The Highs and Lows of Inpatient Diabetes Management
The High’s and Low’s of Inpatient Diabetes Management Cora Espina, ARNP, CWCN University of Washington Medical Center University of Washington, School of Medicine Division of Endocrinology espina@uw. edu

UW School of Pharmacy Facebook
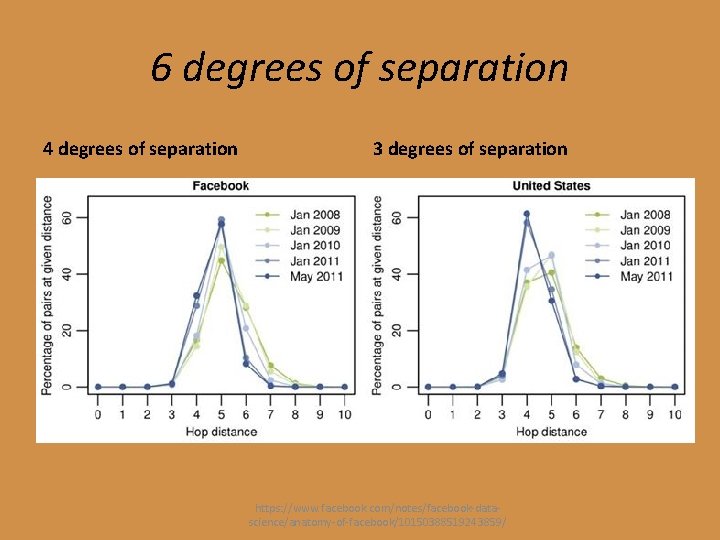
6 degrees of separation 4 degrees of separation 3 degrees of separation https: //www. facebook. com/notes/facebook-datascience/anatomy-of-facebook/10150388519243859/
Prevalence of Diabetes • As many as 1 in 3 American adults will have diabetes by 2050 if present trends continue professional. diabetes. org/facts
REVIEW
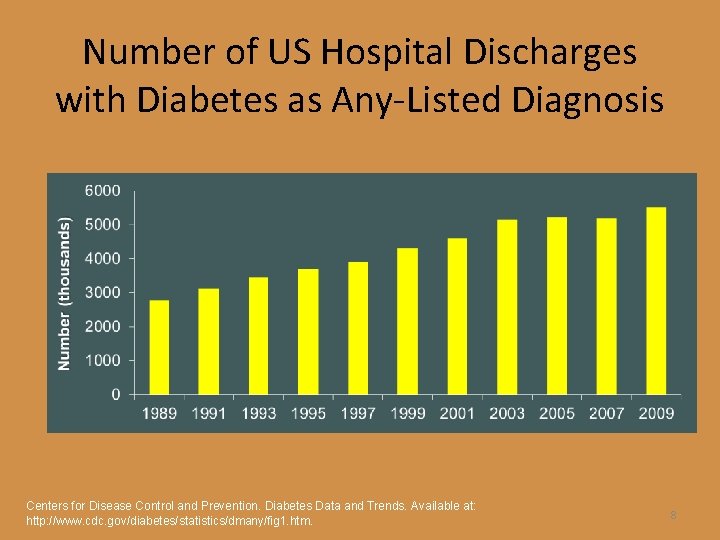
Number of US Hospital Discharges with Diabetes as Any-Listed Diagnosis Centers for Disease Control and Prevention. Diabetes Data and Trends. Available at: http: //www. cdc. gov/diabetes/statistics/dmany/fig 1. htm. 8
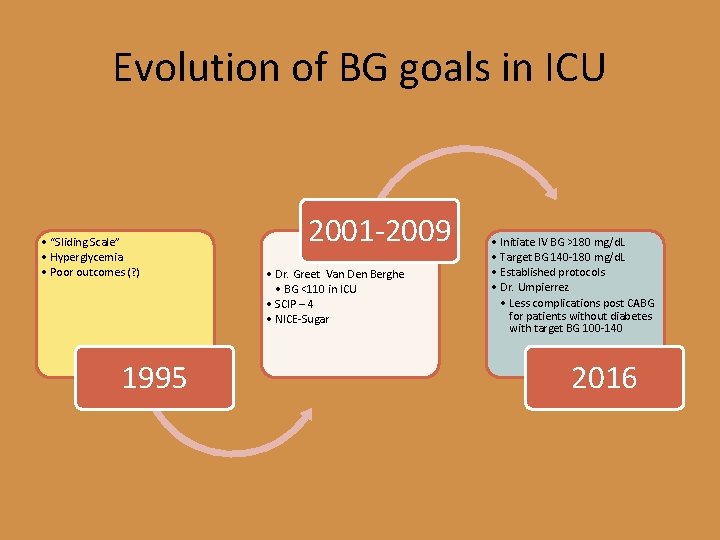
Evolution of BG goals in ICU • “Sliding Scale” • Hyperglycemia • Poor outcomes (? ) 1995 2001 -2009 • Dr. Greet Van Den Berghe • BG <110 in ICU • SCIP – 4 • NICE-Sugar • Initiate IV BG >180 mg/d. L • Target BG 140 -180 mg/d. L • Established protocols • Dr. Umpierrez • Less complications post CABG for patients without diabetes with target BG 100 -140 2016
Three Types of Hyperglycemia in Hospitalized Patient • Known history of diabetes • Existing, but unrecognized, diabetes • Stress hyperglycemmia – Medications – Surgery (stress hormones) – Sedentary Clement et al. Diabetes Care. 2004; 27: 553 -591.
Other - Immunosuppressant Drugs • Calcineurin Inhibitors – Tacrolimus (FK-506) – Cyclosporine – Destruction of beta cells, can be permanent – Hard on kidneys • Corticosteroids – Prednisone, Dexamethasone – Fam hx, obesity, hx of DM – Reduced insulin uptake by the muscles – Low/Normal Fasting BG, High Prandial needs
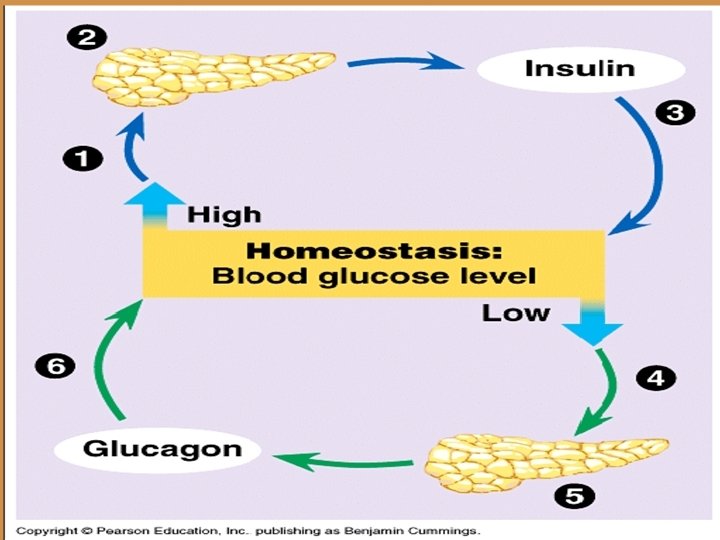
Etiology of hyperglycemia Type 1 – insulin deficient LADA, CFRD, Pancreatic DM Type 2 – insulin resistant Steroids, enteral feeding, TPN, stress
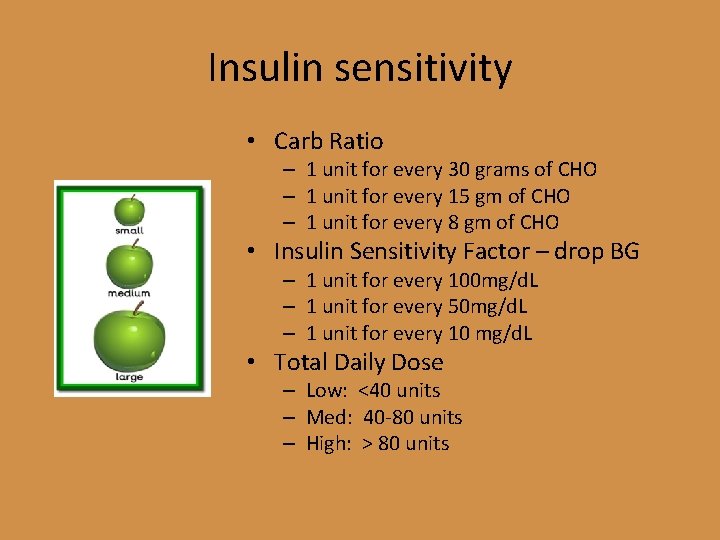
Insulin sensitivity • Carb Ratio – 1 unit for every 30 grams of CHO – 1 unit for every 15 gm of CHO – 1 unit for every 8 gm of CHO • Insulin Sensitivity Factor – drop BG – 1 unit for every 100 mg/d. L – 1 unit for every 50 mg/d. L – 1 unit for every 10 mg/d. L • Total Daily Dose – Low: <40 units – Med: 40 -80 units – High: > 80 units
Hospital Management of DM • • • Know the etiology – where is the problem Know action/onset/pharmacology of meds Know your patient Identify goals during hospitalization Plan for discharge Medications
Admission Orders • Insulin only • Why we under dose Insulin? – Patients sometimes poor historians – Patients sometimes not compliant – Sometimes basal insulin covering prandial needs – Sometimes poor appetite or NPO
Discontinue Oral Medications • Not associated with Lows – Metformin • • Decreases hepatic glucose production Increases insulin sensitivity Watch Renal Function, diuresing Lactic Acidosis – dye studies – Pioglitazone, Rosiglitazone • • Action on muscle uptake of insulin Good - Lipid control Bad - Heart Failure Too Slow
Secretagogues • Stimulate beta cell to release insulin from the pancreas • Potential for Lows • Renal Status – Glipizide, Glyburide, Glimiperide – Repaglinide
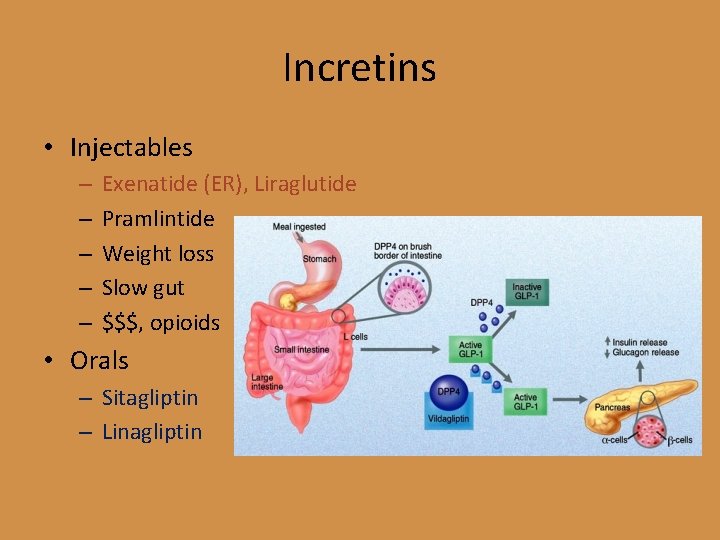
Incretins • Injectables – – – Exenatide (ER), Liraglutide Pramlintide Weight loss Slow gut $$$, opioids • Orals – Sitagliptin – Linagliptin
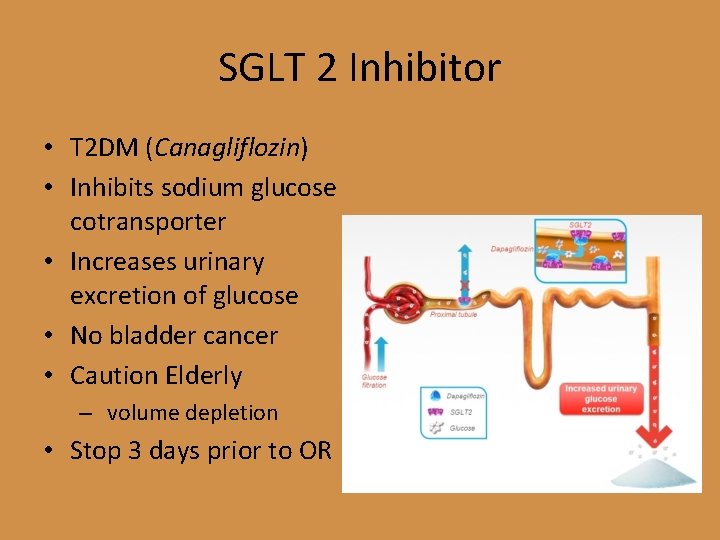
SGLT 2 Inhibitor • T 2 DM (Canagliflozin) • Inhibits sodium glucose cotransporter • Increases urinary excretion of glucose • No bladder cancer • Caution Elderly – volume depletion • Stop 3 days prior to OR
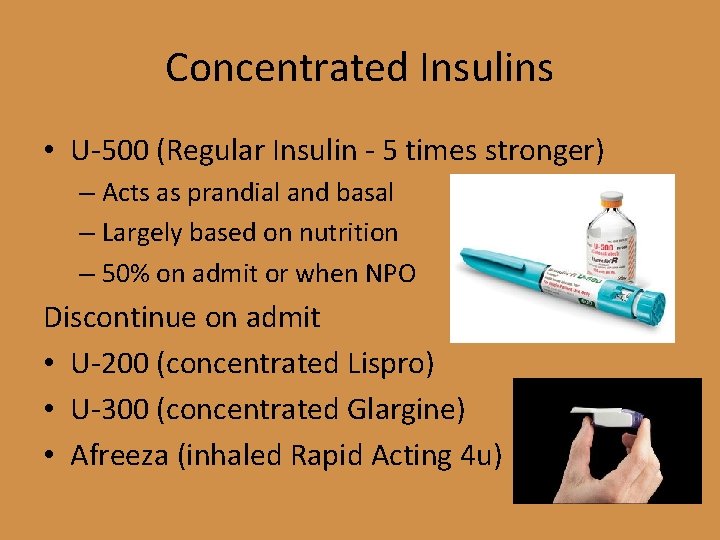
Concentrated Insulins • U-500 (Regular Insulin - 5 times stronger) – Acts as prandial and basal – Largely based on nutrition – 50% on admit or when NPO Discontinue on admit • U-200 (concentrated Lispro) • U-300 (concentrated Glargine) • Afreeza (inhaled Rapid Acting 4 u)
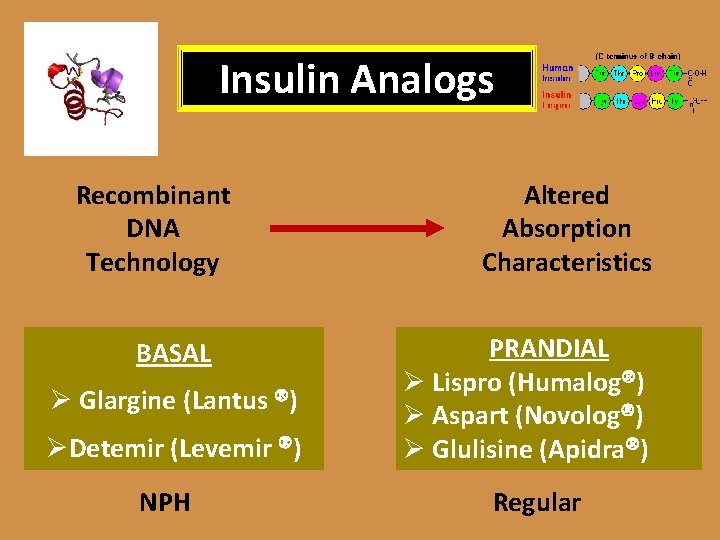
Insulin Analogs Recombinant DNA Technology BASAL Ø Glargine (Lantus ) ØDetemir (Levemir ) NPH Altered Absorption Characteristics PRANDIAL Ø Lispro (Humalog ) Ø Aspart (Novolog ) Ø Glulisine (Apidra ) Regular
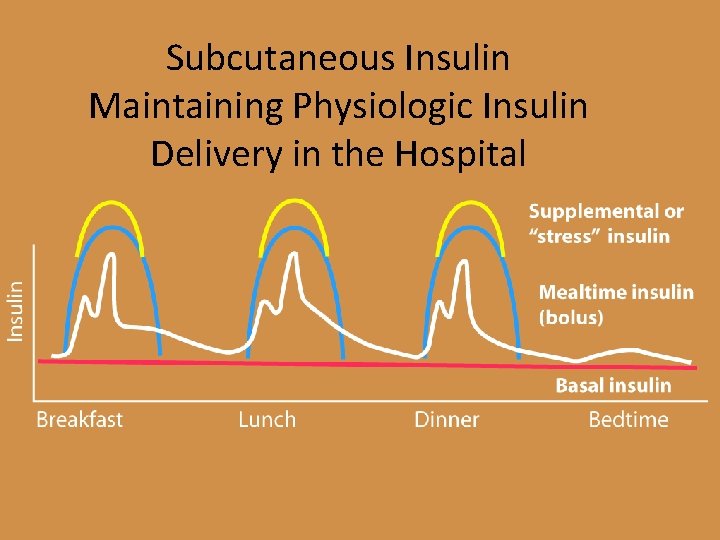
Subcutaneous Insulin Maintaining Physiologic Insulin Delivery in the Hospital
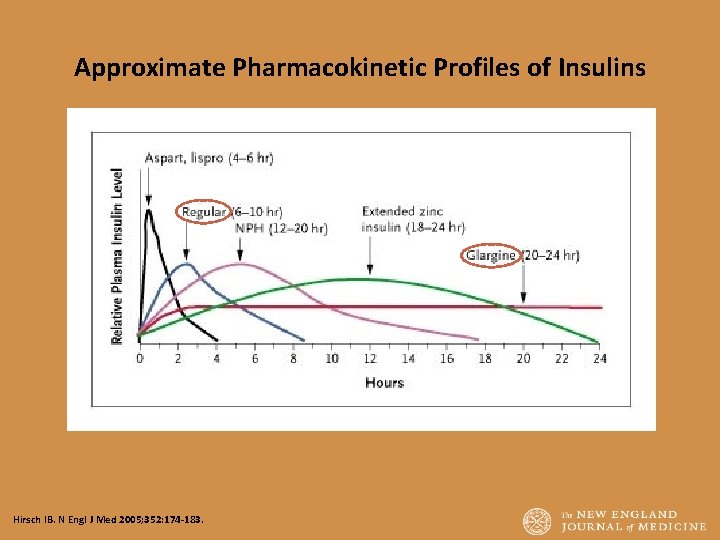
Approximate Pharmacokinetic Profiles of Insulins Hirsch IB. N Engl J Med 2005; 352: 174 -183.
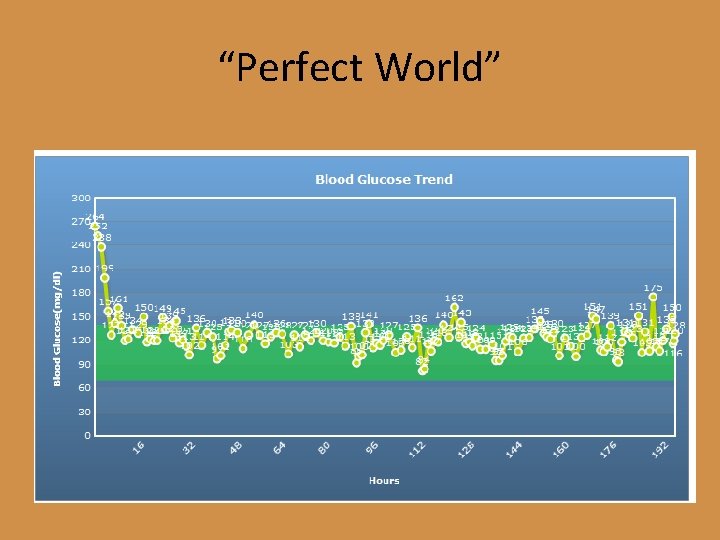
“Perfect World”
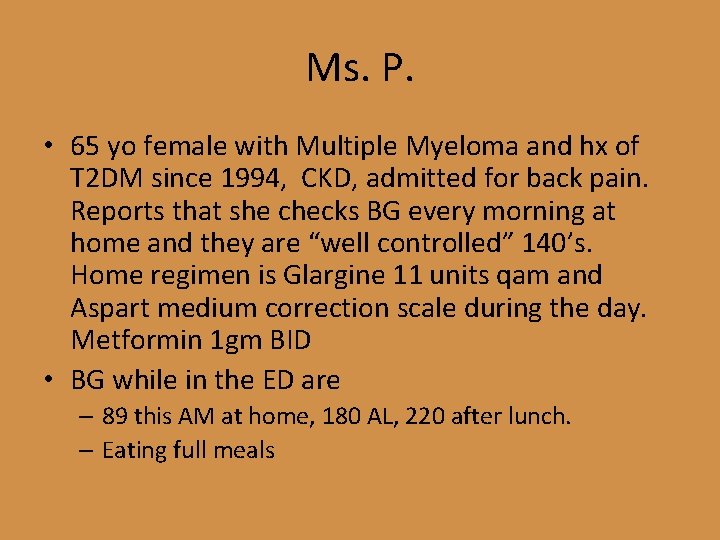
Ms. P. • 65 yo female with Multiple Myeloma and hx of T 2 DM since 1994, CKD, admitted for back pain. Reports that she checks BG every morning at home and they are “well controlled” 140’s. Home regimen is Glargine 11 units qam and Aspart medium correction scale during the day. Metformin 1 gm BID • BG while in the ED are – 89 this AM at home, 180 AL, 220 after lunch. – Eating full meals
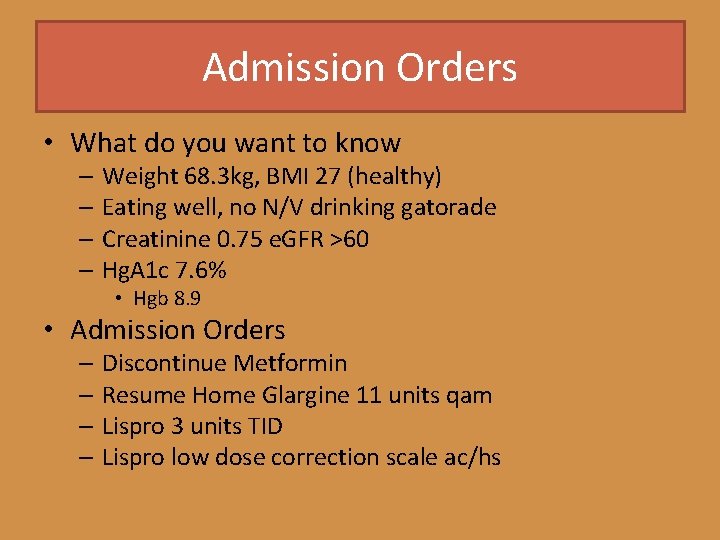
Admission Orders • What do you want to know – Weight 68. 3 kg, BMI 27 (healthy) – Eating well, no N/V drinking gatorade – Creatinine 0. 75 e. GFR >60 – Hg. A 1 c 7. 6% • Hgb 8. 9 • Admission Orders – Discontinue Metformin – Resume Home Glargine 11 units qam – Lispro 3 units TID – Lispro low dose correction scale ac/hs
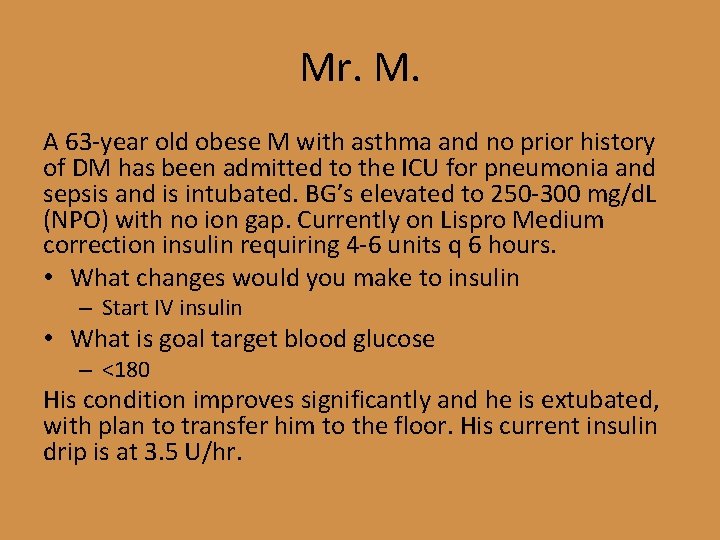
Mr. M. A 63 -year old obese M with asthma and no prior history of DM has been admitted to the ICU for pneumonia and sepsis and is intubated. BG’s elevated to 250 -300 mg/d. L (NPO) with no ion gap. Currently on Lispro Medium correction insulin requiring 4 -6 units q 6 hours. • What changes would you make to insulin – Start IV insulin • What is goal target blood glucose – <180 His condition improves significantly and he is extubated, with plan to transfer him to the floor. His current insulin drip is at 3. 5 U/hr.
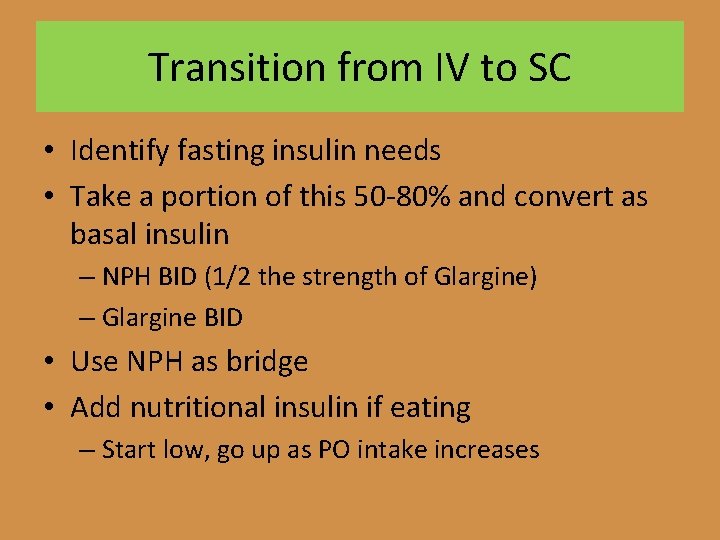
Transition from IV to SC • Identify fasting insulin needs • Take a portion of this 50 -80% and convert as basal insulin – NPH BID (1/2 the strength of Glargine) – Glargine BID • Use NPH as bridge • Add nutritional insulin if eating – Start low, go up as PO intake increases
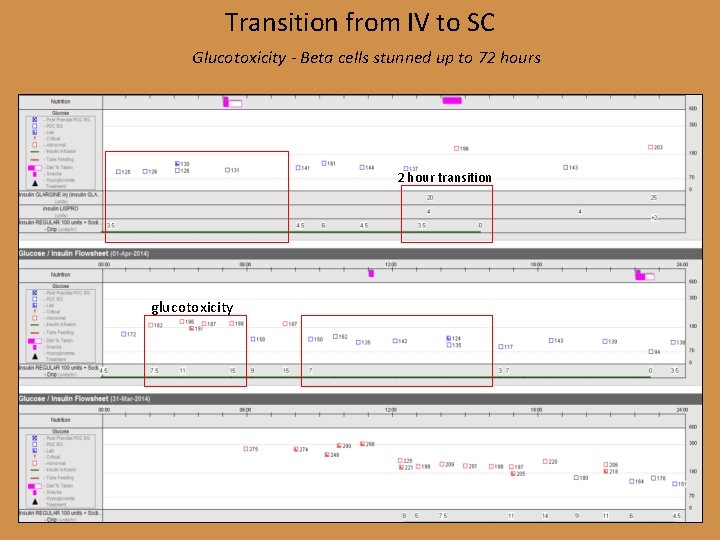
Transition from IV to SC Glucotoxicity - Beta cells stunned up to 72 hours 2 hour transition glucotoxicity
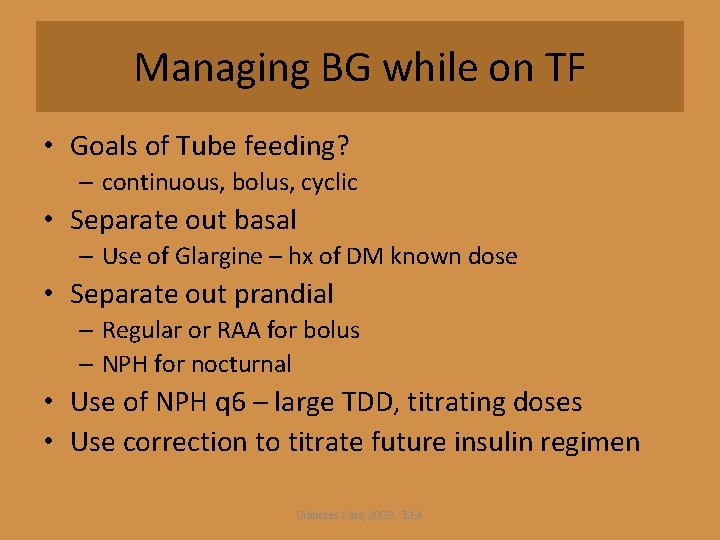
Managing BG while on TF • Goals of Tube feeding? – continuous, bolus, cyclic • Separate out basal – Use of Glargine – hx of DM known dose • Separate out prandial – Regular or RAA for bolus – NPH for nocturnal • Use of NPH q 6 – large TDD, titrating doses • Use correction to titrate future insulin regimen Diabetes Care, 2009. 32; 4
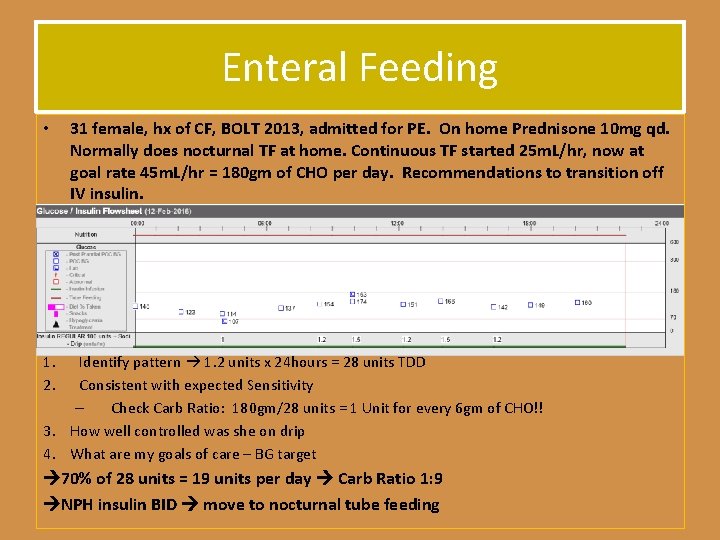
Enteral Feeding • 31 female, hx of CF, BOLT 2013, admitted for PE. On home Prednisone 10 mg qd. Normally does nocturnal TF at home. Continuous TF started 25 m. L/hr, now at goal rate 45 m. L/hr = 180 gm of CHO per day. Recommendations to transition off IV insulin. 1. 2. Identify pattern 1. 2 units x 24 hours = 28 units TDD Consistent with expected Sensitivity – Check Carb Ratio: 180 gm/28 units = 1 Unit for every 6 gm of CHO!! 3. How well controlled was she on drip 4. What are my goals of care – BG target 70% of 28 units = 19 units per day Carb Ratio 1: 9 NPH insulin BID move to nocturnal tube feeding
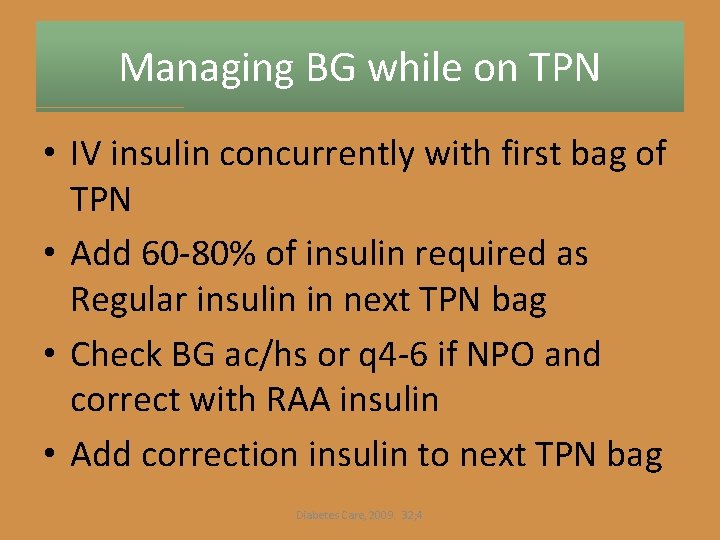
Managing BG while on TPN • IV insulin concurrently with first bag of TPN • Add 60 -80% of insulin required as Regular insulin in next TPN bag • Check BG ac/hs or q 4 -6 if NPO and correct with RAA insulin • Add correction insulin to next TPN bag Diabetes Care, 2009. 32; 4
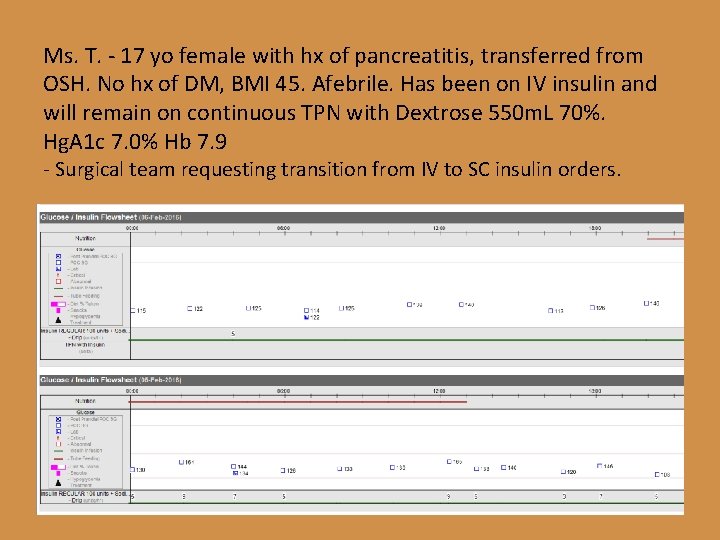
Ms. T. - 17 yo female with hx of pancreatitis, transferred from OSH. No hx of DM, BMI 45. Afebrile. Has been on IV insulin and will remain on continuous TPN with Dextrose 550 m. L 70%. Hg. A 1 c 7. 0% Hb 7. 9 - Surgical team requesting transition from IV to SC insulin orders.
CASES
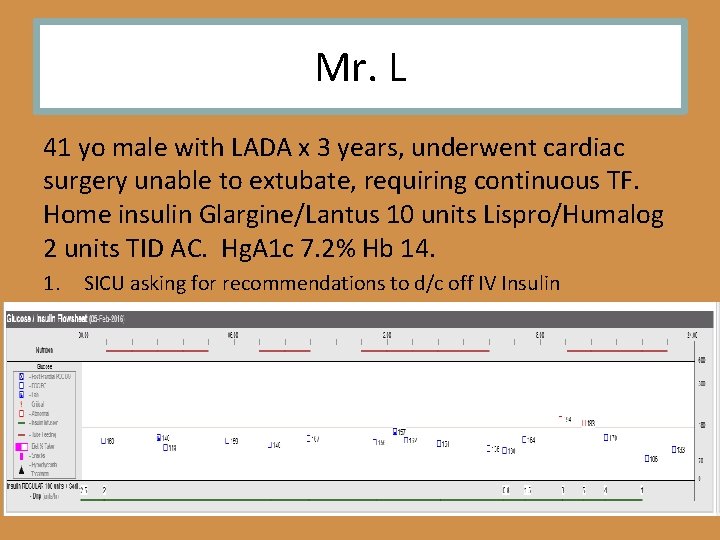
Mr. L 41 yo male with LADA x 3 years, underwent cardiac surgery unable to extubate, requiring continuous TF. Home insulin Glargine/Lantus 10 units Lispro/Humalog 2 units TID AC. Hg. A 1 c 7. 2% Hb 14. 1. SICU asking for recommendations to d/c off IV Insulin
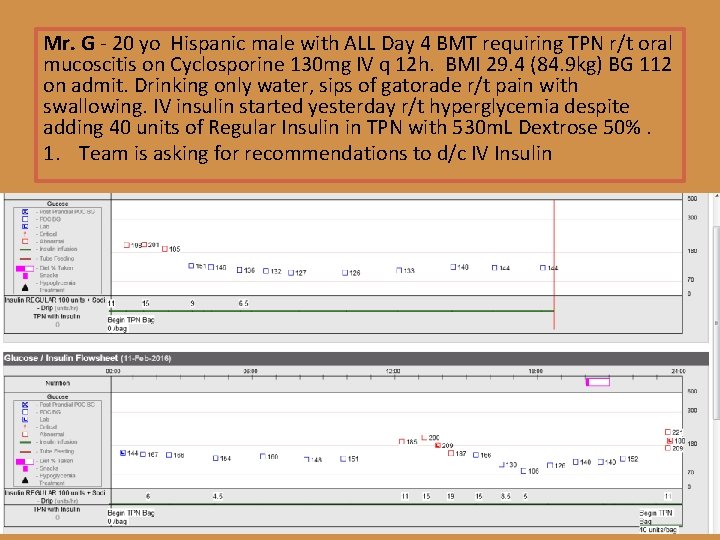
Mr. G - 20 yo Hispanic male with ALL Day 4 BMT requiring TPN r/t oral mucoscitis on Cyclosporine 130 mg IV q 12 h. BMI 29. 4 (84. 9 kg) BG 112 on admit. Drinking only water, sips of gatorade r/t pain with swallowing. IV insulin started yesterday r/t hyperglycemia despite adding 40 units of Regular Insulin in TPN with 530 m. L Dextrose 50%. 1. Team is asking for recommendations to d/c IV Insulin
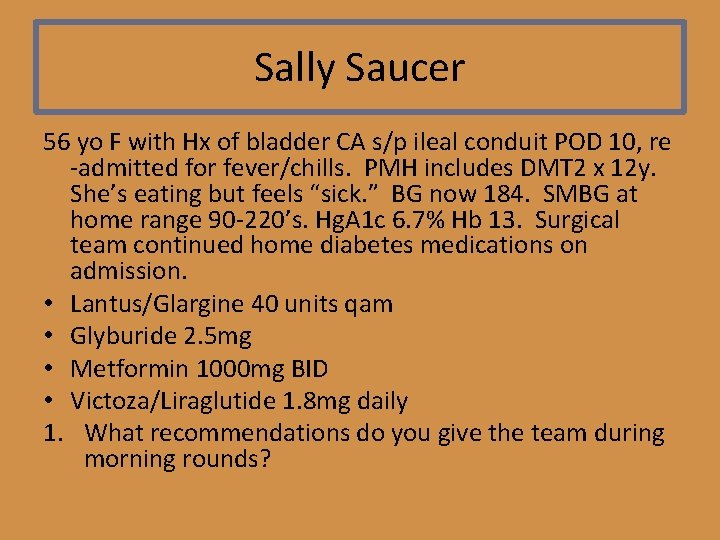
Sally Saucer 56 yo F with Hx of bladder CA s/p ileal conduit POD 10, re -admitted for fever/chills. PMH includes DMT 2 x 12 y. She’s eating but feels “sick. ” BG now 184. SMBG at home range 90 -220’s. Hg. A 1 c 6. 7% Hb 13. Surgical team continued home diabetes medications on admission. • Lantus/Glargine 40 units qam • Glyburide 2. 5 mg • Metformin 1000 mg BID • Victoza/Liraglutide 1. 8 mg daily 1. What recommendations do you give the team during morning rounds?
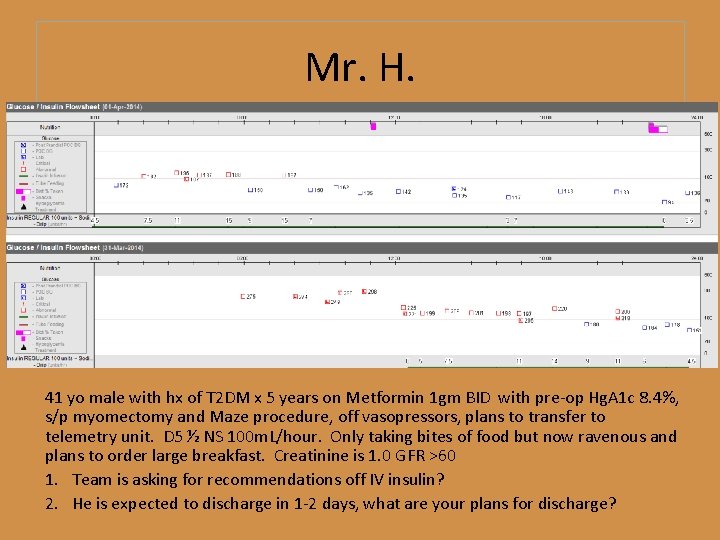
Mr. H. 41 yo male with hx of T 2 DM x 5 years on Metformin 1 gm BID with pre-op Hg. A 1 c 8. 4%, s/p myomectomy and Maze procedure, off vasopressors, plans to transfer to telemetry unit. D 5 ½ NS 100 m. L/hour. Only taking bites of food but now ravenous and plans to order large breakfast. Creatinine is 1. 0 GFR >60 1. Team is asking for recommendations off IV insulin? 2. He is expected to discharge in 1 -2 days, what are your plans for discharge?
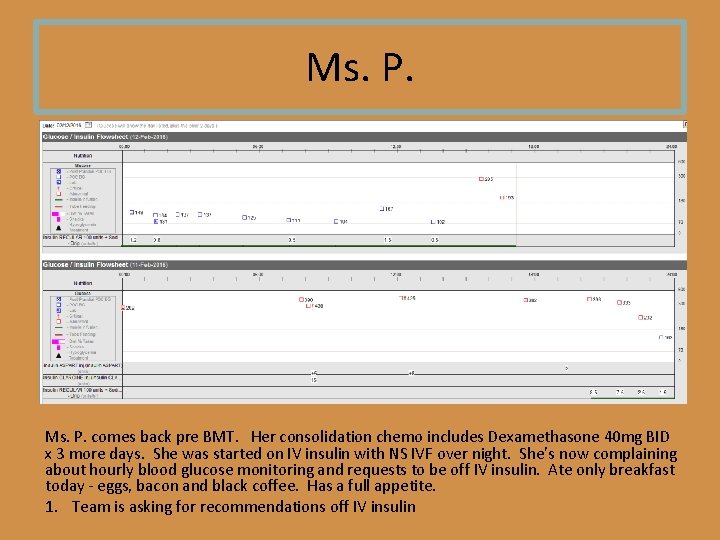
Ms. P. comes back pre BMT. Her consolidation chemo includes Dexamethasone 40 mg BID x 3 more days. She was started on IV insulin with NS IVF over night. She’s now complaining about hourly blood glucose monitoring and requests to be off IV insulin. Ate only breakfast today - eggs, bacon and black coffee. Has a full appetite. 1. Team is asking for recommendations off IV insulin
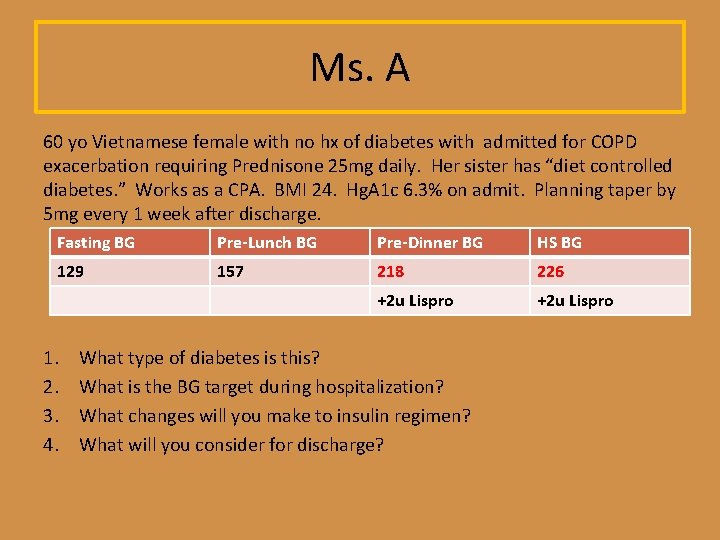
Ms. A 60 yo Vietnamese female with no hx of diabetes with admitted for COPD exacerbation requiring Prednisone 25 mg daily. Her sister has “diet controlled diabetes. ” Works as a CPA. BMI 24. Hg. A 1 c 6. 3% on admit. Planning taper by 5 mg every 1 week after discharge. Fasting BG Pre-Lunch BG Pre-Dinner BG HS BG 129 157 218 226 +2 u Lispro 1. 2. 3. 4. What type of diabetes is this? What is the BG target during hospitalization? What changes will you make to insulin regimen? What will you consider for discharge?
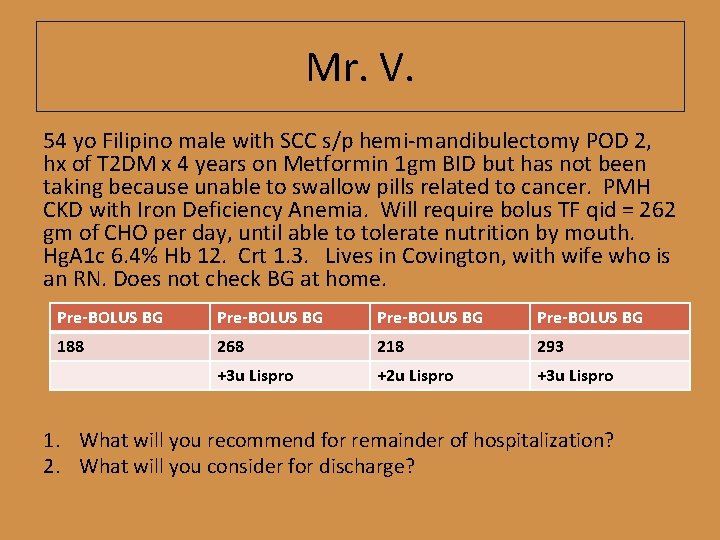
Mr. V. 54 yo Filipino male with SCC s/p hemi-mandibulectomy POD 2, hx of T 2 DM x 4 years on Metformin 1 gm BID but has not been taking because unable to swallow pills related to cancer. PMH CKD with Iron Deficiency Anemia. Will require bolus TF qid = 262 gm of CHO per day, until able to tolerate nutrition by mouth. Hg. A 1 c 6. 4% Hb 12. Crt 1. 3. Lives in Covington, with wife who is an RN. Does not check BG at home. Pre-BOLUS BG 188 268 218 293 +3 u Lispro +2 u Lispro +3 u Lispro 1. What will you recommend for remainder of hospitalization? 2. What will you consider for discharge?
- Slides: 41