The Continuum of Care An Approach to Therapy







- Slides: 33
The Continuum of Care: An Approach to Therapy for the Patient With an Amputation Dr. Lynn Geyer, DPT Covenant Health. Care Physical Medicine and Rehabilitation April 23, 2016 Neuro Symposium

130, 000+ amputations occur yearly in the United States Standards of care recommend that people with amputations be in contact with at least one professional from their healthcare team every 3 months for the first 18 months post amputation, and then every 6 months in order to reach their full potential

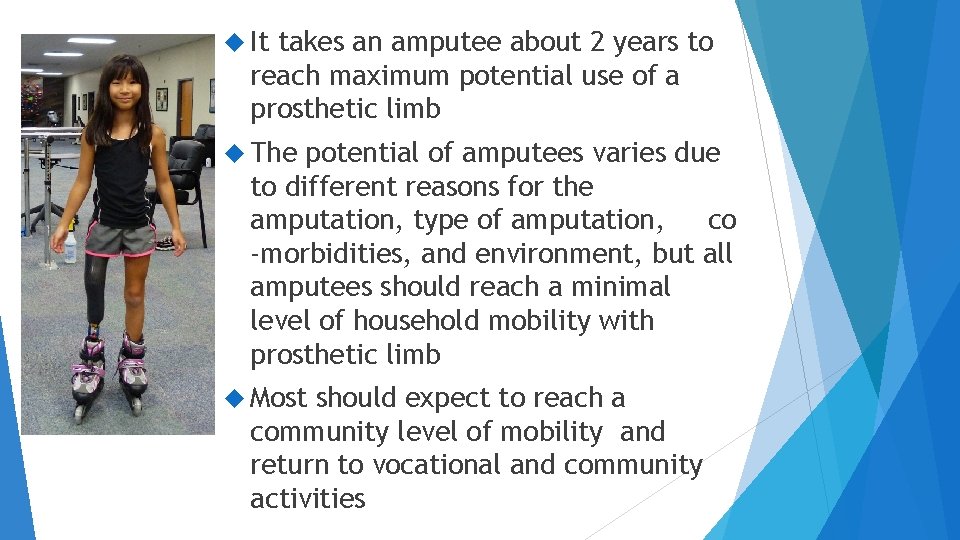
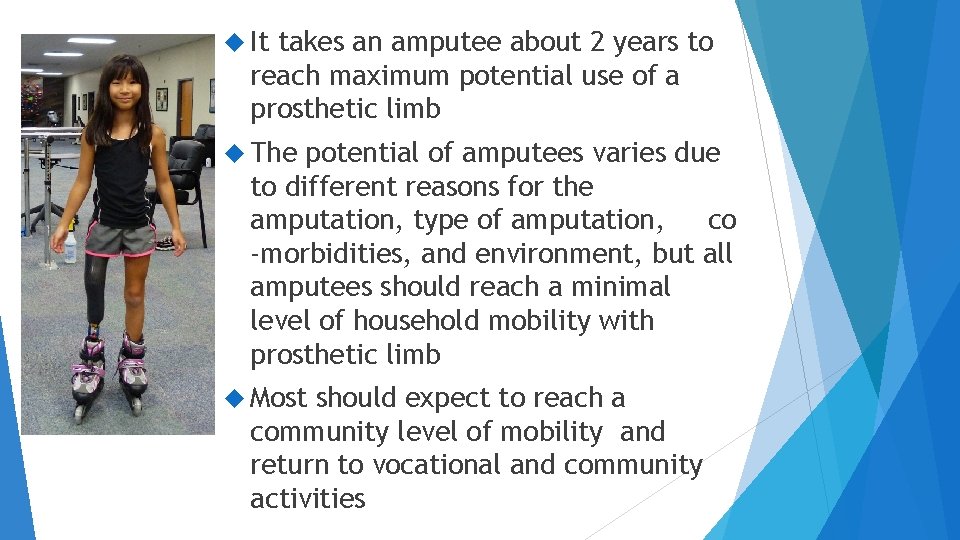
It takes an amputee about 2 years to reach maximum potential use of a prosthetic limb The potential of amputees varies due to different reasons for the amputation, type of amputation, co -morbidities, and environment, but all amputees should reach a minimal level of household mobility with prosthetic limb Most should expect to reach a community level of mobility and return to vocational and community activities
Mobility Potential Most amputees will start in a wheelchair, but can quickly be up and moving in a walker with or without a prosthetic leg within a few weeks of amputation All amputees should be expected to reach a minimum of household ambulation and should never be expected to be wheelchair bound
Prosthetic Limbs After an amputation, you should expect to receive and start using a prosthetic limb within 1 -2 months, some may begin as soon as 1 week

Who’s Who of Amputee Care Primary Care Physician – Family physician Physiatrist – Physical Medicine and Rehabilitation physician Physical Therapist – Specialist in lower extremity amputee and neurology therapy Prosthetist – Creator of prosthetic limb Case Management/Social Worker – Community resources Wound Clinic – Care of the residual limb and any other wound/skin issues Pain Clinic – Physicians who specialize in pain management Psychology – Psychologist or Psychiatrist Dietician – Specialist in food education

Stages of Rehabilitation Preoperative Acute Stage Sub-Acute to Chronic Stage Community Integration/Stable Stage
Preoperative Stage For those patients who have a planned amputation Rehabilitation through physical therapy and/or cardiac rehabilitation Education for the surgery, prosthetic, goals for mobility
Preoperative Stage, continued Healthcare professionals the patient should be in contact with Primary Care Physician Surgeon Prosthetic Physical Company/Prosthetist Therapist or Cardiac Rehab Unit

Acute Stage Amputation Therapy occurs in the hospital Discharge plan to home or another rehabilitation facility
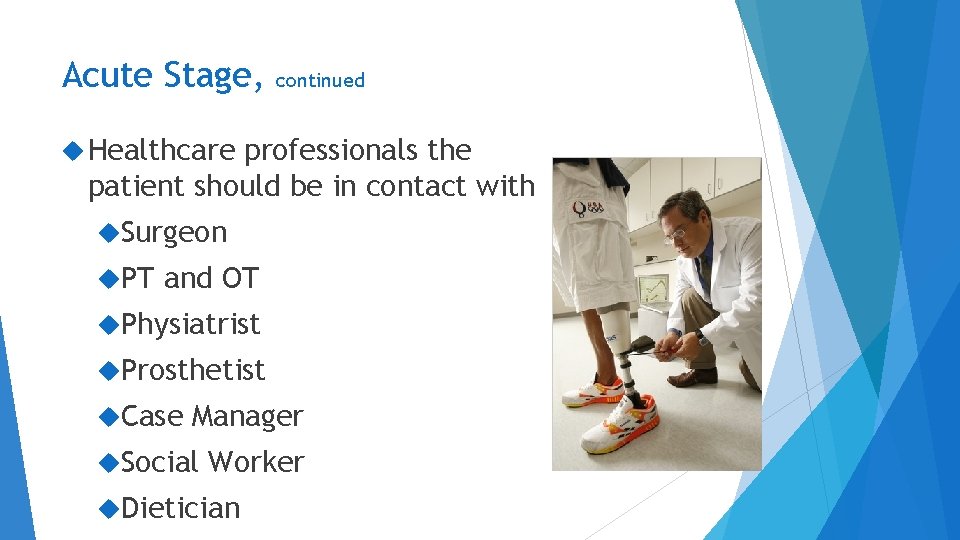
Acute Stage, continued Healthcare professionals the patient should be in contact with Surgeon PT and OT Physiatrist Prosthetist Case Manager Social Worker Dietician
Sub-Acute to Chronic Stage Time frame: Patient discharges from the hospital throughout outpatient therapy needs Therapy setting ideally at discharge from the hospital would be an inpatient rehabilitation unit, can also be a skilled nursing rehabilitation unit Discharge could also be to home with home therapy or home with outpatient therapy Receive a prosthetic limb and begin to use
Sub-Acute to Chronic Stage, continued Healthcare professionals the patient should be in contact with Surgeon Physical and Occupational Therapists Physiatrist Prosthetist Case Manager/Social Worker Psychology Dietician if diet needs monitored or changed Wound Center
Sub-Acute to Chronic Stage, continued Prosthetic During this time, the prosthetic limb will begin with a temporary/preparatory limb Over time the prosthetic limb will be upgraded to an improved temporary and eventually a permeant limb Many factors involved with decisions in prosthetic available
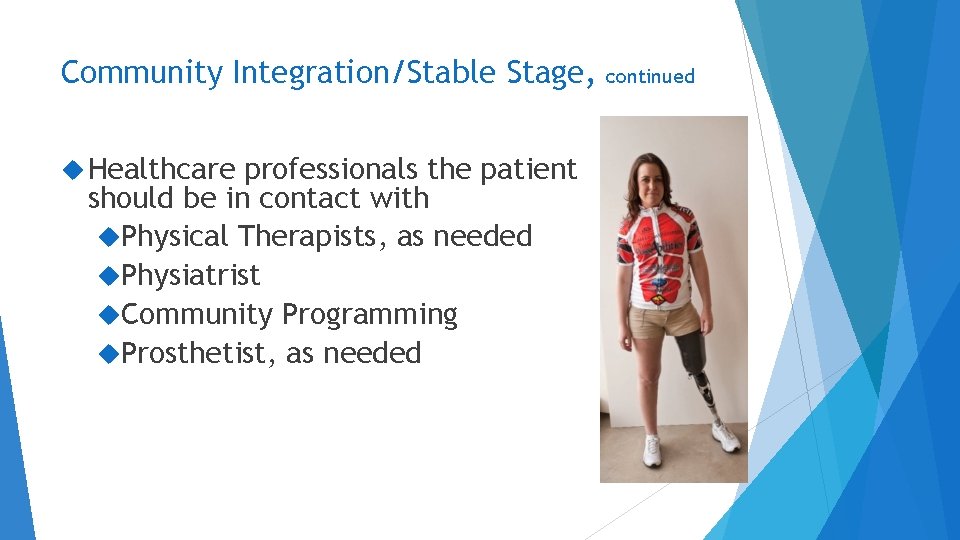
Community Integration/Stable Stage Return to work, recreational activities May still be completing outpatient therapy with physical therapy or may be only completing a home exercise or gym program Community programs available to assist with maintaining progress and continuing to make progress
Community Integration/Stable Stage, Healthcare professionals the patient should be in contact with Physical Therapists, as needed Physiatrist Community Programming Prosthetist, as needed continued

Amputee Mobility Predictor
K Levels Medicare Functional Classification Level for LE amputations 5 level system categorizes the mobility potential and abilities of a person at time of testing Defines reimbursement and availability for a prosthetic prescription Measured by use of the Amputee Mobility Predictor Test K Levels can be used to judge progress throughout an episode of care and to update a prosthetic limb to include more technology and improved components
K Levels K Level 0: Cannot use a prosthetic, nor transfer and walk K Level 1: Household Ambulator K Level 2: Limited Community Ambulator K Level 3: Community Ambulator K Level 4: Advanced Ambulator
K Level 1 “Household Ambulator” Ability or potential to use a prosthetic Transfers Ambulation on level surfaces at fixed cadence
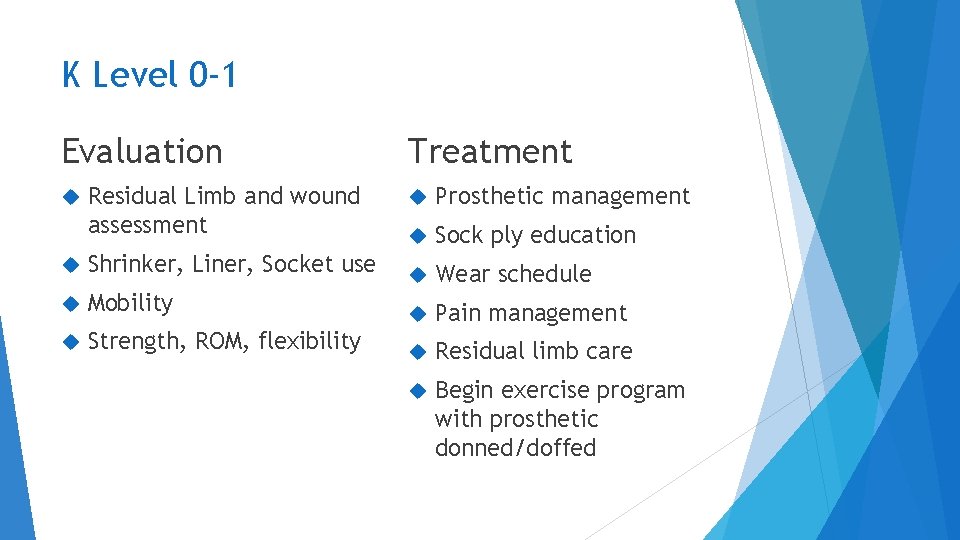
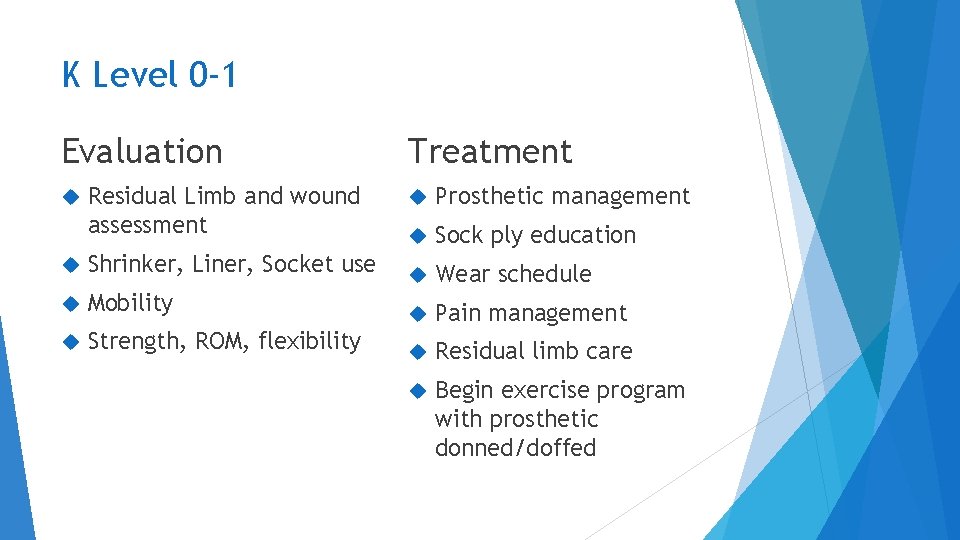
K Level 0 -1 Evaluation Residual Limb and wound assessment Treatment Prosthetic management Sock ply education Shrinker, Liner, Socket use Wear schedule Mobility Pain management Strength, ROM, flexibility Residual limb care Begin exercise program with prosthetic donned/doffed
K Level 2 “Limited Community Ambulator” Has ability or potential for ambulation over low level environmental barriers Curbs Stairs Uneven surfaces Minimal change in speed
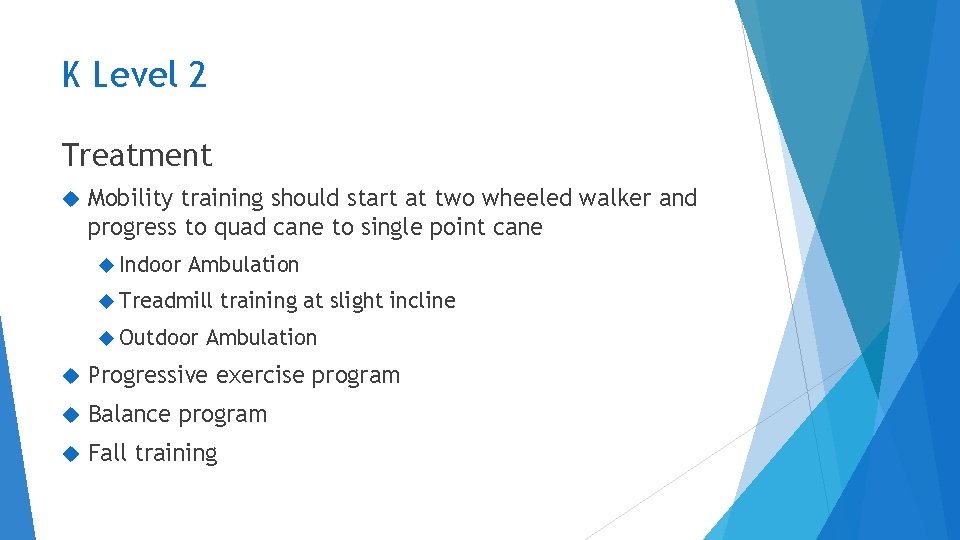
K Level 2 Treatment Mobility training should start at two wheeled walker and progress to quad cane to single point cane Indoor Ambulation Treadmill Outdoor training at slight incline Ambulation Progressive exercise program Balance program Fall training
K Level 3 “Unlimited Community Ambulator” Ambulate most environmental barriers Demands of prosthetic use beyond simple locomotion Ambulates at various speeds
K Level 3 Mobility training should be progressing towards no assistive device Treadmill training with more incline Outdoor Ambulation Balance and weight shifting exercises
K Level 4 High Level Exceeds basic ambulation skills High impact, stress, and energy levels
K Level 4 Jumping Running High level balance, sports Gym progression Progression towards the CHAMP testing tool
Goals for a person with an amputation should include the person becoming as independent as possible, maximizing mobility, and improving quality of life With standards of care applied and many referrals made to help the person progress, these goals should be attained
Covenant Health. Care References Covenant Health. Care Physiatrists Dr. Babu Nahata (director) Dr. Thomas Raymond Covenant Health. Care Physical Medicine and Rehabilitation Amputee Specialists Michigan Outpatient PMR at the 515 N. Michigan Campus (989) 583 -2752 Physical Therapy, Occupational Therapy, and Speech Therapy Post Acute/Hospital Rehabilitation at the Michigan Campus Covenant Transitional Care Unit Covenant Inpatient Rehabilitation Step Up! Amputee Mobility Clinic 2 nd Thursday of the month during specified months Free Clinic for anyone with or who wants to know more about amputee mobility

Questions?