The Female Reproductive System Chapter 28 Lecture 17
- Slides: 22
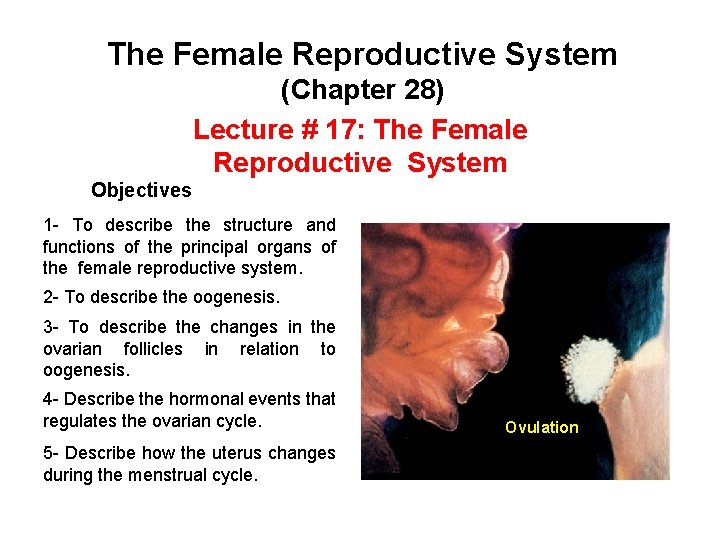
The Female Reproductive System (Chapter 28) Lecture # 17: The Female Reproductive System Objectives 1 - To describe the structure and functions of the principal organs of the female reproductive system. 2 - To describe the oogenesis. 3 - To describe the changes in the ovarian follicles in relation to oogenesis. 4 - Describe the hormonal events that regulates the ovarian cycle. 5 - Describe how the uterus changes during the menstrual cycle. Ovulation
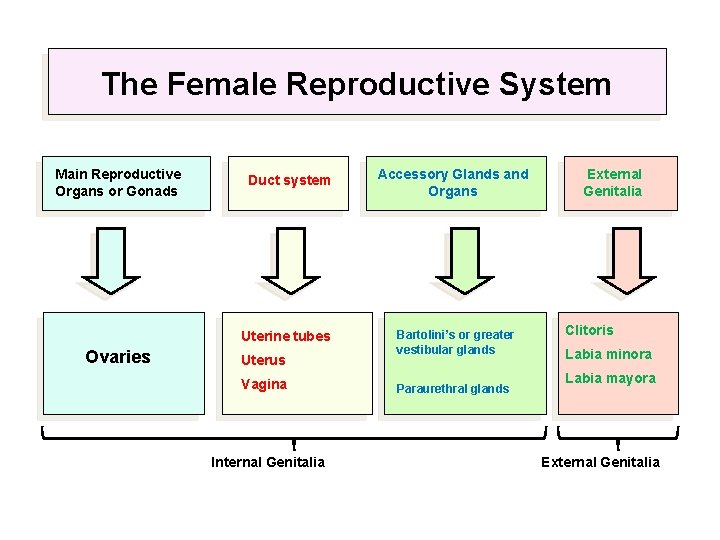
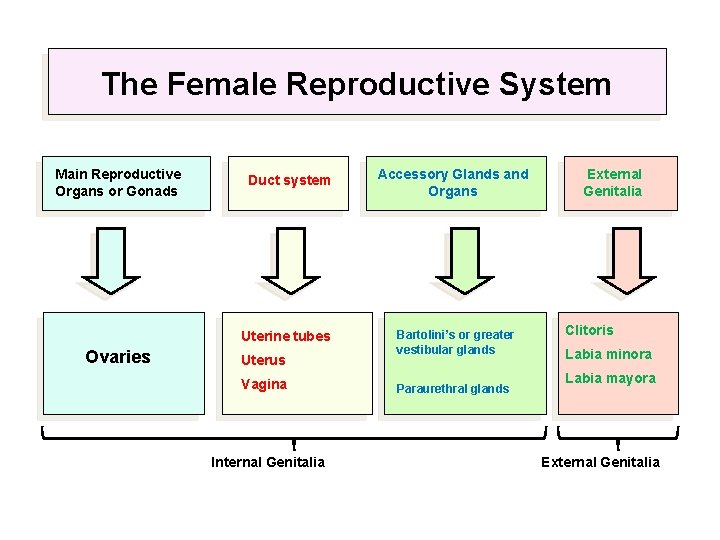
The Female Reproductive System Main Reproductive Organs or Gonads Duct system Uterine tubes Ovaries Uterus Vagina Internal Genitalia Accessory Glands and Organs Bartolini’s or greater vestibular glands Paraurethral glands External Genitalia Clitoris Labia minora Labia mayora External Genitalia
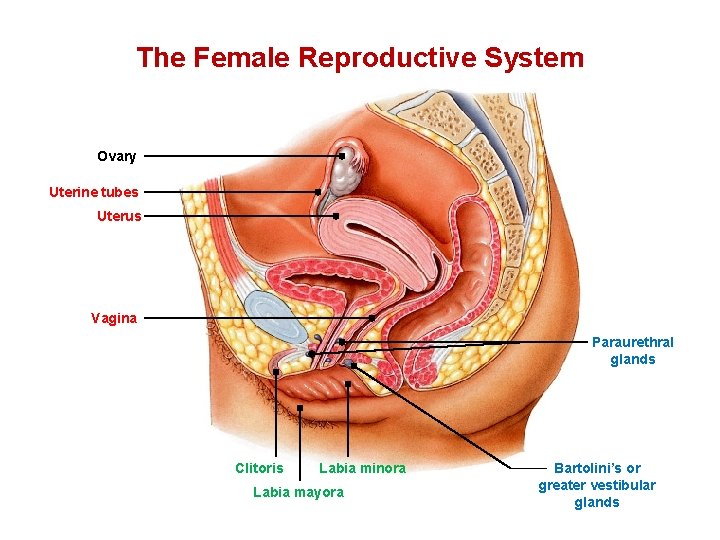
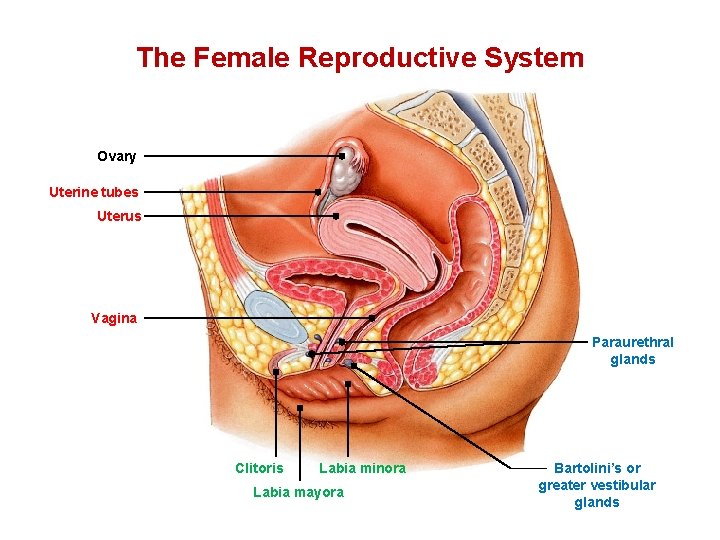
The Female Reproductive System Ovary Uterine tubes Uterus Vagina Paraurethral glands Clitoris Labia minora Labia mayora Bartolini’s or greater vestibular glands
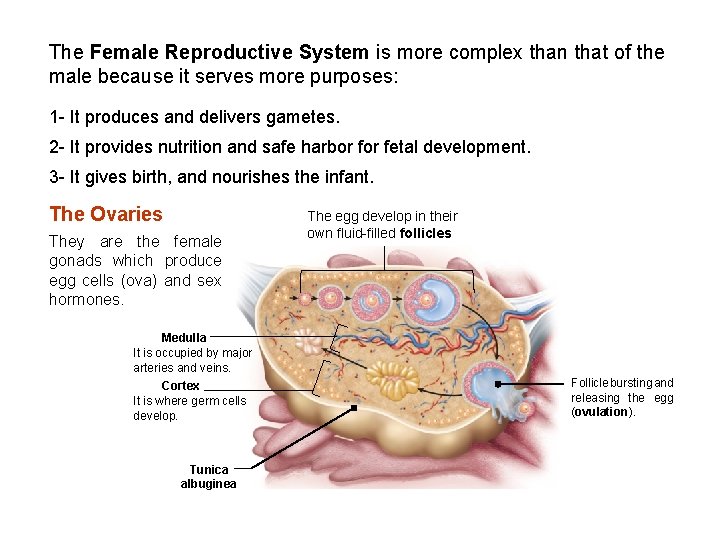
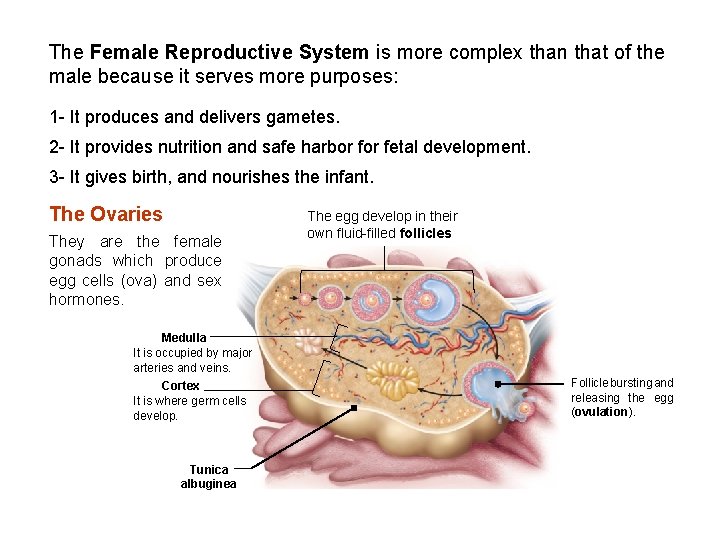
The Female Reproductive System is more complex than that of the male because it serves more purposes: 1 - It produces and delivers gametes. 2 - It provides nutrition and safe harbor fetal development. 3 - It gives birth, and nourishes the infant. The Ovaries They are the female gonads which produce egg cells (ova) and sex hormones. Medulla It is occupied by major arteries and veins. Cortex It is where germ cells develop. Tunica albuginea The egg develop in their own fluid-filled follicles Follicle bursting and releasing the egg (ovulation).
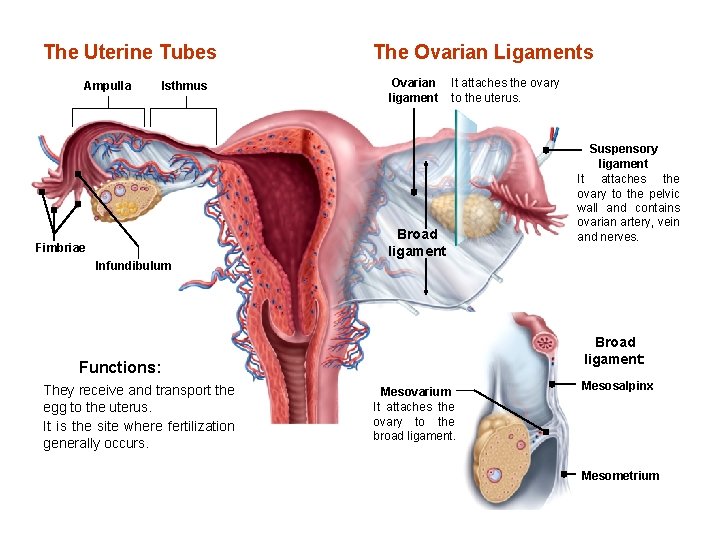
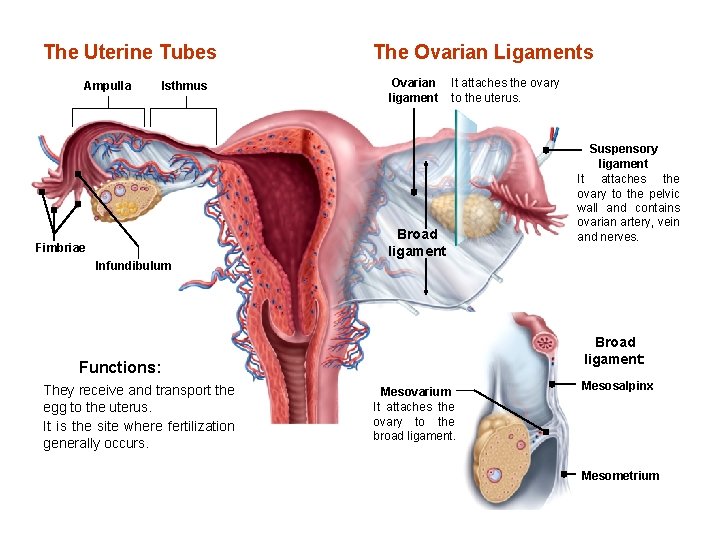
The Uterine Tubes Ampulla Isthmus Fimbriae Infundibulum The Ovarian Ligaments Ovarian ligament It attaches the ovary to the uterus. Broad ligament: Functions: They receive and transport the egg to the uterus. It is the site where fertilization generally occurs. Suspensory ligament It attaches the ovary to the pelvic wall and contains ovarian artery, vein and nerves. Mesovarium It attaches the ovary to the broad ligament. Mesosalpinx Mesometrium
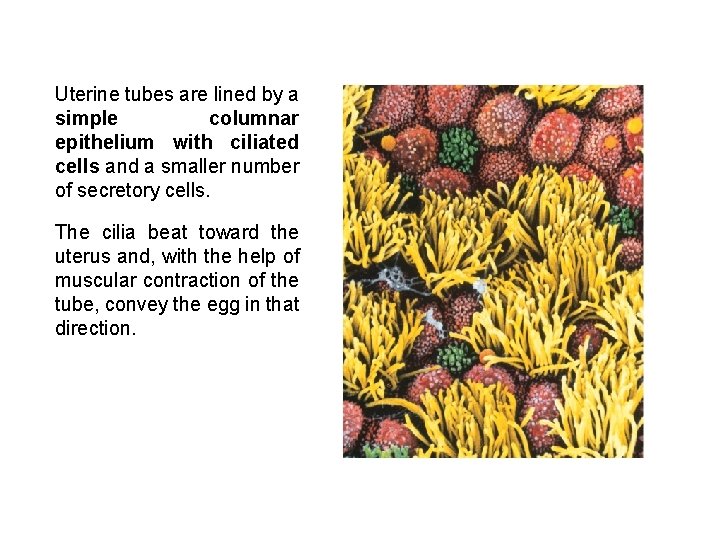
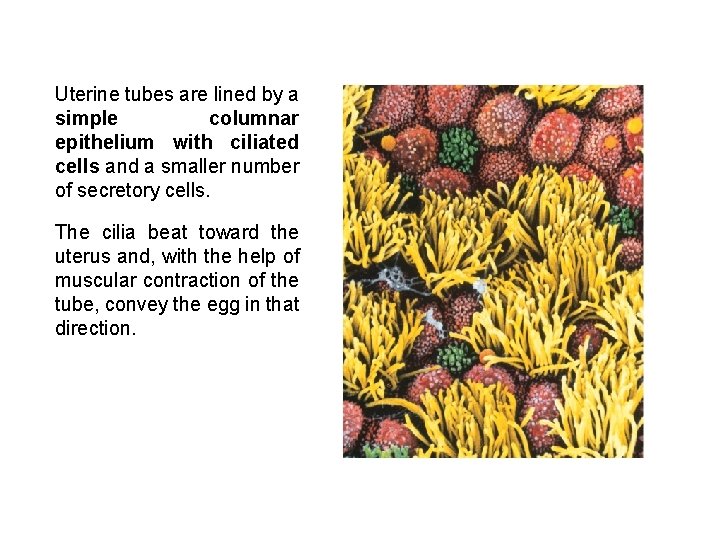
Uterine tubes are lined by a simple columnar epithelium with ciliated cells and a smaller number of secretory cells. The cilia beat toward the uterus and, with the help of muscular contraction of the tube, convey the egg in that direction.
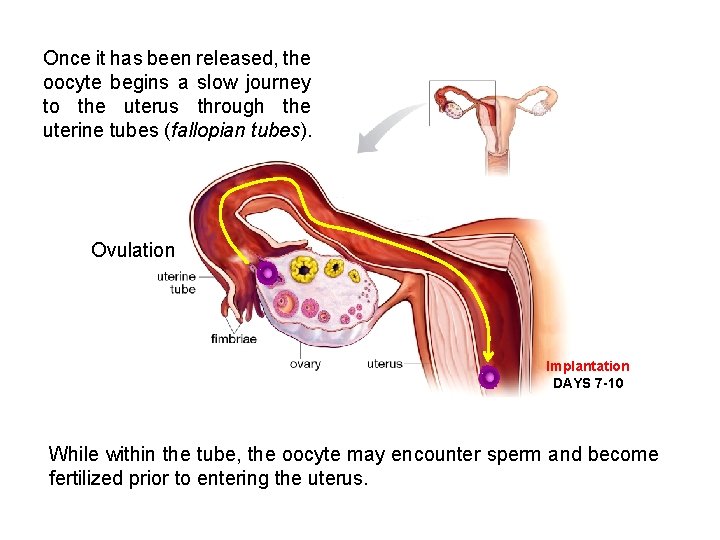
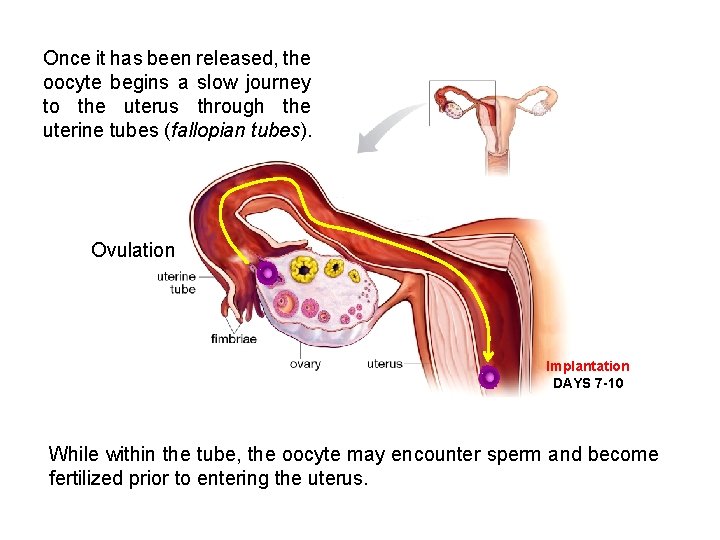
Once it has been released, the oocyte begins a slow journey to the uterus through the uterine tubes (fallopian tubes). Ovulation Implantation DAYS 7 -10 While within the tube, the oocyte may encounter sperm and become fertilized prior to entering the uterus.
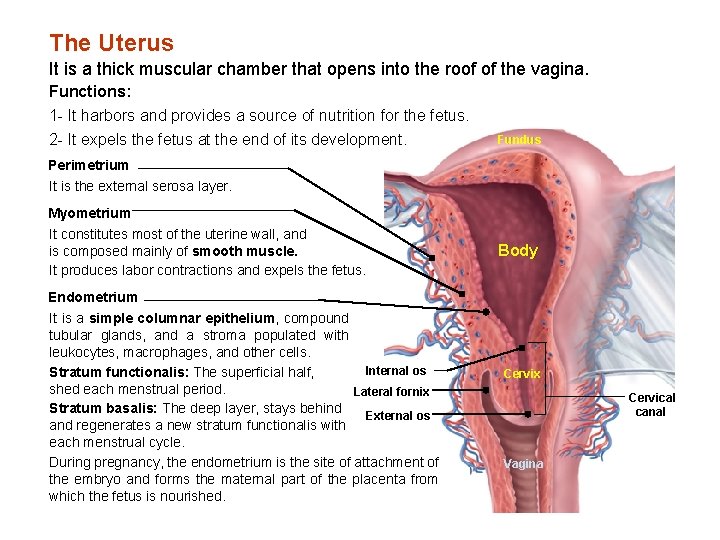
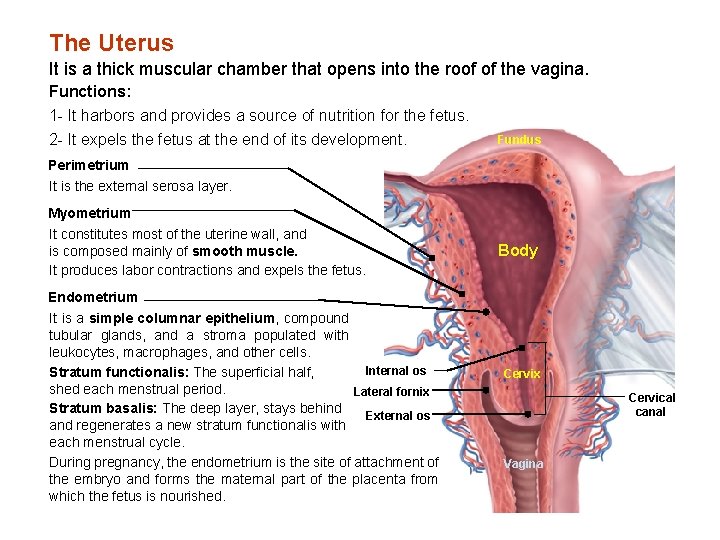
The Uterus It is a thick muscular chamber that opens into the roof of the vagina. Functions: 1 - It harbors and provides a source of nutrition for the fetus. 2 - It expels the fetus at the end of its development. Fundus Perimetrium It is the external serosa layer. Myometrium It constitutes most of the uterine wall, and is composed mainly of smooth muscle. It produces labor contractions and expels the fetus. Body Endometrium It is a simple columnar epithelium, compound tubular glands, and a stroma populated with leukocytes, macrophages, and other cells. Internal os Stratum functionalis: The superficial half, shed each menstrual period. Lateral fornix Stratum basalis: The deep layer, stays behind External os and regenerates a new stratum functionalis with each menstrual cycle. During pregnancy, the endometrium is the site of attachment of the embryo and forms the maternal part of the placenta from which the fetus is nourished. Cervix Cervical canal Vagina
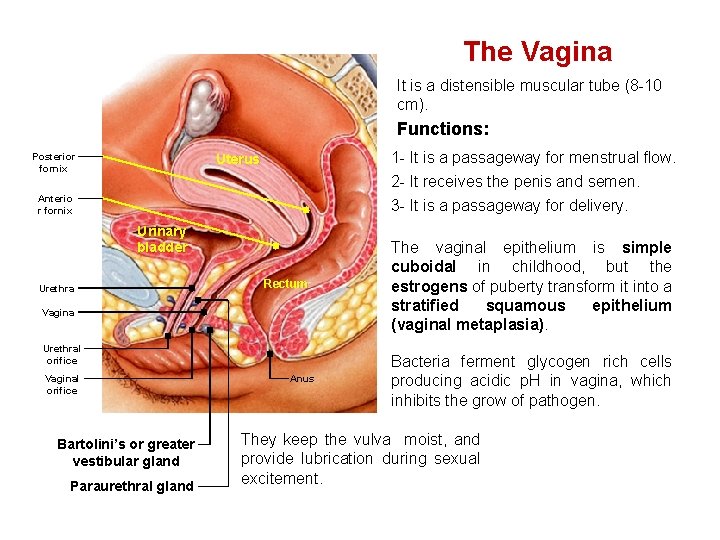
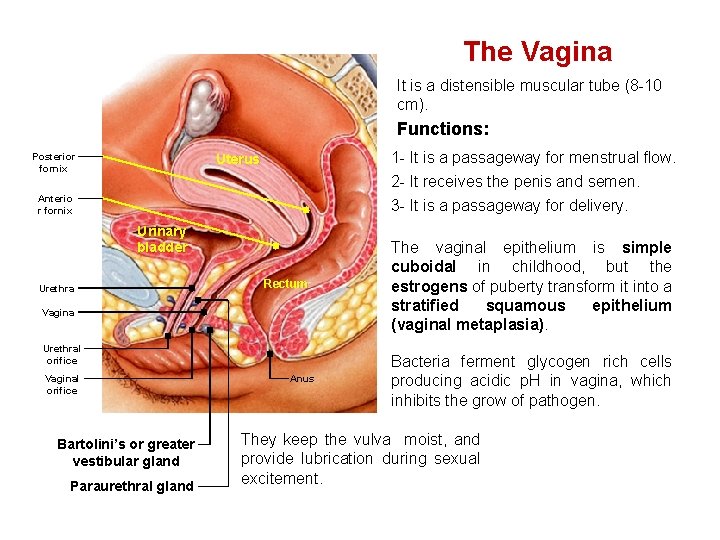
The Vagina It is a distensible muscular tube (8 -10 cm). Functions: Posterior fornix 1 - It is a passageway for menstrual flow. 2 - It receives the penis and semen. 3 - It is a passageway for delivery. Uterus Anterio r fornix Urinary bladder Urethra Rectum Vagina Urethral orifice Vaginal orifice Bartolini’s or greater vestibular gland Paraurethral gland Anus The vaginal epithelium is simple cuboidal in childhood, but the estrogens of puberty transform it into a stratified squamous epithelium (vaginal metaplasia). Bacteria ferment glycogen rich cells producing acidic p. H in vagina, which inhibits the grow of pathogen. They keep the vulva moist, and provide lubrication during sexual excitement.
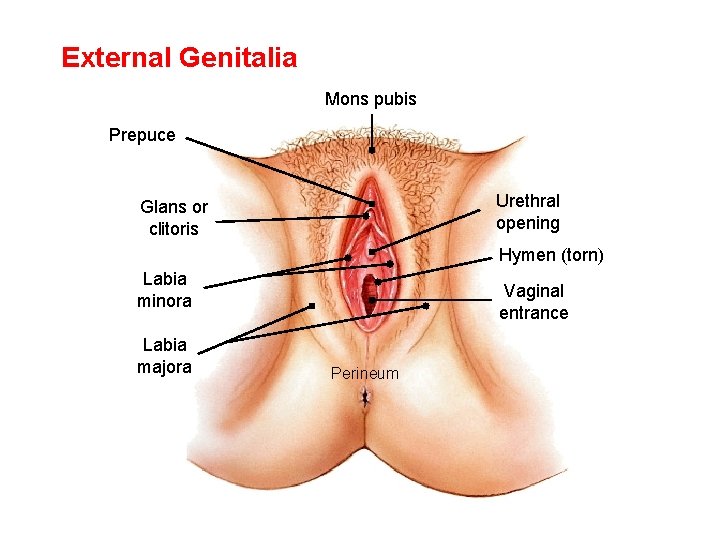
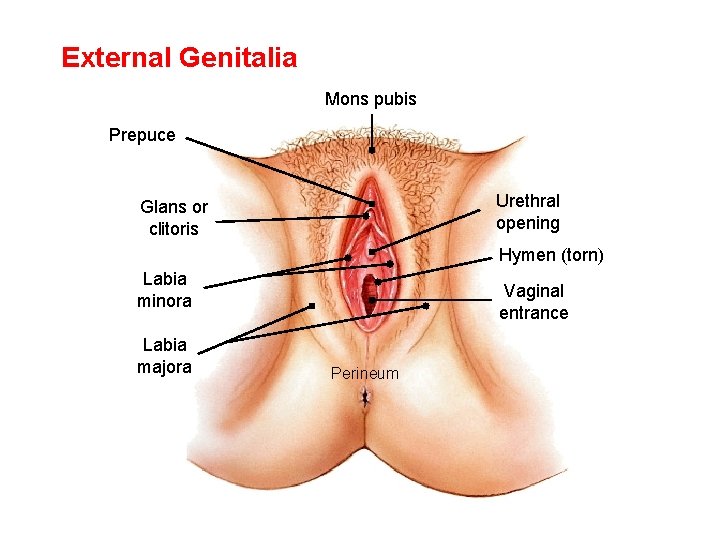
External Genitalia Mons pubis Prepuce Urethral opening Glans or clitoris Hymen (torn) Labia minora Labia majora Vaginal entrance Perineum
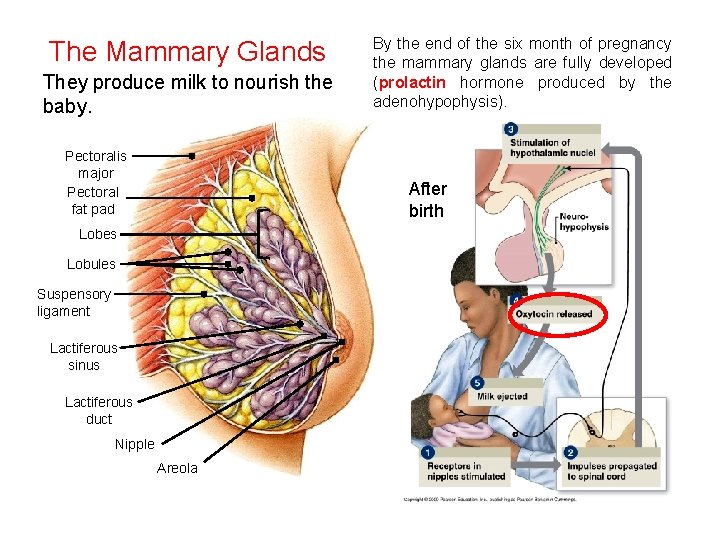
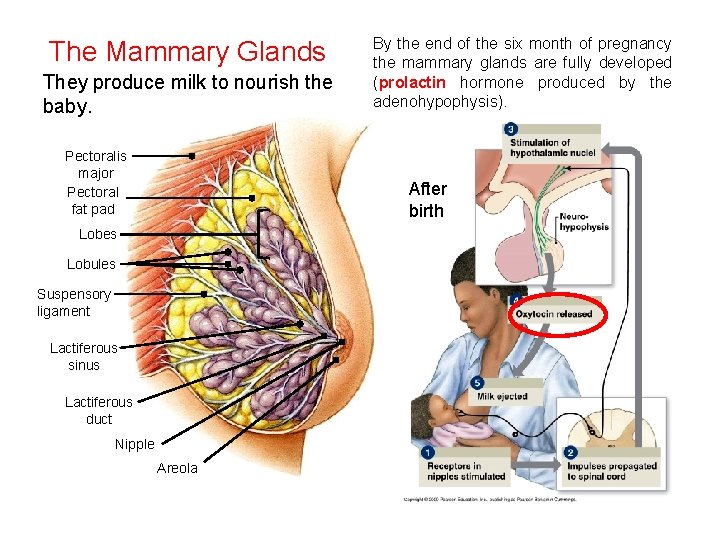
The Mammary Glands They produce milk to nourish the baby. Pectoralis major Pectoral fat pad By the end of the six month of pregnancy the mammary glands are fully developed (prolactin hormone produced by the adenohypophysis). After birth Lobes Lobules Suspensory ligament Lactiferous sinus Lactiferous duct Nipple Areola
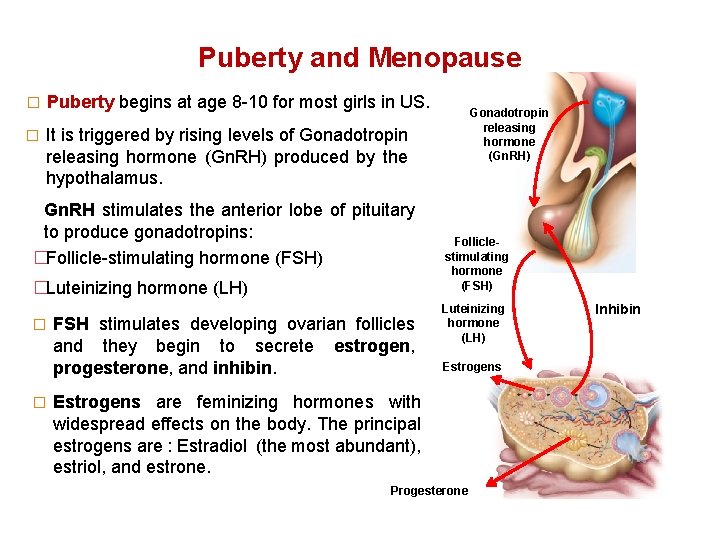
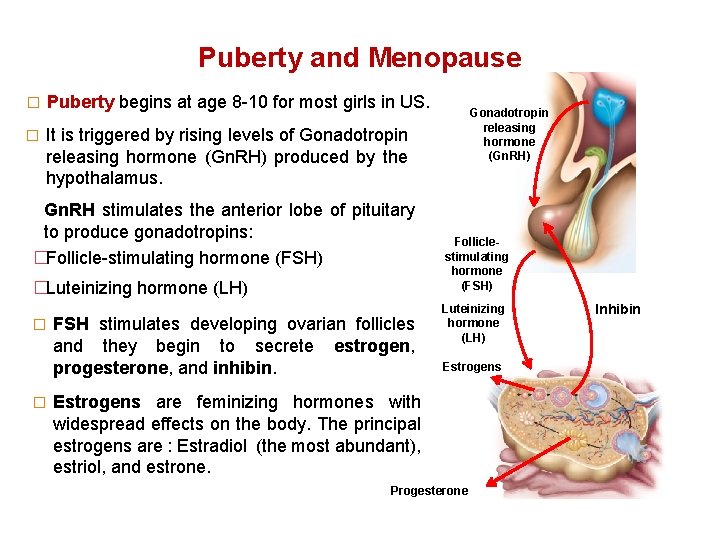
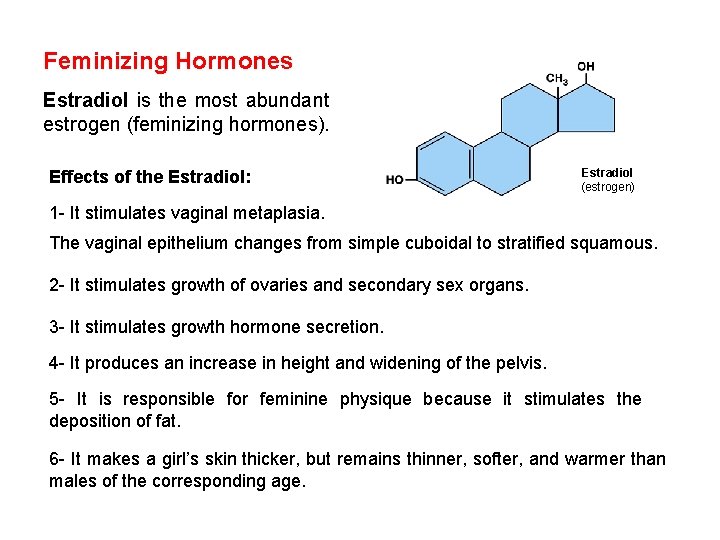
Puberty and Menopause � Puberty begins at age 8 -10 for most girls in US. � It is triggered by rising levels of Gonadotropin releasing hormone (Gn. RH) produced by the hypothalamus. Gn. RH stimulates the anterior lobe of pituitary to produce gonadotropins: �Follicle-stimulating hormone (FSH) �Luteinizing hormone (LH) � � FSH stimulates developing ovarian follicles and they begin to secrete estrogen, progesterone, and inhibin. Gonadotropin releasing hormone (Gn. RH) Folliclestimulating hormone (FSH) Luteinizing hormone (LH) Estrogens are feminizing hormones with widespread effects on the body. The principal estrogens are : Estradiol (the most abundant), estriol, and estrone. Progesterone Inhibin
Feminizing Hormones Estradiol is the most abundant estrogen (feminizing hormones). Effects of the Estradiol: Estradiol (estrogen) 1 - It stimulates vaginal metaplasia. The vaginal epithelium changes from simple cuboidal to stratified squamous. 2 - It stimulates growth of ovaries and secondary sex organs. 3 - It stimulates growth hormone secretion. 4 - It produces an increase in height and widening of the pelvis. 5 - It is responsible for feminine physique because it stimulates the deposition of fat. 6 - It makes a girl’s skin thicker, but remains thinner, softer, and warmer than males of the corresponding age.
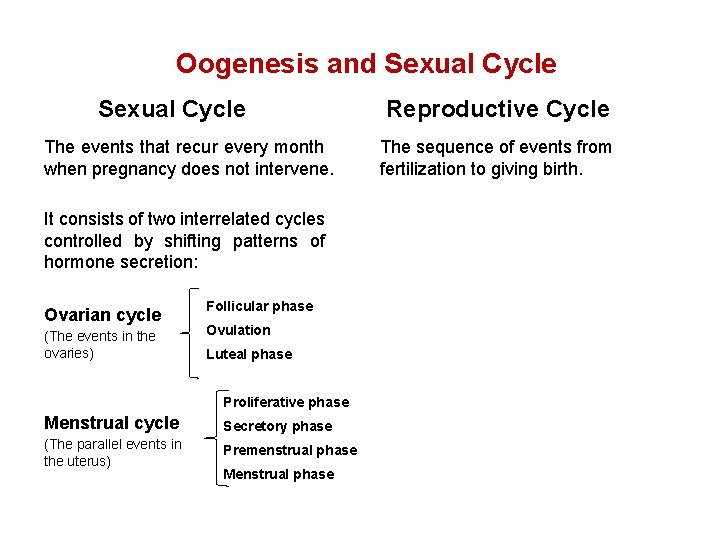
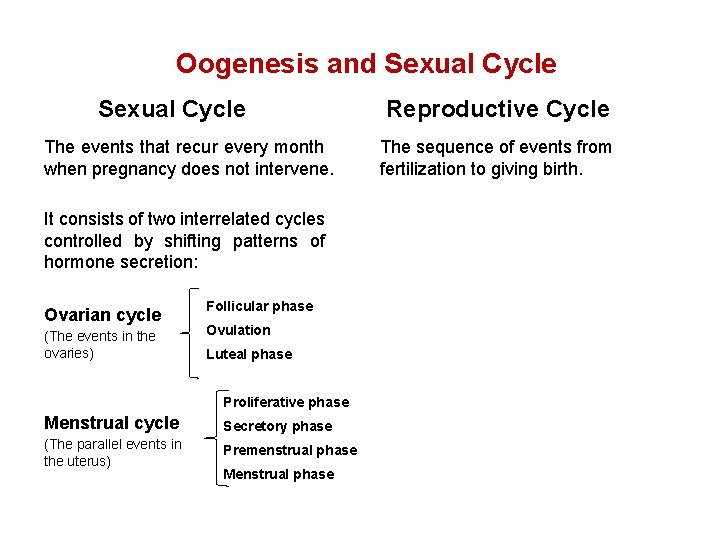
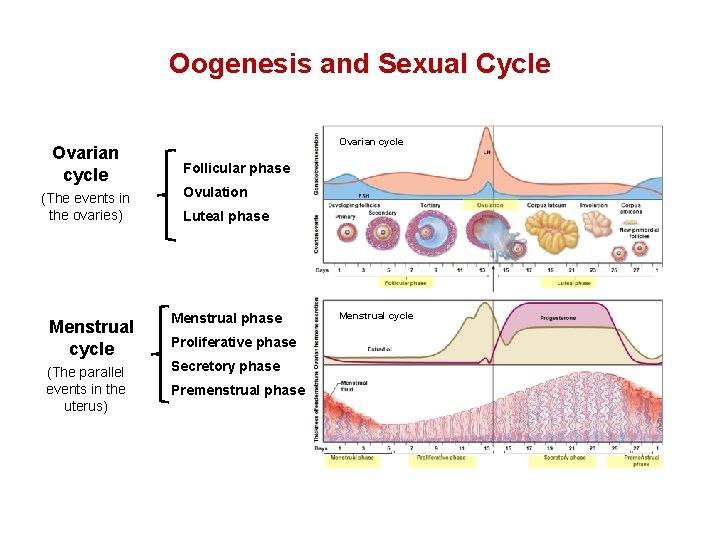
Oogenesis and Sexual Cycle The events that recur every month when pregnancy does not intervene. It consists of two interrelated cycles controlled by shifting patterns of hormone secretion: Ovarian cycle (The events in the ovaries) Follicular phase Ovulation Luteal phase Proliferative phase Menstrual cycle Secretory phase (The parallel events in the uterus) Premenstrual phase Menstrual phase Reproductive Cycle The sequence of events from fertilization to giving birth.
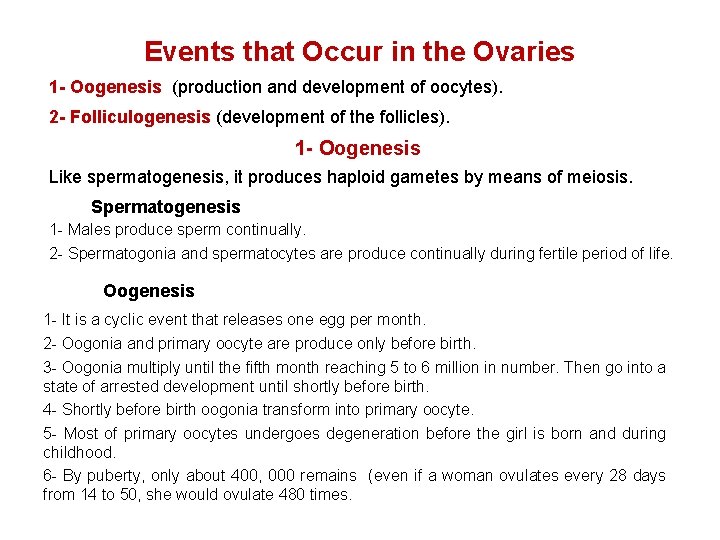
Events that Occur in the Ovaries 1 - Oogenesis (production and development of oocytes). 2 - Folliculogenesis (development of the follicles). 1 - Oogenesis Like spermatogenesis, it produces haploid gametes by means of meiosis. Spermatogenesis 1 - Males produce sperm continually. 2 - Spermatogonia and spermatocytes are produce continually during fertile period of life. Oogenesis 1 - It is a cyclic event that releases one egg per month. 2 - Oogonia and primary oocyte are produce only before birth. 3 - Oogonia multiply until the fifth month reaching 5 to 6 million in number. Then go into a state of arrested development until shortly before birth. 4 - Shortly before birth oogonia transform into primary oocyte. 5 - Most of primary oocytes undergoes degeneration before the girl is born and during childhood. 6 - By puberty, only about 400, 000 remains (even if a woman ovulates every 28 days from 14 to 50, she would ovulate 480 times.
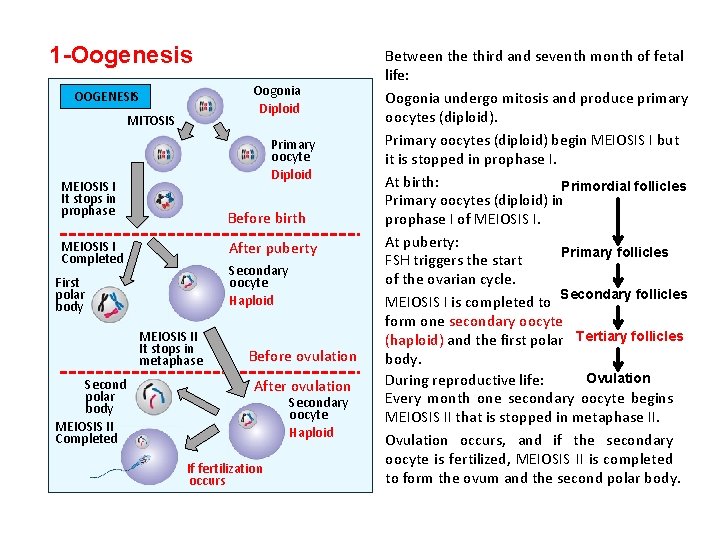
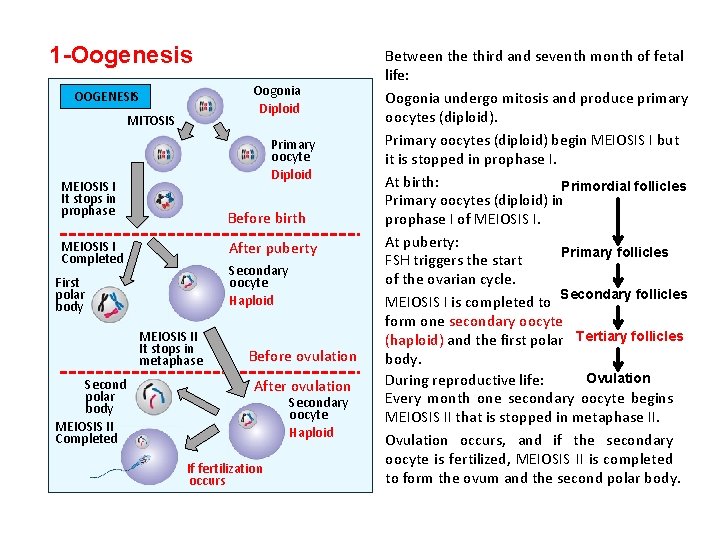
1 -Oogenesis Oogonia Diploid OOGENESIS MITOSIS Primary oocyte Diploid MEIOSIS I It stops in prophase Before birth After puberty MEIOSIS I Completed Secondary oocyte Haploid First polar body MEIOSIS II It stops in metaphase Second polar body MEIOSIS II Completed Before ovulation After ovulation Secondary oocyte Haploid If fertilization occurs Between the third and seventh month of fetal life: Oogonia undergo mitosis and produce primary oocytes (diploid). Primary oocytes (diploid) begin MEIOSIS I but it is stopped in prophase I. At birth: Primordial follicles Primary oocytes (diploid) in prophase I of MEIOSIS I. At puberty: Primary follicles FSH triggers the start of the ovarian cycle. MEIOSIS I is completed to Secondary follicles form one secondary oocyte (haploid) and the first polar Tertiary follicles body. Ovulation During reproductive life: Every month one secondary oocyte begins MEIOSIS II that is stopped in metaphase II. Ovulation occurs, and if the secondary oocyte is fertilized, MEIOSIS II is completed to form the ovum and the second polar body.
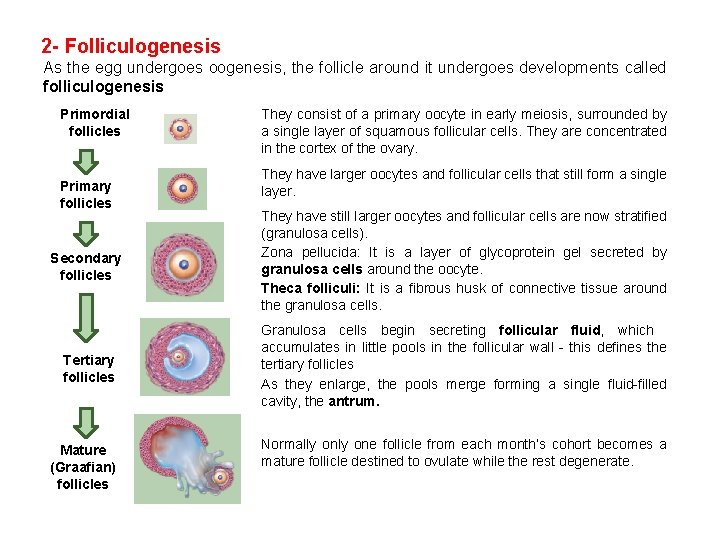
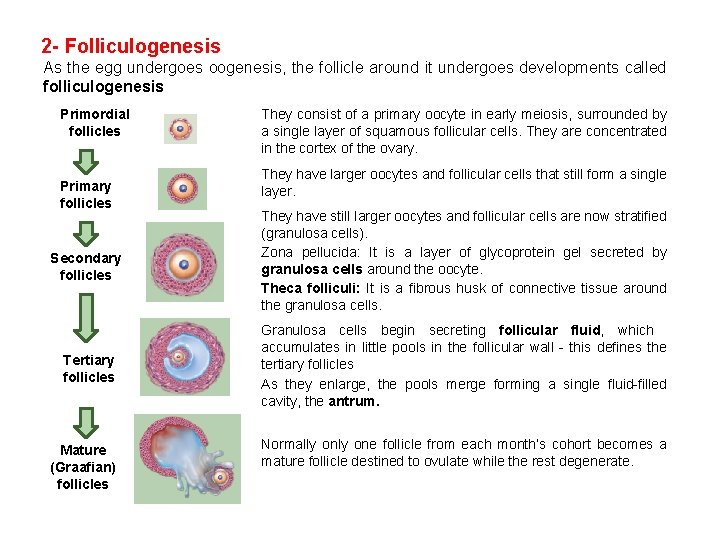
2 - Folliculogenesis As the egg undergoes oogenesis, the follicle around it undergoes developments called folliculogenesis Primordial follicles Primary follicles They consist of a primary oocyte in early meiosis, surrounded by a single layer of squamous follicular cells. They are concentrated in the cortex of the ovary. They have larger oocytes and follicular cells that still form a single layer. Secondary follicles They have still larger oocytes and follicular cells are now stratified (granulosa cells). Zona pellucida: It is a layer of glycoprotein gel secreted by granulosa cells around the oocyte. Theca folliculi: It is a fibrous husk of connective tissue around the granulosa cells. Tertiary follicles Granulosa cells begin secreting follicular fluid, which accumulates in little pools in the follicular wall - this defines the tertiary follicles As they enlarge, the pools merge forming a single fluid-filled cavity, the antrum. Mature (Graafian) follicles Normally one follicle from each month’s cohort becomes a mature follicle destined to ovulate while the rest degenerate.
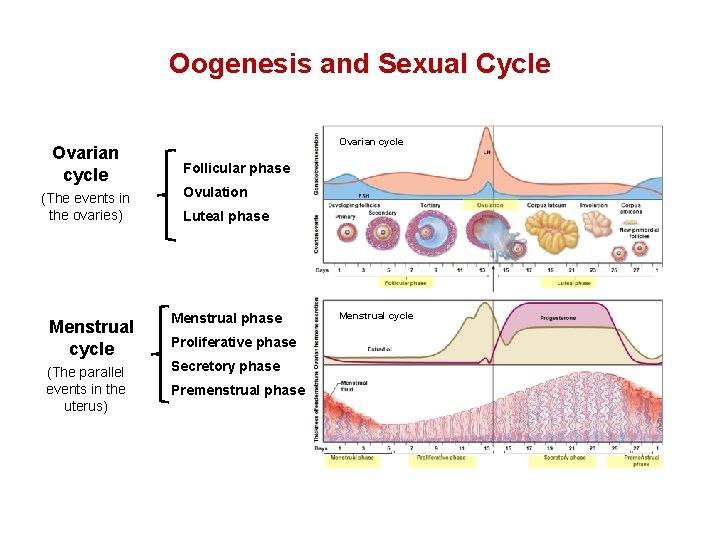
Oogenesis and Sexual Cycle Ovarian cycle (The events in the ovaries) Ovarian cycle Follicular phase Ovulation Luteal phase Menstrual cycle Menstrual phase (The parallel events in the uterus) Secretory phase Proliferative phase Premenstrual phase Menstrual cycle
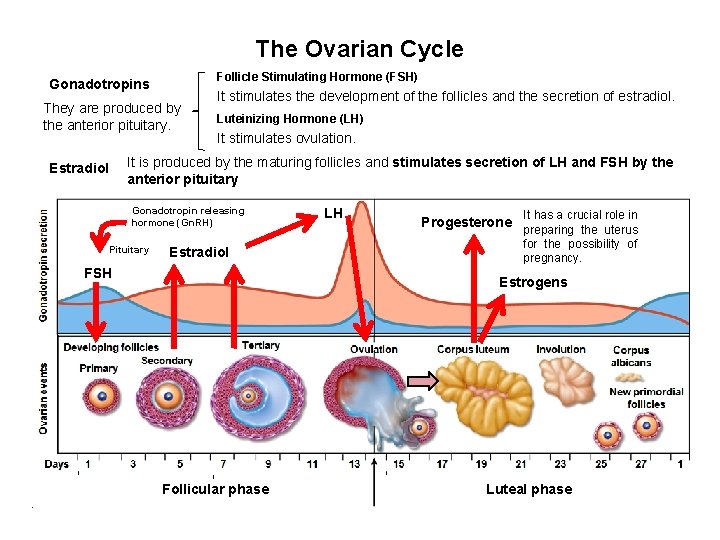
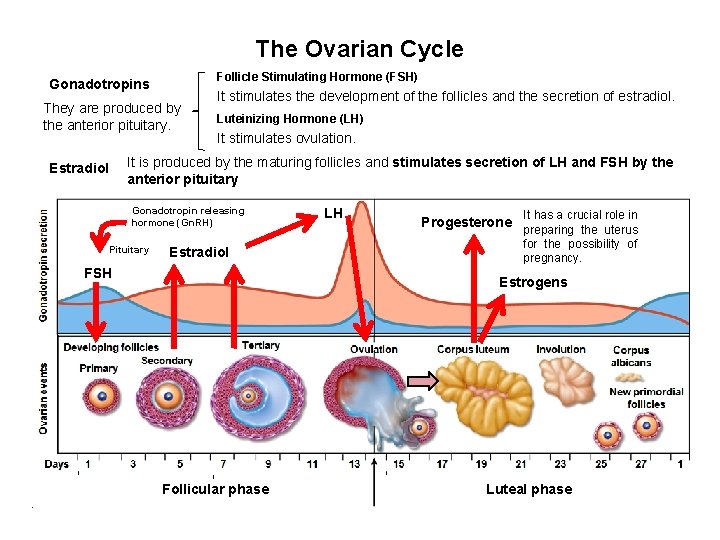
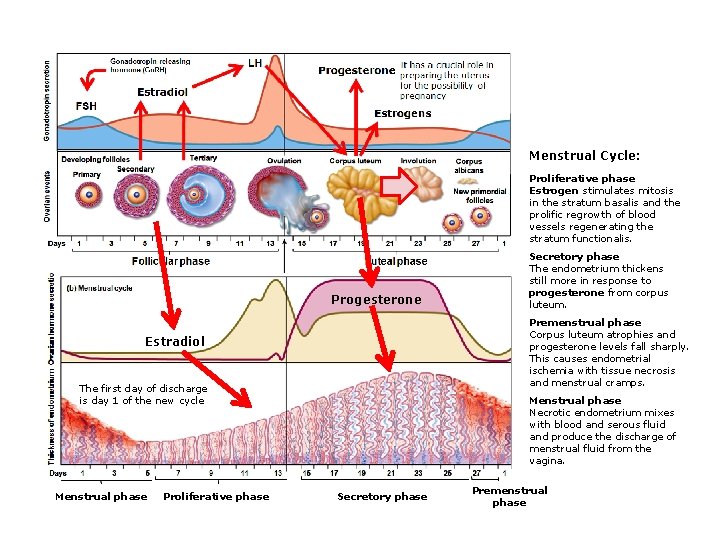
The Ovarian Cycle Follicle Stimulating Hormone (FSH) Gonadotropins They are produced by the anterior pituitary. It stimulates the development of the follicles and the secretion of estradiol. Luteinizing Hormone (LH) It stimulates ovulation. It is produced by the maturing follicles and stimulates secretion of LH and FSH by the anterior pituitary Estradiol Gonadotropin releasing hormone (Gn. RH) Pituitary Estradiol FSH LH It has a crucial role in Progesterone preparing the uterus for the possibility of pregnancy. Estrogens Follicular phase Luteal phase
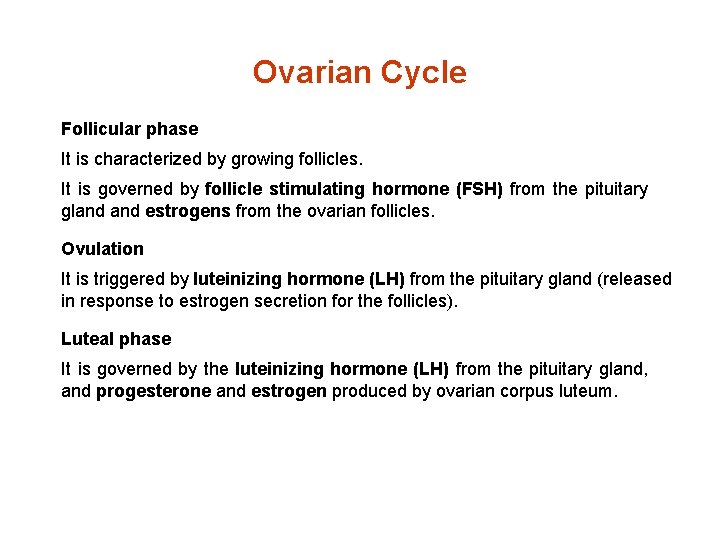
Ovarian Cycle Follicular phase It is characterized by growing follicles. It is governed by follicle stimulating hormone (FSH) from the pituitary gland estrogens from the ovarian follicles. Ovulation It is triggered by luteinizing hormone (LH) from the pituitary gland (released in response to estrogen secretion for the follicles). Luteal phase It is governed by the luteinizing hormone (LH) from the pituitary gland, and progesterone and estrogen produced by ovarian corpus luteum.
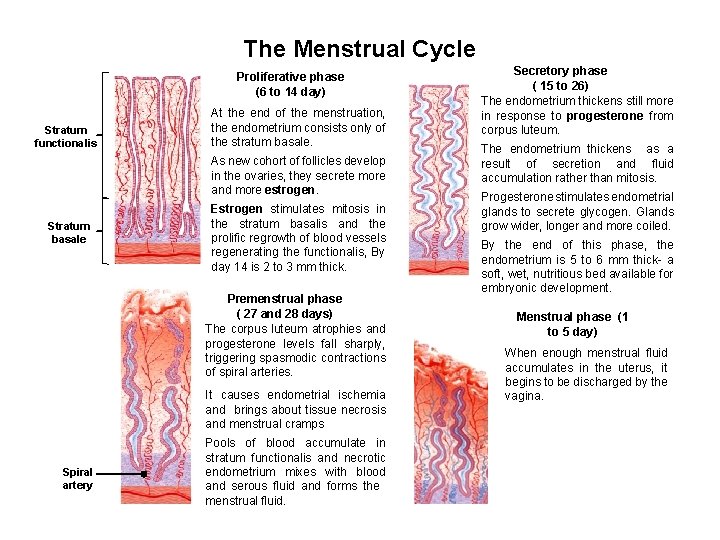
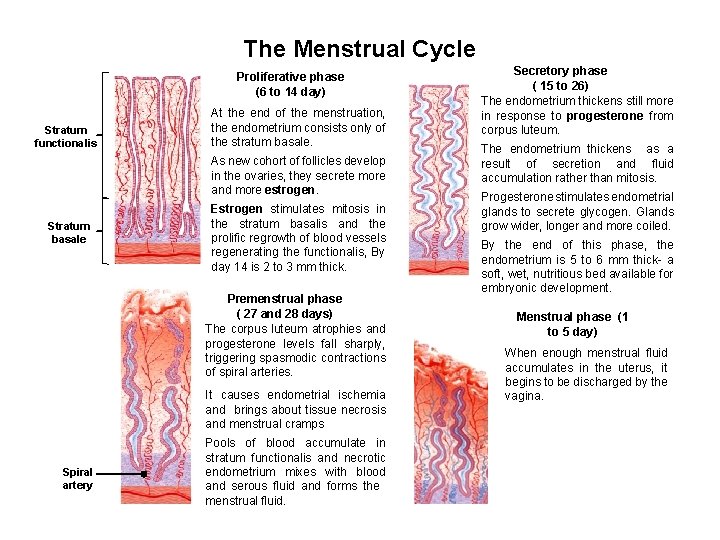
The Menstrual Cycle Proliferative phase (6 to 14 day) Stratum functionalis At the end of the menstruation, the endometrium consists only of the stratum basale. As new cohort of follicles develop in the ovaries, they secrete more and more estrogen. Stratum basale Estrogen stimulates mitosis in the stratum basalis and the prolific regrowth of blood vessels regenerating the functionalis, By day 14 is 2 to 3 mm thick. Premenstrual phase ( 27 and 28 days) The corpus luteum atrophies and progesterone levels fall sharply, triggering spasmodic contractions of spiral arteries. It causes endometrial ischemia and brings about tissue necrosis and menstrual cramps Spiral artery Pools of blood accumulate in stratum functionalis and necrotic endometrium mixes with blood and serous fluid and forms the menstrual fluid. Secretory phase ( 15 to 26) The endometrium thickens still more in response to progesterone from corpus luteum. The endometrium thickens as a result of secretion and fluid accumulation rather than mitosis. Progesterone stimulates endometrial glands to secrete glycogen. Glands grow wider, longer and more coiled. By the end of this phase, the endometrium is 5 to 6 mm thick- a soft, wet, nutritious bed available for embryonic development. Menstrual phase (1 to 5 day) When enough menstrual fluid accumulates in the uterus, it begins to be discharged by the vagina.
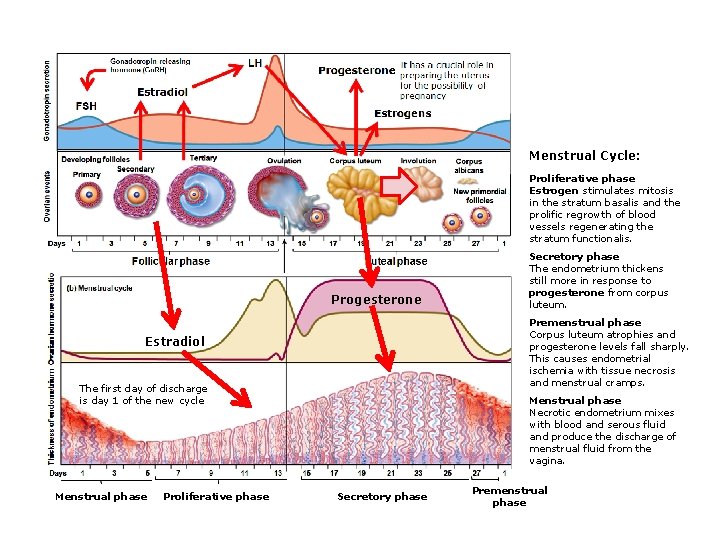
Menstrual Cycle: Proliferative phase Estrogen stimulates mitosis in the stratum basalis and the prolific regrowth of blood vessels regenerating the stratum functionalis. Progesterone Premenstrual phase Corpus luteum atrophies and progesterone levels fall sharply. This causes endometrial ischemia with tissue necrosis and menstrual cramps. Estradiol The first day of discharge is day 1 of the new cycle Menstrual phase Proliferative phase Secretory phase The endometrium thickens still more in response to progesterone from corpus luteum. Menstrual phase Necrotic endometrium mixes with blood and serous fluid and produce the discharge of menstrual fluid from the vagina. Secretory phase Premenstrual phase