The Clinical Aspects of Enzyme Deficiencies in Haematology
- Slides: 20
The Clinical Aspects of Enzyme Deficiencies in Haematology Dr Pasquale Barbaro Paediatric Haematologist The Children’s Hospital at Westmead
Summary • • Red cell enzyme deficiencies Enzyme deficiencies in platelet function defects Enzyme deficiencies implicated in Neutropenia Enzyme deficiencies implicated in Bone Marrow failure
Red Cell Enzyme deficiencies • Red Cell Metabolism • During maturation, RCs lose their nucleus, organelles and mitochondria • Require cellular metabolic pathways to ensure red cell membrane and haemoglobin integrity • Require ATP to drive K/Na pump essential for membrane integrity • Require NADH to protect from oxidative stress • Require 2, 3 bisphophoglycerate to regulate oxygen affinity • Red cell enzyme deficiencies lead to non-spheroctyic haemolytic anaemia • Chronic or intermittent haemolysis • Pallor, jaundice • Anaemia, reticulocytosis, hyperbilirubinaemia • Splenomegaly • Gall stone production • Iron overload
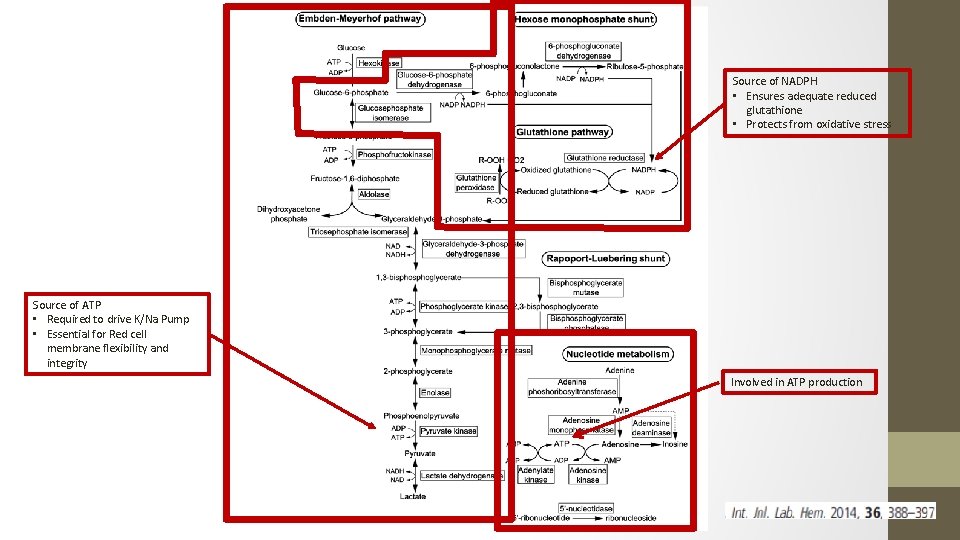
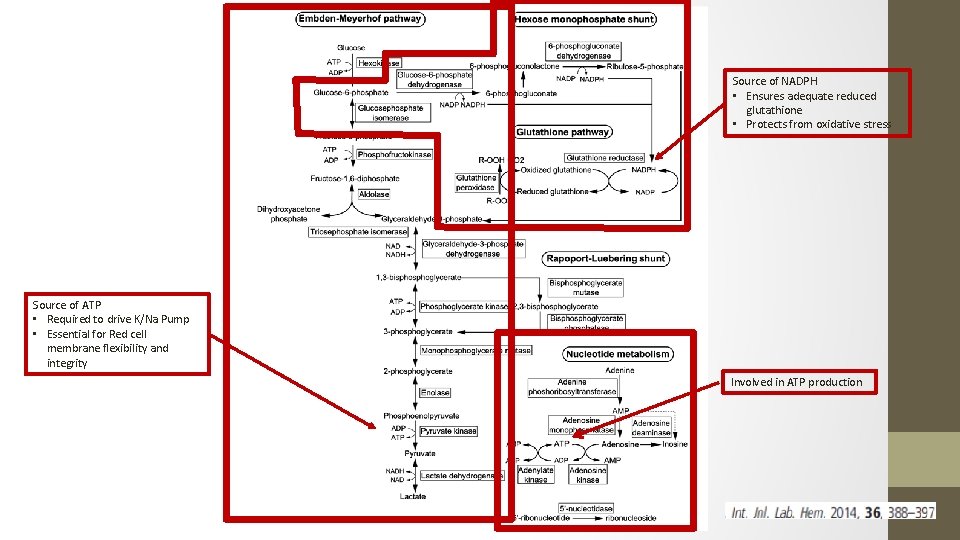
Source of NADPH • Ensures adequate reduced glutathione • Protects from oxidative stress Source of ATP • Required to drive K/Na Pump • Essential for Red cell membrane flexibility and integrity Involved in ATP production
Embden-Meyerhof pathway • ATP production • Enzyme deficiencies lead to chronic non spherocytic haemolysis of various severities • Many also have non haematological manifestations • Neurological • Myopathy • Most common: • Pyruvate Kinase deficiency • Glucose-6 -phosphate isomerase deficiency • Phosphofructokinase deficiency • All have autosomal recessive inheritance • Except Phosphoglycerate kinase deficiency – X-Linked
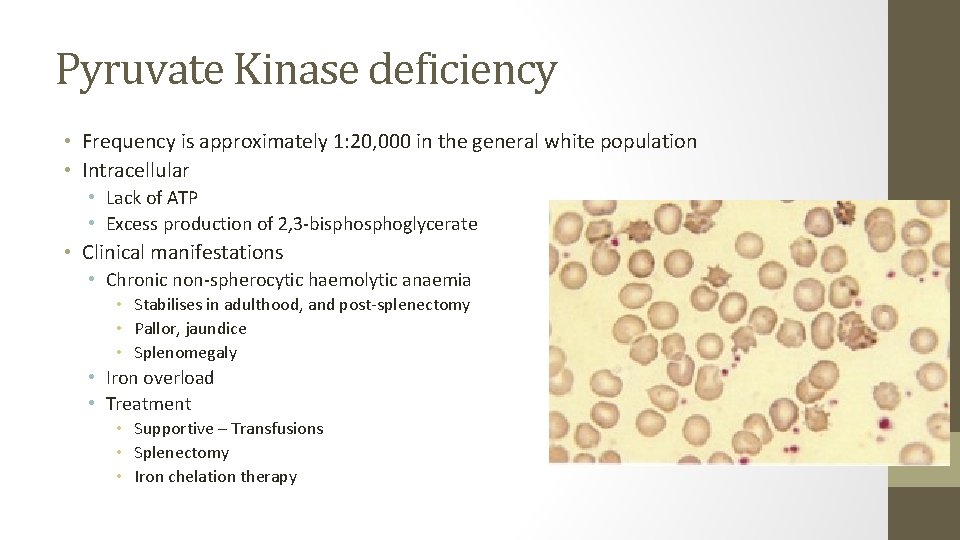
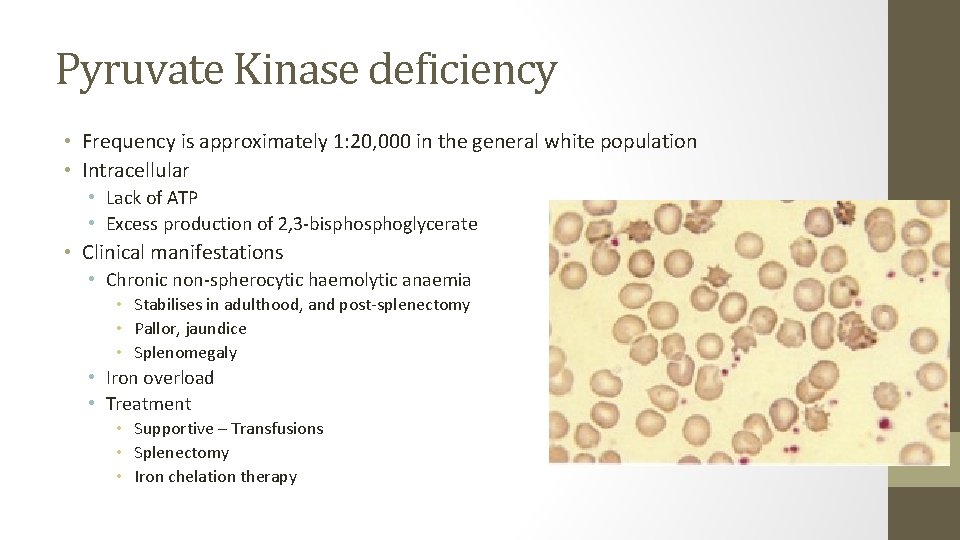
Pyruvate Kinase deficiency • Frequency is approximately 1: 20, 000 in the general white population • Intracellular • Lack of ATP • Excess production of 2, 3 -bisphoglycerate • Clinical manifestations • Chronic non-spherocytic haemolytic anaemia • Stabilises in adulthood, and post-splenectomy • Pallor, jaundice • Splenomegaly • Iron overload • Treatment • Supportive – Transfusions • Splenectomy • Iron chelation therapy
Glucose phosphate isomerase (GPI) deficiency • More than 50 cases described • Second most common enzyme defect in the red cell anaerobic glycolysis • Clinical features • More severe haemolysis • Hydrops foetalis is more common than in other enzymopathies • May be associated with neurological complications • Granulocyte dysfunction has also been described
Others • Phosphofructokinase • Mild or fully compensated haemolytic anaemia • Myopathy may be more pronounced symptom • Aldolase • Moderate to severe haemolysis • Neurological and muscle dysfunction • Recurrent rhabdomyolysis • Triose-phosphate • Most severe enzyme defect in EM pathway • Hydrops foetalis or death in early childhood are common • Severe neurological complications
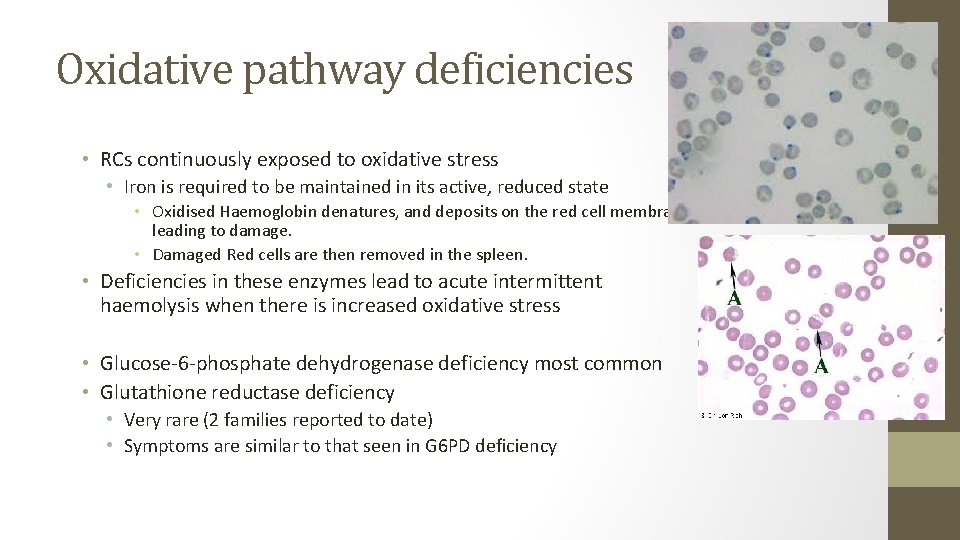
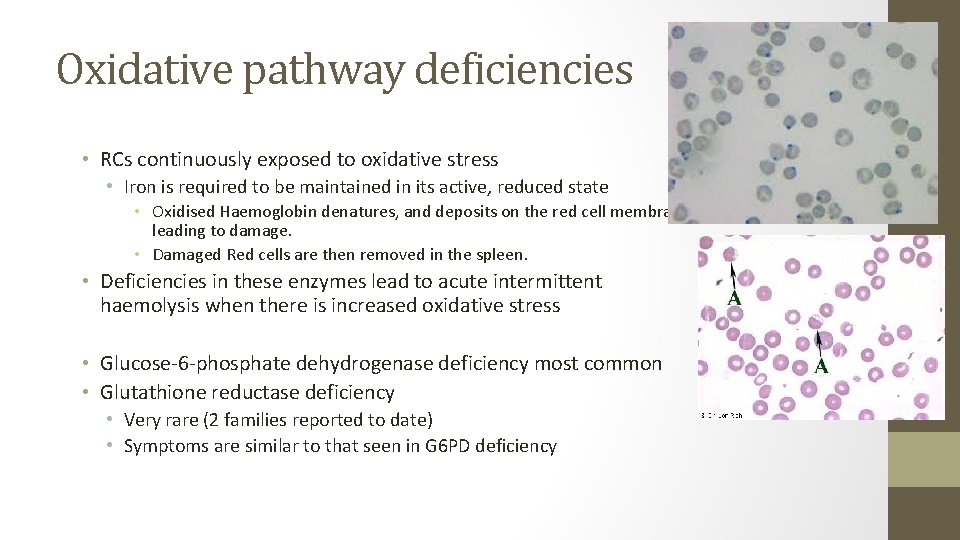
Oxidative pathway deficiencies • RCs continuously exposed to oxidative stress • Iron is required to be maintained in its active, reduced state • Oxidised Haemoglobin denatures, and deposits on the red cell membrane leading to damage. • Damaged Red cells are then removed in the spleen. • Deficiencies in these enzymes lead to acute intermittent haemolysis when there is increased oxidative stress • Glucose-6 -phosphate dehydrogenase deficiency most common • Glutathione reductase deficiency • Very rare (2 families reported to date) • Symptoms are similar to that seen in G 6 PD deficiency
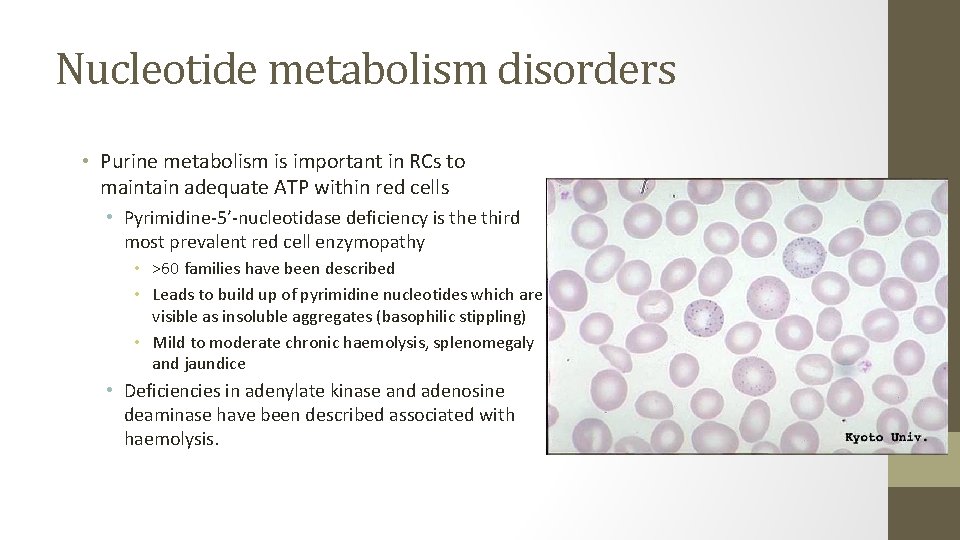
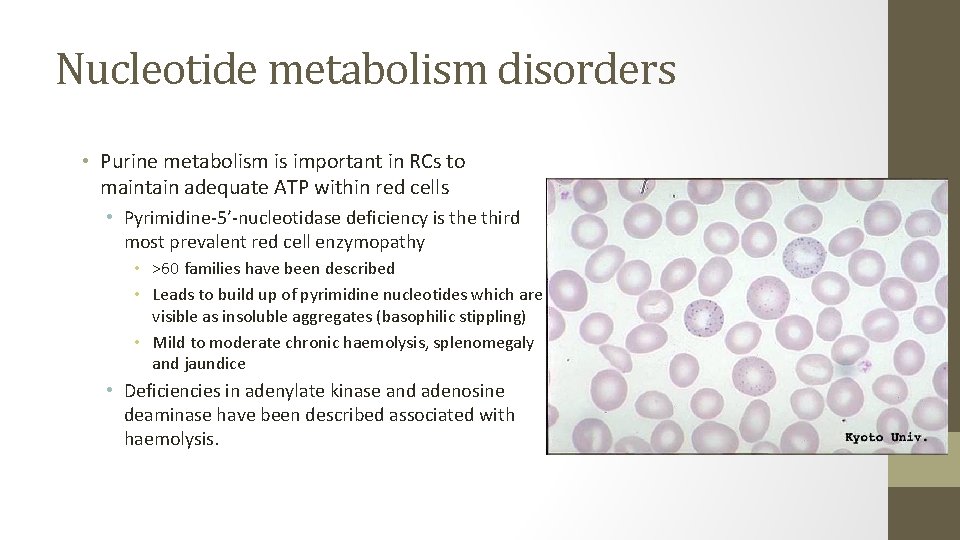
Nucleotide metabolism disorders • Purine metabolism is important in RCs to maintain adequate ATP within red cells • Pyrimidine-5’-nucleotidase deficiency is the third most prevalent red cell enzymopathy • >60 families have been described • Leads to build up of pyrimidine nucleotides which are visible as insoluble aggregates (basophilic stippling) • Mild to moderate chronic haemolysis, splenomegaly and jaundice • Deficiencies in adenylate kinase and adenosine deaminase have been described associated with haemolysis.
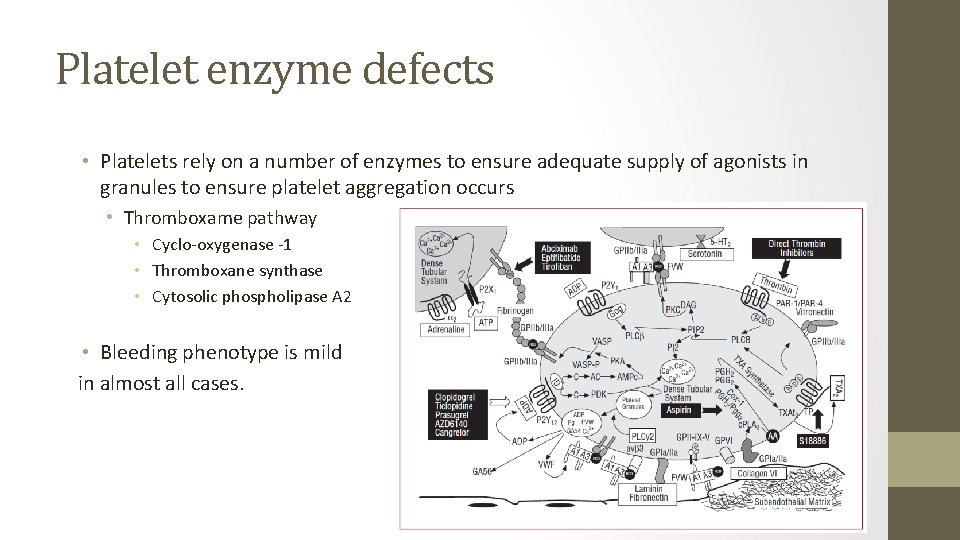
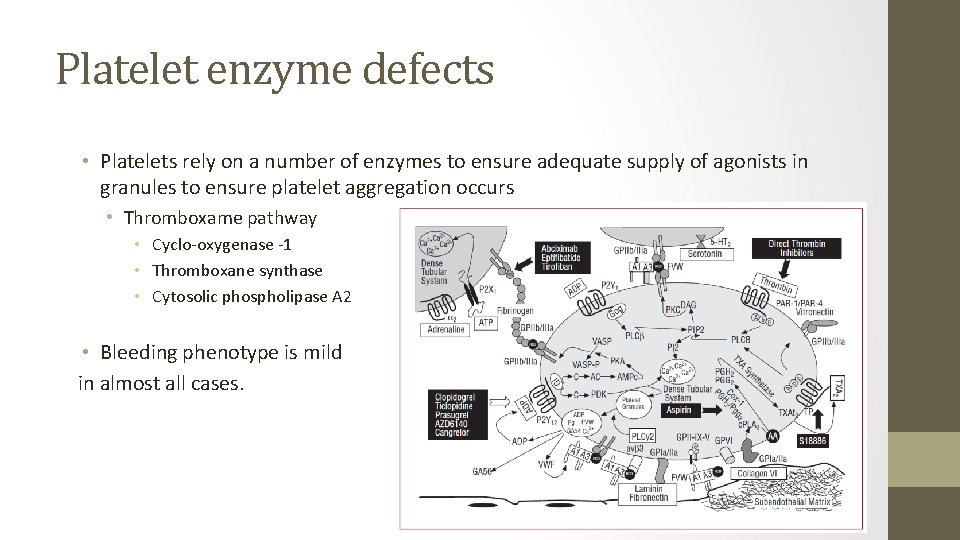
Platelet enzyme defects • Platelets rely on a number of enzymes to ensure adequate supply of agonists in granules to ensure platelet aggregation occurs • Thromboxame pathway • Cyclo-oxygenase -1 • Thromboxane synthase • Cytosolic phospholipase A 2 • Bleeding phenotype is mild in almost all cases.
Enzyme defects causing Congenital Neutropenia • Marked neutropenia (<0. 2 x 10^9/L) • Presents in the first year of life with recurrent infections and neutropenia • May be isolated or syndromic • Isolated forms are associated with mutations in Neutrophil Elastase (ELANE), HAX 1, GFI 1. • Many syndromic forms associated with chronic neutropenia • Glycogen storage disease Type 1 b - Glucose-6 -phosphate translocase • Glucose-6 -phosphatase catalytic subunit 3 (G 6 PC 3) deficiency • Barth Syndrome – tafazzin (a mitochondrial phopspholipid transacylase) deficiency
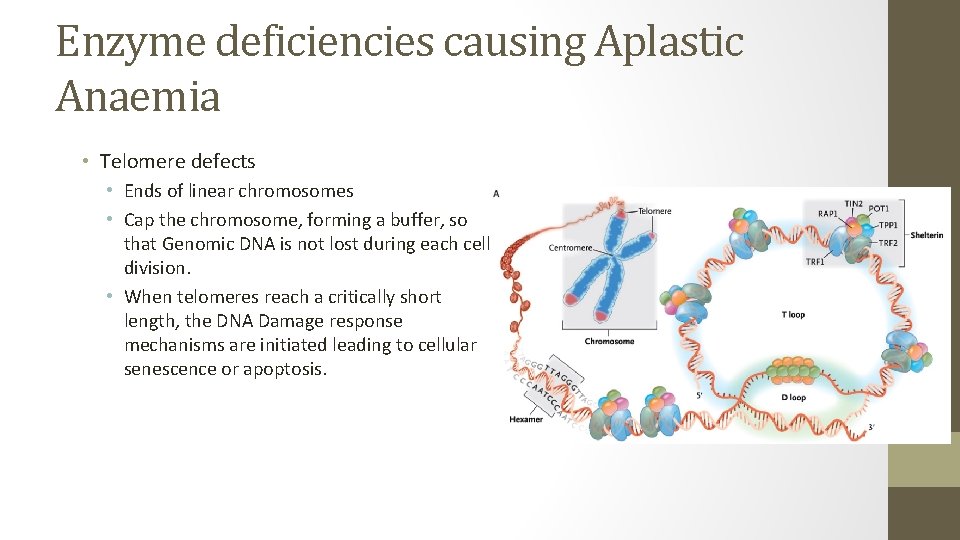
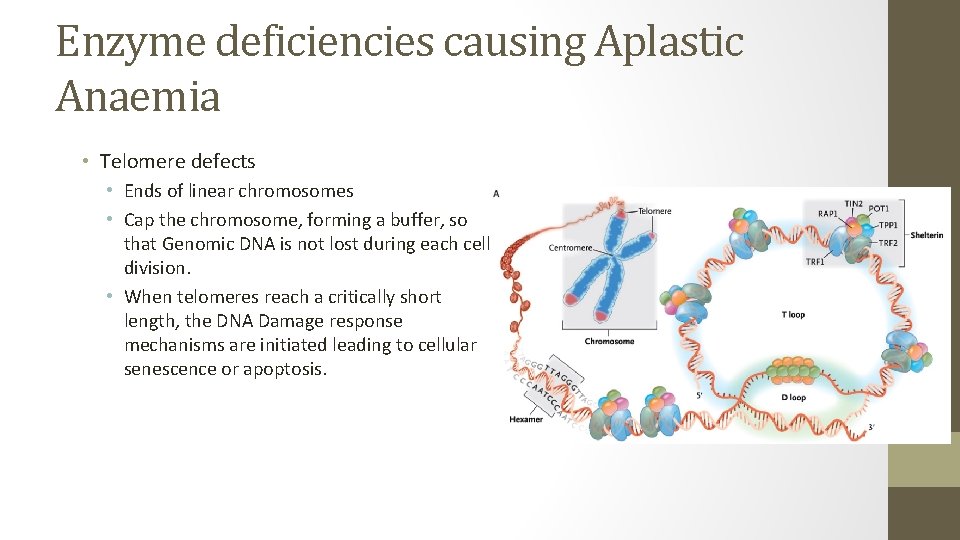
Enzyme deficiencies causing Aplastic Anaemia • Telomere defects • Ends of linear chromosomes • Cap the chromosome, forming a buffer, so that Genomic DNA is not lost during each cell division. • When telomeres reach a critically short length, the DNA Damage response mechanisms are initiated leading to cellular senescence or apoptosis.
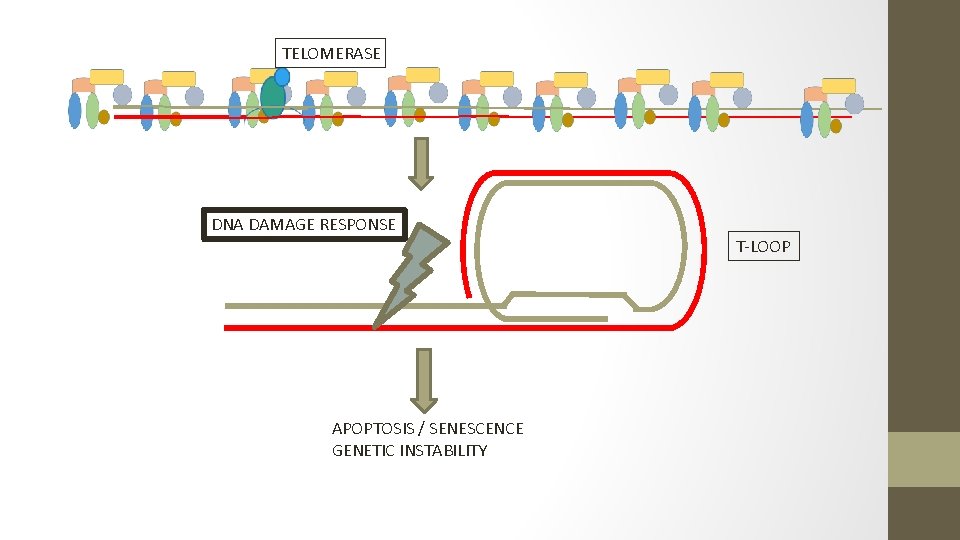
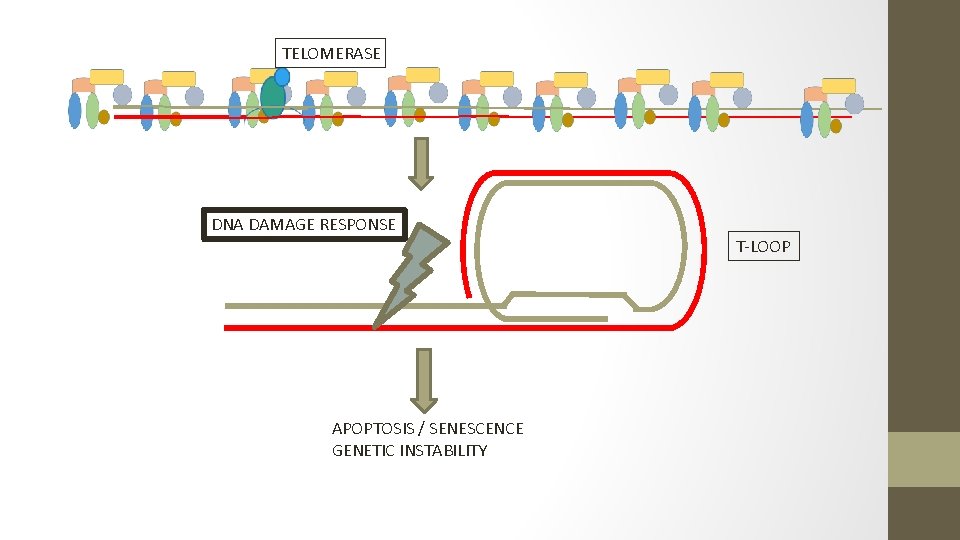
TELOMERASE DNA DAMAGE RESPONSE APOPTOSIS / SENESCENCE GENETIC INSTABILITY T-LOOP
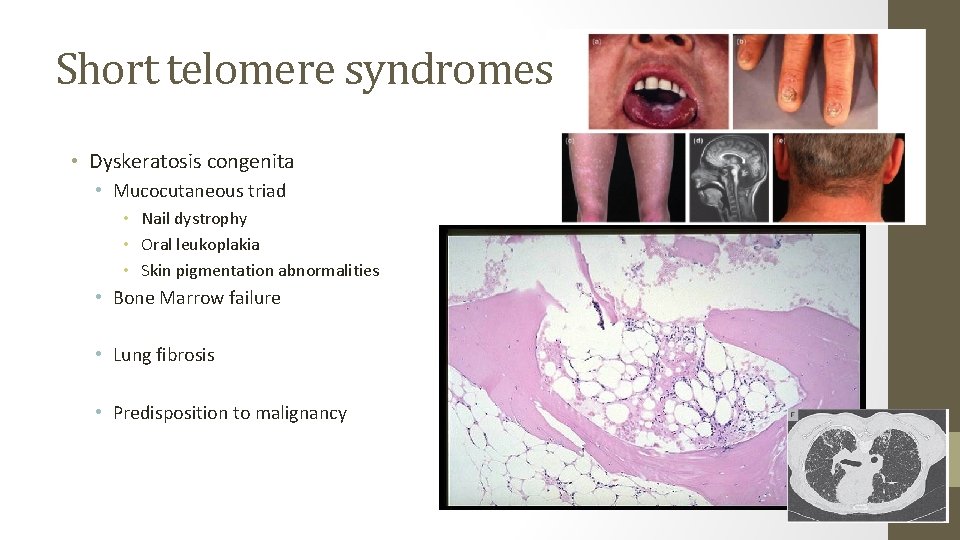
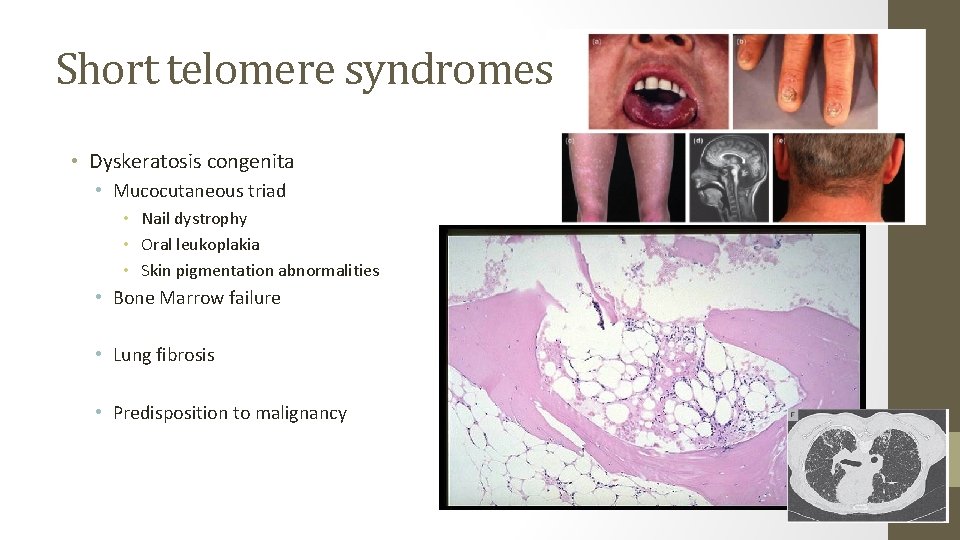
Short telomere syndromes • Dyskeratosis congenita • Mucocutaneous triad • Nail dystrophy • Oral leukoplakia • Skin pigmentation abnormalities • Bone Marrow failure • Lung fibrosis • Predisposition to malignancy
Short telomere syndromes • Deficiencies in the specialised polymerase, Telomerase is found in the majority of cases • Telomerase is a multiunit holoenzyme made up of Telomerase Reverse Transcriptase (TERT), Telomerase RNA component (TERC) and Dyskerin. • Deficiencies in the helicase RTEL 1 is also found in a minority of cases of DC • RTEL 1 catalyses the unfolding of the T-loop so that the telomere can be elongated.
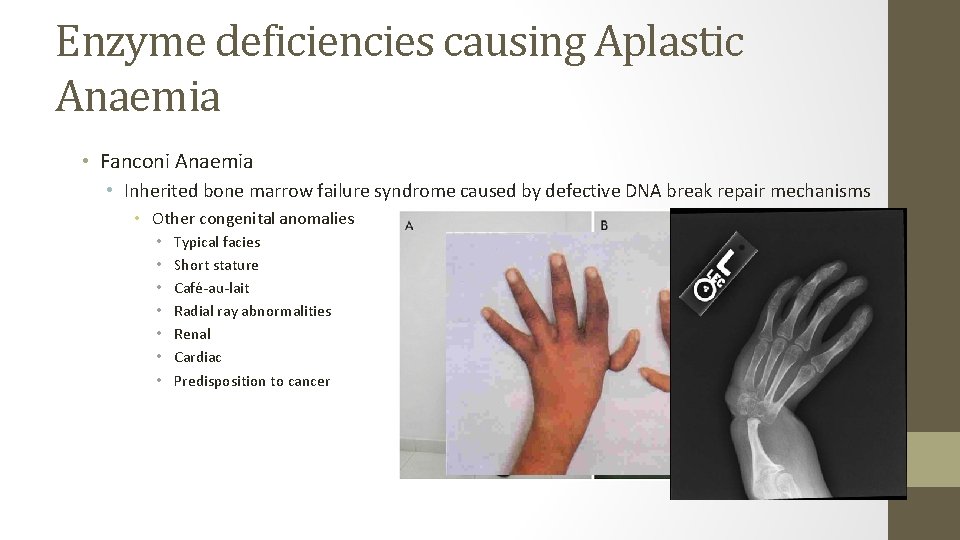
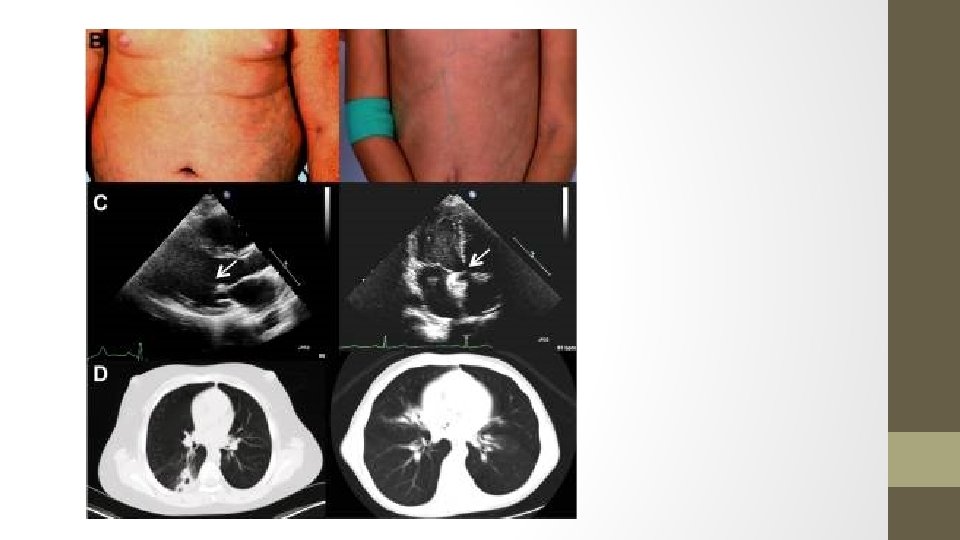
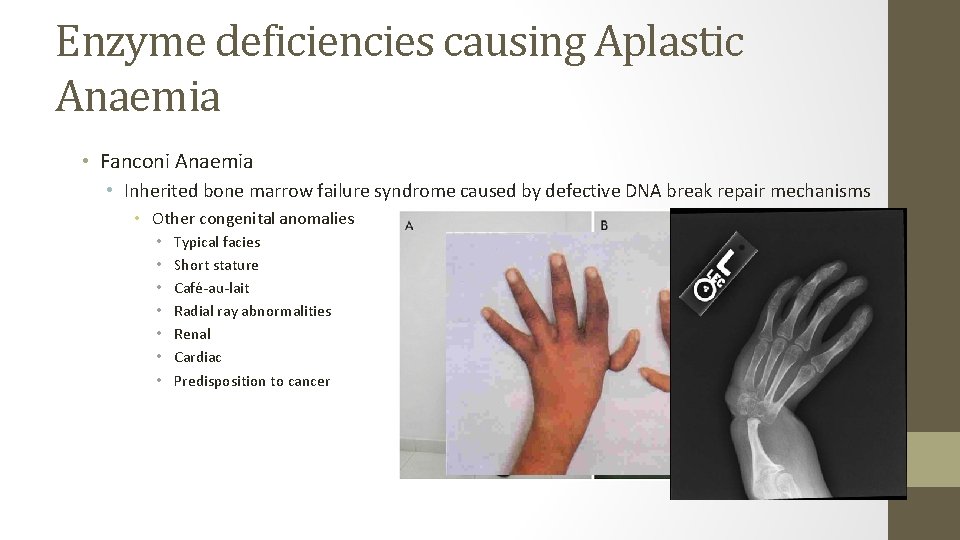
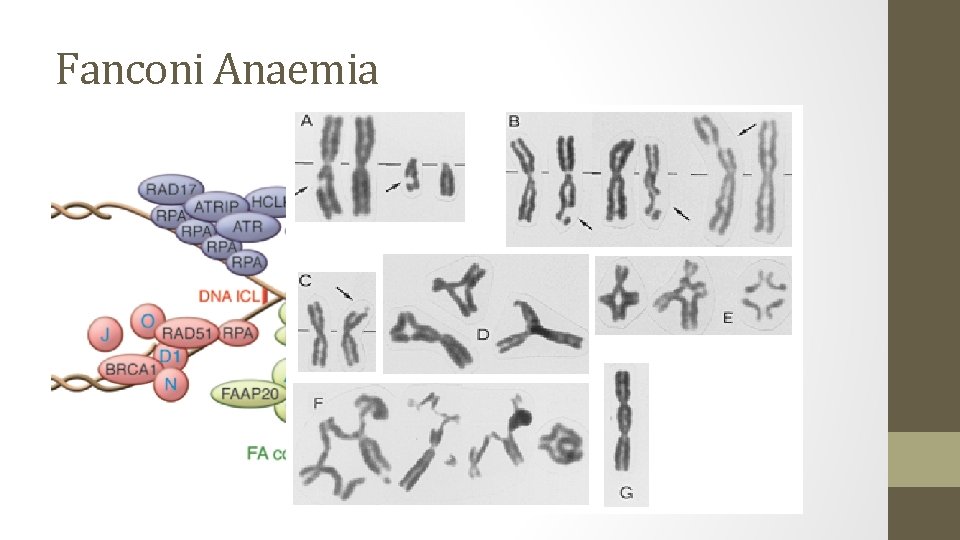
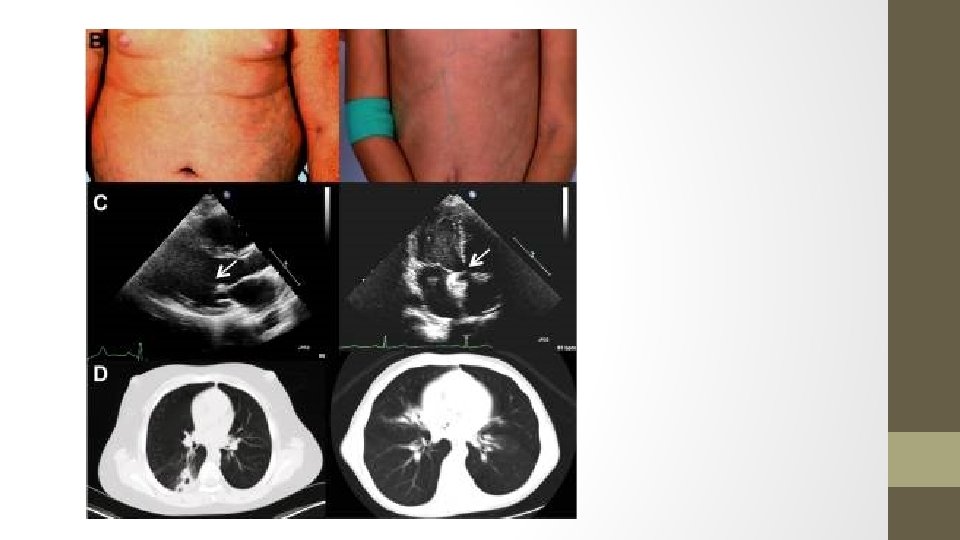
Enzyme deficiencies causing Aplastic Anaemia • Fanconi Anaemia • Inherited bone marrow failure syndrome caused by defective DNA break repair mechanisms • Other congenital anomalies • • Typical facies Short stature Café-au-lait Radial ray abnormalities Renal Cardiac Predisposition to cancer
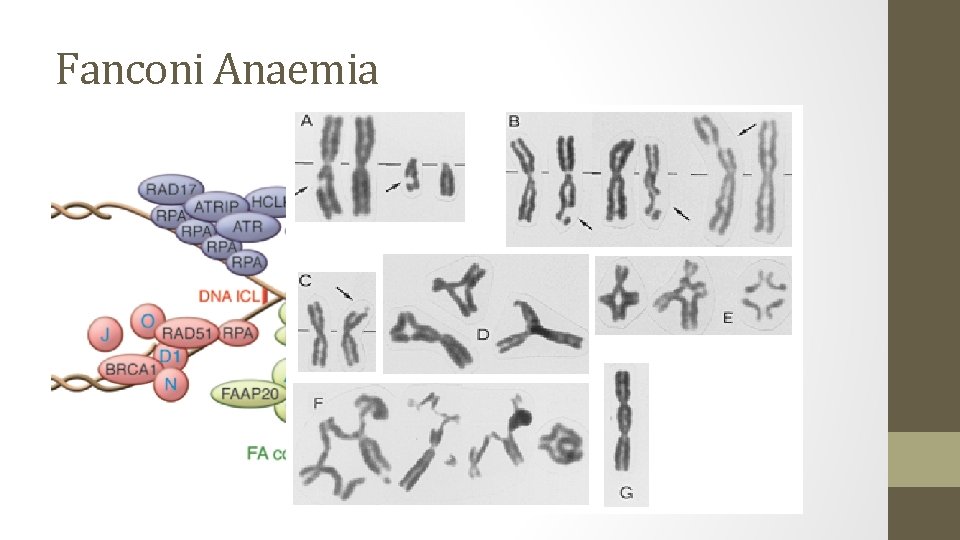
Fanconi Anaemia
Conclusion • Enzymes are essential for function of all haematopoietic cell lineages • Defects in enzymes can lead to a large variety of haematological conditions • • Haemolytic anaemias Bleeding disorders Neutropenia Bone marrow failure • Treatment is mostly supportive, with bone marrow transplantation able to cure defect in more severe cases.