THE DIFFICULT AIRWAY MANAGEMENT IN ADULT CRITICAL CARE





- Slides: 60
THE DIFFICULT AIRWAY MANAGEMENT IN ADULT CRITICAL CARE 5 MAY 2014 J MATSHE
AIRWAY MANAGEMENT Obligatory & Necessary skill for ALLL Critical care practitioners FAILURE to maintain airway & provide adequate oxygenation=↑ patient morbidity & mortality; psychologically-distressing to attending registrar ALL Critical Care patients-Initially viewed to have a potentially difficult airway & REMEMBER have less physiological reserves VS airway intervention @ elective surgery
DEFINITION DIFFICULT AIRWAY: Acc to ASA guidelines 2013=Clinical situation whereby conventionally trained anaesthetist experiences DIFFICULTY with either: MASK VENTILATION or TRACHEAL INTUBATION or BOTH ( “CAN’T INTUBATE, CAN’T VENTILATE”) NB: AVOID!!!!!!!
DIFFICULT MASK VENTILATION Unassited anaesthetist cannot maintain arterial oxygen saturation ≥ 90% by mask ventilation using 100% Oxygen & positive pressure OR Cannot reverse signs of inadequate ventilation eg. Absence of chest movement & exhaled CO 2 OR Presence of cyanosis
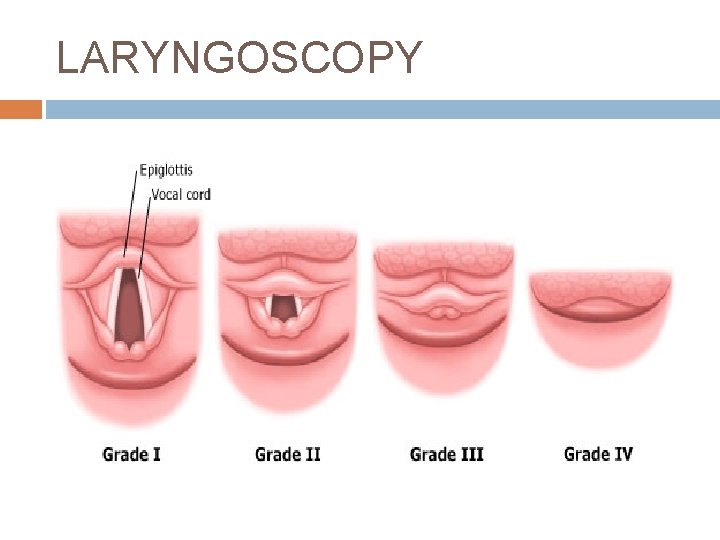
DIFFICULT LARYNGOSCOPY Difficulty visualising any portion of vocal cords using a conventional laryngoscope: Cormack Lehane 3(epiglottis only)/4(soft palate only)
DIFFICULT ENDO-TRACHEAL INTUBATION › 3 Attempts @ inserting ET tube Or › 10 minutes to perform using conventional equipment
OUTLINE INDICATIONS FOR INTUBATION AIRWAY ASSESSMENT & PREDICTING DIFFICULT AIRWAY: PRE-INTUBATION STRATEGY -Preparation -Pre-Oxygenation -Positioning -Premedication PLANS & BACK UP PLANS ADJUNCTS
INDICATIONS FOR INTUBATION Inadequate Oxygenation Inadequate Ventilation Anticipate development of inadequate oxygenation/ventilation Airway protection
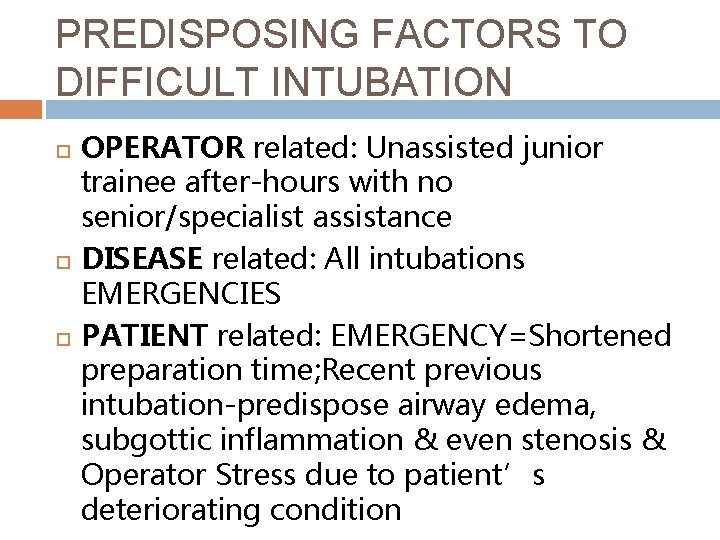
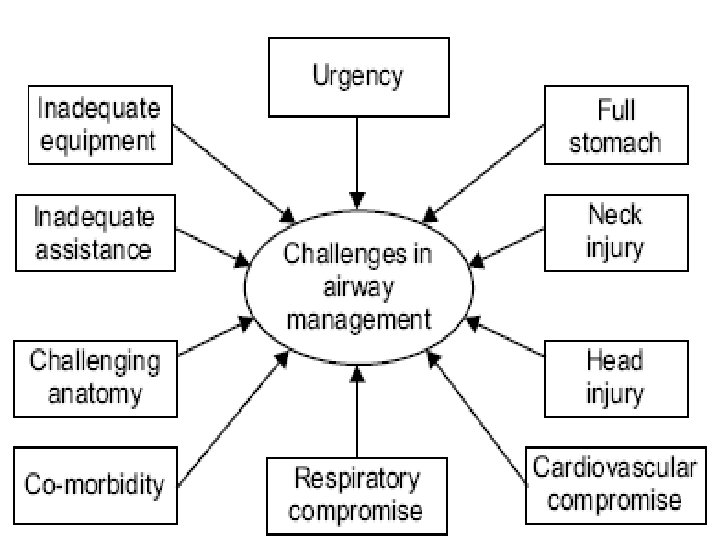
PREDISPOSING FACTORS TO DIFFICULT INTUBATION OPERATOR related: Unassisted junior trainee after-hours with no senior/specialist assistance DISEASE related: All intubations EMERGENCIES PATIENT related: EMERGENCY=Shortened preparation time; Recent previous intubation-predispose airway edema, subgottic inflammation & even stenosis & Operator Stress due to patient’s deteriorating condition
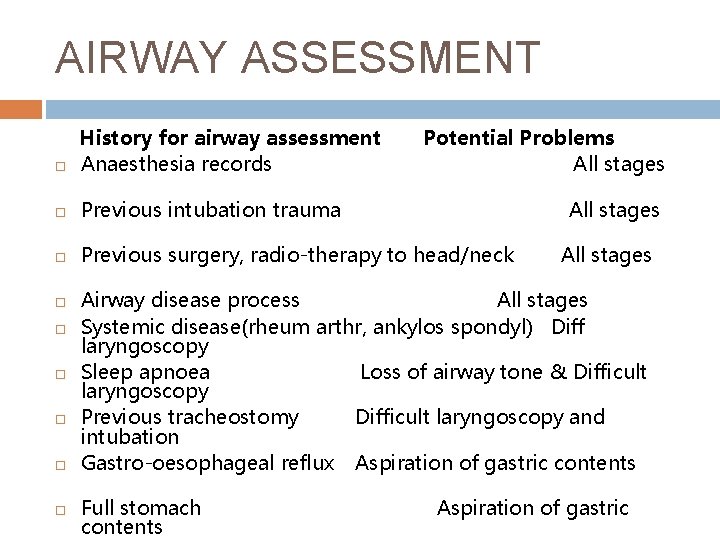
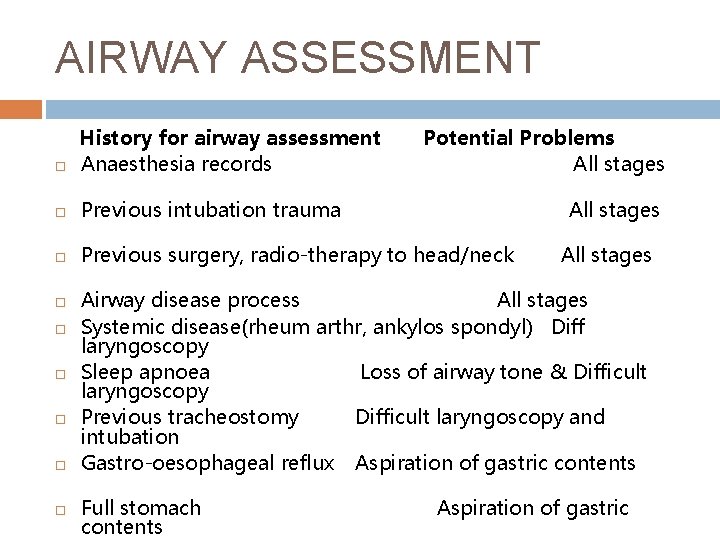
AIRWAY ASSESSMENT History for airway assessment Anaesthesia records Previous intubation trauma Previous surgery, radio-therapy to head/neck Potential Problems All stages Airway disease process All stages Systemic disease(rheum arthr, ankylos spondyl) Diff laryngoscopy Sleep apnoea Loss of airway tone & Difficult laryngoscopy Previous tracheostomy Difficult laryngoscopy and intubation Gastro-oesophageal reflux Aspiration of gastric contents Full stomach contents Aspiration of gastric
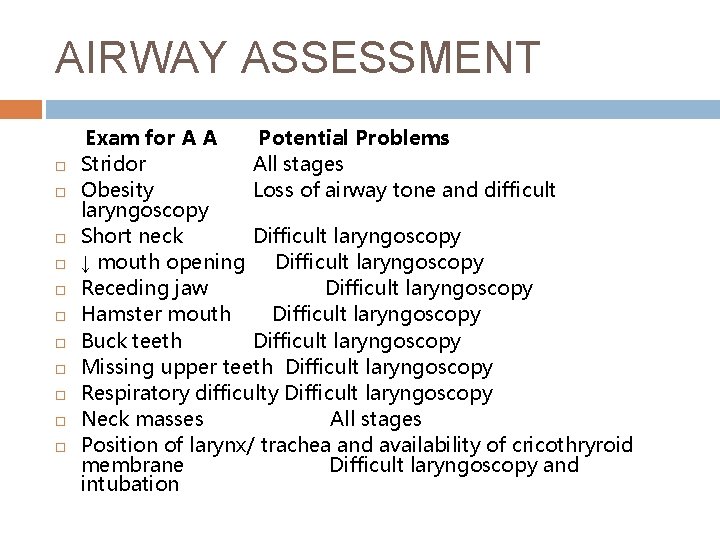
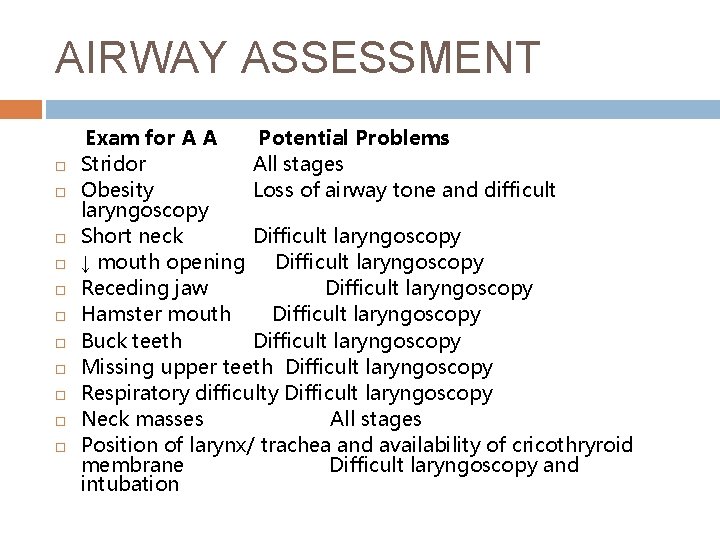
AIRWAY ASSESSMENT Exam for A A Potential Problems Stridor All stages Obesity Loss of airway tone and difficult laryngoscopy Short neck Difficult laryngoscopy ↓ mouth opening Difficult laryngoscopy Receding jaw Difficult laryngoscopy Hamster mouth Difficult laryngoscopy Buck teeth Difficult laryngoscopy Missing upper teeth Difficult laryngoscopy Respiratory difficulty Difficult laryngoscopy Neck masses All stages Position of larynx/ trachea and availability of cricothryroid membrane Difficult laryngoscopy and intubation
BAG MASK VENTILATION
BAG MASK VENTILATION INTEGRAL component of Airway mx If done correctly & successfully: Gives time to prepare for definitive airway mx Entails 3 Principles: Patent Airway, Good mask seal & Proper ventilation
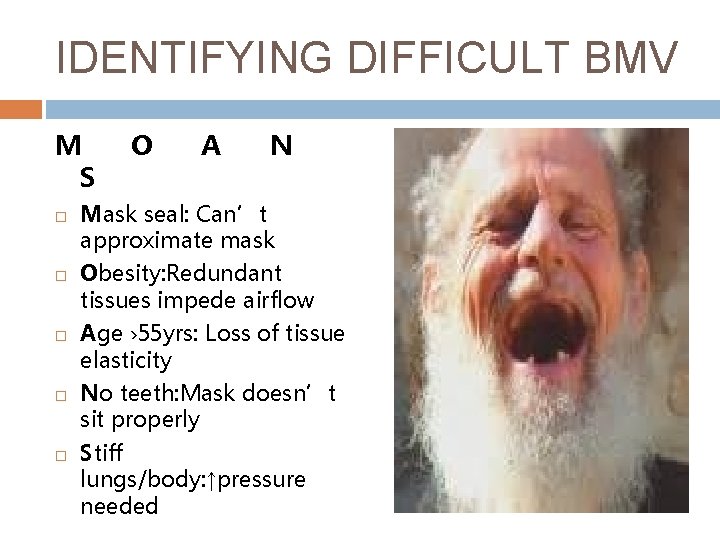
IDENTIFYING DIFFICULT BMV M S O A N Mask seal: Can’t approximate mask Obesity: Redundant tissues impede airflow Age › 55 yrs: Loss of tissue elasticity No teeth: Mask doesn’t sit properly Stiff lungs/body: ↑pressure needed

OPENING AIRWAY MANOUVERE 1 HEAD TILT CHIN LIFT: 1 ST HAND DOWNWARD PRESSURE TOFOREHEAD ; 2 ND HAND INDEX & MIDDLE FINGERS LIFT CHIN
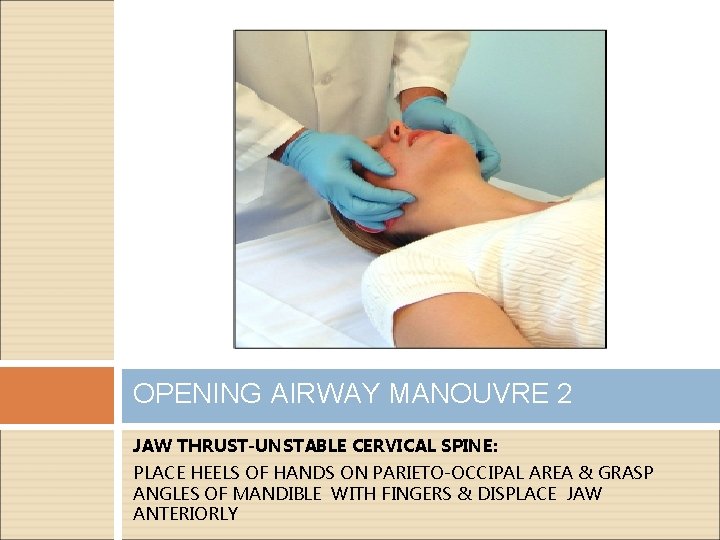
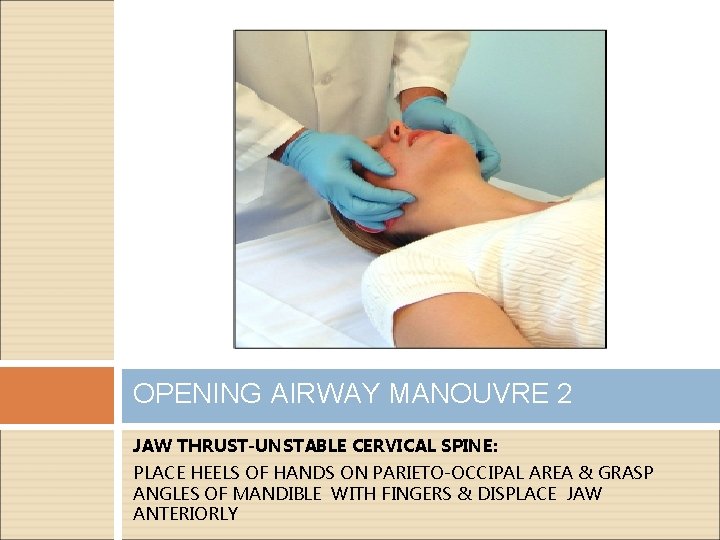
OPENING AIRWAY MANOUVRE 2 JAW THRUST-UNSTABLE CERVICAL SPINE: PLACE HEELS OF HANDS ON PARIETO-OCCIPAL AREA & GRASP ANGLES OF MANDIBLE WITH FINGERS & DISPLACE JAW ANTERIORLY
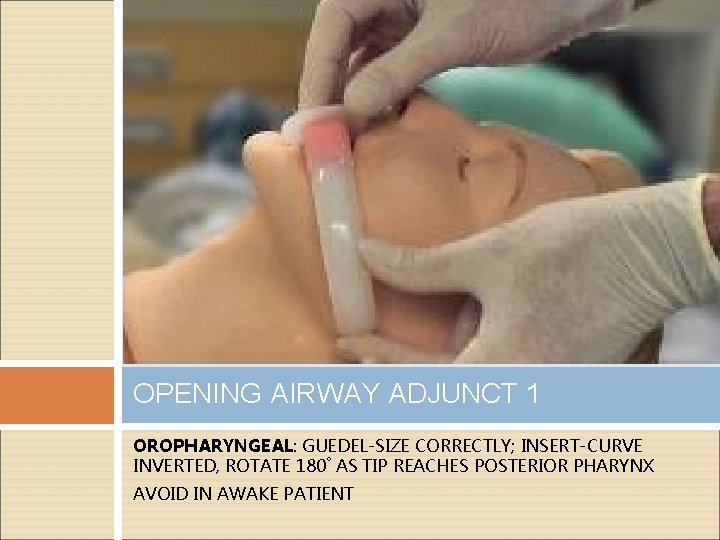
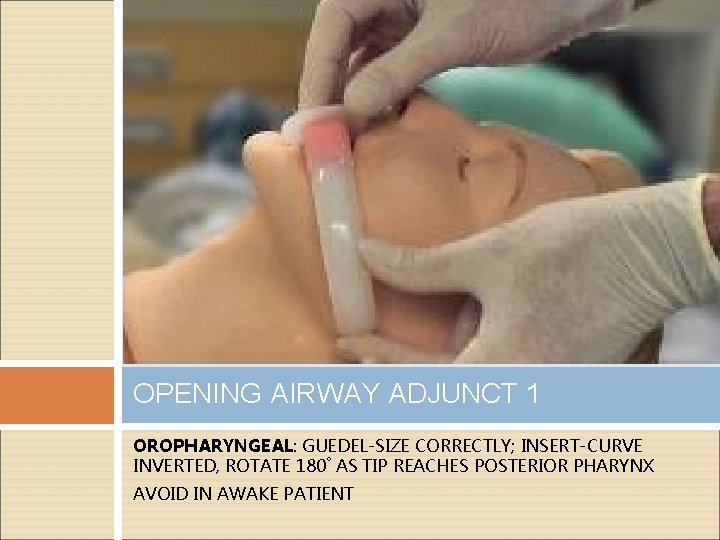
OPENING AIRWAY ADJUNCT 1 OROPHARYNGEAL: GUEDEL-SIZE CORRECTLY; INSERT-CURVE INVERTED, ROTATE 180˚ AS TIP REACHES POSTERIOR PHARYNX AVOID IN AWAKE PATIENT
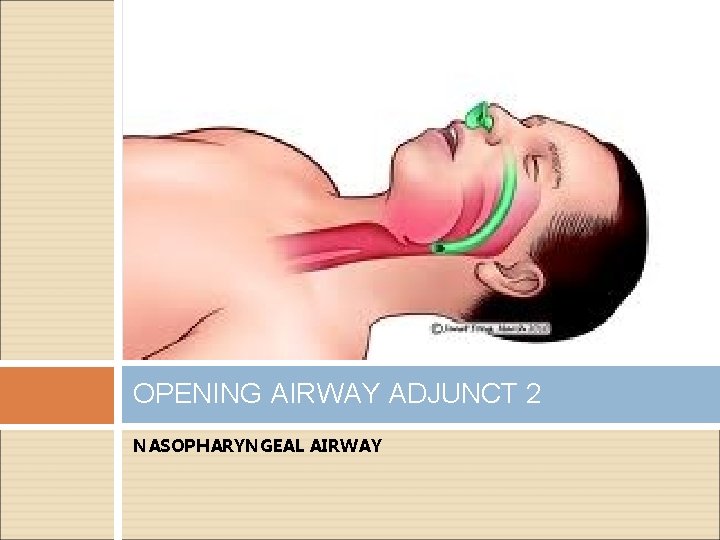
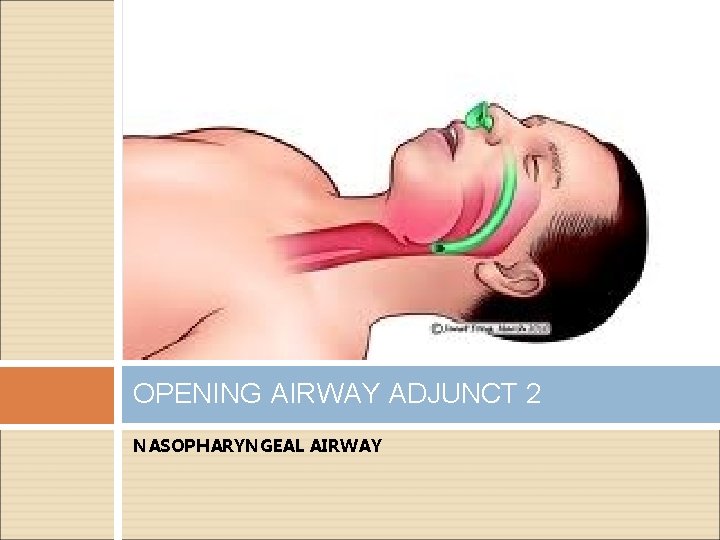
OPENING AIRWAY ADJUNCT 2 NASOPHARYNGEAL AIRWAY
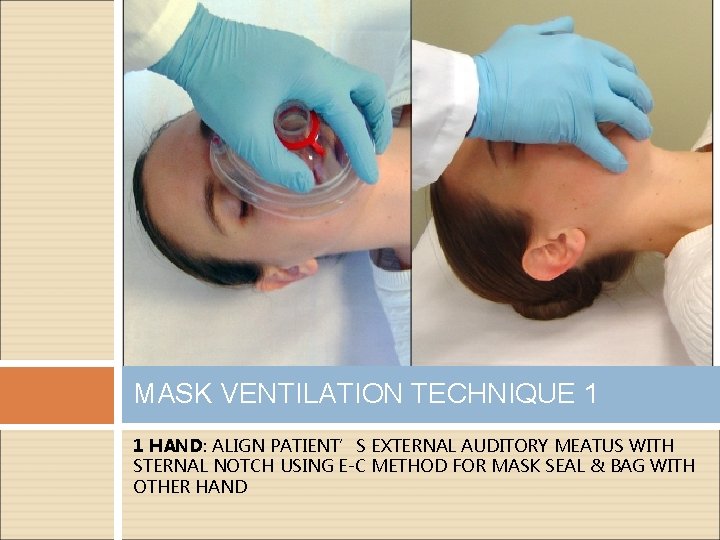
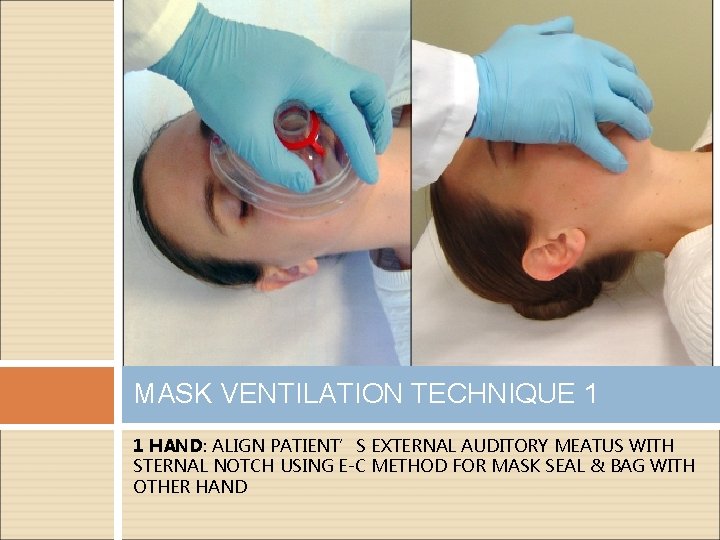
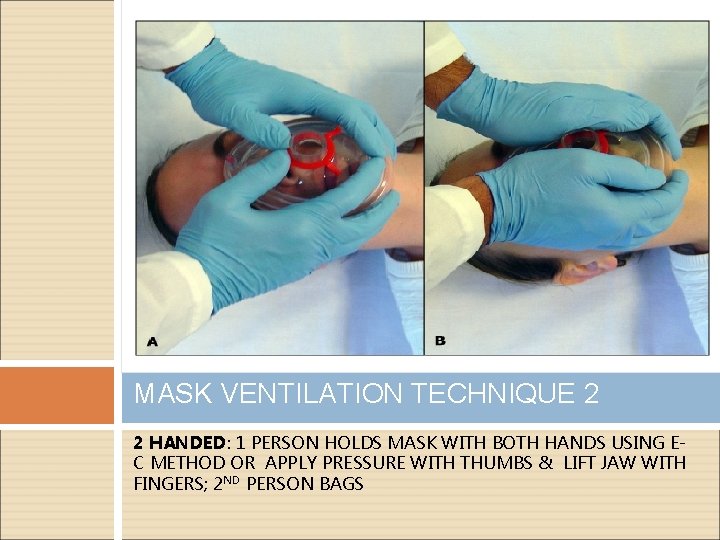
MASK VENTILATION TECHNIQUE 1 1 HAND: ALIGN PATIENT’S EXTERNAL AUDITORY MEATUS WITH STERNAL NOTCH USING E-C METHOD FOR MASK SEAL & BAG WITH OTHER HAND
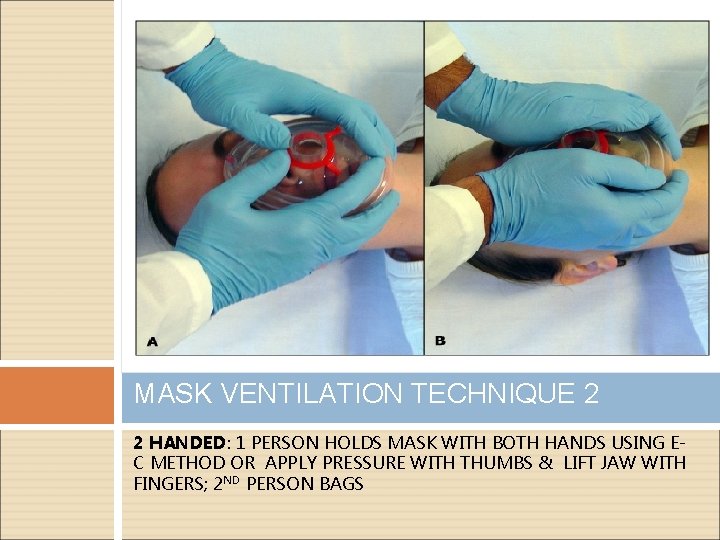
MASK VENTILATION TECHNIQUE 2 2 HANDED: 1 PERSON HOLDS MASK WITH BOTH HANDS USING EC METHOD OR APPLY PRESSURE WITH THUMBS & LIFT JAW WITH FINGERS; 2 ND PERSON BAGS
ENDOTRACHEAL INTUBATION
THE DIFFICULT INTUBATION Failure to intubate can result in severe adverse events such as: Airway trauma Aspiration Hypoxemia/Anoxic brain injury Hypotension Cardiac arrest & Death BE PREPARED & HAVE A PLAN
IDENTIFYING THE DIFFICULT INTUBATION L E M O LOOK EVALUATE 3 -3 -2 MALLAMPATI OBSTRUCTION/OBESITY NECK MOBILITY N
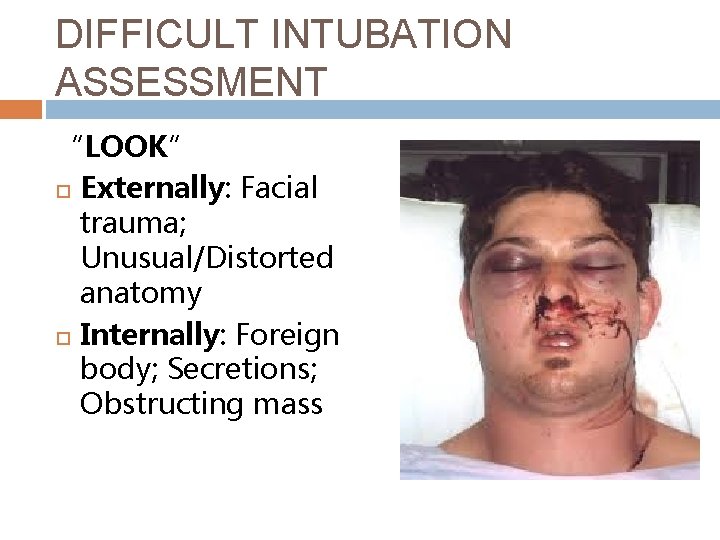
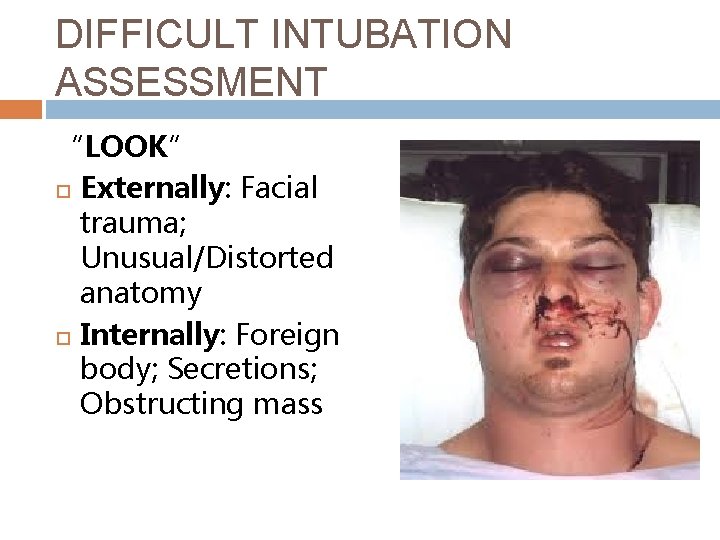
DIFFICULT INTUBATION ASSESSMENT “LOOK” Externally: Facial trauma; Unusual/Distorted anatomy Internally: Foreign body; Secretions; Obstructing mass
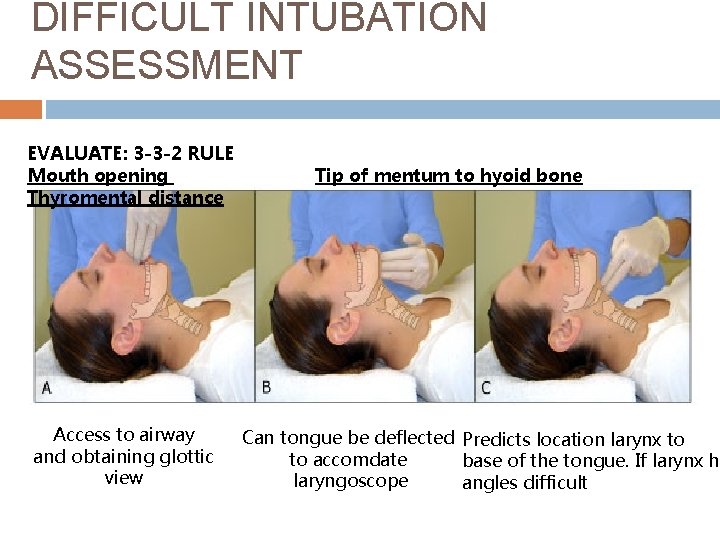
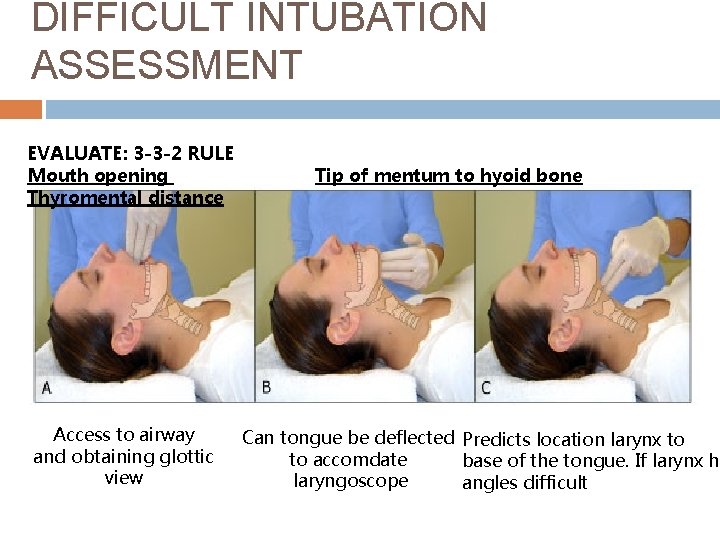
DIFFICULT INTUBATION ASSESSMENT EVALUATE: 3 -3 -2 RULE Mouth opening Thyromental distance Access to airway and obtaining glottic view Tip of mentum to hyoid bone Can tongue be deflected Predicts location larynx to to accomdate base of the tongue. If larynx hi laryngoscope angles difficult
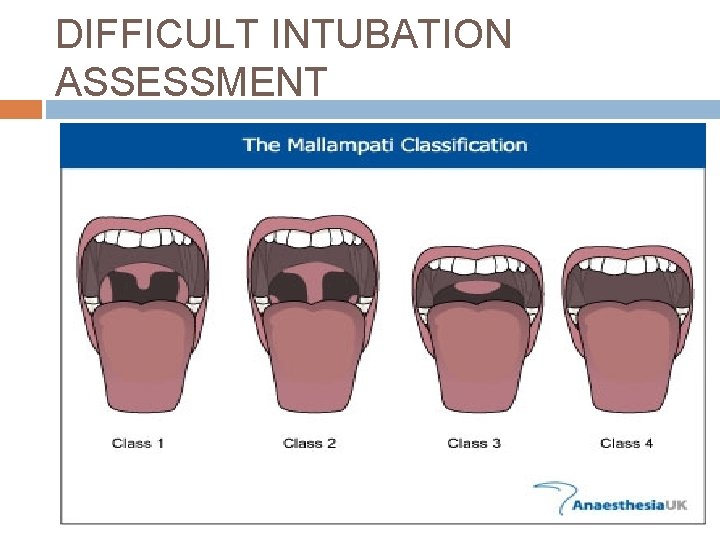
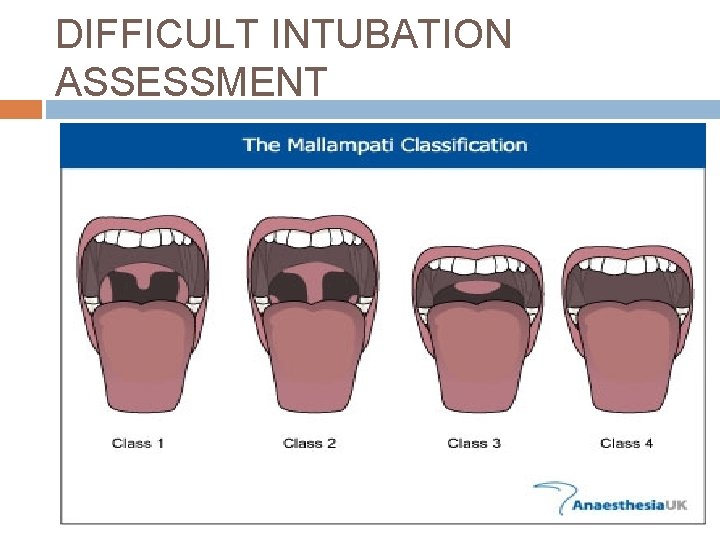
DIFFICULT INTUBATION ASSESSMENT
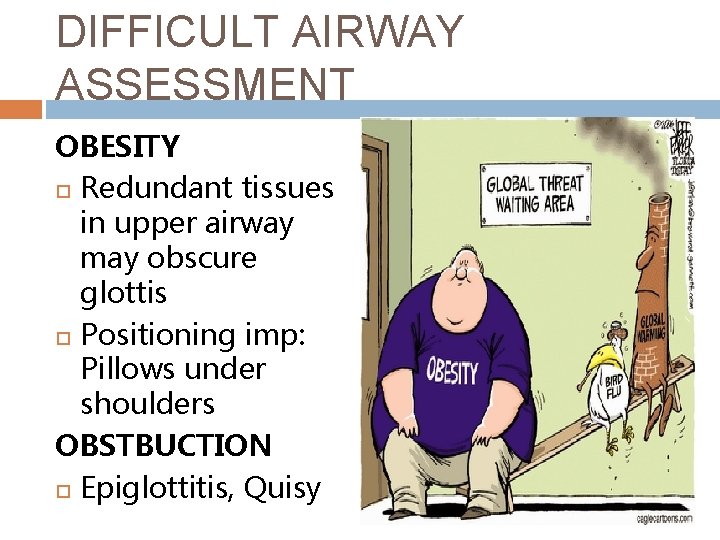
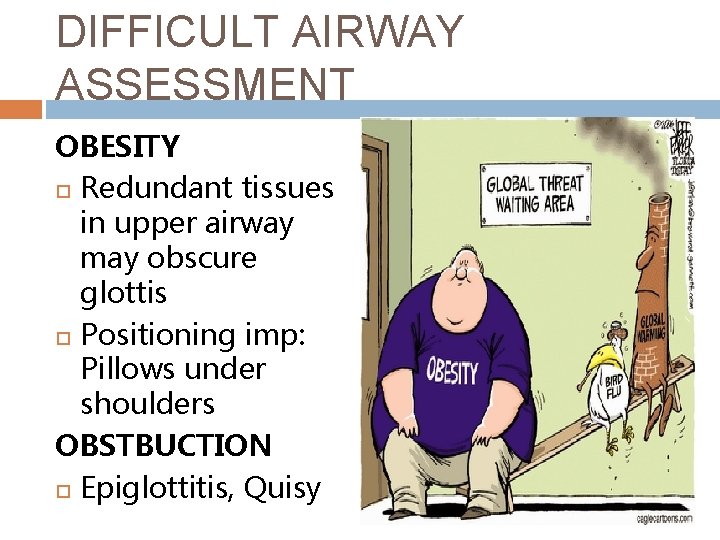
DIFFICULT AIRWAY ASSESSMENT OBESITY Redundant tissues in upper airway may obscure glottis Positioning imp: Pillows under shoulders OBSTBUCTION Epiglottitis, Quisy
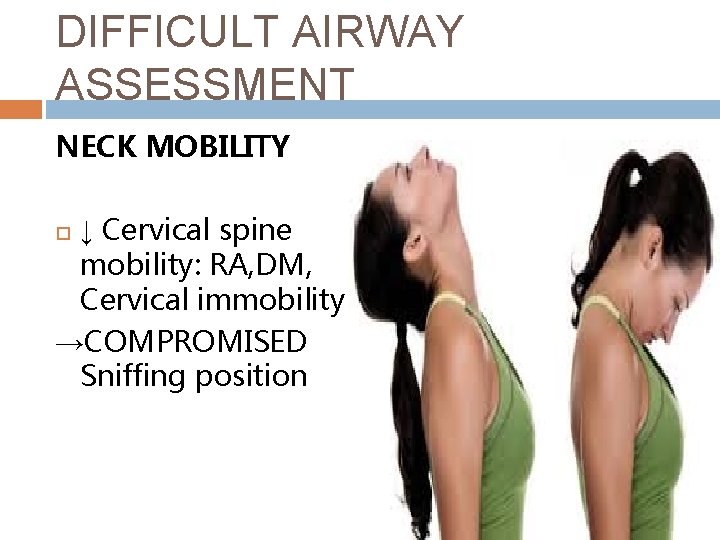
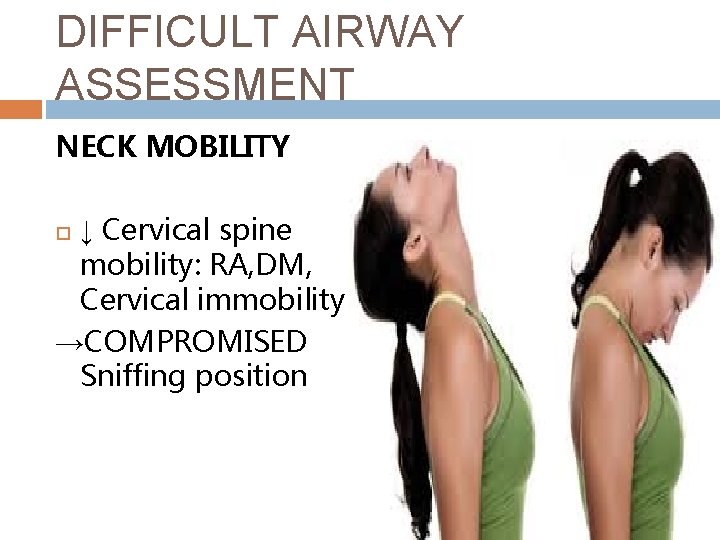
DIFFICULT AIRWAY ASSESSMENT NECK MOBILITY ↓ Cervical spine mobility: RA, DM, Cervical immobility →COMPROMISED Sniffing position
PRE-INTUBATION STRATEGY PREPARATION PRE-OXYGENATION POSITIONING PREMEDICATION
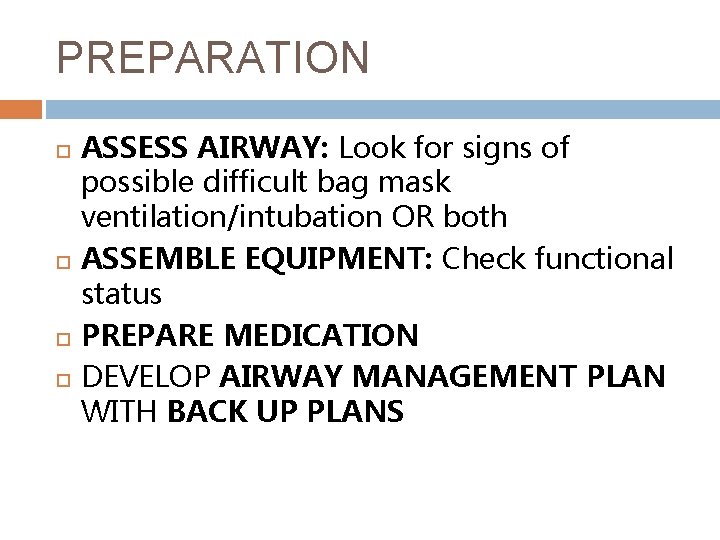
PREPARATION ASSESS AIRWAY: Look for signs of possible difficult bag mask ventilation/intubation OR both ASSEMBLE EQUIPMENT: Check functional status PREPARE MEDICATION DEVELOP AIRWAY MANAGEMENT PLAN WITH BACK UP PLANS
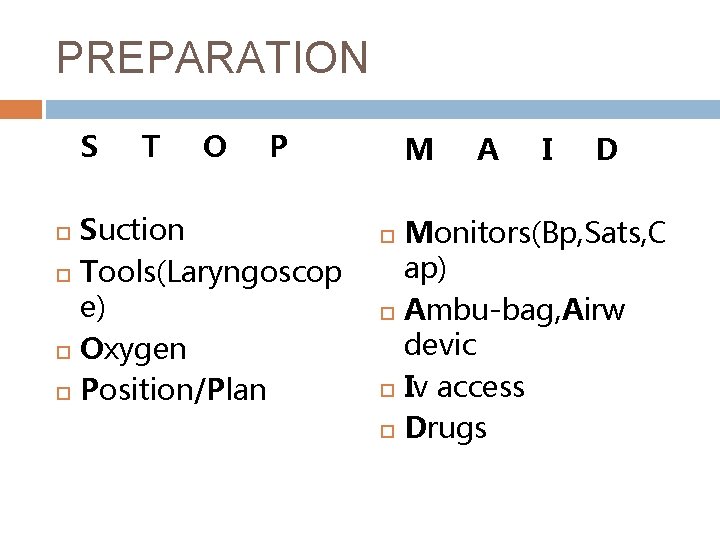
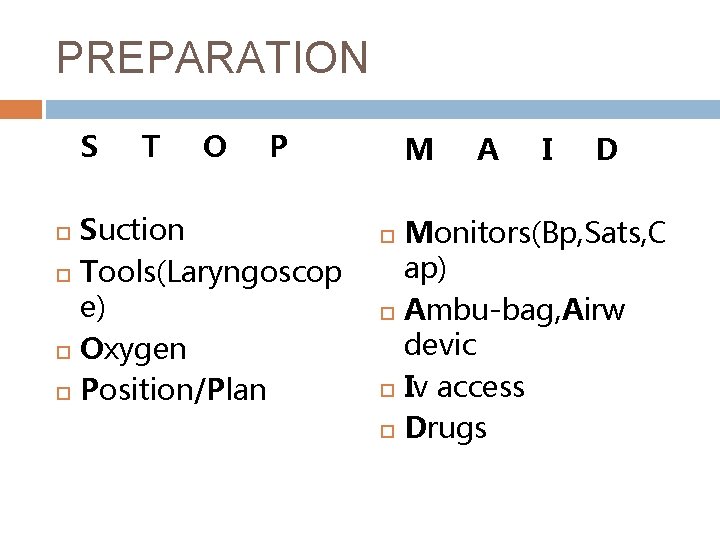
PREPARATION S T O P Suction Tools(Laryngoscop e) Oxygen Position/Plan M A I D Monitors(Bp, Sats, C ap) Ambu-bag, Airw devic Iv access Drugs
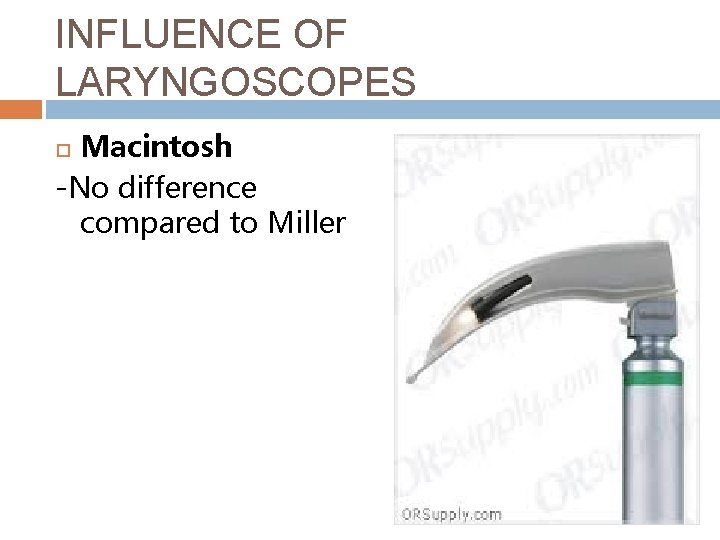
INFLUENCE OF LARYNGOSCOPES Macintosh -No difference compared to Miller
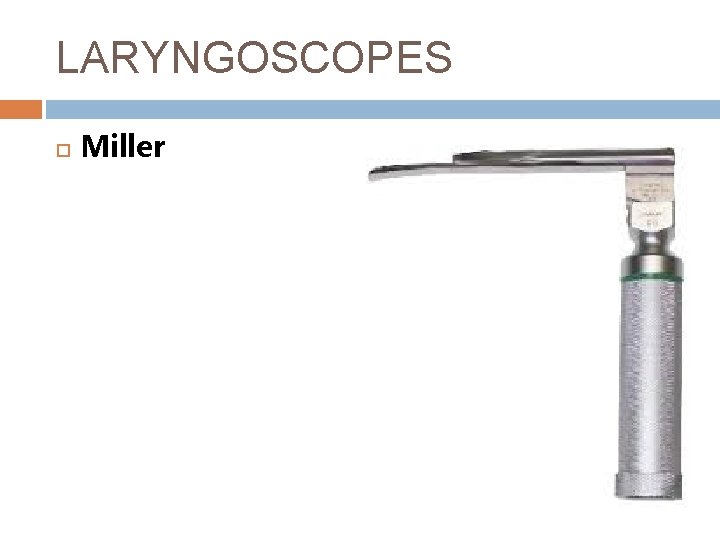
LARYNGOSCOPES Miller
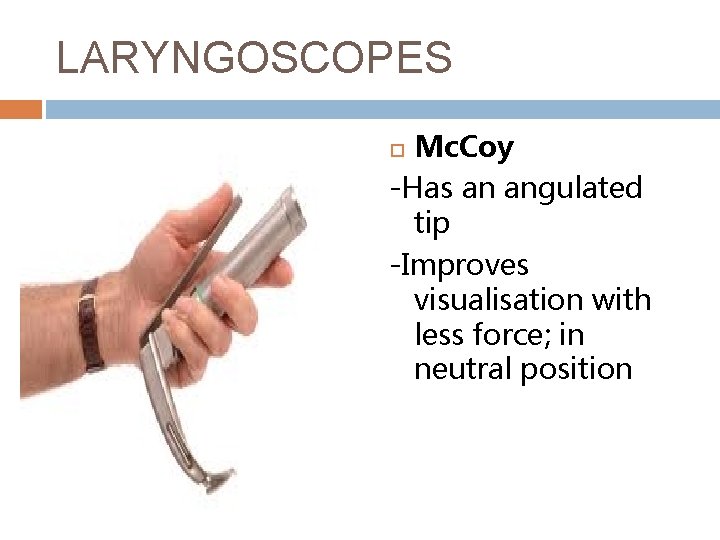
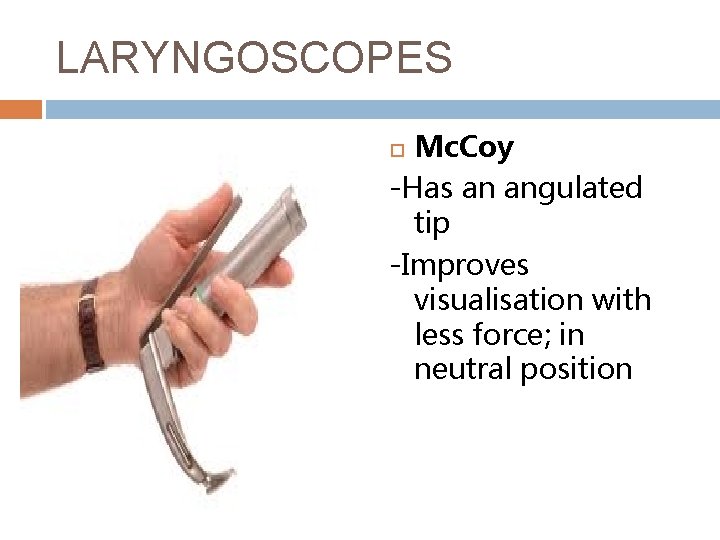
LARYNGOSCOPES Mc. Coy -Has an angulated tip -Improves visualisation with less force; in neutral position

LARYNGOSCOPES Bullard/Airtraq -Rigid fibre-optic laryngoscope -Alignment of axes not required
PREOXYGENATION Establish oxygen reservoir -Replace nitrogenous room air mixture with 100% oxygen Challenge in ICU -Head of bed elevation -NIPPV q Challenge in Obesity & Critically ill patients -Desaturate much quicker
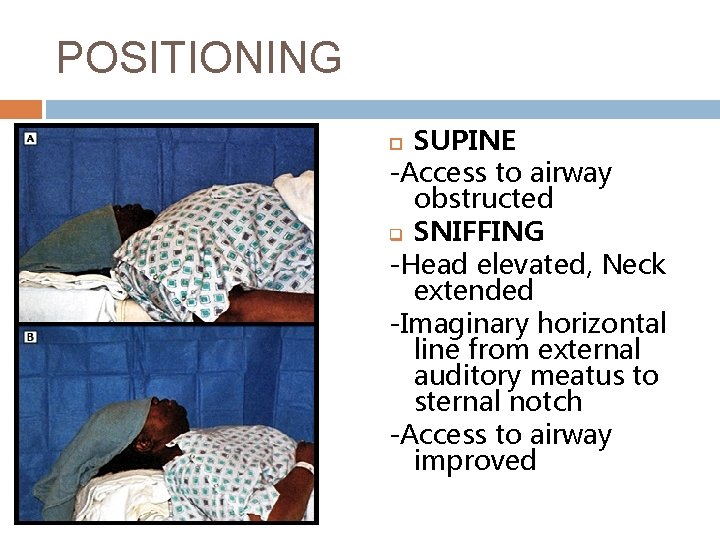
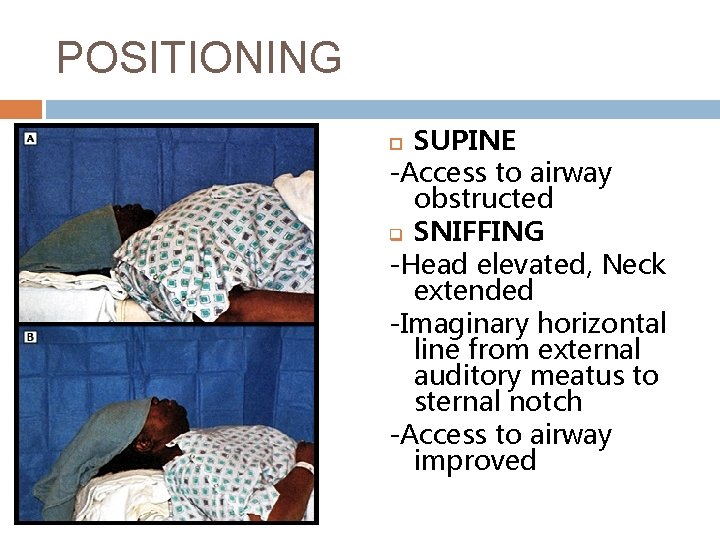
POSITIONING SUPINE -Access to airway obstructed q SNIFFING -Head elevated, Neck extended -Imaginary horizontal line from external auditory meatus to sternal notch -Access to airway improved
PREMEDICATION ICU pts-require very little or no drugs L O A D Lidocaine: Reactive airways & ↑ICP Opioids: Blunt sympathetic response & ↑BP Atropine: Bradycardia in kids particularly Defasciculating agent-↓dose competitive neuromuscular blockade: ↑ICP
INDUCTION AGENTS KETAMINE: Sedation & Analgesia; No hypotension; Bronchodilatory effect; Respiratory drive preserved; ↑ICP & BP. Dose: 1 -2 mg/kg iv PROPOFOL: Rapid onset; No analgesia; Hypotension. Dose: 1. 5 -3 mg/kg iv MIDAZOLAM: Time to effect › 15 min ; Hypotension. Dose: 0. 1 -0. 3 mg/kg iv ETOMIDATE: Rapid onset; No analgesia/Hypotension. Dose: 0. 3 mg/kg
MUSCLE RELAXANTS SUXAMETHONIUM Onset 45 -60 sec; DOA 6 -10 min. Dose: 1 -1. 5 mg/kg iv; C/IRhabdomyolysis, Hyperkalemia, Burns › 72 hrs & Hx Malignant HT ROCURONIUM Onset 60 min; Longer DOA than Sux. Dose 0. 8 1. 2 mg/kg iv
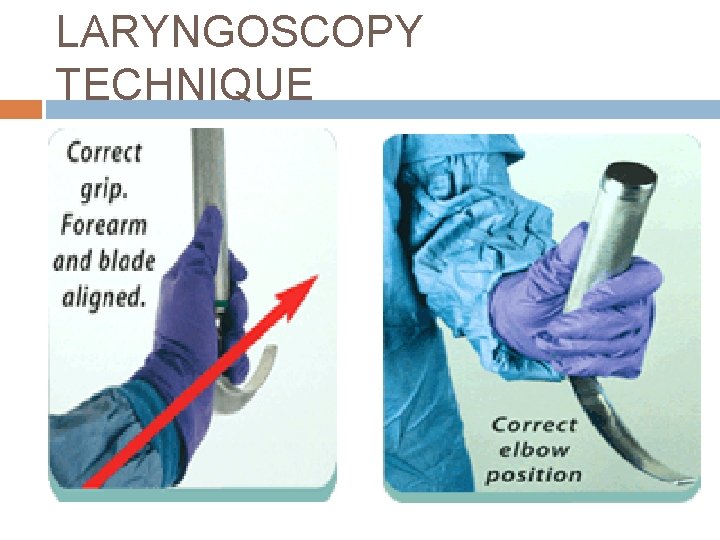
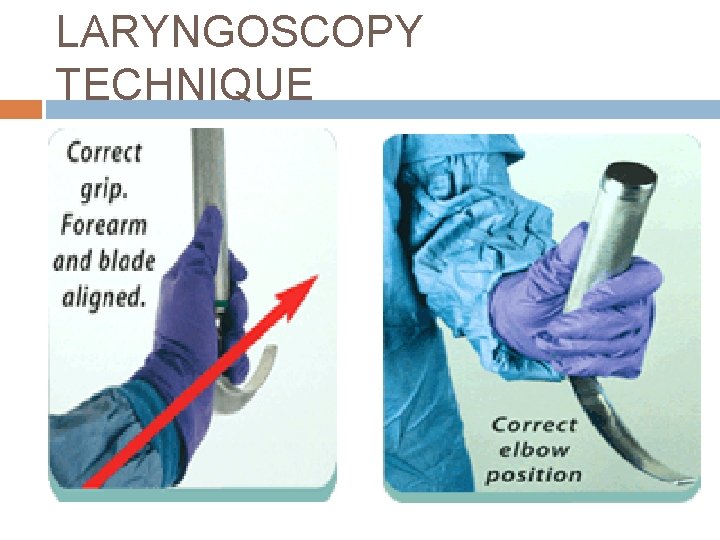
LARYNGOSCOPY TECHNIQUE
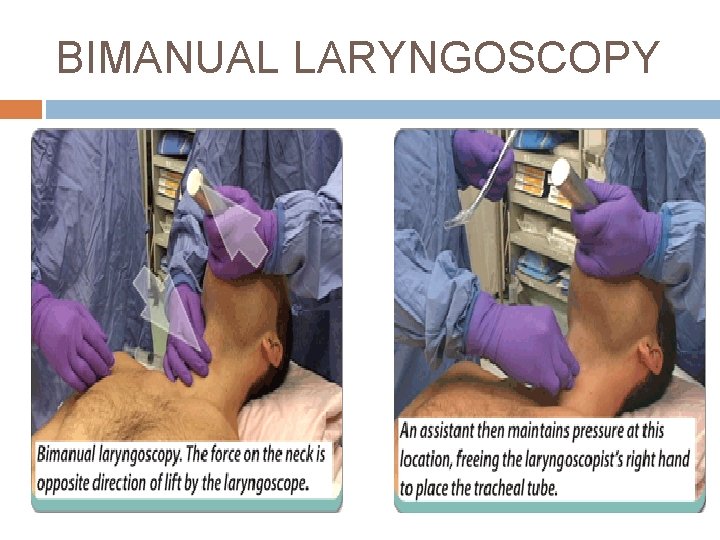
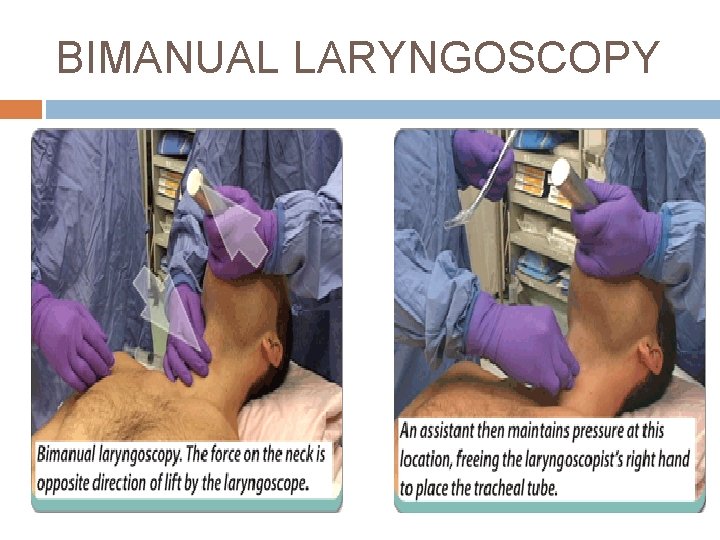
BIMANUAL LARYNGOSCOPY
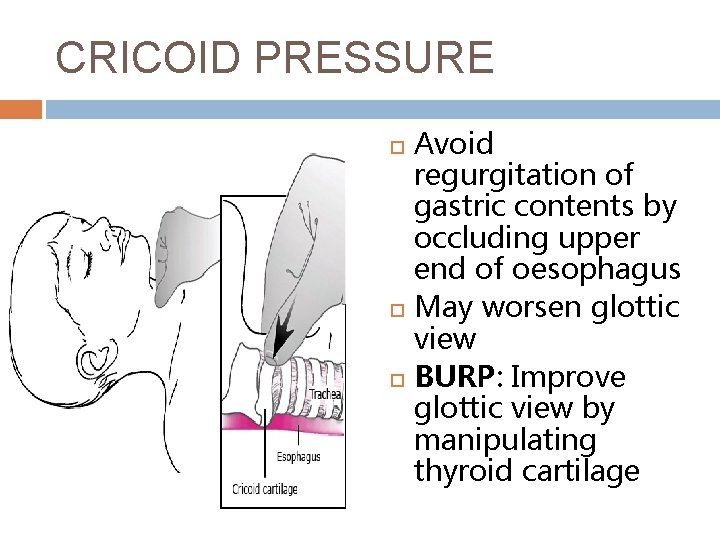
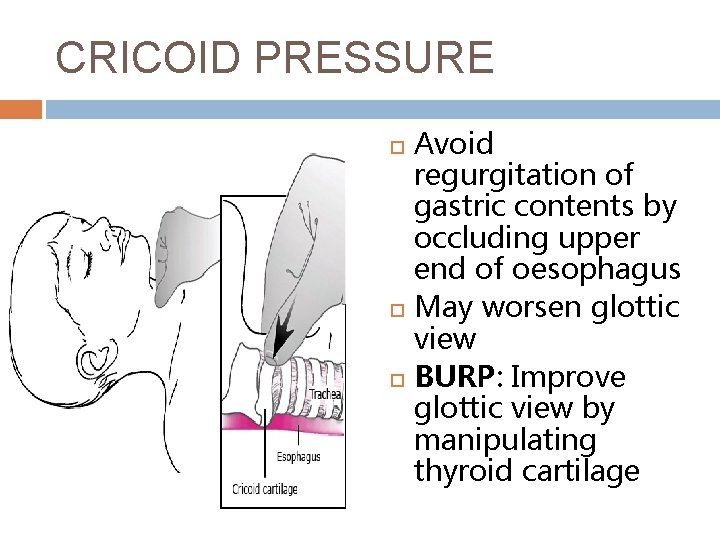
CRICOID PRESSURE Avoid regurgitation of gastric contents by occluding upper end of oesophagus May worsen glottic view BURP: Improve glottic view by manipulating thyroid cartilage
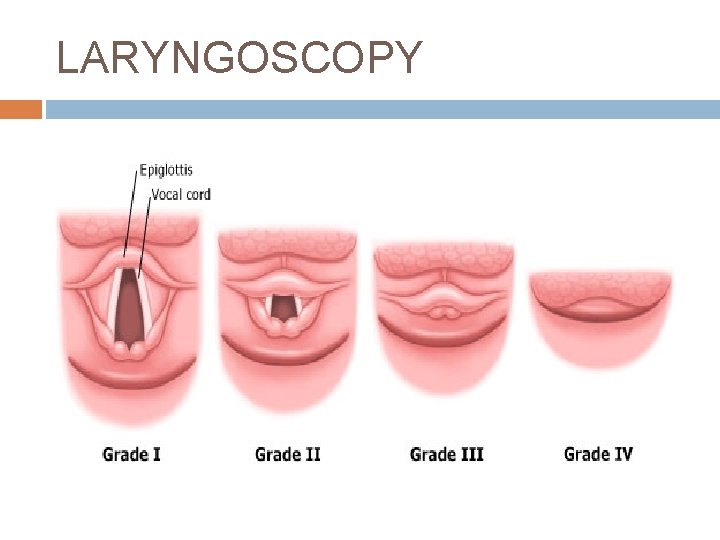
LARYNGOSCOPY
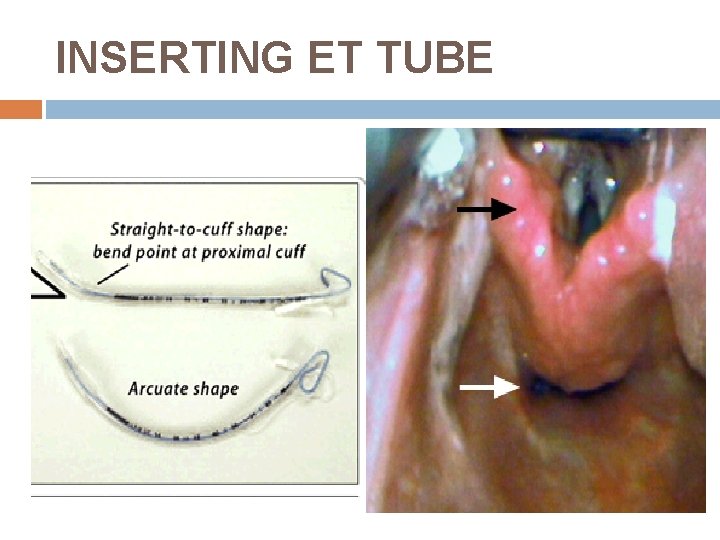
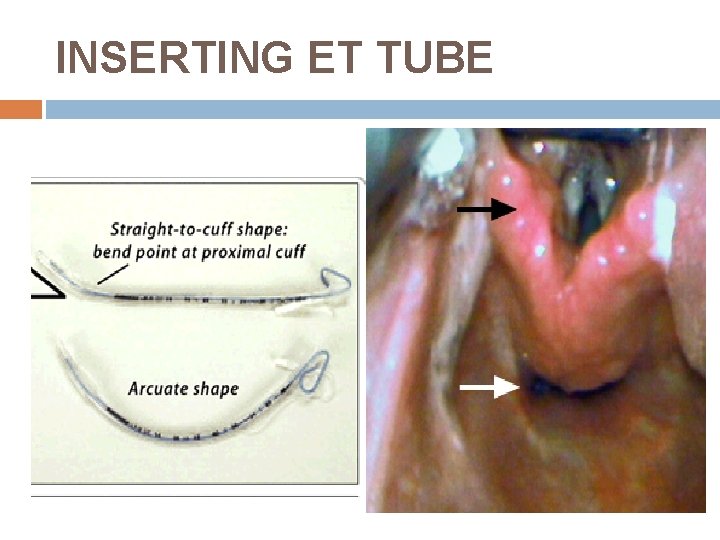
INSERTING ET TUBE
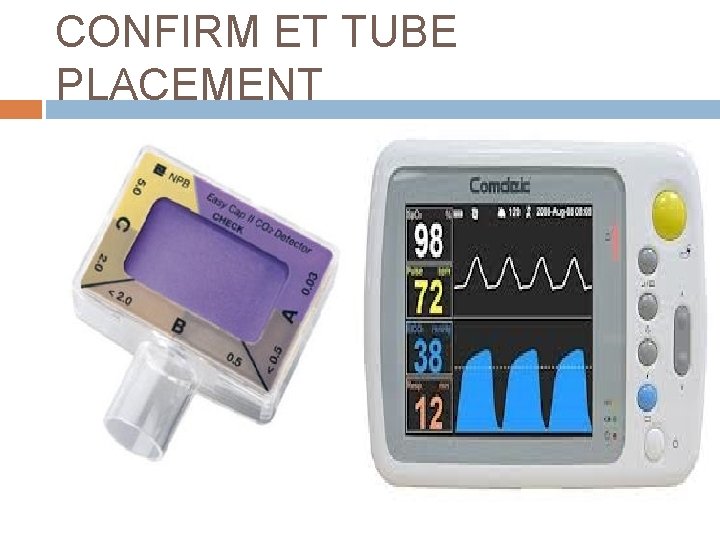
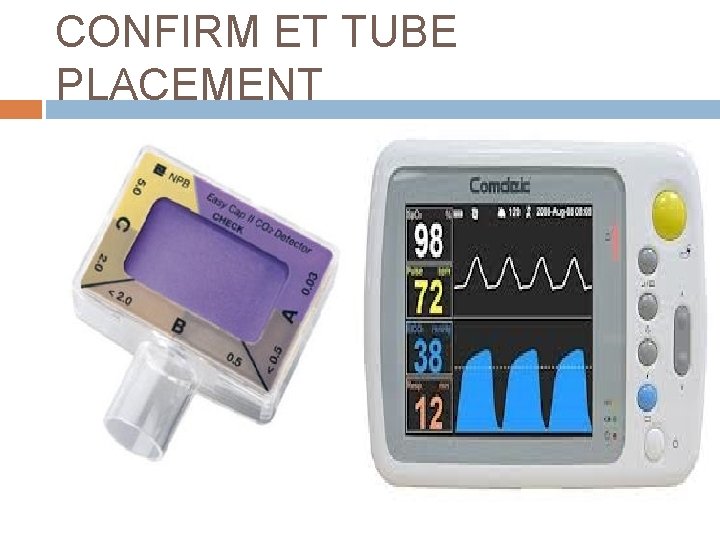
CONFIRM ET TUBE PLACEMENT
AIRWAY ADJUNCTS BOUGIE VIDEO LARYNGOSCOPE LMA CRICOTHYROID CANNULA SURGICAL CRICOTHYROIDOTOMY KIT
BOUGIE
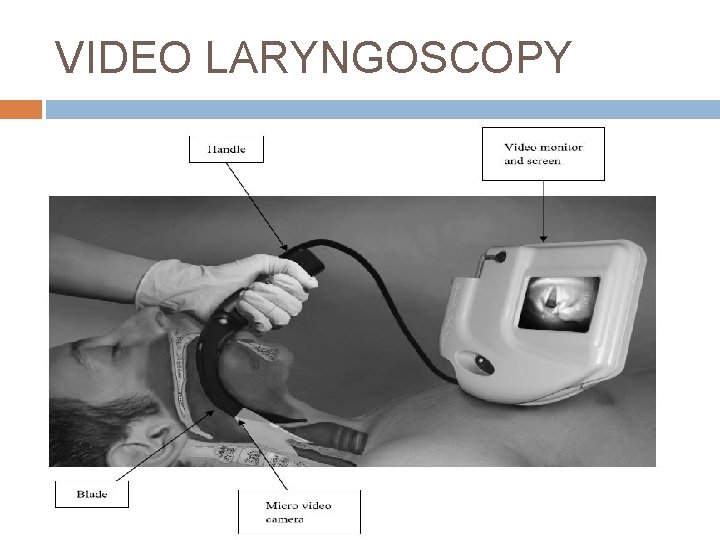
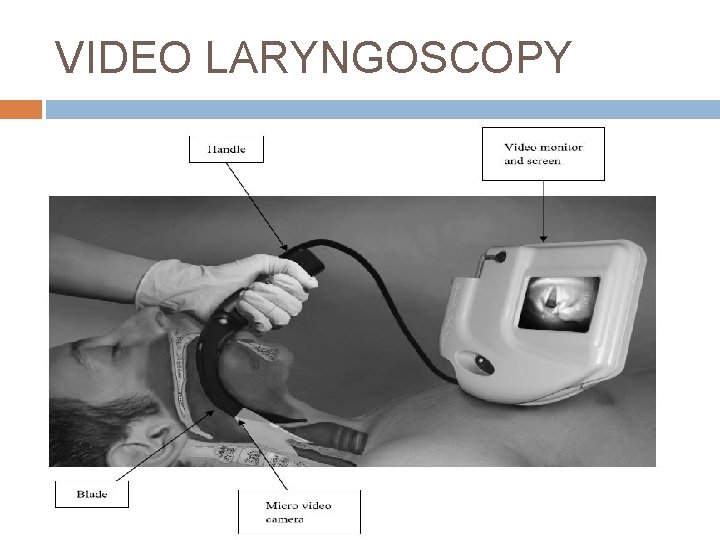
VIDEO LARYNGOSCOPY

VIDEO LARYNGOSCOPES GLIDESCOPE

VIDEO LARYNGOSCOPES C-MAC

LMAs CLASSIC LMA INTUBATING LMA/FASTRACK
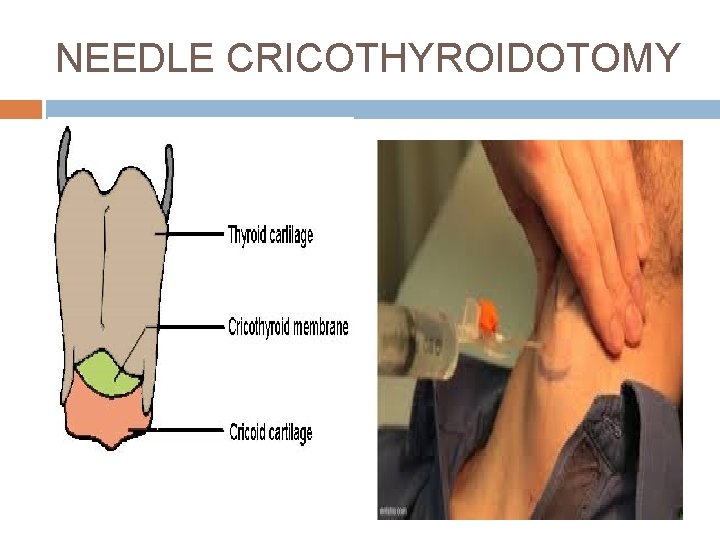
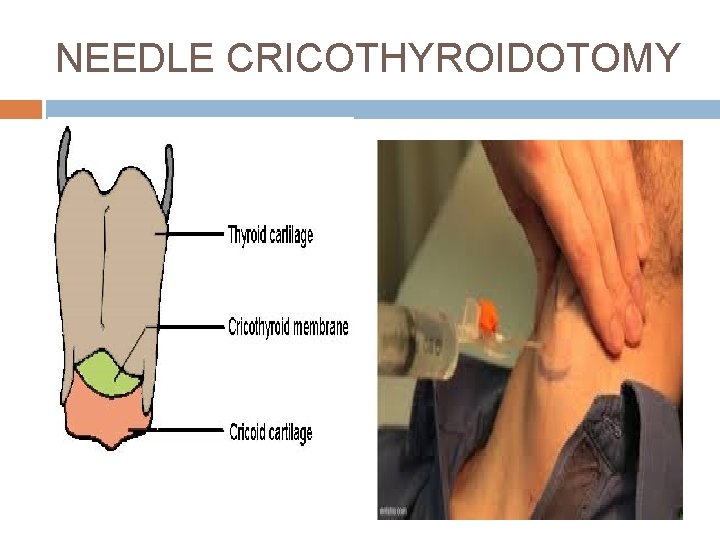
NEEDLE CRICOTHYROIDOTOMY
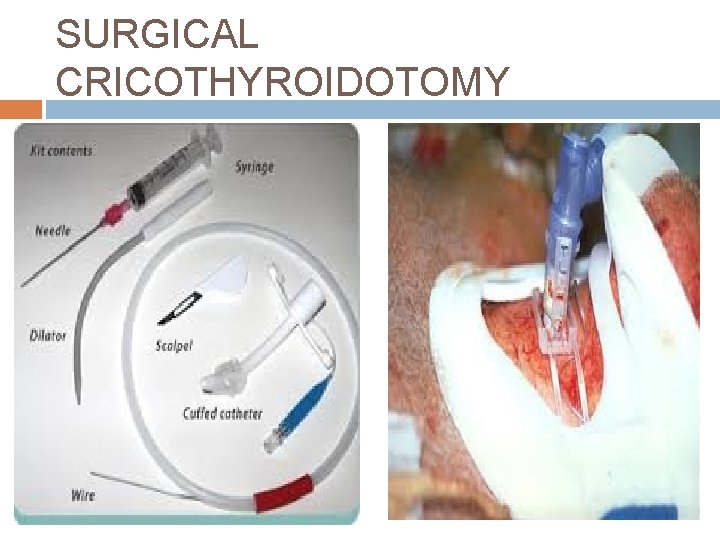
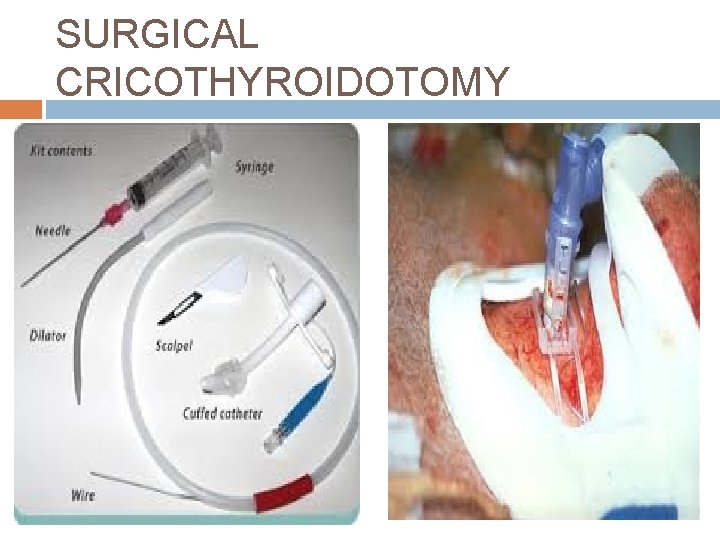
SURGICAL CRICOTHYROIDOTOMY
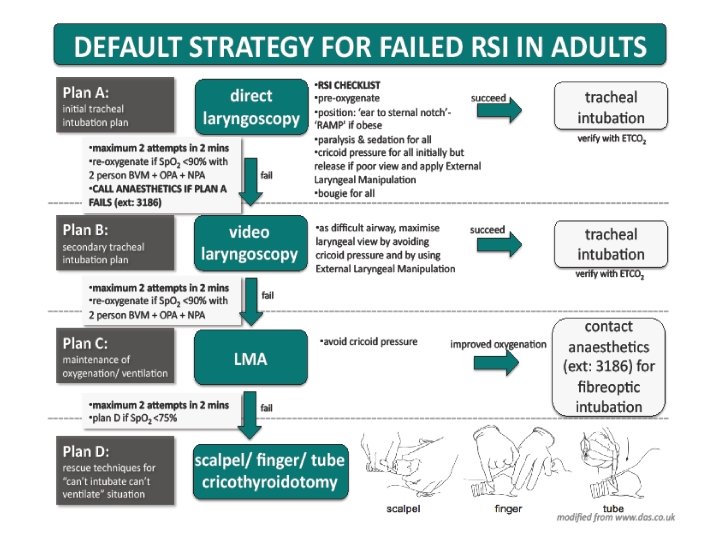
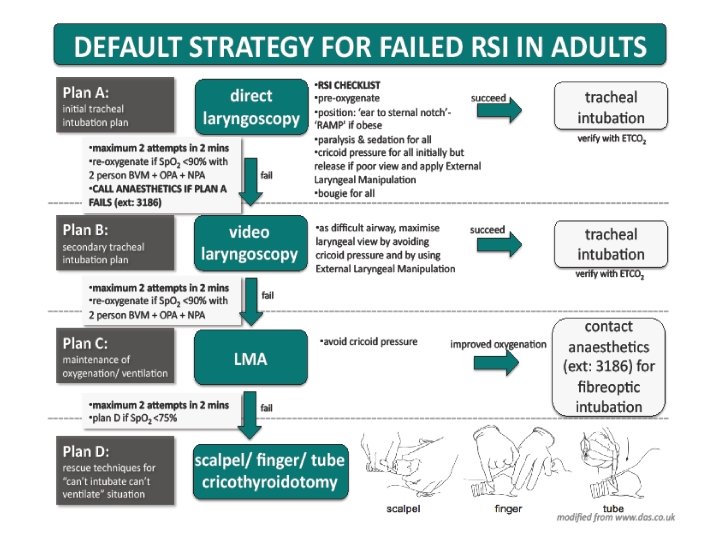
THE PLAN AND BACK UP PLANS. . .
REFERENCES Critical care medicine. 2008; 36(7): 2163 -2173 Anaesthesiology. 2013; 118: Practice guidelines for manangement of the difficult airway Critical care and resuscitation. 2003; 5: 43 -52 Endotracheal intubation in ICU by Dr D Oxman 2013