The Knowledge Base Required for a Successful TDP
The Knowledge Base Required for a Successful TDP Program The essential knowledge base includes the: • Anatomic alterations of the lungs • Pathophysiologic mechanisms activated • Clinical manifestations that develop • Treatment modalities used to correct the problem
The Assessment Process Skills Required for a Successful TDP Program The practitioner must: • Systematically gather clinical information • Formulate an assessment • Select an optimal treatment • Document in a clear and precise manner
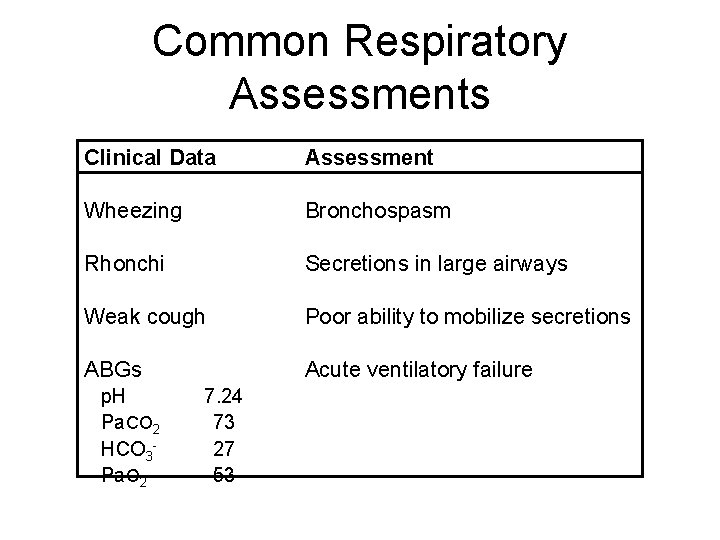
Common Respiratory Assessments Clinical Data Assessment Wheezing Bronchospasm Rhonchi Secretions in large airways Weak cough Poor ability to mobilize secretions ABGs Acute ventilatory failure p. H Pa. CO 2 HCO 3 Pa. O 2 7. 24 73 27 53
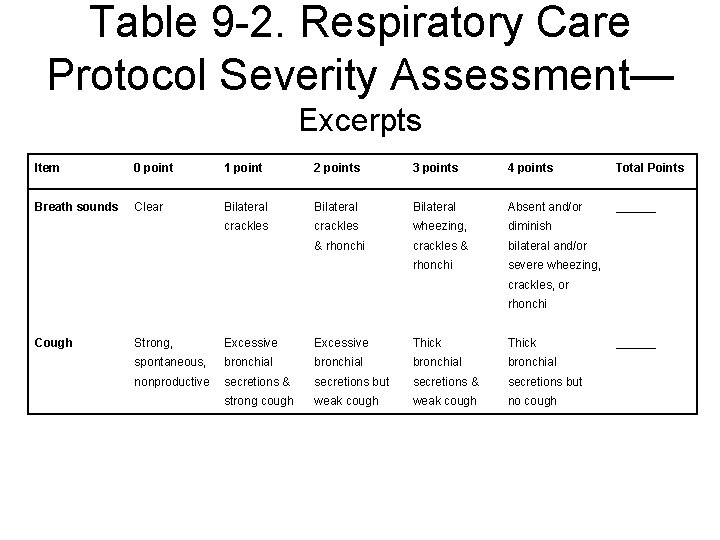
Table 9 -2. Respiratory Care Protocol Severity Assessment— Excerpts Item 0 point 1 point 2 points 3 points 4 points Total Points Breath sounds Clear Bilateral Absent and/or ______ crackles wheezing, diminish & rhonchi crackles & bilateral and/or rhonchi severe wheezing, crackles, or rhonchi Cough Strong, Excessive Thick spontaneous, bronchial nonproductive secretions & secretions but strong cough weak cough no cough ______

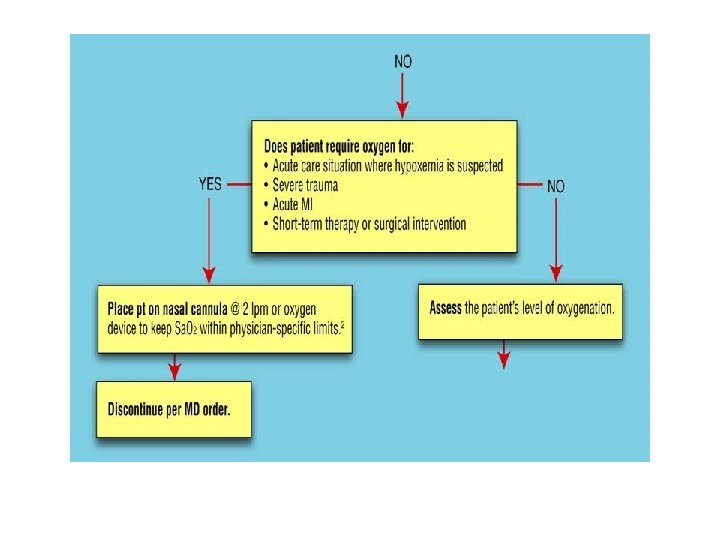
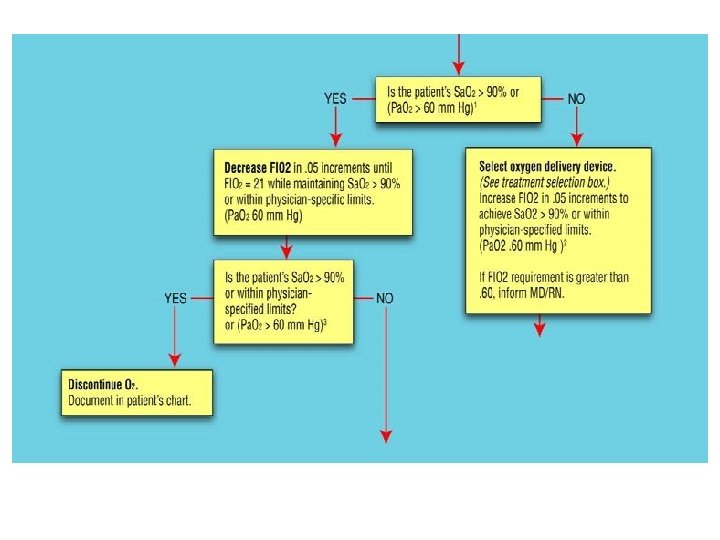
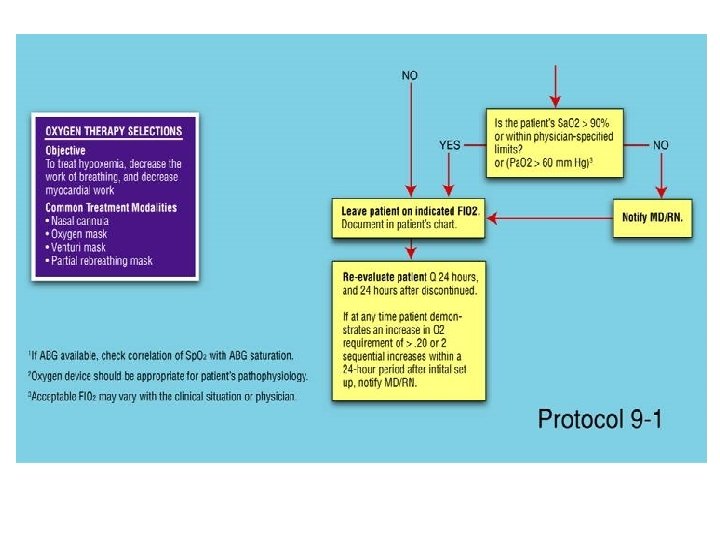
Problem-Oriented Medical Record (POMR) 1. Systematically gather clinical data 2. Formulate an assessment 3. Develop an appropriate treatment plan
SOAP— Most Common POMR S: Subjective information O: Objective information A: Assessment (cause of subjective and objective data) P: Plan (treatment selection)
CHARTING and Recordkeeping
Types of Patient Records • Traditional chart • Problem-oriented medical record (POMR) • Computer documentation
Computer Documentation • • So-called paperless medical record Easy access Eliminates need to make phone calls Other health-care departments can review records • Computers include electronic signature as part of log-in
Documentation Formats • Problem-oriented medical record (POMR) – Is an alternative documentation format used by some healthcare institutions – Four parts the database, problem list, the plan, and the progress notes • SOAP format most often used type of documentation
Problem-Oriented Medical Record (POMR) 1. Systematically gather clinical data 2. Formulate an assessment 3. Develop an appropriate treatment plan 4. SOAP— Most Common POMR
SOAP— Most Common POMR S: Subjective information O: Objective information A: Assessment (cause of subjective and objective data) P: Plan (treatment selection)
D. SOAP format for respiratory care progress notes: �S = subjective, information obtained from the patient or relatives �O = objective, information obtained by the caregiver’s observations of the patient, laboratory or diagnostic tests, or physical examination �A = assessment, the analysis of the patient’s problem �P = plan of action to resolve the problem
S. O. A. P. Example � � S = “I can’t breathe!” O = Respiratory rate 28, Pulse 115, BP 157/88, breath sounds show bilateral wheezing, diaphoretic, dry, tight cough. A = Asthma exacerbation P = Hand held nebulizer with bronchodilator x 3, Q 20 minutes. Measure peak flow rates before and after each treatment.
I. � A. Charting The medical records or chart is a legal document that contains all the information pertaining to the patient’s stay in the hospital. It is owned by the HEALTH CARE PROVIDER and all information is confidential. The patient has the right to access this information, even have a copy if desired. It should not contain opinions or assumptions, only objective descriptions of the patient’s condition or behavior.
Legal Aspects of Documentation
Legal Aspects of Recordkeeping • Legally, the documentation of the care given to a patient must be completed. • If no documentation is recorded, no care was given at all. • Hospital accreditation agencies will carefully evaluate the medical records of patients.

Legal Aspects of Recordkeeping • If documentation is not done the hospital and the practitioner could be accused of patient neglect. • Proper documentation of care is valuable only in reference to standards and criteria of care. • Respiratory care departments, like all other departments in healthcare most have standards for their own patients.
Legal Aspects of Recordkeeping • For each standard, criteria must be outlined so that adequacy of patient care be measured. • Documentation was reflect the standards of the department.
Practical Aspects of Recordkeeping • Recordkeeping is one of the most important parts of our duties. • Documentation must be done for each medication, treatment, and procedure. • Accounts of patient’s condition and activities must be charted correctly and be very clear. • Briefness is important, although a complete account of each patient encounter
General Rules for Recordkeeping • Legible. Print or hand write entries in chart. • No ditto marks. • Begin with date and time, then enter order and sign the chart: A. French/ RCP RRT-NPS. • Do not use ditto marks. • Errors? Don’t erase, or use correction tape. If a mistake, drawn a line through it, write date and write the word error above it, with your initials • Chart patient complaints and general behavior
General Rules of Recordkeeping • Leave no blank or empty lines. Draw a line through the center of the empty space in order to prevent someone else from signing in your area. • Discuss patient, not self. Pt. set up on 2 L N/C. (Not I set pt. up on 2 L N/C). Use the present tense when writing in information. • Use Standard abbreviations • Spell Correctly • Document conversations with patient and healthcare providers that you feel are important
Your Signature. . . � L. Smith, S. R. T.
Errors In Charting � Errors cannot be erased! � Instead, draw a single line through the error and write “error” above it. Place your initials next to it. Then chart the correct information.
Charting Patient Complaints and Behavior � � � Describe clearly and concisely. When possible, chart using quotes of the patients own words or give examples of behavior. Example: Patient stated, “I will not wear my oxygen. It isn’t helping me and I can’t afford it!”

� Wrong: Patient was very angry or combative during treatment. I think he didn’t want to finish the treatment because he needed more sedation medication. � Right: Patient refused to finish treatment. Patient started to swing his fists at me. RN notified.
B. Chart Components 1. Admission sheet—contains patient information such as name, address, religion, admitting diagnosis, physician, etc. 2. Physician’s orders—orders and prescriptions 3. History and physical—contains the patient’s medical history and physical examination performed by a physician

4. Progress notes—contains a day-by-day record of the patient’s progress (written by the physician) 5. Nurse’s notes—nursing care given to the patient that includes patient complaints, response to therapy, etc. 6. Medication record—drugs and IV fluids given
7. Vital signs graph—records patient’s temperature, respirations, blood pressure and heart rate. 8. I/O sheet—records the patient’s intake and output over time 9. Laboratory sheet—contains all lab results

� � � 10. Anesthesia and surgery—may contain surgery consent forms, anesthesia and surgery notes during the procedure 11. Respiratory/physical therapy notes— records specialized treatment performed on the patient 12. Others—consults, flowsheets, Emergency room notes
- Slides: 34