The Endocrine Physiology The Pituitary Gland Dr Khalid











- Slides: 48

The Endocrine Physiology The Pituitary Gland Dr. Khalid Alregaiey
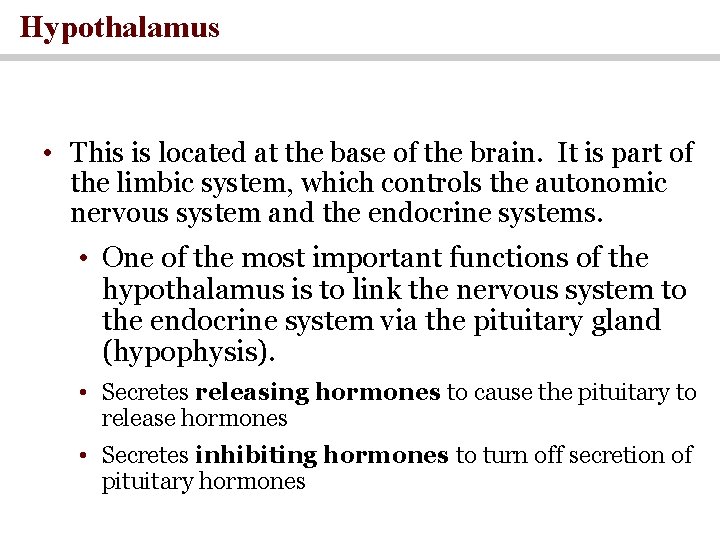
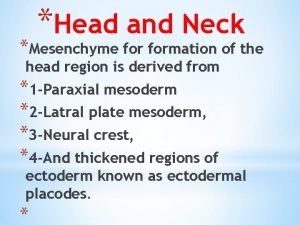
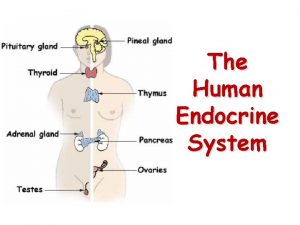
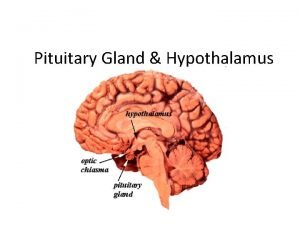
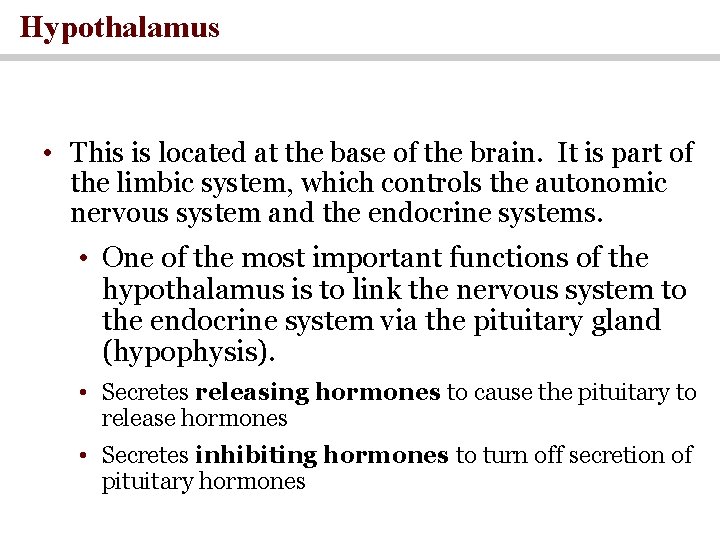
Hypothalamus • This is located at the base of the brain. It is part of the limbic system, which controls the autonomic nervous system and the endocrine systems. • One of the most important functions of the hypothalamus is to link the nervous system to the endocrine system via the pituitary gland (hypophysis). • Secretes releasing hormones to cause the pituitary to release hormones • Secretes inhibiting hormones to turn off secretion of pituitary hormones

Three Methods of Hypothalamic Control over the Endocrine System
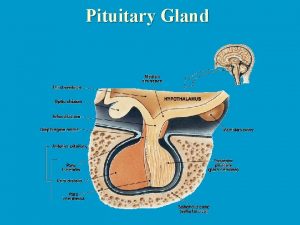
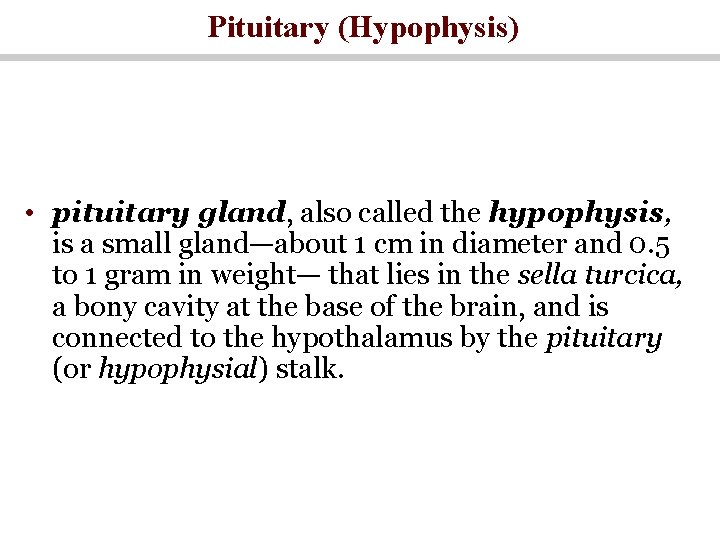
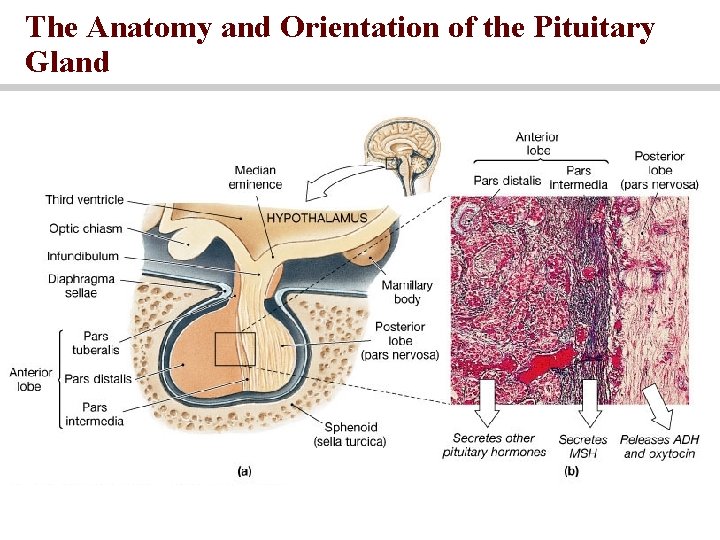
Pituitary (Hypophysis) • pituitary gland, also called the hypophysis, is a small gland—about 1 cm in diameter and 0. 5 to 1 gram in weight— that lies in the sella turcica, a bony cavity at the base of the brain, and is connected to the hypothalamus by the pituitary (or hypophysial) stalk.

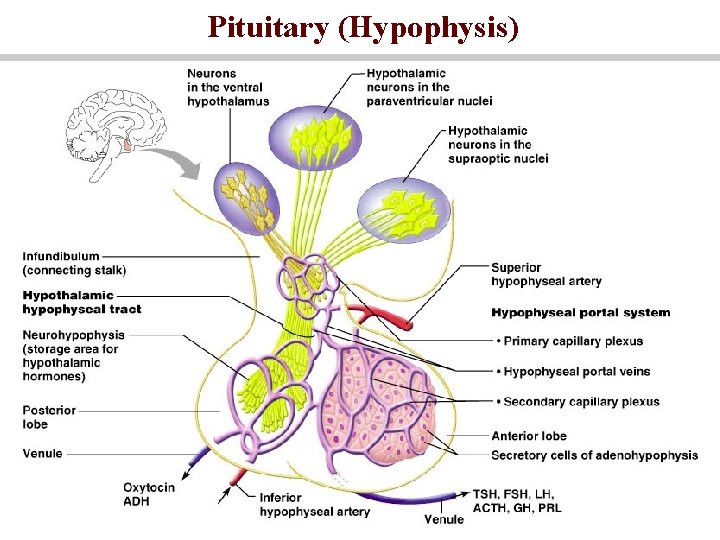
Pituitary (Hypophysis) • Neurohypophysis – posterior lobe (neural tissue) and the infundibulum • Receives, stores, and releases hormones from the hypothalamus • Adenohypophysis – anterior lobe, made up of glandular tissue • Synthesizes and secretes a number of hormones
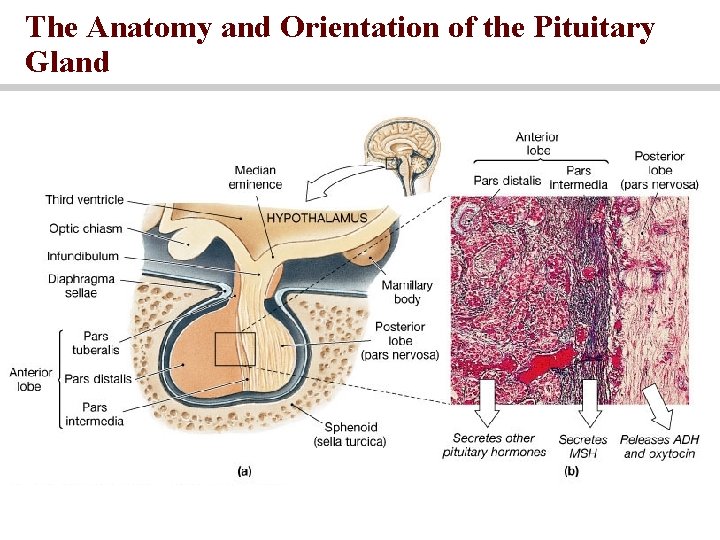
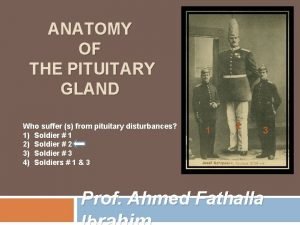
The Anatomy and Orientation of the Pituitary Gland
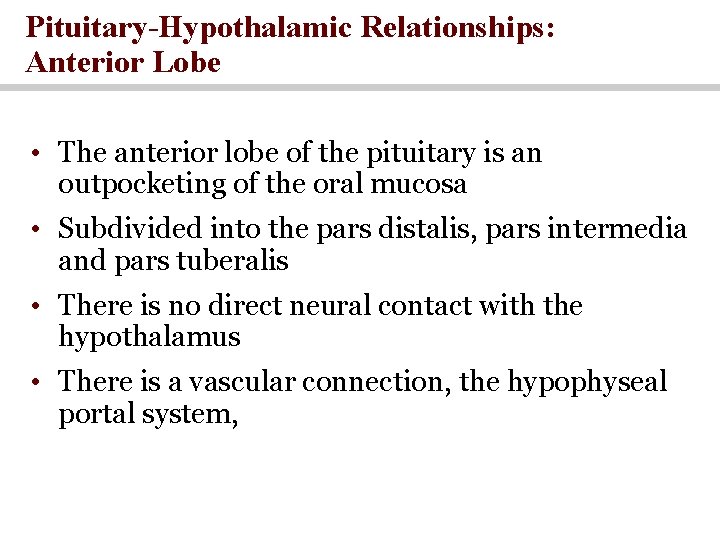
Pituitary-Hypothalamic Relationships: Anterior Lobe • The anterior lobe of the pituitary is an outpocketing of the oral mucosa • Subdivided into the pars distalis, pars intermedia and pars tuberalis • There is no direct neural contact with the hypothalamus • There is a vascular connection, the hypophyseal portal system,

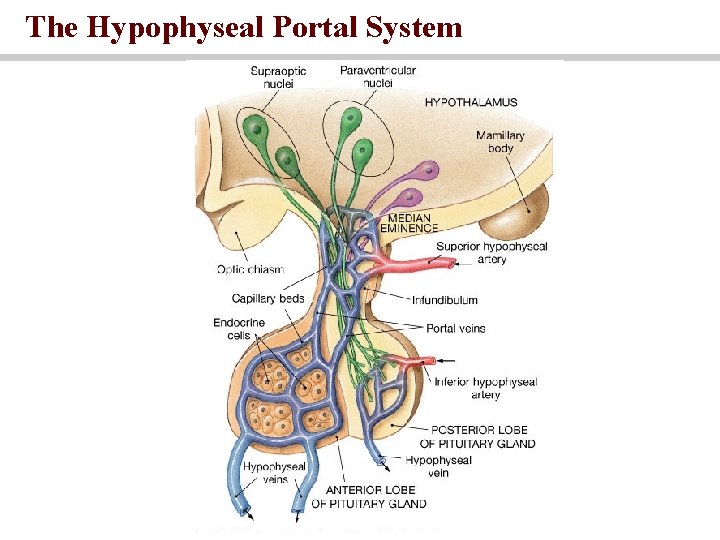
Hypophyseal portal system • At the median eminence, neurons release regulatory factors through fenestrated capillaries • Releasing hormones • Inhibiting hormones • All blood entering the portal system will reach the intended target cells before returning to the general circulation
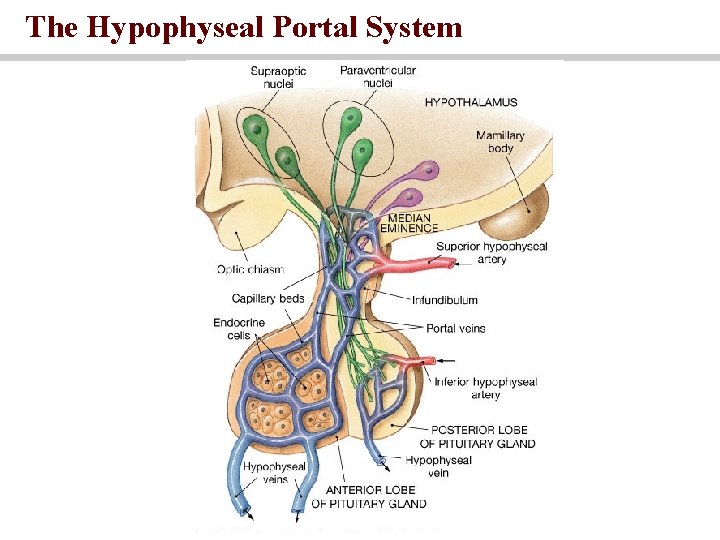
The Hypophyseal Portal System
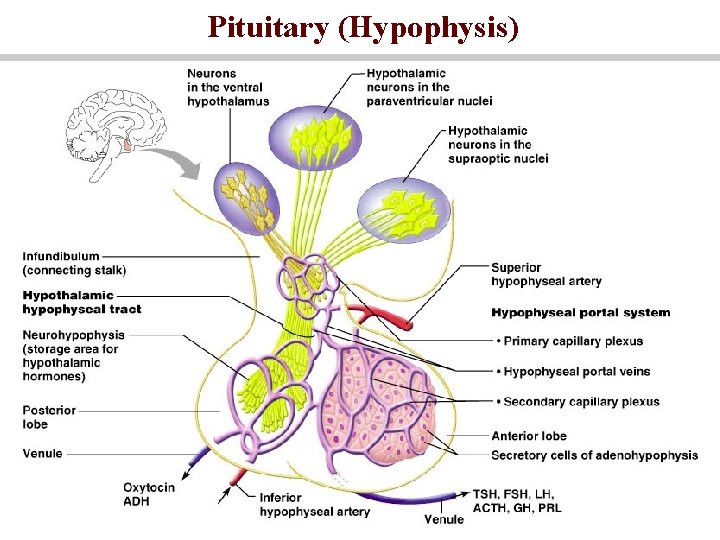
Pituitary (Hypophysis)
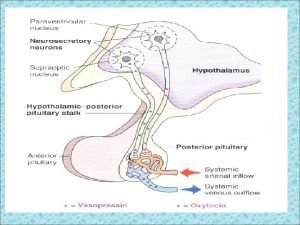
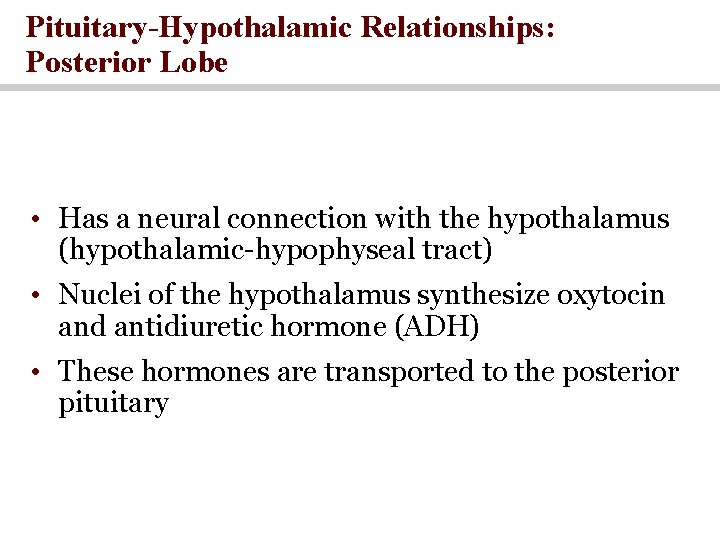
Pituitary-Hypothalamic Relationships: Posterior Lobe • Has a neural connection with the hypothalamus (hypothalamic-hypophyseal tract) • Nuclei of the hypothalamus synthesize oxytocin and antidiuretic hormone (ADH) • These hormones are transported to the posterior pituitary

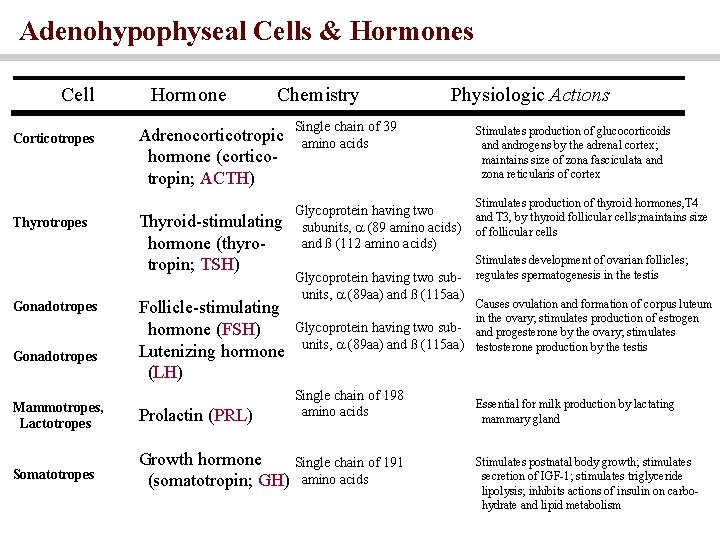
Adenophypophyseal Hormones • The six hormones of the adenohypophysis: • Are abbreviated as GH, TSH, ACTH, FSH, LH, and PRL • Regulate the activity of other endocrine glands • In addition, pro-opiomelanocortin (POMC): • Has been isolated from the pituitary • Is enzymatically split into ACTH, opiates, and MSH
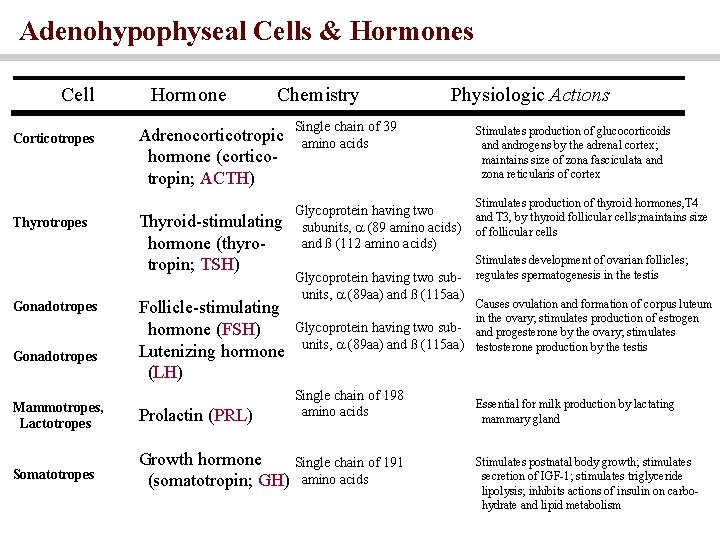
Adenohypophyseal Cells & Hormones Cell Corticotropes Thyrotropes Gonadotropes Hormone Chemistry Adrenocorticotropic hormone (corticotropin; ACTH) Thyroid-stimulating hormone (thyrotropin; TSH) Follicle-stimulating hormone (FSH) Lutenizing hormone (LH) Physiologic Actions Single chain of 39 amino acids Glycoprotein having two subunits, (89 amino acids) and ß (112 amino acids) Glycoprotein having two subunits, (89 aa) and ß (115 aa) Stimulates production of glucocorticoids androgens by the adrenal cortex; maintains size of zona fasciculata and zona reticularis of cortex Stimulates production of thyroid hormones, T 4 and T 3, by thyroid follicular cells; maintains size of follicular cells Stimulates development of ovarian follicles; regulates spermatogenesis in the testis Causes ovulation and formation of corpus luteum in the ovary; stimulates production of estrogen Glycoprotein having two sub- and progesterone by the ovary; stimulates units, (89 aa) and ß (115 aa) testosterone production by the testis Single chain of 198 amino acids Mammotropes, Lactotropes Prolactin (PRL) Somatotropes Growth hormone Single chain of 191 (somatotropin; GH) amino acids Essential for milk production by lactating mammary gland Stimulates postnatal body growth; stimulates secretion of IGF-1; stimulates triglyceride lipolysis; inhibits actions of insulin on carbohydrate and lipid metabolism
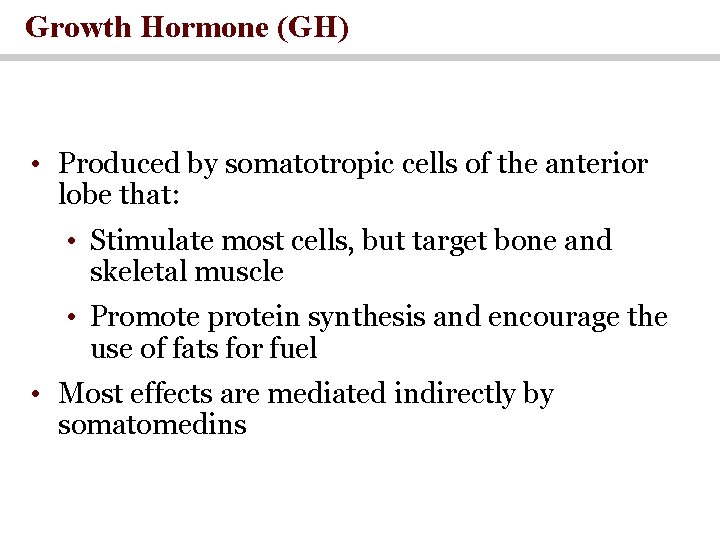
Growth Hormone (GH) • Produced by somatotropic cells of the anterior lobe that: • Stimulate most cells, but target bone and skeletal muscle • Promote protein synthesis and encourage the use of fats for fuel • Most effects are mediated indirectly by somatomedins
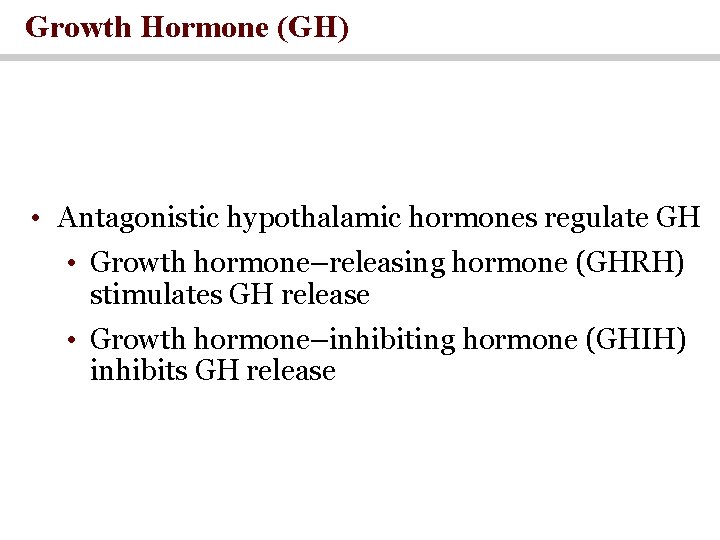
Growth Hormone (GH) • Antagonistic hypothalamic hormones regulate GH • Growth hormone–releasing hormone (GHRH) stimulates GH release • Growth hormone–inhibiting hormone (GHIH) inhibits GH release
Growth hormone promotes growth of many body cells • Promote increased size of the cells • Increased mitosis • Specific differentiation of certain types of cells such as bone growth cells and early muscle cells
Growth hormone has several metabolic effects 1 - Increased rate of proteins synthesis in most cells of the body 2 - Increased mobilization of fatty acids from adipose tissue, increased free fatty acid in the blood, and increased use of fatty acids for energy. 3 - Decreased rate of glucose utilization through the body
1 - Increased rate of proteins synthesis in most cells of the body (anabolic effect) GH promotes protein deposition in tissues : • enhancement of amino acid transport through the cell membrane • enhancement of RNA translation to cause protein synthesis by the ribosomes • Increased nuclear transcription of DNA to form RNA • Decreased catabolism of protein and amino acids
increased mobilization of fatty acids • release of fatty acids from adipose tissue • increasing the FFA in the body fluids • conversing of FFA to acetyl coemzyme A • fat is used for energy in preference to the use of carbohydrates and proteins. • >>> ++GH>> +++ acetoacetic formed by the liver>>> causing ketosis>>>fatty liver.
decreased rate of glucose utilization through the body (decrease carbohydrate utilization) • Decreased glucose uptake in tissues such as skeletal muscle and fat • Increased glucose production by the liver • increased insulin secretion (cause insulin resistance). • Excess secretion of growth hormone =metabolic disturbances very similar to patients with type II diabetes. (diabetogenic effect)
Necessity of insulin and carbohydrate for the growth promoting action of growth hormone • Animal +lacks of pancreas>>>>no growth hormone effect • Animal+ diet without carbohydrate >>>> no growth hormone effect • Carbohydrate and insulin>>production of energy • Insulin : transport of amino acids into cells and glucose transport stimulation
Growth hormone stimulates cartilage and bone Growth • Increased deposition of protein by the chondrocytic and osteogenic cells that cause bone growth • Increased rate of reproduction of these cells • Converting chondrocytes into osteogenic cells, that causing deposition of new bone

Factors Affecting GH Secretion Stimulation Glucose decrease Free fatty acid decrease Amino acid increase (arginine) Fasting Prolonged caloric deprivation Stress Exercise Puberty Androgens and estrogens Sleep Inhibition Somatostatin Glucose increase Free fatty acid increase Somatomedins Growth hormone Senescence
Metabolic vs. Growth actions of Growth Hormone • Growth actions of growth hormone are mediated by insulin-like growth factor 1 (IGF-1) • Metabolic actions are direct.

Metabolic Action of Growth Hormone
Thyroid Stimulating Hormone (Thyrotropin) • Tropic hormone that stimulates the normal development and secretory activity of the thyroid gland • Triggered by hypothalamic peptide thyrotropinreleasing hormone (TRH) • Rising blood levels of thyroid hormones act on the pituitary and hypothalamus to block the release of TSH
Adrenocorticotropic Hormone (Corticotropin) • Stimulates the adrenal cortex to release corticosteroids • Triggered by hypothalamic corticotropin-releasing hormone (CRH) in a daily rhythm • Internal and external factors such as fever, hypoglycemia, and stressors can trigger the release of CRH
Gonadotropins • Gonadotropins – follicle-stimulating hormone (FSH) and luteinizing hormone (LH) • Regulate the function of the ovaries and testes • FSH stimulates gamete (egg or sperm) production • Absent from the blood in prepubertal boys and girls • Triggered by the hypothalamic gonadotropinreleasing hormone (Gn. RH) during and after puberty
Functions of Gonadotropins • In females • LH works with FSH to cause maturation of the ovarian follicle • LH works alone to trigger ovulation (expulsion of the egg from the follicle) • LH promotes synthesis and release of estrogens and progesterone
Functions of Gonadotropins • In males • LH stimulates interstitial cells of the testes (Leydig cells) to produce testosterone

Prolactin (PRL) • In females, stimulates milk production by the breasts • Inhibited by prolactin-inhibiting hormone (PIH) (dopamine) • Blood levels rise toward the end of pregnancy • Suckling stimulates PRH release and encourages continued milk production
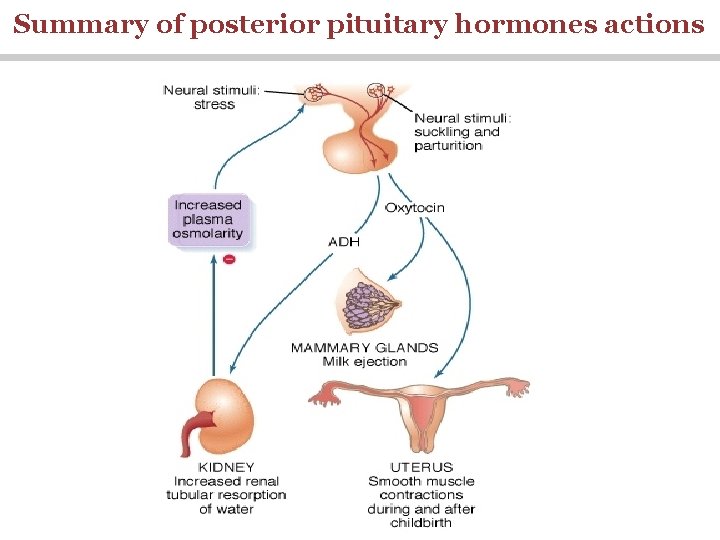
The Posterior Pituitary and Hypothalamic Hormones • The posterior lobe is a downgrowth of hypothalamic neural tissue • Has a neural connection with the hypothalamus (hypothalamichypophyseal tract) • Nuclei of the hypothalamus synthesize oxytocin and antidiuretic hormone (ADH) • These hormones are transported to the posterior pituitary

Pituitary (Hypophysis)
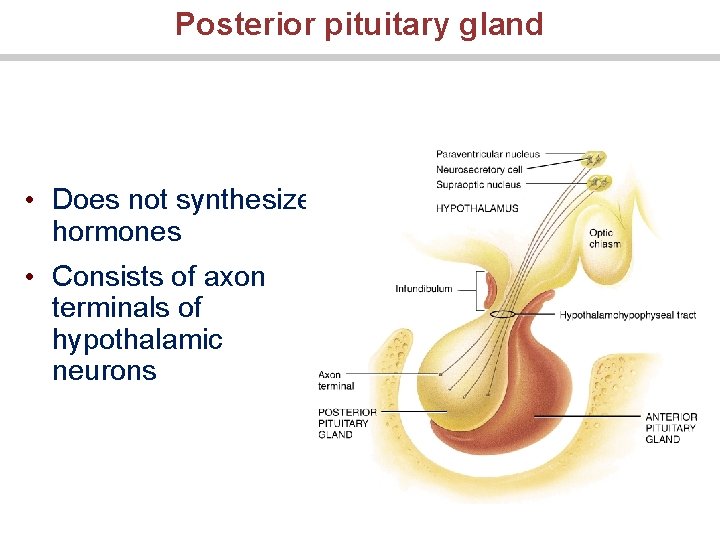
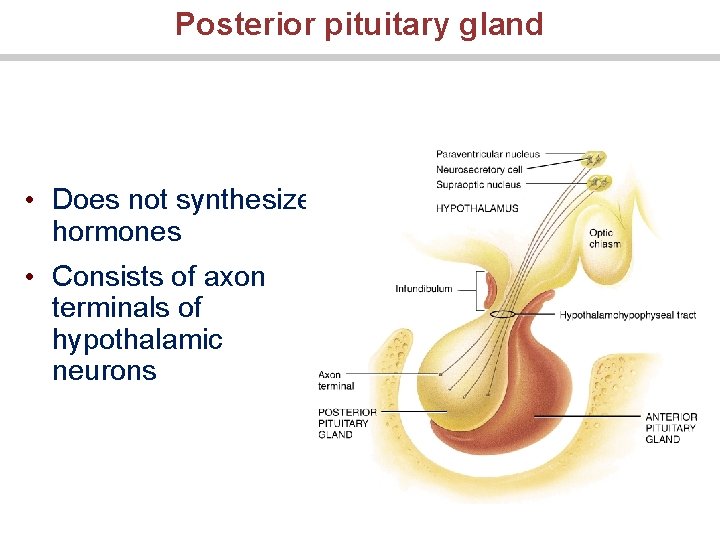
Posterior pituitary gland • Does not synthesize hormones • Consists of axon terminals of hypothalamic neurons
Antidiuretic Hormone (ADH) (vasopressin)
Synthesis of ADH • It is synthesized as pre-prohormone and processed into a nonapeptide • ADH synthesized in the cell bodies of hypothalamic neurons(supraoptic nucleus) • ADH is stored in the posterior pituitary
Receptors of ADH (vasopressin) • There are 2 types of receptors for ADH: • V 1 • V 2 V 1 receptors mediate vasoconstriction V 2 receptors are located in the principle cells in distal convoluted tubule and collecting ducts in the kidneys
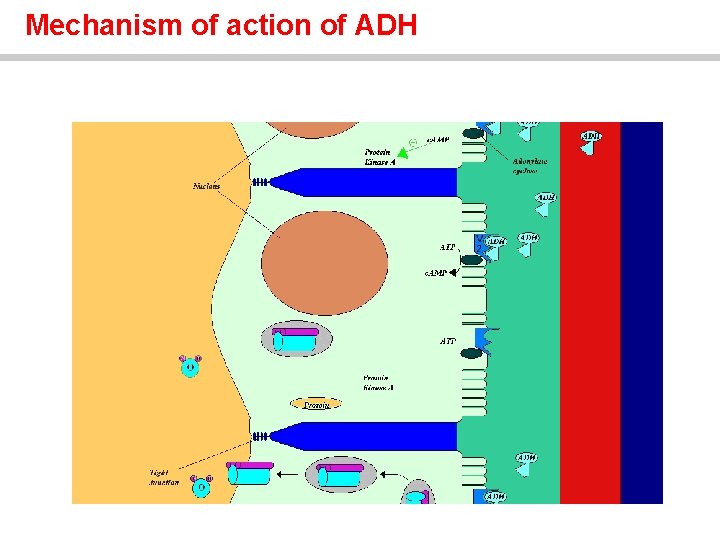
Mechanism of action of ADH: Antidiuresis • ADH binds to V 2 receptors on the principle cells of the distal convoluted tubules and collecting ducts. • Via adenylate cyclase/c. AMP induces production of specific proteins into the luminal membrane and enhances permeability of cell to water. • Increased membrane permeability to water permits back diffusion of free water, resulting in increased urine osmolality (concentrates urine).
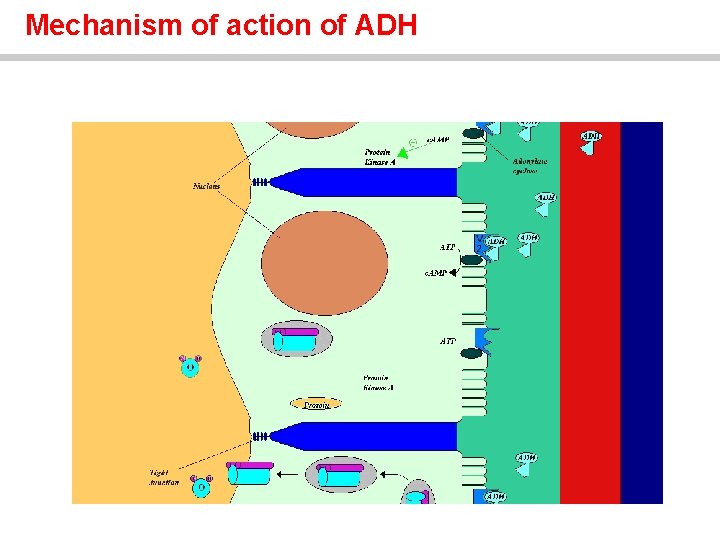
Mechanism of action of ADH
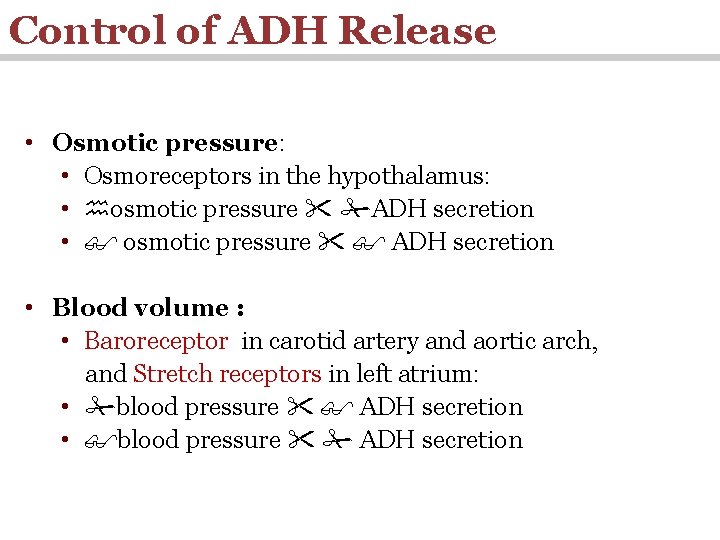
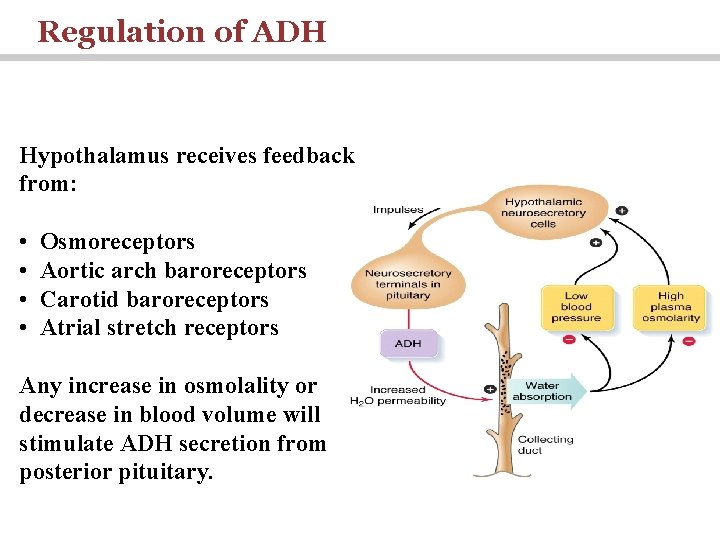
Control of ADH Release • Osmotic pressure: • Osmoreceptors in the hypothalamus: • osmotic pressure ADH secretion • osmotic pressure ADH secretion • Blood volume : • Baroreceptor in carotid artery and aortic arch, and Stretch receptors in left atrium: • blood pressure ADH secretion
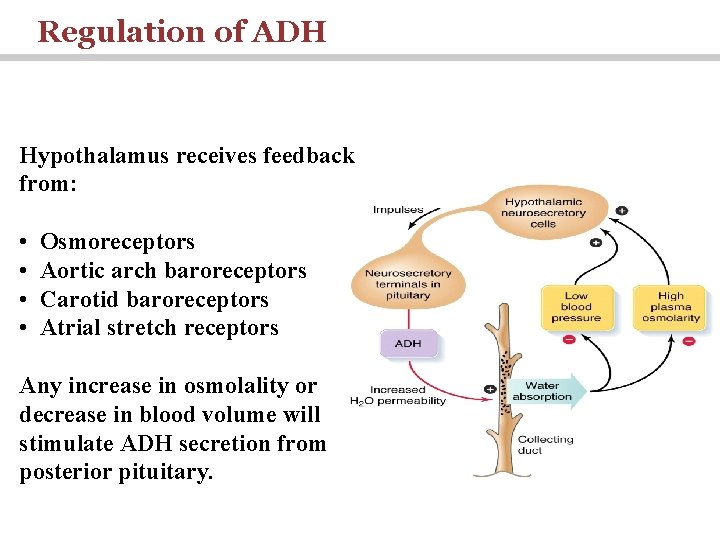
Regulation of ADH Hypothalamus receives feedback from: • • Osmoreceptors Aortic arch baroreceptors Carotid baroreceptors Atrial stretch receptors Any increase in osmolality or decrease in blood volume will stimulate ADH secretion from posterior pituitary.

ADH V 1 receptor Increased Blood Pressure
Oxytocin
Synthesis of Oxytocin • Oxytocin is synthesized in the cell bodies of hypothalamic neurons(paraventricular nucleus) • Oxytocin is stored in the posterior pituitary
Functions of oxytocin • Oxytocin is a strong stimulant of uterine contraction • Regulated by a positive feedback mechanism • This leads to increased intensity of uterine contractions, ending in birth • Oxytocin triggers milk ejection (“letdown” reflex) Contracts the myoepithelial cells of the alveoli
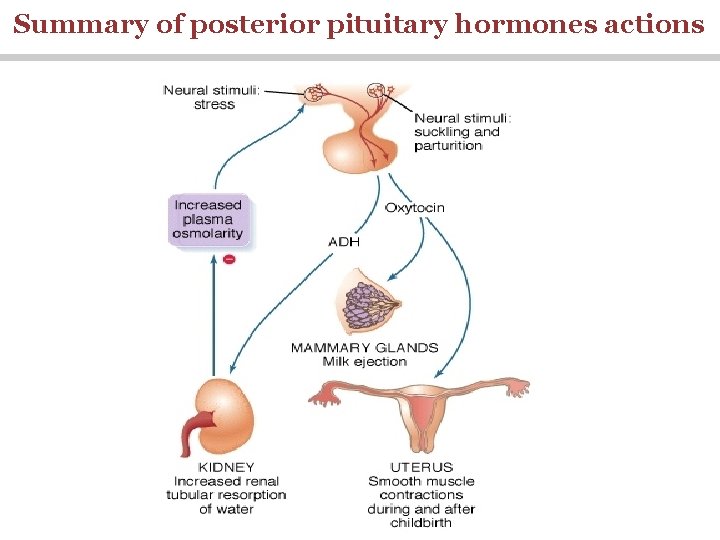
Summary of posterior pituitary hormones actions

ADH Disorders • Diabetes Insipidus: Neurogenic (central): (failure of neurohypophysis to synthesize or secrete ADH) Nephrogenic: (failure of the kidney to respond appropriately to ADH) 47
ADH Disorders • SIADH: • The syndrome of inappropriate antidiuretic hormone (ADH) secretion (SIADH) is defined by the hyponatremia and hypo-osmolality resulting from inappropriate, continued secretion or action of the hormone despite normal or increased plasma volume, which results in impaired water excretion. 48
 Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Pineal gland pituitary gland
Pineal gland pituitary gland Hashitoxicosis
Hashitoxicosis Dwrfism
Dwrfism Division of pituitary gland
Division of pituitary gland Hyposecretion of prolactin
Hyposecretion of prolactin Posterior abdominal wall nerves
Posterior abdominal wall nerves Dictalie
Dictalie Endocrine weight loss
Endocrine weight loss Anterior pituitary
Anterior pituitary Anterior pituitary gland
Anterior pituitary gland Blood supply of pituitary gland
Blood supply of pituitary gland Pituitary gland anatomical relations
Pituitary gland anatomical relations Hypothalamus hormones
Hypothalamus hormones Pituitary gland
Pituitary gland Colloid anatomy
Colloid anatomy Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Embryonic origin of pituitary gland
Embryonic origin of pituitary gland Janos lobe
Janos lobe Oxytocin
Oxytocin Organ systems
Organ systems Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Gland
Gland Sketch of pituitary gland
Sketch of pituitary gland Hypersecretion of prolactin
Hypersecretion of prolactin Pituitary gland disorders
Pituitary gland disorders Pituitary gland nerve supply
Pituitary gland nerve supply Pituitary gland
Pituitary gland Pituitary gland hormones
Pituitary gland hormones Triple f gland for flight fright and fight is
Triple f gland for flight fright and fight is Hypophyseal fossa and pituitary gland
Hypophyseal fossa and pituitary gland Estrogen effect
Estrogen effect Physiology of thyroid gland
Physiology of thyroid gland Khalid karaoui
Khalid karaoui Sana khalid
Sana khalid Khalid nationality
Khalid nationality Khalid al habib
Khalid al habib Cipralex side effects
Cipralex side effects Khalid bazaid
Khalid bazaid Complete the tag question your name is ali khalid
Complete the tag question your name is ali khalid Welcome to the english class images
Welcome to the english class images Jurnal jamal
Jurnal jamal Quarter turn belt drive
Quarter turn belt drive Nauman khalid md
Nauman khalid md Arzoo khalid
Arzoo khalid Dr samra khalid
Dr samra khalid 911 in roman numerals
911 in roman numerals Khalid alsadhan
Khalid alsadhan Khalid al dossary
Khalid al dossary