The Hester Davis Fall Risk Assessment Scale The


- Slides: 42
The Hester Davis Fall Risk Assessment Scale & The Implementation of Individualized Fall Prevention CASEY O’CONNOR, BSN RN
Let’s Introduce Ourselves… • Work Experience: RN at LLUMC since 2012 Unit 7300: Cardiac Acute Care Unit 7100: Cardiothoracic ICU Currently: Clinical Nurse Educator with Pharmacy Provides education for patients being discharged on infusion therapies • Education: ADN in 2012 BSN in 2017 MSN expected in 2019
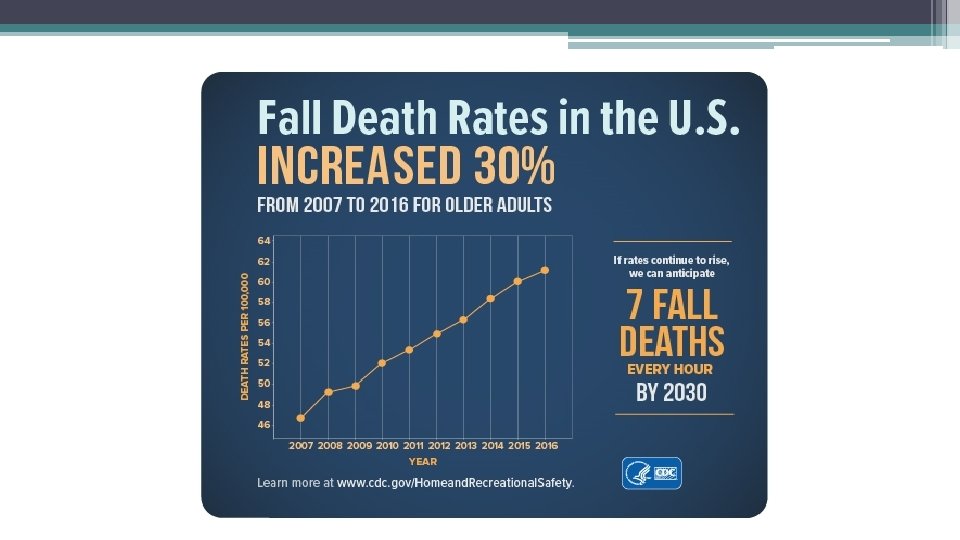
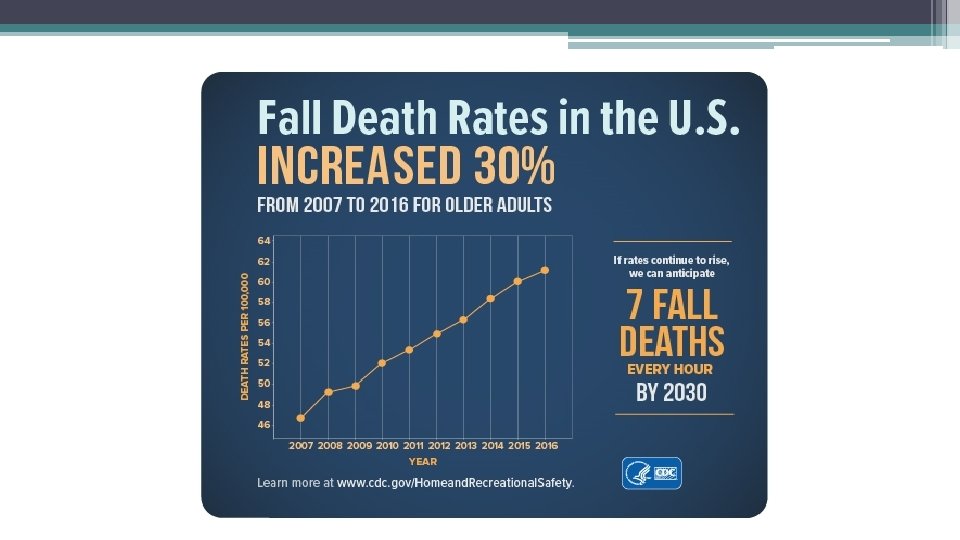
Background • • • Falls are the leading cause of injury-related deaths in adults over age 65. A broken hip at this age can dramatically change a patient’s life. Falls have even been attributed to patients needing a liver transplant Per Centers for Disease Control and Prevention (CDC) , costs of falls among older adults: Ø Over 800, 000 patients a year are hospitalized due to fall injury Ø Average hospital cost for fall injury is over $30, 000 (But the cost to the patient can be greater!)
Hester-Davis Falls Data Quarter 4 - 2018
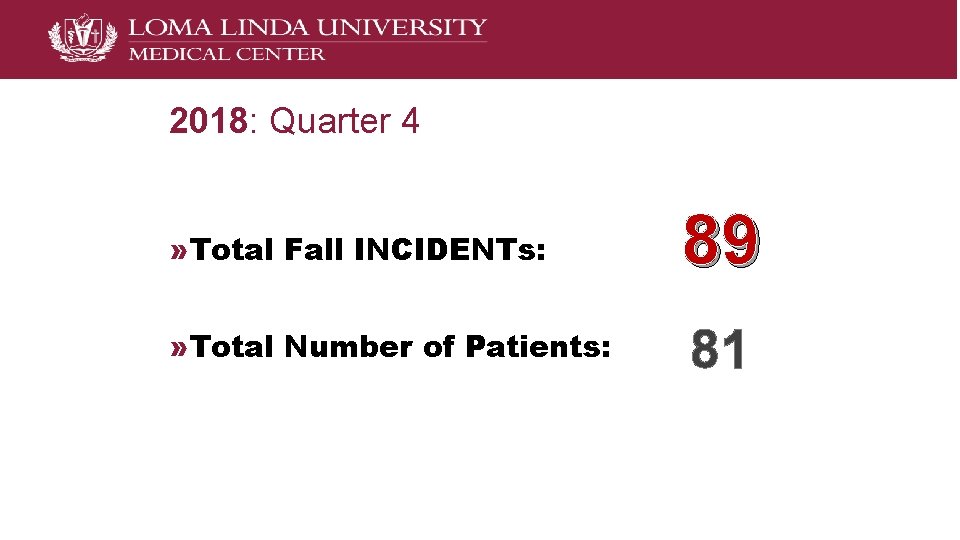
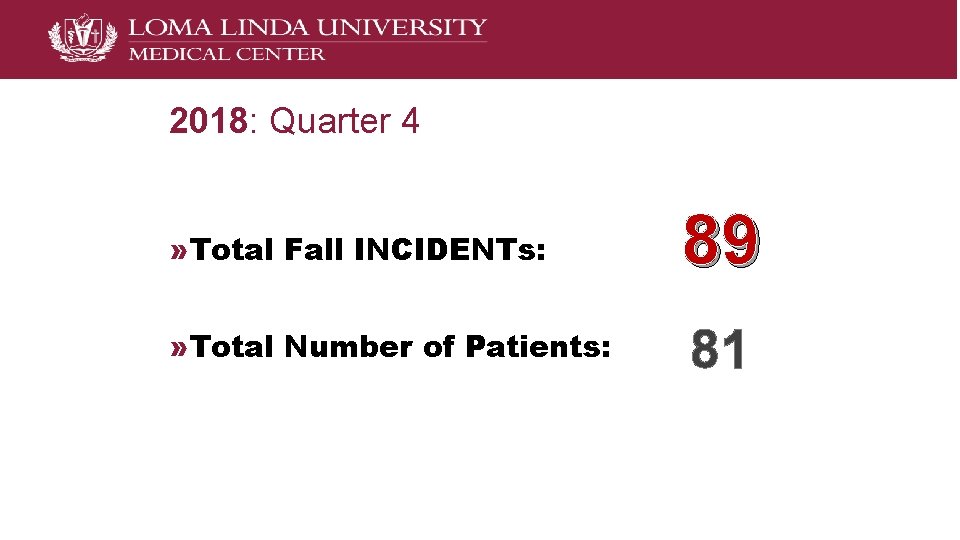
2018: Quarter 4 » Total Fall INCIDENTs: 89 » Total Number of Patients: 81
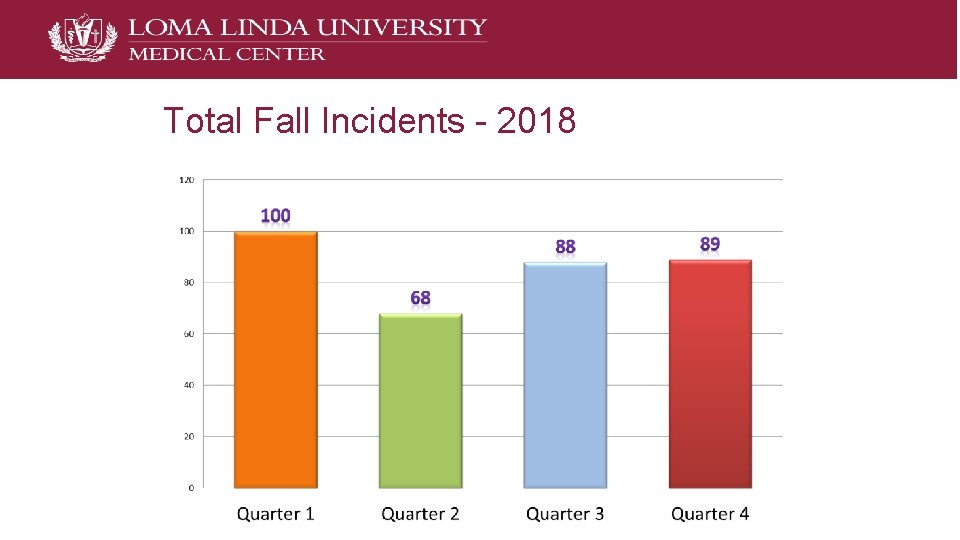
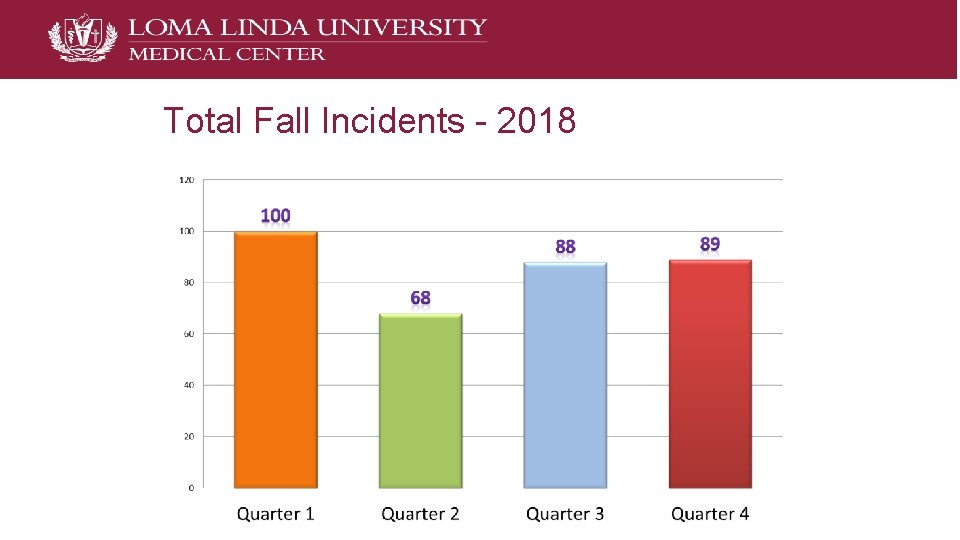
Total Fall Incidents - 2018
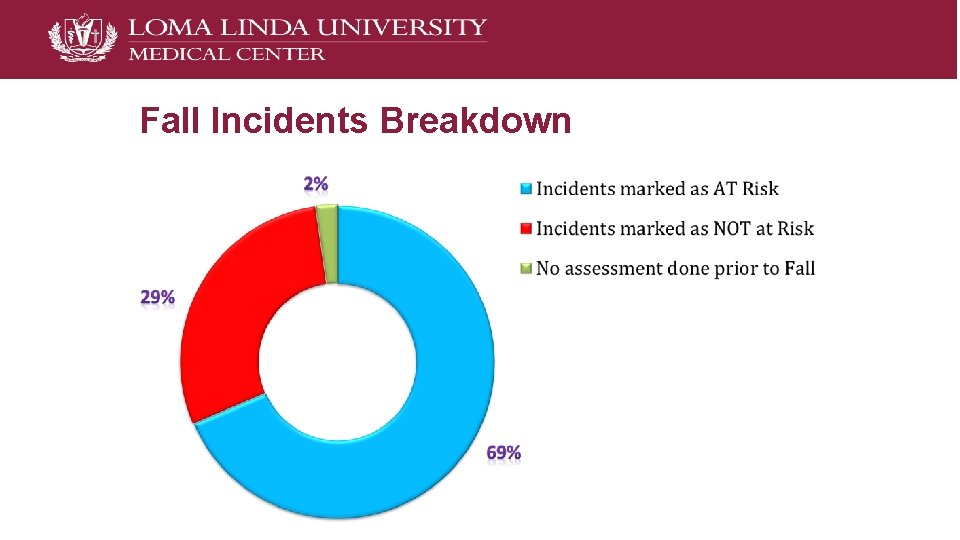
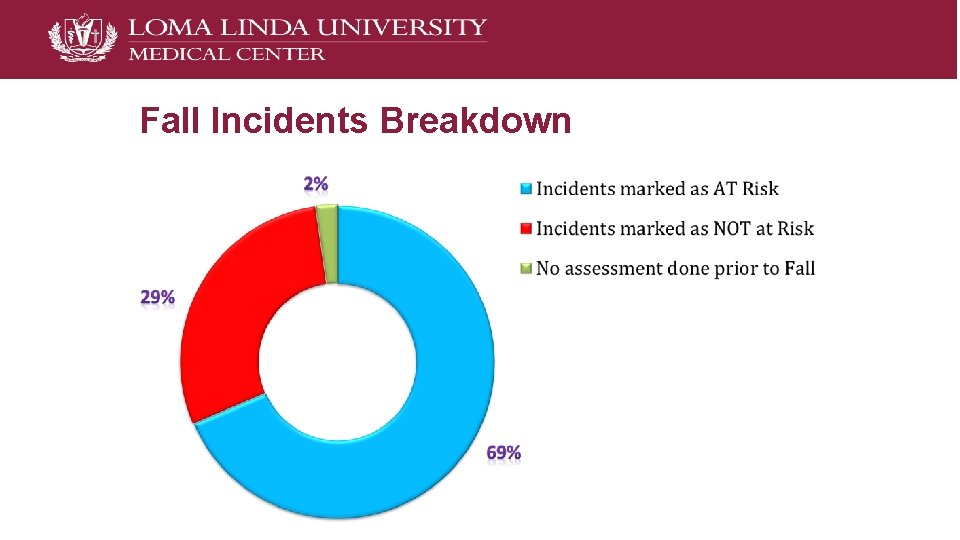
Fall Incidents Breakdown
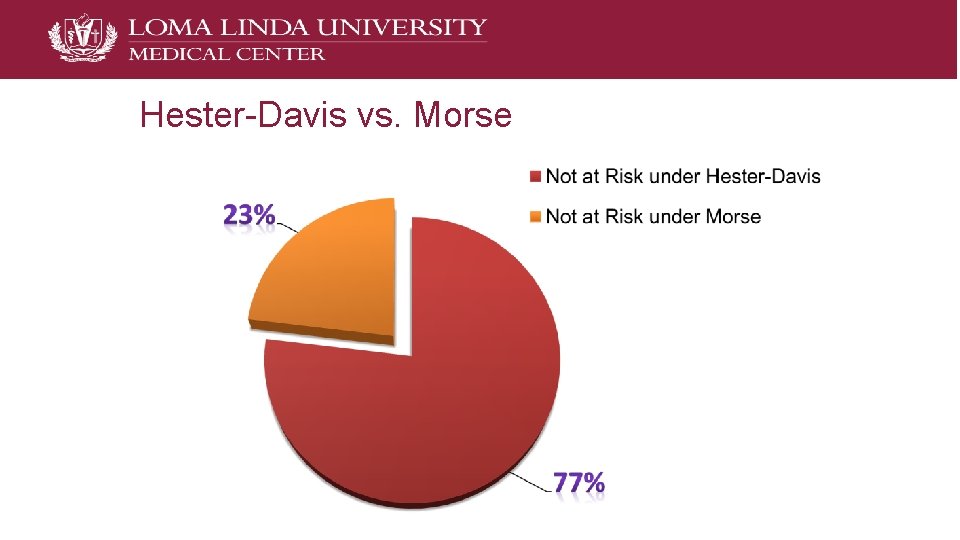
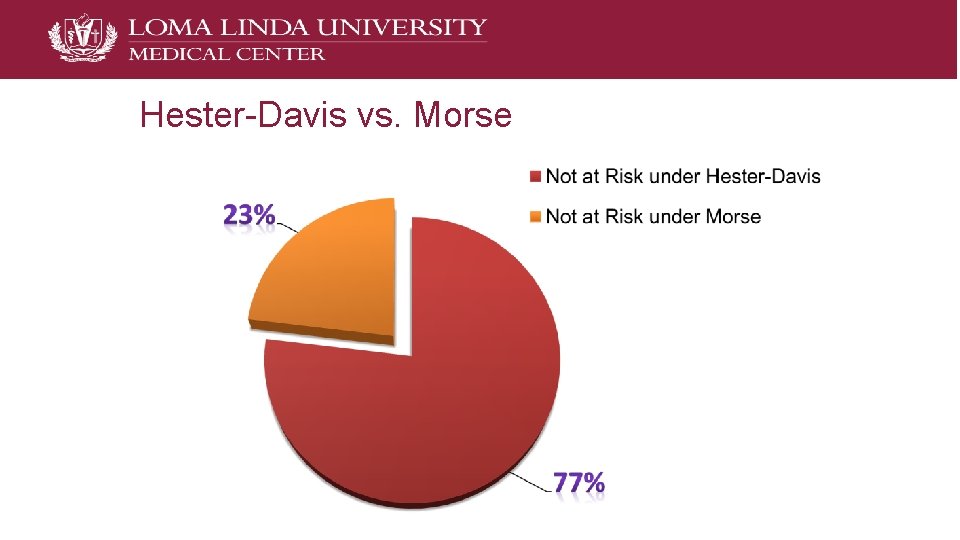
Hester-Davis vs. Morse
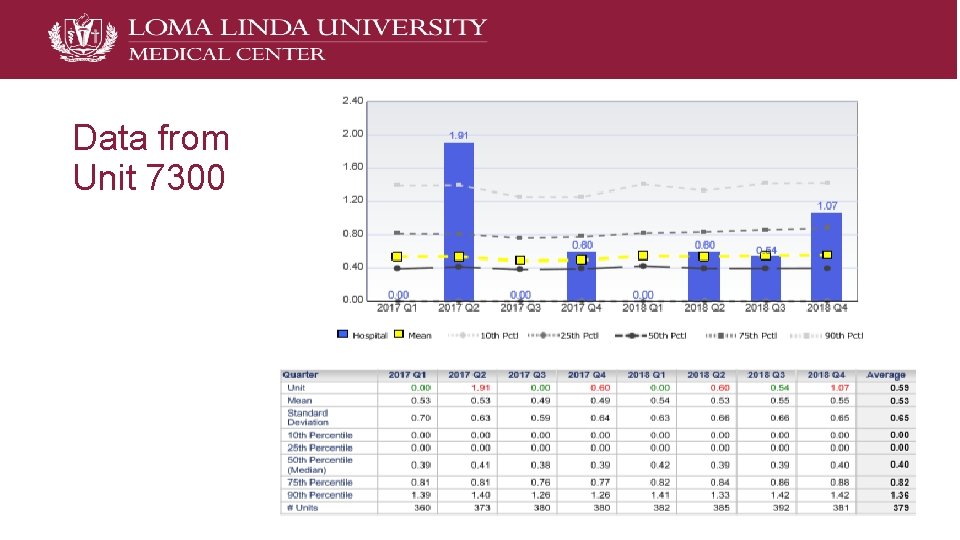
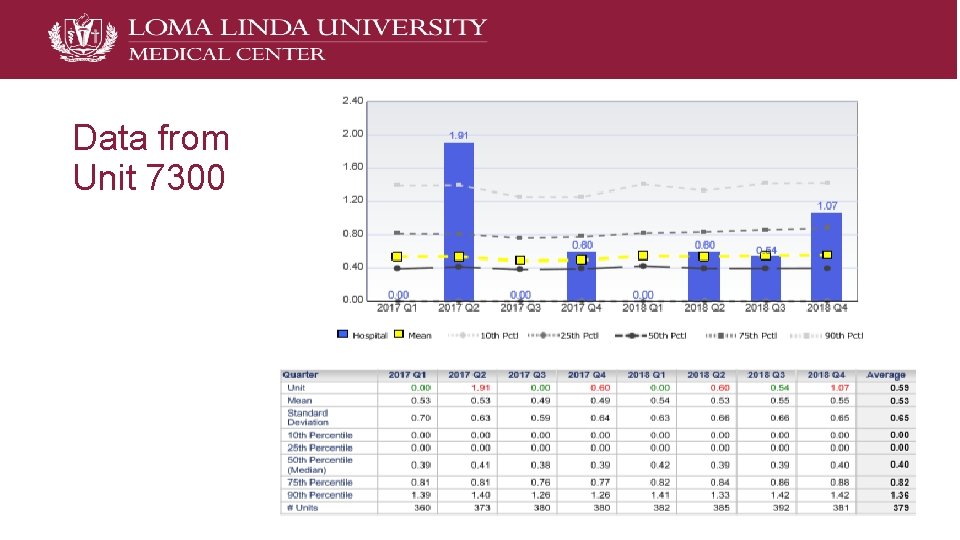
Data from Unit 7300
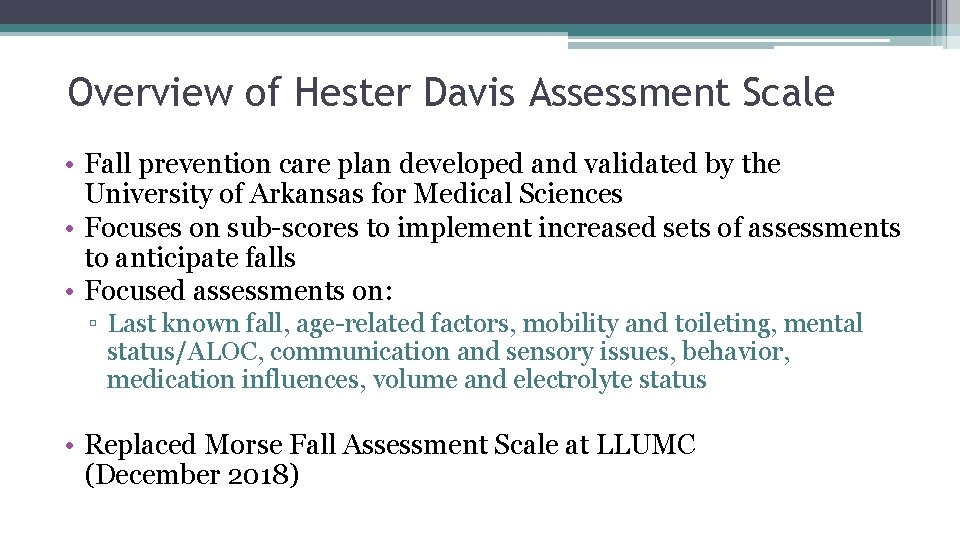
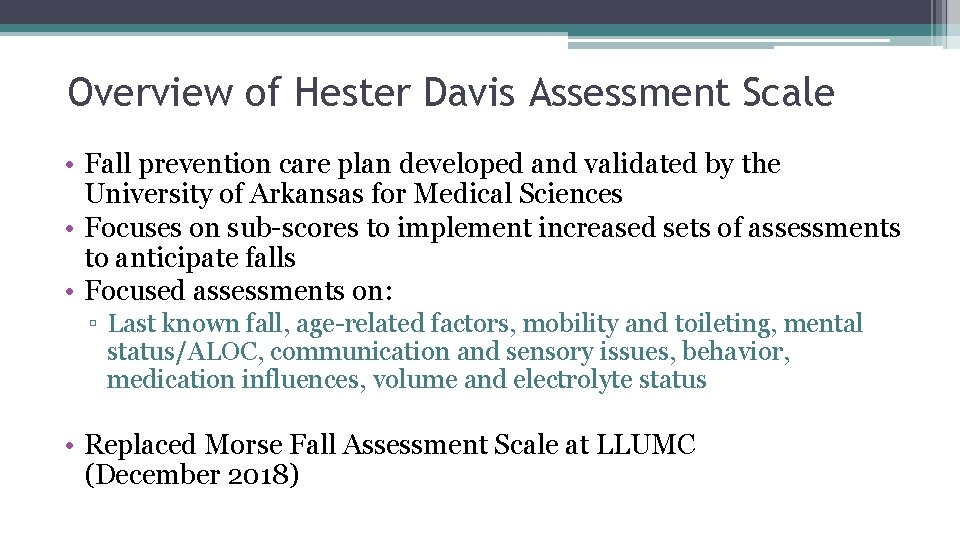
Overview of Hester Davis Assessment Scale • Fall prevention care plan developed and validated by the University of Arkansas for Medical Sciences • Focuses on sub-scores to implement increased sets of assessments to anticipate falls • Focused assessments on: ▫ Last known fall, age-related factors, mobility and toileting, mental status/ALOC, communication and sensory issues, behavior, medication influences, volume and electrolyte status • Replaced Morse Fall Assessment Scale at LLUMC (December 2018)
Assessment Scale Subcategories 1. 2. 3. 4. Last known fall Mobility Medications Mental Status/LOC/ Awareness 5. Toileting needs 6. Volume/electrolyte status 7. Communication/sensory 8. Behavior
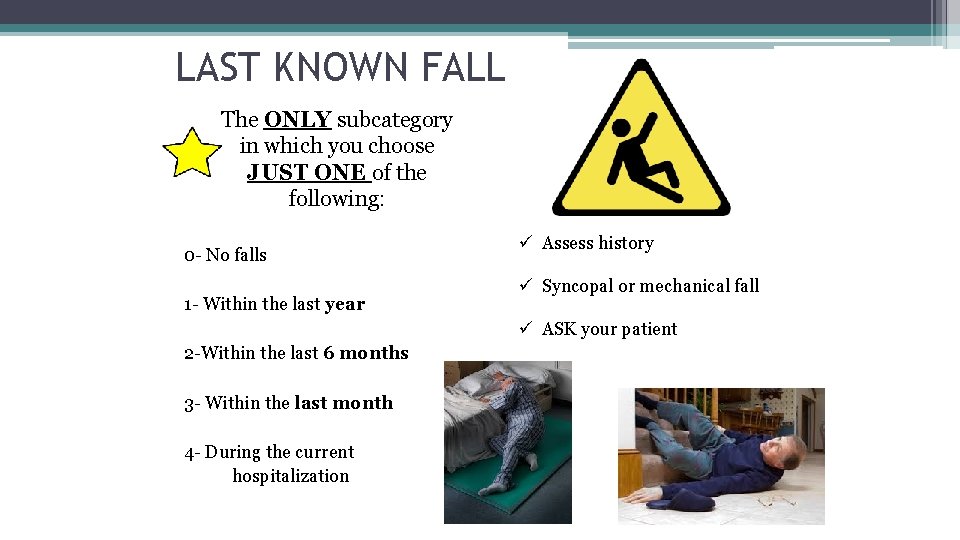
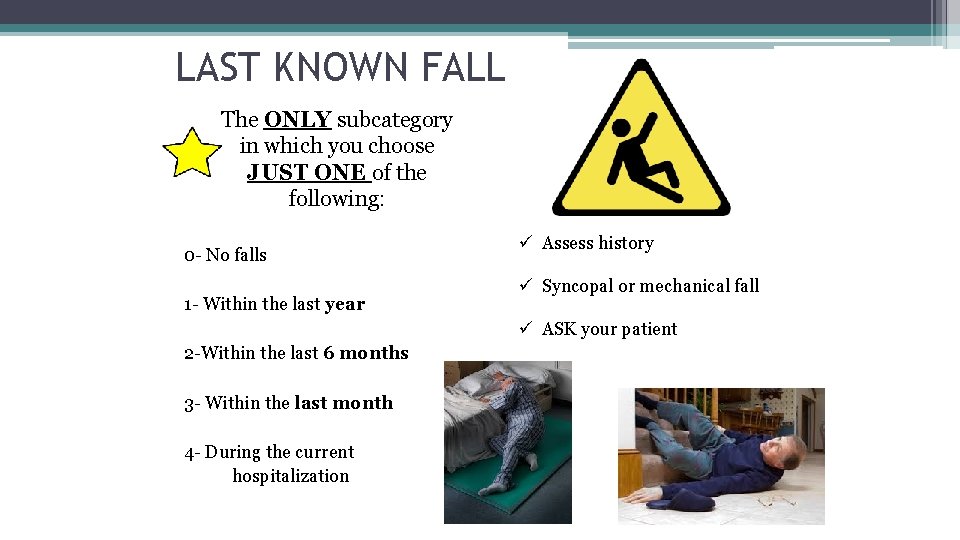
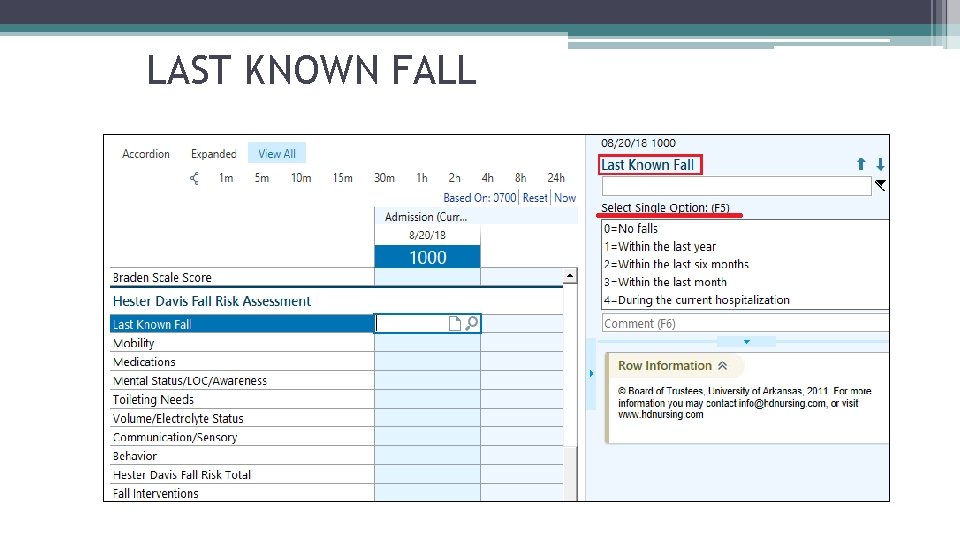
LAST KNOWN FALL The ONLY subcategory in which you choose JUST ONE of the following: 0 - No falls 1 - Within the last year ü Assess history ü Syncopal or mechanical fall ü ASK your patient 2 -Within the last 6 months 3 - Within the last month 4 - During the current hospitalization
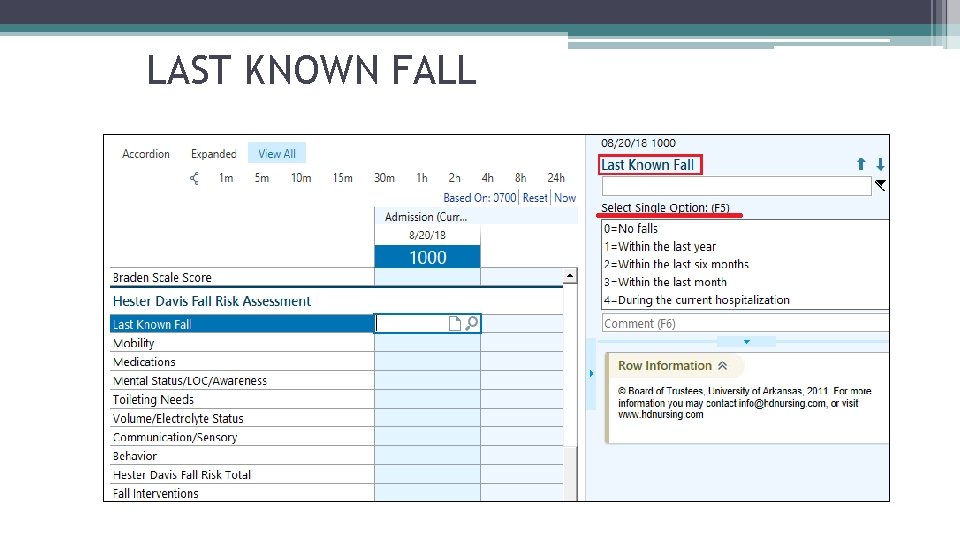
LAST KNOWN FALL
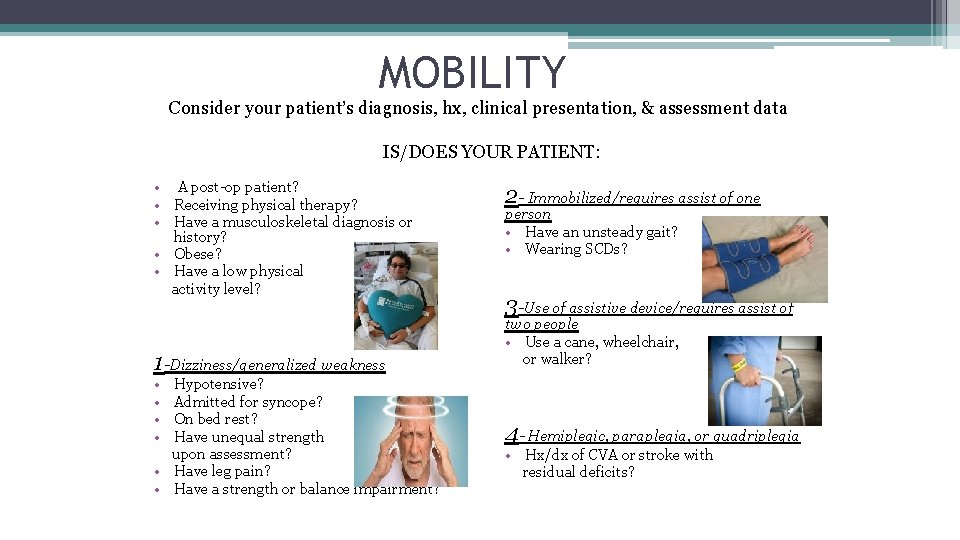
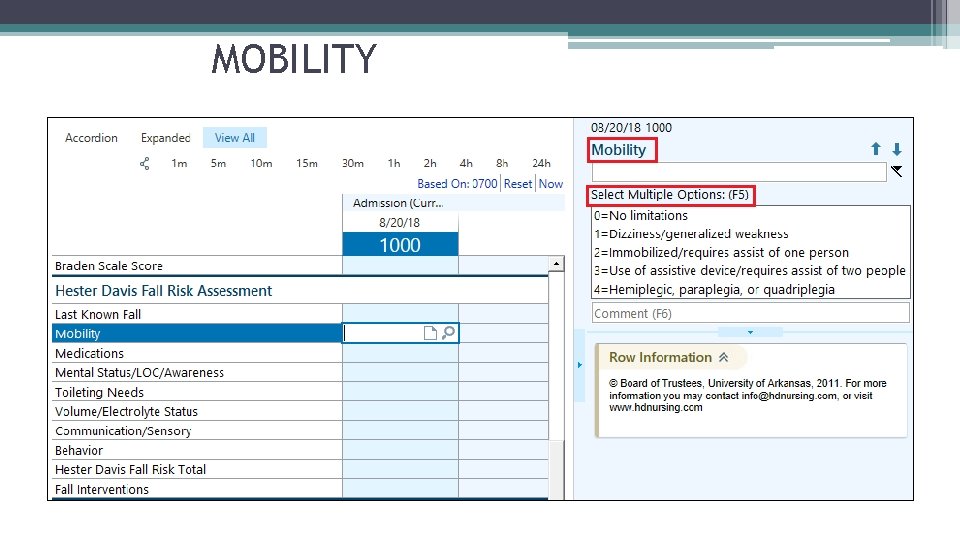
MOBILITY Consider your patient’s diagnosis, hx, clinical presentation, & assessment data IS/DOES YOUR PATIENT: • A post-op patient? • Receiving physical therapy? • Have a musculoskeletal diagnosis or history? • Obese? • Have a low physical activity level? 1 -Dizziness/generalized weakness • • Hypotensive? Admitted for syncope? On bed rest? Have unequal strength upon assessment? • Have leg pain? • Have a strength or balance impairment? 2 - Immobilized/requires assist of one person • Have an unsteady gait? • Wearing SCDs? 3 -Use of assistive device/requires assist of two people • Use a cane, wheelchair, or walker? 4 - Hemiplegic, paraplegia, or quadriplegia • Hx/dx of CVA or stroke with residual deficits?
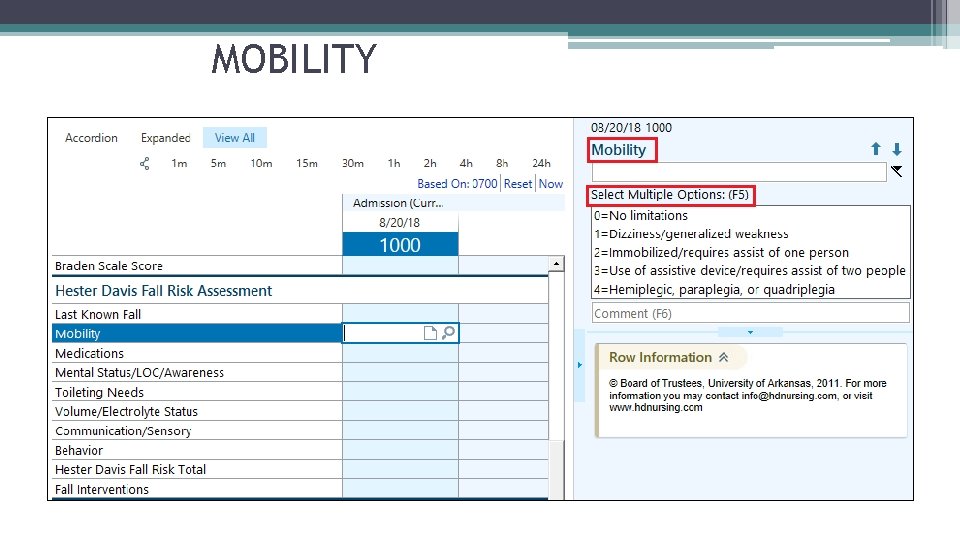
MOBILITY
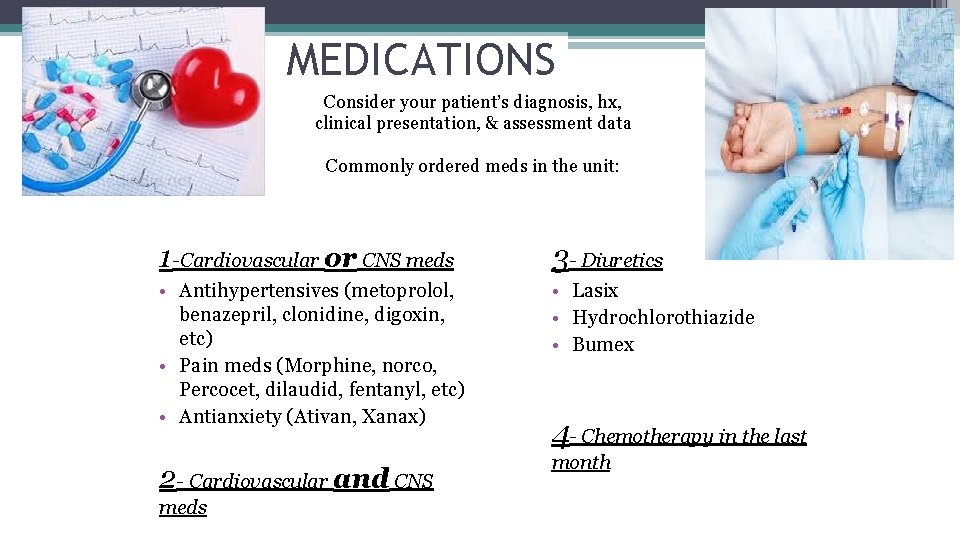
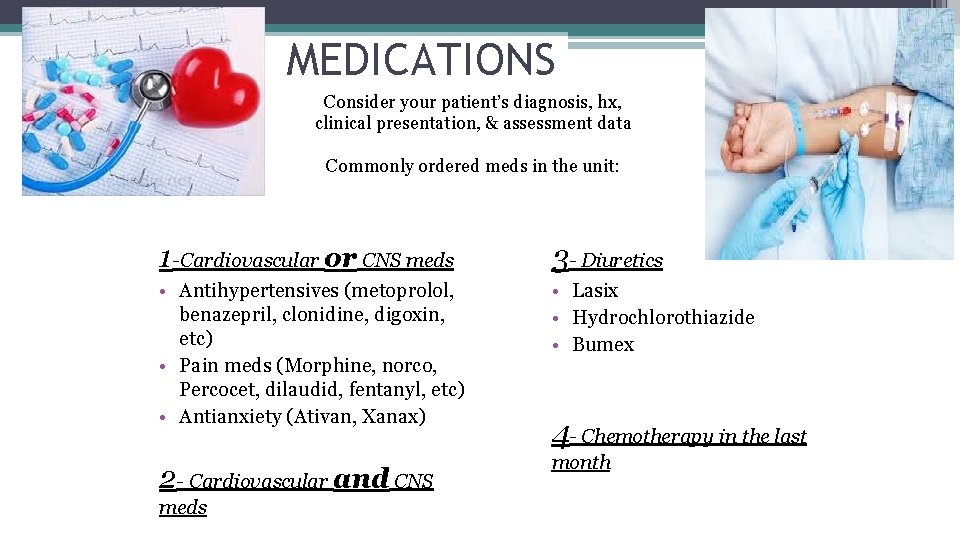
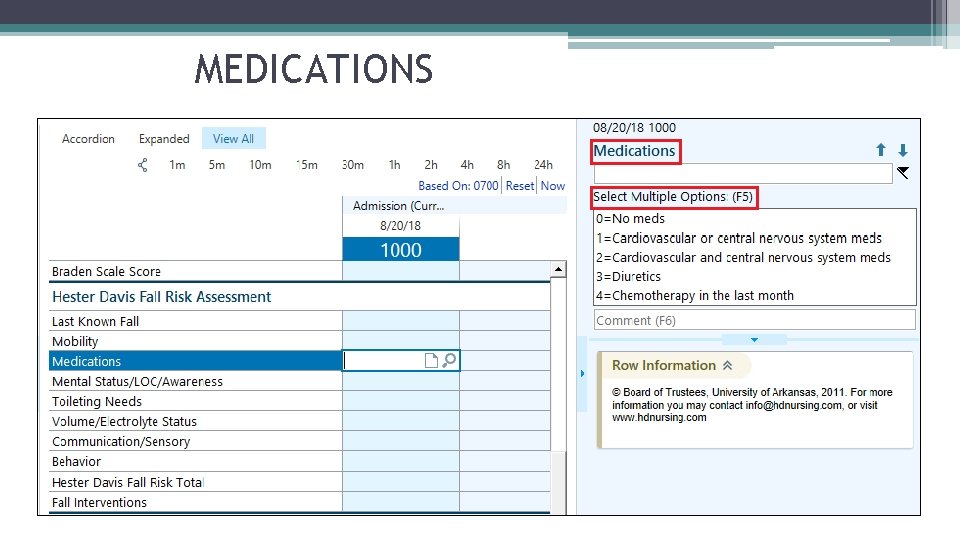
MEDICATIONS Consider your patient’s diagnosis, hx, clinical presentation, & assessment data Commonly ordered meds in the unit: 1 -Cardiovascular or CNS meds 3 - Diuretics • Antihypertensives (metoprolol, benazepril, clonidine, digoxin, etc) • Pain meds (Morphine, norco, Percocet, dilaudid, fentanyl, etc) • Antianxiety (Ativan, Xanax) • Lasix • Hydrochlorothiazide • Bumex 2 - Cardiovascular and CNS month meds 4 - Chemotherapy in the last
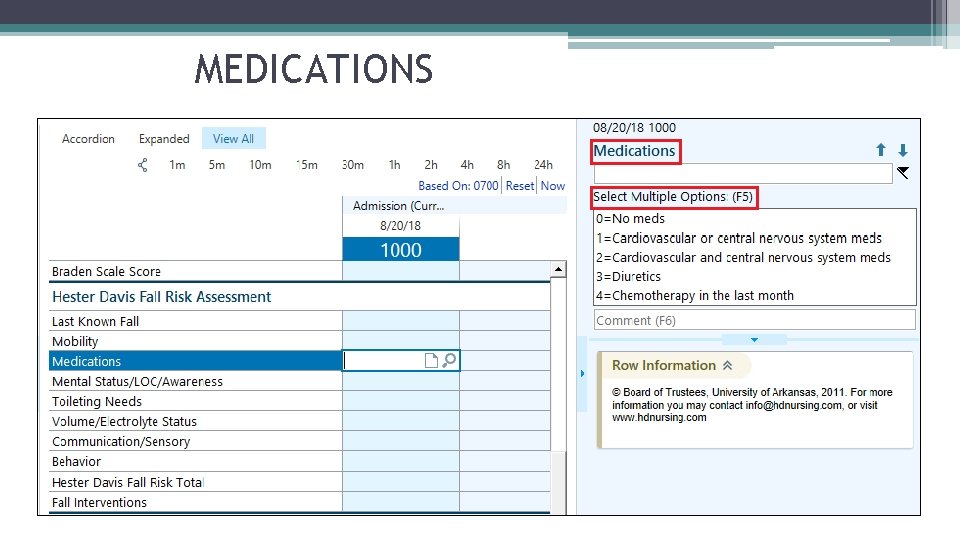
MEDICATIONS

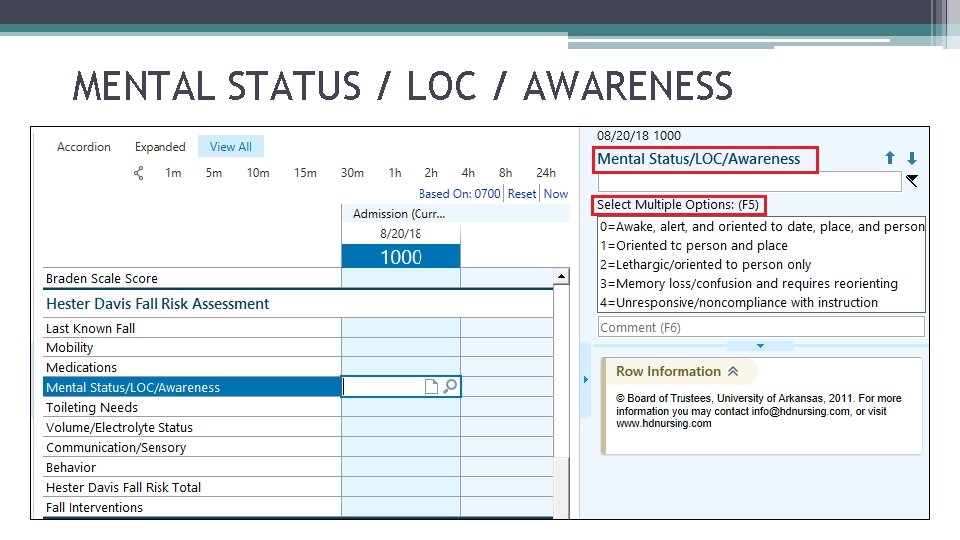
MENTAL STATUS / LOC / AWARENESS Consider your patient’s diagnosis, hx, clinical presentation, & assessment data 1 - Oriented to person & place 2 - Lethargic / Oriented to person only 3 - Memory loss / Confusion and requires reorienting 4 - Unresponsive / Noncompliant with instruction
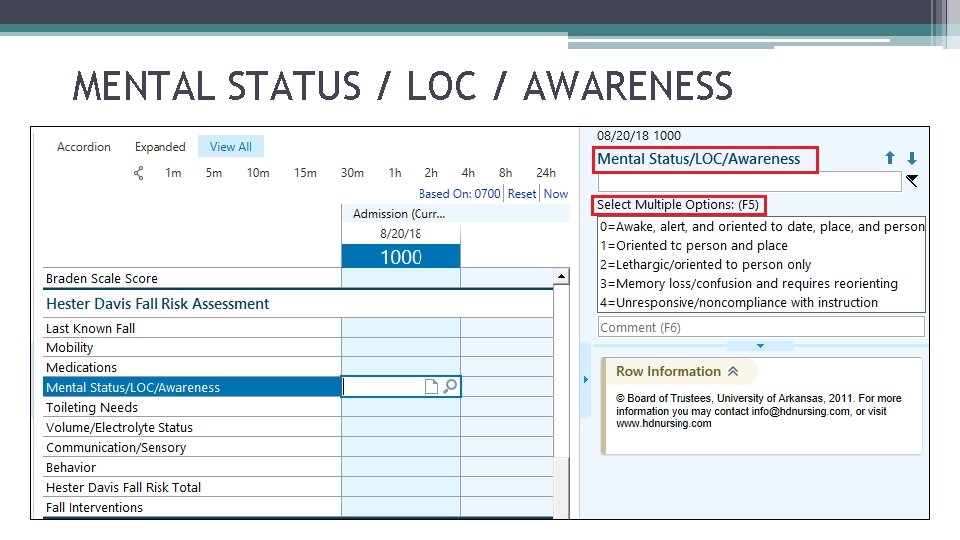
MENTAL STATUS / LOC / AWARENESS
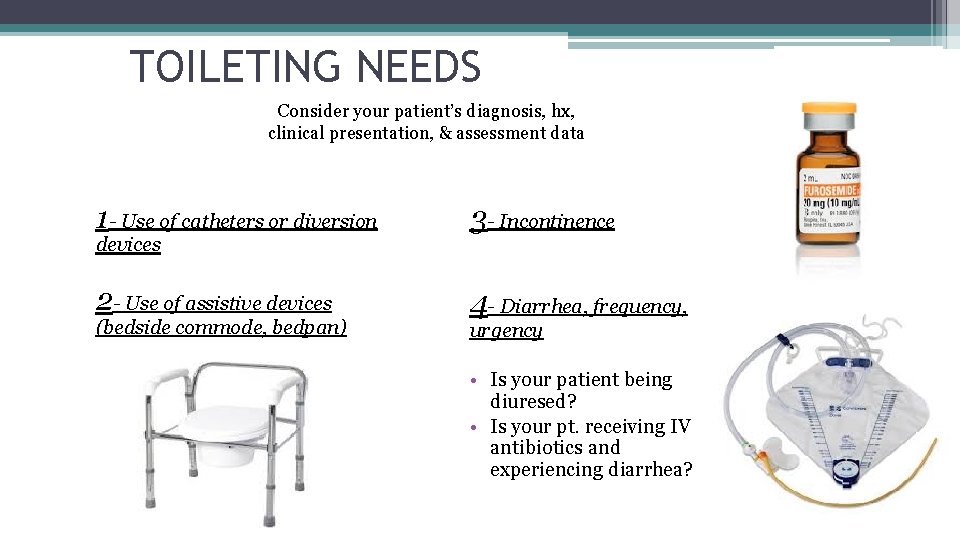
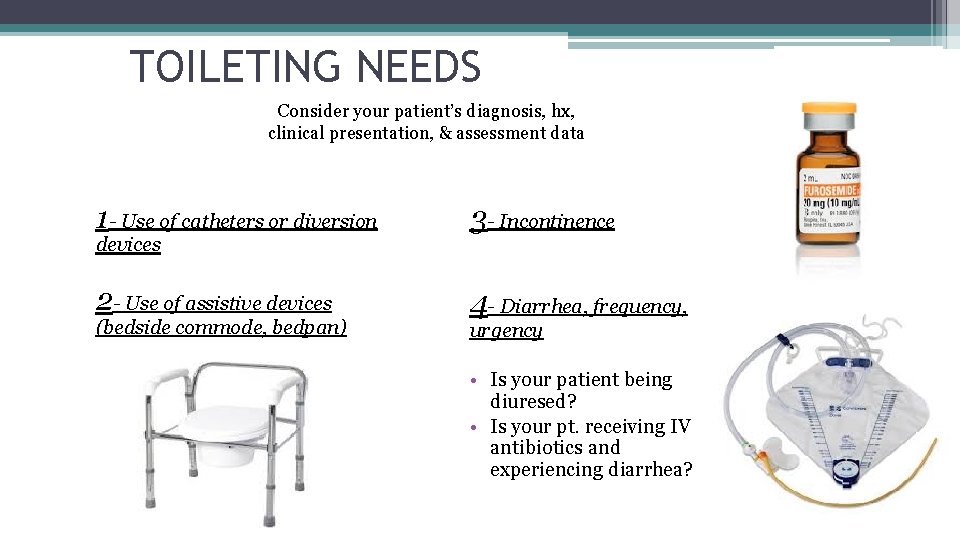
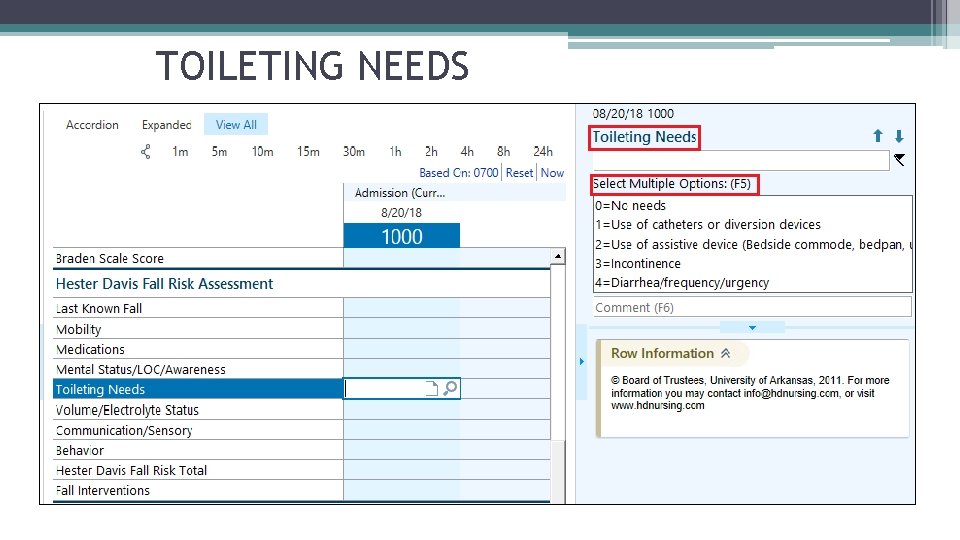
TOILETING NEEDS Consider your patient’s diagnosis, hx, clinical presentation, & assessment data 1 - Use of catheters or diversion 3 - Incontinence 2 - Use of assistive devices 4 - Diarrhea, frequency, devices (bedside commode, bedpan) urgency • Is your patient being diuresed? • Is your pt. receiving IV antibiotics and experiencing diarrhea?
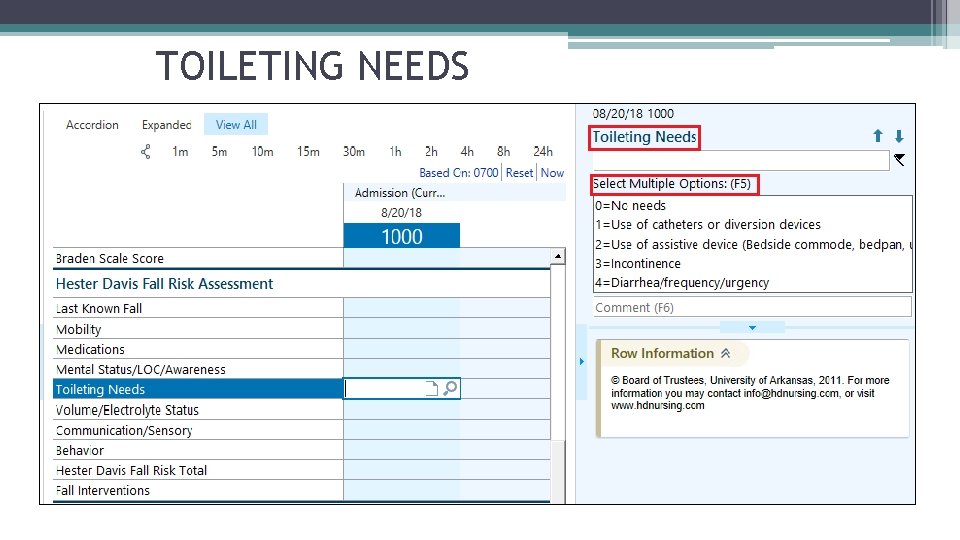
TOILETING NEEDS
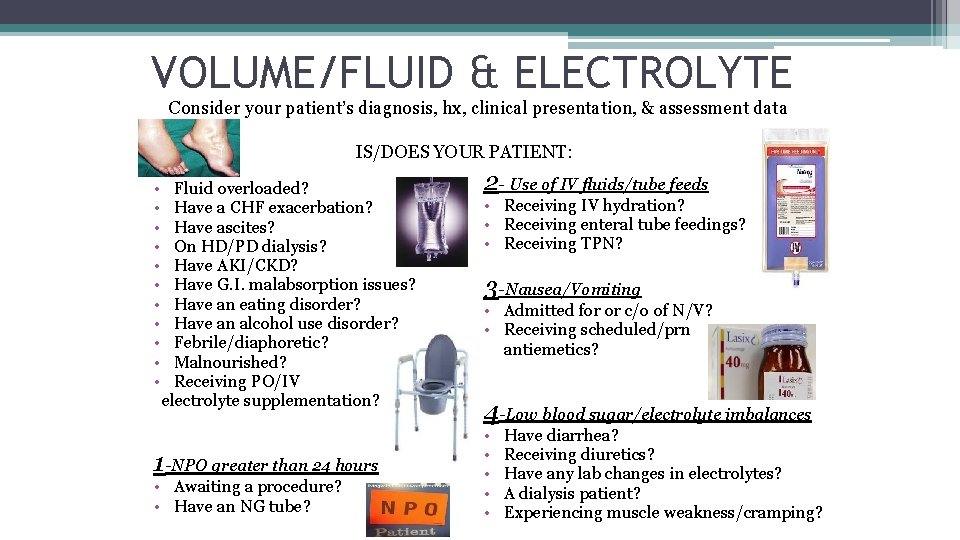
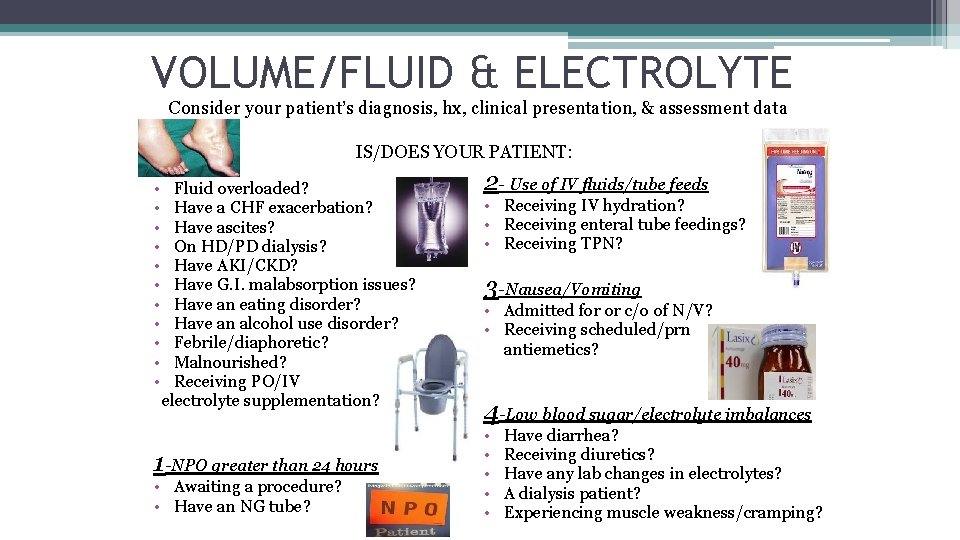
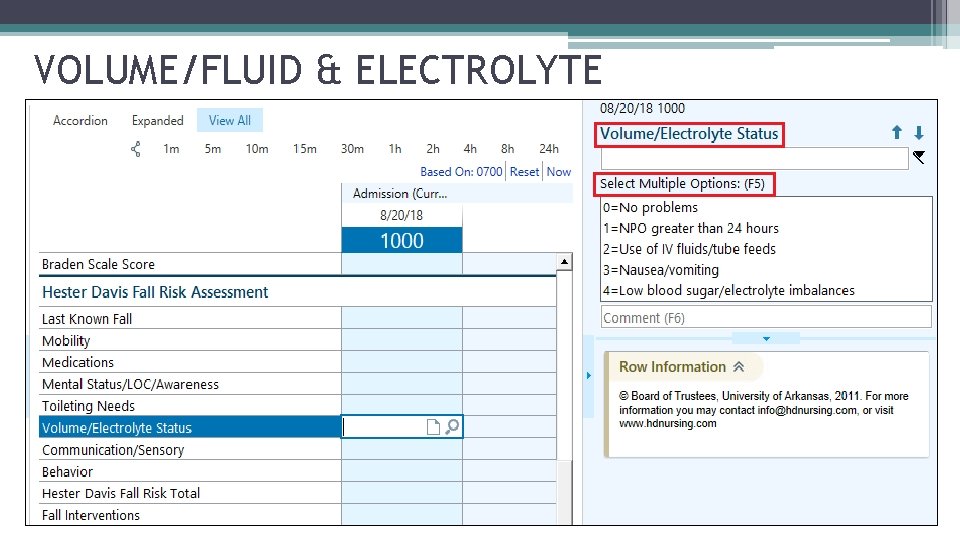
VOLUME/FLUID & ELECTROLYTE Consider your patient’s diagnosis, hx, clinical presentation, & assessment data IS/DOES YOUR PATIENT: • • • Fluid overloaded? Have a CHF exacerbation? Have ascites? On HD/PD dialysis? Have AKI/CKD? Have G. I. malabsorption issues? Have an eating disorder? Have an alcohol use disorder? Febrile/diaphoretic? Malnourished? Receiving PO/IV electrolyte supplementation? 1 -NPO greater than 24 hours • Awaiting a procedure? • Have an NG tube? 2 - Use of IV fluids/tube feeds • Receiving IV hydration? • Receiving enteral tube feedings? • Receiving TPN? 3 -Nausea/Vomiting • Admitted for or c/o of N/V? • Receiving scheduled/prn antiemetics? 4 -Low blood sugar/electrolyte imbalances • • • Have diarrhea? Receiving diuretics? Have any lab changes in electrolytes? A dialysis patient? Experiencing muscle weakness/cramping?
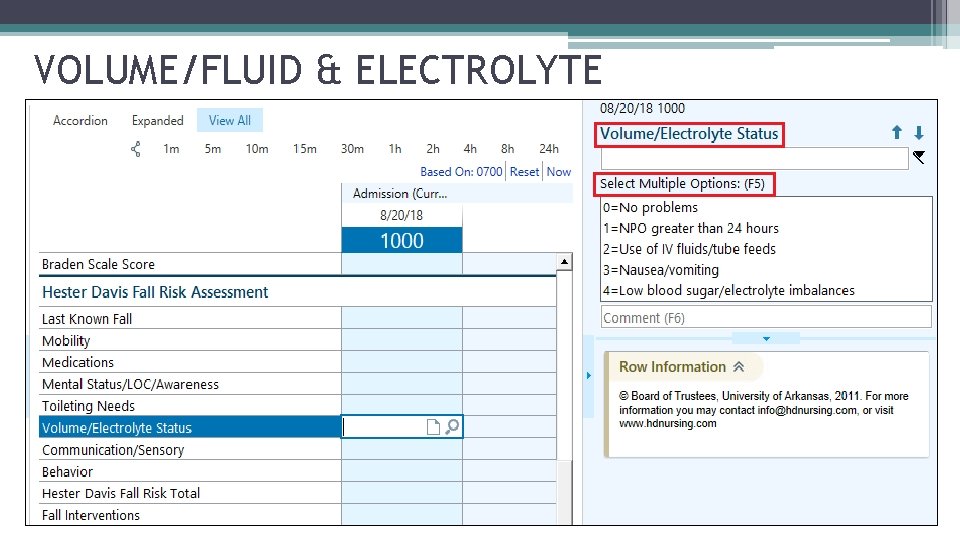
VOLUME/FLUID & ELECTROLYTE
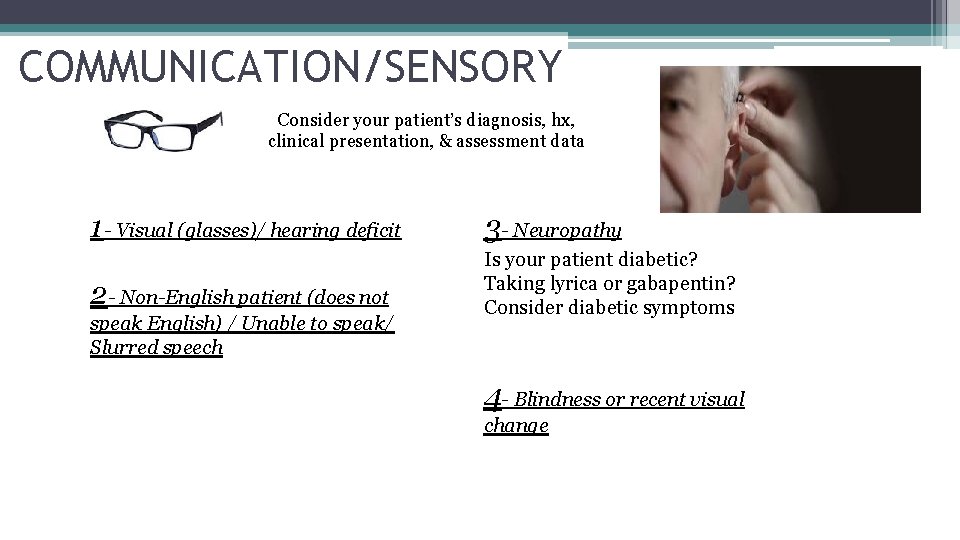
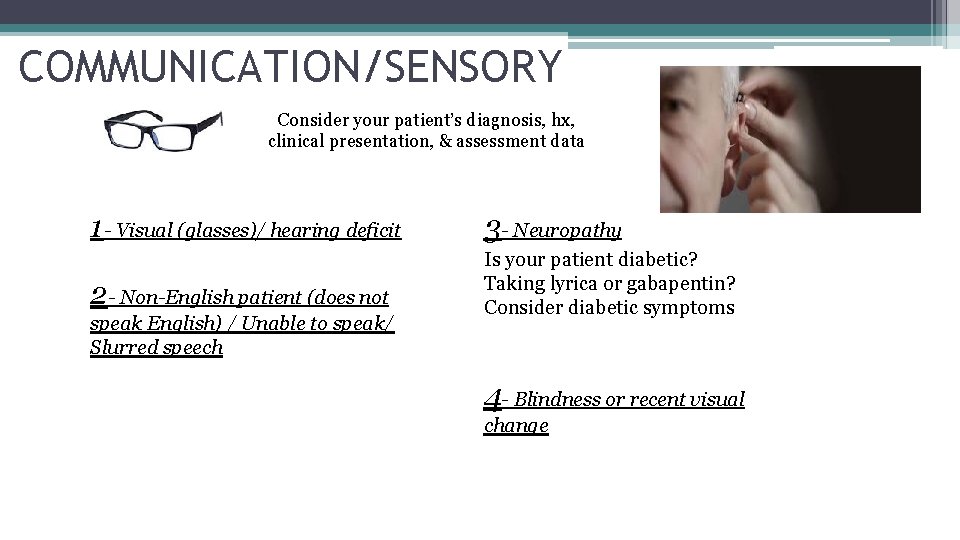
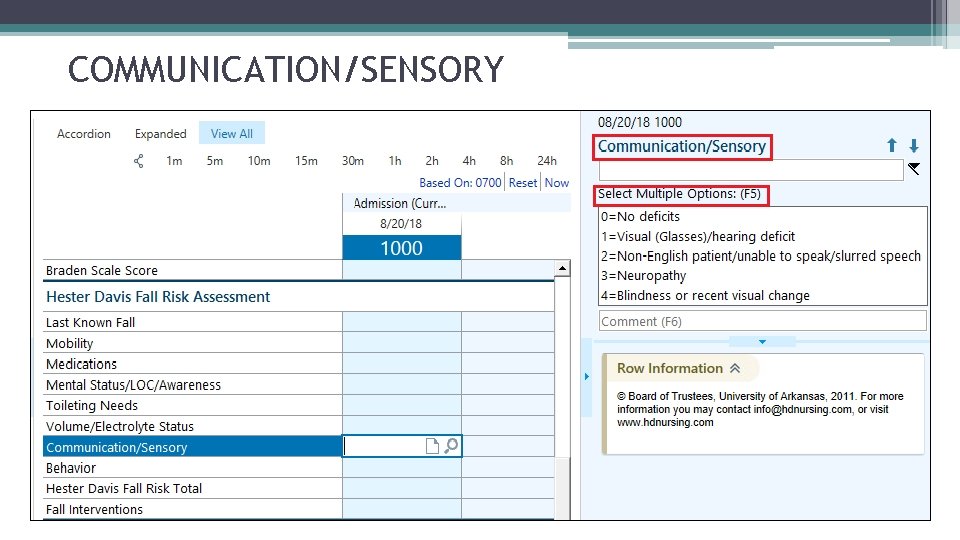
COMMUNICATION/SENSORY Consider your patient’s diagnosis, hx, clinical presentation, & assessment data 1 - Visual (glasses)/ hearing deficit 3 - Neuropathy 2 - Non-English patient (does not Is your patient diabetic? Taking lyrica or gabapentin? Consider diabetic symptoms speak English) / Unable to speak/ Slurred speech 4 - Blindness or recent visual change
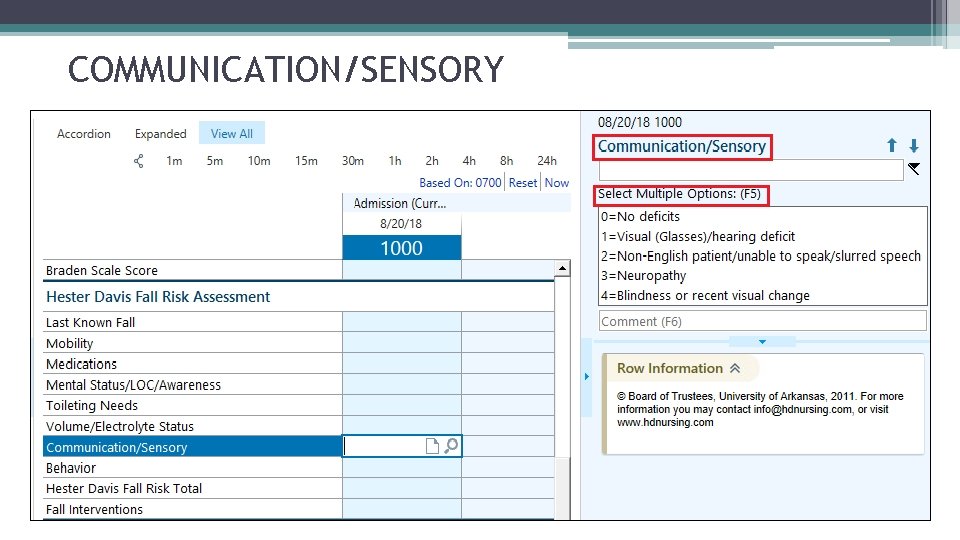
COMMUNICATION/SENSORY
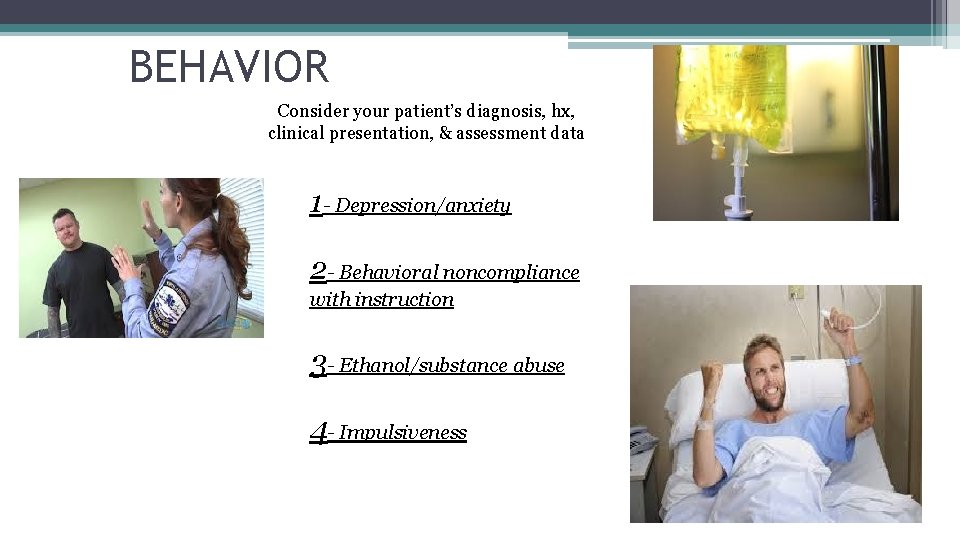
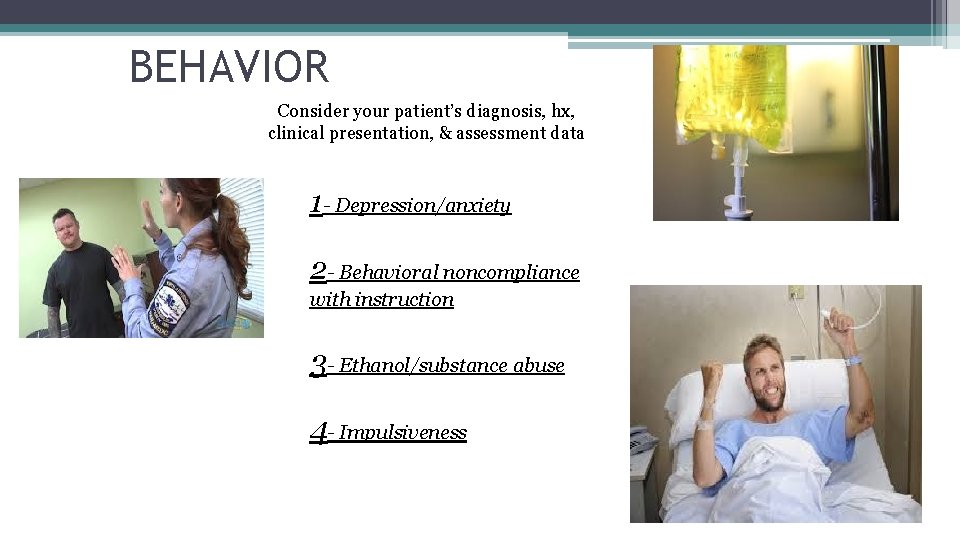
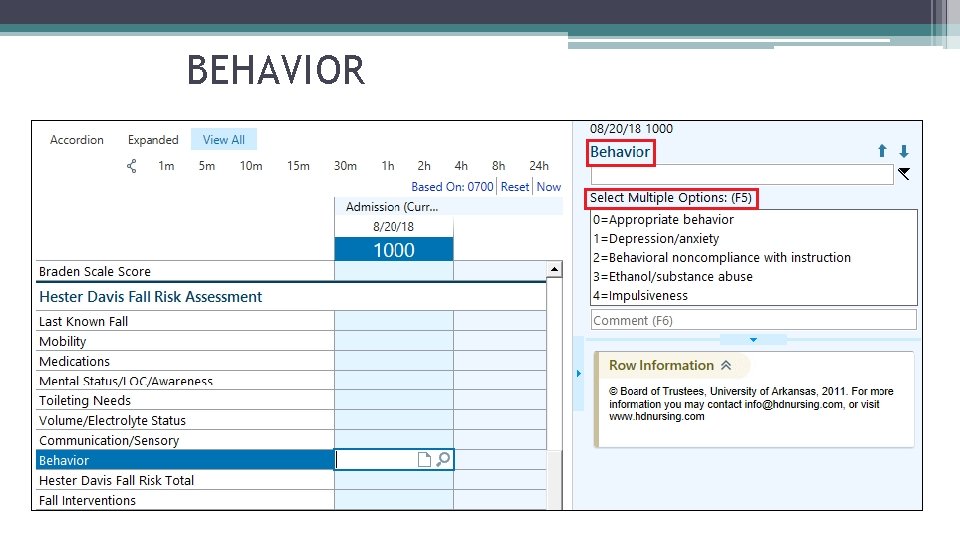
BEHAVIOR Consider your patient’s diagnosis, hx, clinical presentation, & assessment data 1 - Depression/anxiety 2 - Behavioral noncompliance with instruction 3 - Ethanol/substance abuse 4 - Impulsiveness
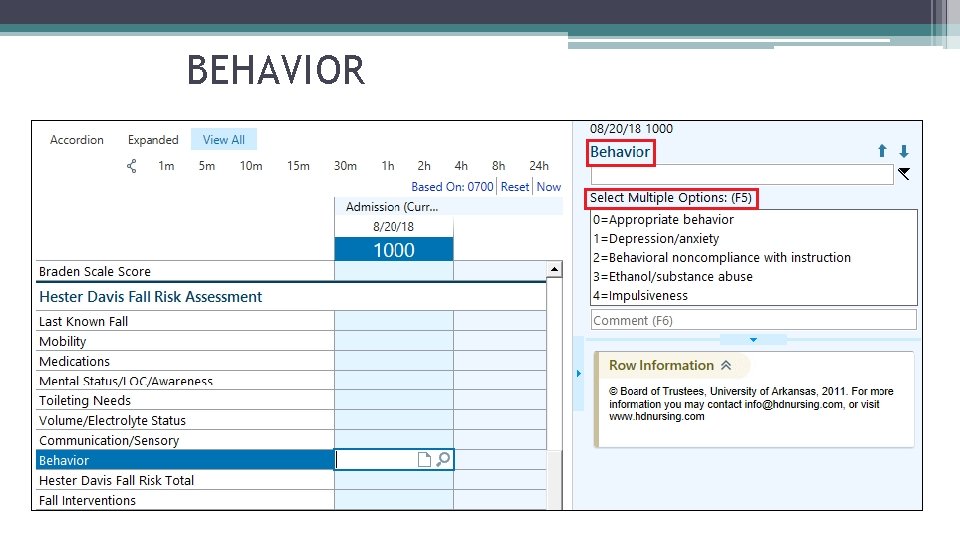
BEHAVIOR
Knowledge Check • Can you select more than one answer in each subcategory? • What does a score of 3 or greater in any subcategory indicate?
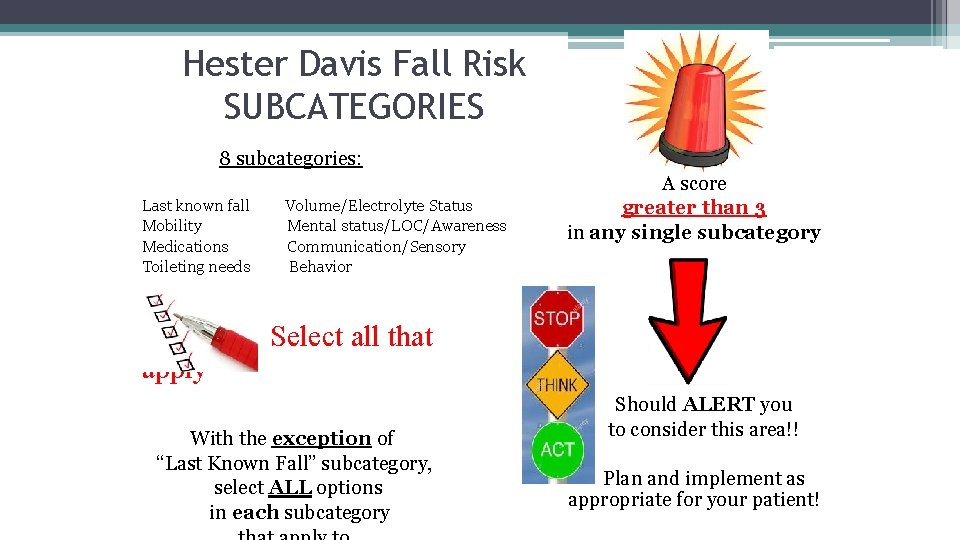
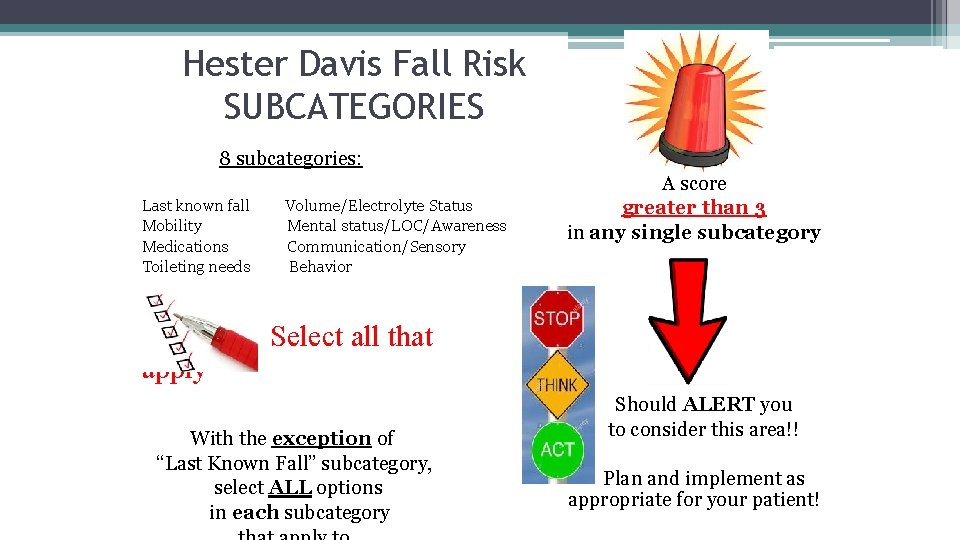
Hester Davis Fall Risk SUBCATEGORIES 8 subcategories: Last known fall Mobility Medications Toileting needs apply Volume/Electrolyte Status Mental status/LOC/Awareness Communication/Sensory Behavior A score greater than 3 in any single subcategory Select all that With the exception of “Last Known Fall” subcategory, select ALL options in each subcategory Should ALERT you to consider this area!! Plan and implement as appropriate for your patient!
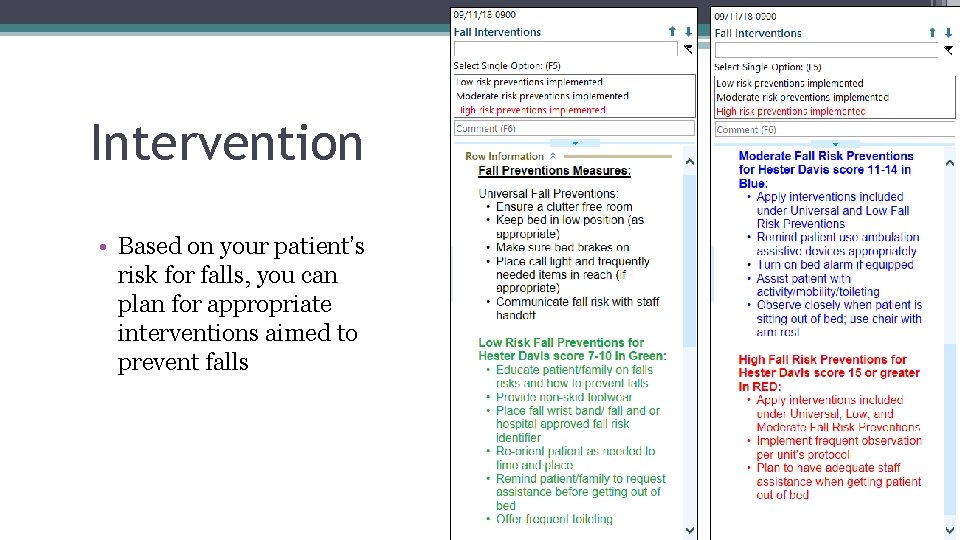
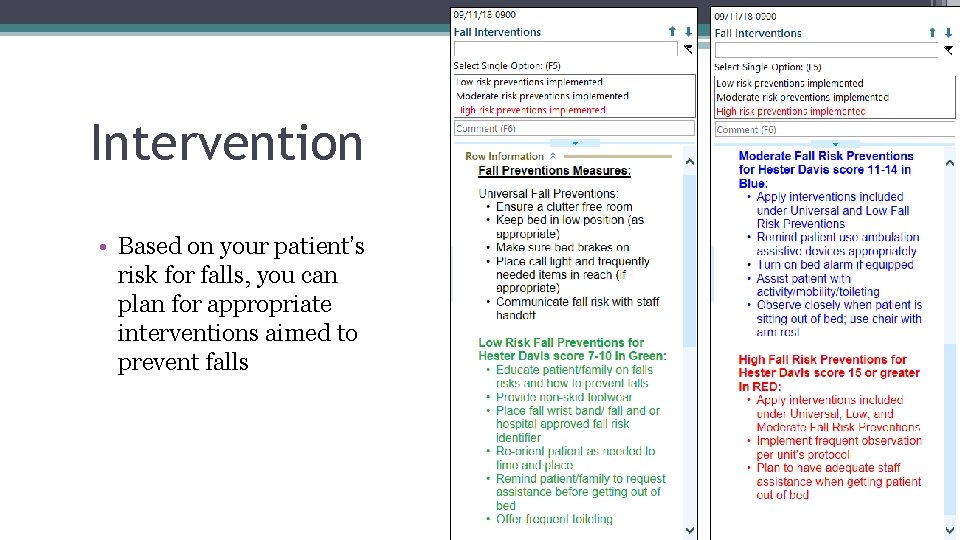
Intervention • Based on your patient’s risk for falls, you can plan for appropriate interventions aimed to prevent falls

Additional Interventions • Include ancillary teams (PT, OT, PCA) for fall prevention to strengthen team efforts • Use patient care boards to communicate fall risk status to patient’s and their families • Adding fall prevention for the plan for the day on the patient care board
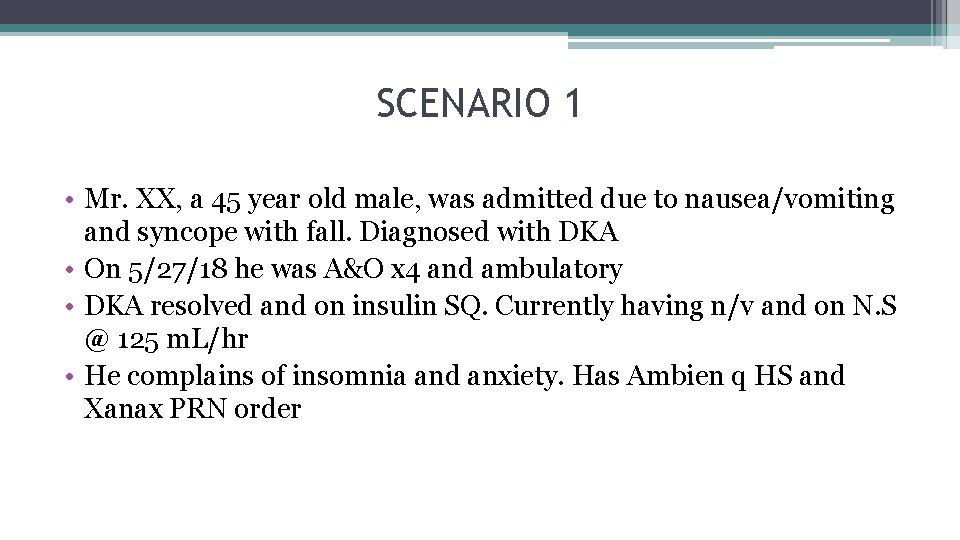
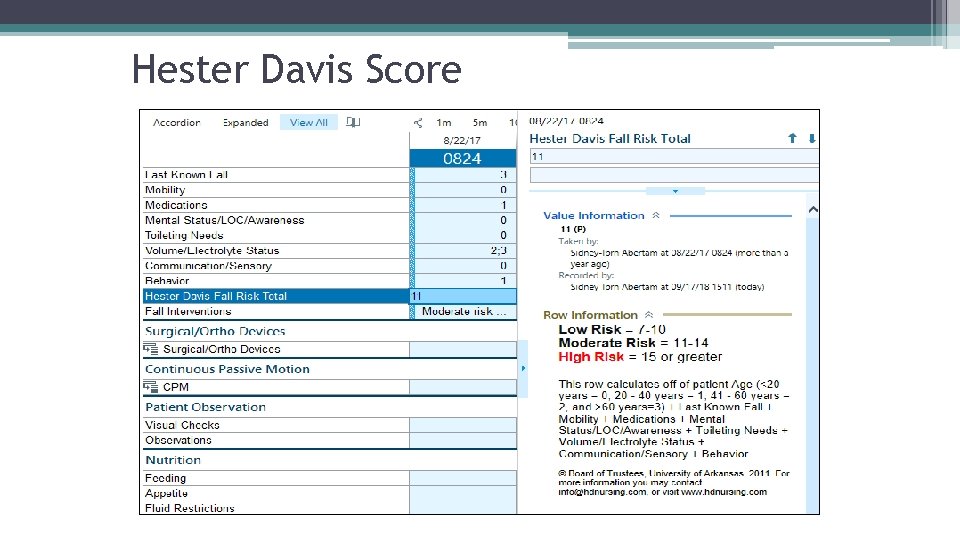
SCENARIO 1 • Mr. XX, a 45 year old male, was admitted due to nausea/vomiting and syncope with fall. Diagnosed with DKA • On 5/27/18 he was A&O x 4 and ambulatory • DKA resolved and on insulin SQ. Currently having n/v and on N. S @ 125 m. L/hr • He complains of insomnia and anxiety. Has Ambien q HS and Xanax PRN order
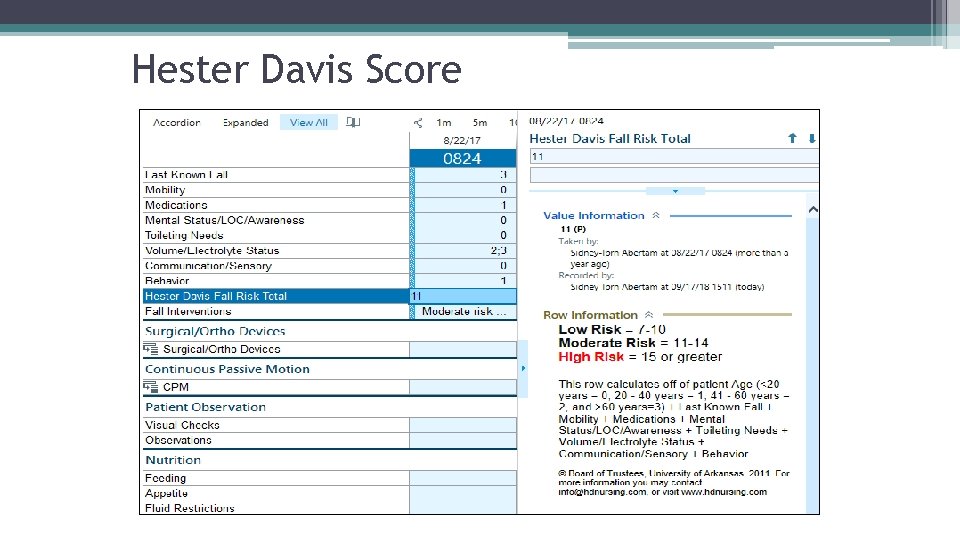
Hester Davis Score
Intervention • Patient is at moderate risk for falls. Implement moderate risk interventions. • However, if you have sub categories with a score > 3, you want to consider additional interventions pertinent for that category.
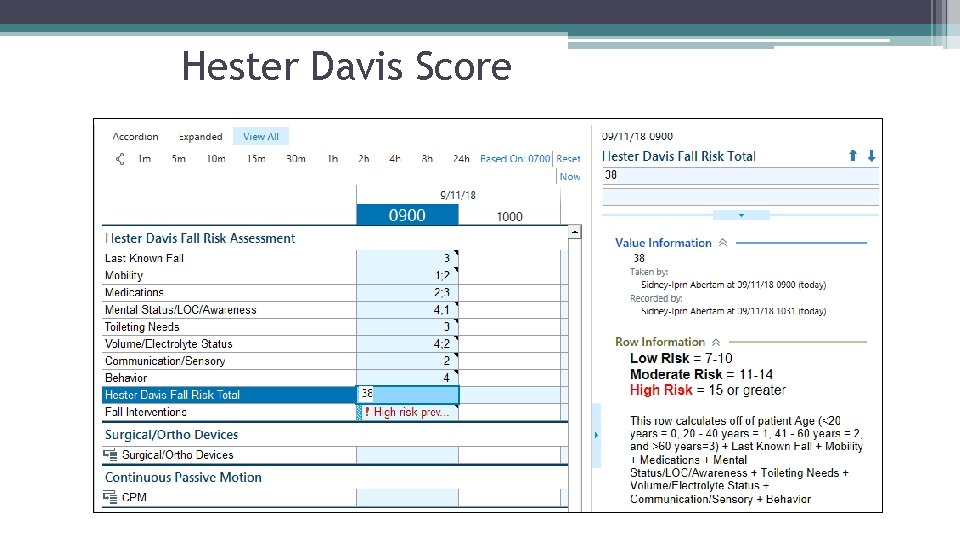
Scenario 2 • C. B, 72 year old female readmitted due to CHF exacerbation and had a fall a week ago at home. • Hx of CVA with right sided weakness and slurred speech. • Oriented to herself only and is delirious and impulsive. • Currently on Dobutamine gtt, Dopamine gtt and Bumex gtt. • Needing frequent electrolyte replacement. • Has Haldol PRN for agitation. • Pt is incontinent.
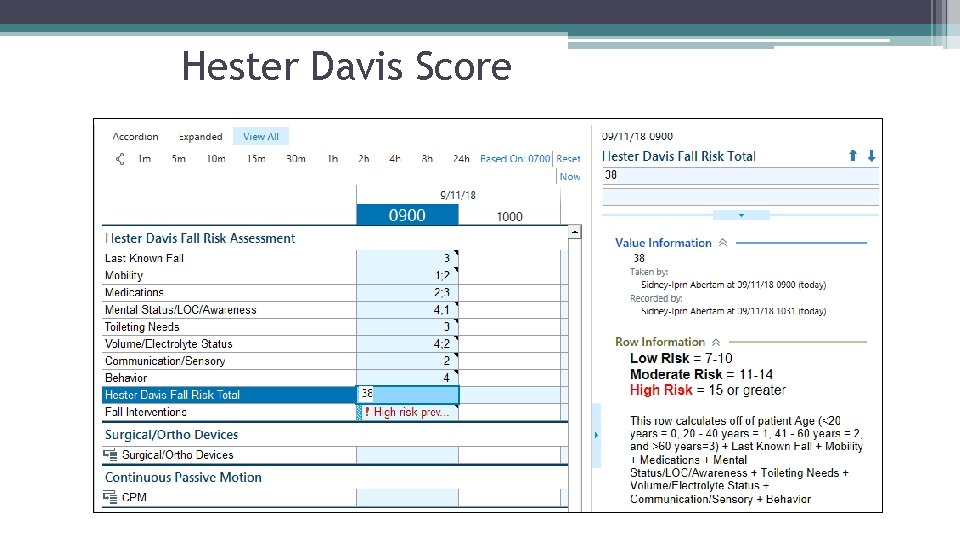
Hester Davis Score
Intervention • Patient is at HIGH risk for falls. Implement HIGH risk interventions. • However, if you have sub categories with a score > 3, you want to consider additional interventions pertinent for that category.
GROUP CASE STUDIES (15 minutes)
ROLE PLAY Let’s put those skills to action!
QUESTIONS?