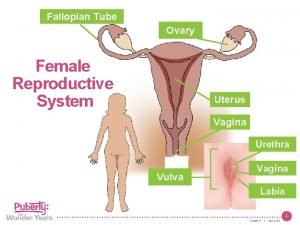
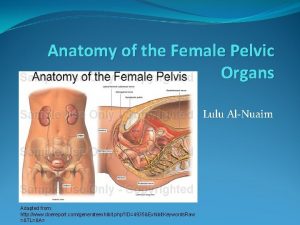
The Female Genital System TOPICS Vulva Cervix Endometrium






























- Slides: 81
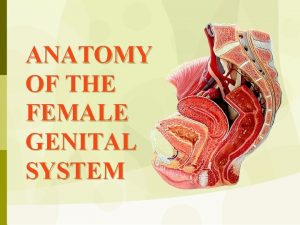
The Female Genital System
TOPICS – Vulva – Cervix – Endometrium – Uterus – Tubes – Ovaries
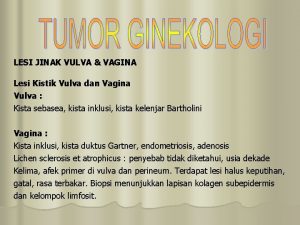
Vulva

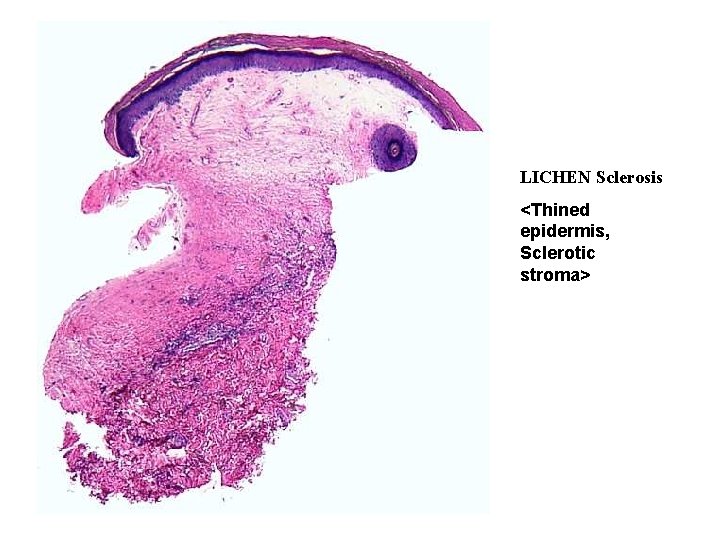
Non-Neoplastic Epithelial DISORDERS • LICHEN Sclerosis (atrophic skin) • LICHEN Simplex Chronicus (hypertrophic skin)
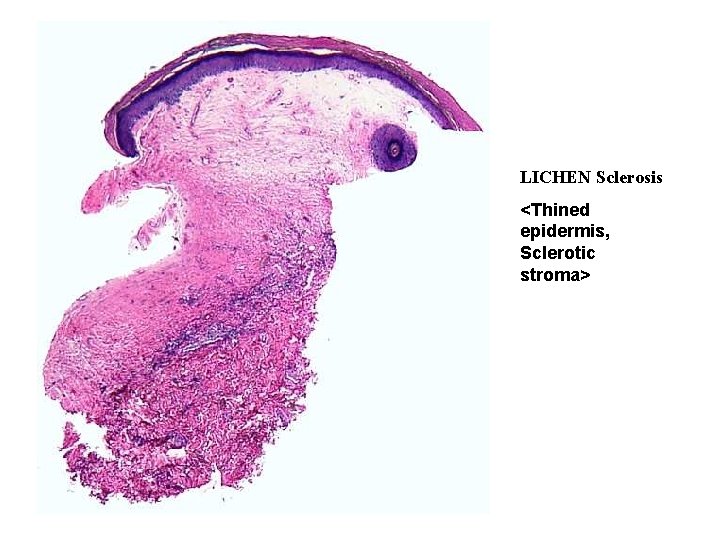
LICHEN Sclerosis <Thined epidermis, Sclerotic stroma>

LICHEN Simplex Chronicus < Hyperkeratosis , Thikened epidermis

CONDYLOMA

INFILTRATING squamous cell carcinoma
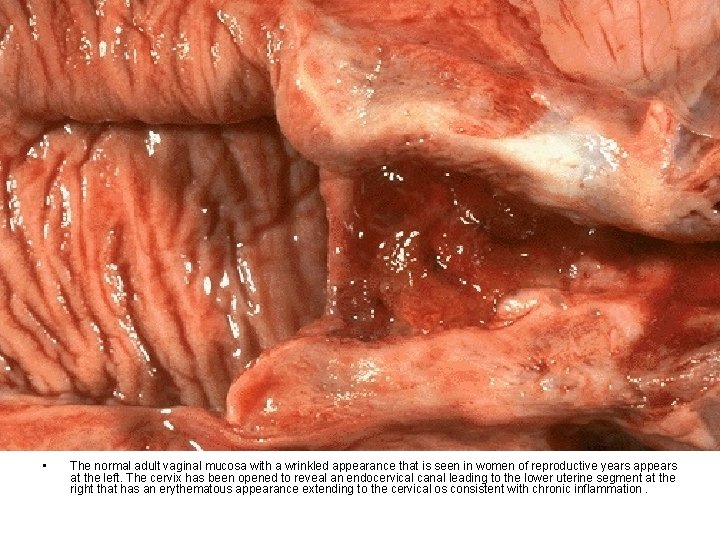
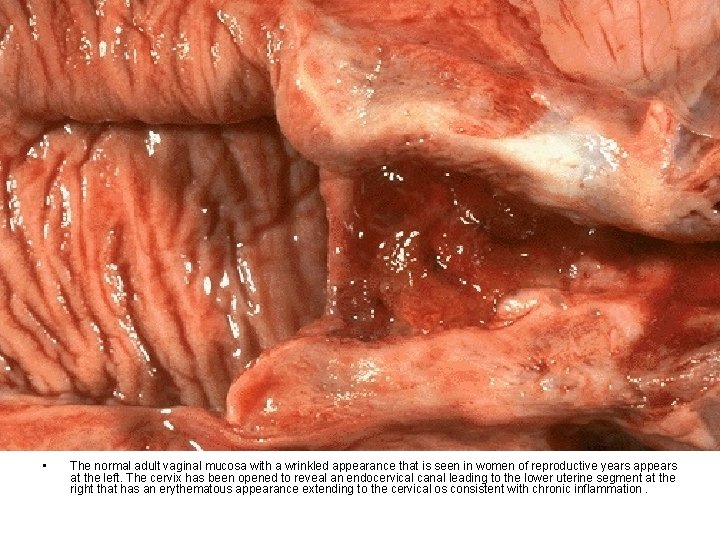
• The normal adult vaginal mucosa with a wrinkled appearance that is seen in women of reproductive years appears at the left. The cervix has been opened to reveal an endocervical canal leading to the lower uterine segment at the right that has an erythematous appearance extending to the cervical os consistent with chronic inflammation.

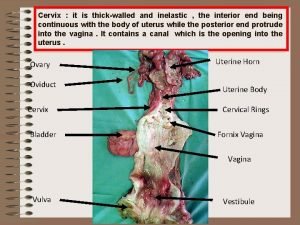
Cervix
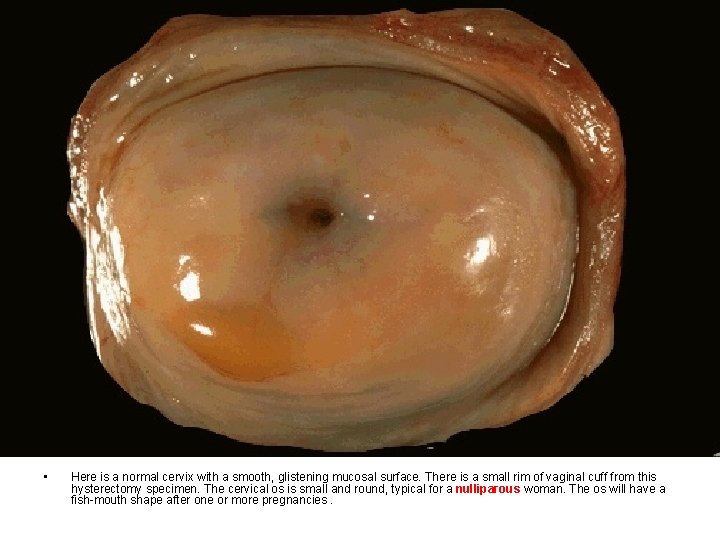
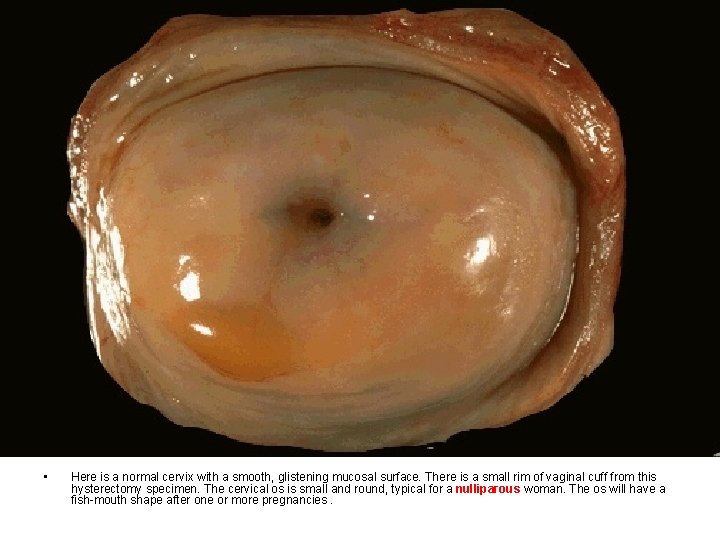
• Here is a normal cervix with a smooth, glistening mucosal surface. There is a small rim of vaginal cuff from this hysterectomy specimen. The cervical os is small and round, typical for a nulliparous woman. The os will have a fish-mouth shape after one or more pregnancies.

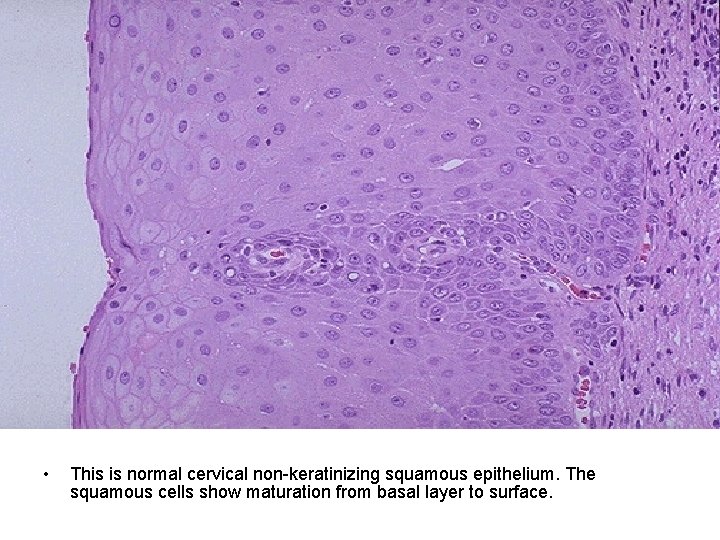
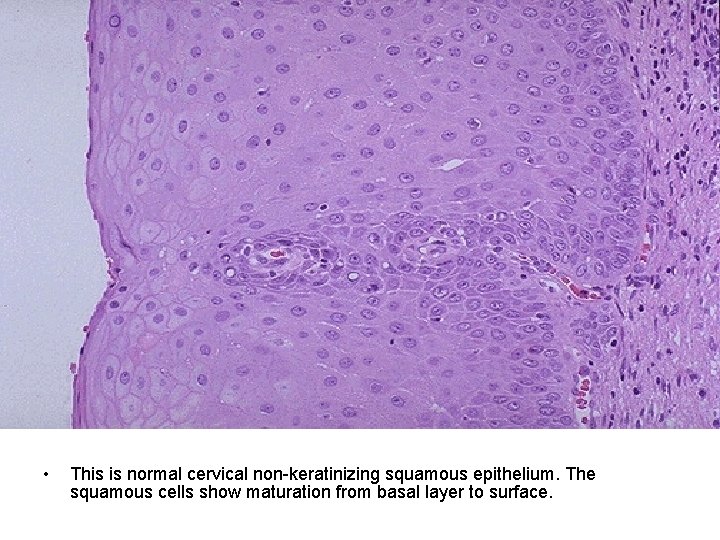
• This is normal cervical non-keratinizing squamous epithelium. The squamous cells show maturation from basal layer to surface.
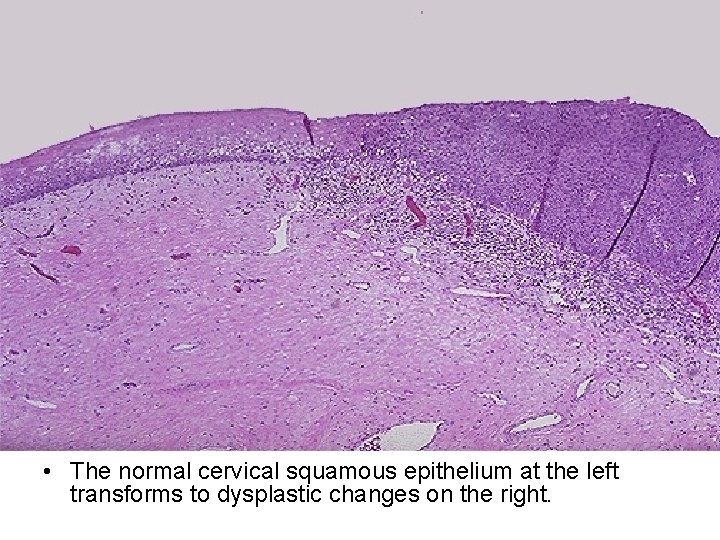
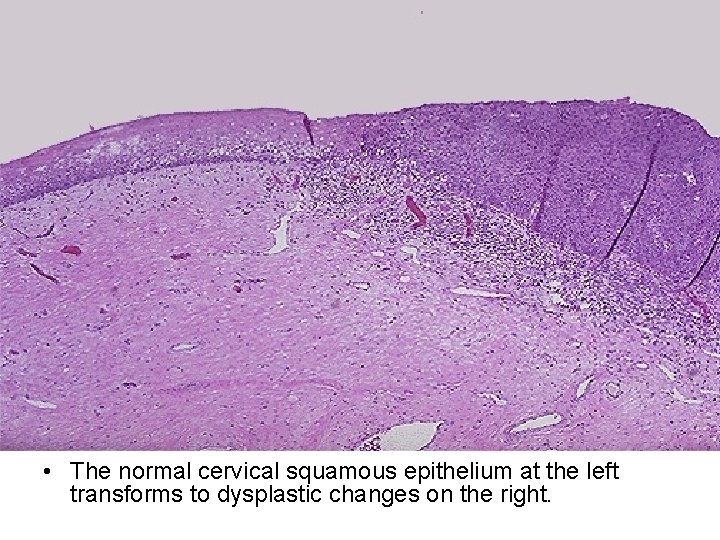
• The normal cervical squamous epithelium at the left transforms to dysplastic changes on the right.

• Cervical squamous dysplasia is seen at medium magnification, extending from the center to the right. The epithelium is normal at the left. Note how the dysplastic cell nuclei at the right are larger and darker, and the dysplastic cells have a disorderly arrangement. This dysplastic process involves the full thickness of the epithelium, but the basal lamina is intact, so this is a high grade squamous intraepithelial lesion (HSIL) that can also be termed cervical intraepithelial neoplasia (CIN) III.

• This is a Pap smear. The cytologic features of normal squamous epithelial cells can be seen at the center top and bottom, with orange to pale blue plate-like squamous cells that have small pyknotic nuclei. The dysplastic cells in the center extending to upper right are smaller overall with darker, more irregular nuclei.
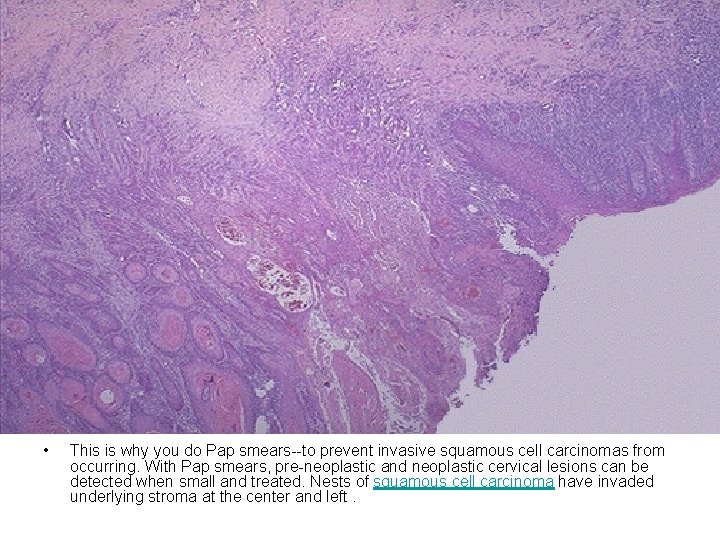
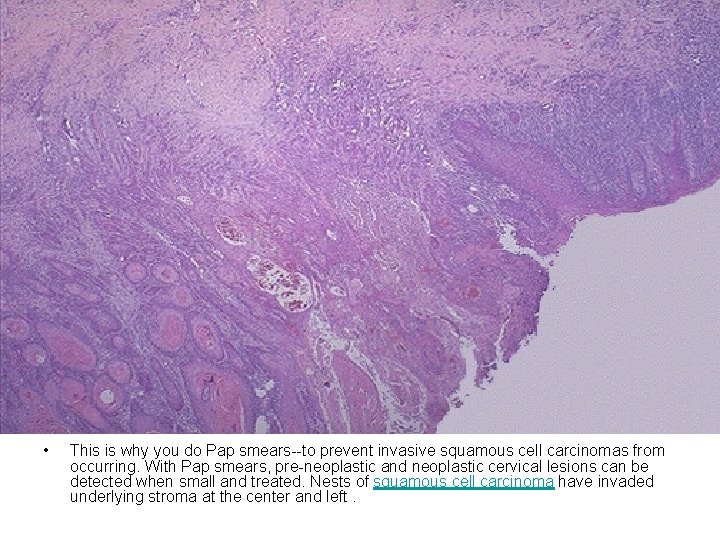
• This is why you do Pap smears--to prevent invasive squamous cell carcinomas from occurring. With Pap smears, pre-neoplastic and neoplastic cervical lesions can be detected when small and treated. Nests of squamous cell carcinoma have invaded underlying stroma at the center and left.
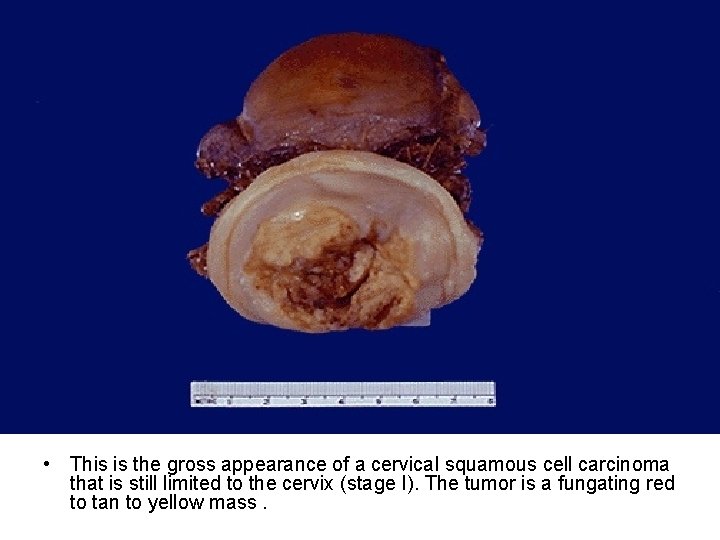
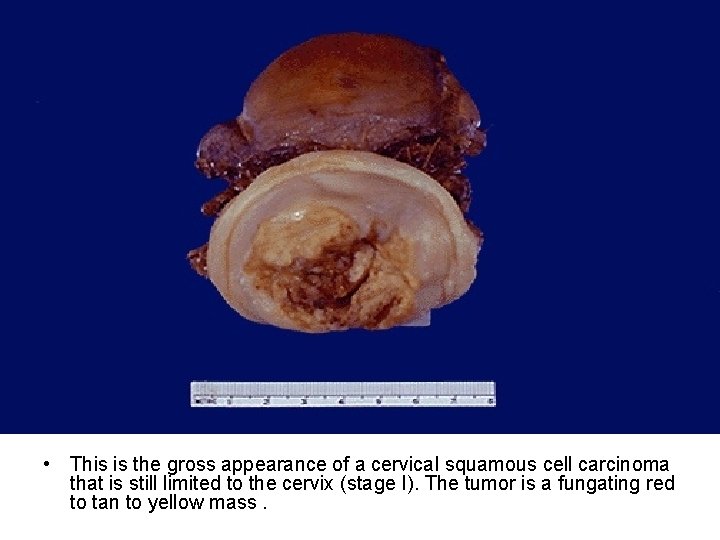
• This is the gross appearance of a cervical squamous cell carcinoma that is still limited to the cervix (stage I). The tumor is a fungating red to tan to yellow mass.
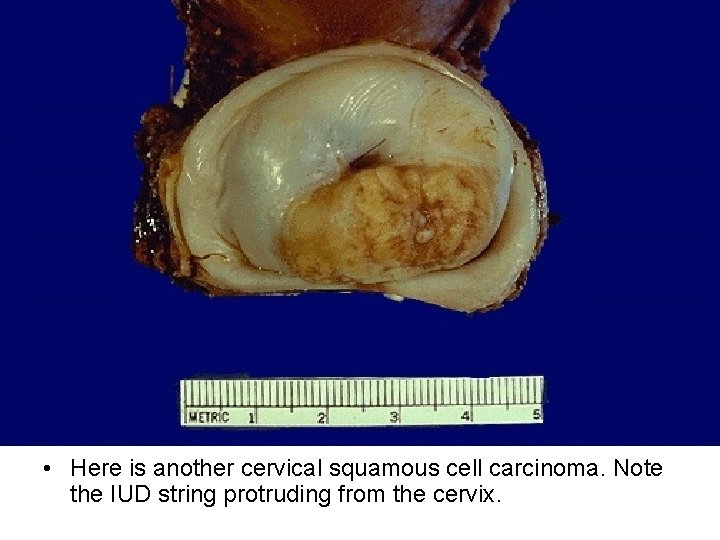
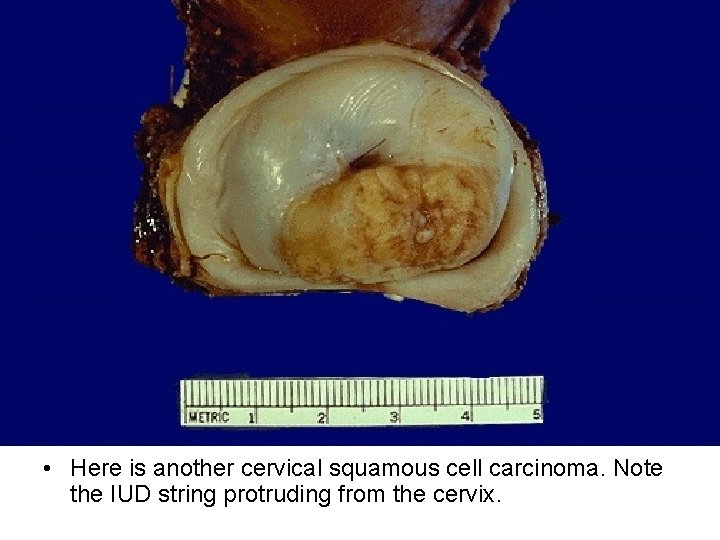
• Here is another cervical squamous cell carcinoma. Note the IUD string protruding from the cervix.
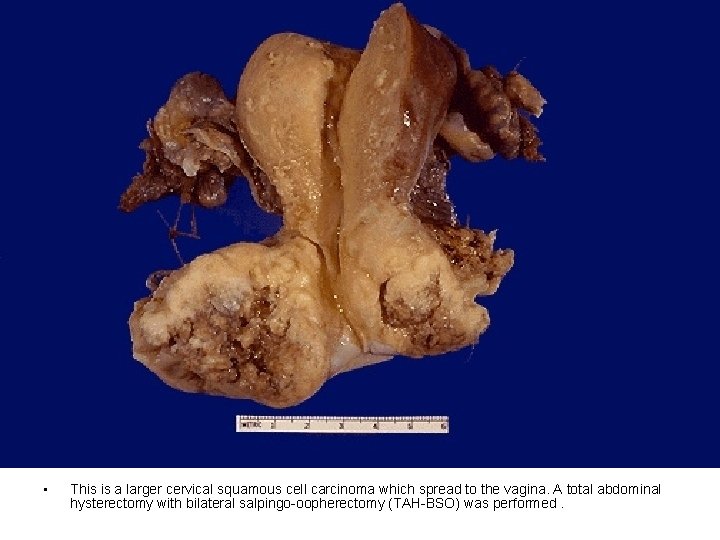
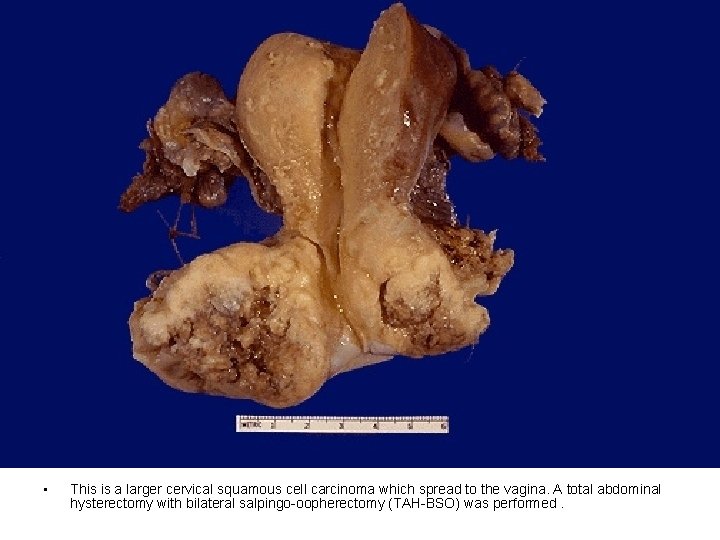
• This is a larger cervical squamous cell carcinoma which spread to the vagina. A total abdominal hysterectomy with bilateral salpingo-oopherectomy (TAH-BSO) was performed.
Endometrium

• This is the microscopic appearance of normal proliferative endometrium in the menstrual cycle. In this phase, tubular glands with columnar cells and surrounding dense stroma are proliferating to build up the endometrium following shedding with previous menstruation.
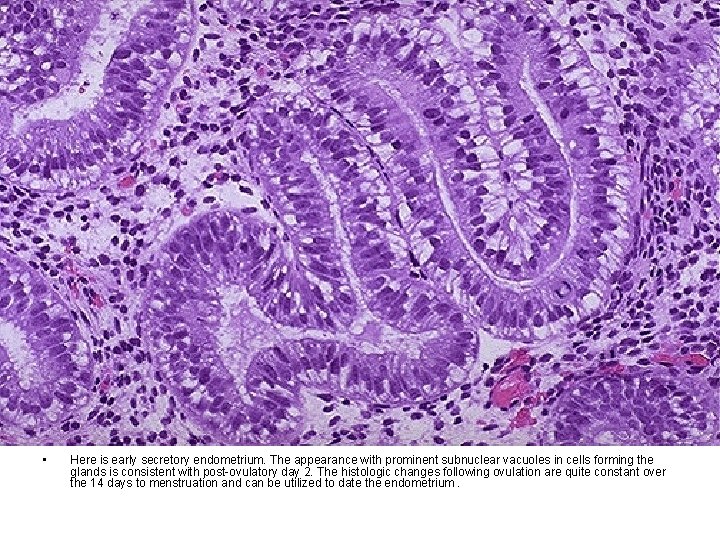
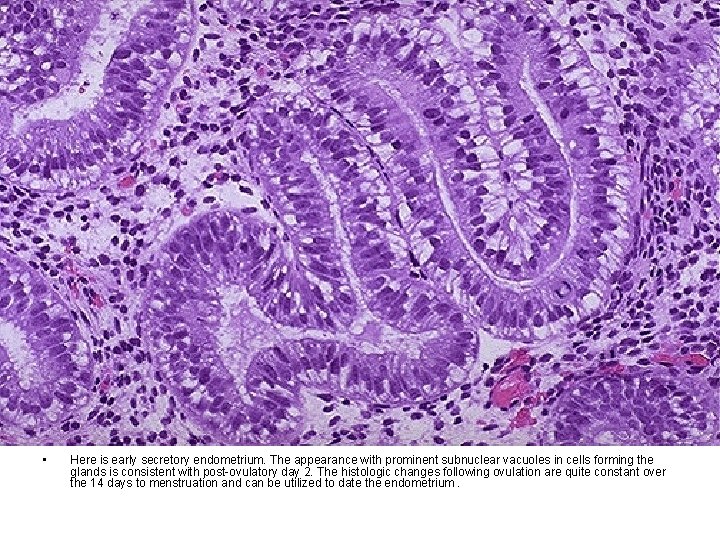
• Here is early secretory endometrium. The appearance with prominent subnuclear vacuoles in cells forming the glands is consistent with post-ovulatory day 2. The histologic changes following ovulation are quite constant over the 14 days to menstruation and can be utilized to date the endometrium.
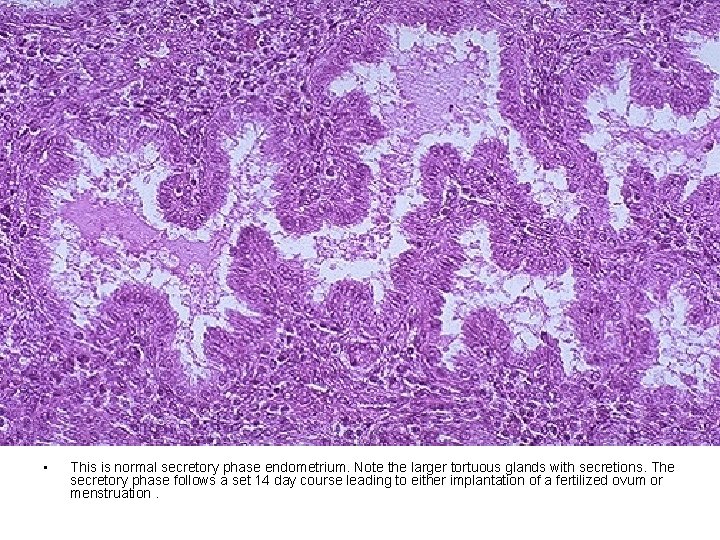
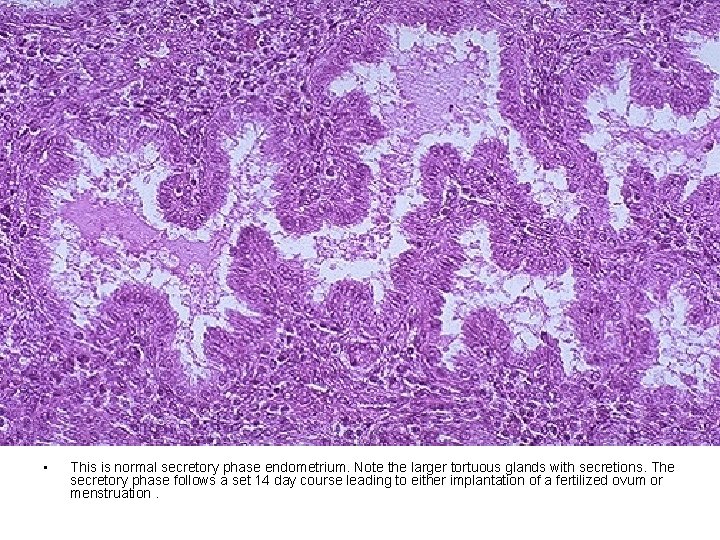
• This is normal secretory phase endometrium. Note the larger tortuous glands with secretions. The secretory phase follows a set 14 day course leading to either implantation of a fertilized ovum or menstruation.

• The endometrial cavity is opened to reveal lush fronds of hyperplastic endometrium. Endometrial hyperplasia usually results with conditions of prolonged estrogen excess and can lead to metrorrhagia (uterine bleeding at irregular intervals), menorrhagia (excessive bleeding with menstrual periods), or menometrorrhagia.
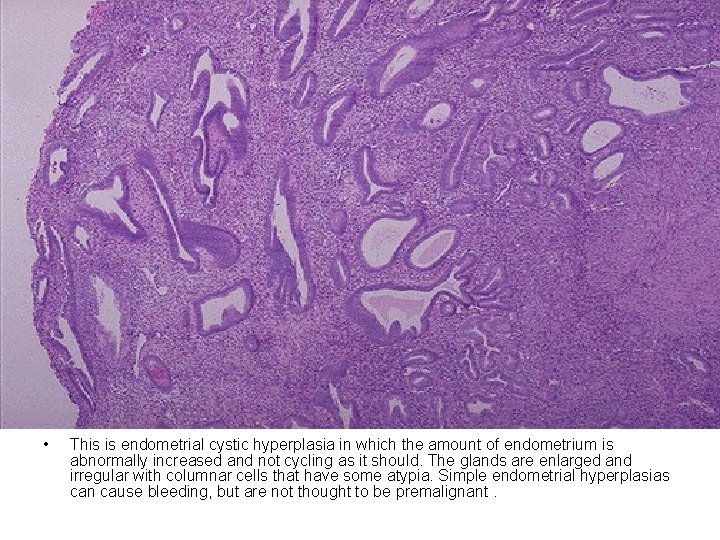
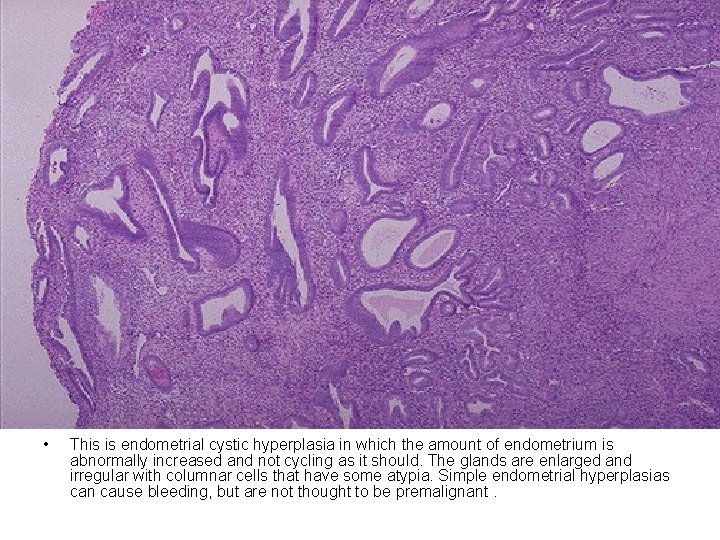
• This is endometrial cystic hyperplasia in which the amount of endometrium is abnormally increased and not cycling as it should. The glands are enlarged and irregular with columnar cells that have some atypia. Simple endometrial hyperplasias can cause bleeding, but are not thought to be premalignant.

• This uterus has been opened anteriorly through cervix and into the endometrial cavity. High in the fundus and projecting into the endometrial cavity is a small endometrial polyp. Such benign polyps may cause uterine bleeding.
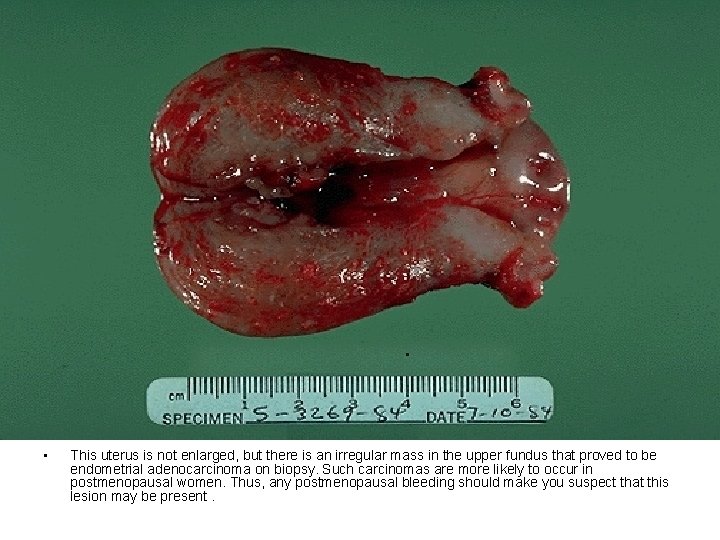
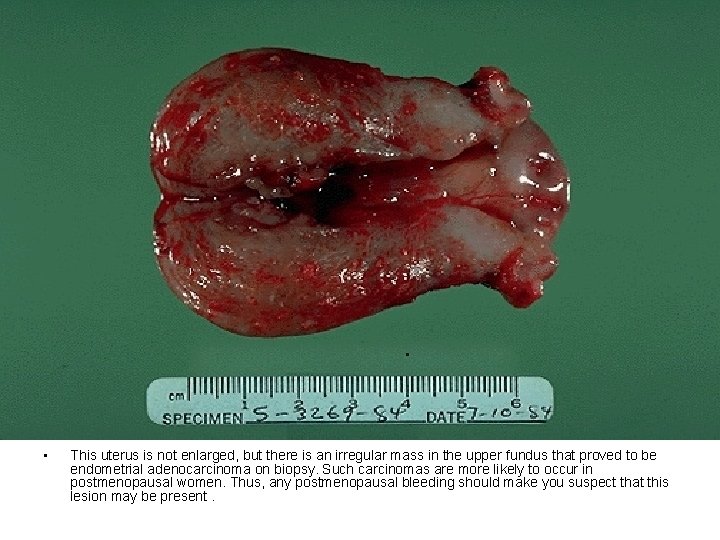
• This uterus is not enlarged, but there is an irregular mass in the upper fundus that proved to be endometrial adenocarcinoma on biopsy. Such carcinomas are more likely to occur in postmenopausal women. Thus, any postmenopausal bleeding should make you suspect that this lesion may be present.

• This adenocarcinoma of the endometrium is more obvious. Irregular masses of white tumor are seen over the surface of this uterus that has been opened anteriorly. The cervix is at the bottom of the picture. This enlarged uterus was no doubt palpable on physical examination. Such a neoplasm often present with abnormal bleeding.

• This is endometrial adenocarcinoma which can be seen invading into the smooth muscle bundles of the myometrial wall of the uterus. This neoplasm has a higher stage than a neoplasm that is just confined to the endometrium or is superficially invasive.
Uterus
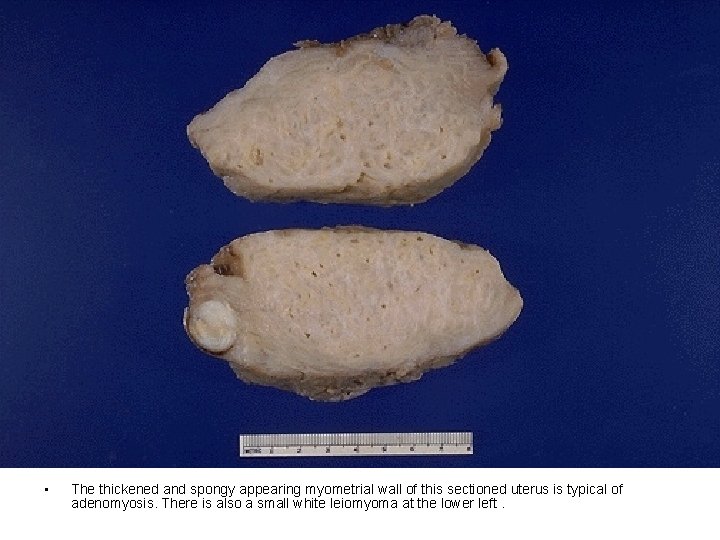
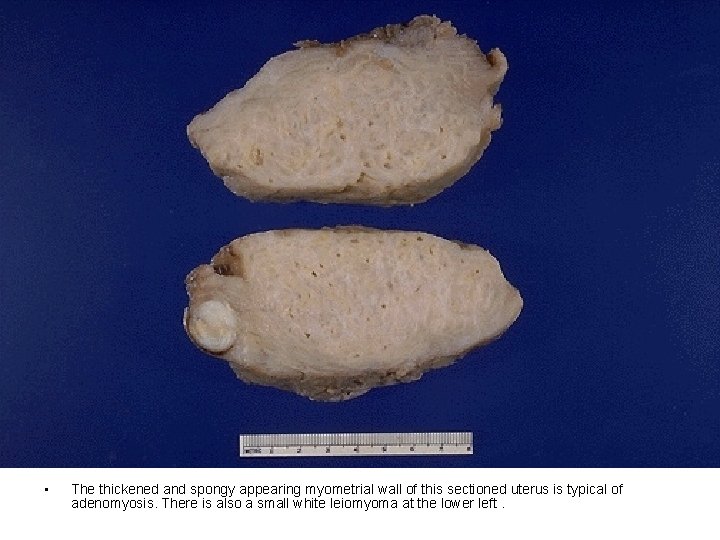
• The thickened and spongy appearing myometrial wall of this sectioned uterus is typical of adenomyosis. There is also a small white leiomyoma at the lower left.
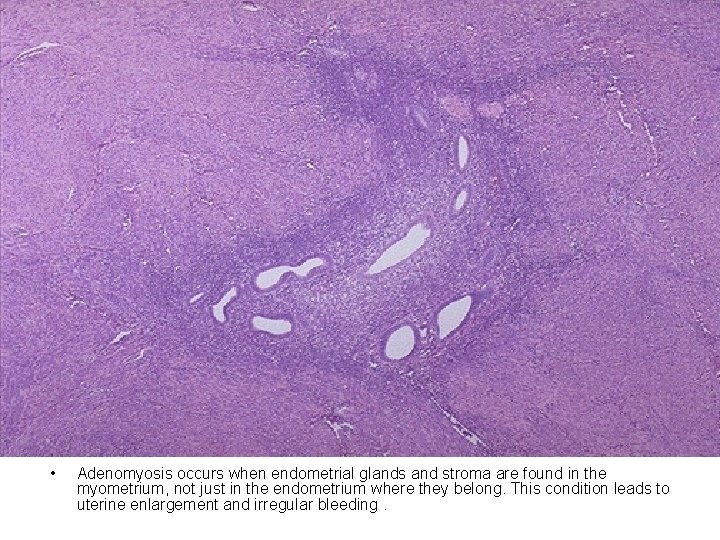
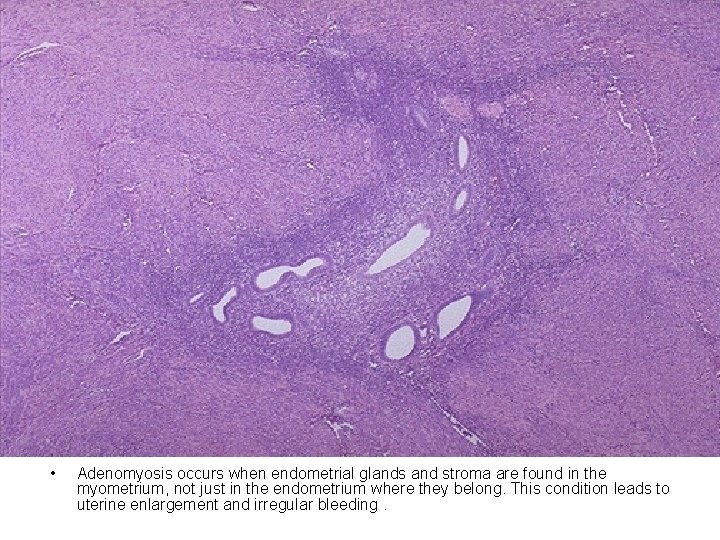
• Adenomyosis occurs when endometrial glands and stroma are found in the myometrium, not just in the endometrium where they belong. This condition leads to uterine enlargement and irregular bleeding.

• When endometrial glands and stroma are found outside the uterus, the condition is known as endometriosis. Up to 10% of women may have this condition. It can be very disabling and painful, even when just a few foci are present. Diagrammed here are typical locations for foci of endometriosis. Sometimes the old dark brown blood collects over time from repeated hemorrhage in a cystic space in the ovary and produces a so-called "chocolate cyst. "
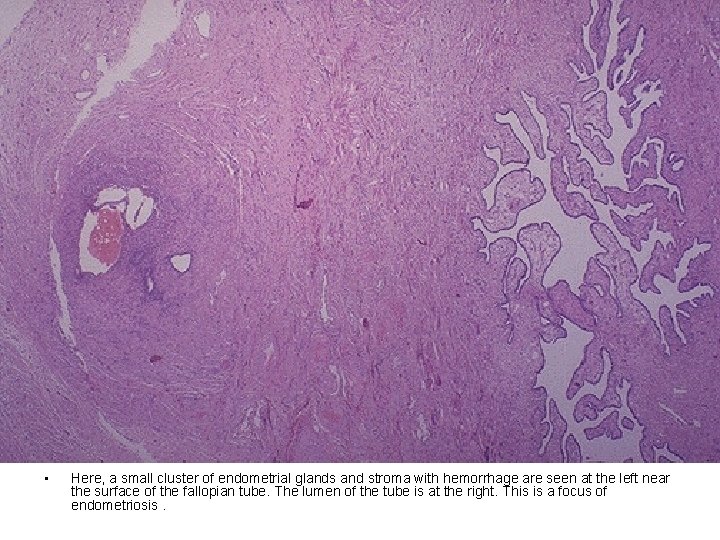
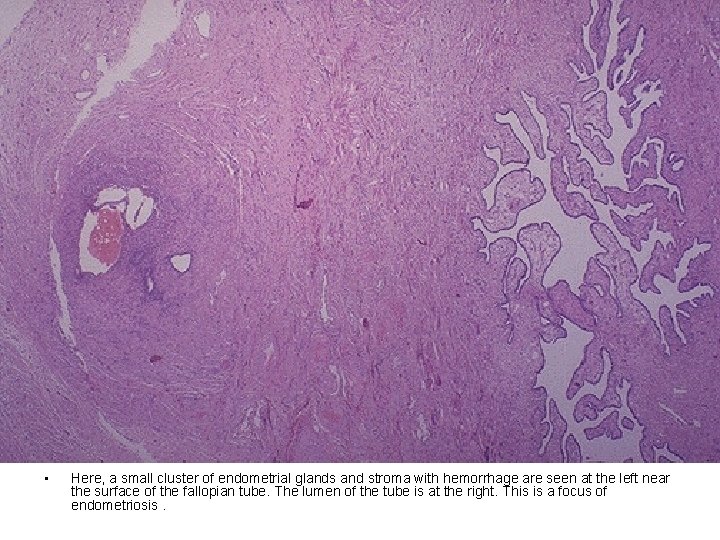
• Here, a small cluster of endometrial glands and stroma with hemorrhage are seen at the left near the surface of the fallopian tube. The lumen of the tube is at the right. This is a focus of endometriosis.
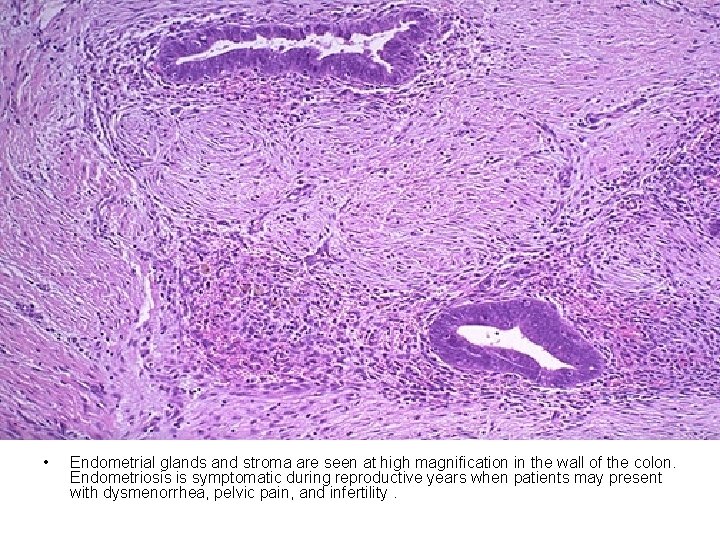
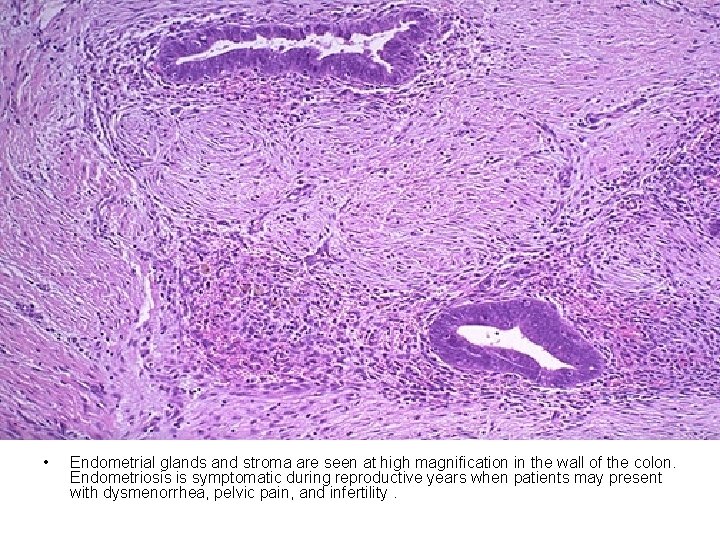
• Endometrial glands and stroma are seen at high magnification in the wall of the colon. Endometriosis is symptomatic during reproductive years when patients may present with dysmenorrhea, pelvic pain, and infertility.
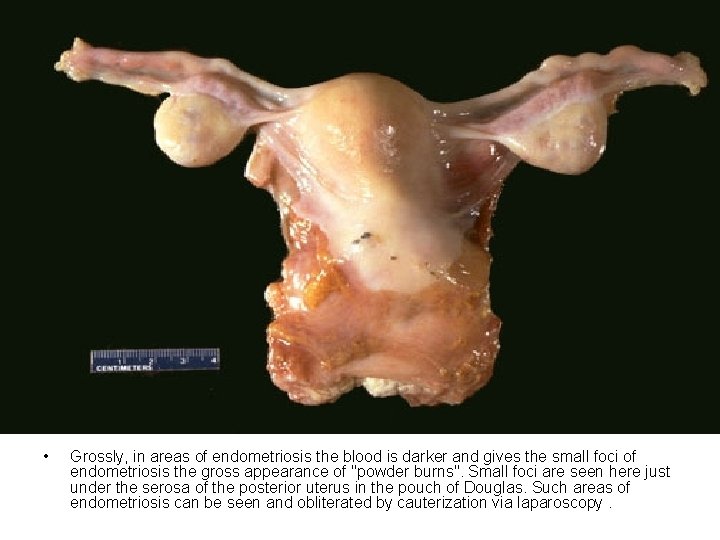
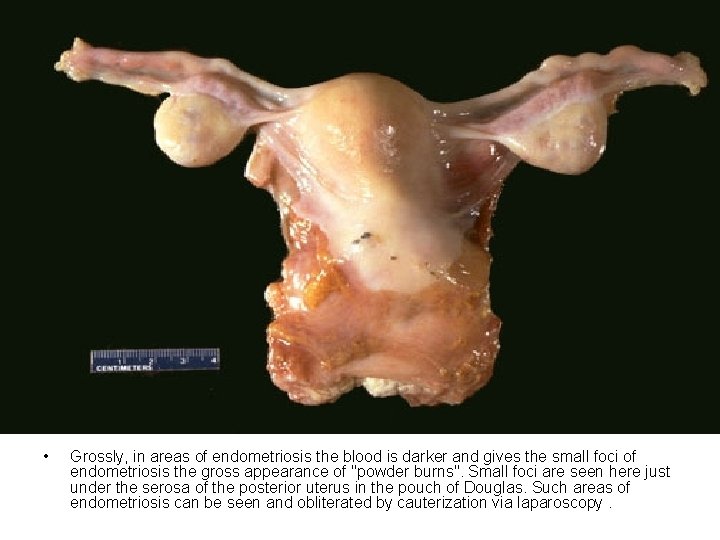
• Grossly, in areas of endometriosis the blood is darker and gives the small foci of endometriosis the gross appearance of "powder burns". Small foci are seen here just under the serosa of the posterior uterus in the pouch of Douglas. Such areas of endometriosis can be seen and obliterated by cauterization via laparoscopy.

• Upon closer view, these five small areas of endometriosis have a reddish-brown to bluish appearance. Typical locations for endometriosis may include: ovaries, uterine ligaments, rectovaginal septum, pelvic peritoneum, and laparotomy scars. Endometriosis may even be found at more distant locations such as appendix and vagina.
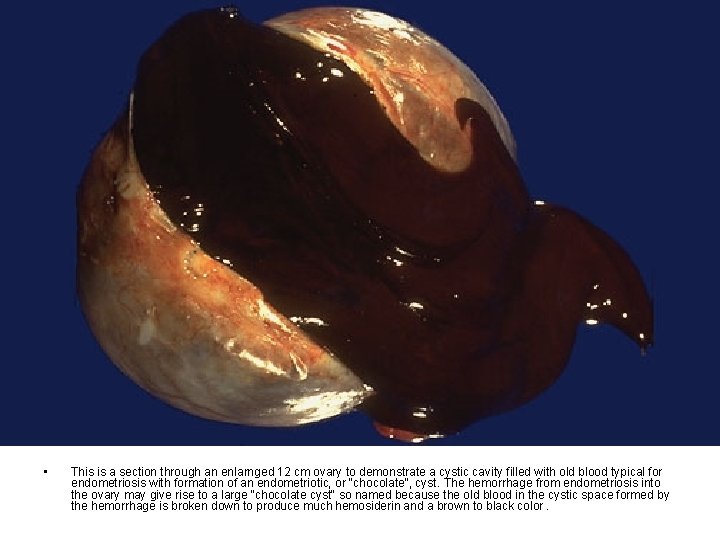
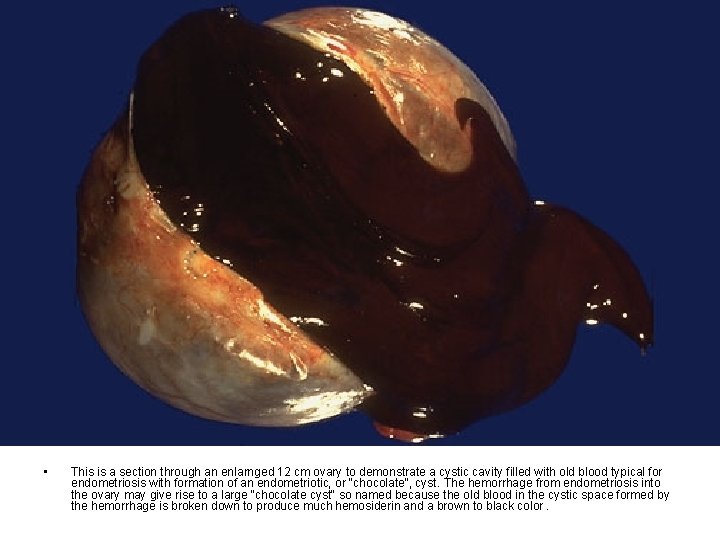
• This is a section through an enlarnged 12 cm ovary to demonstrate a cystic cavity filled with old blood typical for endometriosis with formation of an endometriotic, or "chocolate", cyst. The hemorrhage from endometriosis into the ovary may give rise to a large "chocolate cyst" so named because the old blood in the cystic space formed by the hemorrhage is broken down to produce much hemosiderin and a brown to black color.

• In the upper fundus of the uterus protruding into the endometrial cavity is a nodule that proved to be a leiomyoma. Thus, this is a submucosal leiomyoma. Such benign smooth muscle tumors of the myometrium are very common, perhaps 1 in 5 women has one. They may be the cause of irregular bleeding if placed submucosally, as seen here, or if large.

• Smooth muscle tumors of the uterus are often multiple. Seen here are submucosal, intramural, and subserosal leiomyomata of the uterus.
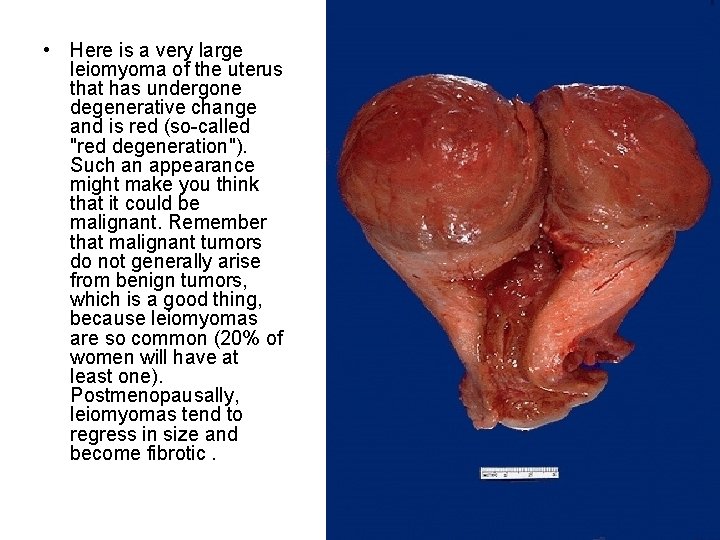
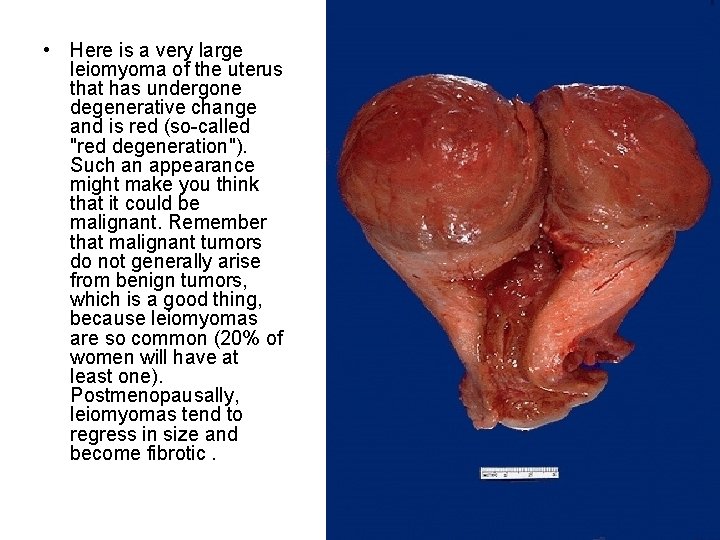
• Here is a very large leiomyoma of the uterus that has undergone degenerative change and is red (so-called "red degeneration"). Such an appearance might make you think that it could be malignant. Remember that malignant tumors do not generally arise from benign tumors, which is a good thing, because leiomyomas are so common (20% of women will have at least one). Postmenopausally, leiomyomas tend to regress in size and become fibrotic.
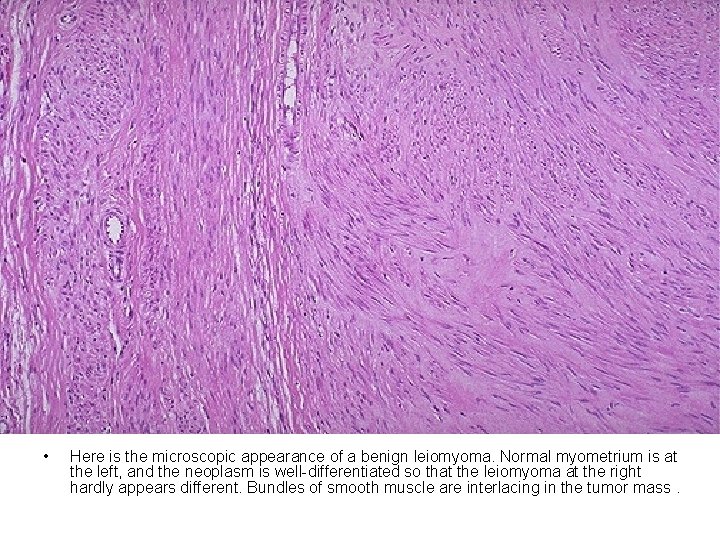
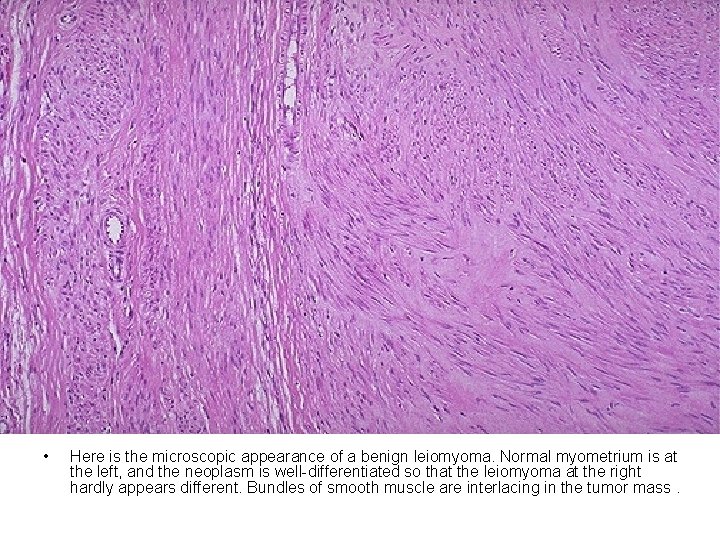
• Here is the microscopic appearance of a benign leiomyoma. Normal myometrium is at the left, and the neoplasm is well-differentiated so that the leiomyoma at the right hardly appears different. Bundles of smooth muscle are interlacing in the tumor mass.

• This is a leiomyosarcoma protruding from myometrium into the endometrial cavity of this uterus that has been opened laterally so that the halves of the cervix appear at right and left. Fallopian tubes and ovaries project from top and bottom. The irregular nature of this mass suggests that is not just an ordinary leiomyoma.
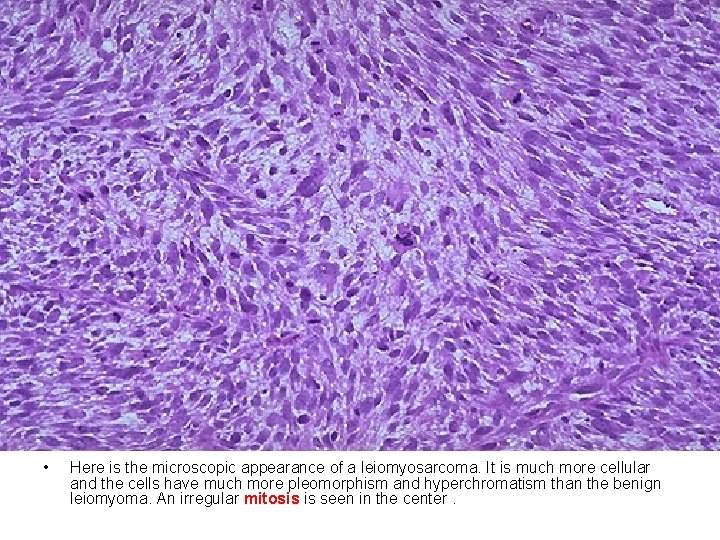
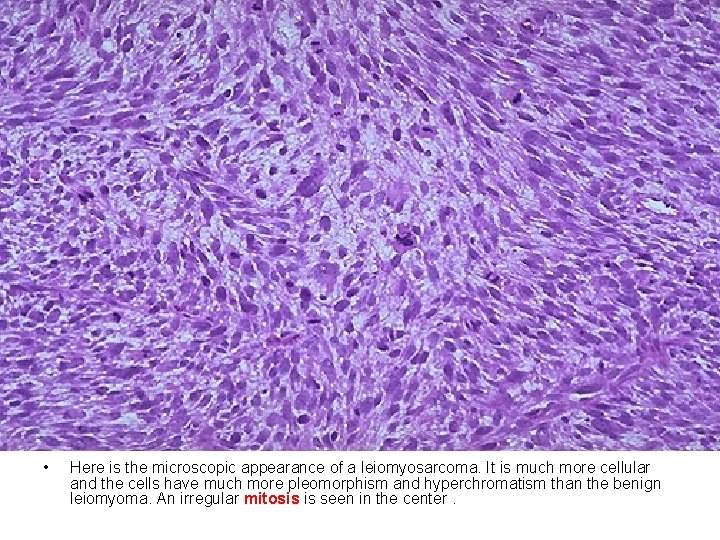
• Here is the microscopic appearance of a leiomyosarcoma. It is much more cellular and the cells have much more pleomorphism and hyperchromatism than the benign leiomyoma. An irregular mitosis is seen in the center.

• As with sarcomas in general, leiomyosarcomas have spindle cells. Several mitoses are seen here, just in this one high power field.
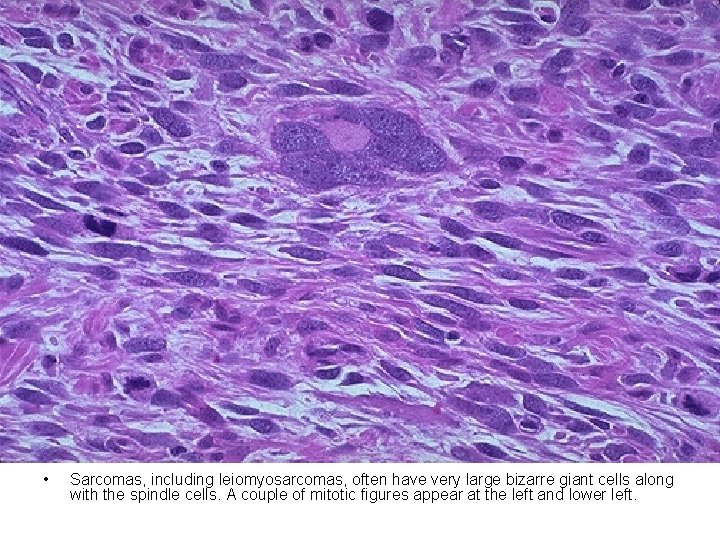
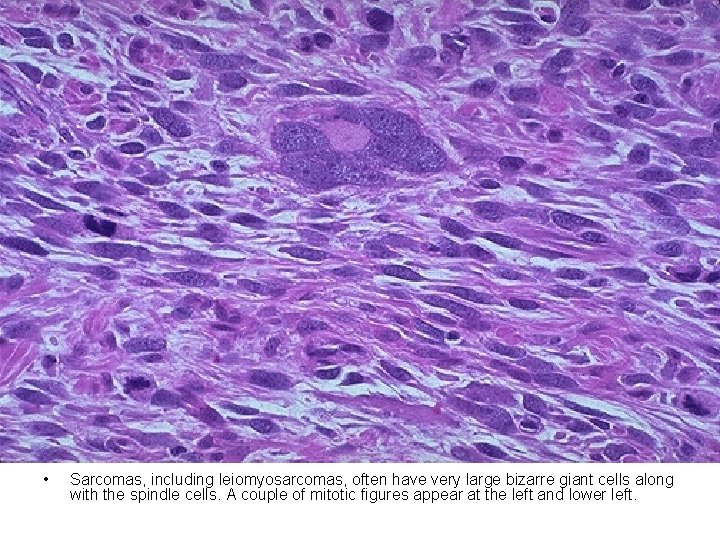
• Sarcomas, including leiomyosarcomas, often have very large bizarre giant cells along with the spindle cells. A couple of mitotic figures appear at the left and lower left.
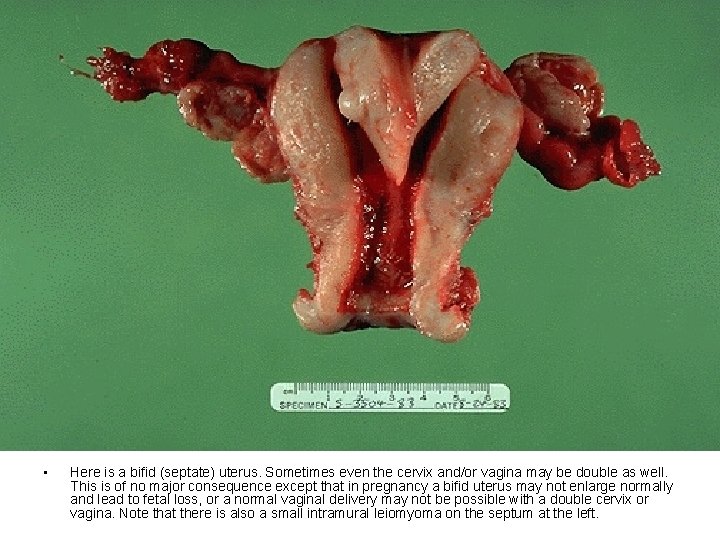
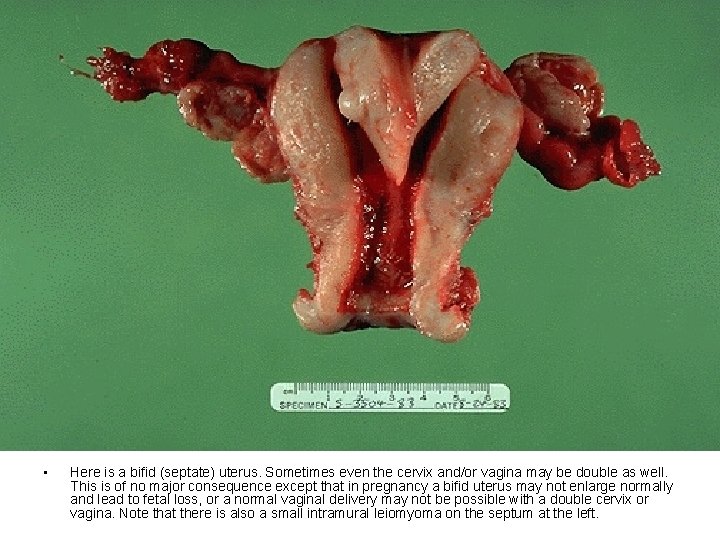
• Here is a bifid (septate) uterus. Sometimes even the cervix and/or vagina may be double as well. This is of no major consequence except that in pregnancy a bifid uterus may not enlarge normally and lead to fetal loss, or a normal vaginal delivery may not be possible with a double cervix or vagina. Note that there is also a small intramural leiomyoma on the septum at the left.
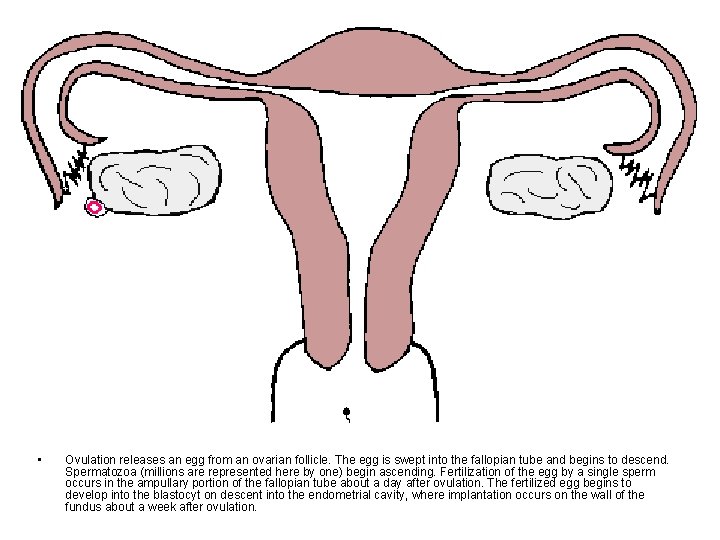
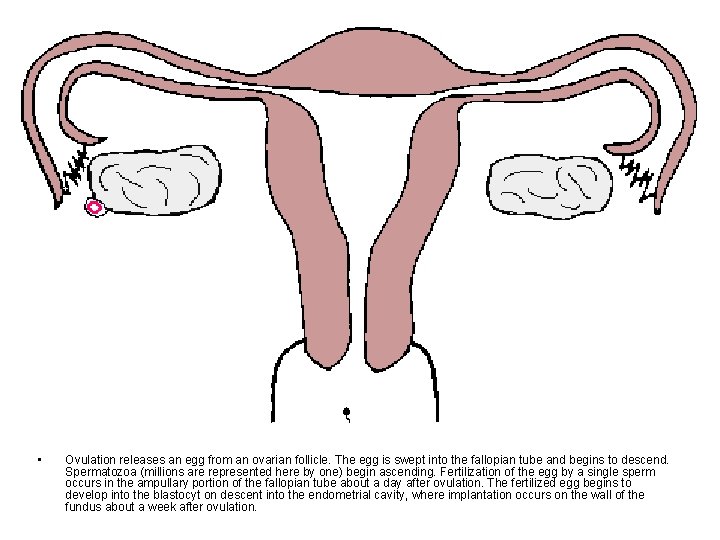
• Ovulation releases an egg from an ovarian follicle. The egg is swept into the fallopian tube and begins to descend. Spermatozoa (millions are represented here by one) begin ascending. Fertilization of the egg by a single sperm occurs in the ampullary portion of the fallopian tube about a day after ovulation. The fertilized egg begins to develop into the blastocyt on descent into the endometrial cavity, where implantation occurs on the wall of the fundus about a week after ovulation.
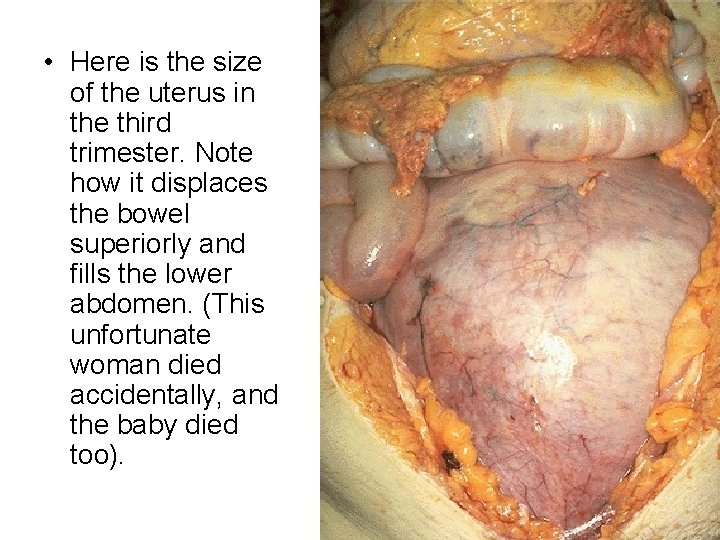
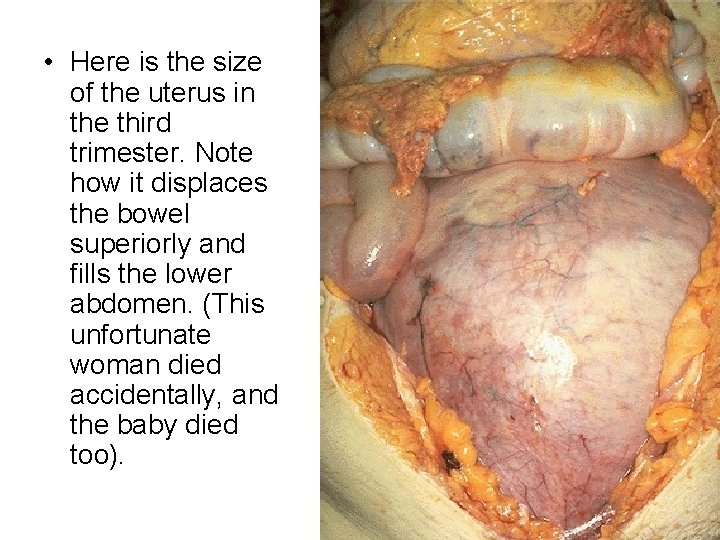
• Here is the size of the uterus in the third trimester. Note how it displaces the bowel superiorly and fills the lower abdomen. (This unfortunate woman died accidentally, and the baby died too).

• This is a normal postpartum uterus 5 days following delivery. Note how quickly the uterus is returning to its normal non-pregnant size.
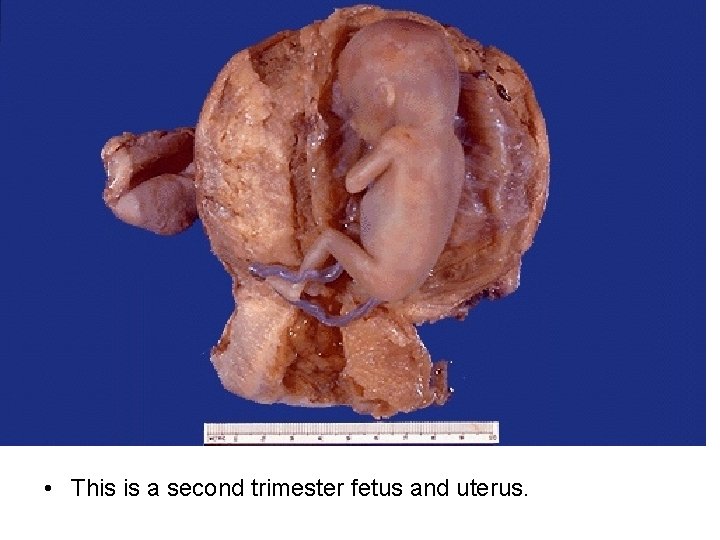
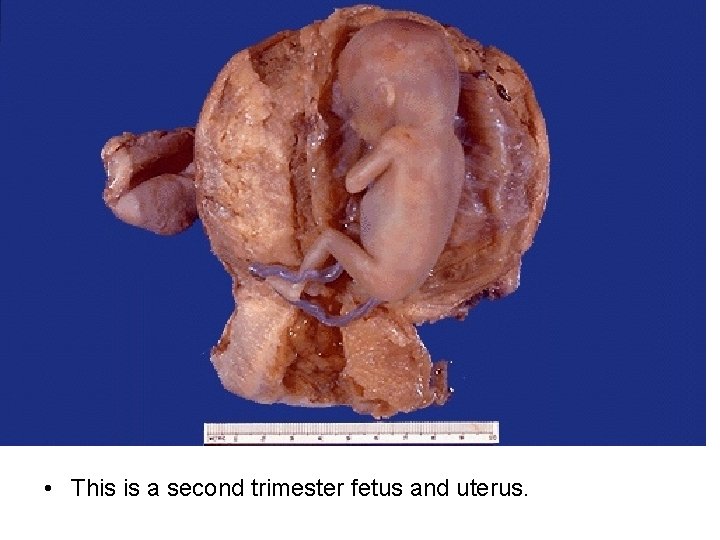
• This is a second trimester fetus and uterus.
Fallopian Tube
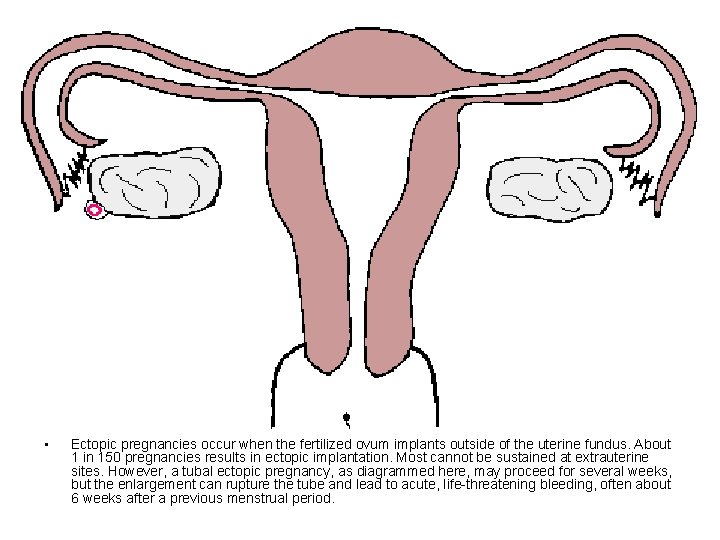
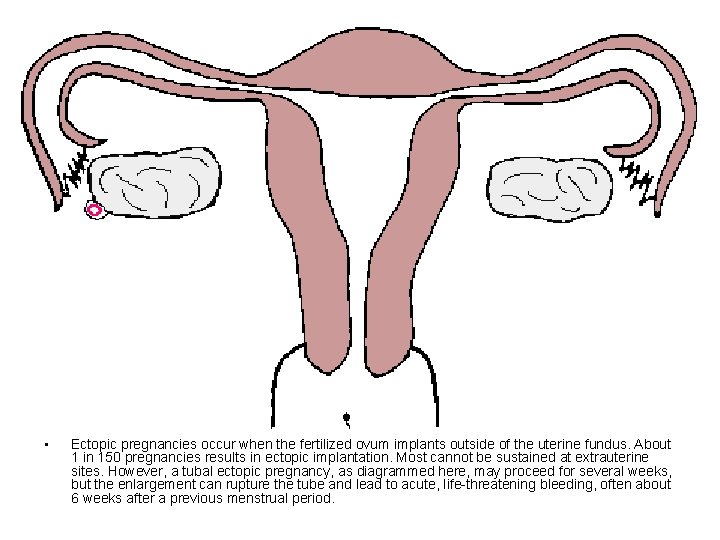
• Ectopic pregnancies occur when the fertilized ovum implants outside of the uterine fundus. About 1 in 150 pregnancies results in ectopic implantation. Most cannot be sustained at extrauterine sites. However, a tubal ectopic pregnancy, as diagrammed here, may proceed for several weeks, but the enlargement can rupture the tube and lead to acute, life-threatening bleeding, often about 6 weeks after a previous menstrual period.

• This is a ruptured tubal ectopic pregnancy. Note the twin fetuses at the lower right adjacent to the blood clot at the left. About half of ectopic pregnancies occur because of an identifiable lesion such as chronic salpingitis from pelvic inflammatory disease or adhesions from appendicitis, endometriosis, or previous laparotomy. However, in half of cases no cause can be found.

• Here is another ectopic pregnancy in a fallopian tube that was excised. This is a medical emergency because of the sudden rupture with hemoperitoneum. Ectopic pregnancy should be considered in the differential diagnosis of acute abdominal pain in a woman of childbearing age.
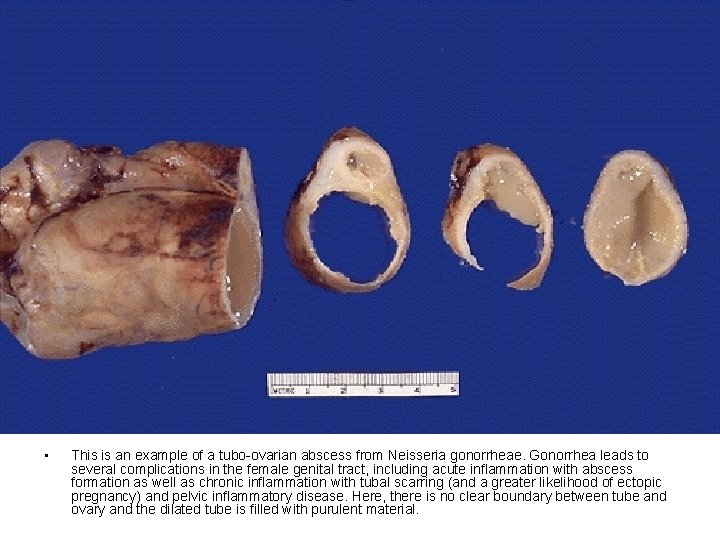
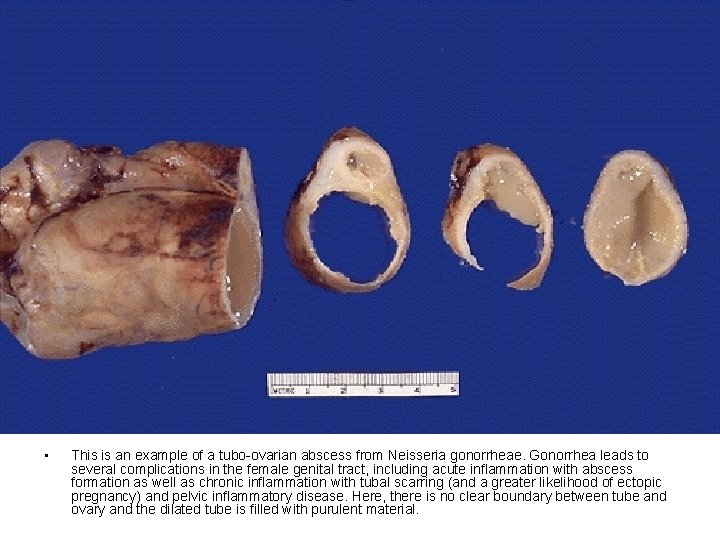
• This is an example of a tubo-ovarian abscess from Neisseria gonorrheae. Gonorrhea leads to several complications in the female genital tract, including acute inflammation with abscess formation as well as chronic inflammation with tubal scarring (and a greater likelihood of ectopic pregnancy) and pelvic inflammatory disease. Here, there is no clear boundary between tube and ovary and the dilated tube is filled with purulent material.
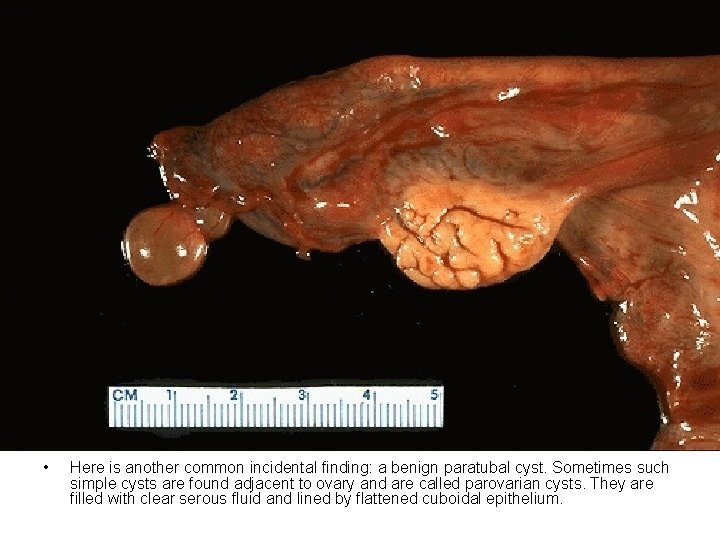
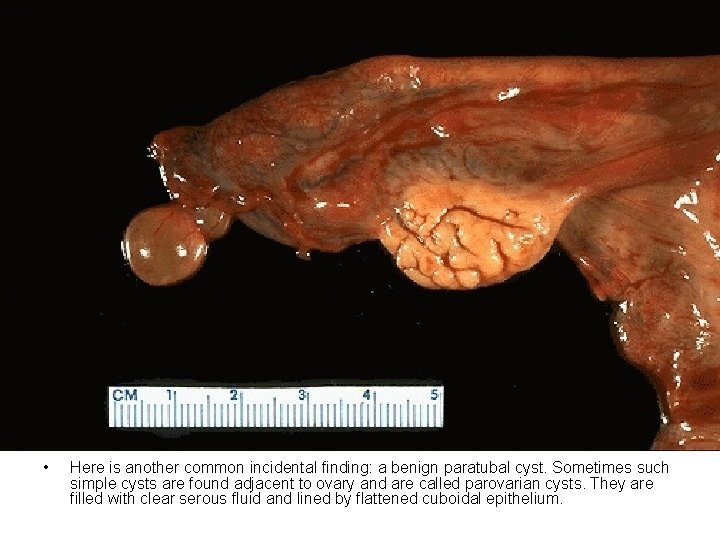
• Here is another common incidental finding: a benign paratubal cyst. Sometimes such simple cysts are found adjacent to ovary and are called parovarian cysts. They are filled with clear serous fluid and lined by flattened cuboidal epithelium.
Ovary

• This is an adult ovary with two corpora lutea. The larger one at the top is a hemorrhagic corpus luteum of menstruation, and the smaller one at the bottom is involuting from a previous menstrual period. If implantation of a fertilized ovum occurs, then the corpus luteum will persist because of HCG from the placenta. Of 400, 000 ovarian follicles present at birth, only about 400 will mature to the point of ovulation during childbearing years.
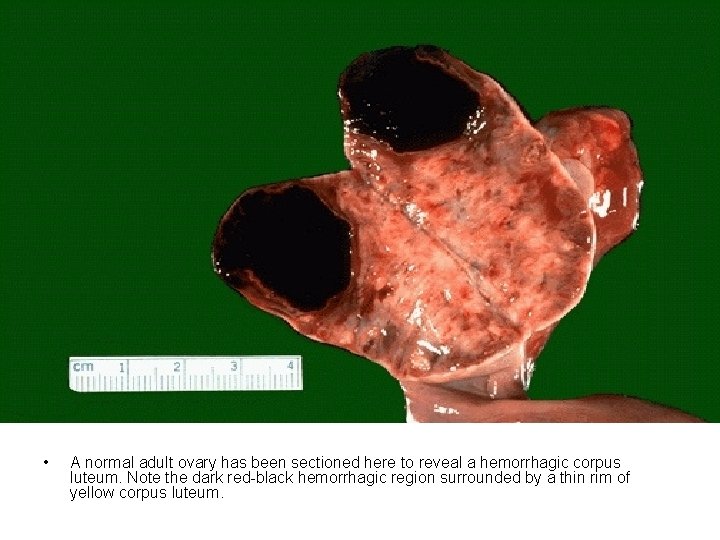
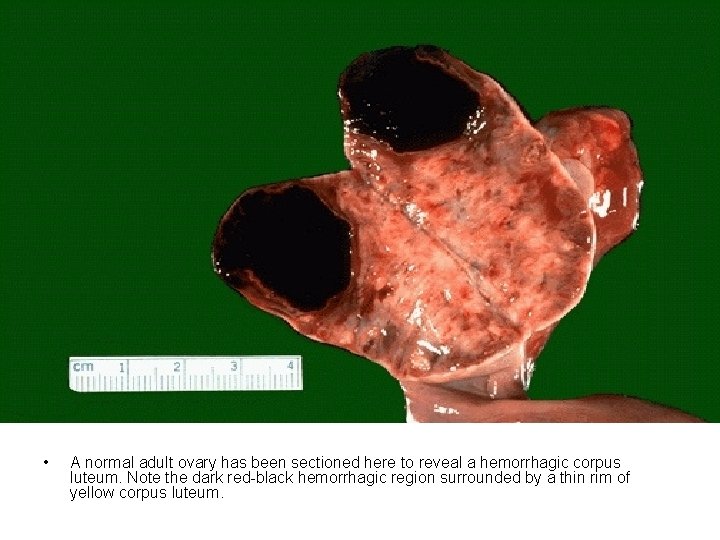
• A normal adult ovary has been sectioned here to reveal a hemorrhagic corpus luteum. Note the dark red-black hemorrhagic region surrounded by a thin rim of yellow corpus luteum.
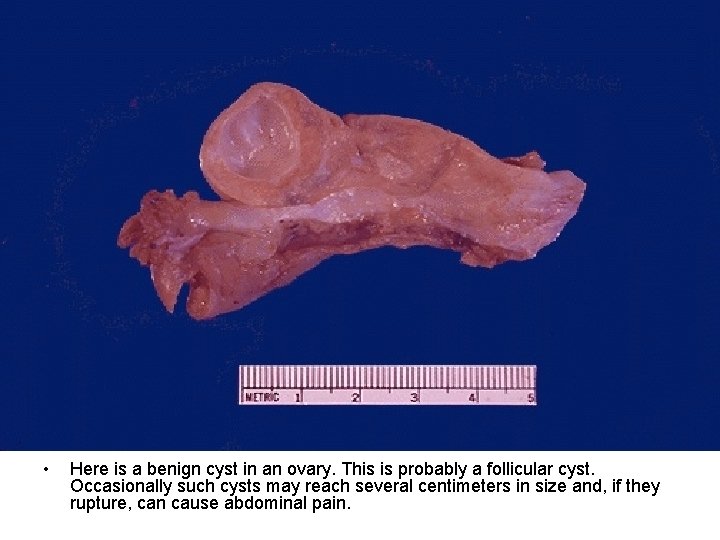
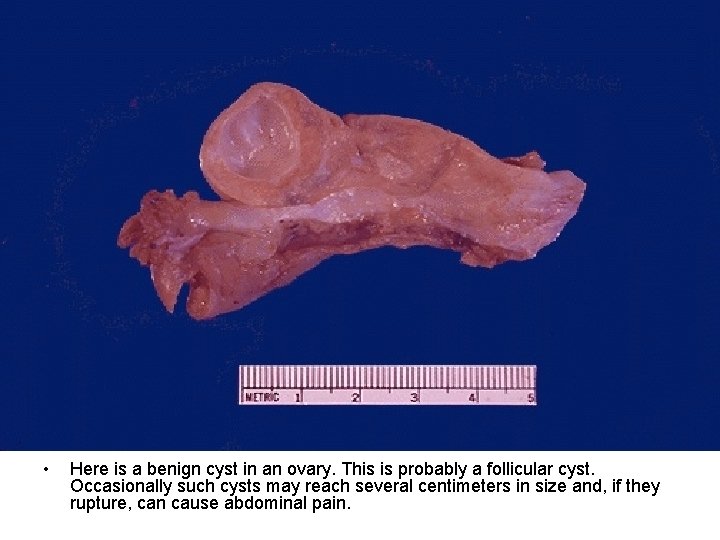
• Here is a benign cyst in an ovary. This is probably a follicular cyst. Occasionally such cysts may reach several centimeters in size and, if they rupture, can cause abdominal pain.
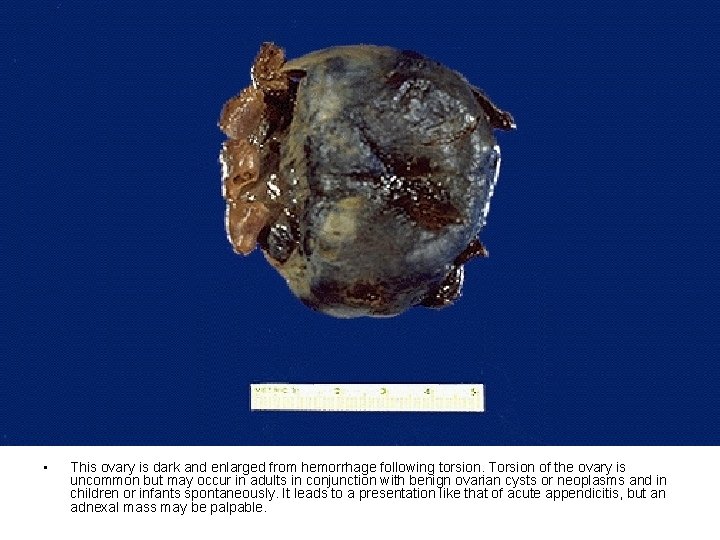
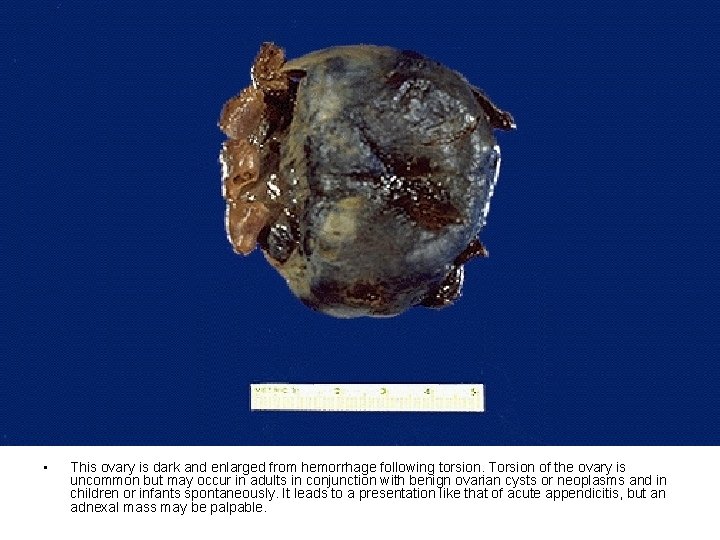
• This ovary is dark and enlarged from hemorrhage following torsion. Torsion of the ovary is uncommon but may occur in adults in conjunction with benign ovarian cysts or neoplasms and in children or infants spontaneously. It leads to a presentation like that of acute appendicitis, but an adnexal mass may be palpable.


• Here is an ovarian stromal tumor that is hard and white and is a fibroma.
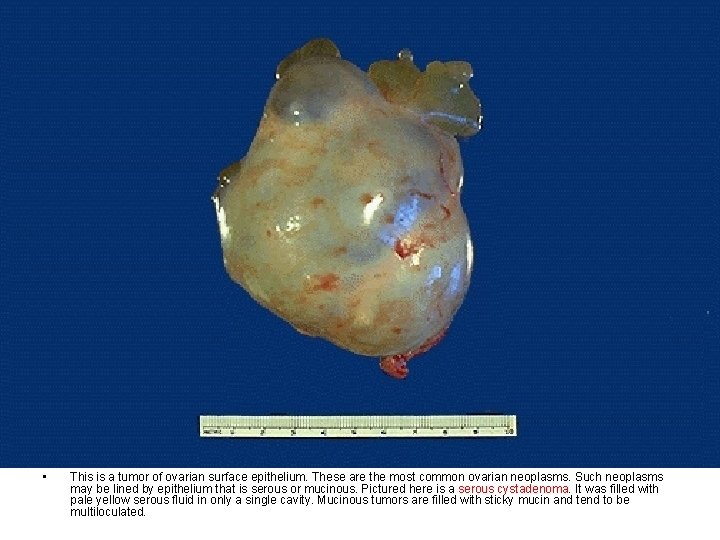
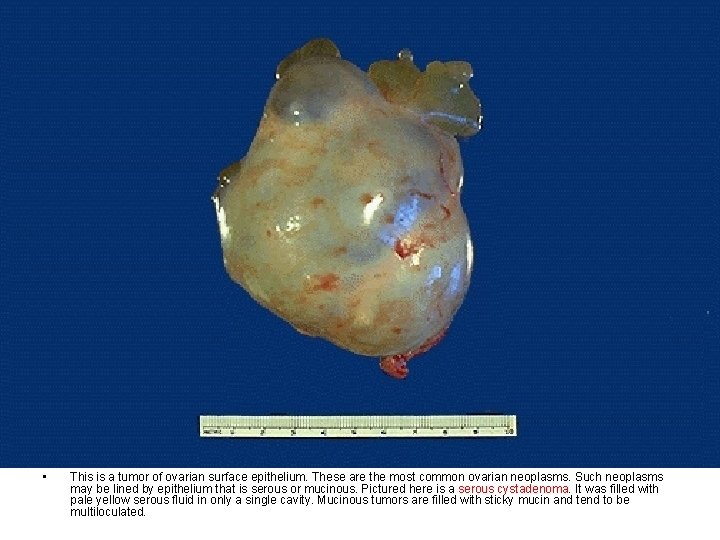
• This is a tumor of ovarian surface epithelium. These are the most common ovarian neoplasms. Such neoplasms may be lined by epithelium that is serous or mucinous. Pictured here is a serous cystadenoma. It was filled with pale yellow serous fluid in only a single cavity. Mucinous tumors are filled with sticky mucin and tend to be multiloculated.

• Benign epithelial tumors of the ovary can reach massive proportions. The serous cystadenoma seen here fills a surgical pan and dwarfs the 4 cm ruler.
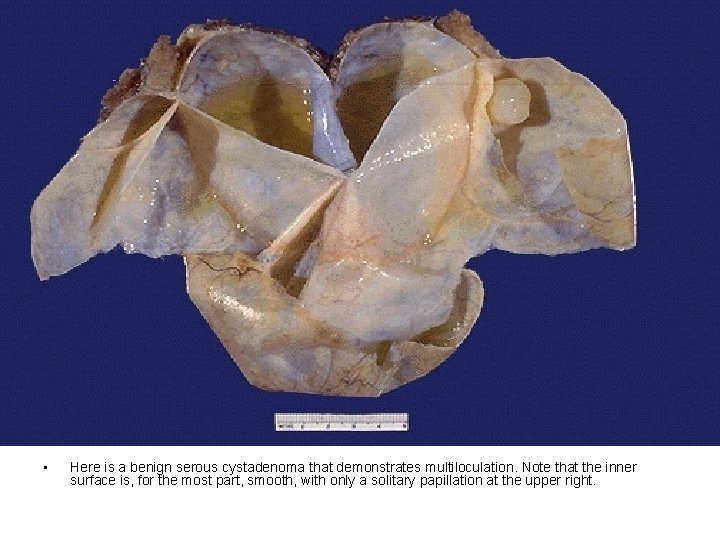
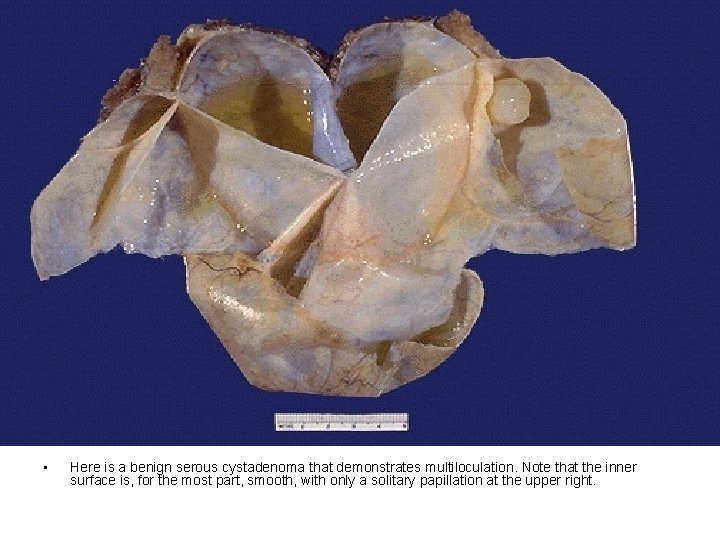
• Here is a benign serous cystadenoma that demonstrates multiloculation. Note that the inner surface is, for the most part, smooth, with only a solitary papillation at the upper right.
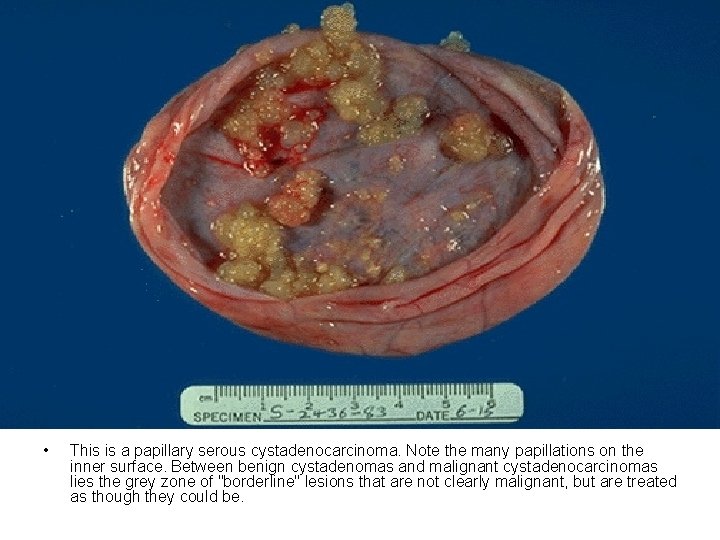
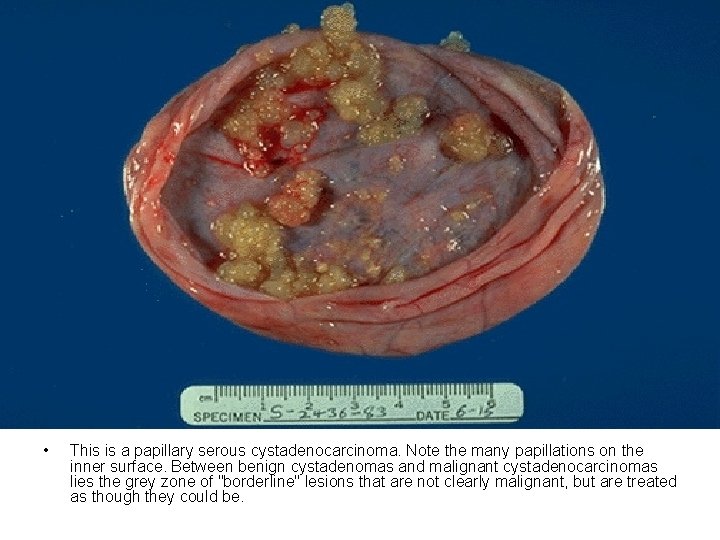
• This is a papillary serous cystadenocarcinoma. Note the many papillations on the inner surface. Between benign cystadenomas and malignant cystadenocarcinomas lies the grey zone of "borderline" lesions that are not clearly malignant, but are treated as though they could be.
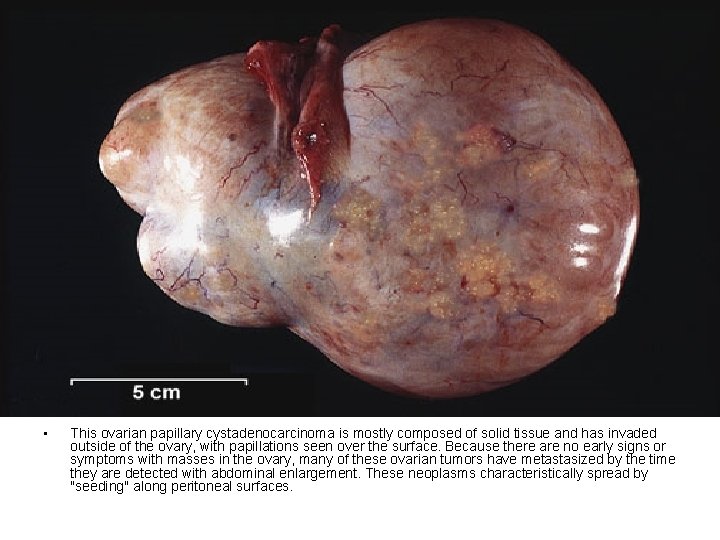
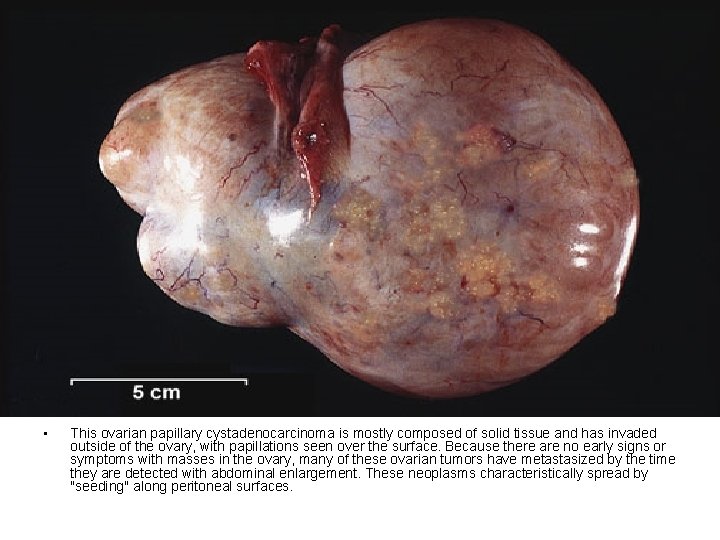
• This ovarian papillary cystadenocarcinoma is mostly composed of solid tissue and has invaded outside of the ovary, with papillations seen over the surface. Because there are no early signs or symptoms with masses in the ovary, many of these ovarian tumors have metastasized by the time they are detected with abdominal enlargement. These neoplasms characteristically spread by "seeding" along peritoneal surfaces.
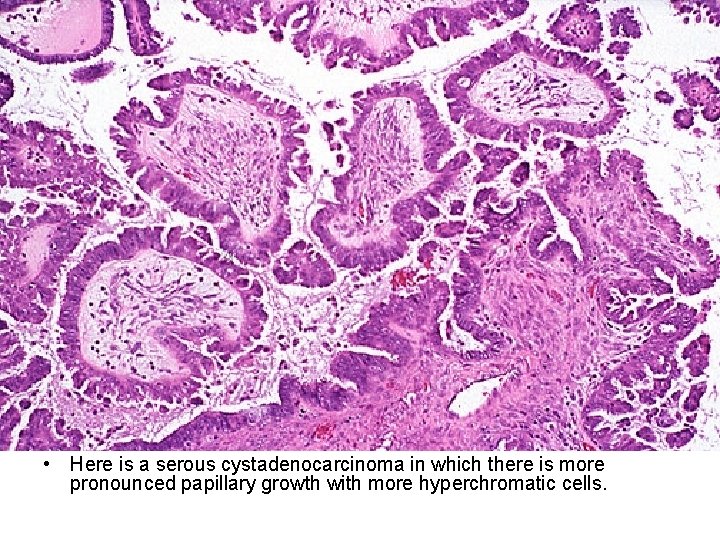
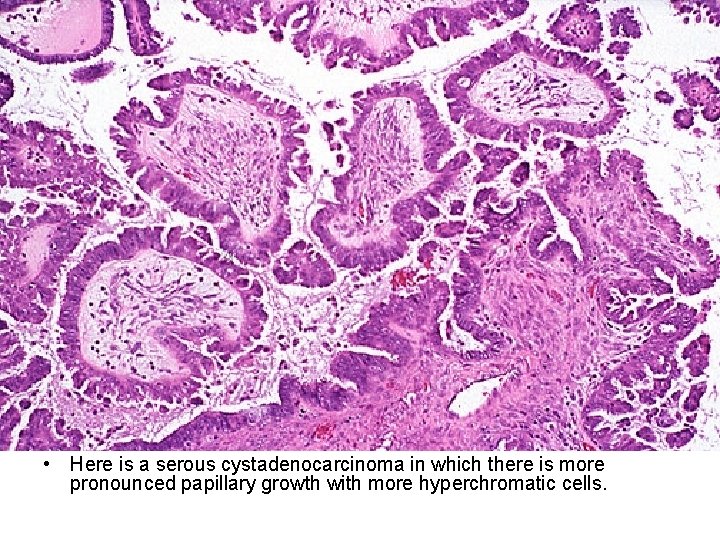
• Here is a serous cystadenocarcinoma in which there is more pronounced papillary growth with more hyperchromatic cells.
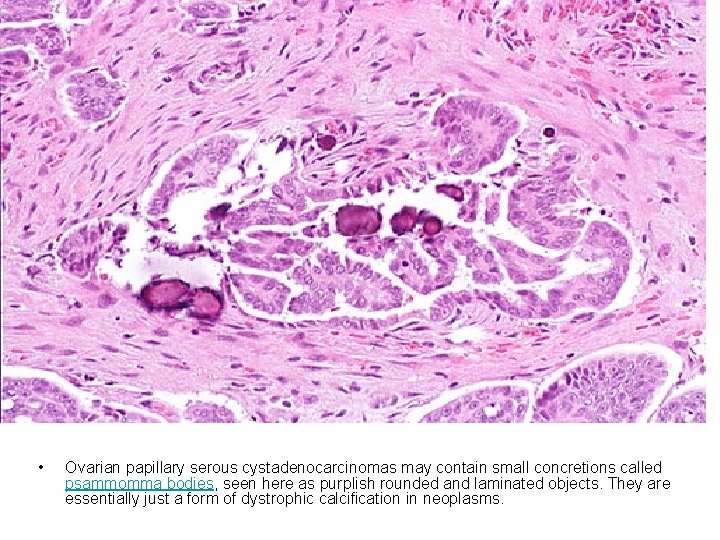
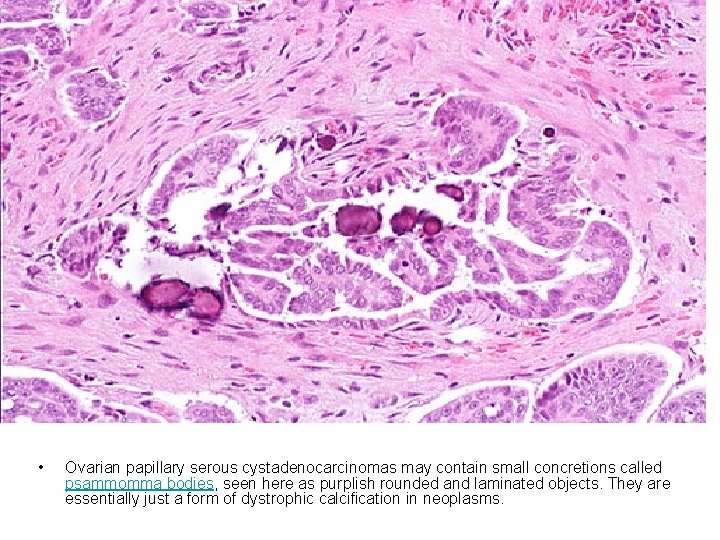
• Ovarian papillary serous cystadenocarcinomas may contain small concretions called psammomma bodies, seen here as purplish rounded and laminated objects. They are essentially just a form of dystrophic calcification in neoplasms.
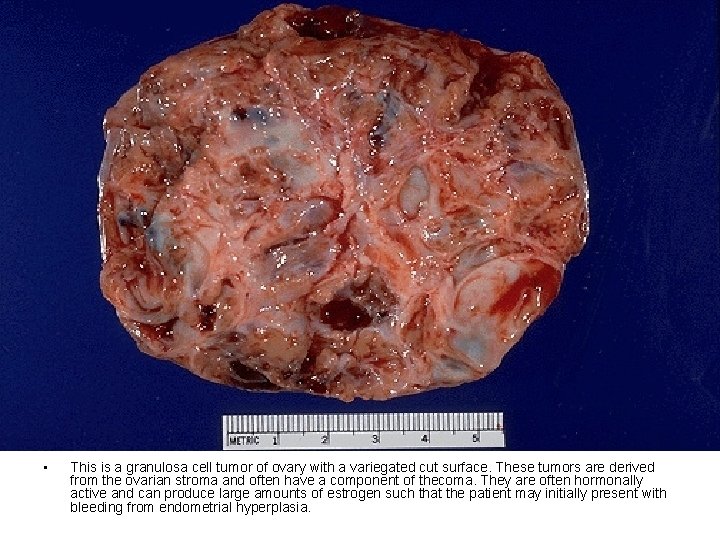
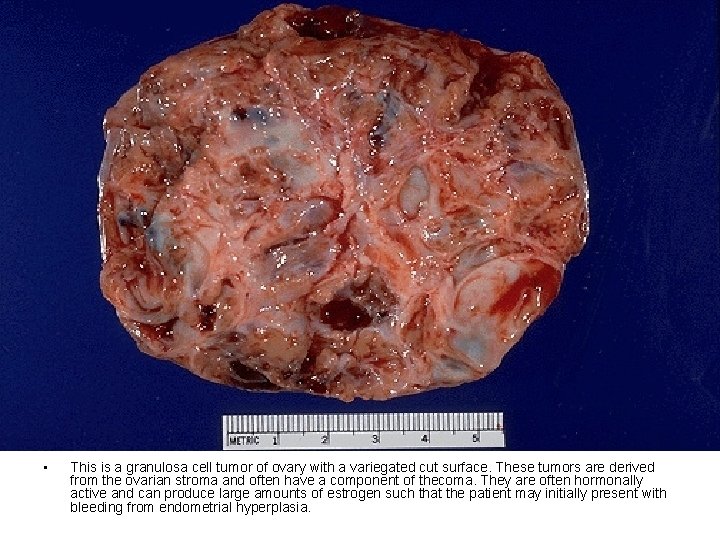
• This is a granulosa cell tumor of ovary with a variegated cut surface. These tumors are derived from the ovarian stroma and often have a component of thecoma. They are often hormonally active and can produce large amounts of estrogen such that the patient may initially present with bleeding from endometrial hyperplasia.
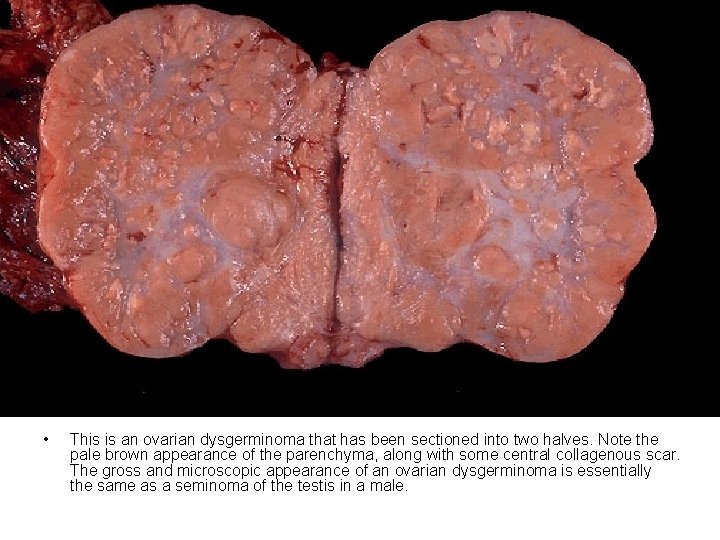
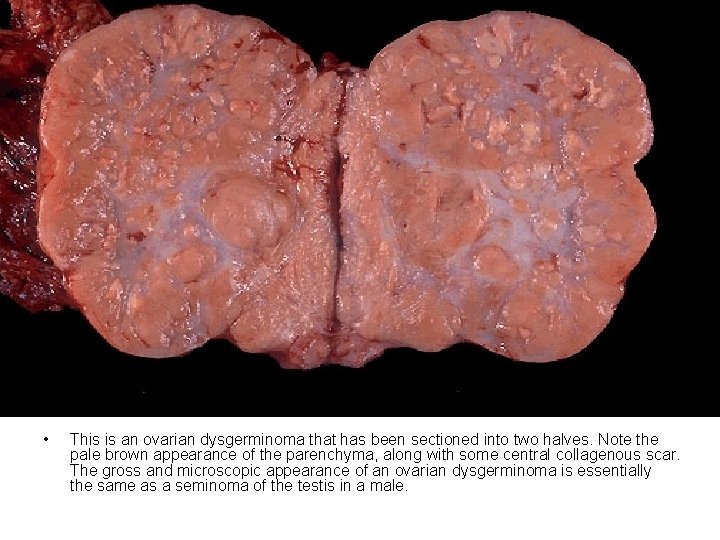
• This is an ovarian dysgerminoma that has been sectioned into two halves. Note the pale brown appearance of the parenchyma, along with some central collagenous scar. The gross and microscopic appearance of an ovarian dysgerminoma is essentially the same as a seminoma of the testis in a male.

• Here are bilateral mature cystic teratomas of the ovaries. These are a form of ovarian germ cell tumor. Histologically, a variety of mature tissue elements may be found. These tumors are often called "dermoid cysts" because they are mostly cystic.
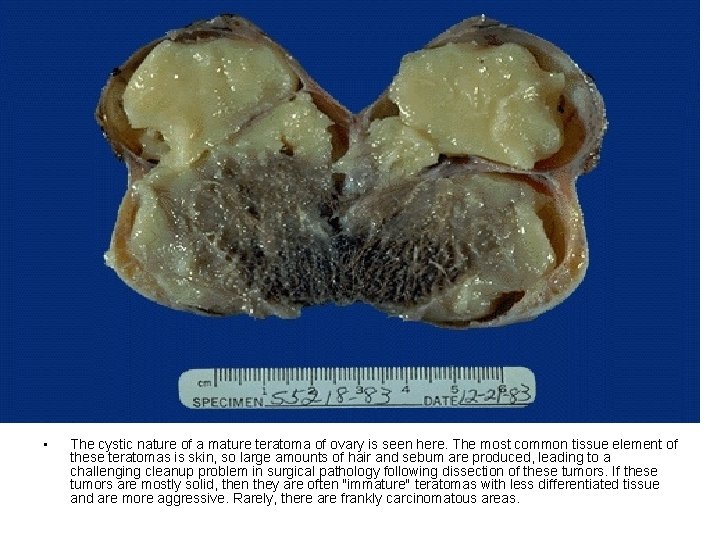
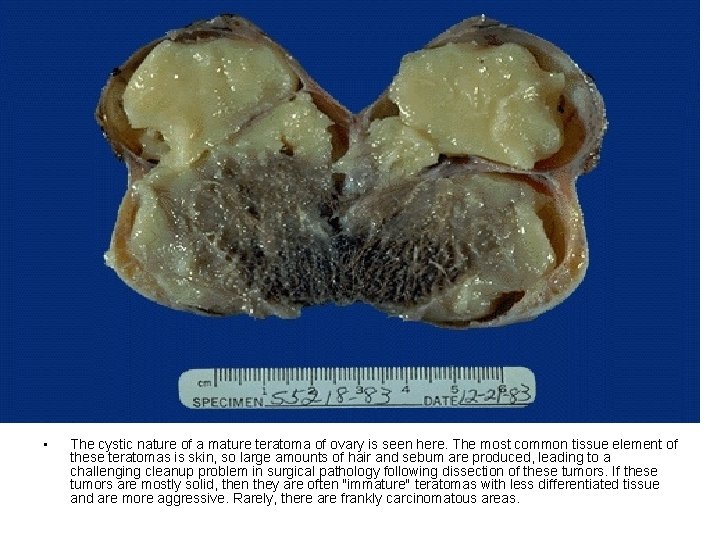
• The cystic nature of a mature teratoma of ovary is seen here. The most common tissue element of these teratomas is skin, so large amounts of hair and sebum are produced, leading to a challenging cleanup problem in surgical pathology following dissection of these tumors. If these tumors are mostly solid, then they are often "immature" teratomas with less differentiated tissue and are more aggressive. Rarely, there are frankly carcinomatous areas.

• There is a large unilateral mature cystic teratoma seen here at the right (in left ovary--the uterus is opened anteriorly). The uterus has an intramural and a subserosal leiomyoma. The other ovary is replaced by a fibroma.

• Microscopically, this teratoma has cartilage, adipose tissue, and intestinal glands at the right, while at the left is a lot of thyroid tissue. This condition can be termed struma ovarii. Rarely, a struma ovarii can even be a cause for hyperthyroidism.

• Metastatic tumors to ovary are uncommon, but there is one situation in which a metastatic adenocarcinoma to ovary appears as a large mass and resembles a primary tumor: a so-called "Krukenberg" tumor of ovary which has a signet ring histologic pattern and usually is metastatic from a primary in gastrointestinal tract. Seen here extending out of the pelvis at autopsy is a large right ovarian mass. .
THANK YOU
 Explaining female anatomy to child
Explaining female anatomy to child How deep is the cervix
How deep is the cervix Cervical ectropion
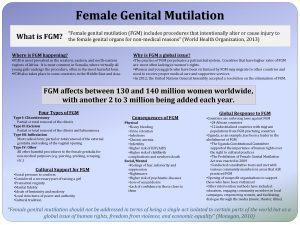
Cervical ectropion Female genital mutilation
Female genital mutilation Anteflexion of uterus
Anteflexion of uterus What is genital mutilation
What is genital mutilation Function of fallopian tube
Function of fallopian tube Kerozis nedir
Kerozis nedir Female body parts pictures name
Female body parts pictures name Lesiones benignas de vulva
Lesiones benignas de vulva Nerve supply uterus
Nerve supply uterus Vulva caracteristicas
Vulva caracteristicas Uterus layers
Uterus layers Vulva
Vulva Vulva
Vulva Lymphatic drainage of vulva
Lymphatic drainage of vulva S
S Batimentos cardíacos normais por idade
Batimentos cardíacos normais por idade Vulva
Vulva Ductos
Ductos Seccion frontal
Seccion frontal Vulvas blancas
Vulvas blancas Vulva
Vulva Vulva
Vulva Vaginal ring
Vaginal ring Vulvitis herpetica
Vulvitis herpetica Cortonen adalah
Cortonen adalah Anterior rhinoscopy structures
Anterior rhinoscopy structures Dr ashley fuller
Dr ashley fuller Klierbuizen
Klierbuizen Zona compacta and zona spongiosa
Zona compacta and zona spongiosa Normal endometrium kalınlığı
Normal endometrium kalınlığı Perimetrium
Perimetrium Function of endometrium
Function of endometrium Trilaminar endometrium
Trilaminar endometrium Funiculus sperm
Funiculus sperm Lush endometrium
Lush endometrium What is the uterine lining
What is the uterine lining Corpus luteum secretes progesterone
Corpus luteum secretes progesterone Tamoxifen endometrium ultrasound
Tamoxifen endometrium ultrasound Endometrum
Endometrum Structure of female
Structure of female Vaginalcytologi
Vaginalcytologi Slidetodoc.com
Slidetodoc.com Function of the vagina
Function of the vagina Cervix anatomy
Cervix anatomy Where is the vulver
Where is the vulver Horizontal vagina
Horizontal vagina Portio ektopia
Portio ektopia Cervical ectropion
Cervical ectropion Cervix vesicae
Cervix vesicae Bishop's score
Bishop's score Puerperiu.
Puerperiu. Organa genitalia feminina interna
Organa genitalia feminina interna Cervixconisatie
Cervixconisatie Cervix defintion
Cervix defintion Uterus cervix
Uterus cervix Inelastic cervix
Inelastic cervix Papsmear
Papsmear Tubotomi
Tubotomi Erosion
Erosion Cervix da vaca
Cervix da vaca Cervix da vaca
Cervix da vaca Cervix da vaca
Cervix da vaca Perimetrium
Perimetrium Cervix anatomy
Cervix anatomy What are the abnormal types of pelvis
What are the abnormal types of pelvis Dexamethasone action in pregnancy
Dexamethasone action in pregnancy Cervix fibonacci
Cervix fibonacci Stages of labor and delivery
Stages of labor and delivery Monoestrus
Monoestrus What std are curable
What std are curable Male genital variation
Male genital variation Genital hijyen
Genital hijyen La etapa falica
La etapa falica Phylum platyhelminthes class turbellaria
Phylum platyhelminthes class turbellaria Genital hijyen
Genital hijyen Genital hijyen nedir
Genital hijyen nedir Historia natural de la enfermedad herpes genital
Historia natural de la enfermedad herpes genital Hsv-2 oral transmission rates
Hsv-2 oral transmission rates Ciclo vital de familia
Ciclo vital de familia Dogfish shark internal anatomy
Dogfish shark internal anatomy