The Clinical Impact of the Ankle Brachial Index
The Clinical Impact of the Ankle Brachial Index Exam CDR Doug E. Henry, PT , CWS® Federal Medical Center - Butner, NC
Objectives � Outline the BOP Guidelines for evaluating vascular disease � Identify the clinical signs of peripheral arterial disease/PAD � Summarize the significance of the ABI examination in relationship to evaluation of PAD � Summarize the strengths & limitations of ABI examination � Describe or interpret how current literature impacts clinical findings of the ABI examination � Outline which class of compression stockings are indicated or contraindicated for pnts
FCC Butner
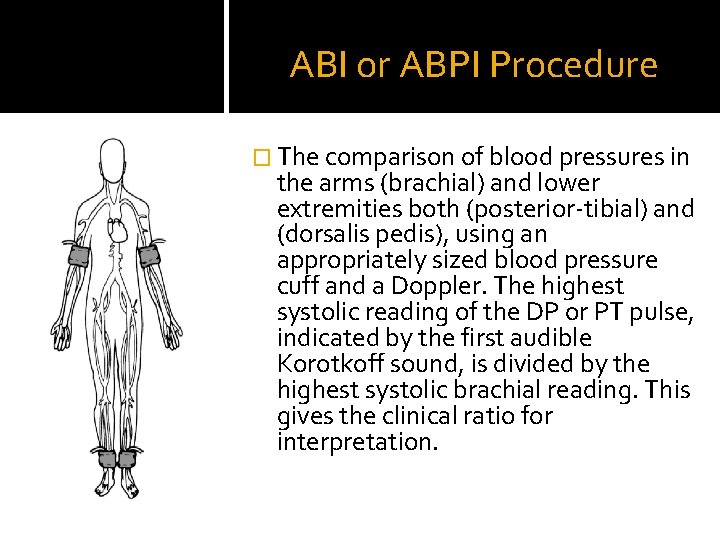
ABI or ABPI Procedure � The comparison of blood pressures in the arms (brachial) and lower extremities both (posterior-tibial) and (dorsalis pedis), using an appropriately sized blood pressure cuff and a Doppler. The highest systolic reading of the DP or PT pulse, indicated by the first audible Korotkoff sound, is divided by the highest systolic brachial reading. This gives the clinical ratio for interpretation.
DELAYED HEALING • • Tissue Ischemia Poor Vascularity Instability of metabolites – Decreased H&H, Dehydration, poor glucose control… Nutrition – Low Albumin for Healing Demand Heavy Bacterial Bio-burden Infection Other
PAD risk factors Atherosclerosis �Tobacco use �Metabolic Syndrome: DM, HTN, Dyslipidemia, Obesity �CAD �Thromboangitis obliterans �Vasculitis �Renal Disease �Raynaud’s Disease �Sickle Cell Disease �Other…
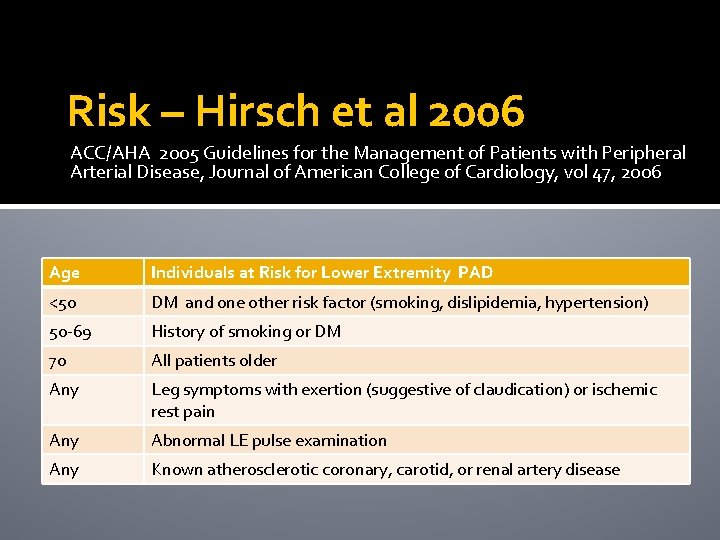
Risk – Hirsch et al 2006 ACC/AHA 2005 Guidelines for the Management of Patients with Peripheral Arterial Disease, Journal of American College of Cardiology, vol 47, 2006 Age Individuals at Risk for Lower Extremity PAD <50 DM and one other risk factor (smoking, dislipidemia, hypertension) 50 -69 History of smoking or DM 70 All patients older Any Leg symptoms with exertion (suggestive of claudication) or ischemic rest pain Any Abnormal LE pulse examination Any Known atherosclerotic coronary, carotid, or renal artery disease
PAD – Presentation �Clinical presentation: Claudication, atrophy, reduction of mobility, integumentary lesions, and delayed or unexplained slow healing wounds. �Local presentation: discoloration, bruising, numbness, weakness, decreased pulses, atrophic appearance.
PAD - Pathophysiology �Diminished blood flow resulting in tissue ischemia, ↓ O 2 levels, ↓ neutrophil activity, ↓inflammatory response =↑ rates of infection… �↑ NON-healing ulcerations → necrosis → gangrene, amputation…
Clinical Practice Guidelines Diabetes Management 2012 Wound Care March 2014 BOP
Committee Members �Jeffrey Allen, MD �Matt Hardin, Dermatologist �CDR Kevin Elker, RN, CWOCN �CAPT Matt Taylor (ret), PT, DPT, OCS, CWS �Pam Baker, RN, CWOCN �Patina Walker-Geer, NP �CDR Christine Fallon, NP, WCC �LCDR Sherrie Wheeler, RN �CDR Cubie Beasley, RN � ….
The Vascular Exam BOP Wound Care CPG DFU VENOUS ARTERIAL

Basic Vascular Evaluation �Skin Temperature �Capillary Refill �Palpation of LE pulses DP & PT �Elevation Pallor �Dependent Rubor �Atrophic foot
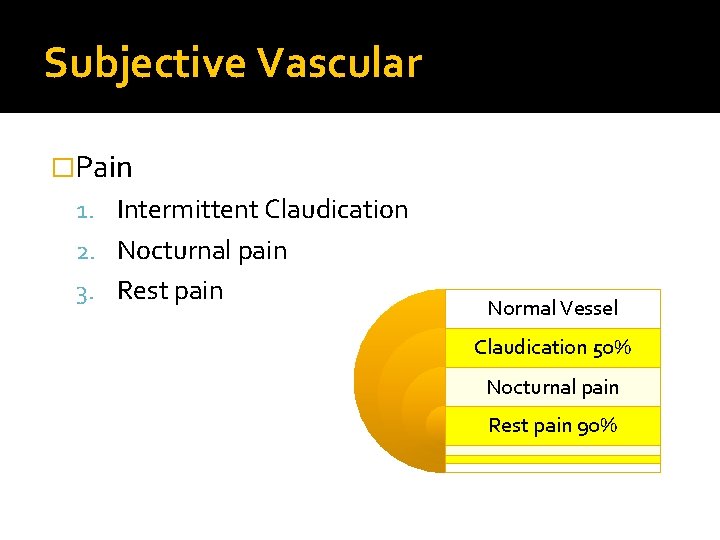
Subjective Vascular �Pain 1. Intermittent Claudication 2. Nocturnal pain 3. Rest pain Normal Vessel Claudication 50% Nocturnal pain Rest pain 90%
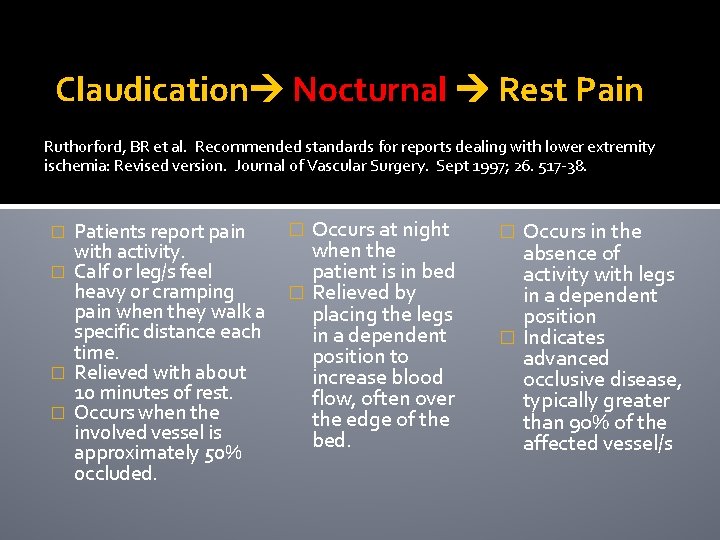
Claudication Nocturnal Rest Pain Ruthorford, BR et al. Recommended standards for reports dealing with lower extremity ischemia: Revised version. Journal of Vascular Surgery. Sept 1997; 26. 517 -38. Patients report pain with activity. � Calf or leg/s feel heavy or cramping pain when they walk a specific distance each time. � Relieved with about 10 minutes of rest. � Occurs when the involved vessel is approximately 50% occluded. � Occurs at night when the patient is in bed � Relieved by placing the legs in a dependent position to increase blood flow, often over the edge of the bed. � Occurs in the absence of activity with legs in a dependent position � Indicates advanced occlusive disease, typically greater than 90% of the affected vessel/s �
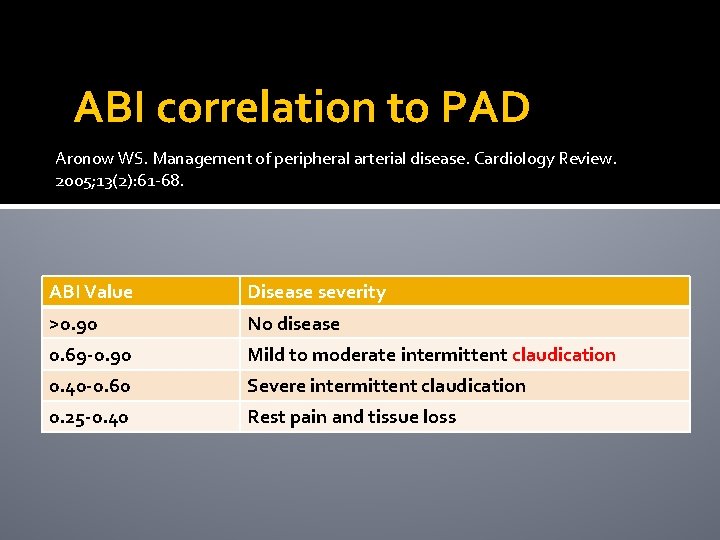
ABI correlation to PAD Aronow WS. Management of peripheral arterial disease. Cardiology Review. 2005; 13(2): 61 -68. ABI Value Disease severity >0. 90 No disease 0. 69 -0. 90 Mild to moderate intermittent claudication 0. 40 -0. 60 Severe intermittent claudication 0. 25 -0. 40 Rest pain and tissue loss
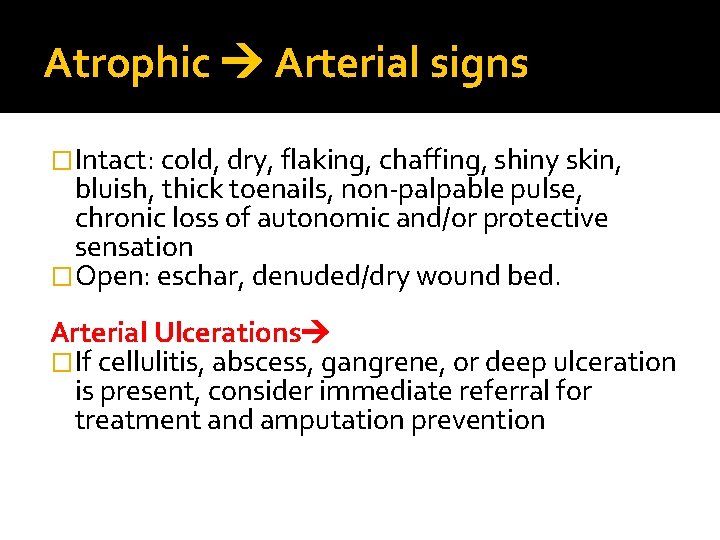
Atrophic Arterial signs �Intact: cold, dry, flaking, chaffing, shiny skin, bluish, thick toenails, non-palpable pulse, chronic loss of autonomic and/or protective sensation �Open: eschar, denuded/dry wound bed. Arterial Ulcerations �If cellulitis, abscess, gangrene, or deep ulceration is present, consider immediate referral for treatment and amputation prevention
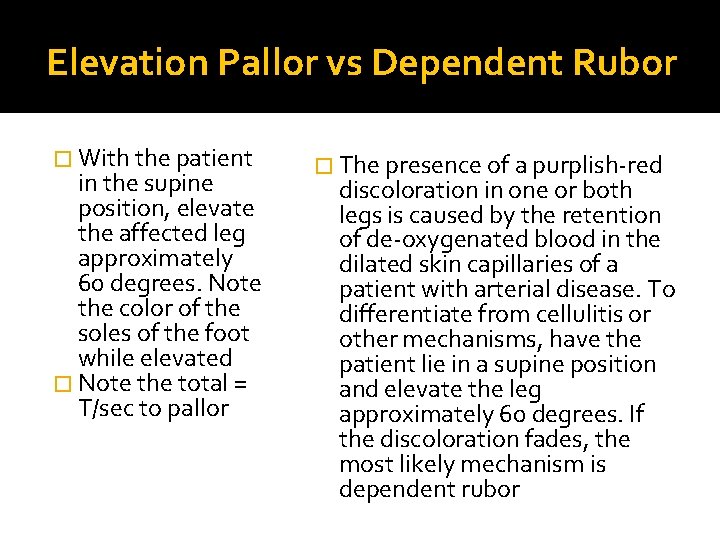
Elevation Pallor vs Dependent Rubor � With the patient in the supine position, elevate the affected leg approximately 60 degrees. Note the color of the soles of the foot while elevated � Note the total = T/sec to pallor � The presence of a purplish-red discoloration in one or both legs is caused by the retention of de-oxygenated blood in the dilated skin capillaries of a patient with arterial disease. To differentiate from cellulitis or other mechanisms, have the patient lie in a supine position and elevate the leg approximately 60 degrees. If the discoloration fades, the most likely mechanism is dependent rubor
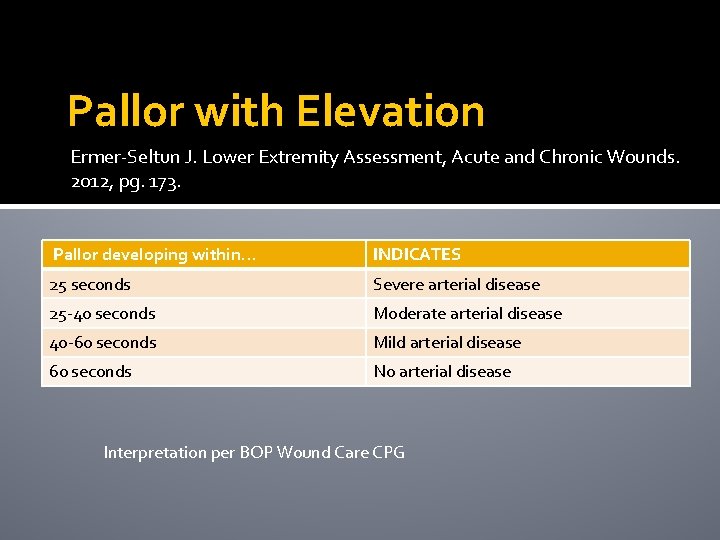
Pallor with Elevation Ermer-Seltun J. Lower Extremity Assessment, Acute and Chronic Wounds. 2012, pg. 173. Pallor developing within… INDICATES 25 seconds Severe arterial disease 25 -40 seconds Moderate arterial disease 40 -60 seconds Mild arterial disease 60 seconds No arterial disease Interpretation per BOP Wound Care CPG

Elevation Pallor vs Dependent Rubor
The Clinical Impact of the ABI EBM
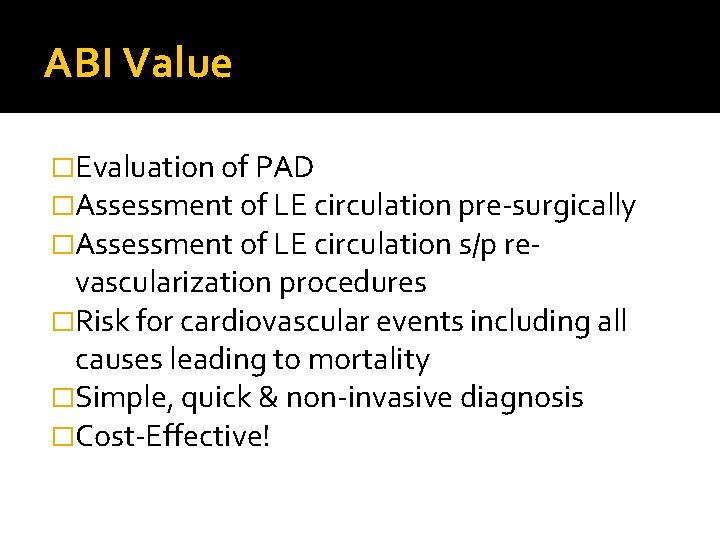
ABI Value �Evaluation of PAD �Assessment of LE circulation pre-surgically �Assessment of LE circulation s/p re- vascularization procedures �Risk for cardiovascular events including all causes leading to mortality �Simple, quick & non-invasive diagnosis �Cost-Effective!
ABI – Mc. Dermott Lower ankle/brachial index, as calculated by averaging the dorsalis pedis & posterior tibial arterial pressure, & association with leg functioning in peripheral arterial disease Mc. Dermott et al, Journal of Vascular Surgery, Dec 2000 • n= 244 men & women age 55+ with & w/o PAD • Outcome measures = walking velocity & endurance measured with 6 min/walk test • Reviewed 3 different methods of calculating ABI to determine the best testing method
ABI – Mc. Dermott cont. �PAD defined as ABI less than < 0. 90 �Method 1: higher LE arterial pressure - 47% �Method 2: lower LE arterial pressure - 59% �Method 3: average of dorsalis pedis & posterior tibial pulses used to calculate ABI 52% �Results: Method #2 was most closely associated with correctly predicting PAD but Method #3 predicted leg function using the outcome measures in regression analysis
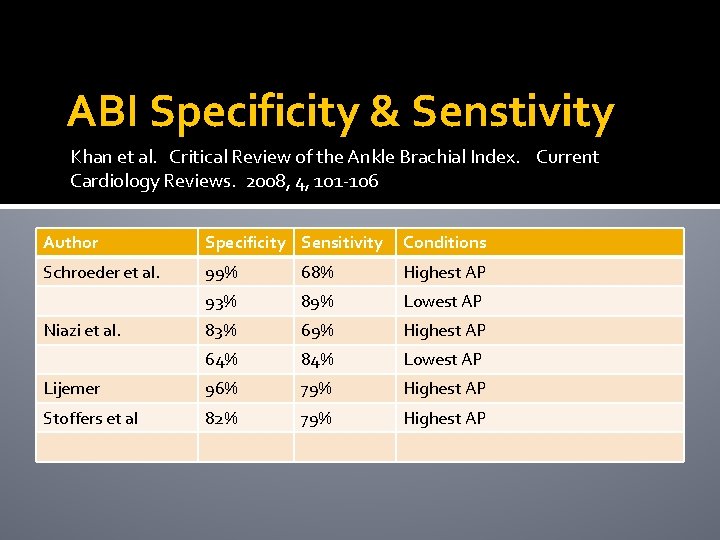
ABI Specificity & Senstivity Khan et al. Critical Review of the Ankle Brachial Index. Current Cardiology Reviews. 2008, 4, 101 -106 Author Specificity Sensitivity Conditions Schroeder et al. 99% 68% Highest AP 93% 89% Lowest AP 83% 69% Highest AP 64% 84% Lowest AP Lijemer 96% 79% Highest AP Stoffers et al 82% 79% Highest AP Niazi et al.
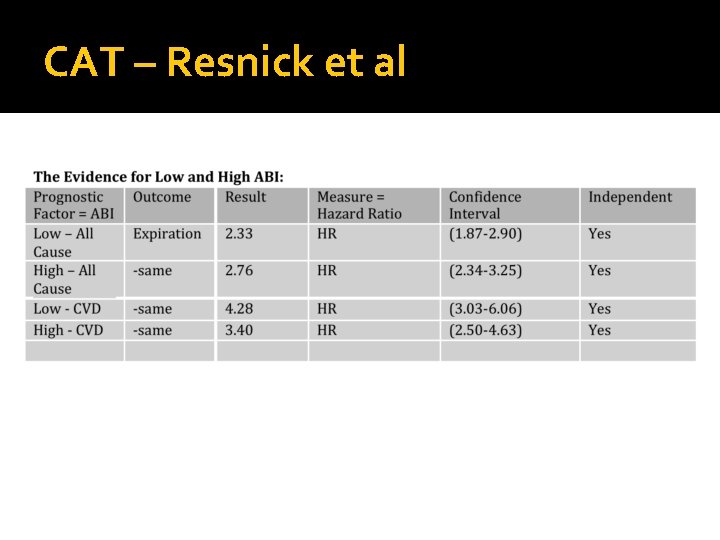
CAT - 2013 • For a 60 year old person with a positive reading less than 0. 80 [0. 90] what is the probability of mortality in this patient? • Relationship of High and Low Ankle Brachial Index to All-Cause and Cardiovascular Disease Mortality: Resnick et al, Circulation 2004
CAT – Resnick et al �n= 4549, age 45 -74, ethnicity native, outcome = mortality, retrospective cohort, level 2 B �Both abnormally low (4. 9%) and high (9. 2%) ABI results are linked to cardiovascular events �All cardiac events were associated including: CVA, TIA, MI… �PAD determined by ABI <0. 90
CAT – Resnick et al
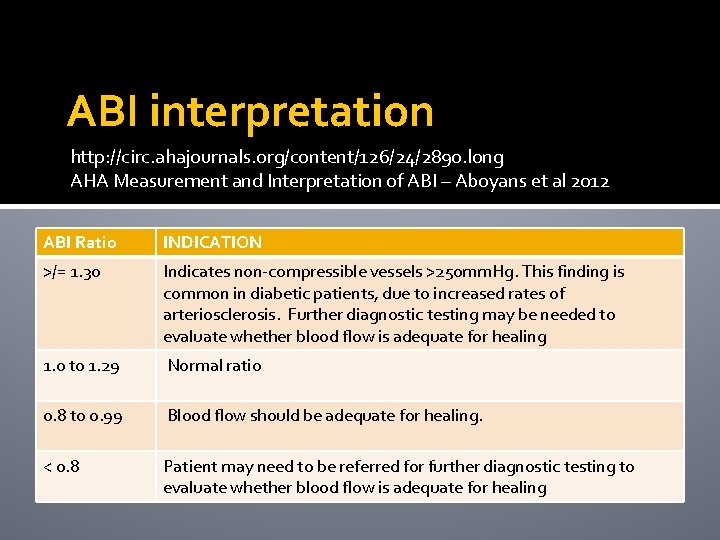
ABI interpretation http: //circ. ahajournals. org/content/126/24/2890. long AHA Measurement and Interpretation of ABI – Aboyans et al 2012 ABI Ratio INDICATION >/= 1. 30 Indicates non-compressible vessels >250 mm. Hg. This finding is common in diabetic patients, due to increased rates of arteriosclerosis. Further diagnostic testing may be needed to evaluate whether blood flow is adequate for healing 1. 0 to 1. 29 Normal ratio 0. 8 to 0. 99 Blood flow should be adequate for healing. < 0. 8 Patient may need to be referred for further diagnostic testing to evaluate whether blood flow is adequate for healing
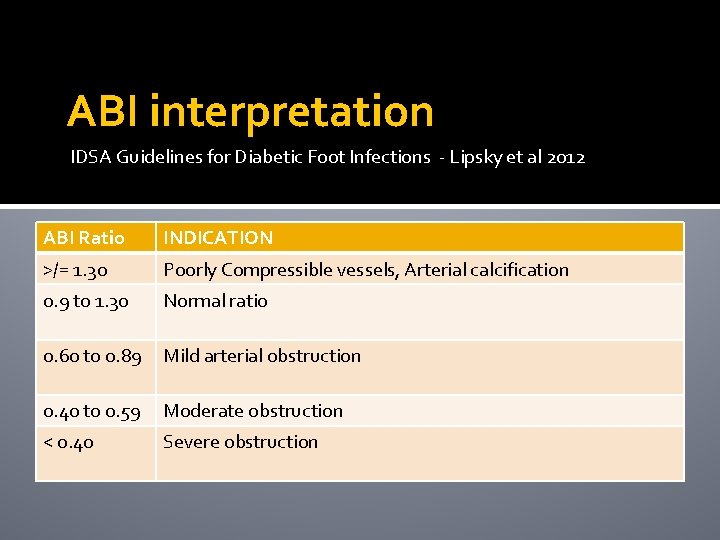
ABI interpretation IDSA Guidelines for Diabetic Foot Infections - Lipsky et al 2012 ABI Ratio INDICATION >/= 1. 30 Poorly Compressible vessels, Arterial calcification 0. 9 to 1. 30 Normal ratio 0. 60 to 0. 89 Mild arterial obstruction 0. 40 to 0. 59 Moderate obstruction < 0. 40 Severe obstruction
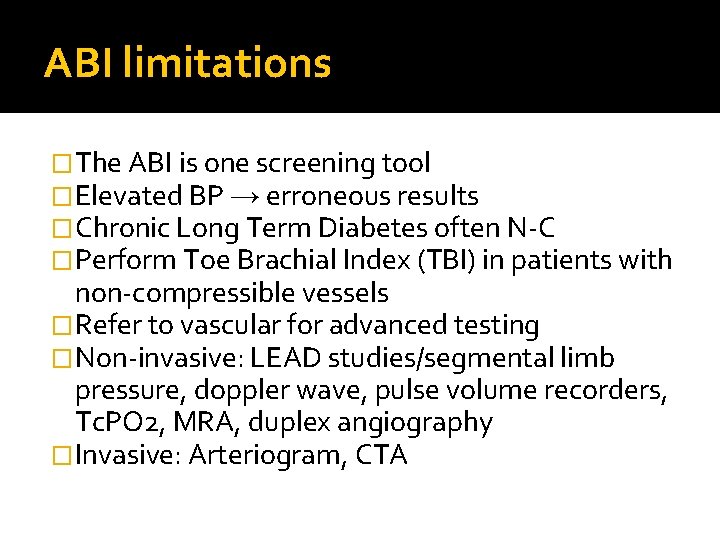
ABI limitations �The ABI is one screening tool �Elevated BP → erroneous results �Chronic Long Term Diabetes often N-C �Perform Toe Brachial Index (TBI) in patients with non-compressible vessels �Refer to vascular for advanced testing �Non-invasive: LEAD studies/segmental limb pressure, doppler wave, pulse volume recorders, Tc. PO 2, MRA, duplex angiography �Invasive: Arteriogram, CTA
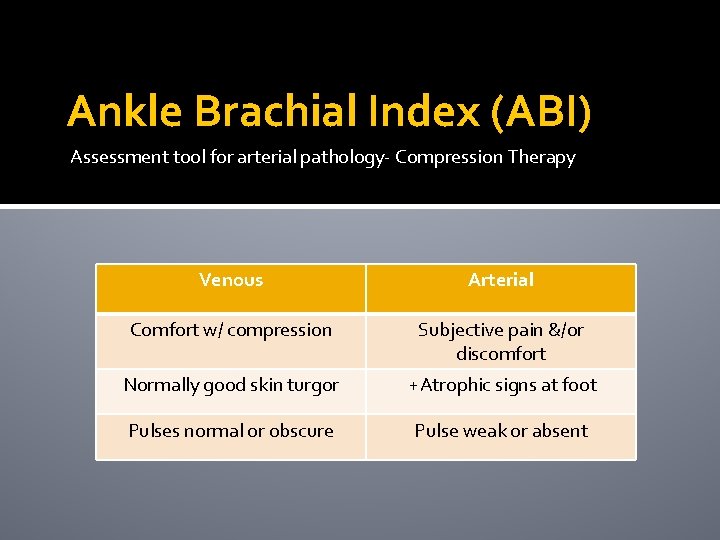
Ankle Brachial Index (ABI) Assessment tool for arterial pathology- Compression Therapy Venous Arterial Comfort w/ compression Subjective pain &/or discomfort Normally good skin turgor +Atrophic signs at foot Pulses normal or obscure Pulse weak or absent
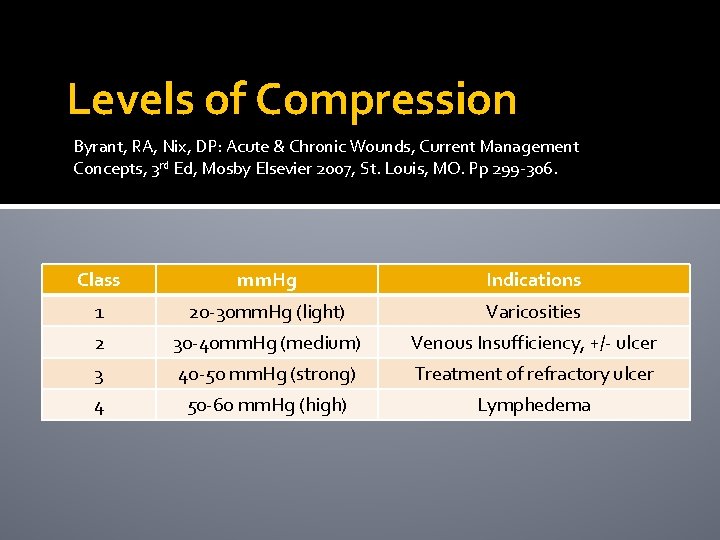
Levels of Compression Byrant, RA, Nix, DP: Acute & Chronic Wounds, Current Management Concepts, 3 rd Ed, Mosby Elsevier 2007, St. Louis, MO. Pp 299 -306. Class mm. Hg Indications 1 20 -30 mm. Hg (light) Varicosities 2 30 -40 mm. Hg (medium) Venous Insufficiency, +/- ulcer 3 40 -50 mm. Hg (strong) Treatment of refractory ulcer 4 50 -60 mm. Hg (high) Lymphedema
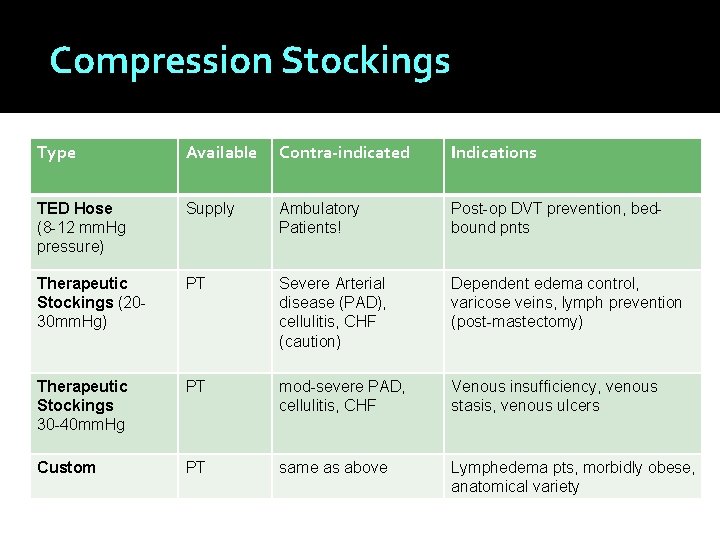
Compression Stockings Type Available Contra-indicated Indications TED Hose (8 -12 mm. Hg pressure) Supply Ambulatory Patients! Post-op DVT prevention, bedbound pnts Therapeutic Stockings (2030 mm. Hg) PT Severe Arterial disease (PAD), cellulitis, CHF (caution) Dependent edema control, varicose veins, lymph prevention (post-mastectomy) Therapeutic Stockings 30 -40 mm. Hg PT mod-severe PAD, cellulitis, CHF Venous insufficiency, venous stasis, venous ulcers Custom PT same as above Lymphedema pts, morbidly obese, anatomical variety
Compression Stockings �Advantages: Provide graded compression, enhance circulation for wound healing, pain relief, and prevention of DVT, variety of styles for ease of application. �Disadvantages: Can be difficult to apply, require compliance, cleaning (cannot be dried in dryer)
Compression Stockings-Instructions � Applied before getting out of bed in the morning, removed at night or bathing ONLY (TED hose worn in bed by the non-ambulatory for prevention) � Wash in washing machine, hang dry � Should last 8 -12 months � D/C if develop chest pains or skin irritation, consider less compression if skin tears at dorsal crease in elderly �Lower compression options=tubi-grip D, E & F
Take home message �The evaluation of arterial disease is a critical step for wound healing at the LE �Treatment delays increase probability of failure �PAD pnts have higher cardiac risks, mortality and amputation risks �Limb salvage in the diabetic population is greatly improved with assertive mgmt!
Vascular examination �PMH �Subjective Report �Clinical Examination �Clinical Tests for Arterial Disease ABI (Sensitivity & Specificity) �Referral: Vascular Medicine
TOOLS D 2 HENRY@BOP. GOV • BOP WOUND CARE CPG • INTERPRETATION 1. 2012 AHA 2. 2012 IDSA • COMPRESSION HOSE GUIDES
Questions… Referral D 2 HENRY@BOP. GOV PMH Subject Report ABI Clinical Findings
- Slides: 40