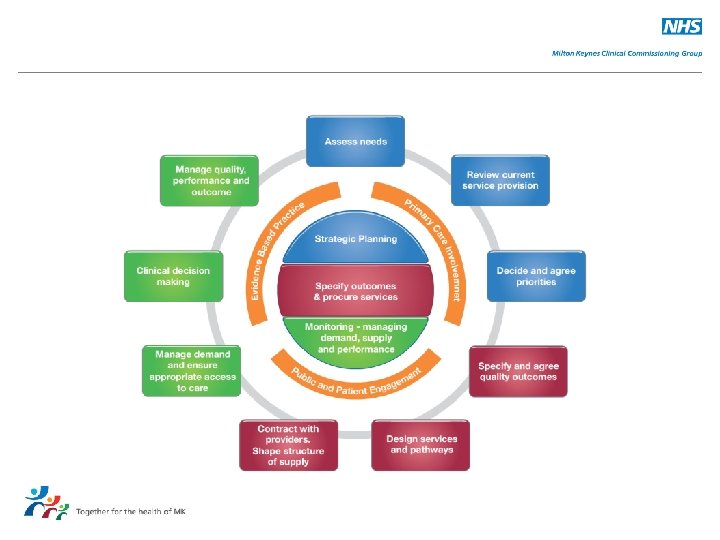
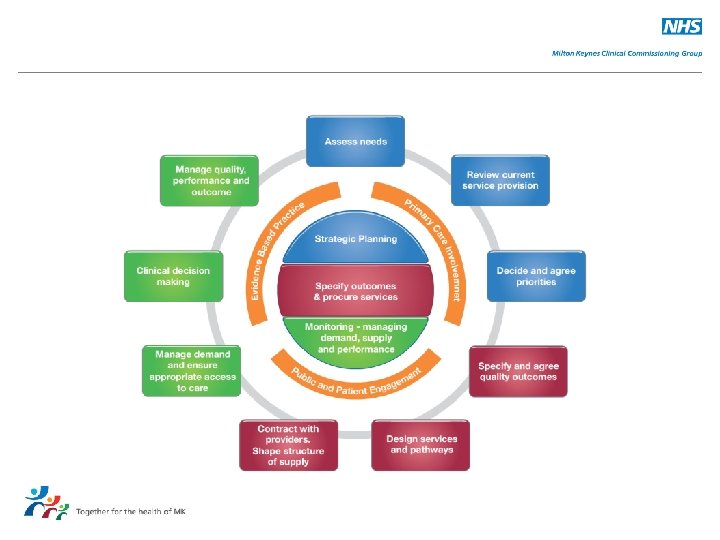
The Commissioning Cycle The Commissioning Cycle The steps
- Slides: 24
The Commissioning Cycle
The Commissioning Cycle The steps: • • • Needs assessment Service provision review Priorities Quality outcomes Design services / pathways Providers/suppliers Demand management Clinical decision making Manage performance and outcomes Underpinned by: • Primary care involvement • Public and Patient engagement • Evidence based practice
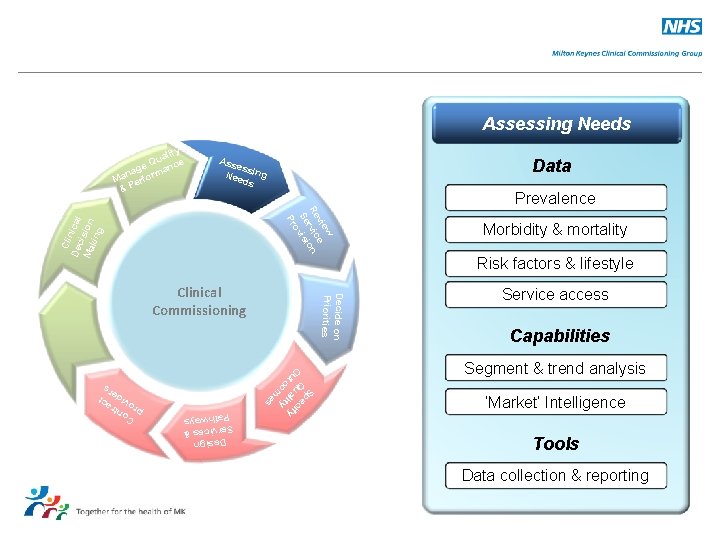
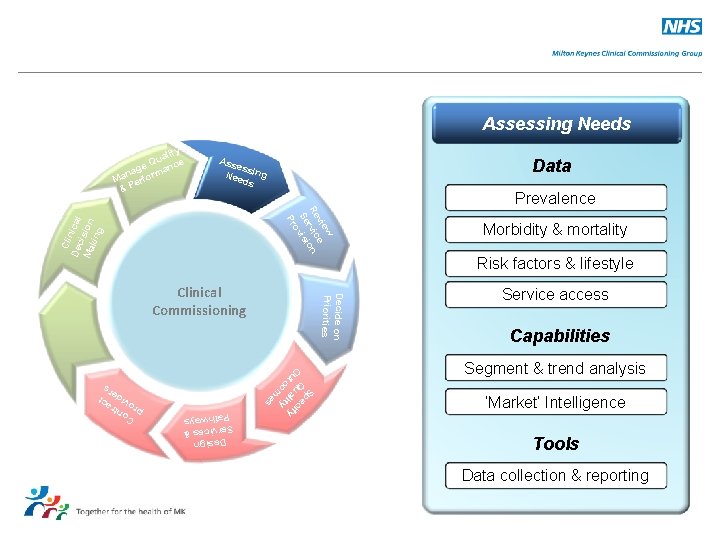
Assessing Needs ity ual e Q e nc nag ma Ma erfor &P Ass ess Nee ing ds Data Prevalence Cli De nical c Ma ision kin g w vie e Re vic ion r Se vis o Pr Sp O Q ec ut ual ify co ity m es Design & Services Pathways ge Mana nd a Dem Decide on Priorities Clinical Commissioning Morbidity & mortality Risk factors & lifestyle Service access Capabilities Segment & trend analysis ‘Market’ Intelligence Tools Data collection & reporting C pr ontr o a v ide ct rs
What is needs assessment? Needs assessment identifies and strives to eliminate overuse, misuse and underuse of healthcare resources • A variety of comprehensive evidence sources can be used that include, but are not limited to the following: • • • • Local knowledge of clinicians, health care providers, commissioners Local Authorities Practice based commissioning data Prescribing data Prevalence and incidence data Community health profiles Housing data Inpatient and outpatient data Lifestyle data Educational attainment data Deprivation indices Views of patients/service users Census and other demographic data Referral data • • Joint Strategic needs Assessments (JSNAs) are local assessments of current and future health and social care needs that could be met by the local authority, CCGs, or the NHS CB JSNAs and the Joint Health and Wellbeing Strategy is produced by health and wellbeing boards to set priorities for future action.
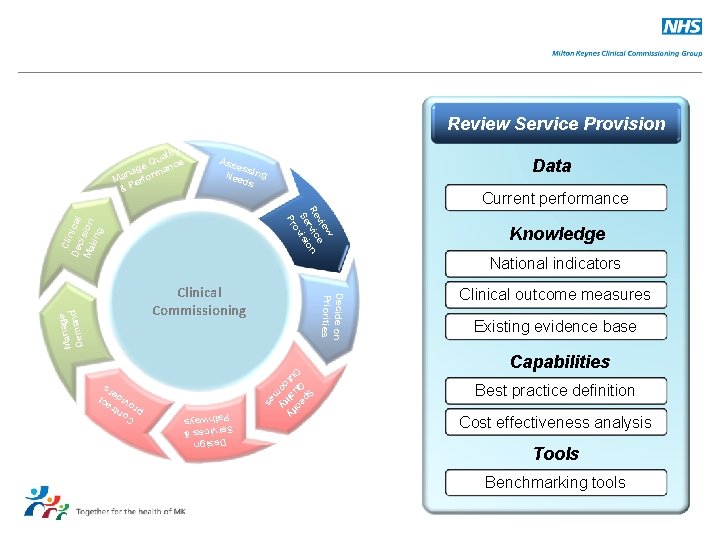
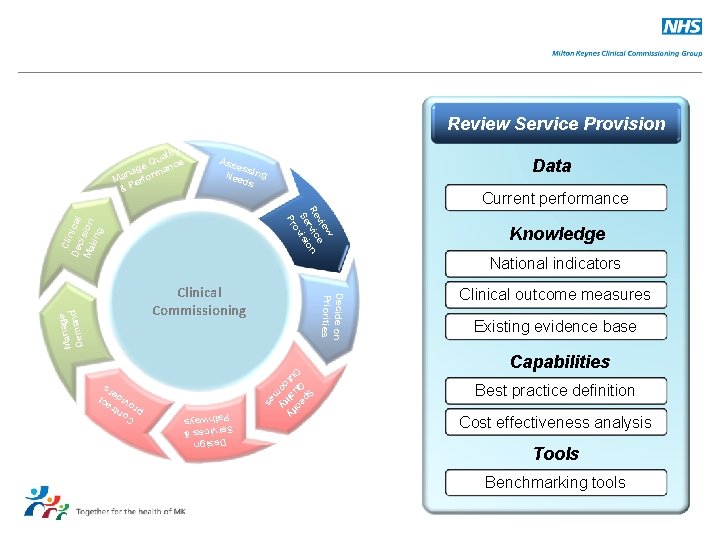
Review Service Provision ity ual e Q e nc nag ma Ma erfor &P Ass ess Nee ing ds Data Current performance Cli De nical c Ma ision kin g w vie e Re vic ion r Se vis o Pr Sp O Q ec ut ual ify co ity m es Design & Services Pathways ge Mana nd a Dem Decide on Priorities Clinical Commissioning Knowledge National indicators Clinical outcome measures Existing evidence base Capabilities Best practice definition Cost effectiveness analysis Tools Benchmarking tools C pr ontr o a v ide ct rs
Review current service provision • • Service reviews are undertaken to demonstrate a thorough understanding of current services provided in relation to the identified health needs. In essence, it is to ensure that services commissioned for the population are effective and of high quality. Key tasks to be considered as part of a service review include: – Understanding the operational delivery, workforce issues and clinical factors for the service – Developing knowledge of clinical effectiveness and evidence base – Benchmarking service against national or other indicators to access efficiency – Reviewing applicable performance indicators or monitoring clinical outcomes – Reviewing user experience and satisfaction with the service – Establish best practice clinical/public health guidelines for the service
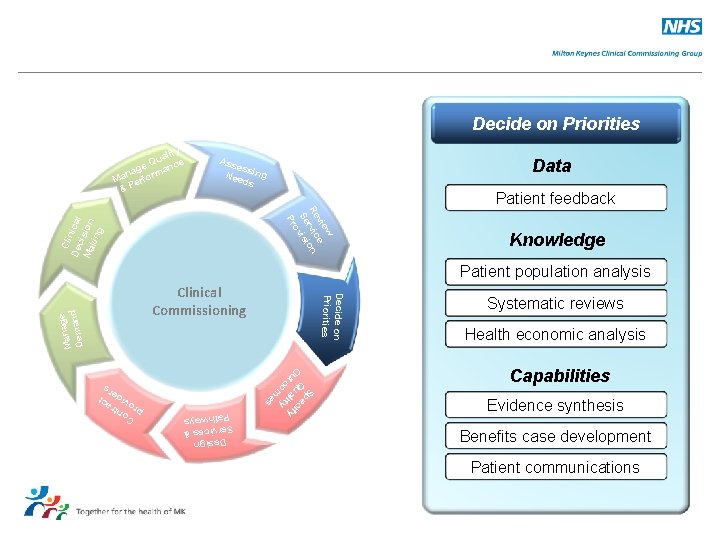
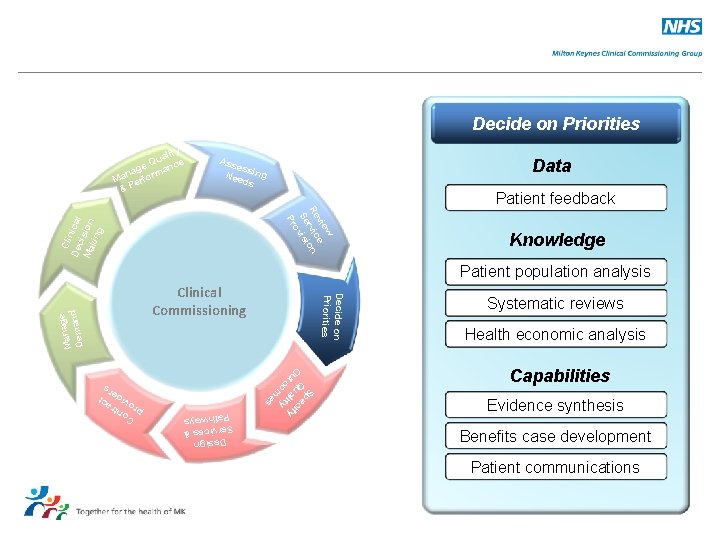
Decide on Priorities ity ual e Q e nc nag ma Ma erfor &P Ass ess Nee ing ds Data Patient feedback Cli De nical c Ma ision kin g w vie e Re vic ion r Se vis o Pr Knowledge Patient population analysis Sp O Q ec ut ual ify co ity m es Design & Services Pathways ge Mana nd a Dem Decide on Priorities Clinical Commissioning Systematic reviews Health economic analysis Capabilities Evidence synthesis Benefits case development Patient communications C pr ontr o a v ide ct rs
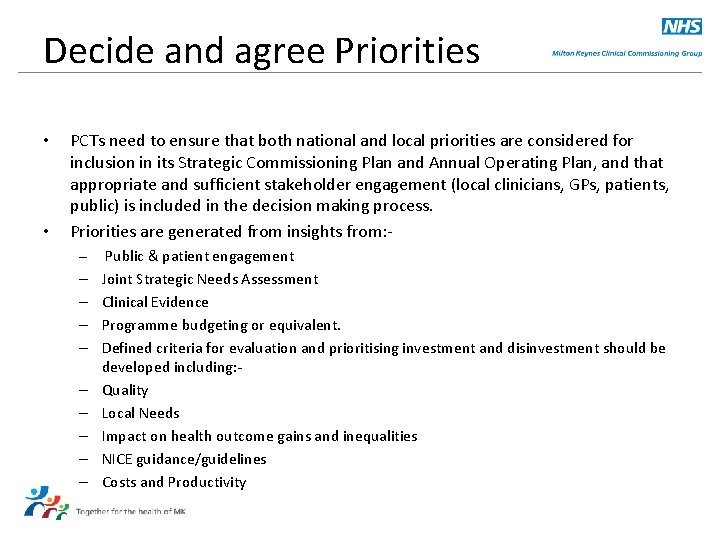
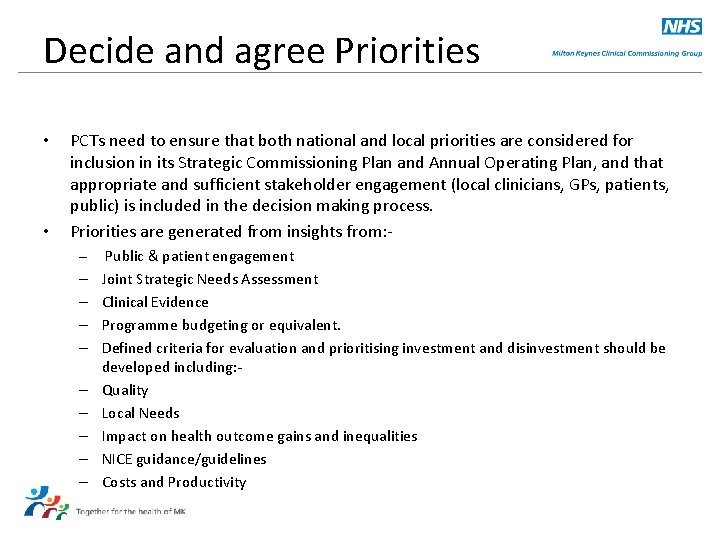
Decide and agree Priorities • • PCTs need to ensure that both national and local priorities are considered for inclusion in its Strategic Commissioning Plan and Annual Operating Plan, and that appropriate and sufficient stakeholder engagement (local clinicians, GPs, patients, public) is included in the decision making process. Priorities are generated from insights from: – Public & patient engagement – – – – – Joint Strategic Needs Assessment Clinical Evidence Programme budgeting or equivalent. Defined criteria for evaluation and prioritising investment and disinvestment should be developed including: Quality Local Needs Impact on health outcome gains and inequalities NICE guidance/guidelines Costs and Productivity
Specify Quality Outcomes ity ual e Q e nc nag ma Ma erfor &P Ass ess Nee ing ds Data Current Achievement Cli De nical c Ma ision kin g w vie e Re vic ion r Se vis o Pr Knowledge Benefits case Sp O Q ec ut ual ify co ity m es Design & Services Pathways ge Mana nd a Dem Decide on Priorities Clinical Commissioning Existing outcome measures National quality indicators Capabilities Outcome measure design Audit design C pr ontr o a v ide ct rs
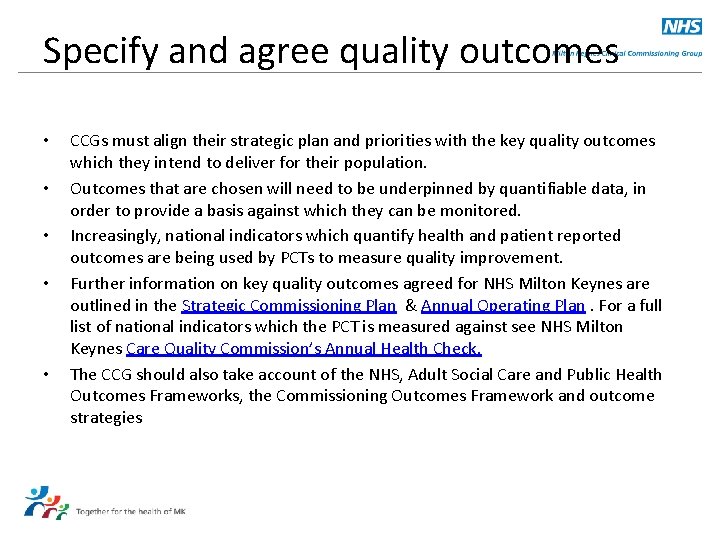
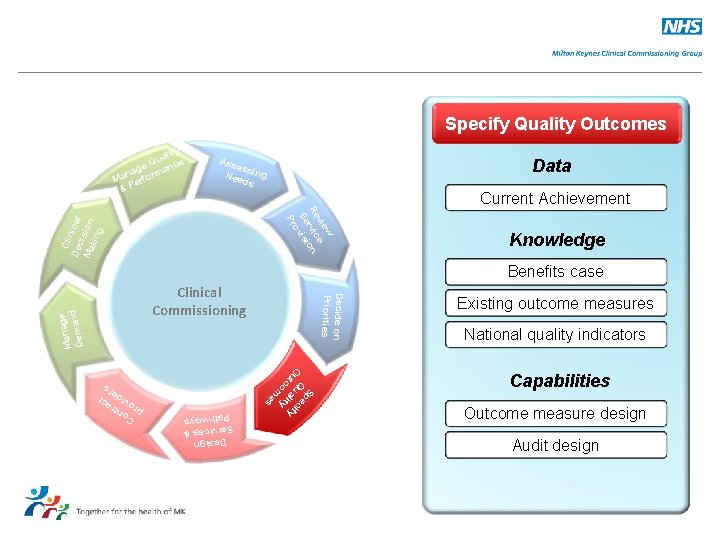
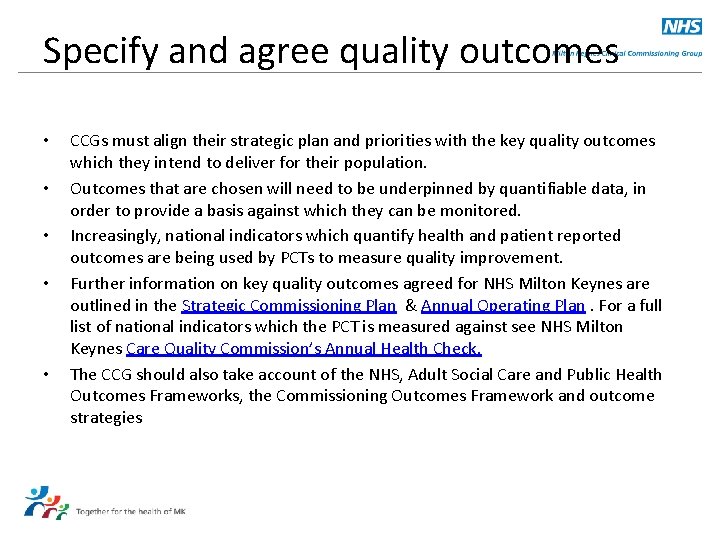
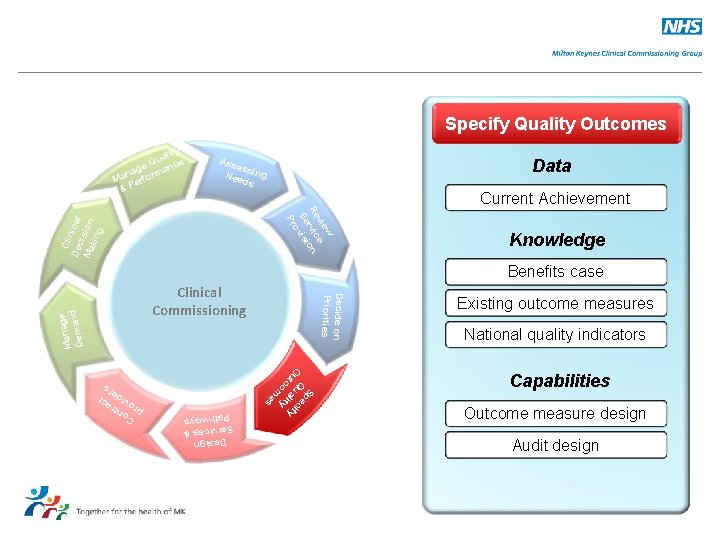
Specify and agree quality outcomes • • • CCGs must align their strategic plan and priorities with the key quality outcomes which they intend to deliver for their population. Outcomes that are chosen will need to be underpinned by quantifiable data, in order to provide a basis against which they can be monitored. Increasingly, national indicators which quantify health and patient reported outcomes are being used by PCTs to measure quality improvement. Further information on key quality outcomes agreed for NHS Milton Keynes are outlined in the Strategic Commissioning Plan & Annual Operating Plan. For a full list of national indicators which the PCT is measured against see NHS Milton Keynes Care Quality Commission’s Annual Health Check. The CCG should also take account of the NHS, Adult Social Care and Public Health Outcomes Frameworks, the Commissioning Outcomes Framework and outcome strategies
Design Service & Pathway ity ual e Q e nc nag ma Ma erfor &P Ass ess Nee ing ds Knowledge Existing pathways Cli De nical c Ma ision kin g w vie e Re vic ion r Se vis o Pr ge Mana nd a Dem Decide on Priorities Clinical Commissioning Evidence synthesis Evidence summaries for single interventions HTAs Capabilities Sp O Q ec ut ual ify co ity m es Pathway adaptation Pathway development Guideline enablement Design & Services Pathways C pr ontr o a v ide ct rs
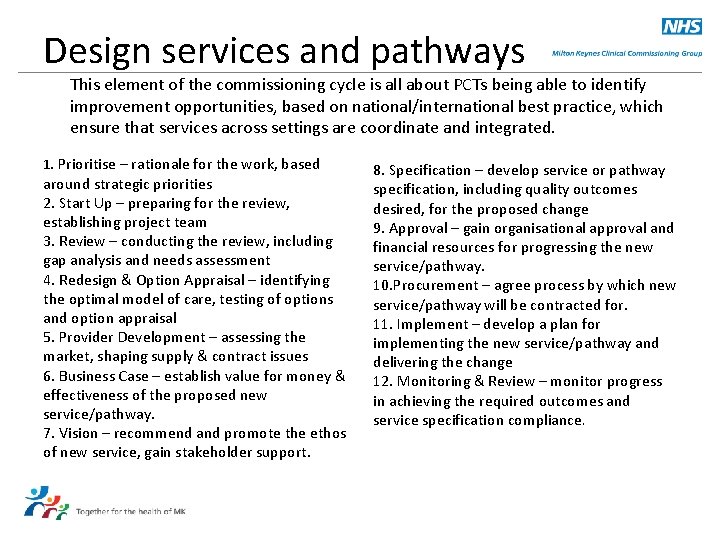
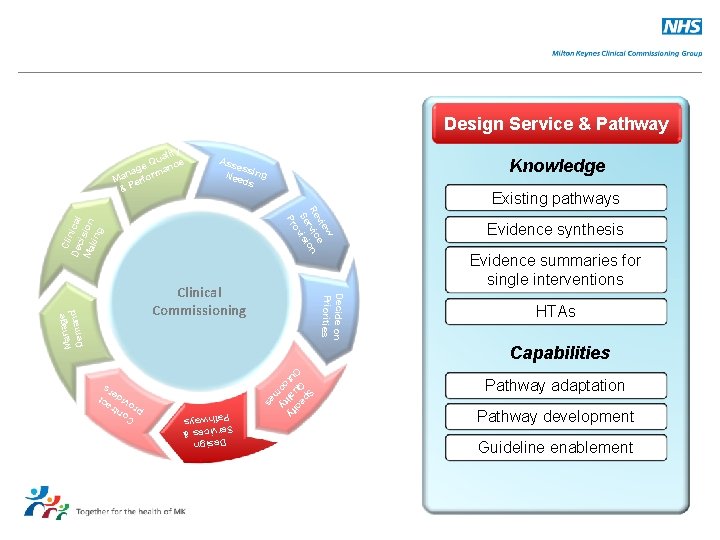
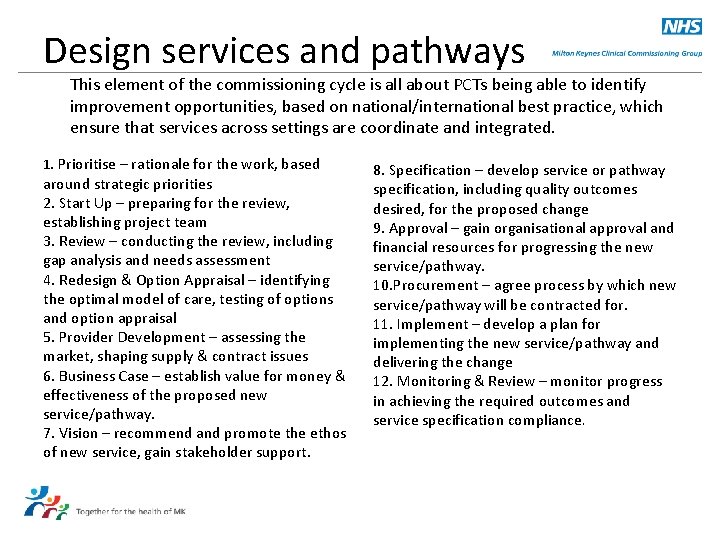
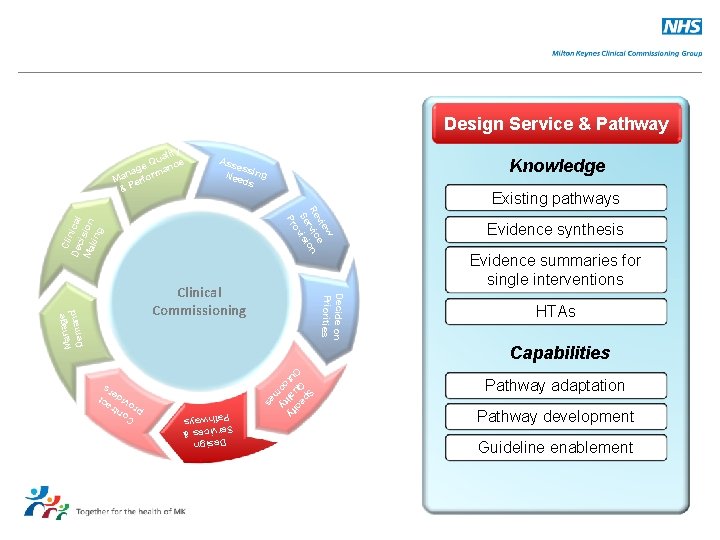
Design services and pathways This element of the commissioning cycle is all about PCTs being able to identify improvement opportunities, based on national/international best practice, which ensure that services across settings are coordinate and integrated. 1. Prioritise – rationale for the work, based around strategic priorities 2. Start Up – preparing for the review, establishing project team 3. Review – conducting the review, including gap analysis and needs assessment 4. Redesign & Option Appraisal – identifying the optimal model of care, testing of options and option appraisal 5. Provider Development – assessing the market, shaping supply & contract issues 6. Business Case – establish value for money & effectiveness of the proposed new service/pathway. 7. Vision – recommend and promote the ethos of new service, gain stakeholder support. 8. Specification – develop service or pathway specification, including quality outcomes desired, for the proposed change 9. Approval – gain organisational approval and financial resources for progressing the new service/pathway. 10. Procurement – agree process by which new service/pathway will be contracted for. 11. Implement – develop a plan for implementing the new service/pathway and delivering the change 12. Monitoring & Review – monitor progress in achieving the required outcomes and service specification compliance.
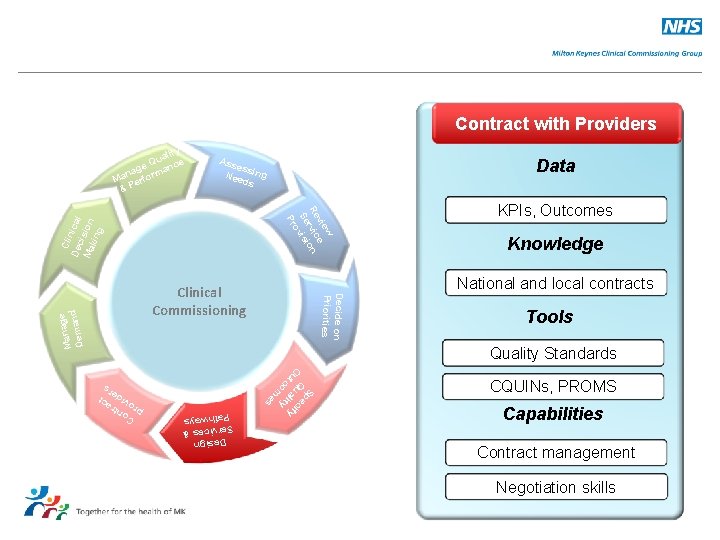
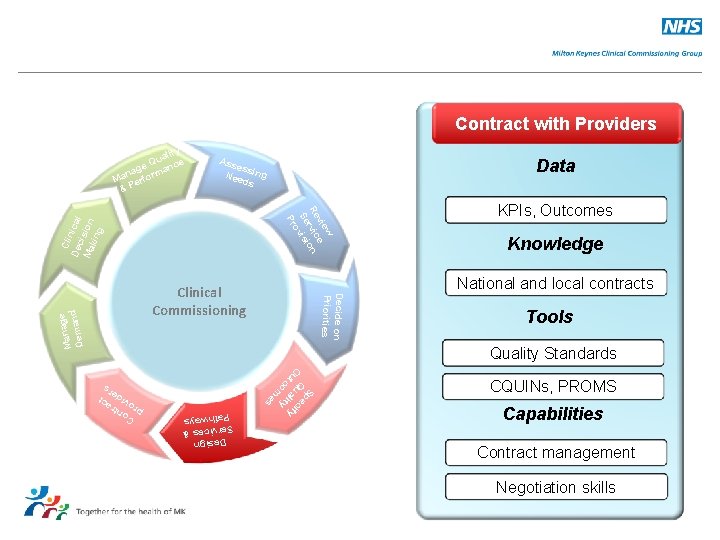
Contract with Providers ity ual e Q e nc nag ma Ma erfor &P Ass ess Nee ing ds Data Cli De nical c Ma ision kin g w vie e Re vic ion r Se vis o Pr Knowledge National and local contracts Decide on Priorities Clinical Commissioning ge Mana nd a Dem KPIs, Outcomes Tools Quality Standards Sp O Q ec ut ual ify co ity m es CQUINs, PROMS Capabilities Contract management Negotiation skills Design & Services Pathways C pr ontr o a v ide ct rs
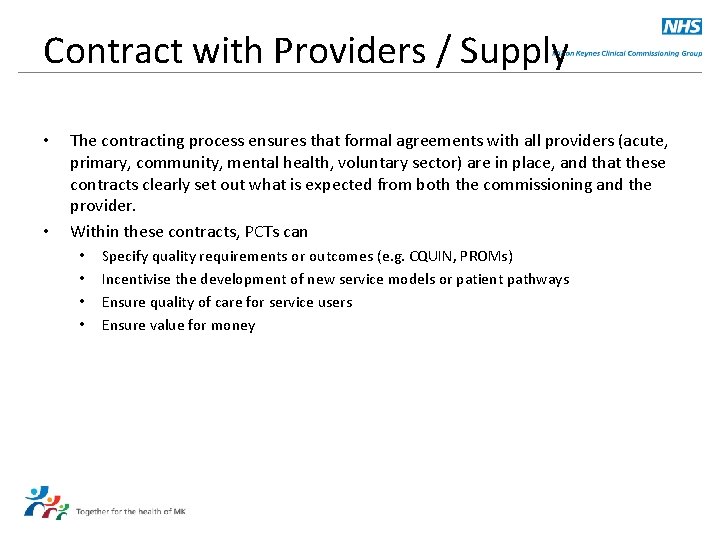
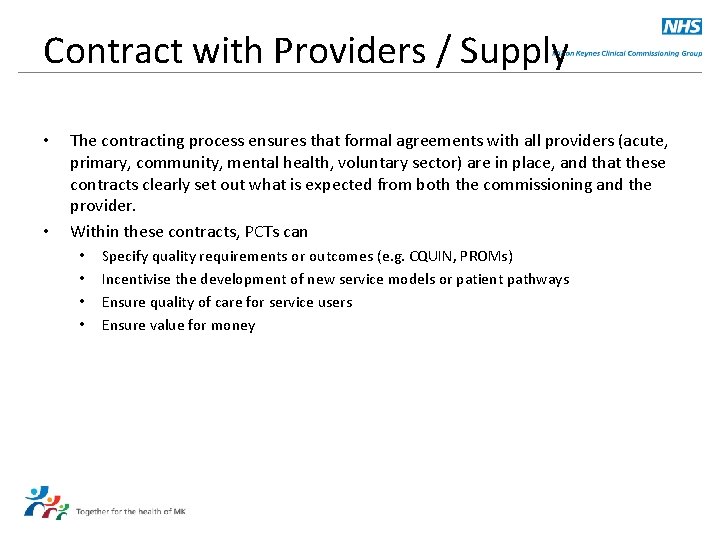
Contract with Providers / Supply • • The contracting process ensures that formal agreements with all providers (acute, primary, community, mental health, voluntary sector) are in place, and that these contracts clearly set out what is expected from both the commissioning and the provider. Within these contracts, PCTs can • • Specify quality requirements or outcomes (e. g. CQUIN, PROMs) Incentivise the development of new service models or patient pathways Ensure quality of care for service users Ensure value for money
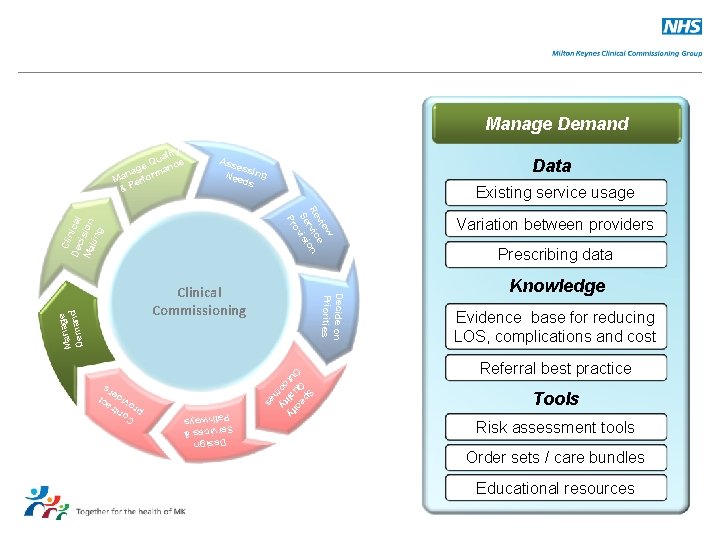
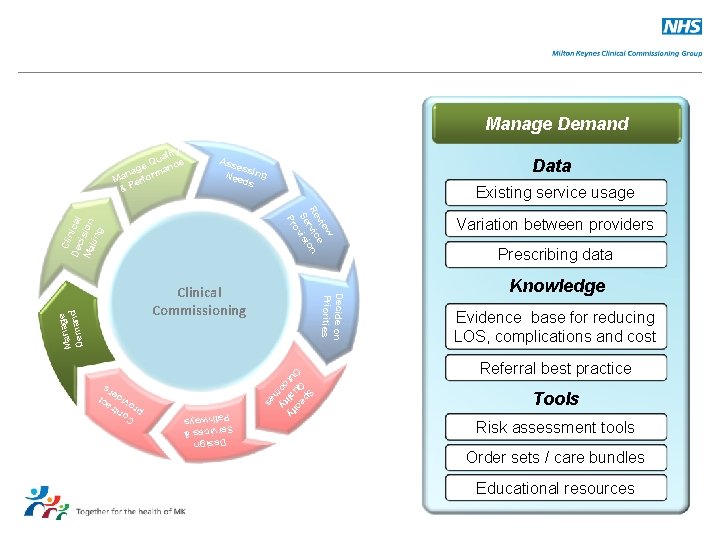
Manage Demand ity ual e Q e nc nag ma Ma erfor &P Ass ess Nee ing ds Data Existing service usage Cli De nical c Ma ision kin g w vie e Re vic ion r Se vis o Pr Sp O Q ec ut ual ify co ity m es Design & Services Pathways ge Mana nd a Dem Decide on Priorities Clinical Commissioning Variation between providers Prescribing data Knowledge Evidence base for reducing LOS, complications and cost Referral best practice Tools Risk assessment tools Order sets / care bundles Educational resources C pr ontr o a v ide ct rs
Manage demand ensure appropriate access to care • • • CCGs will need to have in place a range of responsive providers that they can commission healthcare services from. However, they also need to be able to understand predict current and future demands on those services to ensure that they can accurately predict required future capacity for the population needs identified. Employing their knowledge of future priorities, needs and community aspirations – CCGs can use their role as leader of the local NHS to influence improvement, choice and service design in ways that can best meet future demands.
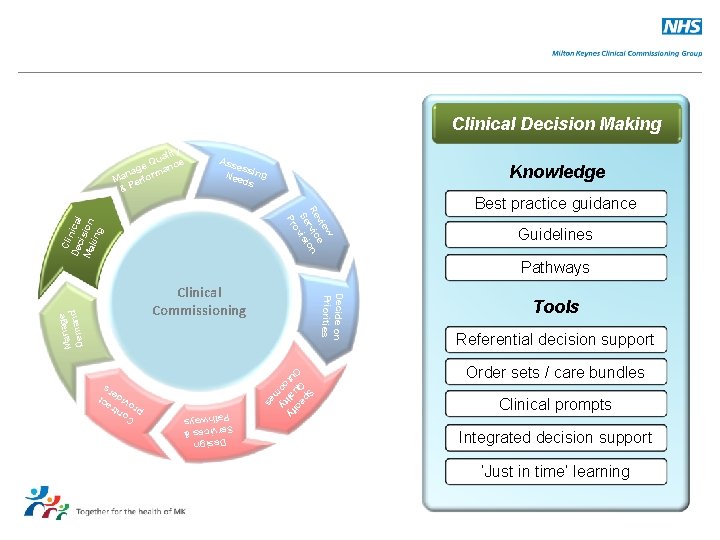
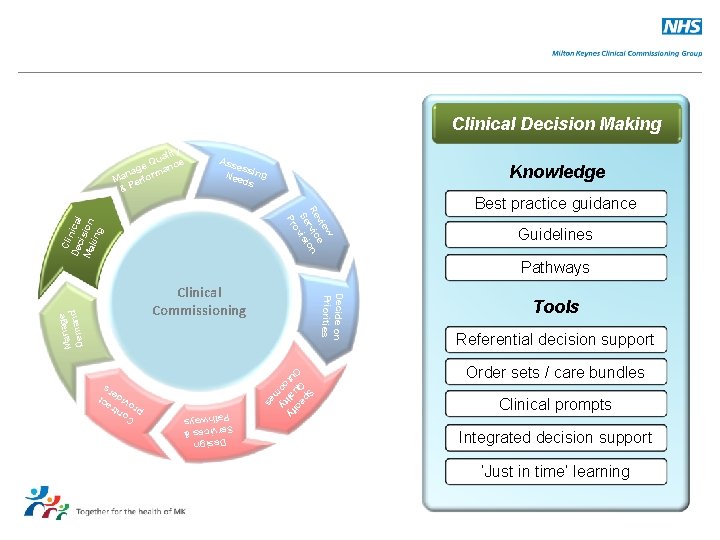
Clinical Decision Making ity ual e Q e nc nag ma Ma erfor &P Ass ess Nee ing ds Knowledge Cli De nical c Ma ision kin g w vie e Re vic ion r Se vis o Pr Guidelines Pathways Decide on Priorities Clinical Commissioning Sp O Q ec ut ual ify co ity m es Design & Services Pathways ge Mana nd a Dem Best practice guidance Tools Referential decision support Order sets / care bundles Clinical prompts Integrated decision support ‘Just in time’ learning C pr ontr o a v ide ct rs
Clinical decision making • The CCG must build a strong framework of clinical involvement in its decision making to ensure that it can: • • • Develop a greater range of more integrated services in community settings Secure great investment for upstream or preventative interventions that keep people healthy for longer, prevent ill health and reduce inequalities Drive continuous quality improvement and innovation across the whole system.
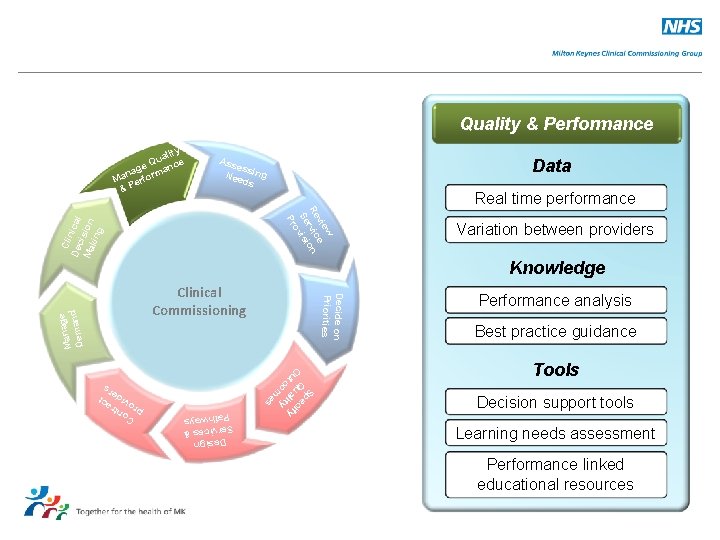
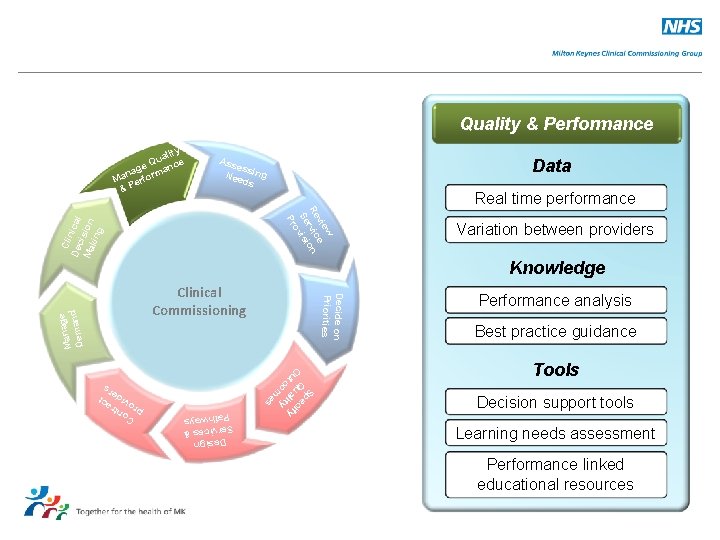
Quality & Performance ity ual e Q e nc nag ma Ma erfor &P Ass ess Nee ing ds Data Real time performance Cli De nical c Ma ision kin g w vie e Re vic ion r Se vis o Pr Knowledge Decide on Priorities Clinical Commissioning Sp O Q ec ut ual ify co ity m es Design & Services Pathways ge Mana nd a Dem Variation between providers Performance analysis Best practice guidance Tools Decision support tools Learning needs assessment Performance linked educational resources C pr ontr o a v ide ct rs
Manage quality, performance & outcome • • • In order to assess whether their strategic goals are being achieved, CCGs need to manage quality and performance of commissioned healthcare effectively. This will involve monitoring and managing the performance of providers against their contracts, including specific quality indicators or key performance indicators. Good data and information sharing systems, plus constructive performance discussions are crucial to this element: – – – Ensuring monthly, quarterly or annual performance reviews are in place as appropriate Clarity as to what checking/ verification is to be done, by whom and how frequently Agreement on what Indicators /KPIs are to be measured, by whom and how frequently. How are the results to be communicated and to whom Who is responsible for following up concerns and in what forums.
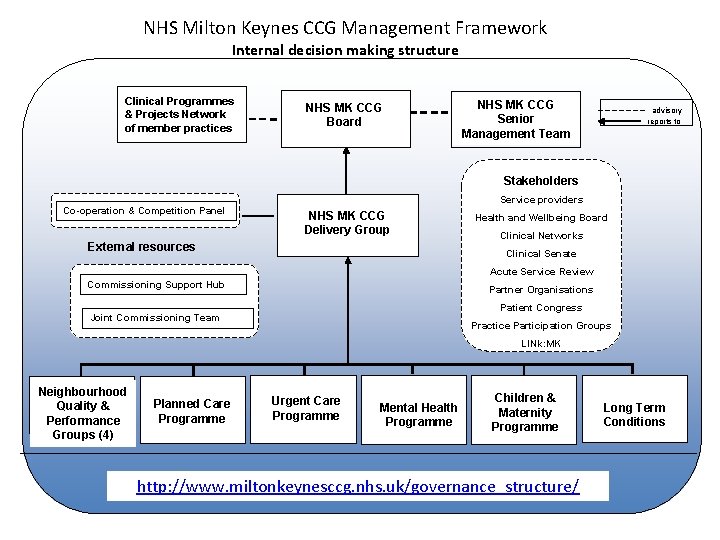
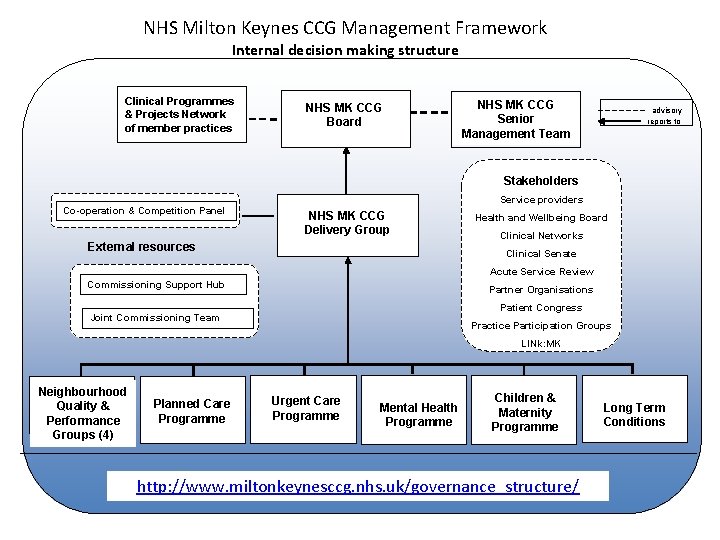
NHS Milton Keynes CCG Management Framework Internal decision making structure Clinical Programmes & Projects Network of member practices NHS MK CCG Board NHS MK CCG Senior Management Team advisory reports to Stakeholders Co-operation & Competition Panel Service providers NHS MK CCG Delivery Group External resources Health and Wellbeing Board Clinical Networks Clinical Senate Acute Service Review Commissioning Support Hub Partner Organisations Patient Congress Joint Commissioning Team Practice Participation Groups LINk: MK Neighbourhood Quality & Performance Groups (4) Planned Care Programme Urgent Care Programme Mental Health Programme Children & Maternity Programme http: //www. miltonkeynesccg. nhs. uk/governance_structure/ Long Term Conditions
Commissioning in Milton Keynes • Read about commissioning in Milton Keynes http: //www. miltonkeynesccg. nhs. uk/commissioning-in-mk/ • Read about the work of the Milton Keynes CCG Programme Boards: http: //www. miltonkeynesccg. nhs. uk/commissioning_programmes/ • See the Commissioning Toolkit of resources to support the work of commissioners: http: //www. miltonkeynesccg. nhs. uk/commissioning_toolkit/ • Sign up for alerts to keep you abreast of the latest commissioning resources – Anne Gray - Commissioning. librarian@miltonkeynes. nhs. uk
Compiled by Anne Gray, Knowledge Officer NHS Milton Keynes CCG September 2012 With acknowledgement to Dr Andrew Jones, Clinical Specialist and Lead for Commissioning, BMJ