The Digestive System Organ groups of digestion Alimentary

- Slides: 48
The Digestive System
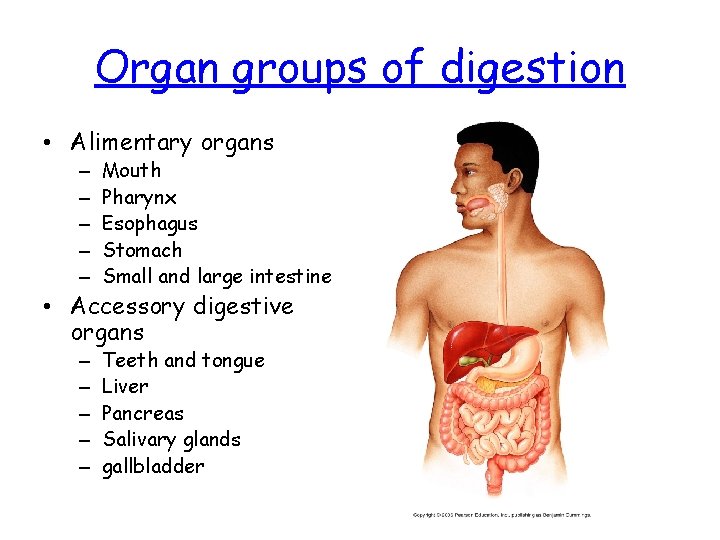
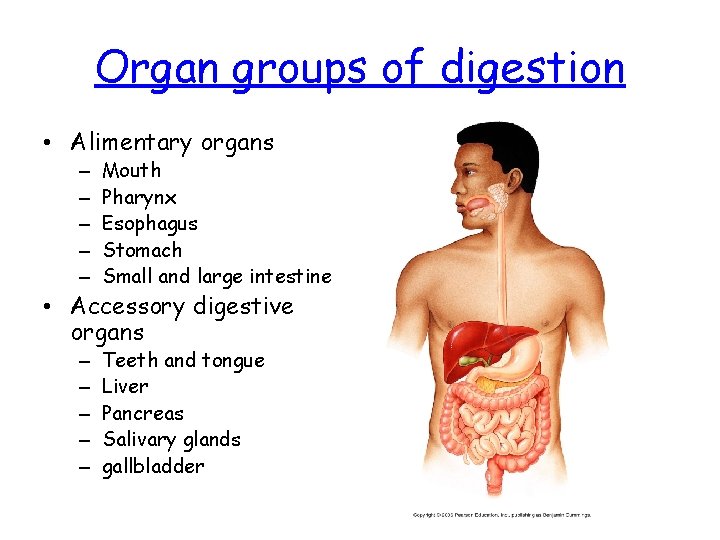
Organ groups of digestion • Alimentary organs – – – Mouth Pharynx Esophagus Stomach Small and large intestine • Accessory digestive organs – – – Teeth and tongue Liver Pancreas Salivary glands gallbladder
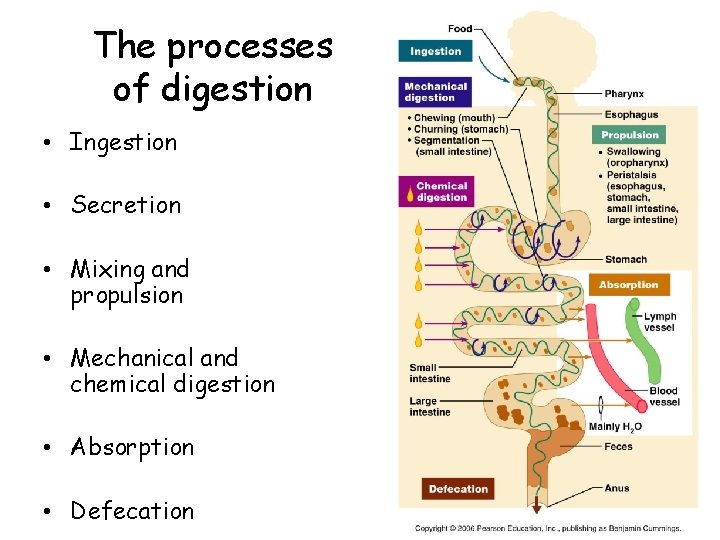
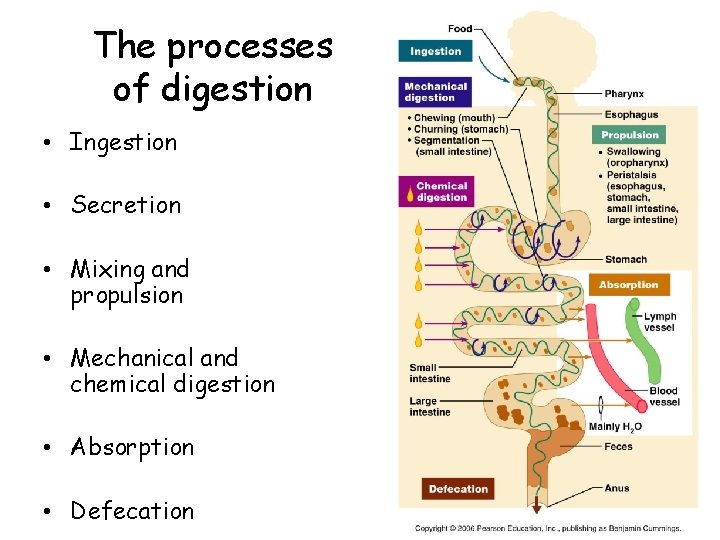
The processes of digestion • Ingestion • Secretion • Mixing and propulsion • Mechanical and chemical digestion • Absorption • Defecation
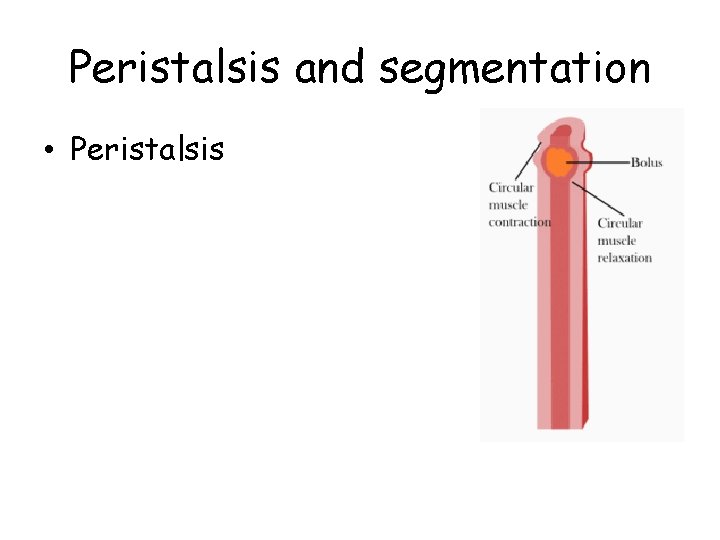
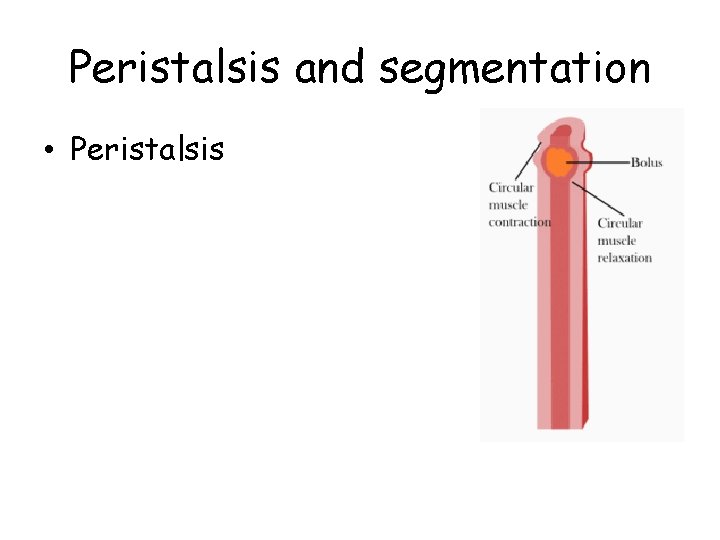
Peristalsis and segmentation • Peristalsis
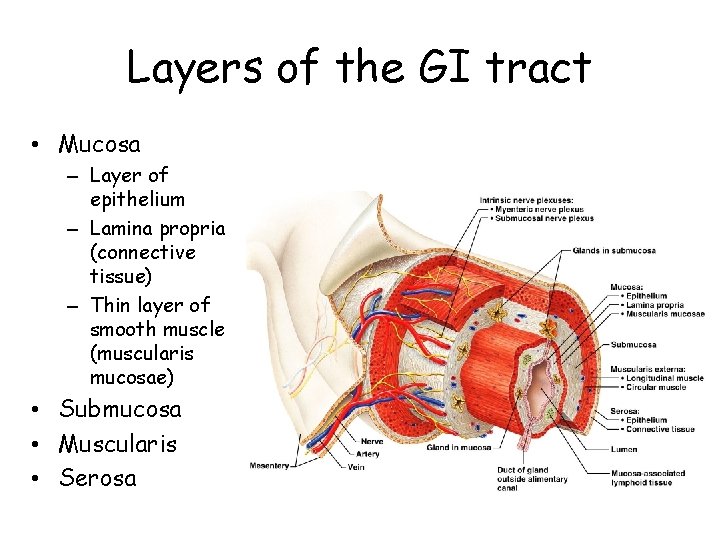
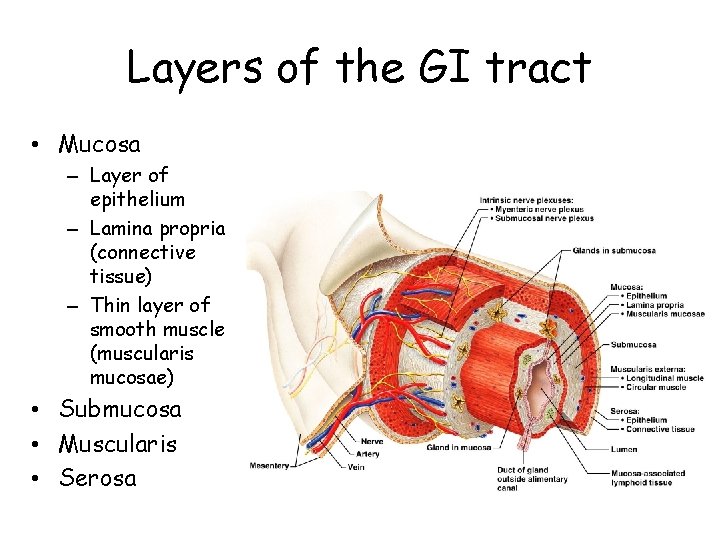
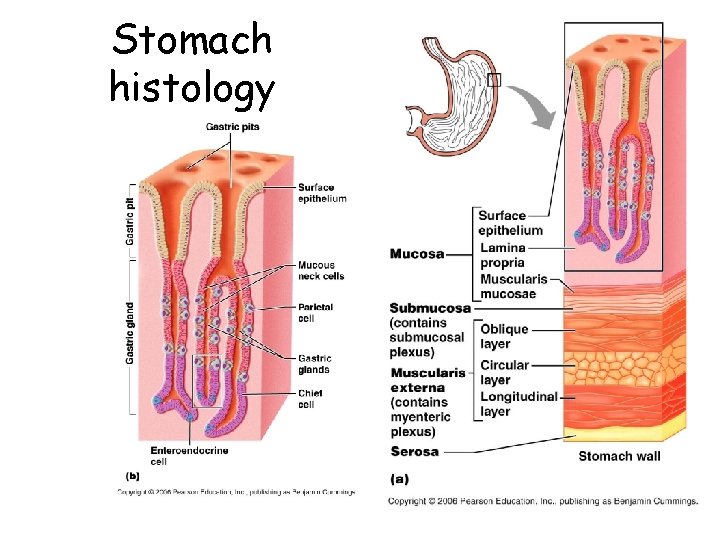
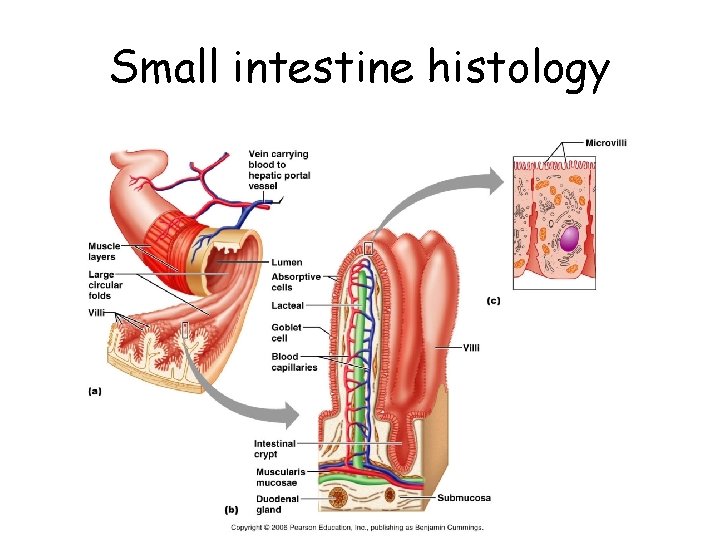
Layers of the GI tract • Mucosa – Layer of epithelium – Lamina propria (connective tissue) – Thin layer of smooth muscle (muscularis mucosae) • Submucosa • Muscularis • Serosa
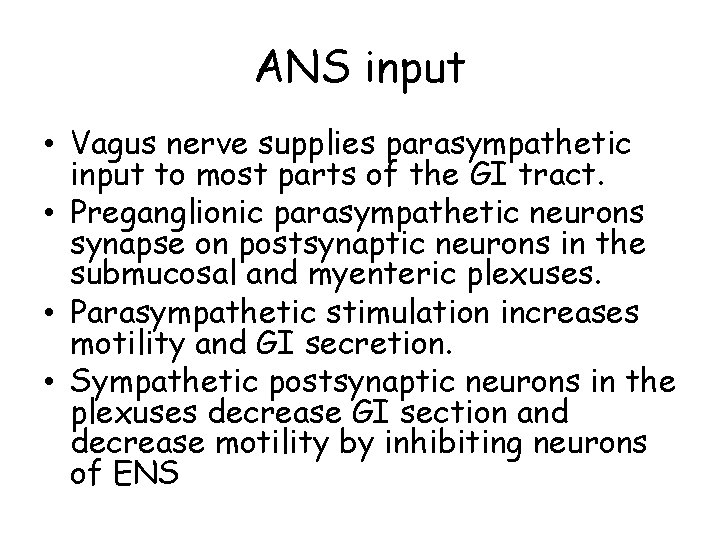
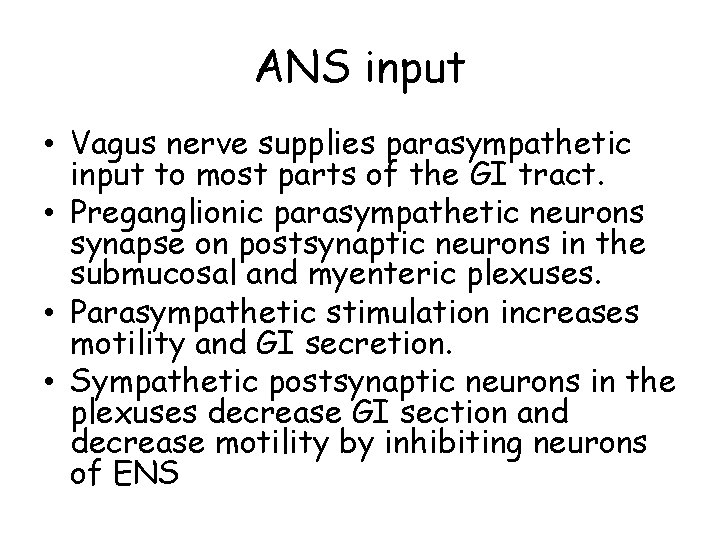
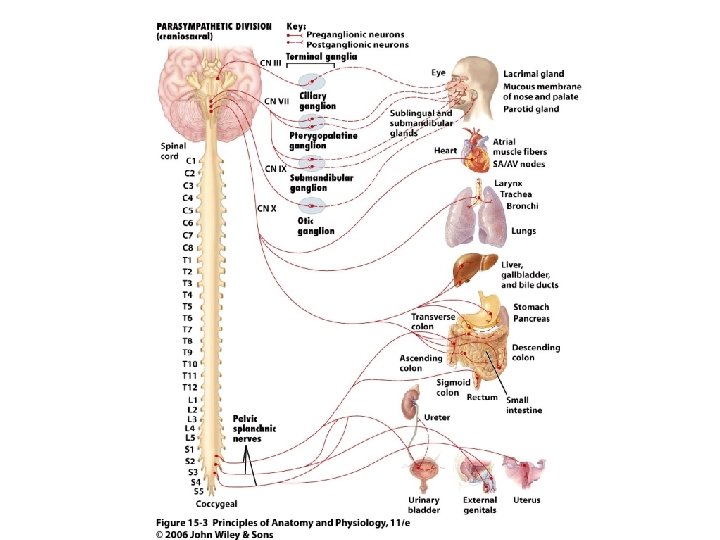
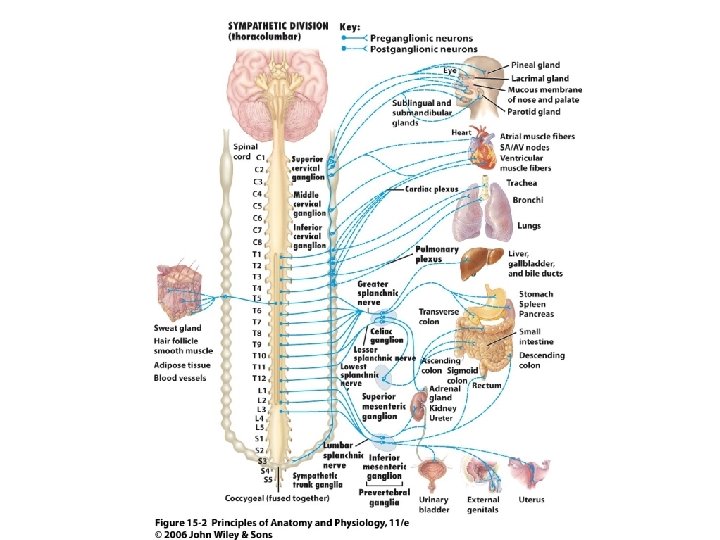
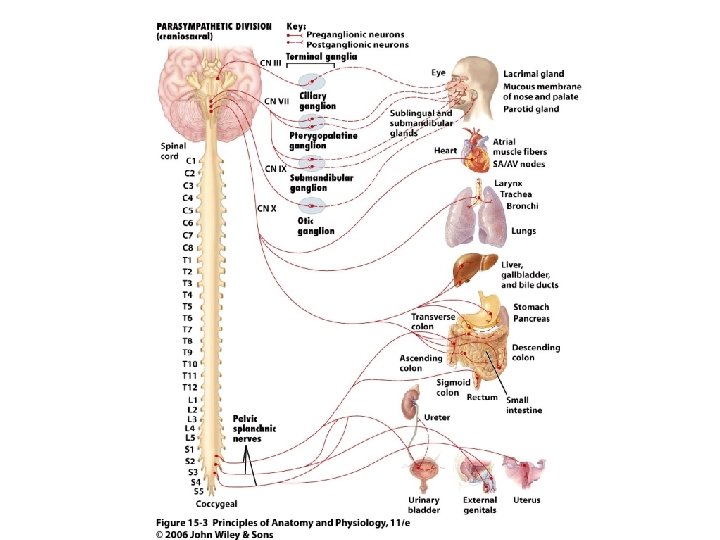
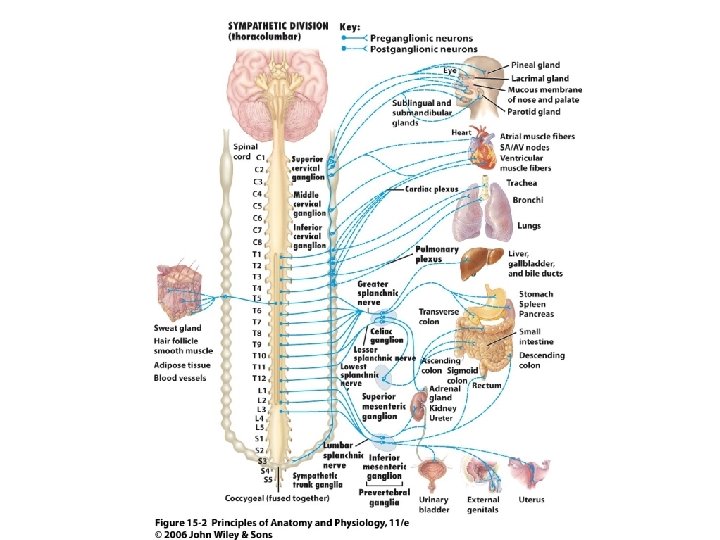
ANS input • Vagus nerve supplies parasympathetic input to most parts of the GI tract. • Preganglionic parasympathetic neurons synapse on postsynaptic neurons in the submucosal and myenteric plexuses. • Parasympathetic stimulation increases motility and GI secretion. • Sympathetic postsynaptic neurons in the plexuses decrease GI section and decrease motility by inhibiting neurons of ENS
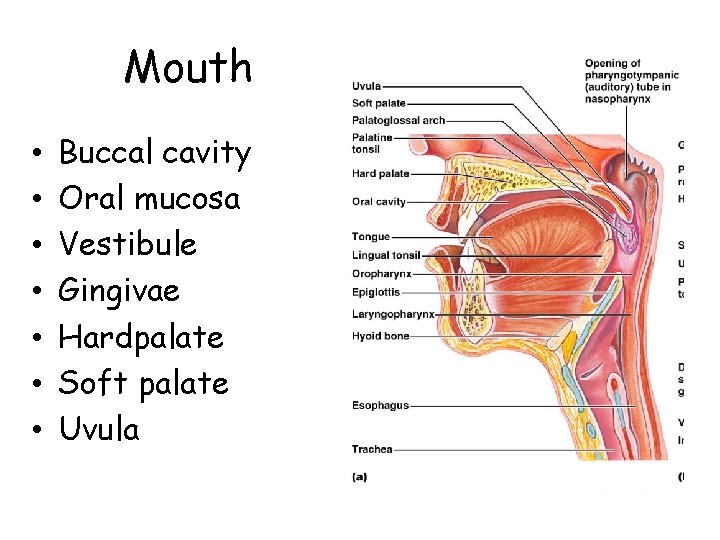
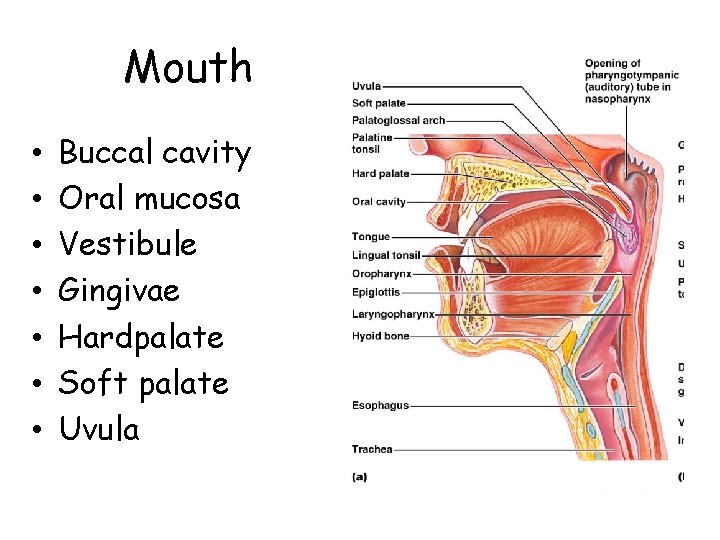
Mouth • • Buccal cavity Oral mucosa Vestibule Gingivae Hardpalate Soft palate Uvula
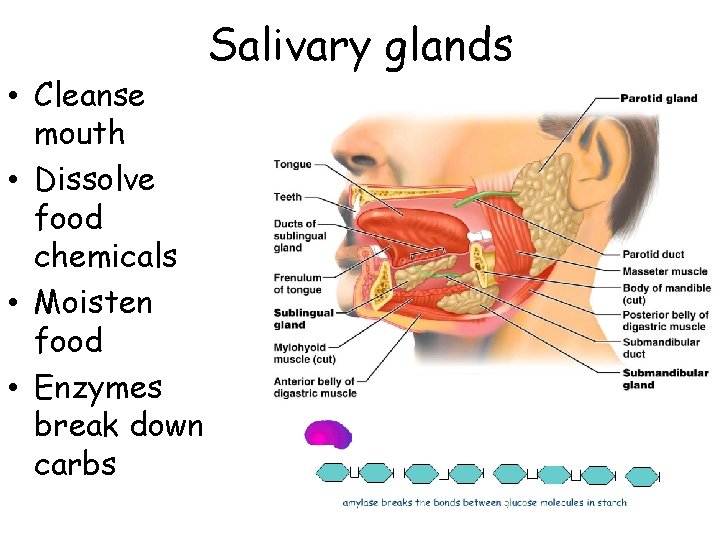
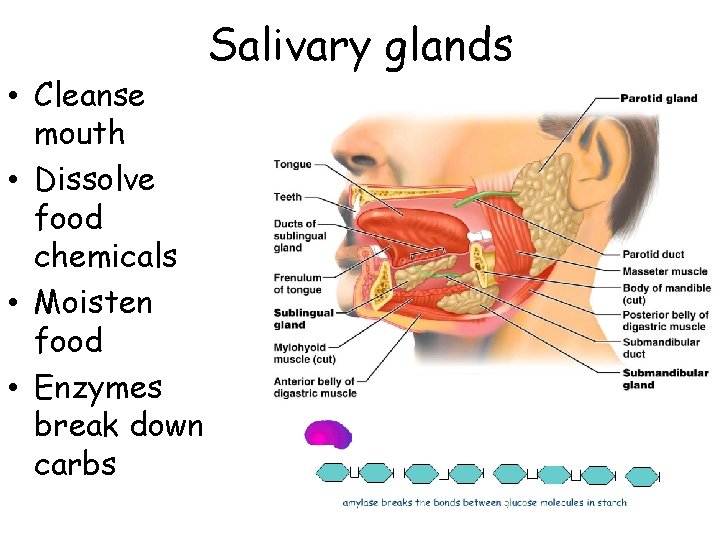
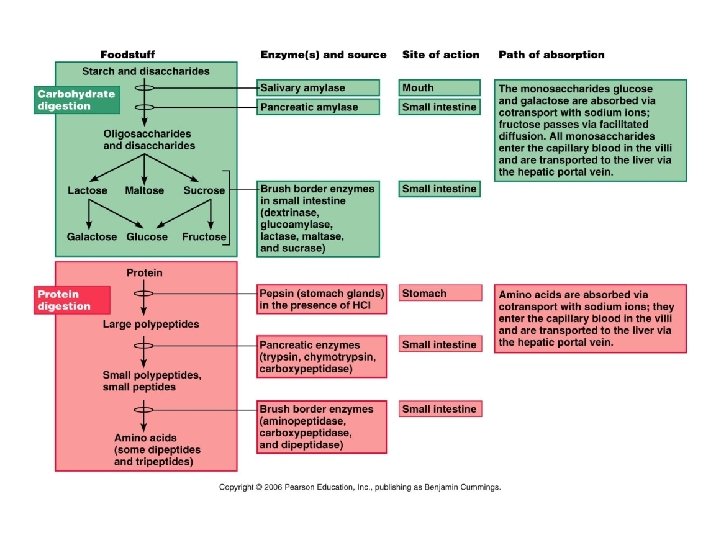
• Cleanse mouth • Dissolve food chemicals • Moisten food • Enzymes break down carbs Salivary glands
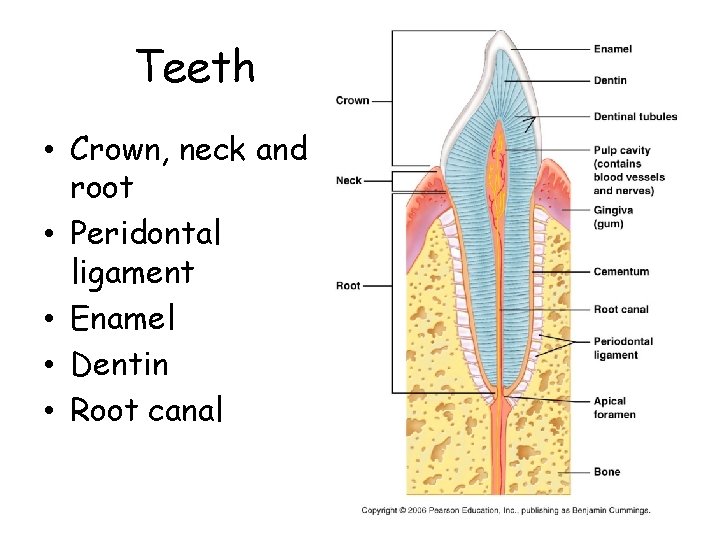
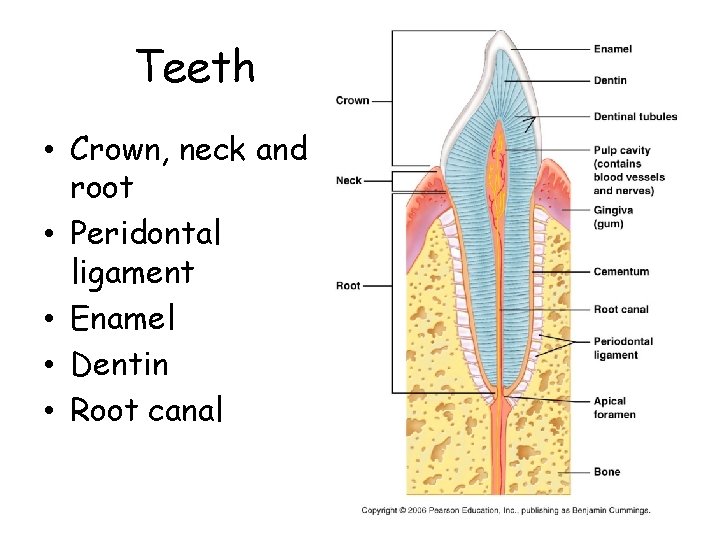
Teeth • Crown, neck and root • Peridontal ligament • Enamel • Dentin • Root canal
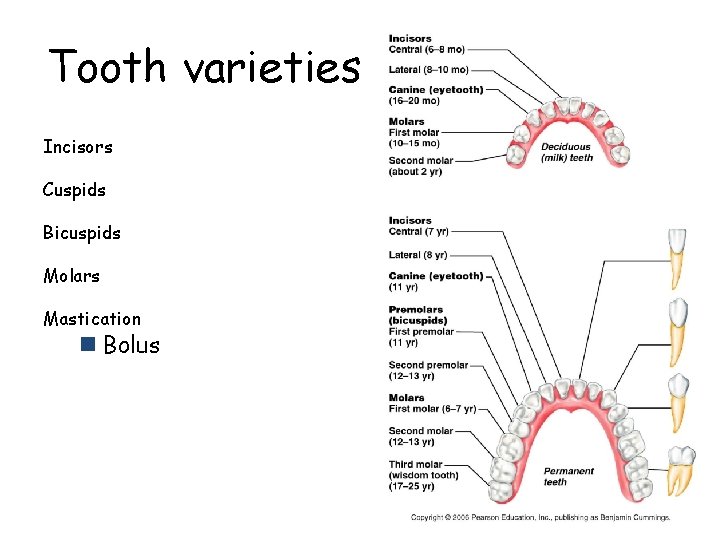
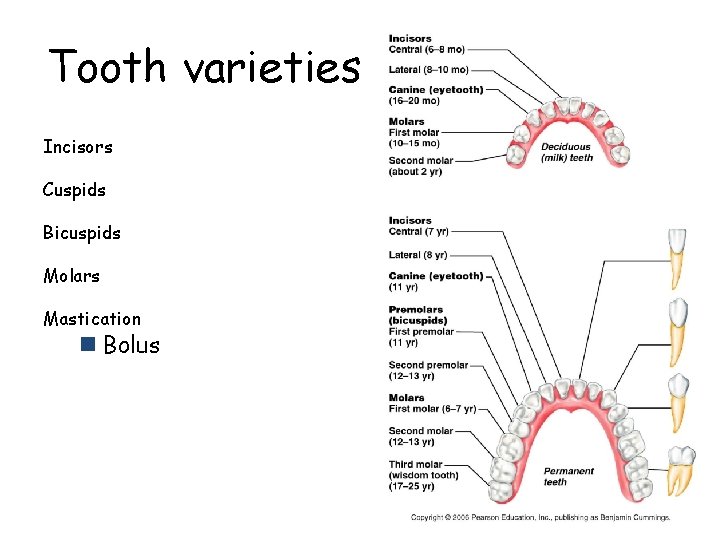
Tooth varieties Incisors Cuspids Bicuspids Molars Mastication n Bolus
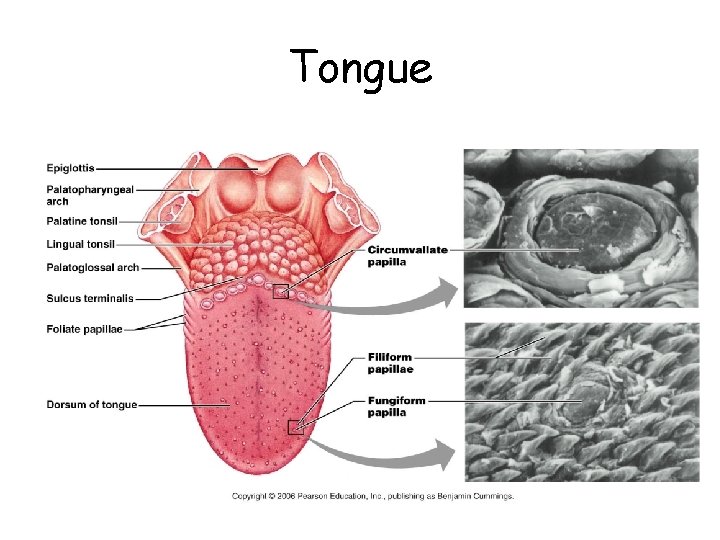
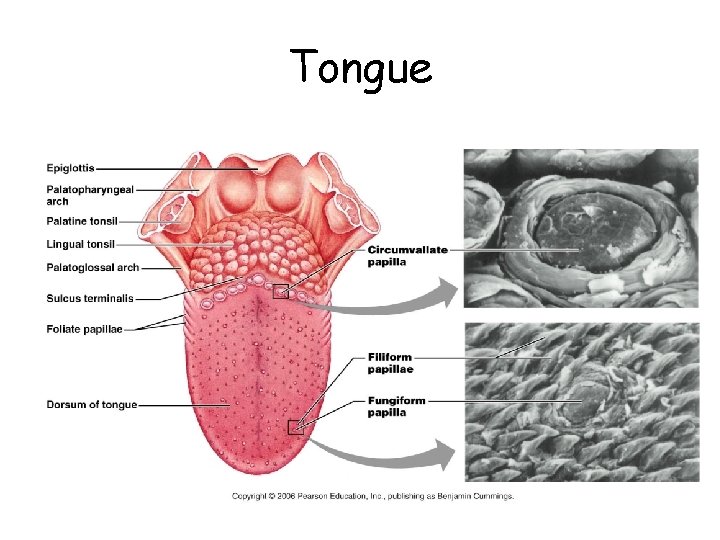
Tongue
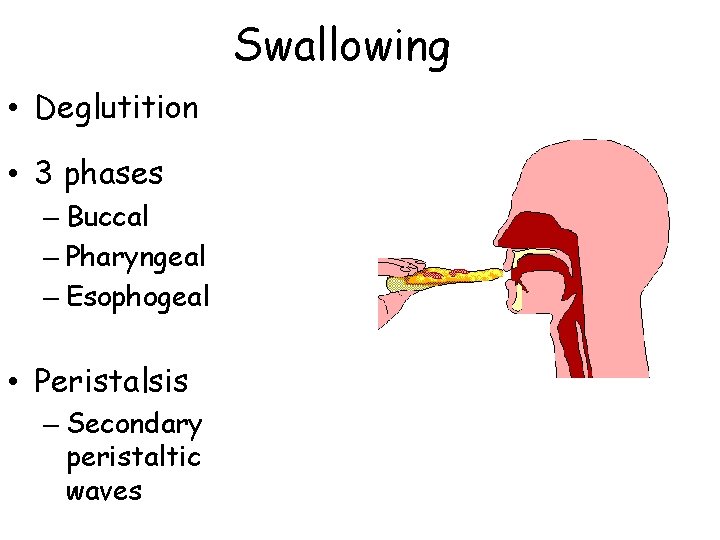
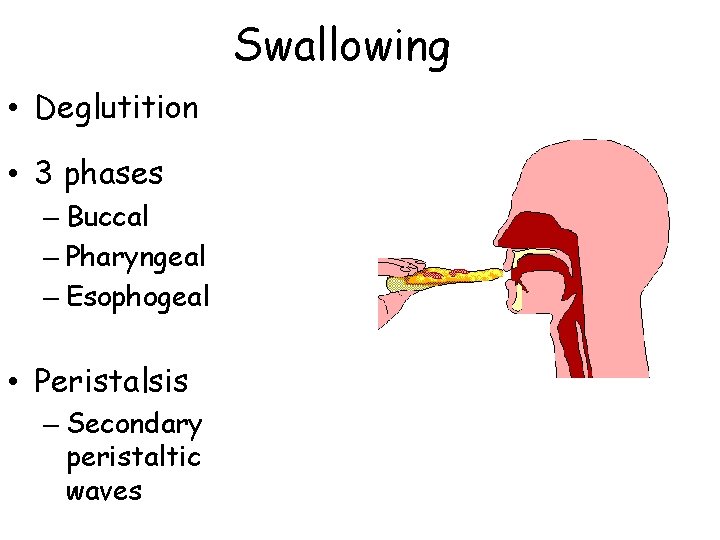
Swallowing • Deglutition • 3 phases – Buccal – Pharyngeal – Esophogeal • Peristalsis – Secondary peristaltic waves
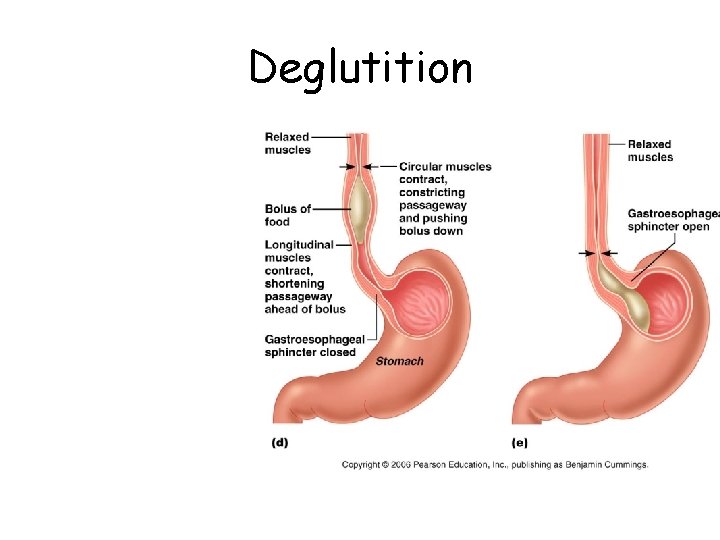
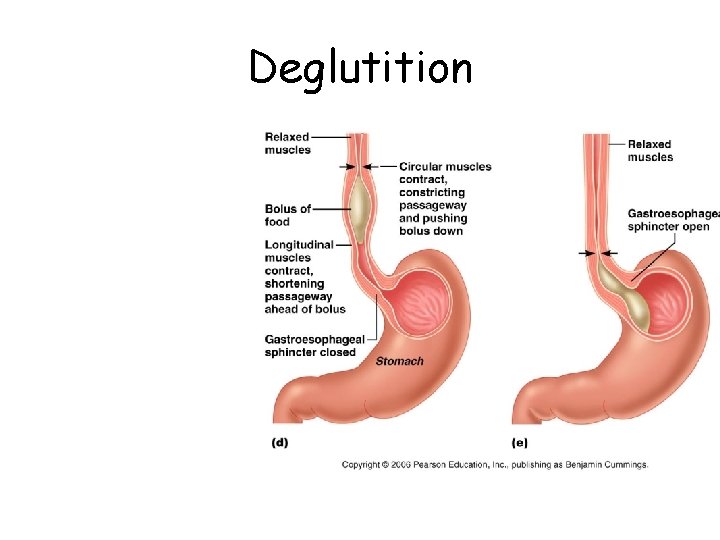
Deglutition
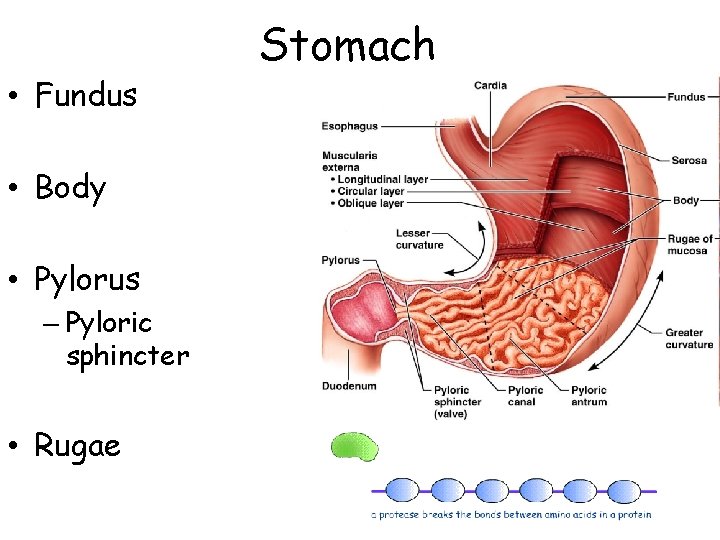
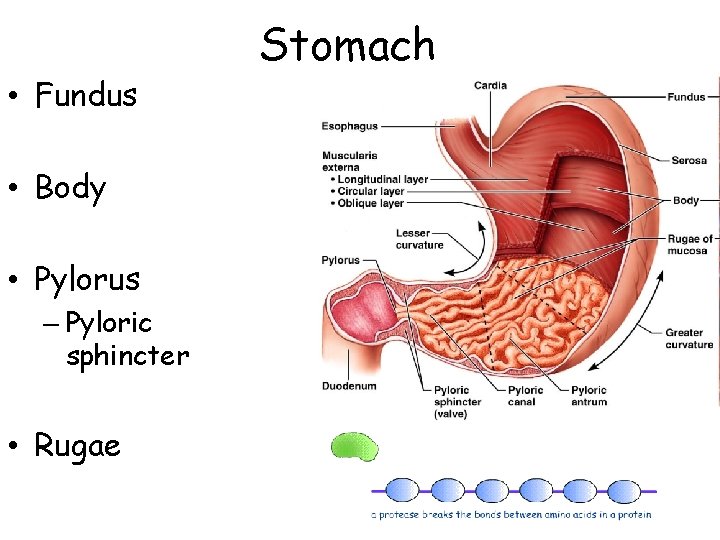
• Fundus • Body • Pylorus – Pyloric sphincter • Rugae Stomach
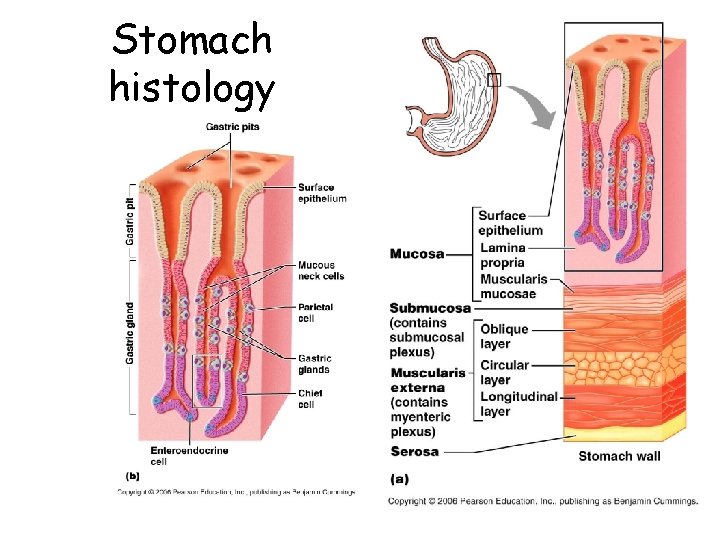
Stomach histology
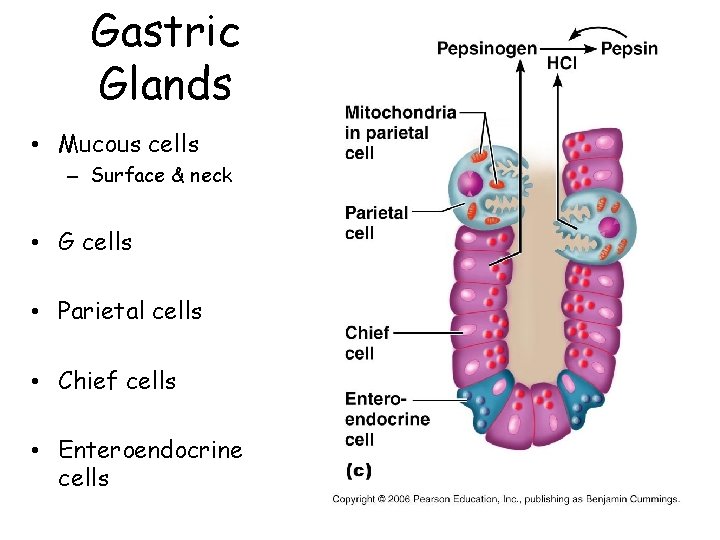
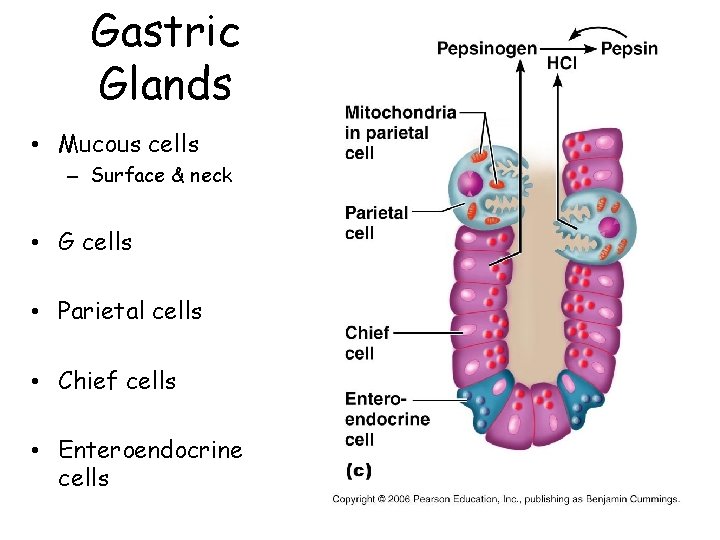
Gastric Glands • Mucous cells – Surface & neck • G cells • Parietal cells • Chief cells • Enteroendocrine cells
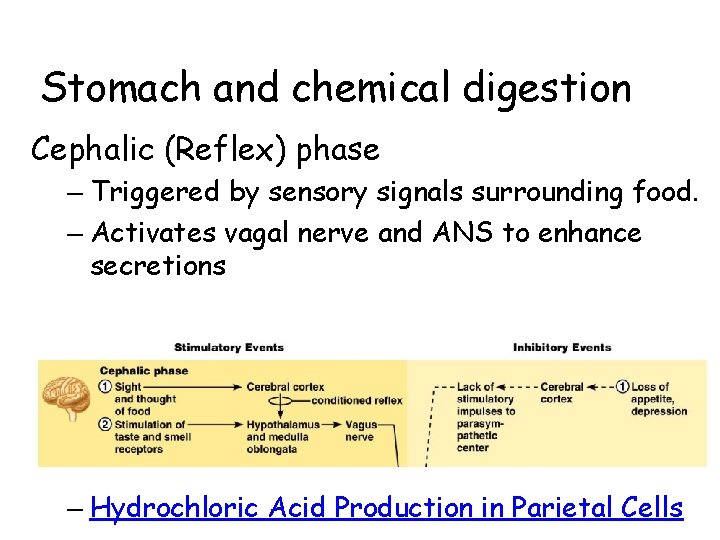
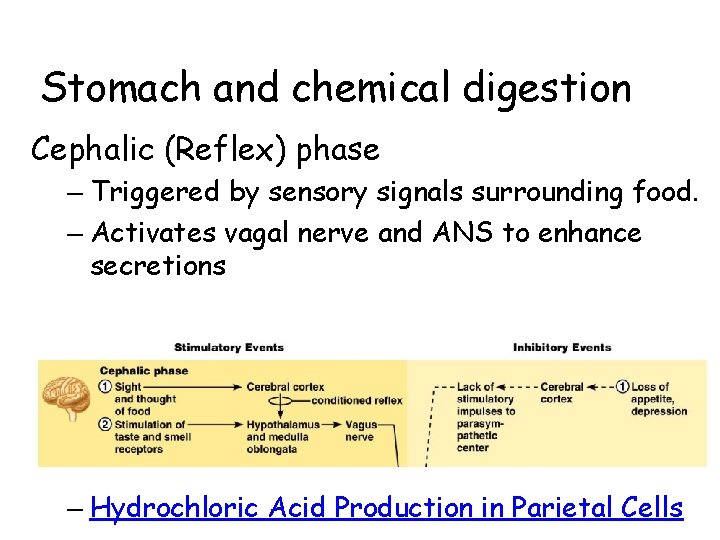
Stomach and chemical digestion Cephalic (Reflex) phase – Triggered by sensory signals surrounding food. – Activates vagal nerve and ANS to enhance secretions – Hydrochloric Acid Production in Parietal Cells
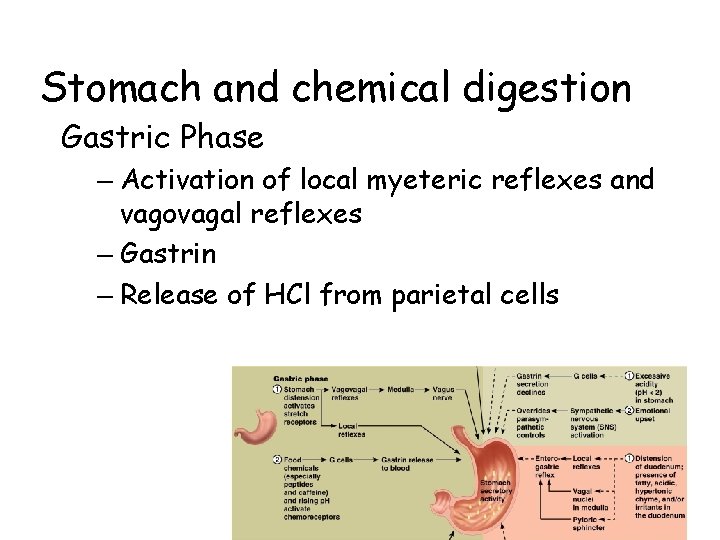
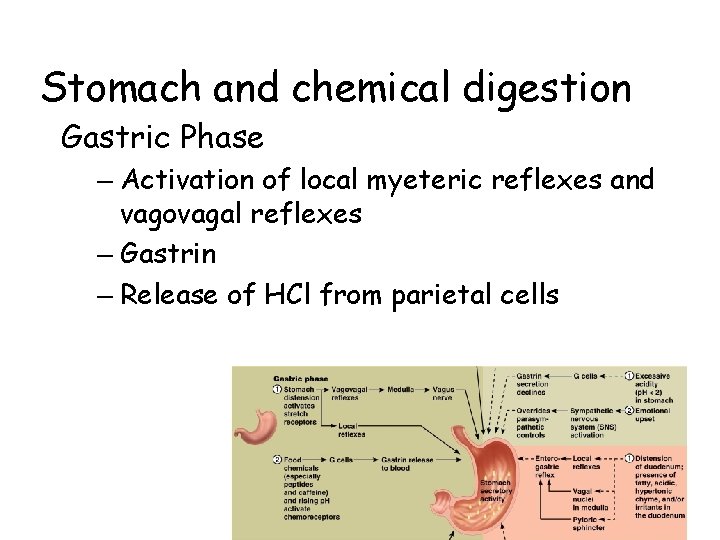
Stomach and chemical digestion Gastric Phase – Activation of local myeteric reflexes and vagovagal reflexes – Gastrin – Release of HCl from parietal cells
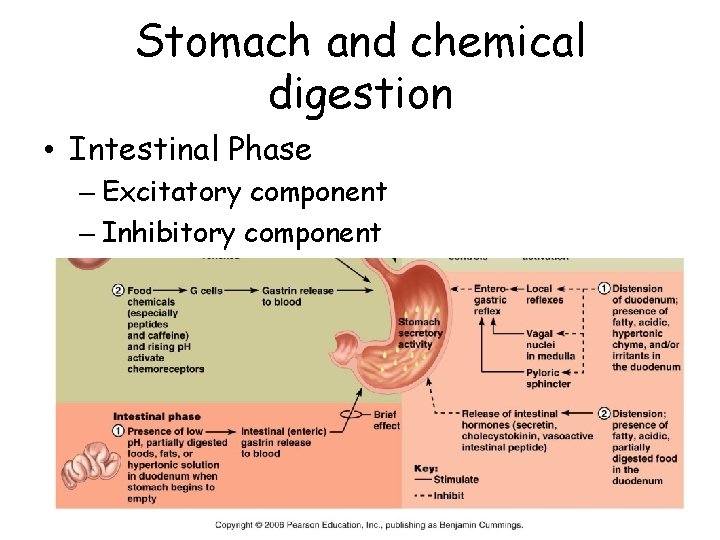
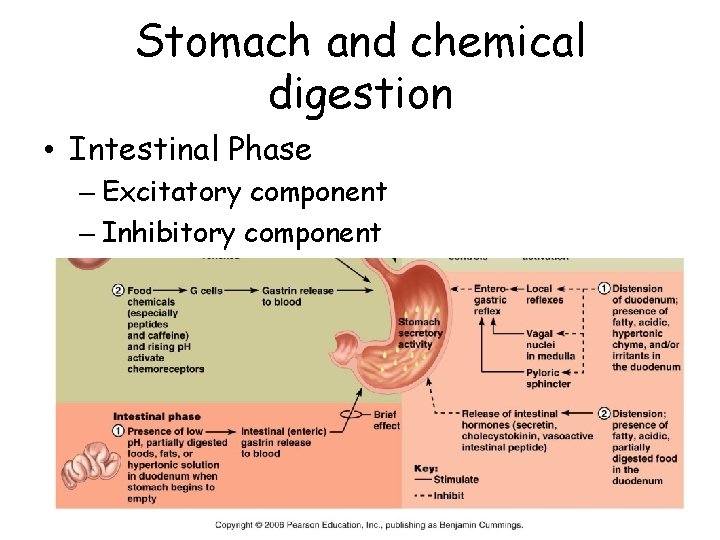
Stomach and chemical digestion • Intestinal Phase – Excitatory component – Inhibitory component
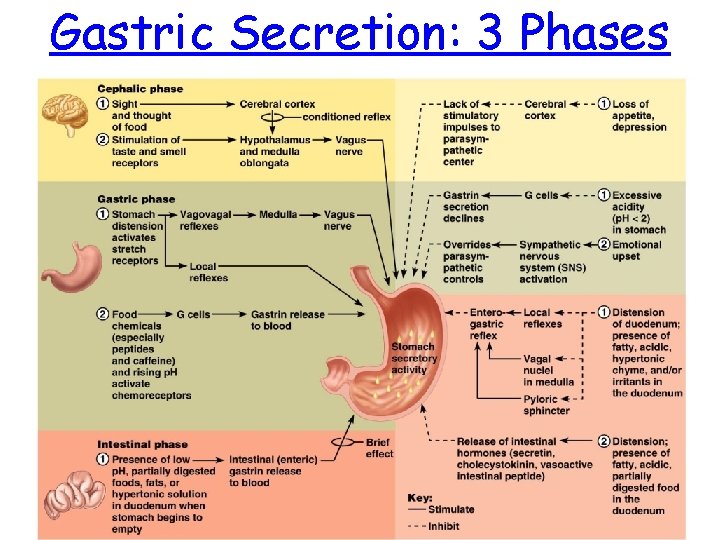
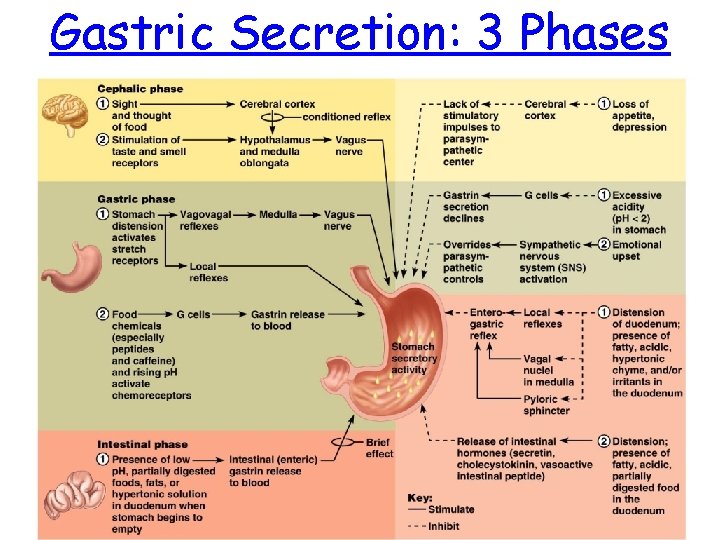
Gastric Secretion: 3 Phases
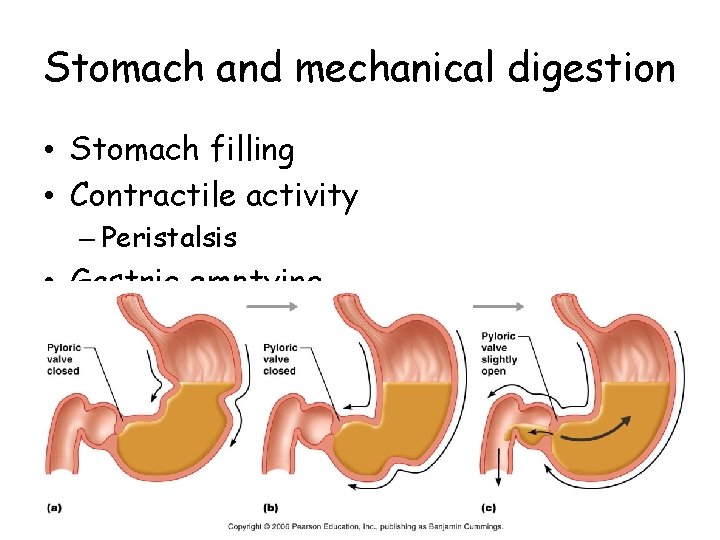
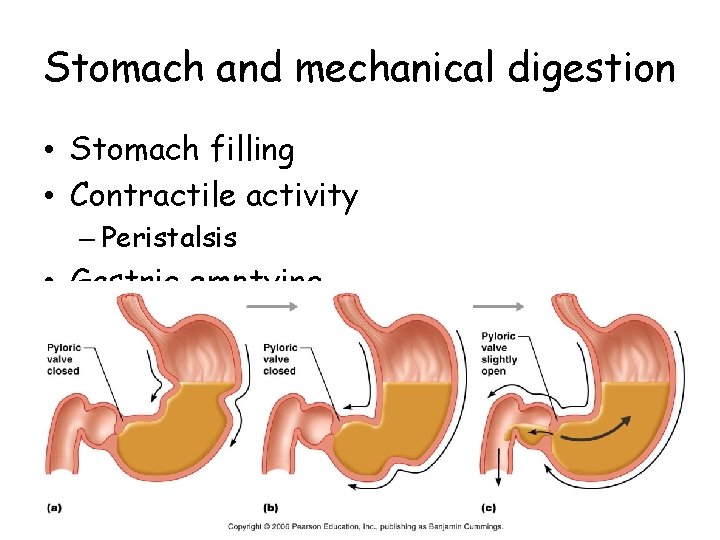
Stomach and mechanical digestion • Stomach filling • Contractile activity – Peristalsis • Gastric emptying
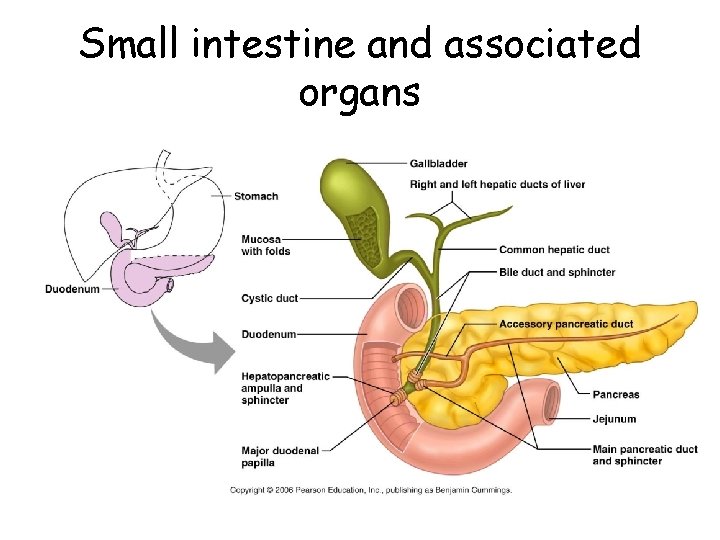
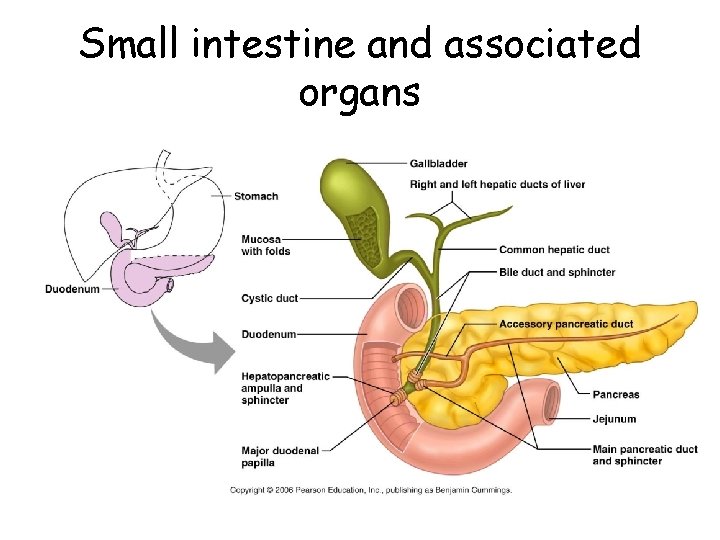
Small intestine and associated organs
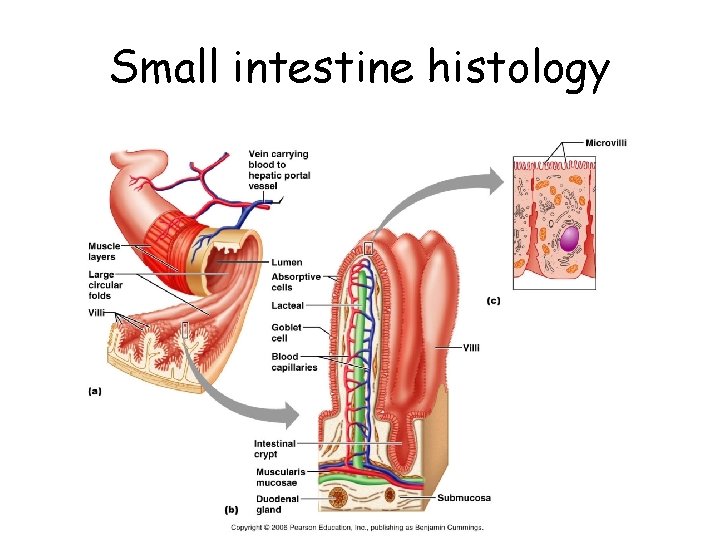
Small intestine histology
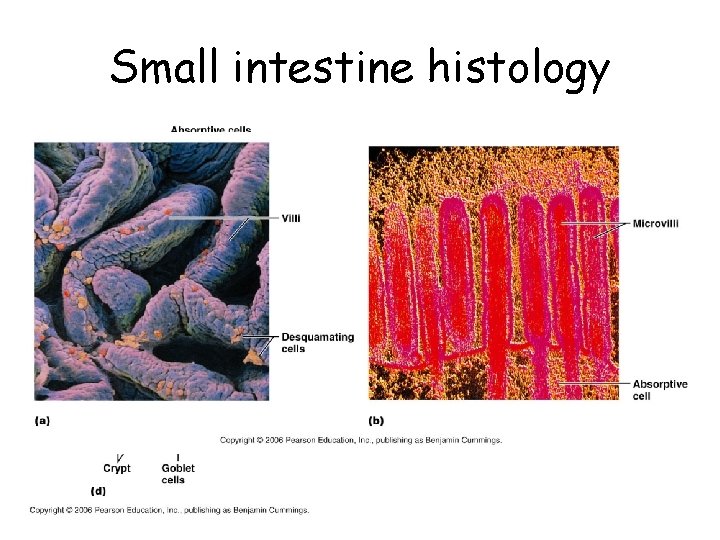
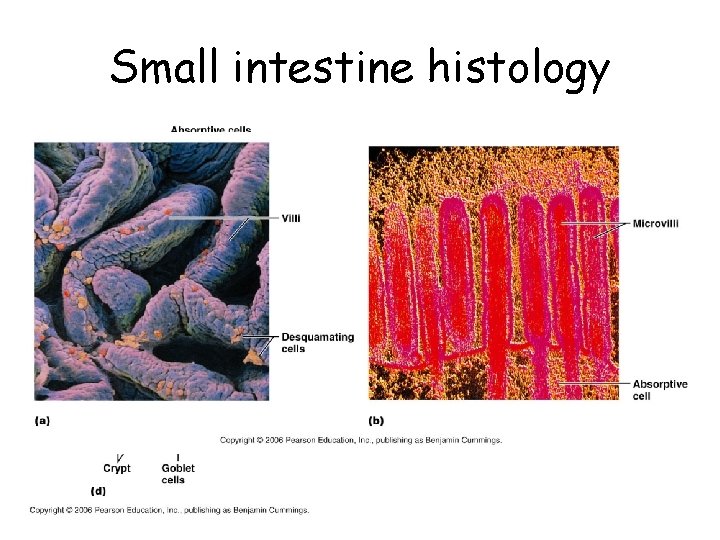
Small intestine histology
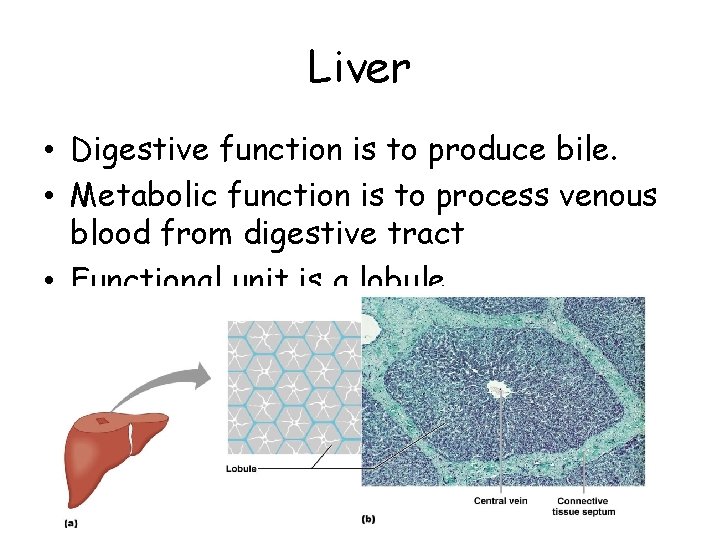
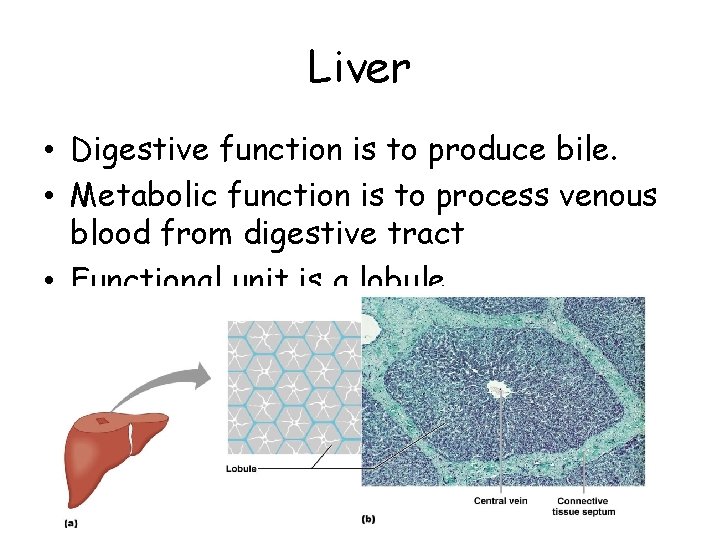
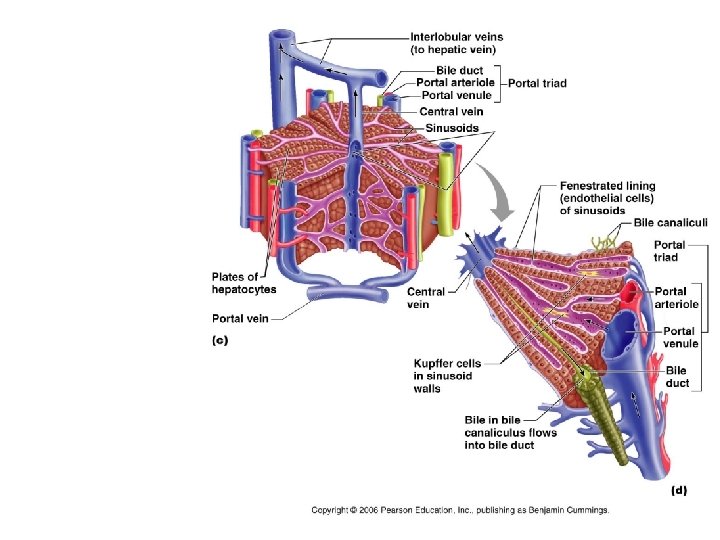
Liver • Digestive function is to produce bile. • Metabolic function is to process venous blood from digestive tract • Functional unit is a lobule
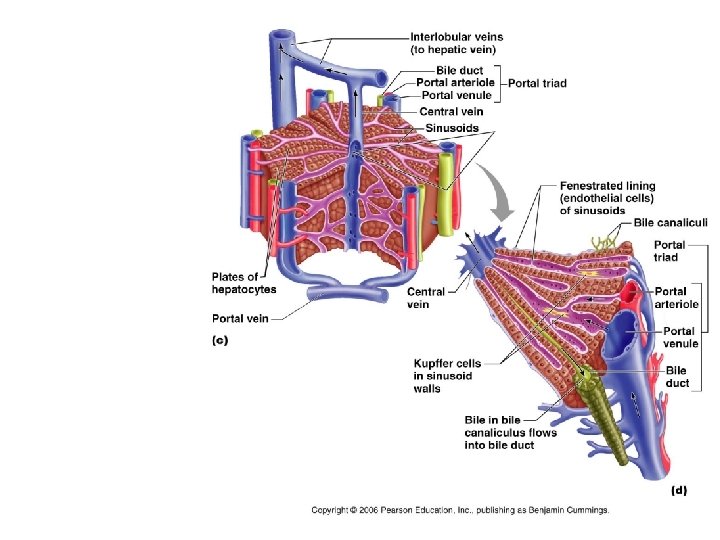
Liver

Liver Functions • • • Carbohydrate metabolism Lipid metabolism Protein metabolism Processing of drugs and hormones Excretion of bilirubin Synthesis of bile salts Storage Phagocytosis Activation of vitamin D
Cholesterol
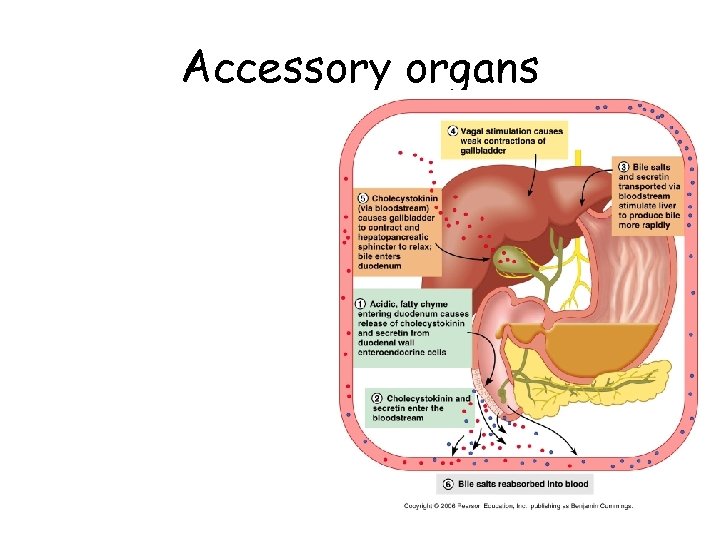
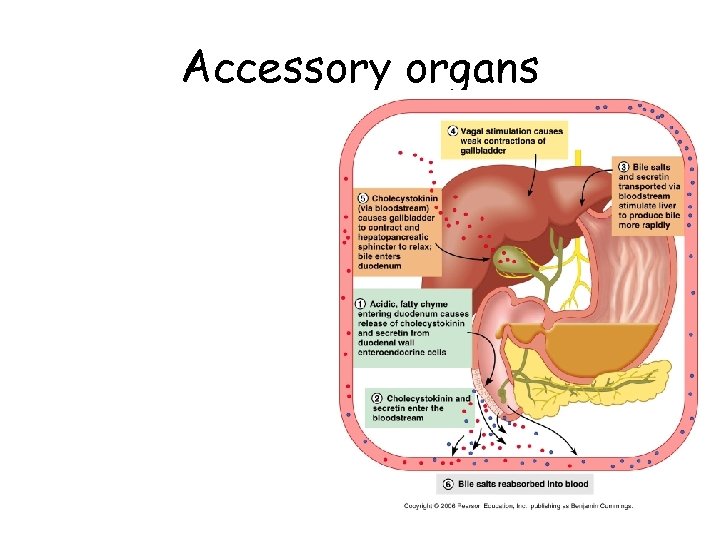
Accessory organs
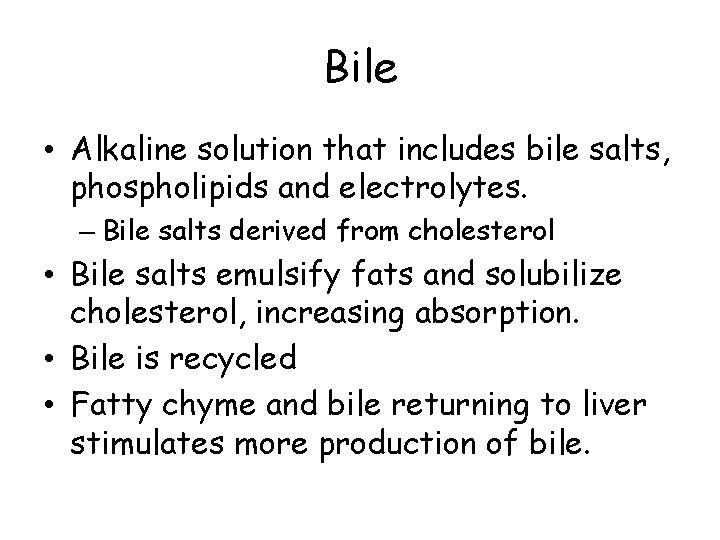
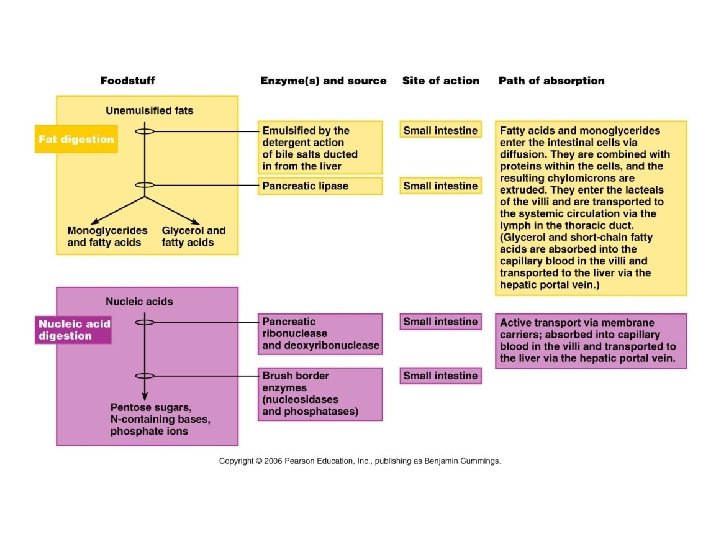
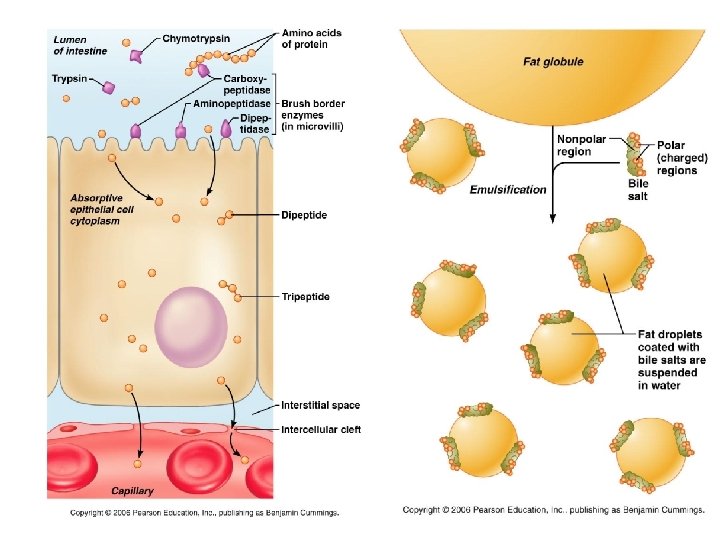
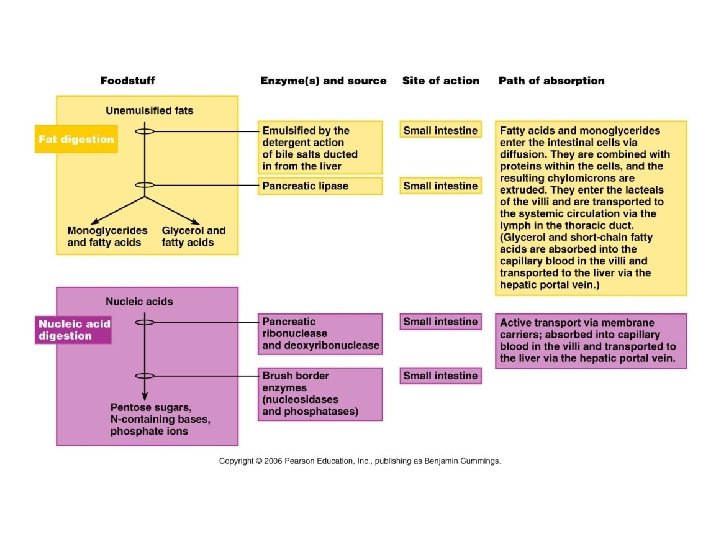
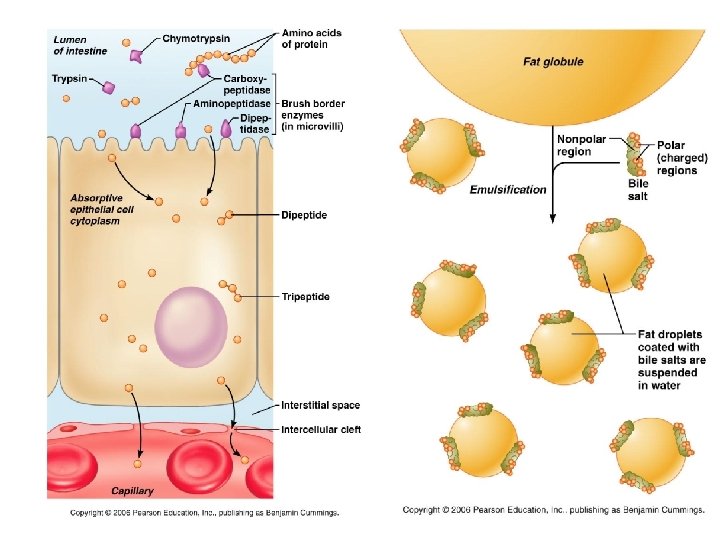
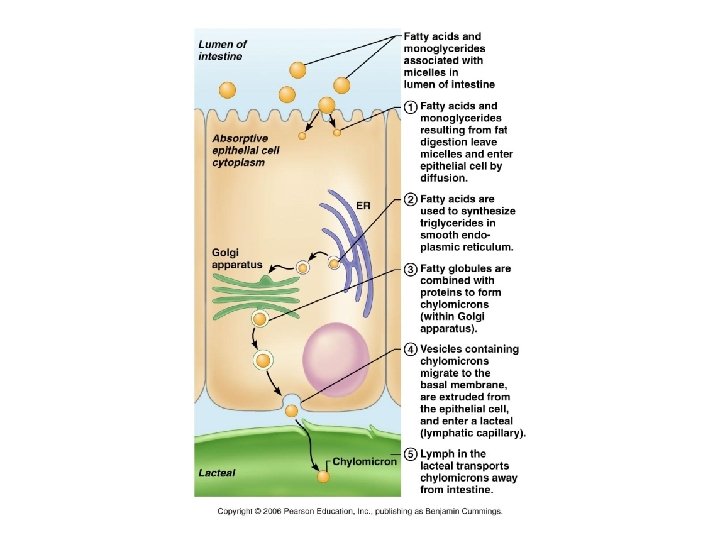
Bile • Alkaline solution that includes bile salts, phospholipids and electrolytes. – Bile salts derived from cholesterol • Bile salts emulsify fats and solubilize cholesterol, increasing absorption. • Bile is recycled • Fatty chyme and bile returning to liver stimulates more production of bile.
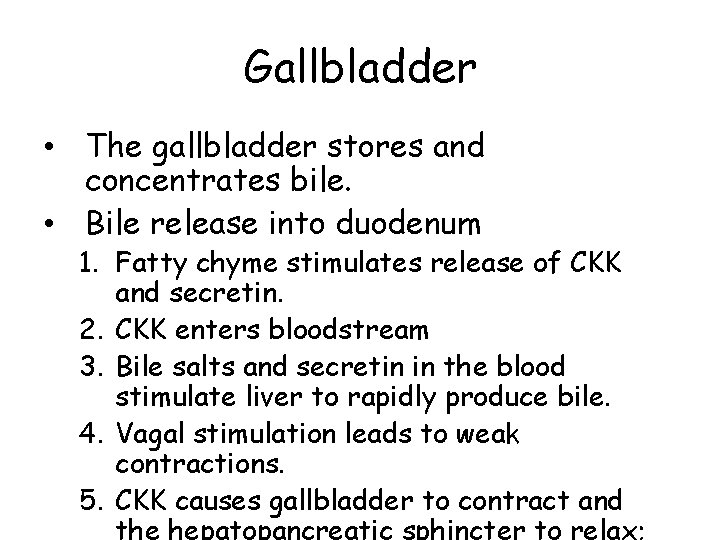
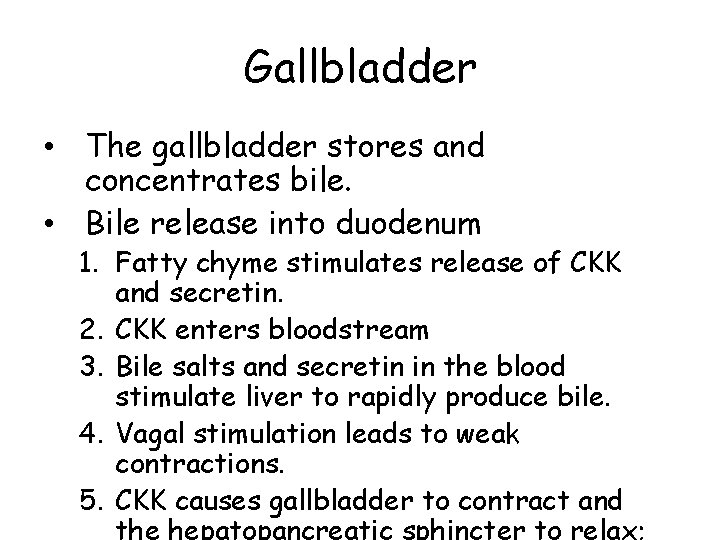
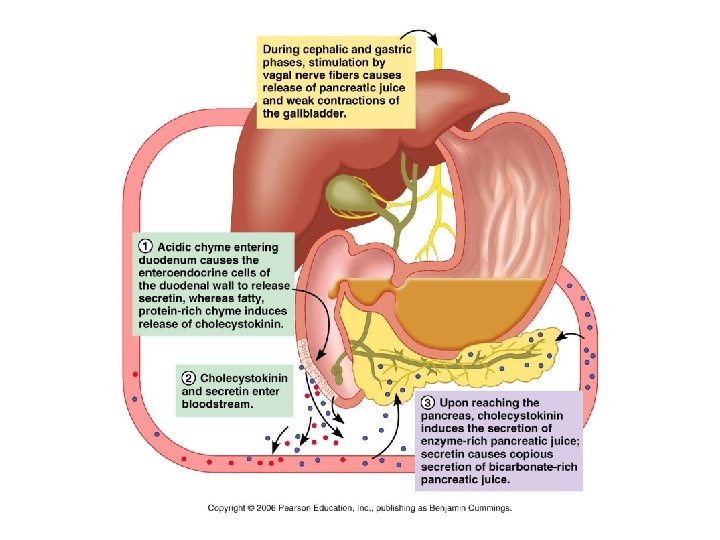
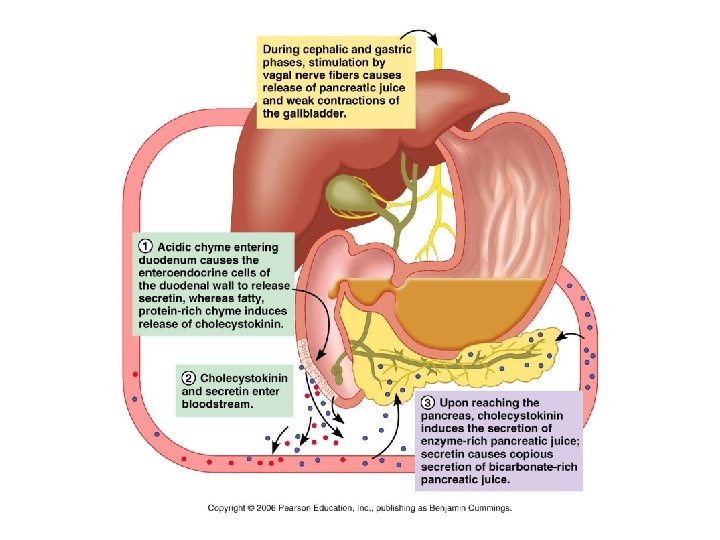
Gallbladder • The gallbladder stores and concentrates bile. • Bile release into duodenum 1. Fatty chyme stimulates release of CKK and secretin. 2. CKK enters bloodstream 3. Bile salts and secretin in the blood stimulate liver to rapidly produce bile. 4. Vagal stimulation leads to weak contractions. 5. CKK causes gallbladder to contract and
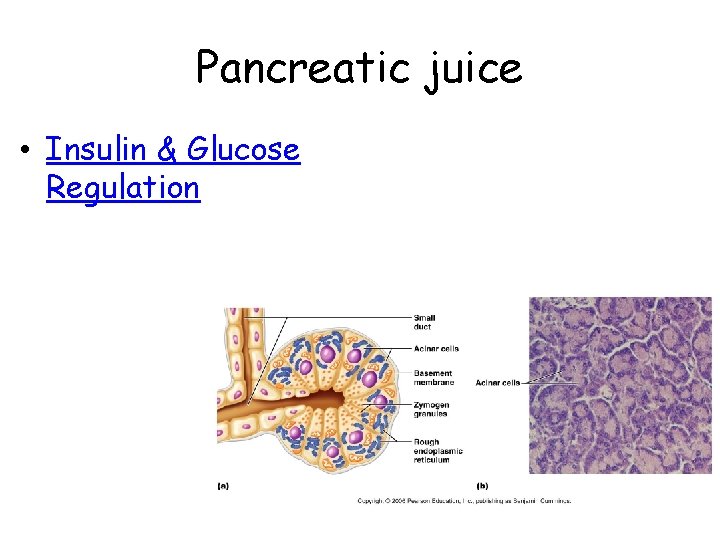
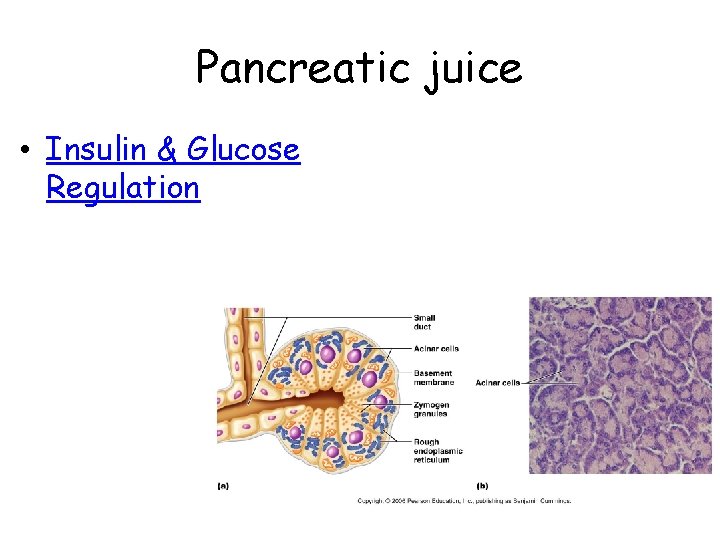
Pancreatic juice • Insulin & Glucose Regulation
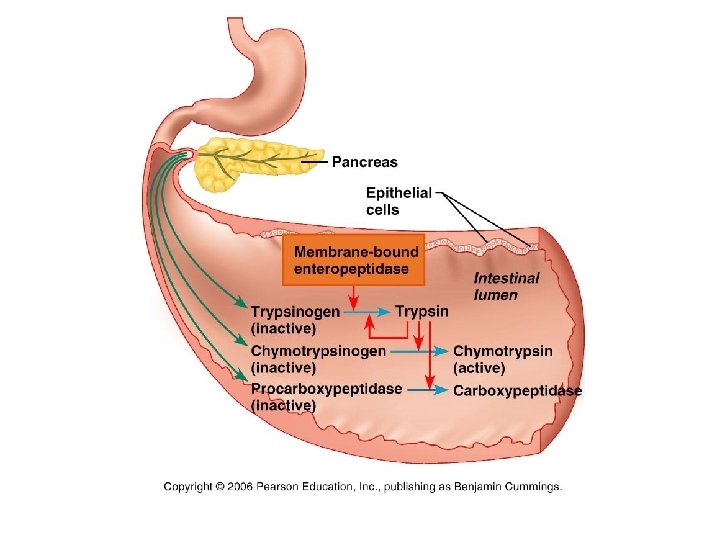
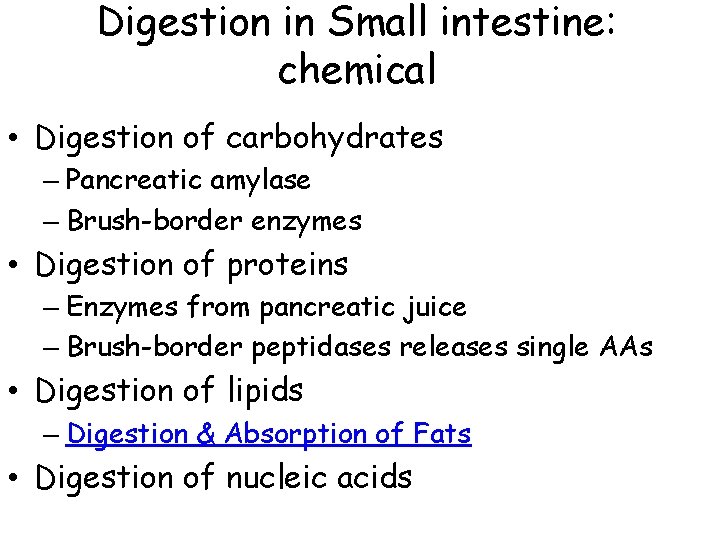
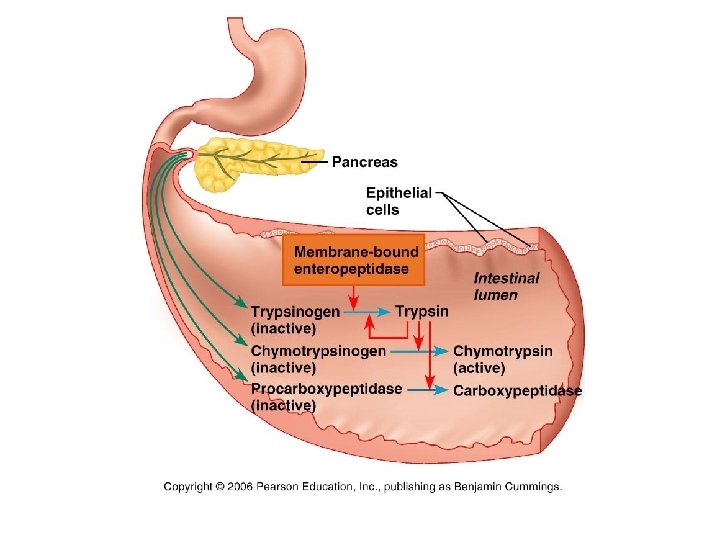
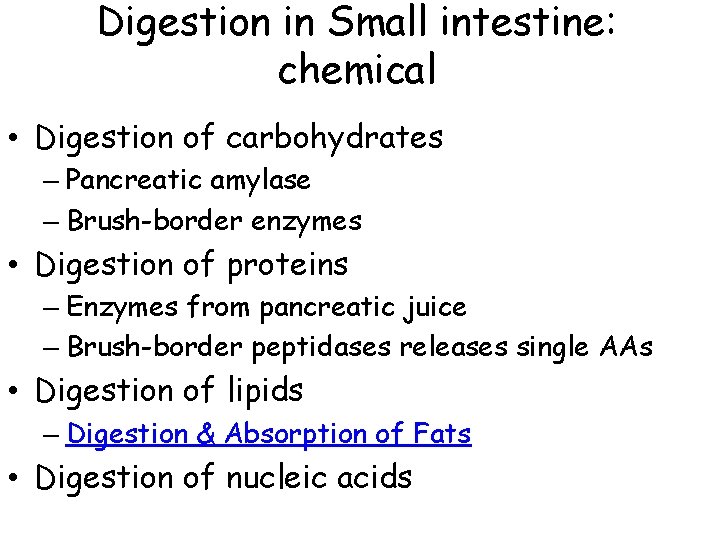
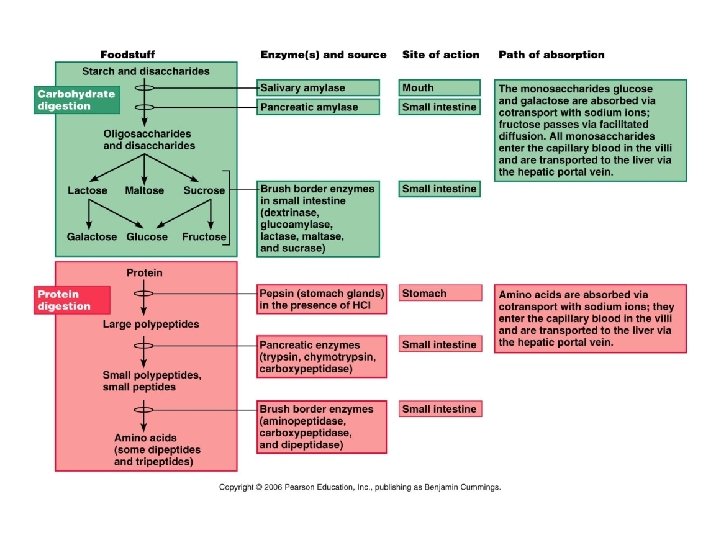
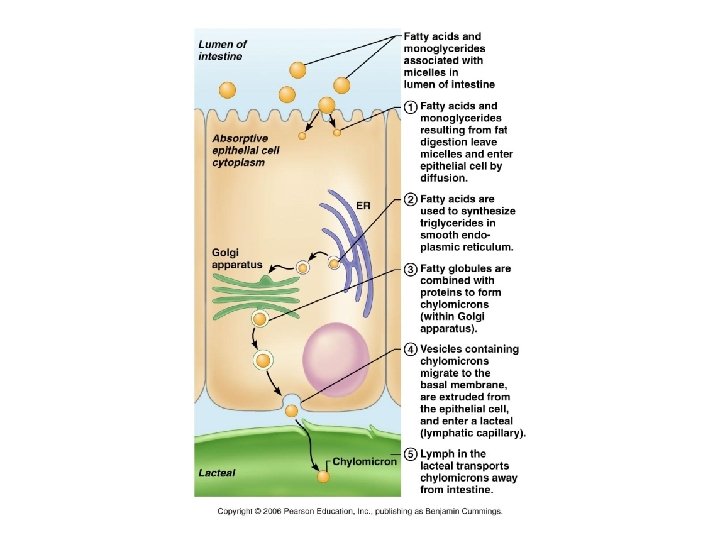
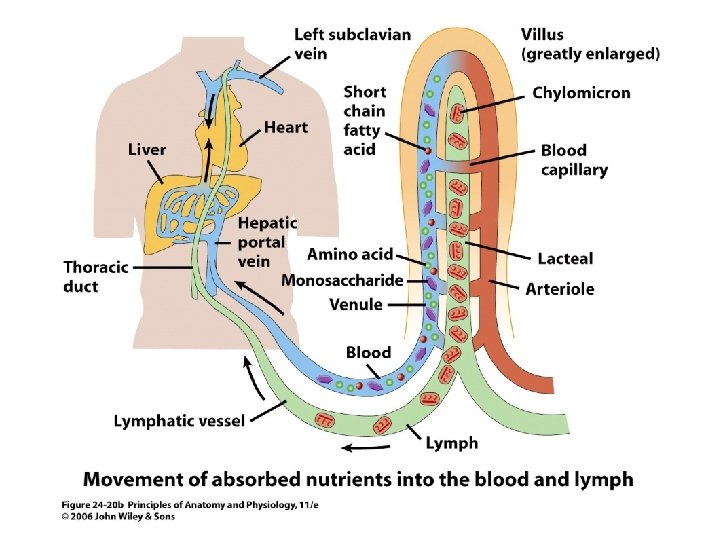
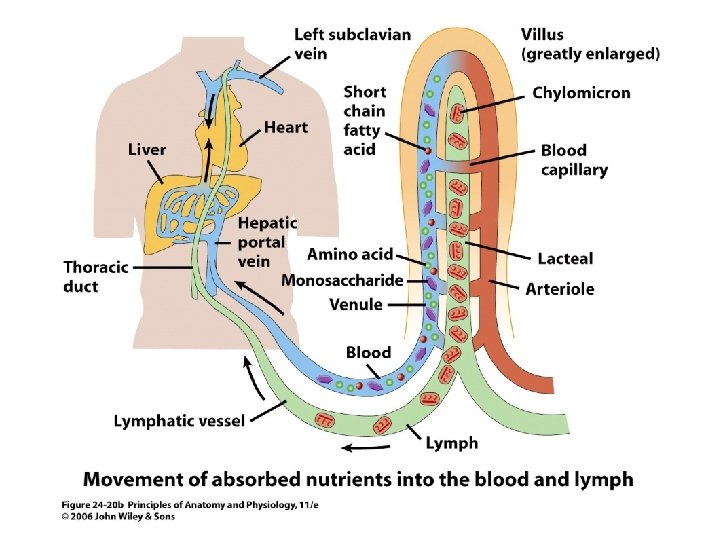
Digestion in Small intestine: chemical • Digestion of carbohydrates – Pancreatic amylase – Brush-border enzymes • Digestion of proteins – Enzymes from pancreatic juice – Brush-border peptidases releases single AAs • Digestion of lipids – Digestion & Absorption of Fats • Digestion of nucleic acids
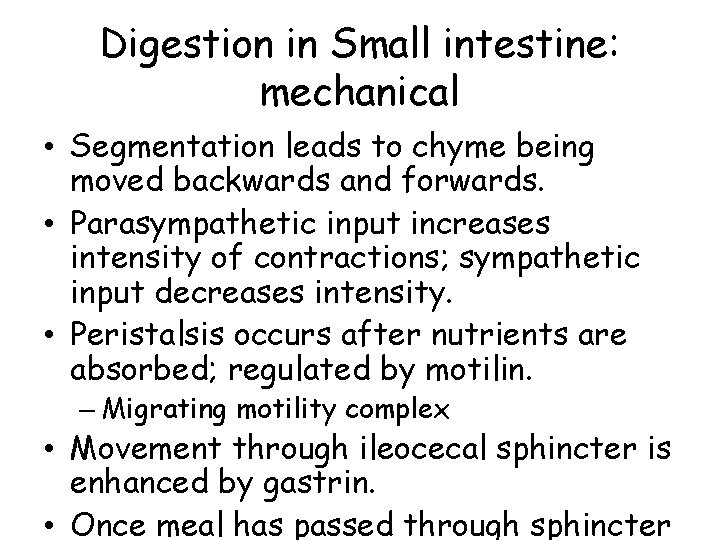
Digestion in Small intestine: mechanical • Segmentation leads to chyme being moved backwards and forwards. • Parasympathetic input increases intensity of contractions; sympathetic input decreases intensity. • Peristalsis occurs after nutrients are absorbed; regulated by motilin. – Migrating motility complex • Movement through ileocecal sphincter is enhanced by gastrin. • Once meal has passed through sphincter
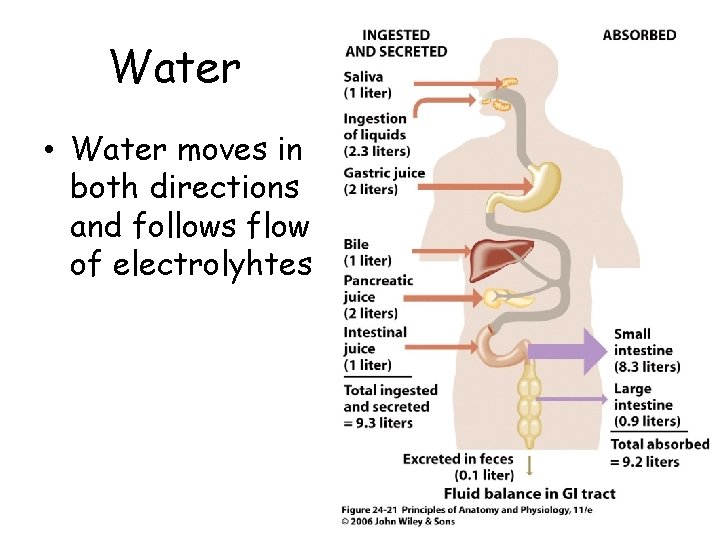
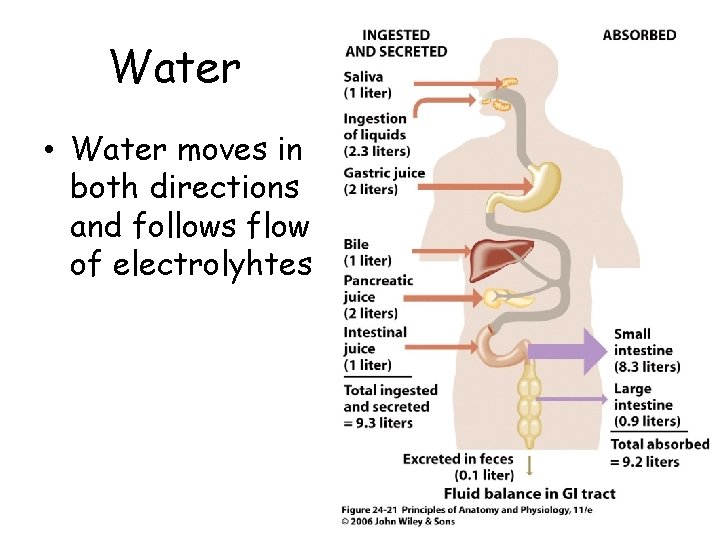
Water • Water moves in both directions and follows flow of electrolyhtes
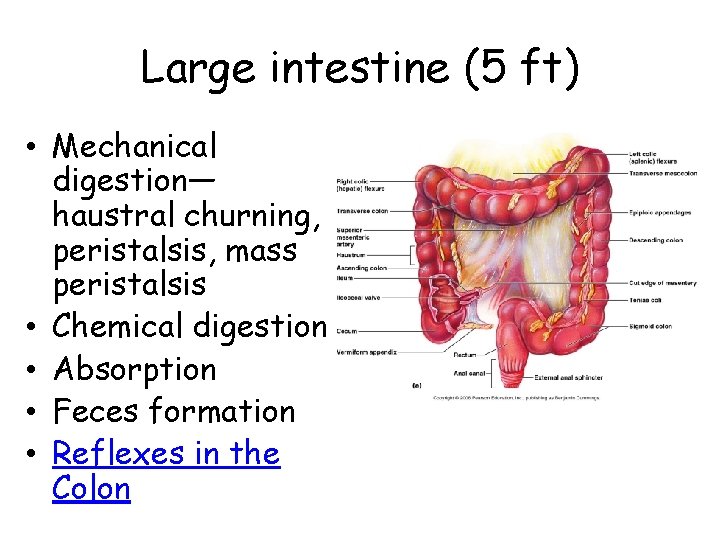
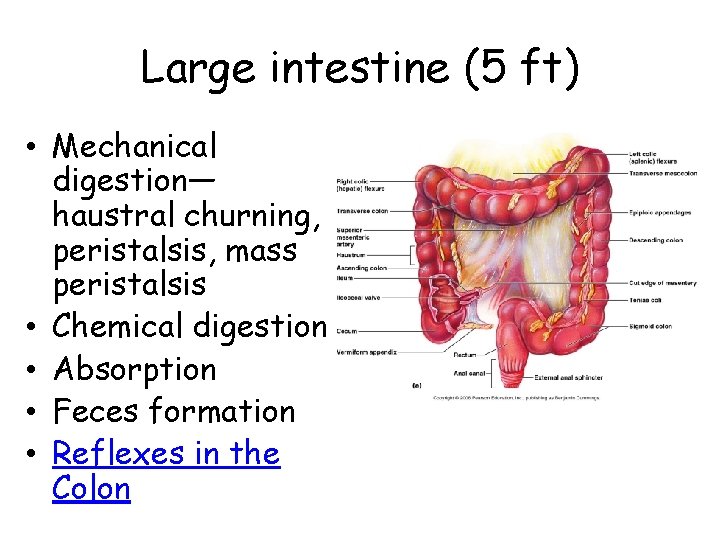
Large intestine (5 ft) • Mechanical digestion— haustral churning, peristalsis, mass peristalsis • Chemical digestion • Absorption • Feces formation • Reflexes in the Colon
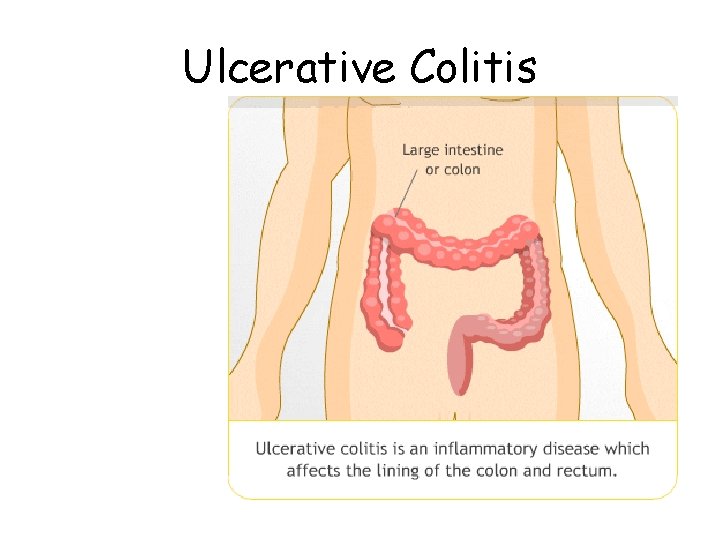
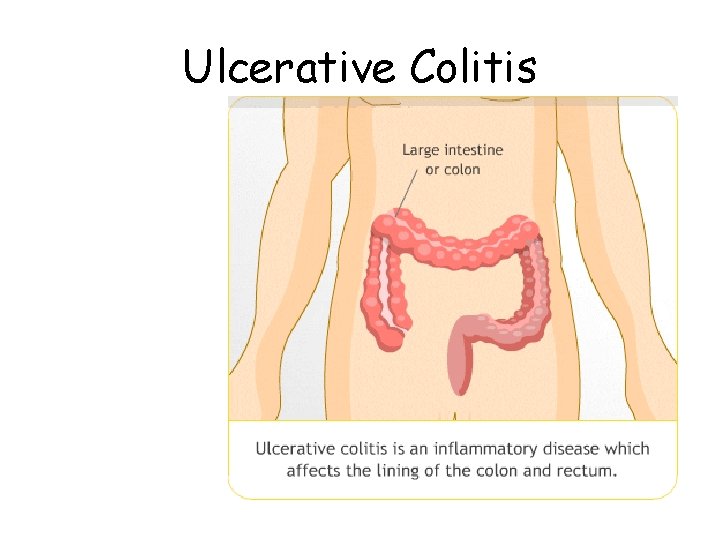
Ulcerative Colitis
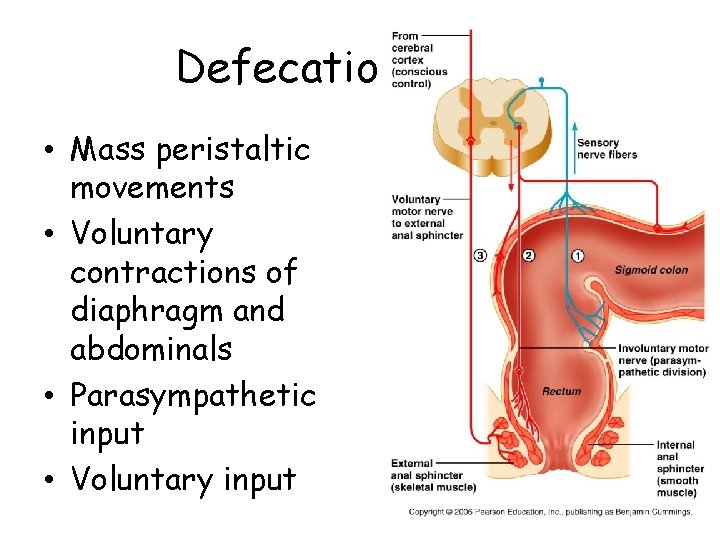
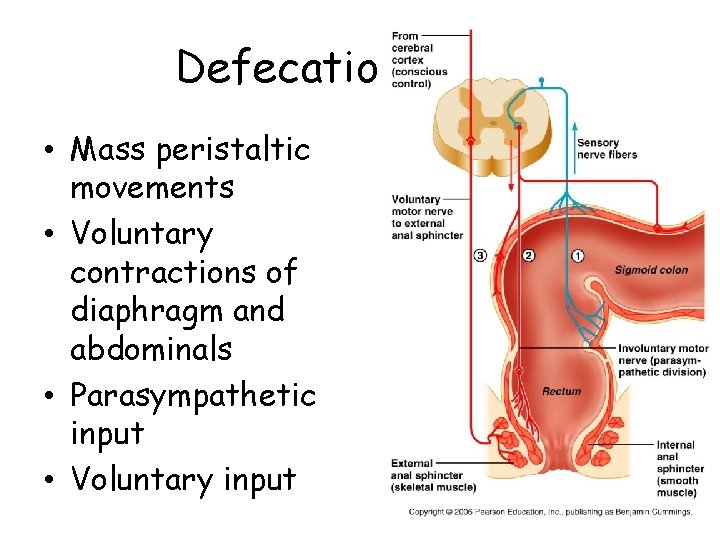
Defecation reflex • Mass peristaltic movements • Voluntary contractions of diaphragm and abdominals • Parasympathetic input • Voluntary input
Resources • • Human Digestion Heart Burn Video Peristalsis Animation Digestive System