The Evolution of STEEEP7 Quantifying Improvement Interventions Against
- Slides: 20
The Evolution of STEEEP-7 Quantifying Improvement Interventions Against the IOM Quality Aims
• The presenters have no conflict of interest to report related to this presentation. • All presenters are employed by the University of Alabama at Birmingham • Dr. Shea Polancich, Ph. D, RN-Joint Appointment UAB Hospital Nursing Administration and Assistant Professor UAB SON • Dr. Terri Poe, DNP, RN-Chief Nursing Officer, UAB Hospital • Dr. Suzie Miltner, Ph. D, RN-Joint Appointment-Assistant Professor UAB SON, Birmingham Veteran’s Administration Hospital
Background • In 2015, the University of Alabama at Birmingham (UAB) CNO identified improvement opportunities from a system-wide perspective • Improvement teams were chartered and improvement facilitator began to work with teams • Projects produced multiple improvement interventions for each project • Difficulty deciding between interventions (outside of the cost) • No current standardized method for comparing improvement interventions • No current method of developing interventions within the organization that ensured that the IOM aims for quality were being met
The Pilot Project-A Case Study • Pressure transducer management was identified as a process in which variation in practice occurred within the organization • Variation existed in cost and supplies, level of provider who initiated and managed the set-up, education and competency assessment, and process management • Improvement team chartered that consisted of nursing managers from all of the inpatient intensive care units (ICU), anesthesia, hospital administration, data management, and an improvement facilitator
Improvement Goals for Project • Decrease variation in practice • Cost effectiveness and efficiency of the process • Patient safety through consistent standard of care and provider competency Primarily, the aims of the improvement, were the IOM quality aims: safe, timely, effective, efficient, equitable, patient-centered care
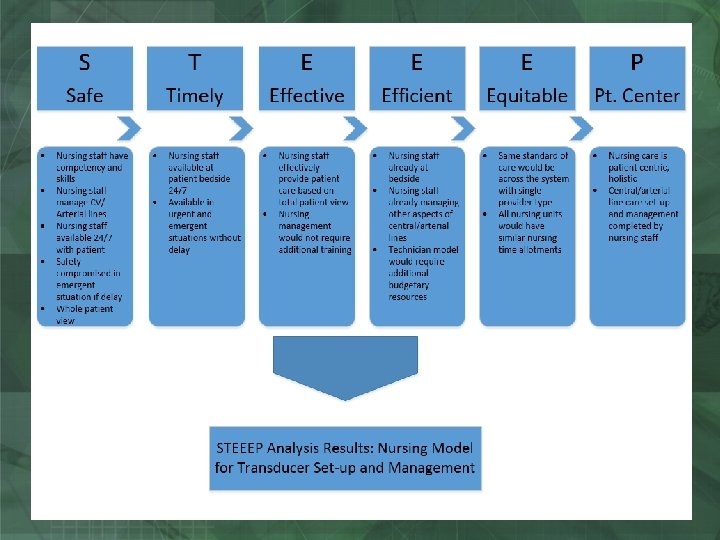
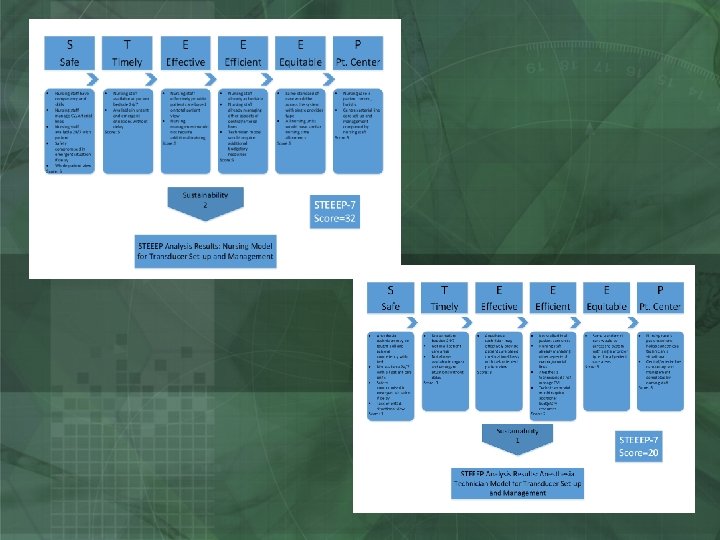
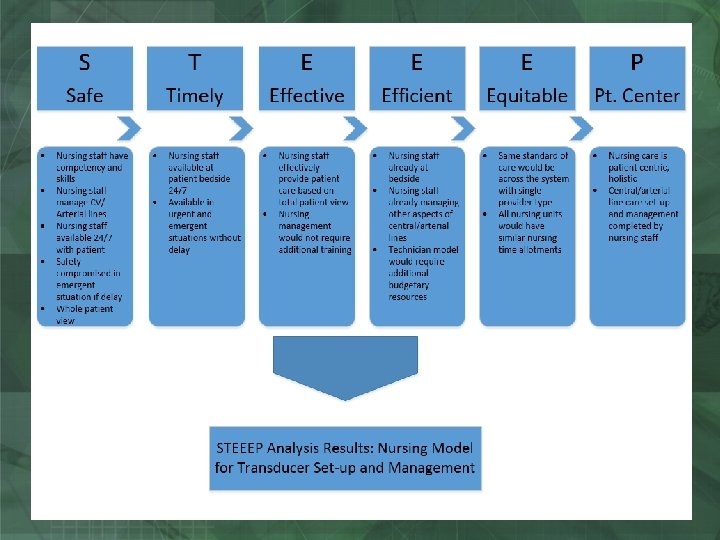
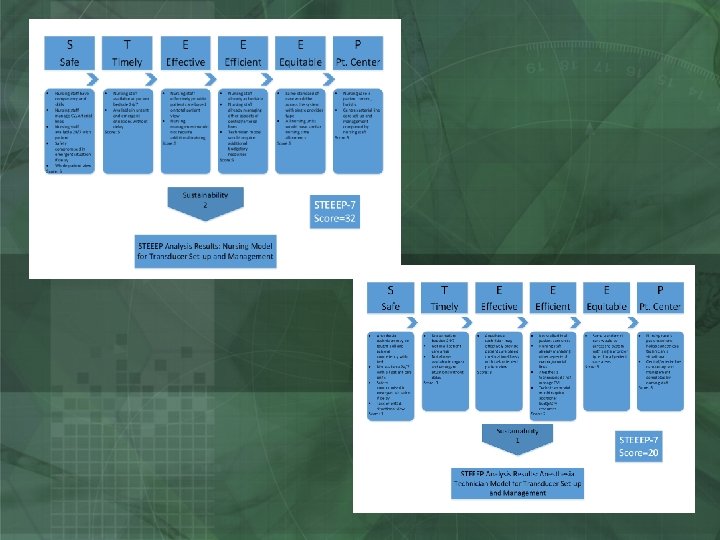
Ensuring the IOM Aims Were Met? • The improvement team reached a point in the process where there were opportunities to review and implement one of 3 different processes: • RN (Registered Nurse)-only managed process for pressure transducer management • Anesthesia tech only managed process for pressure transducer management • Hybrid model incorporating both RN and anesthesia tech providers *Examples that follow will only provide the evaluation of the RN only and anesthesia technician models using the tools
Comparing the 3 Processes • The improvement team was asked to compare three different processes in order to select the best “practice” process for the organization that would decrease variation in practice and produce a single, standardized care delivery process for the patients around pressure transducer management
Evaluating the Processes Against the IOM Quality Aims • It was determined that the best “practice” process would incorporate all aspects of the IOM Quality aims • As such, the improvement facilitator developed a visual method of incorporating the aims into an evaluation process for the improvement team
Initial STEEEP Evaluation Process-Qualitative Assessment • The initial STEEEP evaluation, as it was named was a qualitative assessment of each of the 3 provider management processes identified by the improvement team • Members of the team were asked to evaluate each process based on each of the STEEEP elements • Example provided for the RN-Only Management Model
Feedback on the STEEEP Qualitative Evaluation Tool • The improvement team responded very favorably to the visual aspect of the qualitative tool • The administrative team responded very favorably to the ability to use the aspects of the IOM quality aims to guide process (intervention) selection • The downside of the tool, however, was still how to quantify a difference in two or more processes or interventions
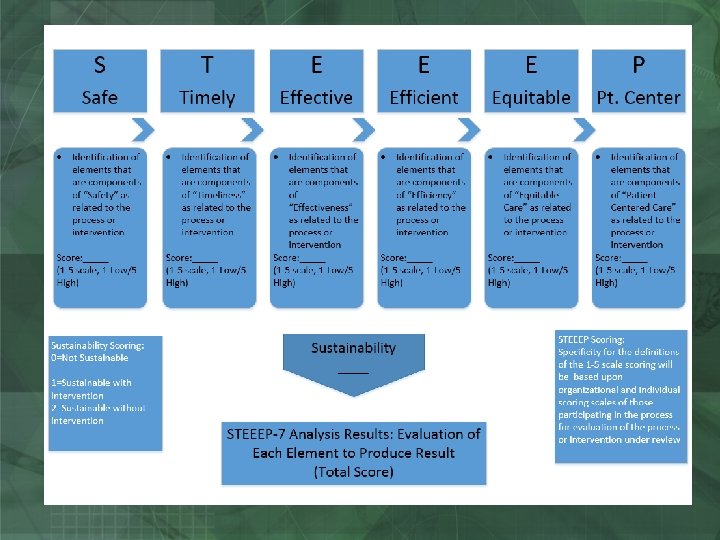
Evolution of the Qualitative STEEEP Tool into the Quantitative STEEEP-7 Tool • The qualitative STEEEP tool was enhanced to provide a quantitative element to the process • Similar in function to the Failure Mode Effects Analysis (FMEA), the STEEEP-7 added a dimension of evaluation scales and scoring analysis • An additional element was also added for “sustainability”. It was determined that sustainability was a frequently cited factor failure of past interventions, so the ability to assess that upfront was important • An example of the STEEEP-7 tool is provided
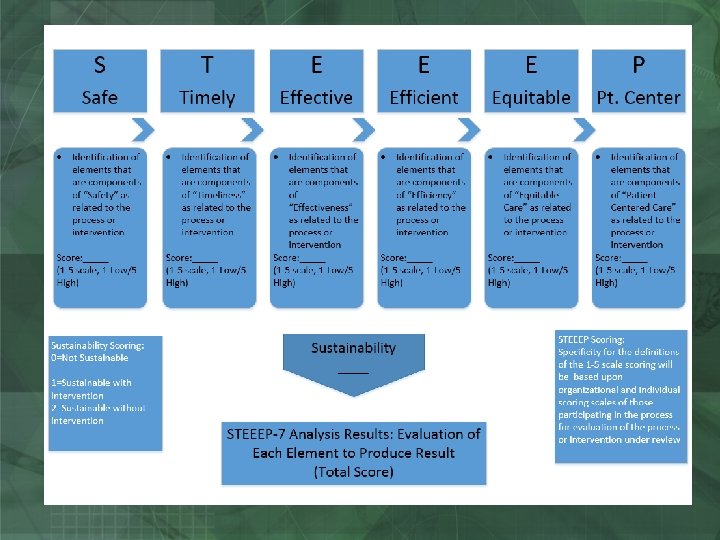
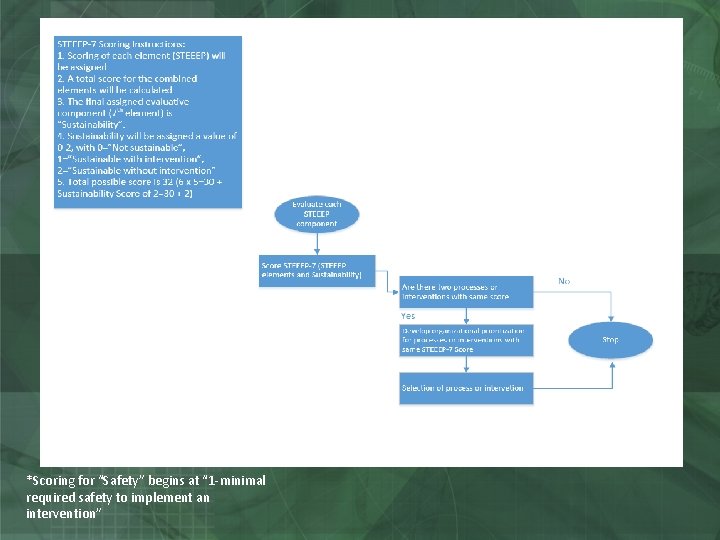
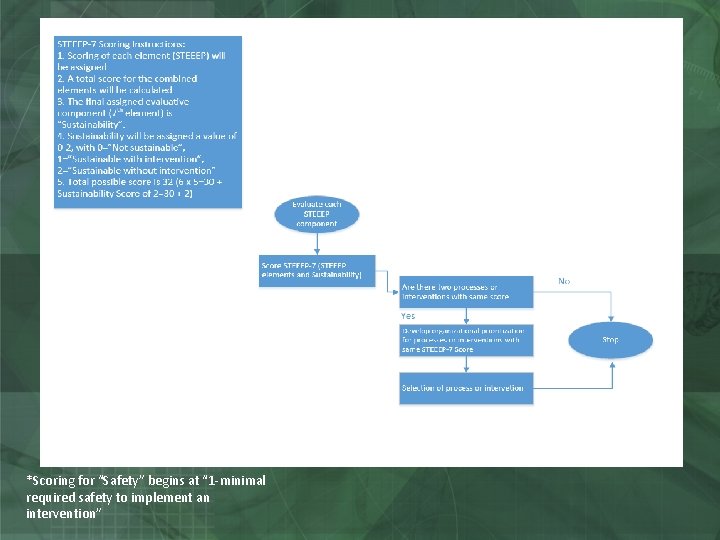
*Scoring for “Safety” begins at “ 1 -minimal required safety to implement an intervention”
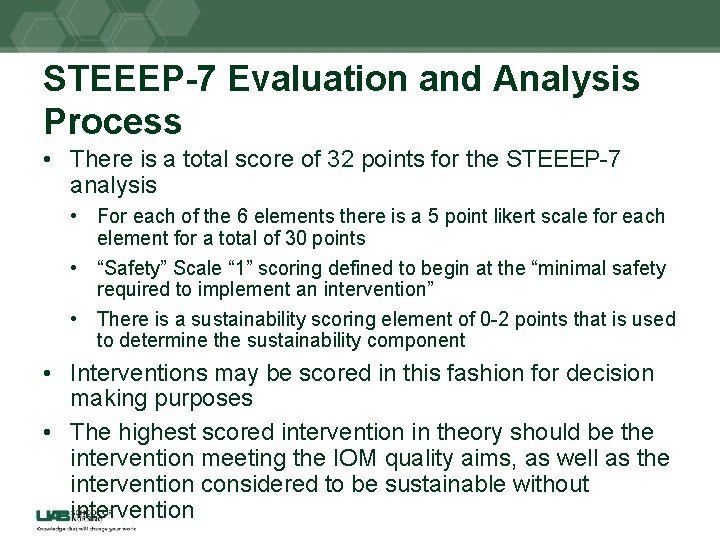
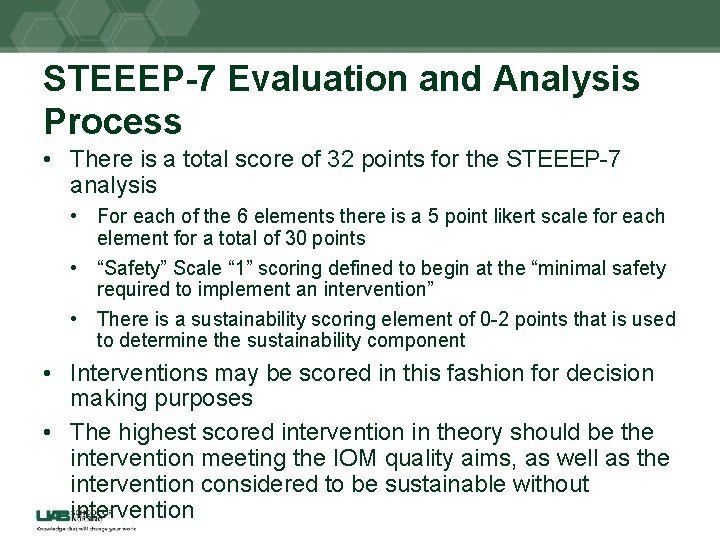
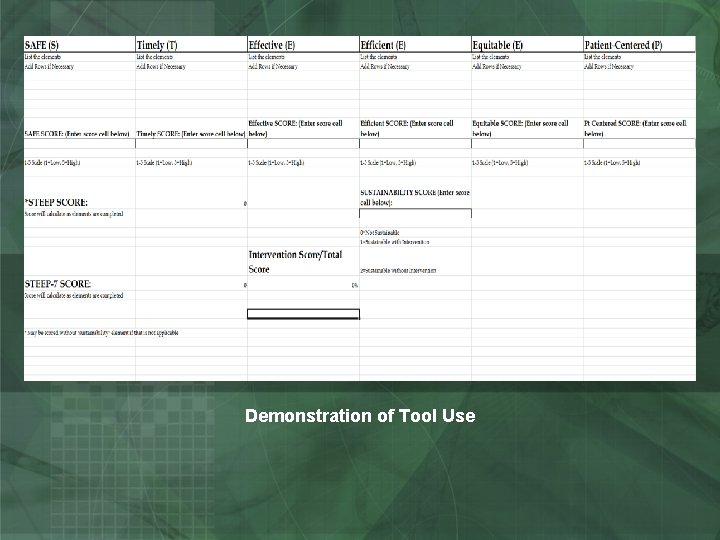
STEEEP-7 Evaluation and Analysis Process • There is a total score of 32 points for the STEEEP-7 analysis • For each of the 6 elements there is a 5 point likert scale for each element for a total of 30 points • “Safety” Scale “ 1” scoring defined to begin at the “minimal safety required to implement an intervention” • There is a sustainability scoring element of 0 -2 points that is used to determine the sustainability component • Interventions may be scored in this fashion for decision making purposes • The highest scored intervention in theory should be the intervention meeting the IOM quality aims, as well as the intervention considered to be sustainable without intervention
User Friendly STEEEP-7 Tool • For ease of use, the STEEEP-7 tool has been converted to an excel spreadsheet containing all the calculations for the process • Those interested in using the tool may request the spreadsheet from polancs@uab. edu
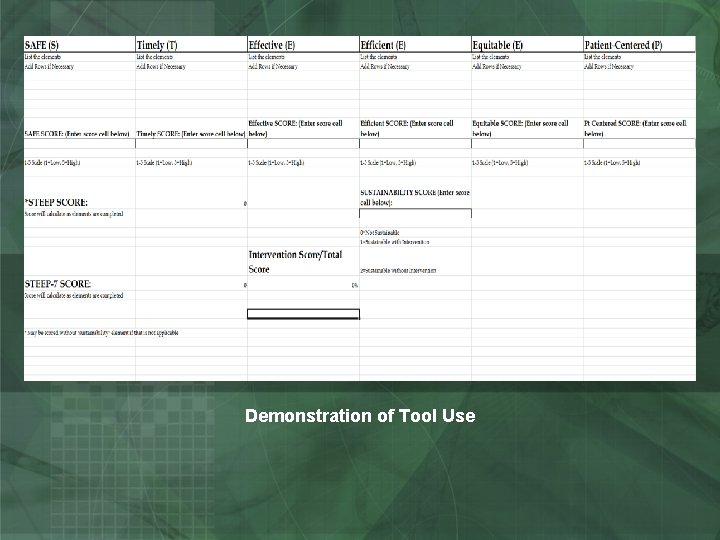
Demonstration of Tool Use
Next Steps • The STEEEP-7 tool is in its early evolutionary stages • The tool has been used in our organization for • Improvement projects • DNP students • Other students • The tool was received favorably by the improvement team and the administration team who used the process • A manuscript describing the evolution of the tool has been accepted for publication by Patient Safety and Quality in Healthcare (PSQH) anticipated publication date of April/May 2016 • We welcome additional testing and use by others.
Development Team • Shea Polancich, Ph. D, RN (spolancich@uabmc. edu or polancs@uab. edu) • Terri Poe, DNP, RN (terripoe@uabmc. edu) • Rebecca Miltner, Ph. D, RN (smiltner@uab. edu)