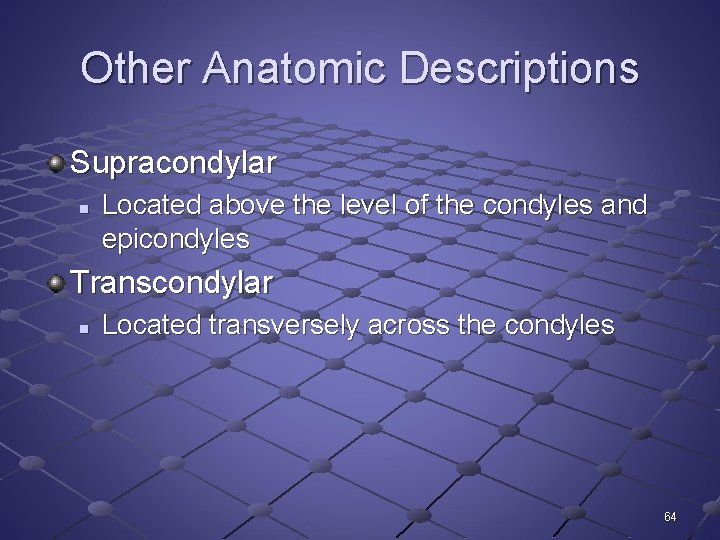
Other Anatomic Descriptions Supracondylar n Located above the level of the condyles and epicondyles Transcondylar n Located transversely across the condyles 64
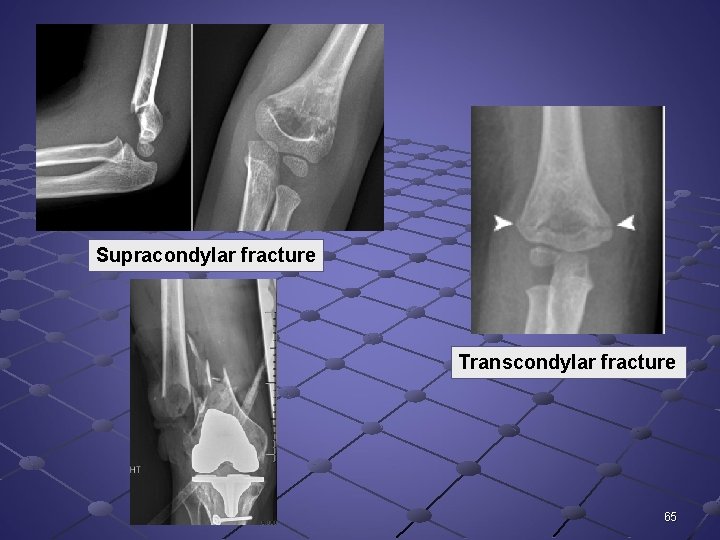
Supracondylar fracture Transcondylar fracture 65
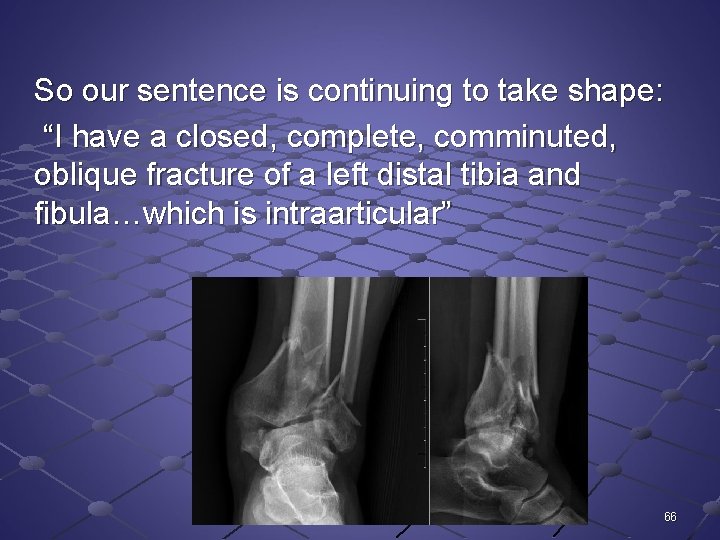
So our sentence is continuing to take shape: “I have a closed, complete, comminuted, oblique fracture of a left distal tibia and fibula…which is intraarticular” 66
Position And Alignment What else is occurring at the fracture? 67
Position: Relationship of fragments to the normal anatomic structure n Are the pieces out of normal position? 68
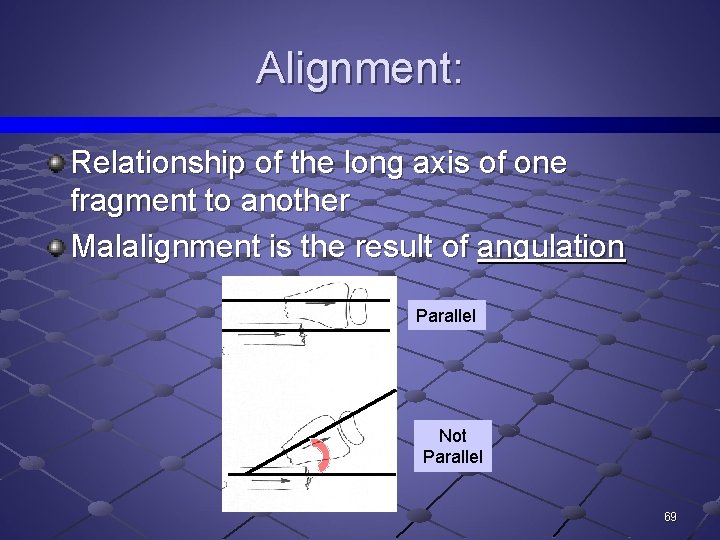
Alignment: Relationship of the long axis of one fragment to another Malalignment is the result of angulation Parallel Not Parallel 69
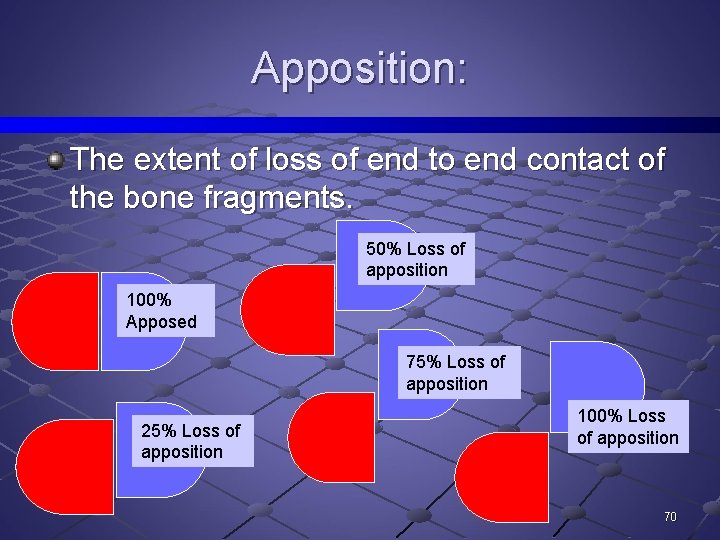
Apposition: The extent of loss of end to end contact of the bone fragments. 50% Loss of apposition 100% Apposed 75% Loss of apposition 25% Loss of apposition 100% Loss of apposition 70
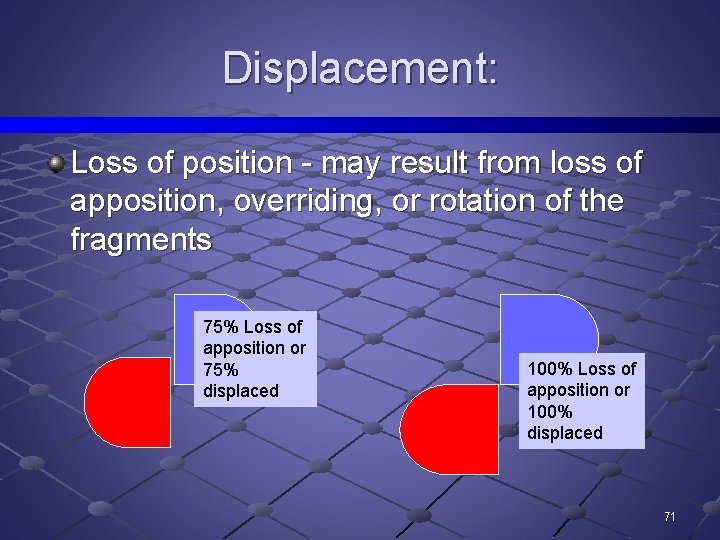
Displacement: Loss of position - may result from loss of apposition, overriding, or rotation of the fragments 75% Loss of apposition or 75% displaced 100% Loss of apposition or 100% displaced 71
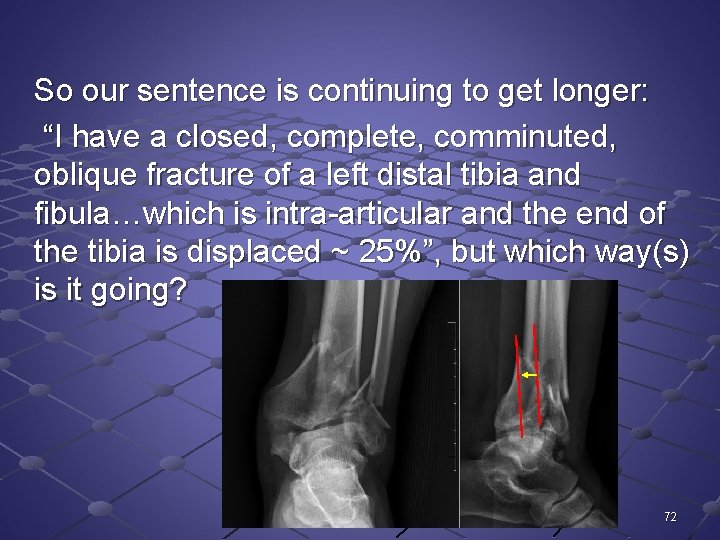
So our sentence is continuing to get longer: “I have a closed, complete, comminuted, oblique fracture of a left distal tibia and fibula…which is intra-articular and the end of the tibia is displaced ~ 25%”, but which way(s) is it going? 72
Direction Of Angulation 73
Describe Angulation By One of 2 Ways: 1. The angle the distal fracture fragment makes in relation to the proximal fragment expressed in number of degrees OR 74
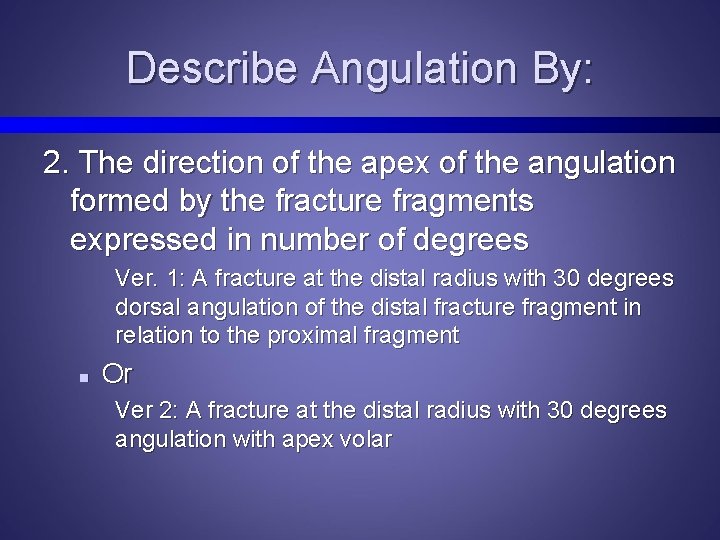
Describe Angulation By: 2. The direction of the apex of the angulation formed by the fracture fragments expressed in number of degrees Ver. 1: A fracture at the distal radius with 30 degrees dorsal angulation of the distal fracture fragment in relation to the proximal fragment n Or Ver 2: A fracture at the distal radius with 30 degrees angulation with apex volar
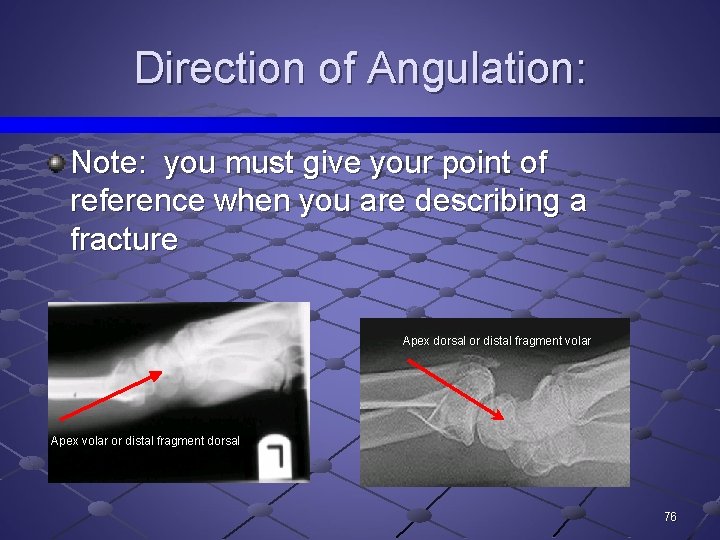
Direction of Angulation: Note: you must give your point of reference when you are describing a fracture Apex dorsal or distal fragment volar Apex volar or distal fragment dorsal 76
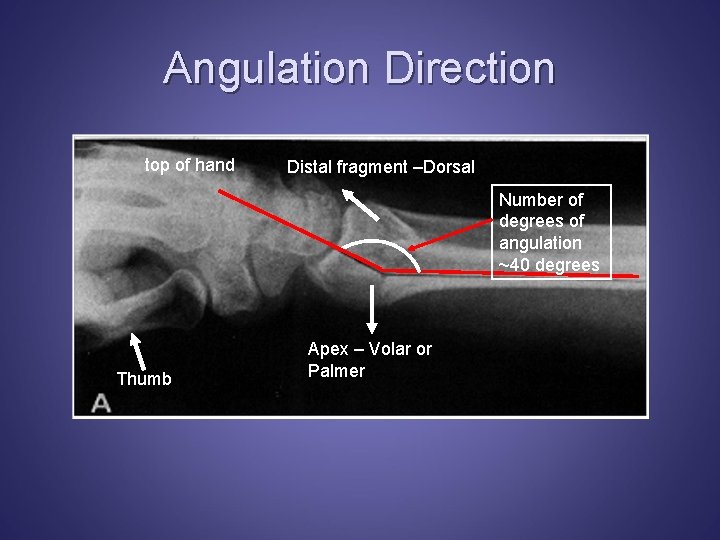
Angulation Direction top of hand Distal fragment –Dorsal Number of degrees of angulation ~40 degrees Thumb Apex – Volar or Palmer
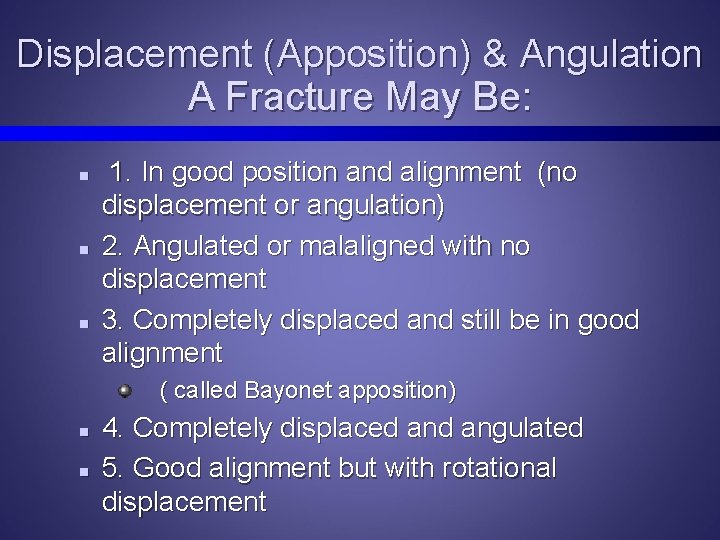
Displacement (Apposition) & Angulation A Fracture May Be: n n n 1. In good position and alignment (no displacement or angulation) 2. Angulated or malaligned with no displacement 3. Completely displaced and still be in good alignment ( called Bayonet apposition) n n 4. Completely displaced angulated 5. Good alignment but with rotational displacement
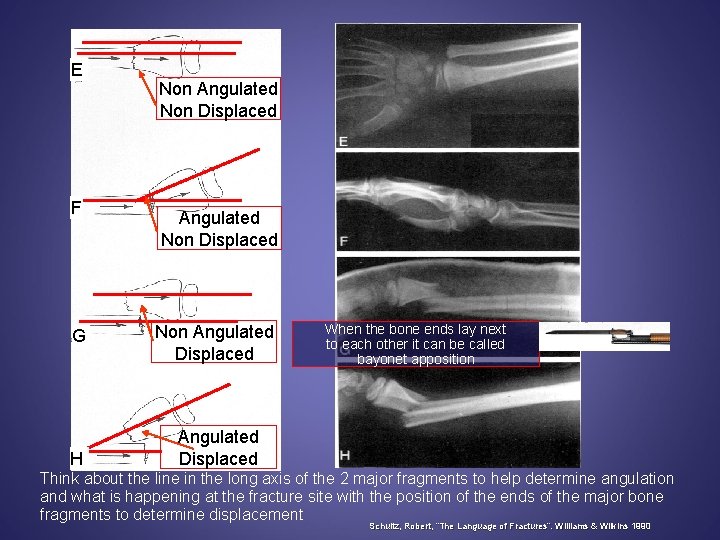
E F G H Non Angulated Non Displaced Non Angulated Displaced When the bone ends lay next to each other it can be called bayonet apposition Angulated Displaced Think about the line in the long axis of the 2 major fragments to help determine angulation and what is happening at the fracture site with the position of the ends of the major bone fragments to determine displacement Schultz, Robert, “The Language of Fractures”. Williams & Wilkins 1990
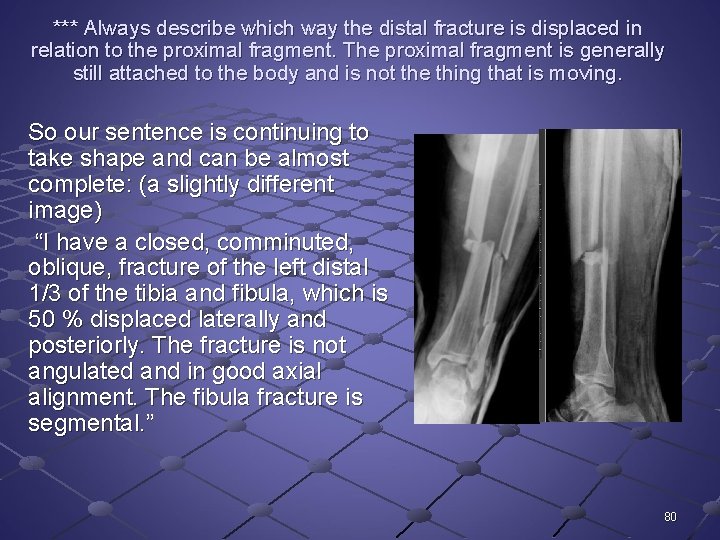
*** Always describe which way the distal fracture is displaced in relation to the proximal fragment. The proximal fragment is generally still attached to the body and is not the thing that is moving. So our sentence is continuing to take shape and can be almost complete: (a slightly different image) “I have a closed, comminuted, oblique, fracture of the left distal 1/3 of the tibia and fibula, which is 50 % displaced laterally and posteriorly. The fracture is not angulated and in good axial alignment. The fibula fracture is segmental. ” 80
Other Terms: Subluxation Dislocation Diastasis 81
Subluxation: Partial loss of continuity between two opposing joint surfaces Always describe the direction of the subluxation by what the distal part is doing in relation to the proximal part. 82

Normal Abnormal Not completely out of the joint. Think about how to describe this.
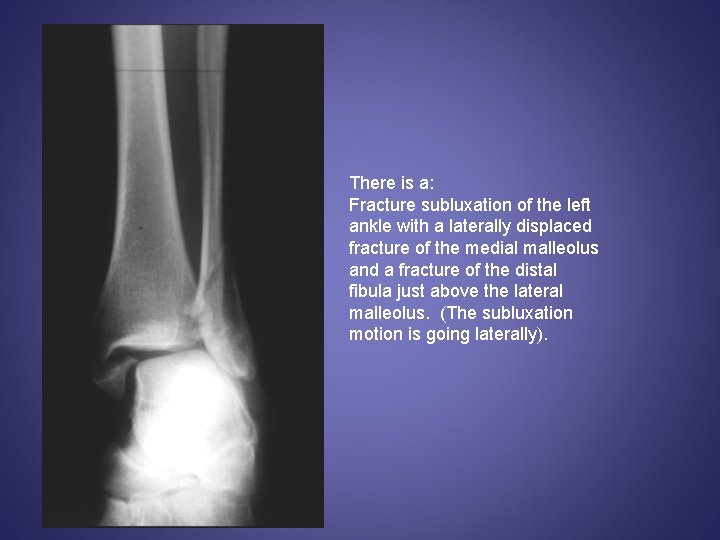
There is a: Fracture subluxation of the left ankle with a laterally displaced fracture of the medial malleolus and a fracture of the distal fibula just above the lateral malleolus. (The subluxation motion is going laterally).
Dislocation: Complete loss of continuity between two opposing joint surfaces Always describe the direction of the dislocation by what the distal part is doing in relation to the proximal part. 85
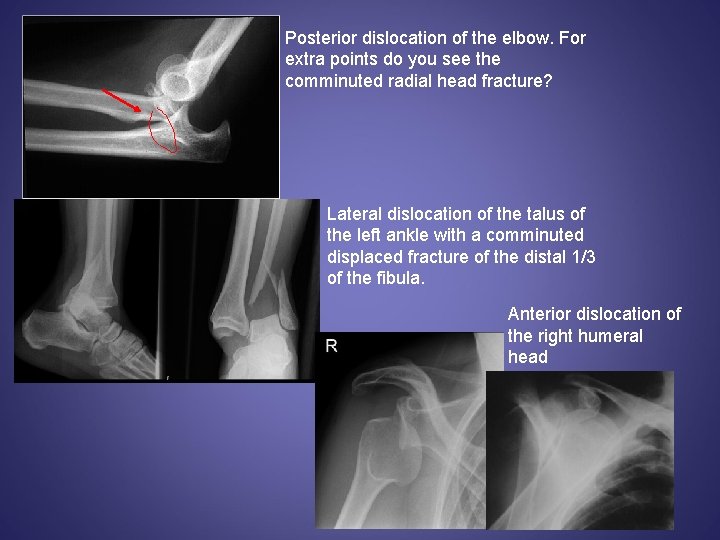
Posterior dislocation of the elbow. For extra points do you see the comminuted radial head fracture? Lateral dislocation of the talus of the left ankle with a comminuted displaced fracture of the distal 1/3 of the fibula. Anterior dislocation of the right humeral head
Diastasis: Separation of normally joined parts n E. G. Pubic symphysis or syndesmotic ligament 87

diastasis
Stress Fracture: Fatigue fracture resulting from repeated trivial trauma. It may be complete or incomplete. 89
Fracture Union Terms: Delayed union Nonunion Pseudoarthrosis Malunion 90
Fracture Union Delayed union: n n Failure of fracture to unite in the time usually required for union to occur Expect fracture to eventually heal but taking longer then usual 91
Fracture Union Nonunion: n Failure of the fracture fragments to unite; the process of bone repair has ceased 92

Fracture Union Pseudoarthrosis: n False joint of dense fibrous of fibrocartilaginous tissue which forms between the two fracture fragments 94
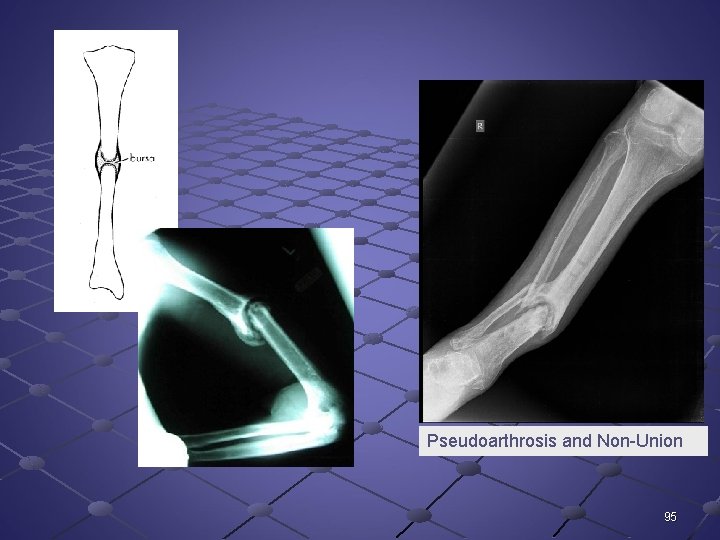
Pseudoarthrosis and Non-Union 95
Fracture Union Malunion: n Union to the fracture with angulation or rotation deformity 96
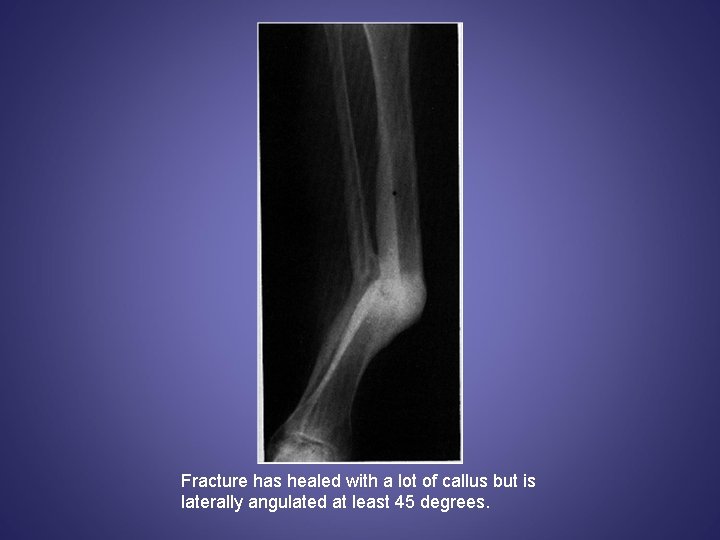
Fracture has healed with a lot of callus but is laterally angulated at least 45 degrees.
There are special descriptors we use when describing fractures which involve the growth plate in children. 98
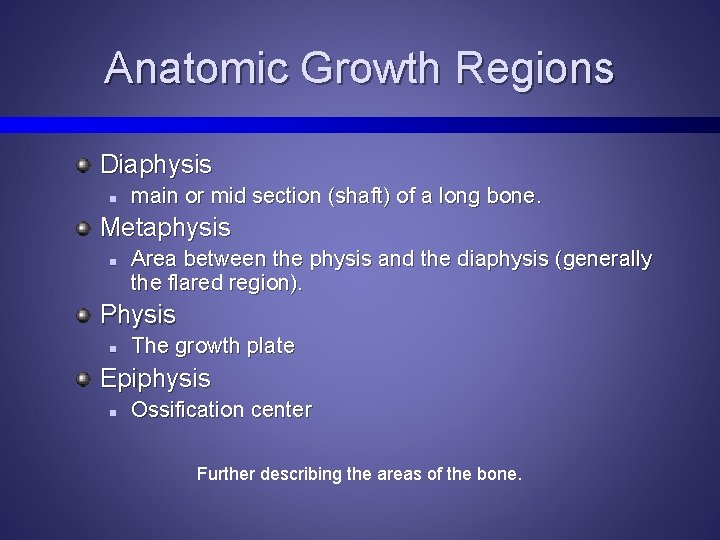
Anatomic Growth Regions Diaphysis n main or mid section (shaft) of a long bone. Metaphysis n Area between the physis and the diaphysis (generally the flared region). Physis n The growth plate Epiphysis n Ossification center Further describing the areas of the bone.
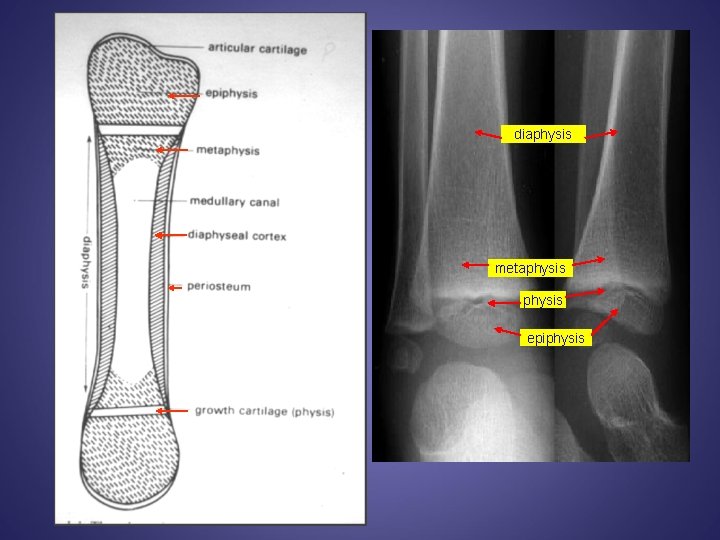
diaphysis metaphysis epiphysis
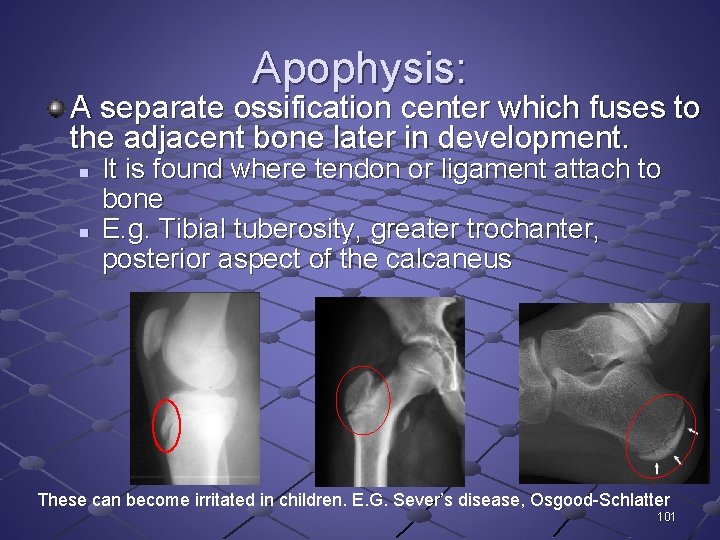
Apophysis: A separate ossification center which fuses to the adjacent bone later in development. n n It is found where tendon or ligament attach to bone E. g. Tibial tuberosity, greater trochanter, posterior aspect of the calcaneus These can become irritated in children. E. G. Sever’s disease, Osgood-Schlatter 101
Classification of Physeal Fractures Salter-Harris classification – Ia. V: n n I. Epiphysis is completely separated from the metaphysis without any x-ray evidence of a metaphyseal fragment II. Fracture plane travels transversely across the physis before exiting through the metaphysis Robert B Salter and W Robert Harris in 1963 How to describe kid’s fractures. The classification was developed to help predict the potential of premature physeal closure. 102
Classification of Physeal Fractures Salter-Harris classification: n n n III. Fracture plane travels transversely across the physis before exiting through the epiphysis IV. Vertical splitting injury crossing both the epiphyseal and metaphyseal regions V. Severe crushing injury to the physis 103
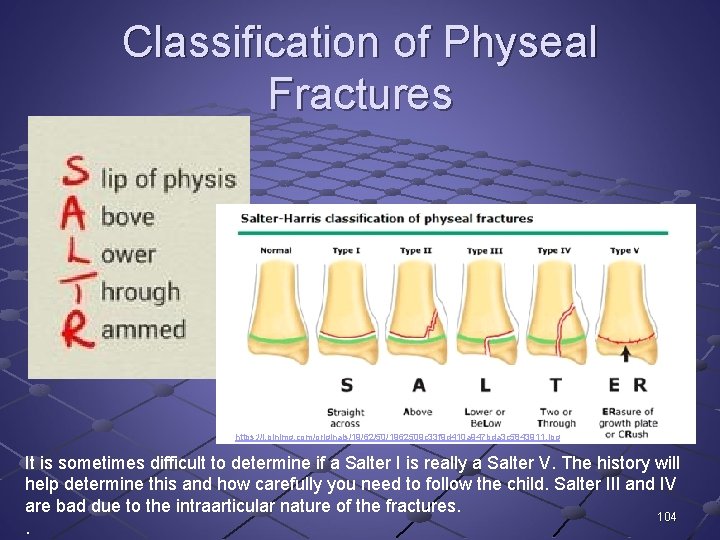
Classification of Physeal Fractures https: //i. pinimg. com/originals/19/62/50/1962509 c 33 f 9 d 410 a 947 bda 3 c 5843911. jpg It is sometimes difficult to determine if a Salter I is really a Salter V. The history will help determine this and how carefully you need to follow the child. Salter III and IV are bad due to the intraarticular nature of the fractures. 104.
Salter-Harris Classification 105
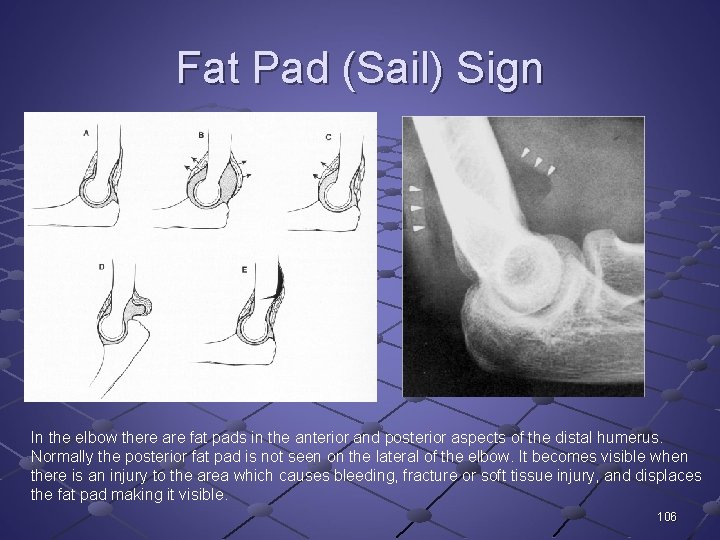
Fat Pad (Sail) Sign In the elbow there are fat pads in the anterior and posterior aspects of the distal humerus. Normally the posterior fat pad is not seen on the lateral of the elbow. It becomes visible when there is an injury to the area which causes bleeding, fracture or soft tissue injury, and displaces the fat pad making it visible. 106
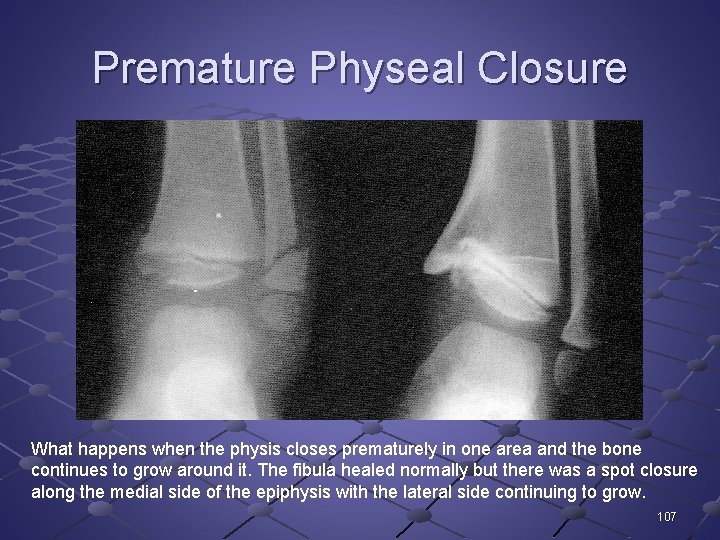
Premature Physeal Closure What happens when the physis closes prematurely in one area and the bone continues to grow around it. The fibula healed normally but there was a spot closure along the medial side of the epiphysis with the lateral side continuing to grow. 107
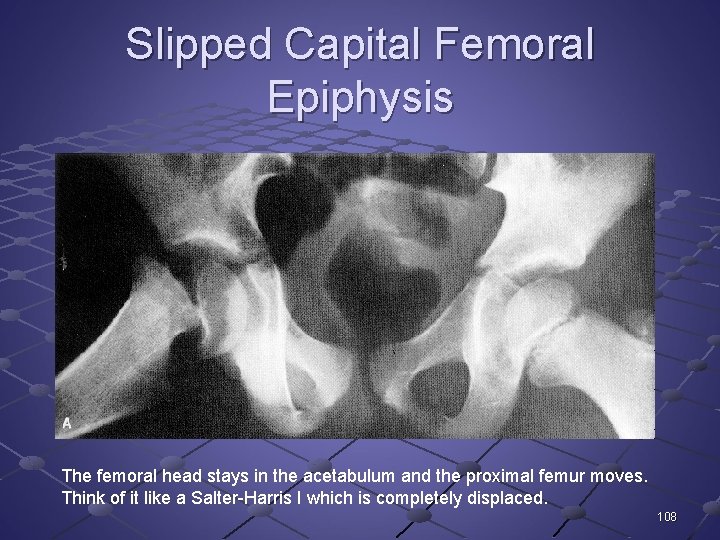
Slipped Capital Femoral Epiphysis The femoral head stays in the acetabulum and the proximal femur moves. Think of it like a Salter-Harris I which is completely displaced. 108
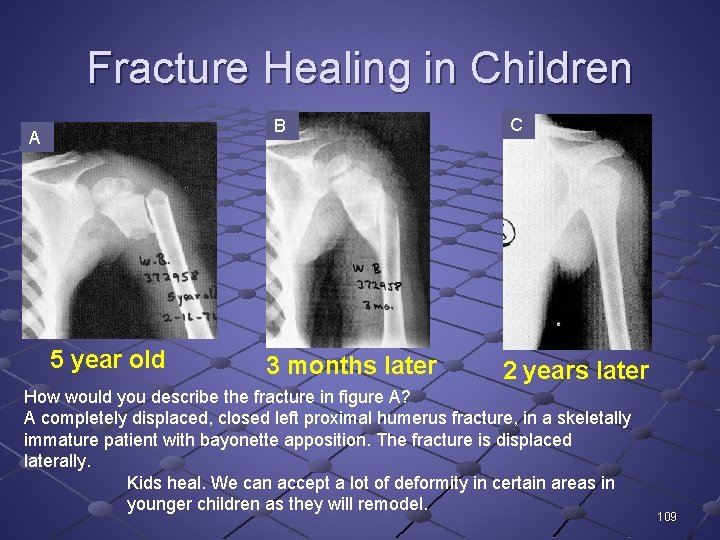
Fracture Healing in Children B A 5 year old 3 months later C 2 years later How would you describe the fracture in figure A? A completely displaced, closed left proximal humerus fracture, in a skeletally immature patient with bayonette apposition. The fracture is displaced laterally. Kids heal. We can accept a lot of deformity in certain areas in younger children as they will remodel. 109
- Slides: 109