The Informed Consent Process From Rules and Regulations
- Slides: 38
The Informed Consent Process: From Rules and Regulations to the Protective Value of Ethics Kimberly Summers, Pharm. D Deputy ACOS for Research South Texas Veterans Health Care System Research & Development Service
Purpose of Consent Process • Research subject will… – Understand nature of the research – Be continually informed of purpose, risks, benefits, and alternative therapies – Make a voluntary decision about participation or continuation
Significant Historical Events in the Development of Informed Consent • Nazi atrocities in World War II drew attention to the lack of international standards on research with human participants and led to the formulation of the Nuremburg Code (1948). • The thalidomide disaster led to the adoption of the "Kefauver Amendment" (1962) to the Food, Drug and Cosmetic Act, requiring drug manufacturers to prove to the FDA the safety and effectiveness of their products and physicians to obtain informed consent from potential subjects before administering investigational medications. • The Declaration of Helsinki drafted by the world Medical Association in 1964 (most recently updated in 2000) builds on the Nuremberg Code and is the basis for Good Clinical Practices used today. • The National Research Act (1974) passed primarily in response to the syphilis study, codified the requirement that human participants in research must be protected and set the stage for the issuance of the Belmont Report.
Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects in Research • Respect for Persons – Individuals should be treated as autonomous agents – Individuals with diminished autonomy are entitled to protections • Beneficence – Do not harm – Maximum possible benefits, and minimize potential harms • Justice – Fair distribution of burdens and benefits of research
Informed Consent: Application of Respect for Persons • Initiated before any forms are signed • Continues through the completion of the subject's involvement in the study • The consent document is only a confirmation of the consent process • Responsibility of the Principal Investigator – Even if obtaining signed informed consent is delegated to another study team member
Main Components of Informed Consent • Selecting participants – Are only those subjects who meet inclusion criteria enrolled? Does the consent form clearly indicate that participation in the research is voluntary? • Information - Does the consent form provide all the information necessary for the individual to make a reasoned decision? • Comprehension - Is the consent form crafted in language understandable to the potential participant?
Selecting Participants • Recruitment of participants needs to be done in a nonbiased and non superior to subordinate setting • Participants should never feel that if they do not participate they will be penalized • Participants should understand why they are being approached for enrollment in the research protocol
Example • One requirement of Psychology 101 is participation in a study on learning practices. • Does this violate the principle of autonomy? • Autonomy means a person must have the right to decide not to be in a study. Participation should not be a class requirement.
Recruitment: Boundaries Between Practice and Research • The distinction between practice and research is often blurred because many times they occur together • The researcher and the participant must be able to distinguish practice from research • The purpose of clinical research is to gain knowledge, not to treat a condition – Therapeutic Misconception – Misunderstanding that being in a clinical trial is automatically “good” for you
Information to Subjects: Describing the Research • • • Research Purpose Research Procedures Risks Benefits Compensation Alternatives • Confidentiality • Disclosure of Potential Conflict of Interest • Research-Related Injury • Contact Information • Withdrawal
Informed Consent Document (ICD) • IRB template for the ICD covers information required to describe the research to potential research subjects • Only the most recent IRB approved and stamped consent form can be used to consent subjects • A signed ICD is required prior to any protocolspecific testing being conducted – If protocol specific testing is done the same day as signed informed consent is obtained, must be clear documentation of the chronological order in the medical record
Comprehension: Ensure Readability of the ICD • Direct the ICD at an eighth-grade reading level • Use simple, straightforward sentences • Use commonly recognizable terms and measurement amounts • Avoid the use of jargon or technical language • Explain terms that may not be easily understood
Comprehension: Assessing Participant Understanding • Ensure that prospective participants understand the extent of their role in the research protocol • Read through the consent document with participants • Discuss participation prior to their involvement in the research protocol • Answer questions and ask open-ended questions
Example • The principal investigator outlines the risks and benefits to a participant. The participant wants to know of her other options. The investigator does not know of any other options and states this to the potential participant. • Is this the correct response to the participant's request? • If there are no clear alternatives to participation, the investigator should simply note nonparticipation as an alternative.
Example • The principal investigator asks a participant to be in her study. The participant agrees, and the investigator has him sign a piece of paper and tells him she will put it in his file. The investigator also says she will mail him information about the study specifics. • Does this violate the principle of autonomy? • Potential participants must be given information they will need before they decide whether or not to enter a study.
Signatures on the ICD • FDA 21 CFR 50 – The patient or authorized representative shall sign and date the informed consent • OHRP 45 CFR 46 - …signed by the patient or legally authorized representative • ICH GCP E 6 4. 8 - …the informed consent should be signed and personally dated by the subject or legally authorized representative • VHA Handbook 1200. 5 - use of a written consent form approved by the IRB and signed and dated by the subject or the subject's legally-authorized representative
Witnessing the Informed Consent Process • When do you need a witness? – – When presenting the ICD verbally Use of a short form If required by the IRB For all VA research involving an ICD • Who can be the witness? – ICH GCP: An impartial witness – a person who is independent of the trial, who cannot be unfairly influenced by people involved in the trial, who attends the informed consent process – VHA Handbook 1200. 5: role is to witness the subject’s or the subject’s legally-authorized representative’s signature
Documenting the Informed Consent Process • A statement that the protocol procedures and the informed consent document were reviewed with the participant • Review of the risks and benefits of the study • Time for questions to be asked answered • Alternative treatment options discussed • Description of the participant’s decision • Copy of ICD provided to participant
Enrollment Consent Template: Research Consent / Enrollment Note • Must be entered into the subject’s health record (CPRS) after IC has been obtained • Template in CPRS flags patients Medical Record in postings • Template contains all the required information for documentation of consent process • Template must be used in order to scan IC document • Note must indicate if the study involves the use of investigational medications
Consent Document Revisions • Study participants must be informed of any new and important information that might affect their willingness to continue participation • If new information, knowledge, or an adverse event has been discovered, it must be communicated to the subjects • The Principal Investigator must evaluate the new information to decide if a revised consent document is required – Evaluate if future participants are affected – Evaluate what information should be given to former or current subjects – May be a requirement of the IRB
Auditing vs Monitoring • Audits are in addition to the more detailed monitoring of studies by the research team and sponsor • Audits are an independent evaluation by someone who is not directly associated with the research
VA Research Compliance Office • Conduct audits and reviews to ensure compliance with all VA and other Federal requirements for the conduct of research • Conduct annual audits of all active studies to insure that informed consent has been properly obtained and documented for each subject since the previous audit
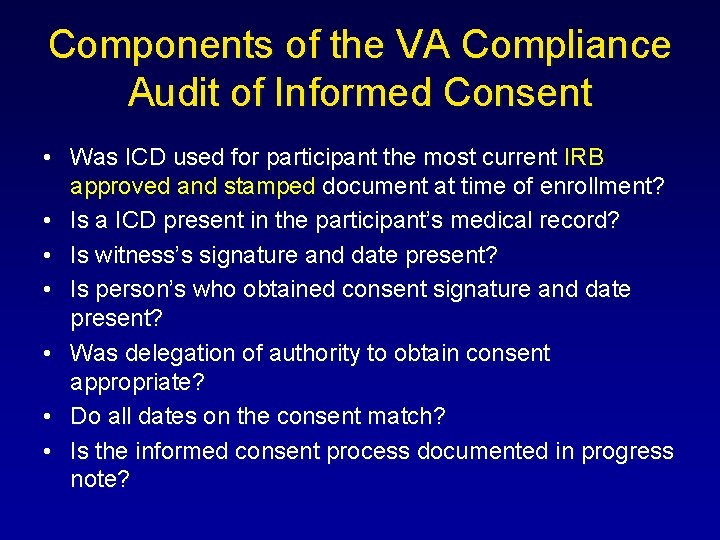
Components of the VA Compliance Audit of Informed Consent • Was ICD used for participant the most current IRB approved and stamped document at time of enrollment? • Is a ICD present in the participant’s medical record? • Is witness’s signature and date present? • Is person’s who obtained consent signature and date present? • Was delegation of authority to obtain consent appropriate? • Do all dates on the consent match? • Is the informed consent process documented in progress note?
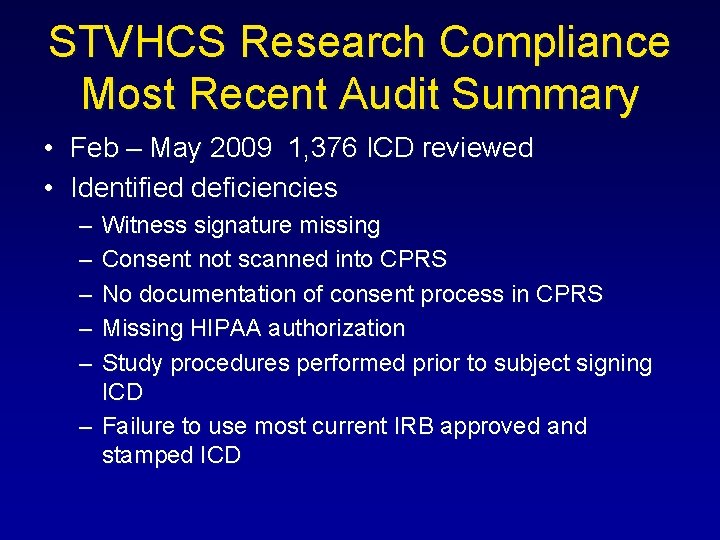
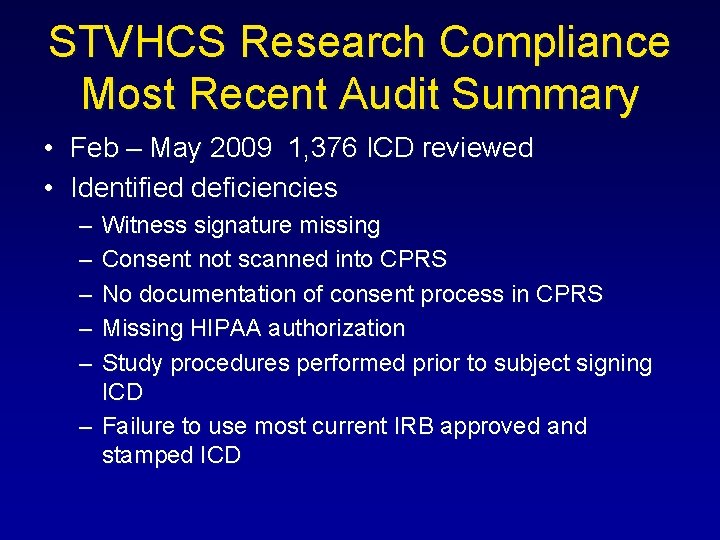
STVHCS Research Compliance Most Recent Audit Summary • Feb – May 2009 1, 376 ICD reviewed • Identified deficiencies – – – Witness signature missing Consent not scanned into CPRS No documentation of consent process in CPRS Missing HIPAA authorization Study procedures performed prior to subject signing ICD – Failure to use most current IRB approved and stamped ICD
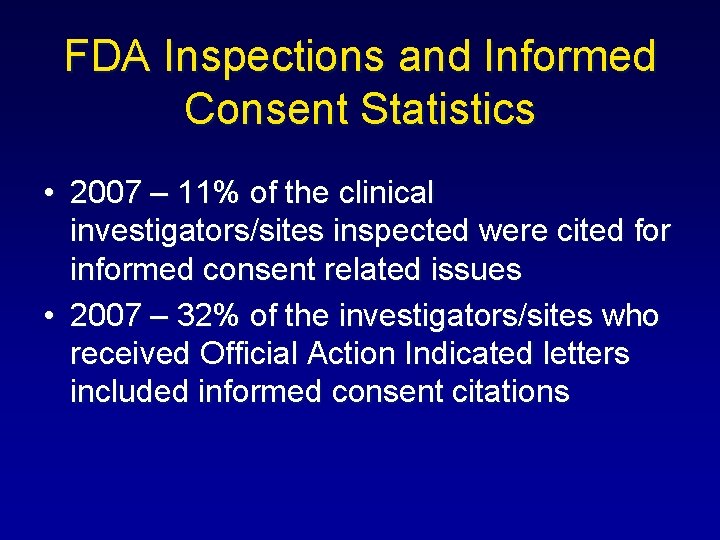
FDA Inspections and Informed Consent Statistics • 2007 – 11% of the clinical investigators/sites inspected were cited for informed consent related issues • 2007 – 32% of the investigators/sites who received Official Action Indicated letters included informed consent citations
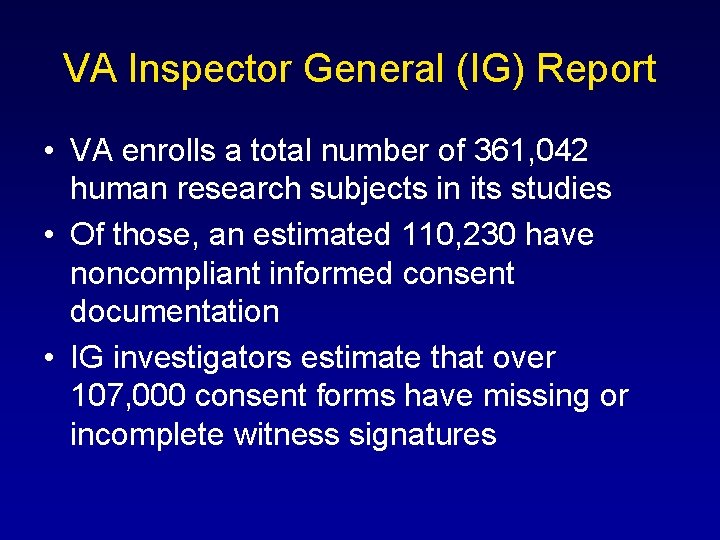
VA Inspector General (IG) Report • VA enrolls a total number of 361, 042 human research subjects in its studies • Of those, an estimated 110, 230 have noncompliant informed consent documentation • IG investigators estimate that over 107, 000 consent forms have missing or incomplete witness signatures
Jesse Gelsinger • 18 year old participant in a gene therapy trial conducted at the University of Pennsylvania • Suffered from ornithine transcarbamylase deficiency (OTC) – X-linked genetic disease of the liver – At the time of enrollment was doing well on a restricted diet and medications • Enrolled in a trial to test the safety of a procedure to inject gene therapy with an adeovirus vector – Procedure was being developed for treatment of infants born with OTC – No direct benefit was expected to current participants • Jesse died 4 days after initiation of the procedure due to a massive immune response triggered by the adenovirus vector
FDA Investigation • Concluded scientists involved, including the lead investigator and the University broke several basic ethical principals
Failure to Recruit Based on Inclusion Criteria • Participant enrolled despite elevated ammonia levels that met exclusion criteria • Jesse’s liver deficiency was worse than any of the previous seventeen research subjects
Failure to Fully Describe the Research: Potential Risks • The consent form approved by the NIH notified participants that monkeys had died from similar treatments • The final consent form distributed to volunteers enrolled at U Penn omitted any mention of the monkey deaths • Jesse and his parents were not aware of the monkey deaths associated with similar treatments
Failure to Fully Describe the Research: Research Procedures • The protocol had a dose ranging component • Jesse was the first participant assigned to the largest dose group • Jesse was not informed that he may receive a dose larger than that given to any previous subject
Failure to Revise Informed Consent Document • Previous subjects in this trial had experienced severe elevated liver enzymes and serious adverse reactions • These adverse effects had not been reported to federal regulators • The consent form had not been amended to include these reactions • Protocol procedures continued with increasing dosages despite warning signs
Failure to Disclose Potential Conflicts of Interest • The lead investigator and the University are reported to have had financial stakes in the research • Financial conflicts of interest for the investigators and/or the institution were not disclosed in the informed consent process
Failure to Assess Participants Understanding • Statement by PAUL GELSINGER: “Jesse was doing exceptionally well on his medications, and nothing should have prevented him from living a full and happy life. He believed, after discussions with representatives from Penn, that the worst that could happen in the trial would be that he would have flu-like symptoms for a week. He was excited to help. ”
Was Jesse able to make an informed decision regarding his participation in this trial?
Statement by Paul Gelsinger I still support our need for clinical trials, but with this caution: Informed consent is only possible if all facets of the research endeavor are ethical and in the open. Because of the secretive and conflicting influences on clinical research, the average research subject has little hope of understanding and giving truly informed consent. All research subjects really want is to be able to trust the system. If we can somehow get that system to apply Jesse's Intent. . . not for recognition and not for money, but only to help. . . then research will get all it wants and more; they'll get research right and have a real prosperity, one they never imagined possible. Until that happens I am so very grateful that we had a legal recourse that enabled us to draw attention to the problems currently inherent in clinical research.
Questions? Kimberly Summers, Pharm. D Office: (210) 617 -5300 ext 15969 Email: kimberlyk. Summers@va. gov