The Healing Process Guidelines for Choosing the Proper



- Slides: 53
The Healing Process Guidelines for Choosing the Proper Modality
Choosing the Proper Modality � How do you know what to use, and how do you know when to use it? ◦ Theoretical knowledge ◦ Practical experience *You can’t follow the same recipe for every patient; avoid “cookie cutter” treatment plans
Modalities in a POC � Modalities should be an adjunct to TEs ◦ ROM and strengthening TEs are the desired end goal � Rehab protocols and progressions must be based primarily on the physiologic responses of the tissues to injury and on an understanding of how various tissues heal � What does this mean? ◦ The therapist must understand the healing process in order to choose the proper modality at the proper time
Modalities in a POC � Decisions on how and when modalities may be best used relies upon: ◦ Recognition of signs and symptoms ◦ Awareness of the time frames associated with the various phases of the healing process � Important to note that the healing process is a continuum ◦ 3 phases are identified ◦ Phases of the healing process overlap and have no true definitive beginning or end points
Check In � Question – Why do we need to understand the healing process in order to create an appropriate POC? � Answer – To pick proper modalities and TEs w/i proper timeframe � Question – In order to decide how and when modalities may be used, what 2 factors do we need to know? � Answer – Signs/symptoms; timeframes associated with phases of healing
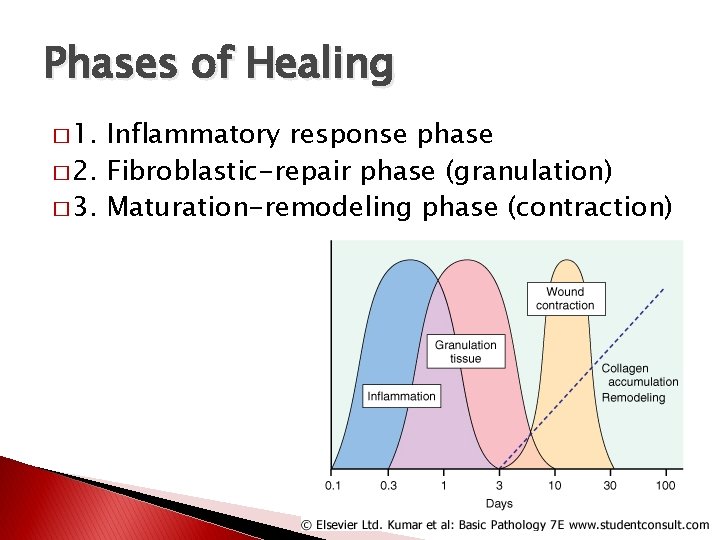
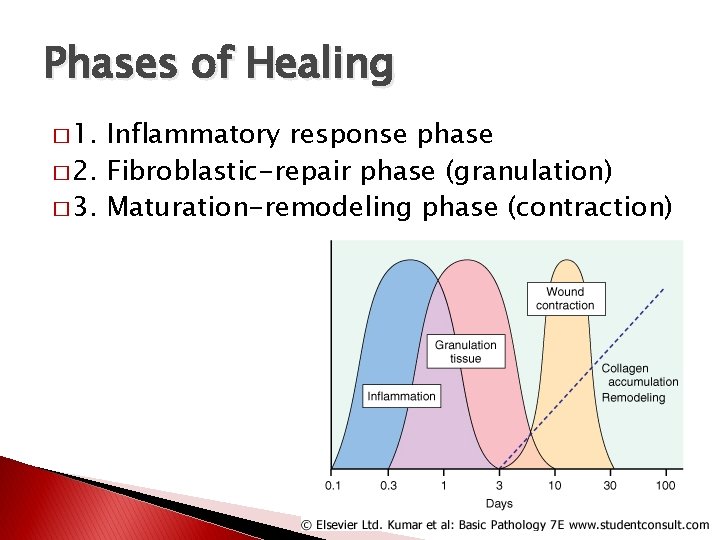
Phases of Healing � 1. Inflammatory response phase � 2. Fibroblastic-repair phase (granulation) � 3. Maturation-remodeling phase (contraction)
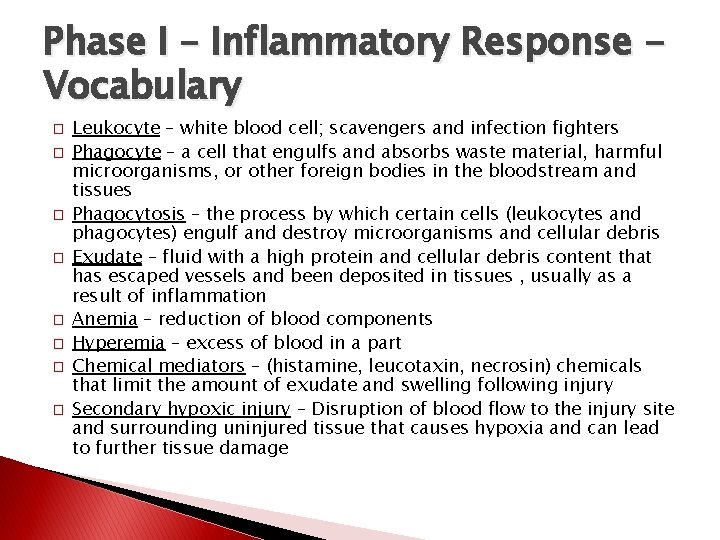
Phase I – Inflammatory Response Vocabulary � � � � Leukocyte – white blood cell; scavengers and infection fighters Phagocyte – a cell that engulfs and absorbs waste material, harmful microorganisms, or other foreign bodies in the bloodstream and tissues Phagocytosis – the process by which certain cells (leukocytes and phagocytes) engulf and destroy microorganisms and cellular debris Exudate – fluid with a high protein and cellular debris content that has escaped vessels and been deposited in tissues , usually as a result of inflammation Anemia – reduction of blood components Hyperemia – excess of blood in a part Chemical mediators – (histamine, leucotaxin, necrosin) chemicals that limit the amount of exudate and swelling following injury Secondary hypoxic injury – Disruption of blood flow to the injury site and surrounding uninjured tissue that causes hypoxia and can lead to further tissue damage
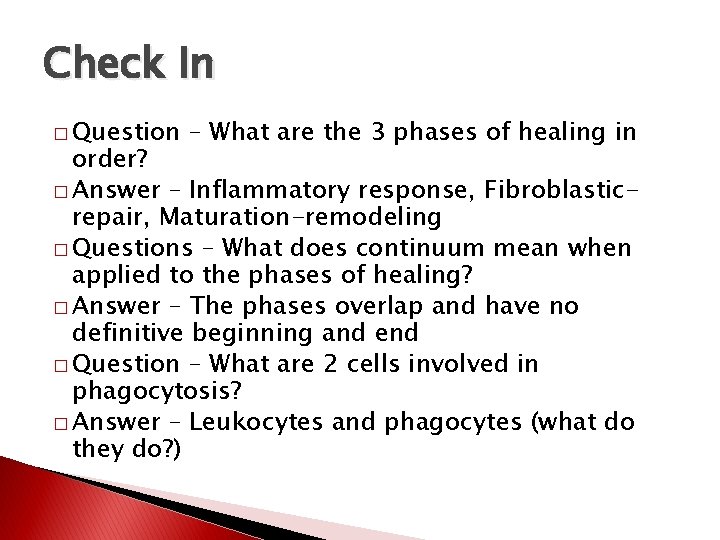
Check In � Question – What are the 3 phases of healing in order? � Answer – Inflammatory response, Fibroblasticrepair, Maturation-remodeling � Questions – What does continuum mean when applied to the phases of healing? � Answer – The phases overlap and have no definitive beginning and end � Question – What are 2 cells involved in phagocytosis? � Answer – Leukocytes and phagocytes (what do they do? )
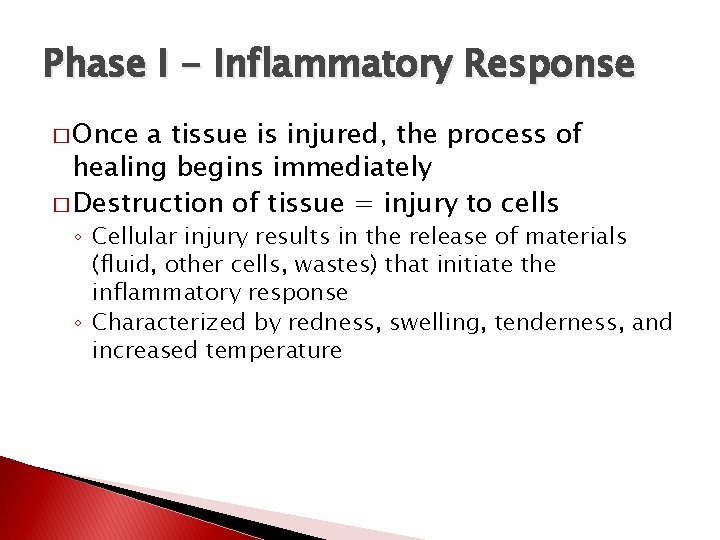
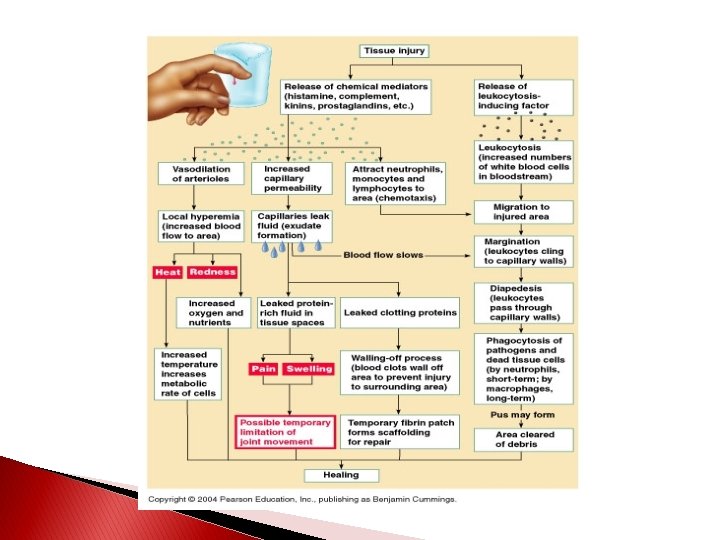
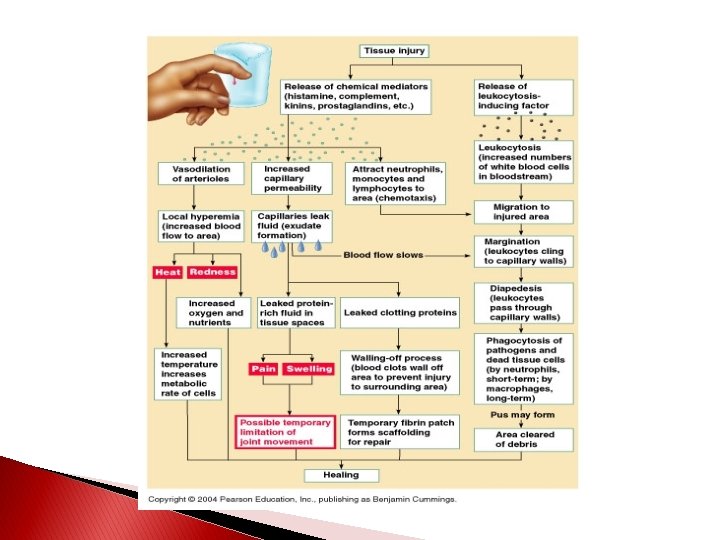
Phase I - Inflammatory Response � Once a tissue is injured, the process of healing begins immediately � Destruction of tissue = injury to cells ◦ Cellular injury results in the release of materials (fluid, other cells, wastes) that initiate the inflammatory response ◦ Characterized by redness, swelling, tenderness, and increased temperature
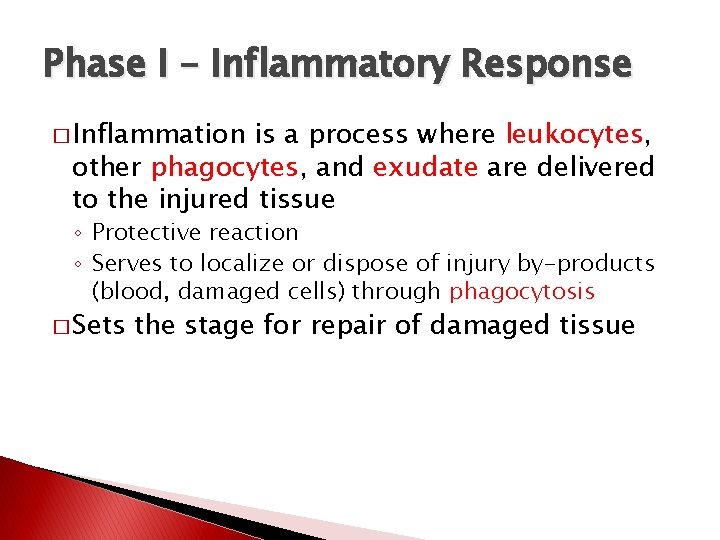
Phase I – Inflammatory Response � Inflammation is a process where leukocytes, other phagocytes, and exudate are delivered to the injured tissue ◦ Protective reaction ◦ Serves to localize or dispose of injury by-products (blood, damaged cells) through phagocytosis � Sets the stage for repair of damaged tissue
Phase I – Inflammatory Response � The immediate response to damage is constriction of the walls of the vessels (spasm) ◦ Lasts 5 -10 minutes ◦ Presses the inner walls of the vessels together to cause local anemia � This is followed by rapid hyperemia as the spasm reverses into dilation of the vessels ◦ Eventually the flow slows and stagnates � The initial movement of exudate into the tissues usually lasts 24 -36 hours (Swelling)
Check In � Question – Destruction of tissue = injury to ? , which in turn leads to the release of what? � Answer – Cells; fluids, other cells, wastes � Question - What does the release of these materials initiate? � Answer – Inflammatory response � Question – Why are leukocytes, phagocytes, and exudate delivered to the area? � Answer – Localize response to begin phagocytosis; protective reaction
Phase I – Inflammatory Response � Swelling � Good – Good or bad? ◦ The exudate brings cells to the injured area that help to eliminate dead cells, tissue, etc. ◦ It also helps to “splint” the area to limit movement � Bad ◦ Painful; ROM limitations; spasm; limits blood flow ◦ Can cause secondary hypoxic injury �The disruption of blood flow to the injured and surrounding healthy tissue causes hypoxia �Hypoxia (lack of oxygen) causes pain, spasm, and further tissue damage
Phase I – Inflammatory Response � Chemical mediators limit the amount of exudate and swelling � Histamine, leucotaxin, and necrosin ◦ Histamine – causes vasodilation and increased cell permeability ◦ Leucotaxin – assists fluid and WBC to move through cell walls to form exudate ◦ Necrosin – responsible for phagocytic activity � *Chemical mediators allow for just enough exudate formation and delivery, but not too much*
Phase I – Inflammatory Response � Platelets do not normally adhere to vessel walls ◦ Good thing, or we would form clots within blood vessels all the time! � Disruption of vessel walls allows platelets and leukocytes to adhere to the damaged spot ◦ This forms a plug to block lymph drainage and localize the injury response � Lastly the damaged cells release a protein that helps to form a fibrin clot that shuts off blood supply to the injured area ◦ Clot formation begins around 12 hours after injury and is completed by 48 hours
Phase I – Inflammatory Response � This combination of factors walls the injured area off during this stage � The leukocytes phagocytize most of the debris toward the end of the phase, which sets the stage for the fibroblastic phase � The initial inflammatory response phase lasts for approximately 2 to 4 days following injury
Check In � � � � � Question – On average, how long does the Inflammatory Response phase last? Answer – Approximately 2 -4 days Question – How long does it take to form a fibrin clot at the injury site? Answer – 12 -48 hours Question – How is swelling good? Answer – Exudate brings cells needed for healing; “splints” the area Question – How is swelling bad? Answer – Painful; limits ROM; can cause secondary hypoxic injury Question – What is a secondary hypoxic injury? Answer – Swelling causes lack of blood flow to uninjured tissue, leading to lack of oxygen and nutrients to healthy cells, leading to tissue death
Phase II – Fibroblastic-Repair Vocabulary � Collagen – the major protein of the white fibers of connective tissue, cartilage, and bone; “the glue that holds the body together” � Fibroblast – an immature, fiber-producing cell � Fibroplasia – period of scar formation � Granulation tissue – delicate connective tissue consisting of fibroblasts, collagen, and capillaries
Phase II – Fibroblastic-Repair � Fibroplasia begins within the first few hours following injury and may last for as long as 4 to 6 weeks � Production and regeneration of tissues leads to scar formation and repair of injured tissue ◦ During this period many of the s/s associated with the inflammatory response subside �Patients typically still report some tenderness and pain with certain stressful movements �As scar formation progresses, tenderness and pain gradually subside
Phase II – Fibroblastic-Repair � Inflammation causes a lack of oxygen to the injured area (hypoxia) � The body responds by growing new capillaries to deliver oxygenated blood ◦ Along with increased blood and oxygen delivery comes nutrients essential for tissue regeneration in the injured area � The fibrin clot begins to break down as new capillaries grow
Phase II – Fibroblastic Repair � The delivery of the nutrients, plus the breakdown of the fibrin clot, causes formation of granulation tissue ◦ Fills in the gaps during the healing process � The fibroblasts in the granulation tissue begin to (perform magic to) form the immature scar tissue � On day 6 or 7 they also begin depositing collagen fibers throughout the scar tissue ◦ Collagen fibers increase tensile strength of the scar ◦ As tensile strength increases, the number of fibroblasts decreases to signal the beginning of the next phase of healing
Check In � Question – When does Fibroblastic Repair begin? � Answer – Within the first few hours of injury (during the 1 st phase) � Question – What happens to tissues in the injured area during the Fibroblastic Repair phase? � Answer – Tissues are repaired and scar tissue is produced to fill in the area � Question – How does the body respond to hypoxia in the injured area? � Answer – The body grows new capillaries � Question - What are the names of the 2 new tissues being produced to fill in the injured space? � Answer – Collagen and granulation tissue
Phase III – Maturation-Remodeling � The is a long-term process � Features realignment or remodeling of the collagen fibers that make up the scar tissue according to the tensile forces to which the scar in subjected ◦ Ongoing process of breakdown and synthesis of collagen that causes an increase in tensile strength of the scar
Phase III – Maturation-Remodeling � With increased stress and strain the collagen fibers realign in a position of maximum efficiency parallel to the lines of tension ◦ The tissue gradually assumes a normal appearance and function ◦ Rarely as strong as uninjured tissue � Usually by the end of approximately 3 weeks a firm, strong, contracted, nonvascular scar exists � The maturation phase of healing may require several years to be totally complete
Check In � Question – Why are therapeutic exercises often used in PT during the Maturation. Remodeling phase of healing? � Answer – To provide tensile forces on the maturing scar tissue in order to cause collagen fibers to line up properly for strength � Question – How long does the Maturation – Remodeling phase take to complete? � Answer – Up to several years
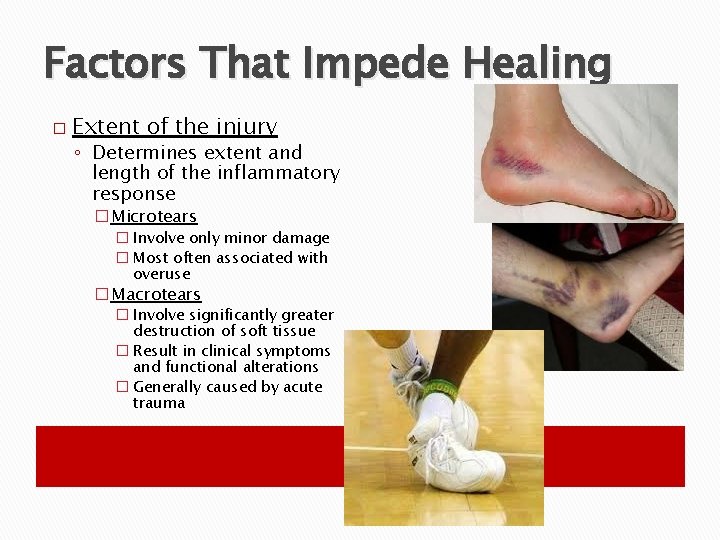
Factors That Impede Healing � Extent of the injury ◦ Determines extent and length of the inflammatory response �Microtears � Involve only minor damage � Most often associated with overuse �Macrotears � Involve significantly greater destruction of soft tissue � Result in clinical symptoms and functional alterations � Generally caused by acute trauma
Factors That Impede Healing � Edema ◦ Increases pressure caused by swelling slows the healing process via: �Separation of tissues �Inhibiting neuromuscular control �Impeding nutrient delivery in the injured part � This is why edema control is so important during initial first aid

Factors That Impede Healing � Hemorrhage ◦ Even the smallest amount of damage to the capillaries causes bleeding ◦ Produces the same negative effects as edema � The presence of bleeding produces additional tissue damage and thus makes the injury worse
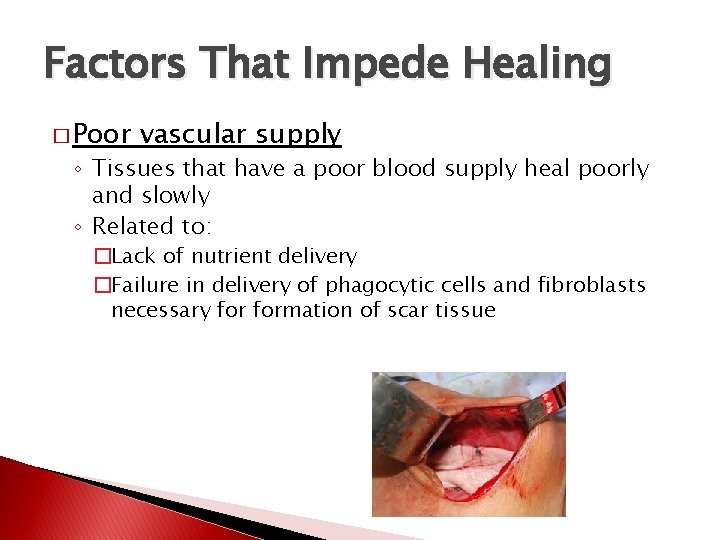
Factors That Impede Healing � Poor vascular supply ◦ Tissues that have a poor blood supply heal poorly and slowly ◦ Related to: �Lack of nutrient delivery �Failure in delivery of phagocytic cells and fibroblasts necessary formation of scar tissue
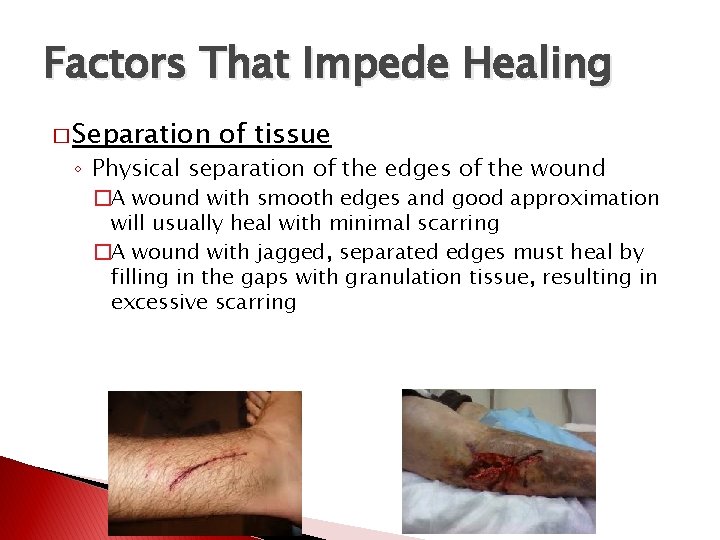
Factors That Impede Healing � Separation of tissue ◦ Physical separation of the edges of the wound �A wound with smooth edges and good approximation will usually heal with minimal scarring �A wound with jagged, separated edges must heal by filling in the gaps with granulation tissue, resulting in excessive scarring
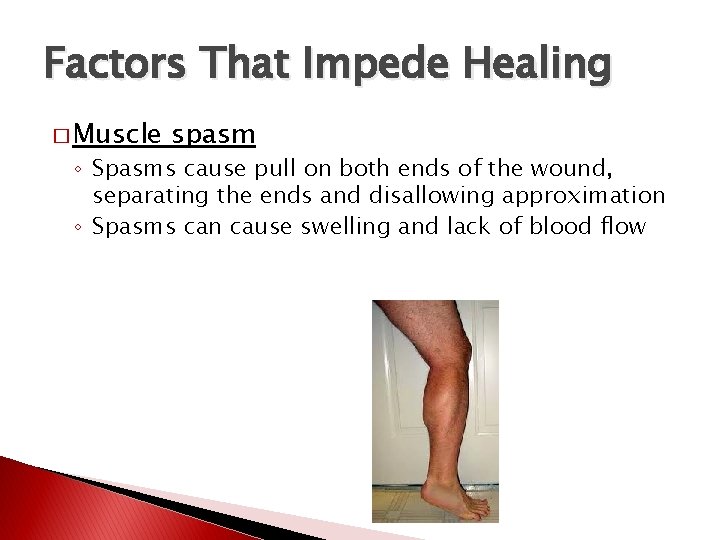
Factors That Impede Healing � Muscle spasm ◦ Spasms cause pull on both ends of the wound, separating the ends and disallowing approximation ◦ Spasms can cause swelling and lack of blood flow
Factors That Impede Healing � Atrophy ◦ Wasting away of muscle tissue begins immediately with injury ◦ Strengthening and early movement of the injured structure minimizes atrophy

Factors That Impede Healing � Corticosteroids ◦ Use of corticosteroids in early stages of healing can inhibit fibroplasia, capillary formation, and collagen synthesis
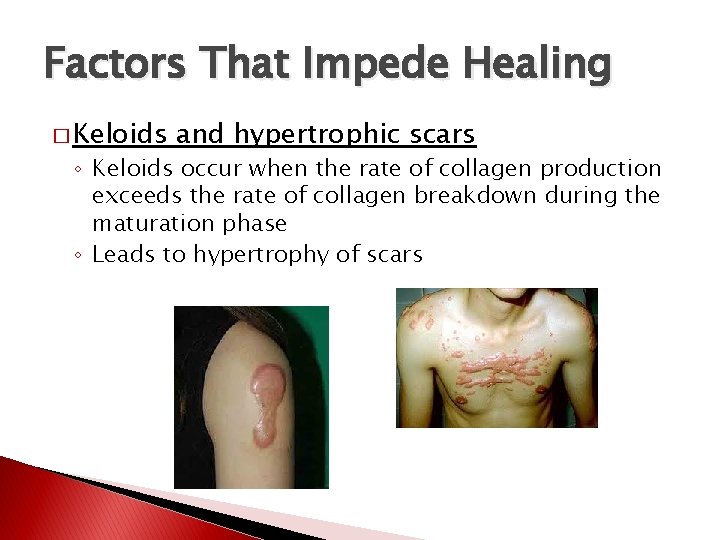
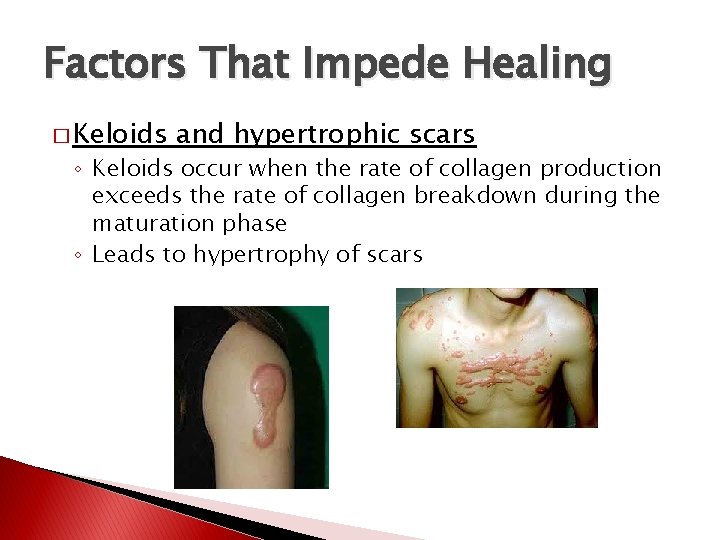
Factors That Impede Healing � Keloids and hypertrophic scars ◦ Keloids occur when the rate of collagen production exceeds the rate of collagen breakdown during the maturation phase ◦ Leads to hypertrophy of scars
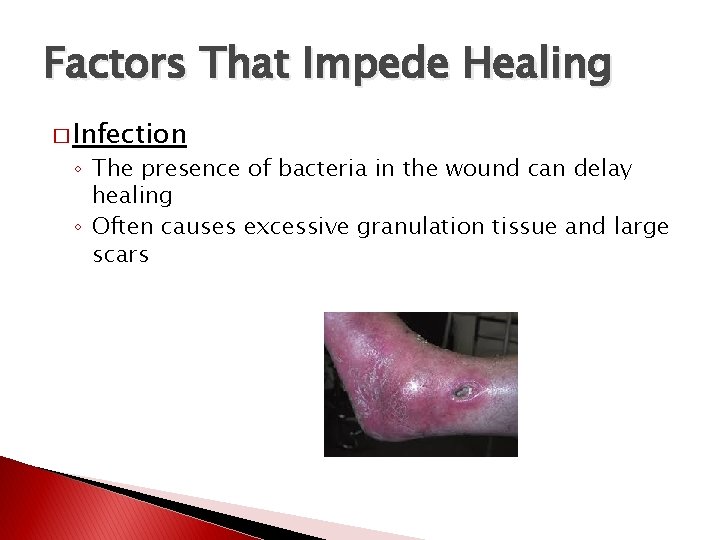
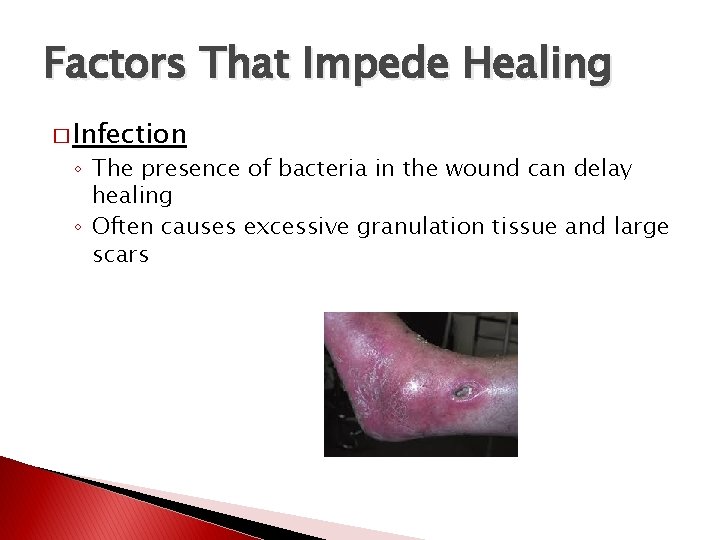
Factors That Impede Healing � Infection ◦ The presence of bacteria in the wound can delay healing ◦ Often causes excessive granulation tissue and large scars
Factors That Impede Healing � Humidity, climate, oxygen tension ◦ Humidity increases the process of forming epithelium �A moist wound promotes the migration of the necrotic tissue to the surface where it is shed ◦ Oxygen tension relates to optimal oxygen saturation and maximal tensile strength development
Factor That Impede Healing � Health, age, and nutrition ◦ Elastic qualities of skin decrease with age ◦ Degenerative diseases also affect wound healing ◦ Nutrition greatly affects wound healing �Vitamins C (scurvy), K (clotting), and A & E (collagen synthesis) �Zinc (enzyme systems) �Amino acids (cell walls)
Injury Management Using Modalities � No matter how old an injury is, it should be classified according to the signs and symptoms (acute vs. chronic) � If the classic s/s of inflammation are present, treat injury as if it is in the inflammatory response phase ◦ S/S of active inflammation present = acute injury ◦ S/S are no longer present = chronic injury
Injury Management Using Modalities � Based upon this definition of acute and chronic, the rehab progression following injury will be based upon 4 phases: ◦ ◦ 1. 2. 3. 4. � The Initial acute Inflammatory response Fibroblastic-repair Maturation-remodeling phases overlap, and time frames vary between patients
Initial Acute Injury Phase � Modality use should be directed toward limiting swelling and reducing pain ◦ ◦ ◦ Cryotherapy (+ elevation) Compression (+ elevation) Electrical stimulation Ultrasound Laser � (Rest – 48 -72 hours)
Initial Acute Injury Phase � Cryotherapy – reduce swelling and pain ◦ Ice bags, cold packs, ice massages ◦ Not cold baths or cold whirlpools � Most important function is to produce analgesia � Should be used with elevation

Initial Acute Injury Phase � Compression (+ elevation) ◦ Intermittent compression (pumping action) � Compression + cold = better � Compression + cold + elevation = best
Initial Acute Injury Phase � Electrical stimulation ◦ Used to address pain in this phase ◦ Avoid intensities that cause muscle contraction as it may increase clotting time
Initial Acute Injury Phase � Ultrasound ◦ Can be used to facilitate healing when used immediately after injury through the 1 st 48 hours ◦ Lower intensities produce nonthermal effects that alter cell membrane permeability to ions that aide in healing
Initial Acute Injury Phase � Low-power laser ◦ Effective in pain modulation ◦ Low power is used so as not to cause tissue death
Inflammatory Response Phase � Begins as early as day 1 and may last as long as day 6 post injury � Goals similar to initial acute injury phase � Modalities include: ◦ Cryotherapy ◦ ◦ �Important to not switch to heat modalities too early �May use contrast baths with longer cold to hot ratio Compression E-stim L-p laser US
Inflammatory Response Phase � After initial acute injury phase, the patient should work on AROM and PROM � Exercise progression determined by injury’s response to exercise � If s/s of inflammation increase with exercise, reduce intensity � Aggressive rehab is desirable, but will always be limited by the healing process
Fibroblastic-Repair Phase � As early as day 4 post-injury and may last a few weeks ◦ Swelling has usually stopped ◦ Tenderness remains with touch and ROM exercises � Modalities ◦ ◦ ◦ include: Cryotherapy => Thermotherapy Compression E-stim Low-power laser US ROM and strengthening exercises
Fibroblastic-Repair Phase � Treatments may switch from cold to heat ◦ Use swelling as an indicator � Thermotherapy increases circulation to an area to promote healing and reduce pain ◦ Includes moist hot packs, paraffin, fluidotherapy, and warm whirlpool
Fibroblastic-Repair Phase � Intermittent compression – facilitates removal of by-products from area � E-stim – now used to elicit muscle contraction for a muscle pumping action to aid in lymphatic flow and to reduce pain � Low-power laser to reduce pain � Ultrasound for nonthermal effects – increase healing factors
Maturation-Remodeling Phase � May last several years � Main goal is to return to activity � The collagen fibers must be realigned according to tensile stresses and strains placed upon them � Most to all modalities are typically safe to use in this phase � Massage is particularly effective in this phase to assist in scar remodeling
Maturation-Remodeling Phase � Thermotherapy ◦ Deep heating most beneficial �Ultrasound, shortwave and microwave diathermy �Increased blood and lymphatic flow ◦ Superficial heating less effective, though helpful for pain and flexibility � E-stim ◦ Pain modulation ◦ Muscle contractions for increasing ROM and strength � Low-powered laser ◦ Pain modulation