THE CIRCULATORY SYSTEM Ch 18 The HEART ASSIGNMENT
- Slides: 45
THE CIRCULATORY SYSTEM § Ch. 18 The HEART
§ ASSIGNMENT: Most Of The Anatomy We Have Already Done In The Lab, So Make Sure To Do The * of slide 1 through 29. As I Will Likely Not Take The Time To Review This Material.
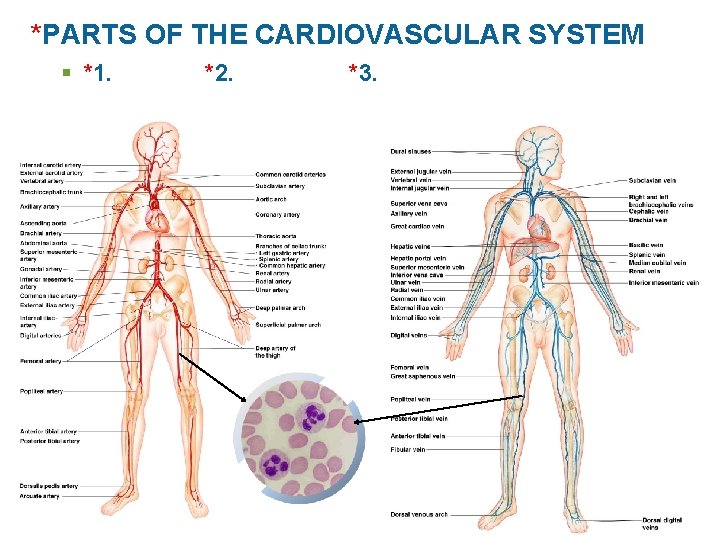
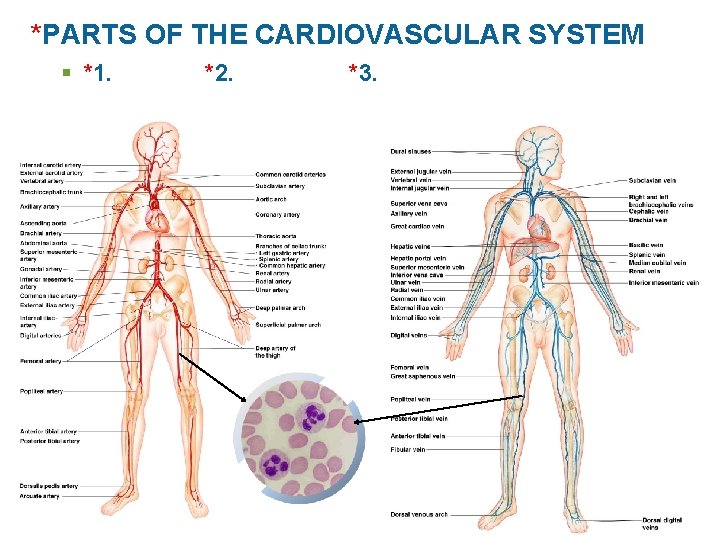
*PARTS OF THE CARDIOVASCULAR SYSTEM § *1. *2. *3.
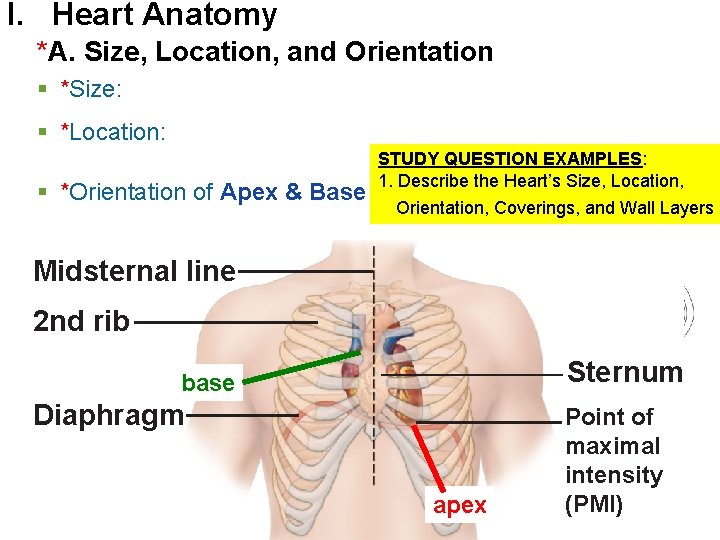
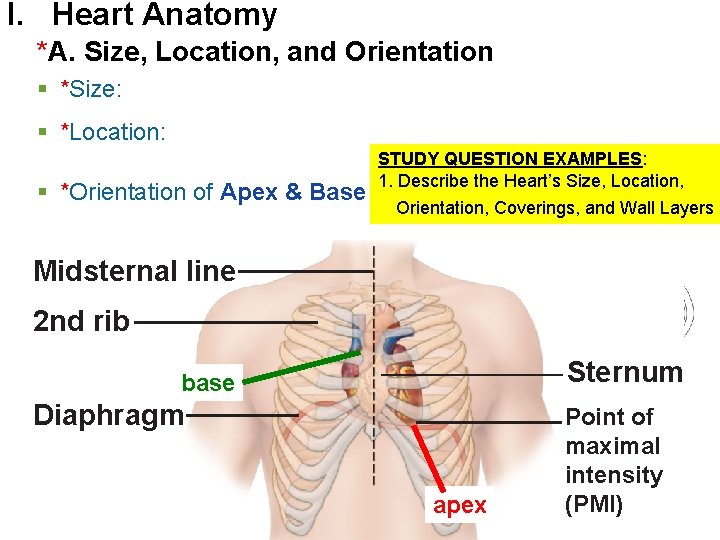
I. Heart Anatomy *A. Size, Location, and Orientation § *Size: § *Location: § *Orientation of Apex & Base STUDY QUESTION EXAMPLES: 1. Describe the Heart’s Size, Location, Orientation, Coverings, and Wall Layers Midsternal line 2 nd rib Sternum base Diaphragm apex Point of maximal intensity (PMI)
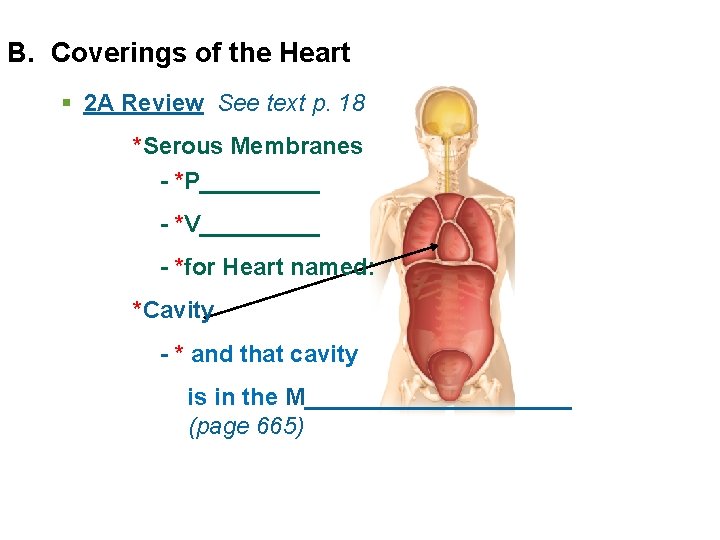
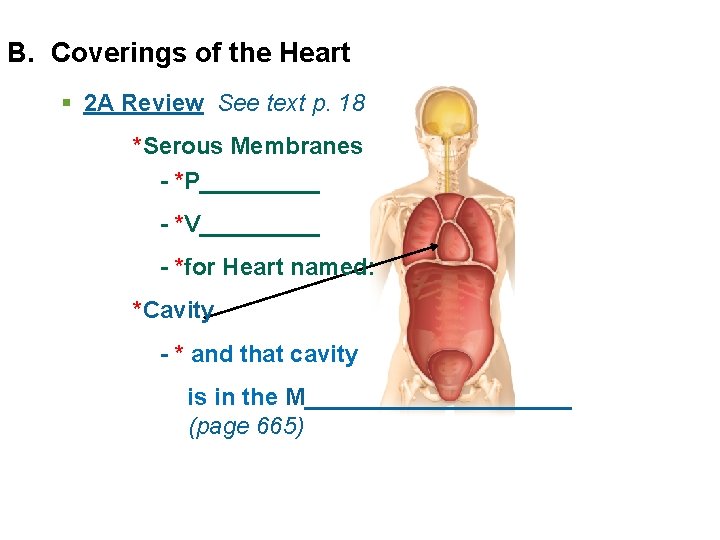
B. Coverings of the Heart § 2 A Review See text p. 18 *Serous Membranes - *P_____ - *V_____ - *for Heart named: *Cavity - * and that cavity is in the M__________ (page 665)
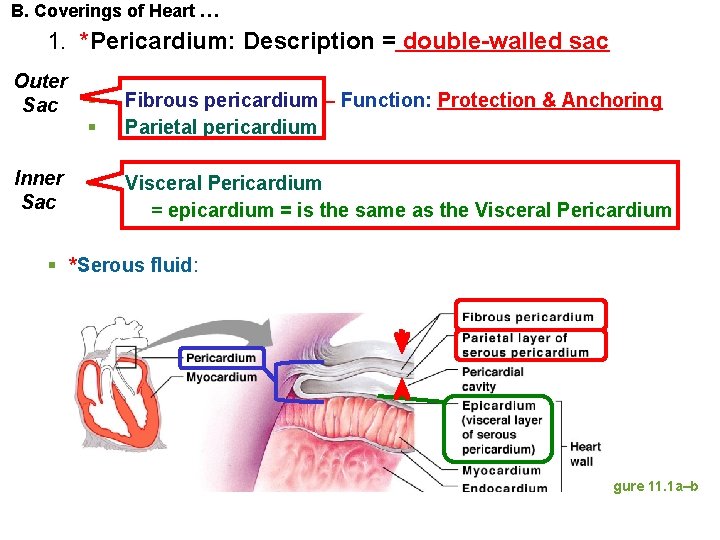
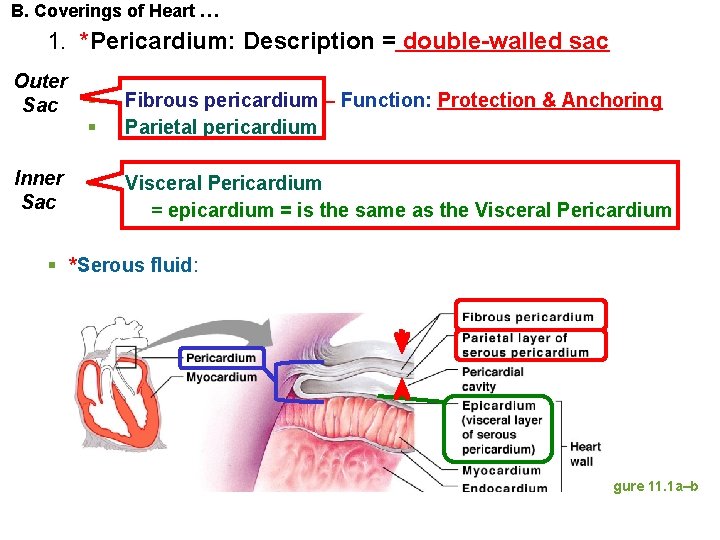
B. Coverings of Heart … 1. *Pericardium: Description = double-walled sac Outer Sac Inner Sac § § Fibrous pericardium – Function: Protection & Anchoring Parietal pericardium § Visceral Pericardium = epicardium = is the same as the Visceral Pericardium § *Serous fluid: Figure 11. 1 a–b
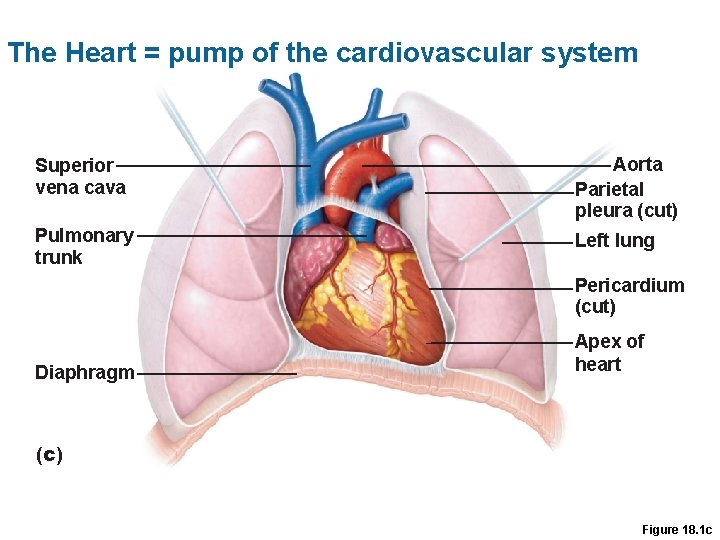
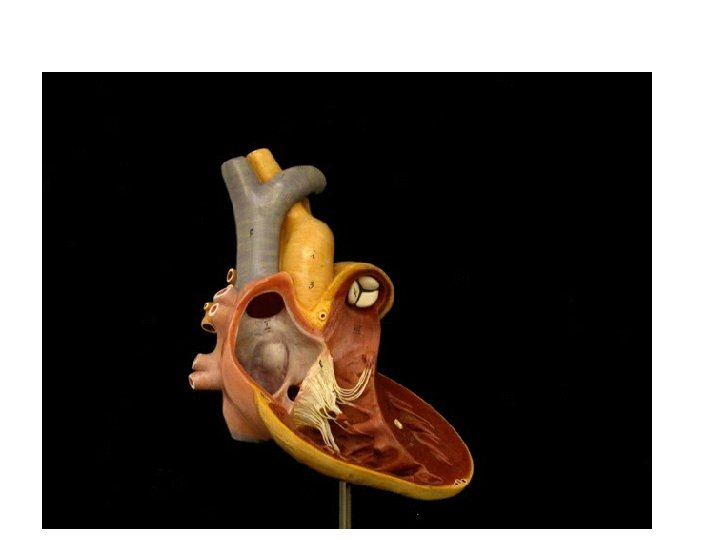
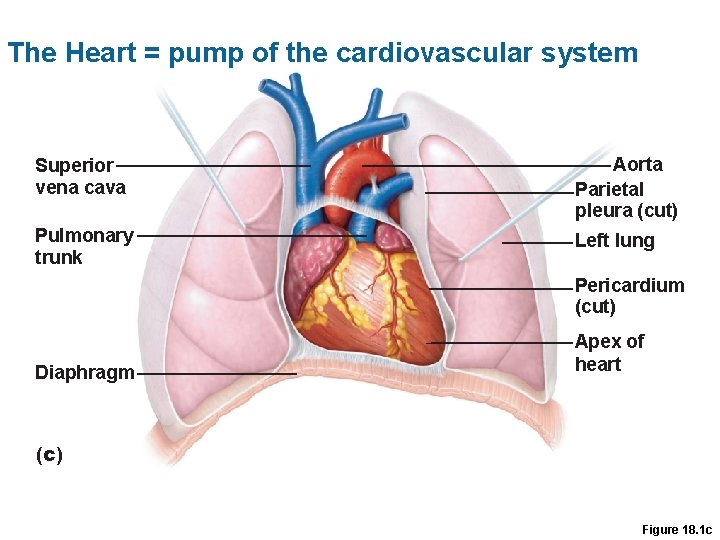
The Heart = pump of the cardiovascular system Superior vena cava Aorta Parietal pleura (cut) Pulmonary trunk Left lung Pericardium (cut) Diaphragm Apex of heart (c) Figure 18. 1 c
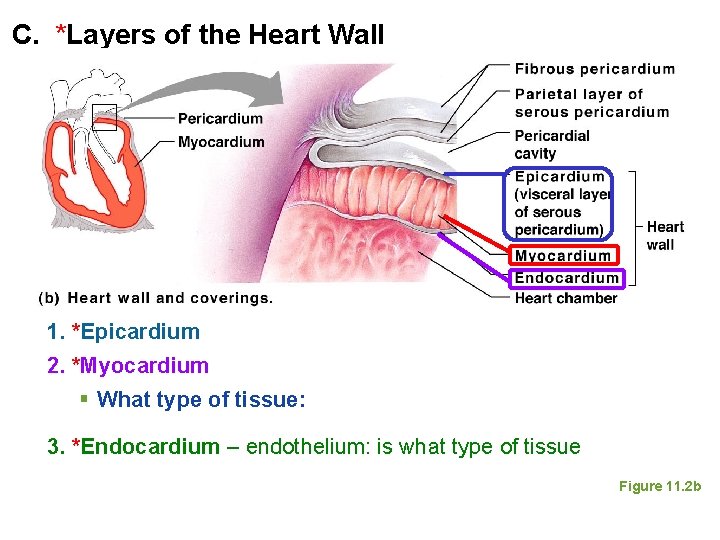
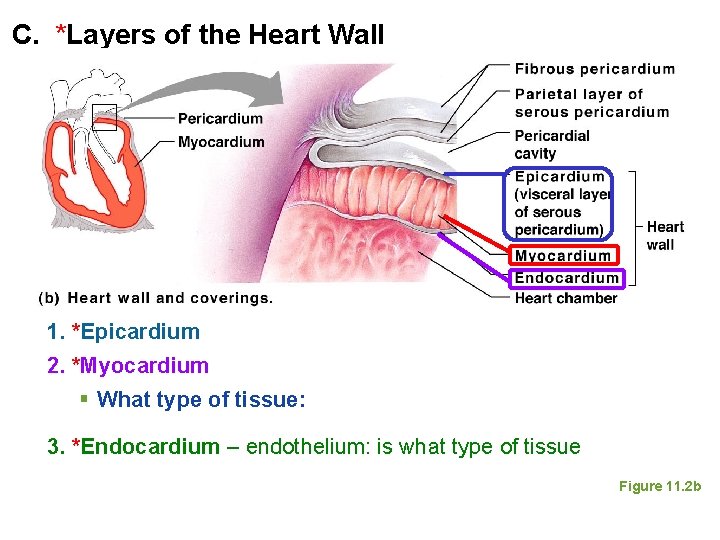
C. *Layers of the Heart Wall 1. *Epicardium 2. *Myocardium § What type of tissue: 3. *Endocardium – endothelium: is what type of tissue Figure 11. 2 b
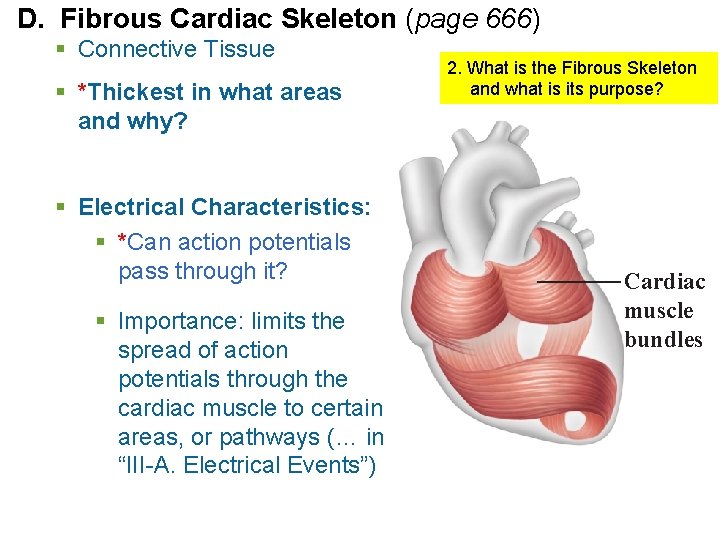
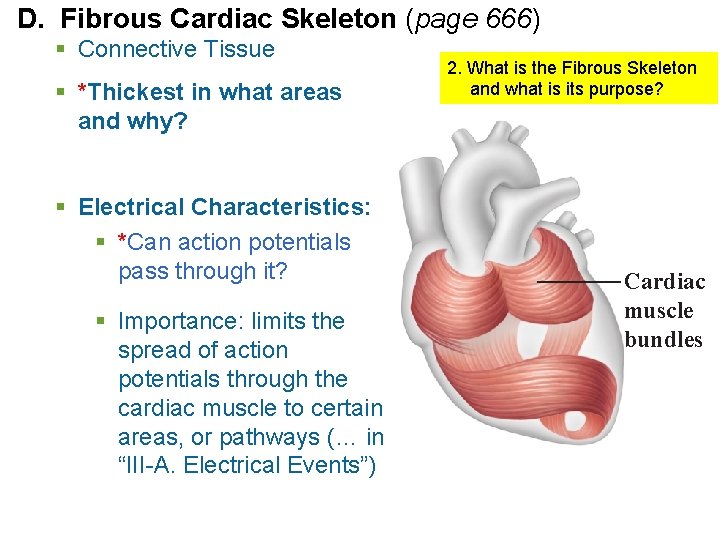
D. Fibrous Cardiac Skeleton (page 666) § Connective Tissue § *Thickest in what areas and why? § Electrical Characteristics: § *Can action potentials pass through it? § Importance: limits the spread of action potentials through the cardiac muscle to certain areas, or pathways (… in “III-A. Electrical Events”) 2. What is the Fibrous Skeleton and what is its purpose? Cardiac muscle bundles
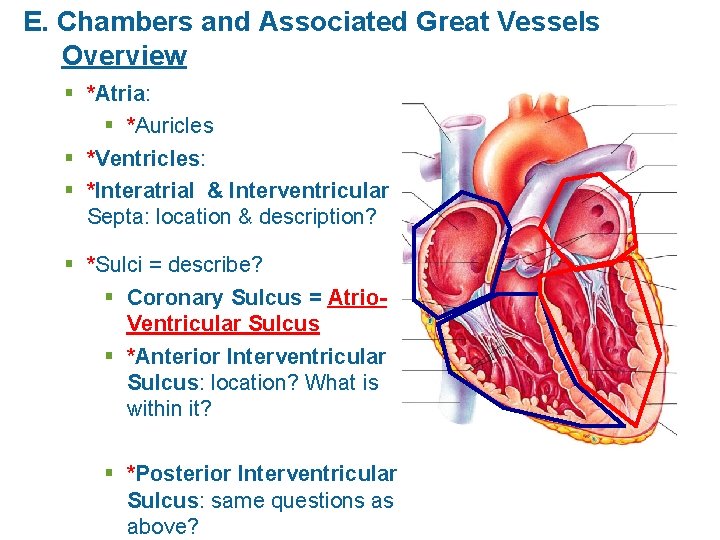
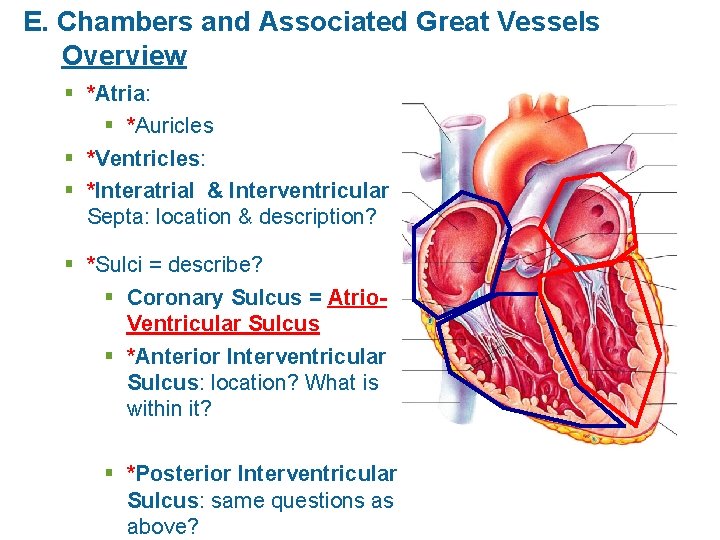
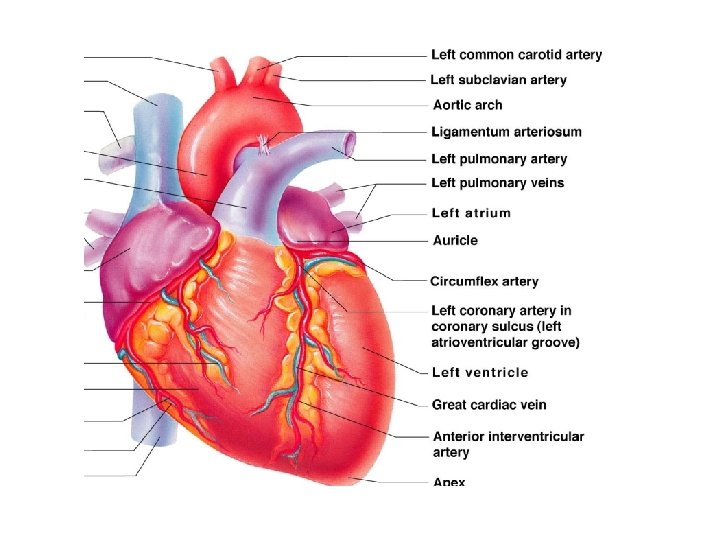
E. Chambers and Associated Great Vessels Overview § *Atria: § *Auricles § *Ventricles: § *Interatrial & Interventricular Septa: location & description? § *Sulci = describe? § Coronary Sulcus = Atrio. Ventricular Sulcus § *Anterior Interventricular Sulcus: location? What is within it? § *Posterior Interventricular Sulcus: same questions as above?
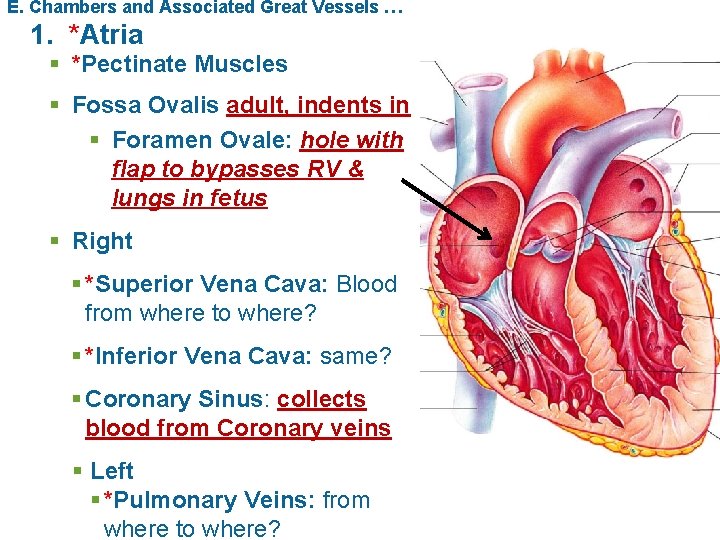
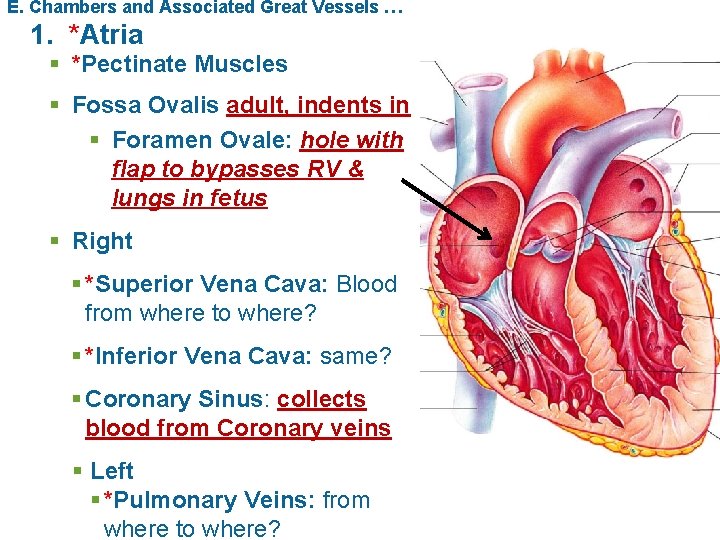
E. Chambers and Associated Great Vessels … 1. *Atria § *Pectinate Muscles § Fossa Ovalis adult, indents in § Foramen Ovale: hole with flap to bypasses RV & lungs in fetus § Right § *Superior Vena Cava: Blood from where to where? § *Inferior Vena Cava: same? § Coronary Sinus: collects blood from Coronary veins § Left § *Pulmonary Veins: from where to where?
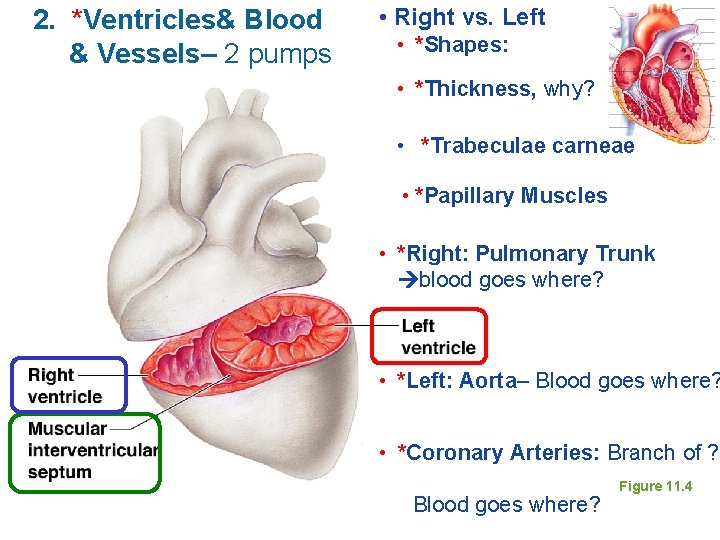
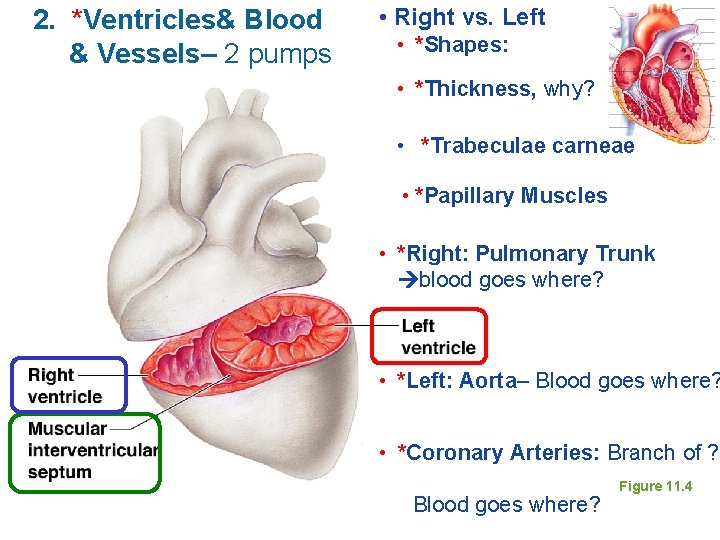
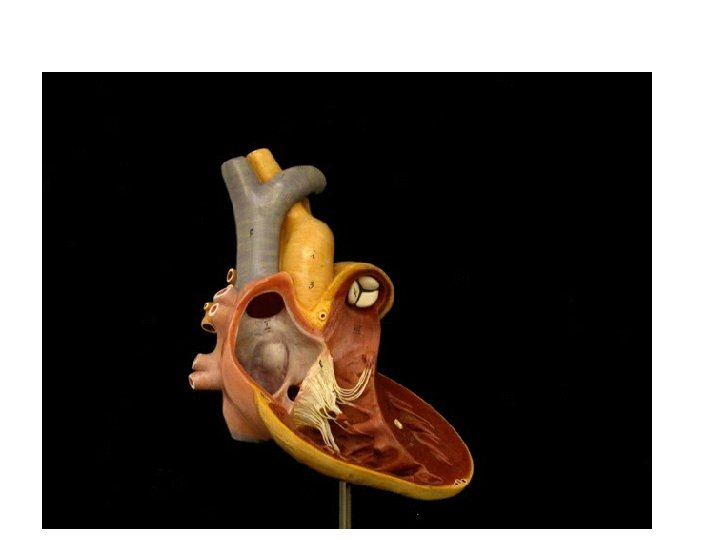
2. *Ventricles& Blood & Vessels– 2 pumps • Right vs. Left • *Shapes: • *Thickness, why? • *Trabeculae carneae • *Papillary Muscles • *Right: Pulmonary Trunk blood goes where? • *Left: Aorta– Blood goes where? • *Coronary Arteries: Branch of ? Blood goes where? Figure 11. 4
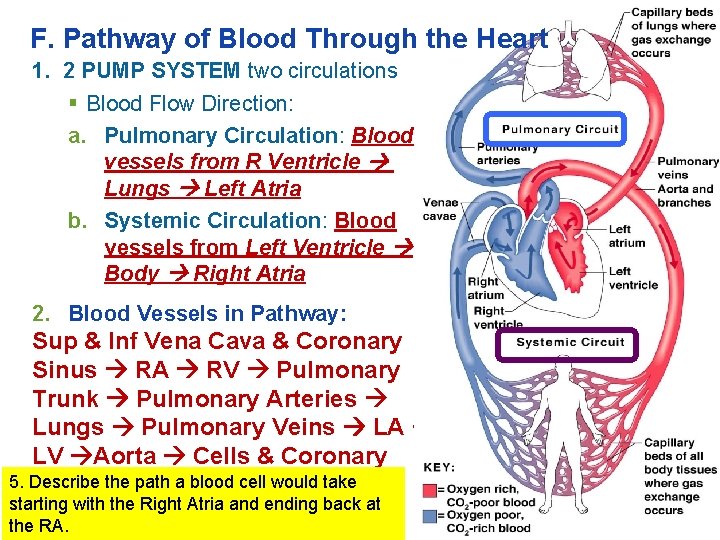
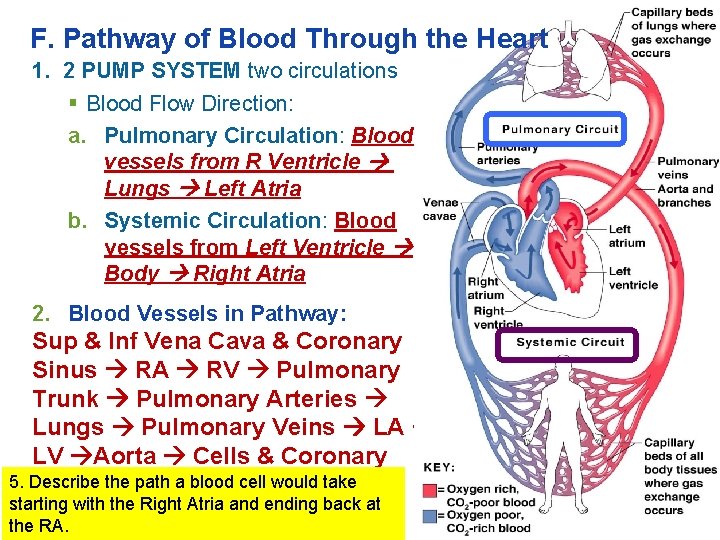
F. Pathway of Blood Through the Heart 1. 2 PUMP SYSTEM two circulations § Blood Flow Direction: a. Pulmonary Circulation: Blood vessels from R Ventricle Lungs Left Atria b. Systemic Circulation: Blood vessels from Left Ventricle Body Right Atria 2. Blood Vessels in Pathway: Sup & Inf Vena Cava & Coronary Sinus RA RV Pulmonary Trunk Pulmonary Arteries Lungs Pulmonary Veins LA LV Aorta Cells & Coronary 5. Describe the path a blood cell would take Arteries starting with the Right Atria and ending back at the RA.
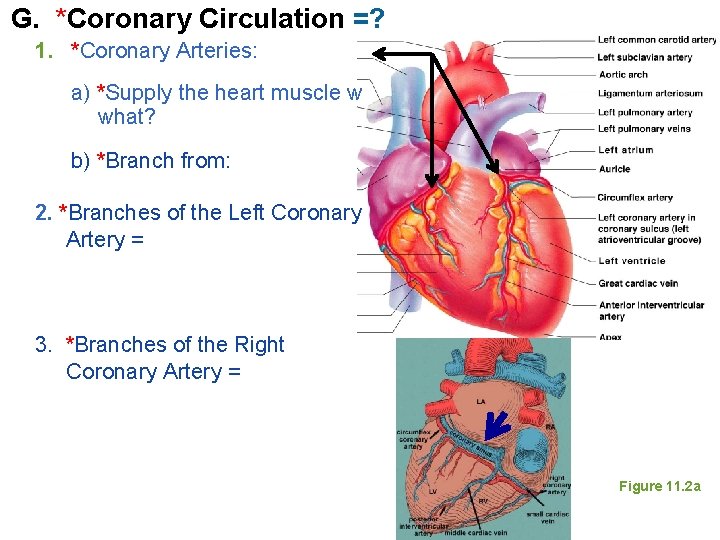
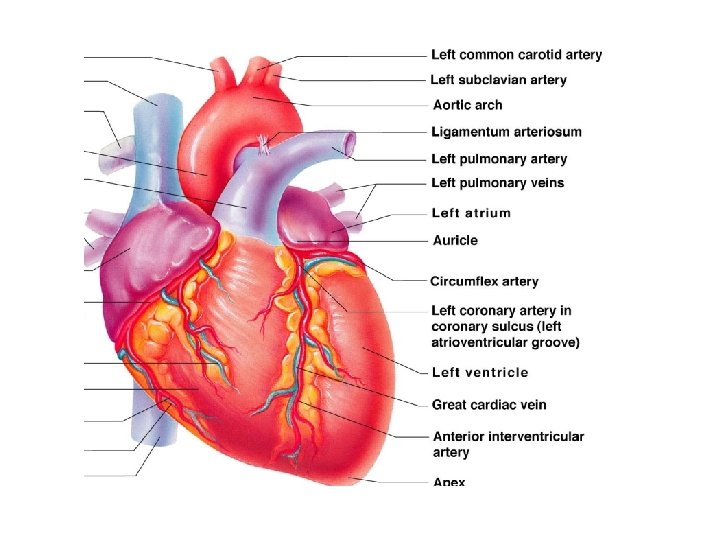
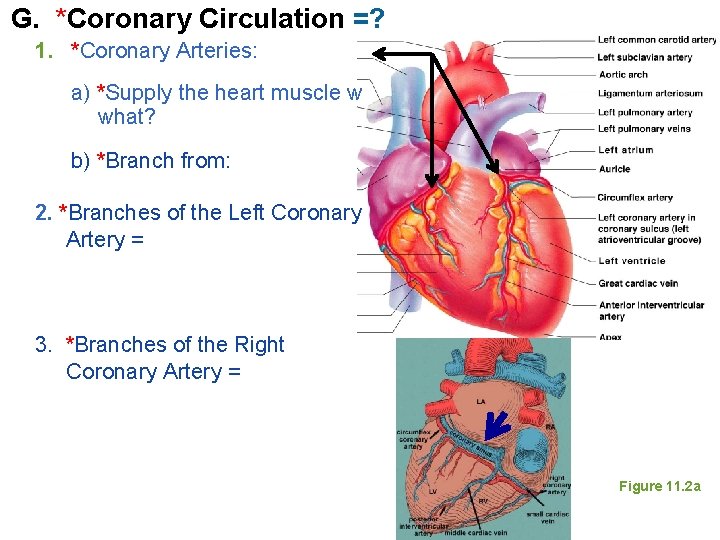
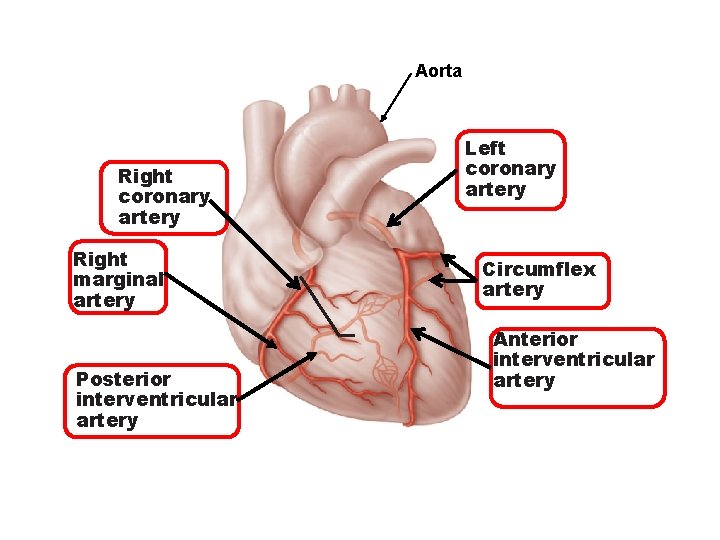
G. *Coronary Circulation =? 1. *Coronary Arteries: a) *Supply the heart muscle w what? b) *Branch from: 2. *Branches of the Left Coronary Artery = 3. *Branches of the Right Coronary Artery = Figure 11. 2 a
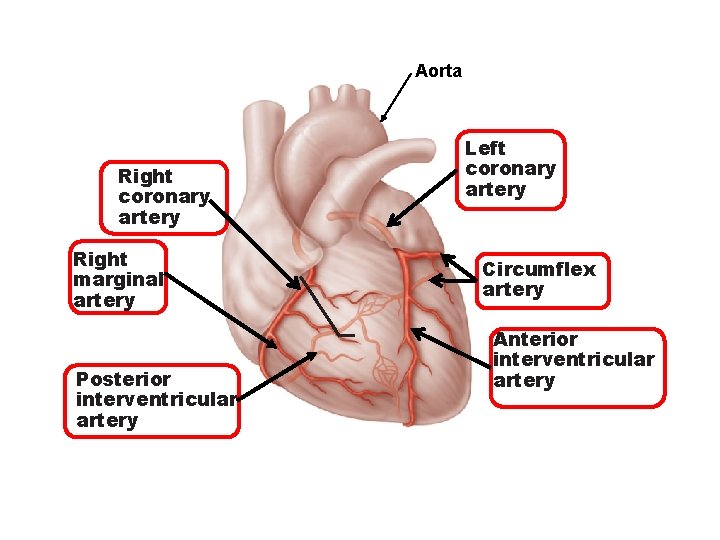
Aorta Right coronary artery Right marginal artery Posterior interventricular artery Left coronary artery Circumflex artery Anterior interventricular artery Figure 18. 7 a
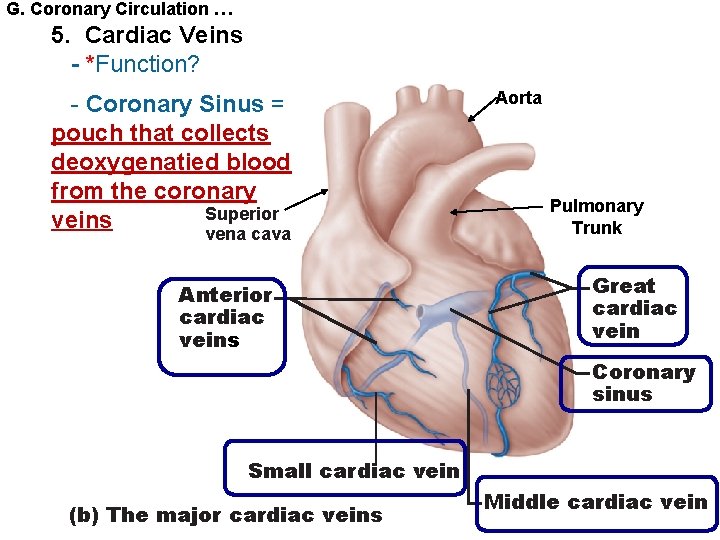
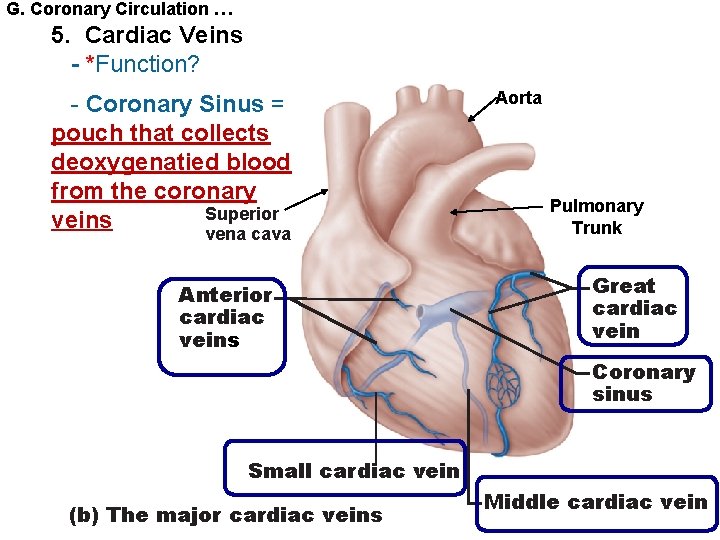
G. Coronary Circulation … 5. Cardiac Veins - *Function? - Coronary Sinus = pouch that collects deoxygenatied blood from the coronary Superior veins vena cava Anterior cardiac veins Aorta Pulmonary Trunk Great cardiac vein Coronary sinus Small cardiac vein (b) The major cardiac veins Middle cardiac vein
6. Homeostatic Imbalances STUDENTS DO § *Angina pectoris § *Myocardial Infarction (heart attack)
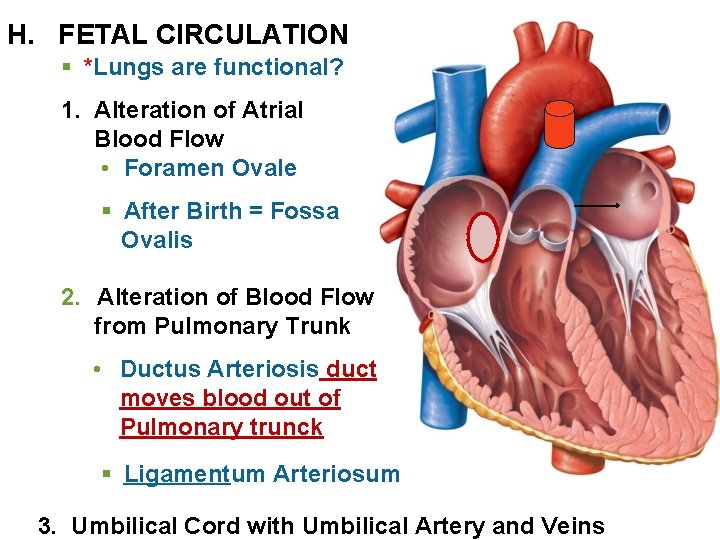
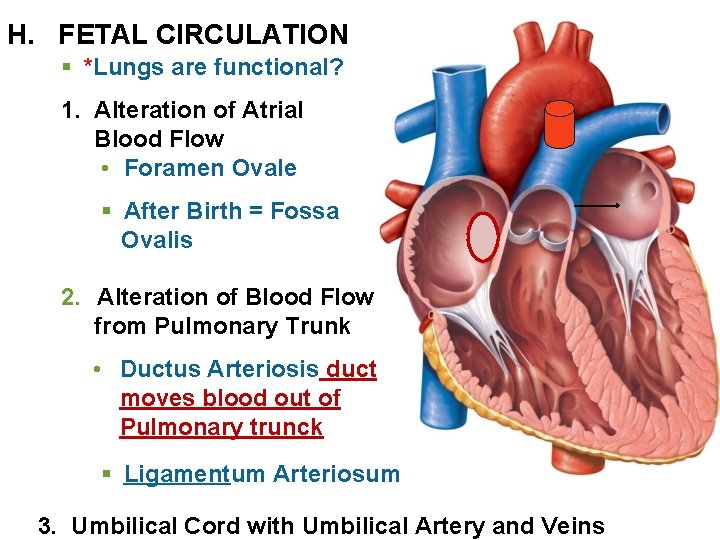
H. FETAL CIRCULATION § *Lungs are functional? 1. Alteration of Atrial Blood Flow • Foramen Ovale § After Birth = Fossa Ovalis 2. Alteration of Blood Flow from Pulmonary Trunk • Ductus Arteriosis duct moves blood out of Pulmonary trunck § Ligamentum Arteriosum 3. Umbilical Cord with Umbilical Artery and Veins
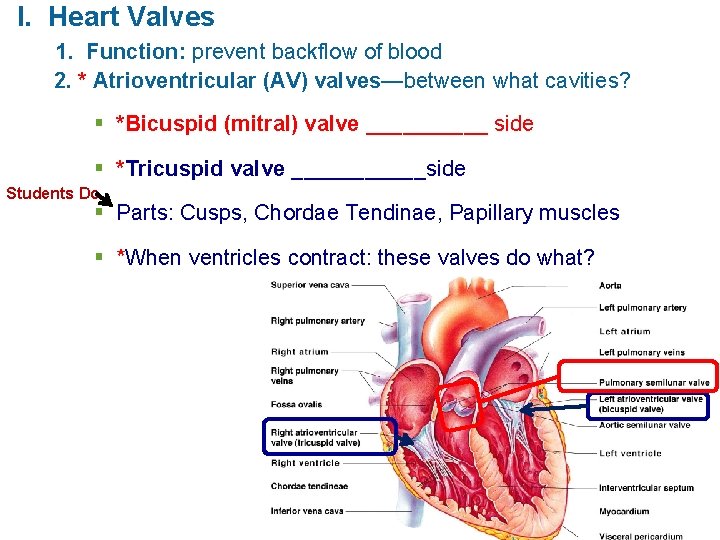
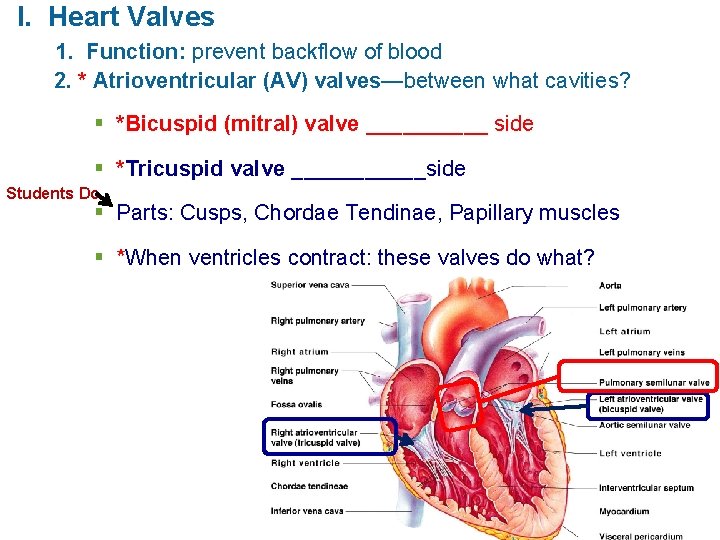
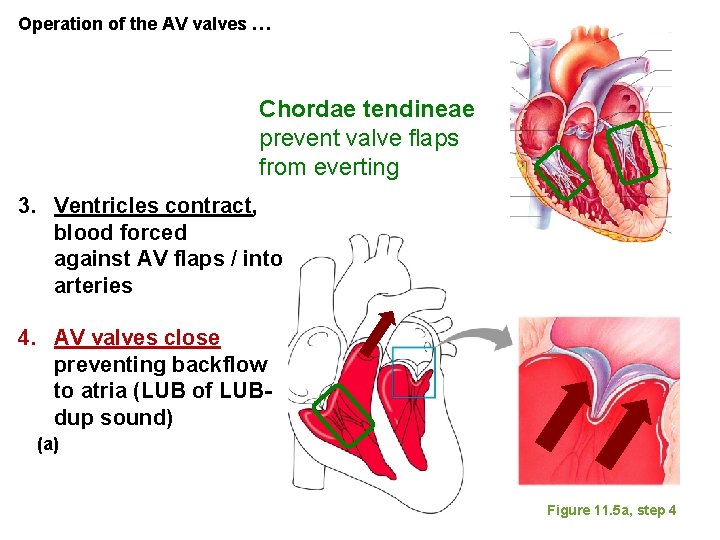
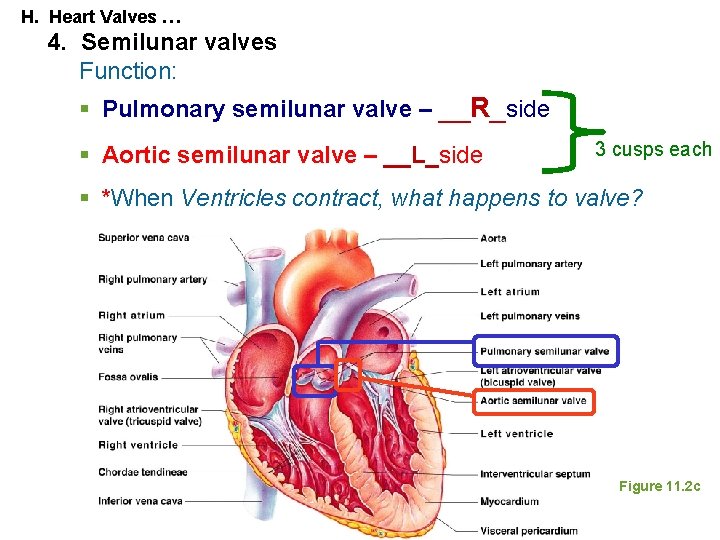
I. Heart Valves 1. Function: prevent backflow of blood 2. * Atrioventricular (AV) valves—between what cavities? § *Bicuspid (mitral) valve _____ side § *Tricuspid valve ______side Students Do § Parts: Cusps, Chordae Tendinae, Papillary muscles § *When ventricles contract: these valves do what?
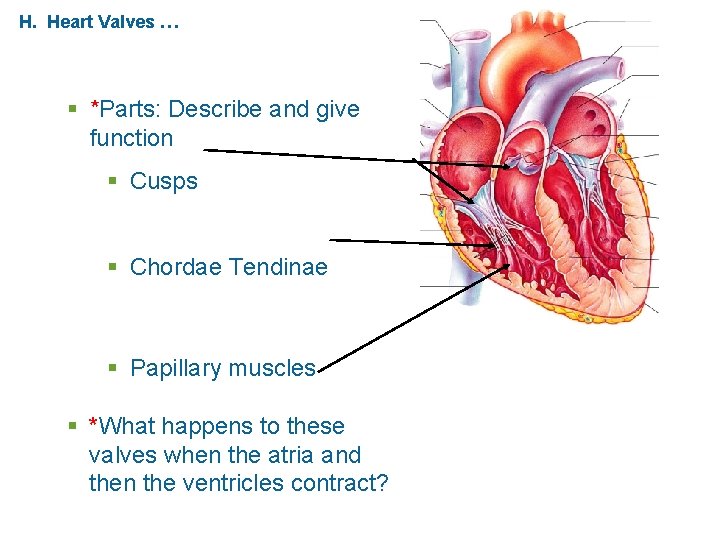
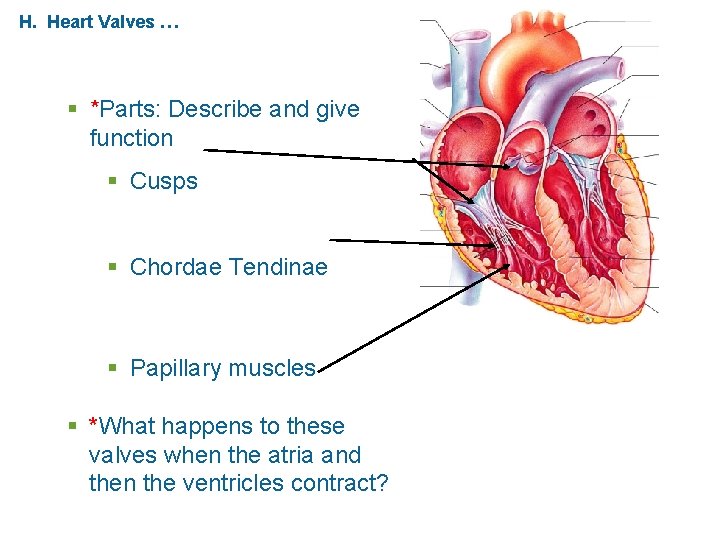
H. Heart Valves … § *Parts: Describe and give function § Cusps § Chordae Tendinae § Papillary muscles § *What happens to these valves when the atria and then the ventricles contract?
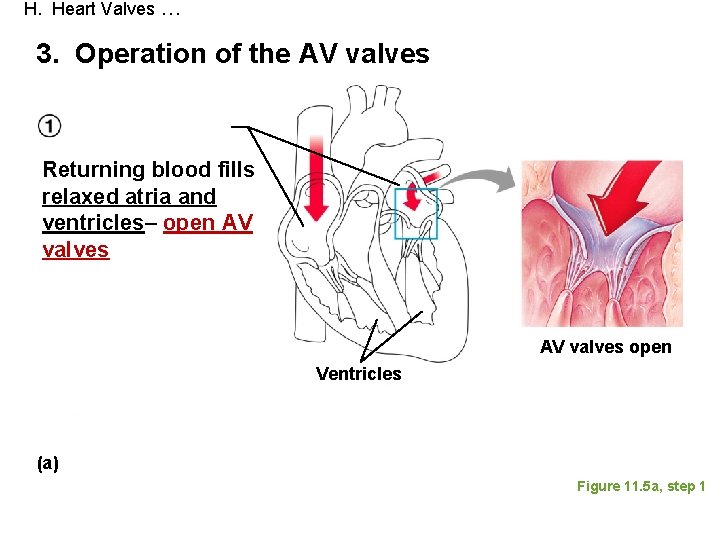
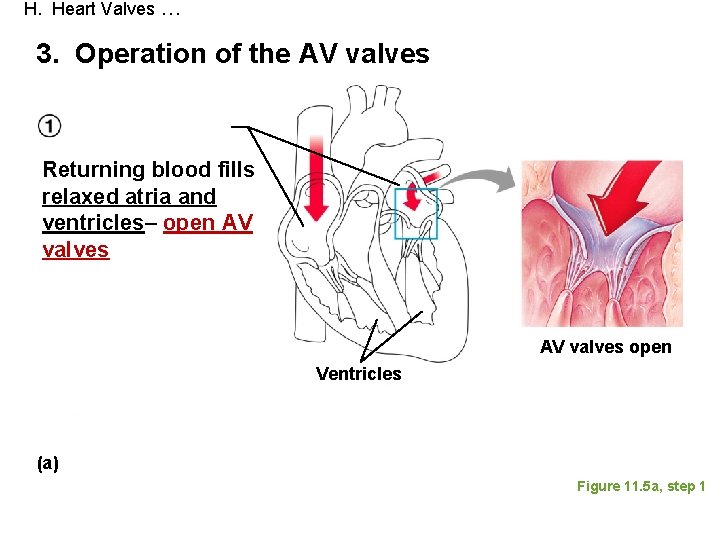
H. Heart Valves … 3. Operation of the AV valves Returning blood fills relaxed atria and ventricles– open AV valves open Ventricles (a) Figure 11. 5 a, step 1
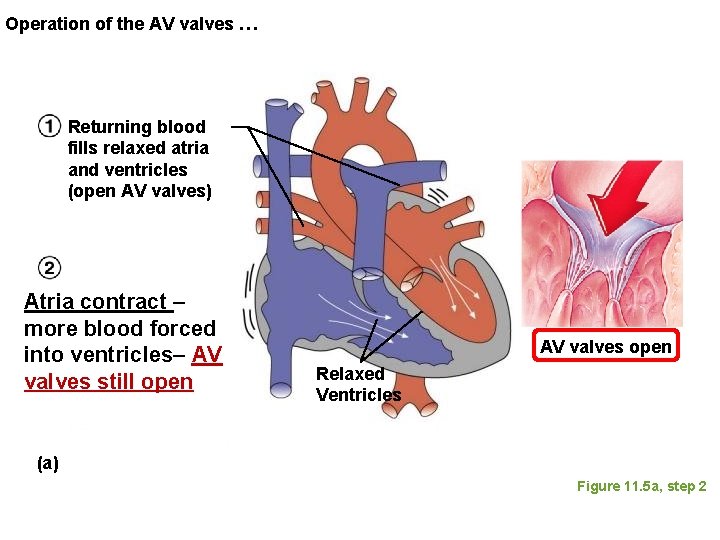
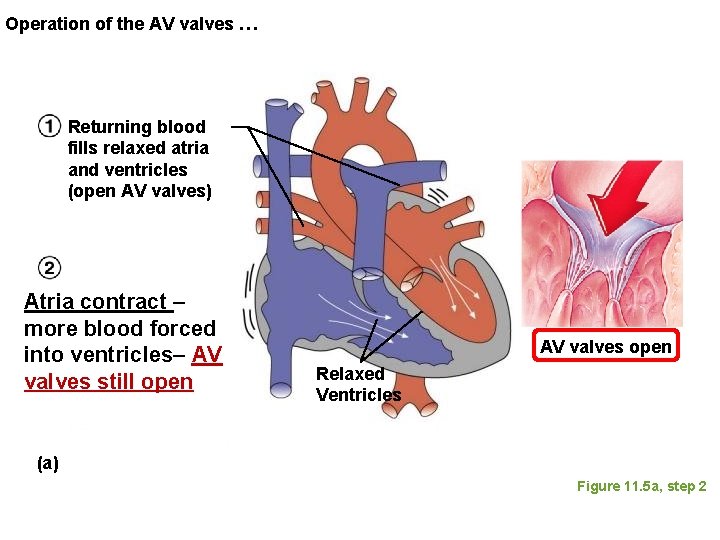
Operation of the AV valves … Returning blood fills relaxed atria and ventricles (open AV valves) Atria contract – more blood forced into ventricles– AV valves still open AV valves open Relaxed Ventricles (a) Figure 11. 5 a, step 2
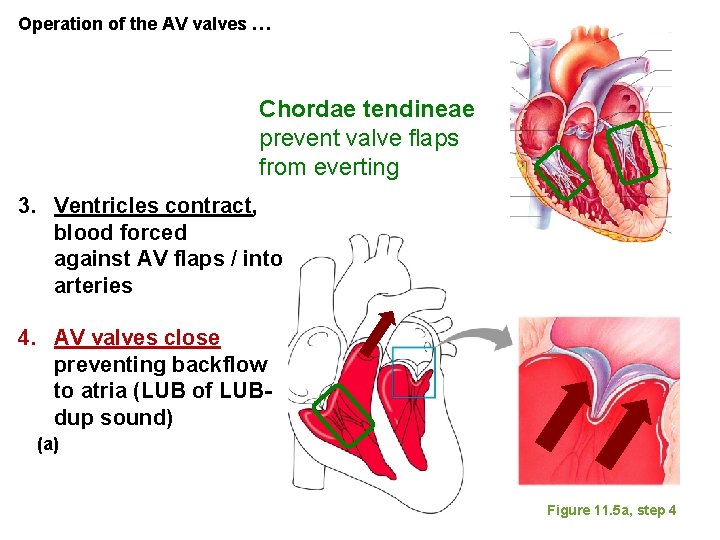
Operation of the AV valves … Chordae tendineae prevent valve flaps from everting 3. Ventricles contract, blood forced against AV flaps / into arteries 4. AV valves close preventing backflow to atria (LUB of LUBdup sound) (a) Figure 11. 5 a, step 4
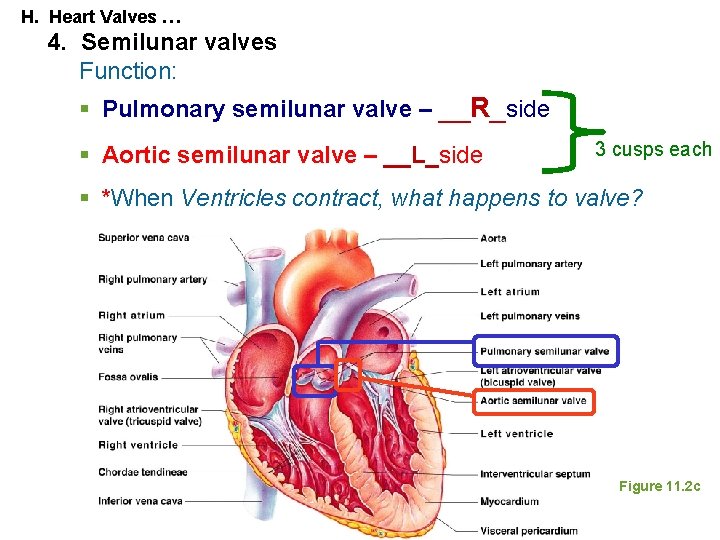
H. Heart Valves … 4. Semilunar valves Function: § Pulmonary semilunar valve – __R_side § Aortic semilunar valve – __L_side 3 cusps each § *When Ventricles contract, what happens to valve? Figure 11. 2 c
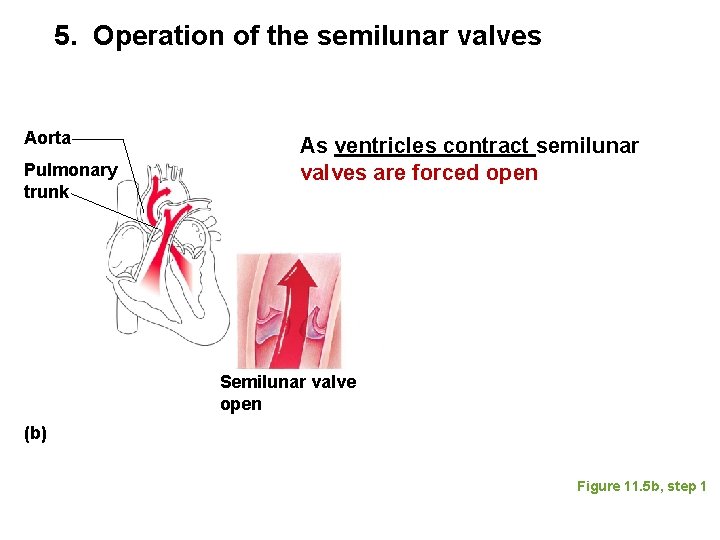
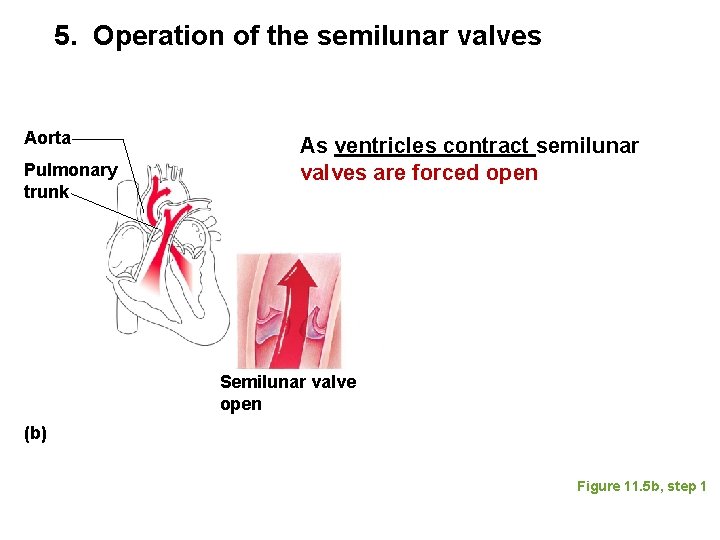
5. Operation of the semilunar valves Aorta Pulmonary trunk As ventricles contract semilunar valves are forced open Semilunar valve open (b) Figure 11. 5 b, step 1
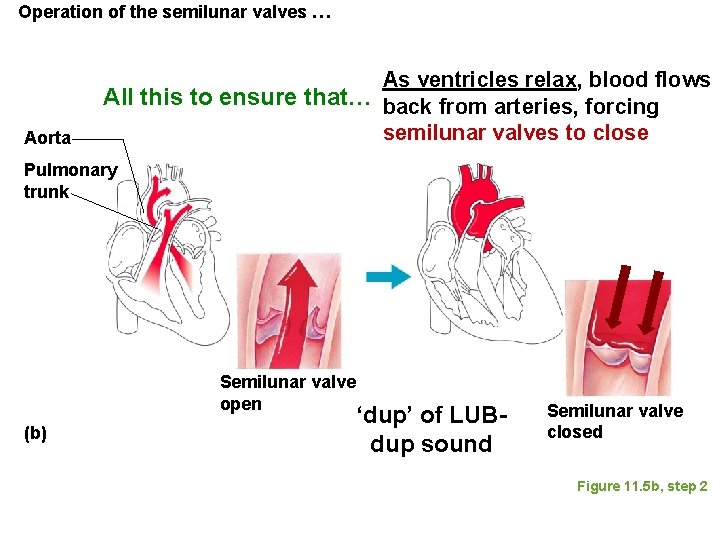
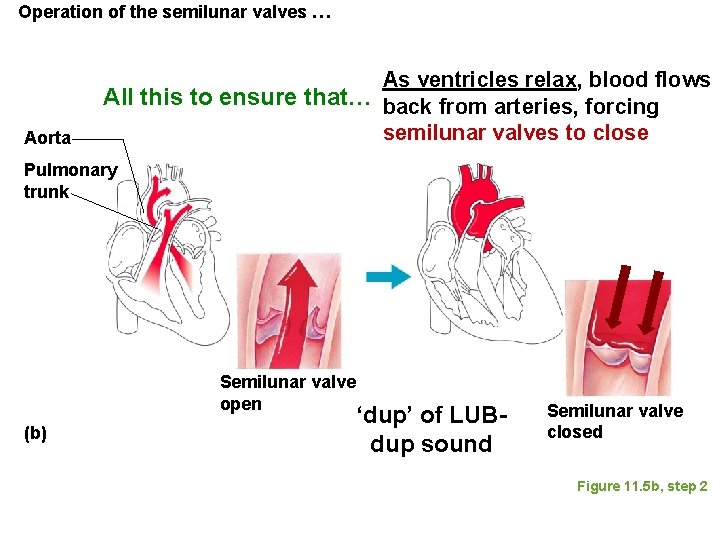
Operation of the semilunar valves … Aorta As ventricles relax, blood flows All this to ensure that… back from arteries, forcing semilunar valves to close Pulmonary trunk Semilunar valve open (b) ‘dup’ of LUBdup sound Semilunar valve closed Figure 11. 5 b, step 2
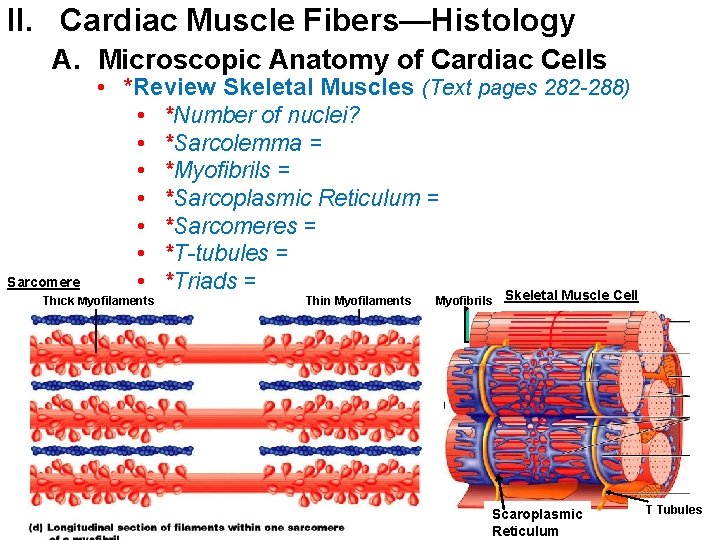
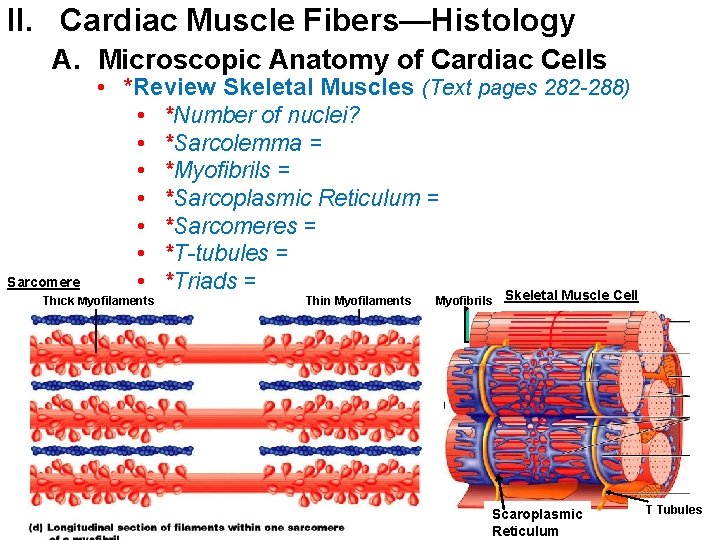
II. Cardiac Muscle Fibers—Histology A. Microscopic Anatomy of Cardiac Cells Sarcomere • *Review Skeletal Muscles (Text pages 282 -288) • *Number of nuclei? • *Sarcolemma = • *Myofibrils = • *Sarcoplasmic Reticulum = • *Sarcomeres = • *T-tubules = • *Triads = Skeletal Muscle Cell Thick Myofilaments Thin Myofilaments Myofibrils Scaroplasmic Reticulum T Tubules
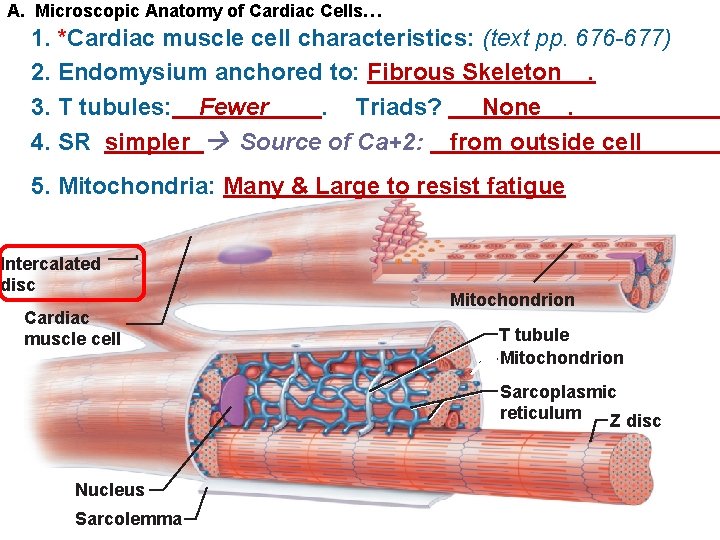
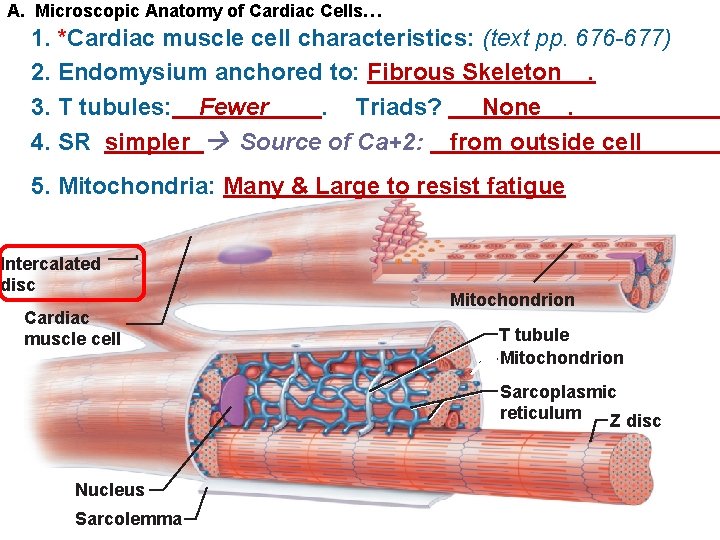
A. Microscopic Anatomy of Cardiac Cells… 1. *Cardiac muscle cell characteristics: (text pp. 676 -677) 2. Endomysium anchored to: Fibrous Skeleton. 3. T tubules: Fewer. Triads? None. 4. SR simpler Source of Ca+2: from outside cell 5. Mitochondria: Many & Large to resist fatigue Intercalated disc Cardiac muscle cell Mitochondrion T tubule Mitochondrion Sarcoplasmic reticulum Z disc Nucleus Sarcolemma
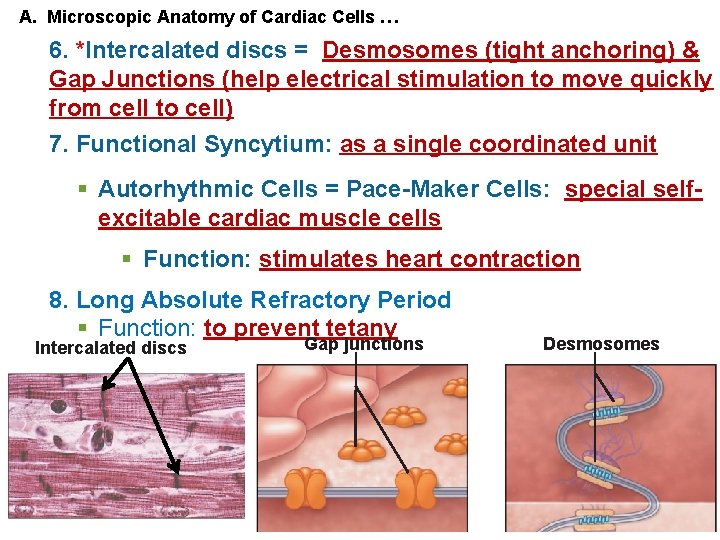
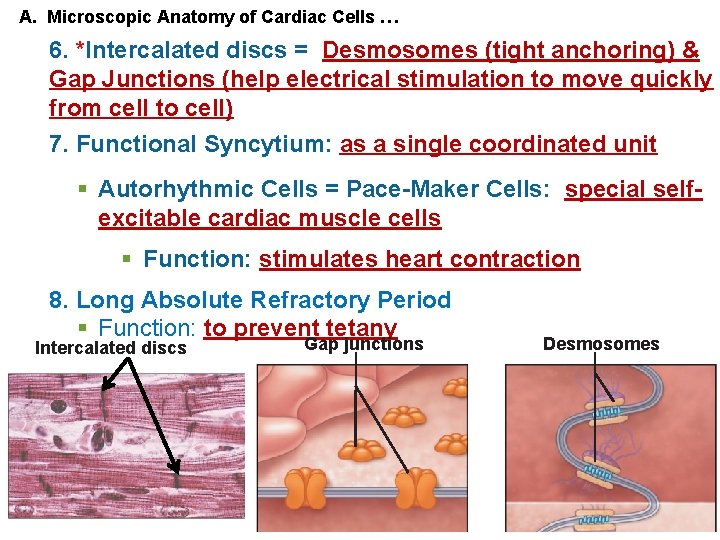
A. Microscopic Anatomy of Cardiac Cells … 6. *Intercalated discs = Desmosomes (tight anchoring) & Gap Junctions (help electrical stimulation to move quickly from cell to cell) 7. Functional Syncytium: as a single coordinated unit § Autorhythmic Cells = Pace-Maker Cells: special selfexcitable cardiac muscle cells § Function: stimulates heart contraction 8. Long Absolute Refractory Period § Function: to prevent tetany Intercalated discs Gap junctions Desmosomes
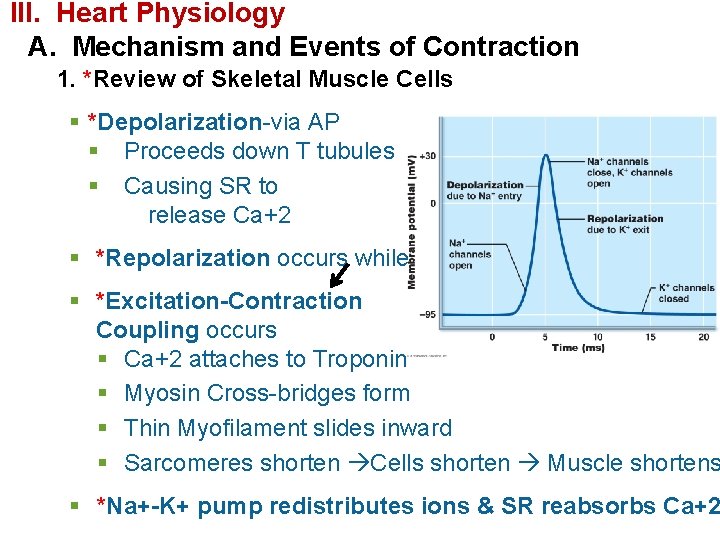
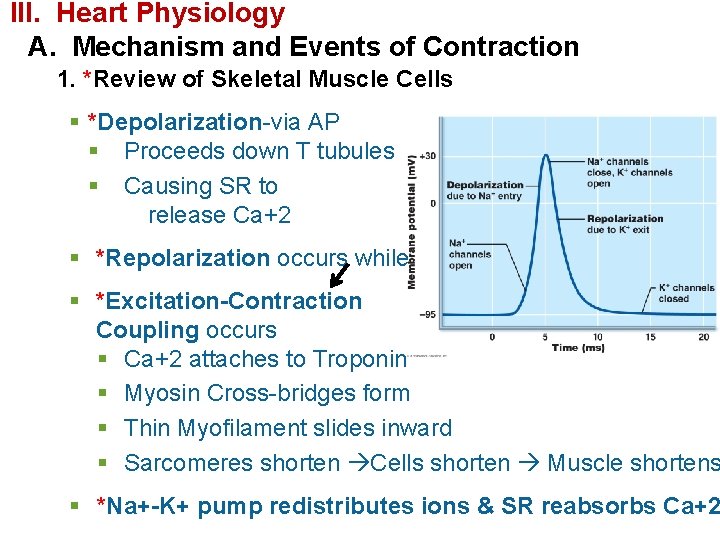
III. Heart Physiology A. Mechanism and Events of Contraction 1. *Review of Skeletal Muscle Cells § *Depolarization-via AP § Proceeds down T tubules § Causing SR to release Ca+2 § *Repolarization occurs while § *Excitation-Contraction Coupling occurs § Ca+2 attaches to Troponin § Myosin Cross-bridges form § Thin Myofilament slides inward § Sarcomeres shorten Cells shorten Muscle shortens § *Na+-K+ pump redistributes ions & SR reabsorbs Ca+2
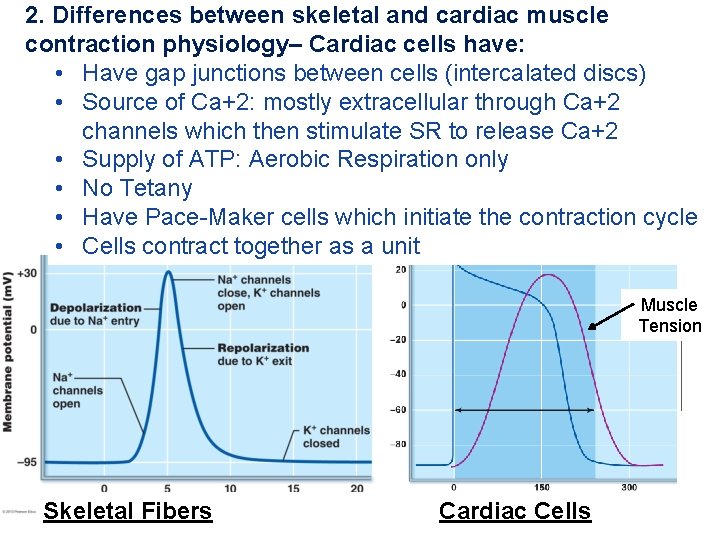
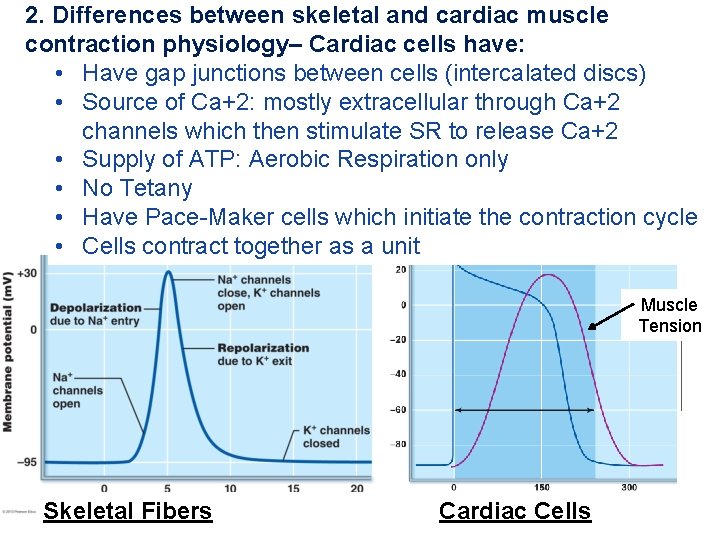
2. Differences between skeletal and cardiac muscle contraction physiology– Cardiac cells have: • Have gap junctions between cells (intercalated discs) • Source of Ca+2: mostly extracellular through Ca+2 channels which then stimulate SR to release Ca+2 • Supply of ATP: Aerobic Respiration only • No Tetany • Have Pace-Maker cells which initiate the contraction cycle • Cells contract together as a unit Muscle Tension Skeletal Fibers Cardiac Cells
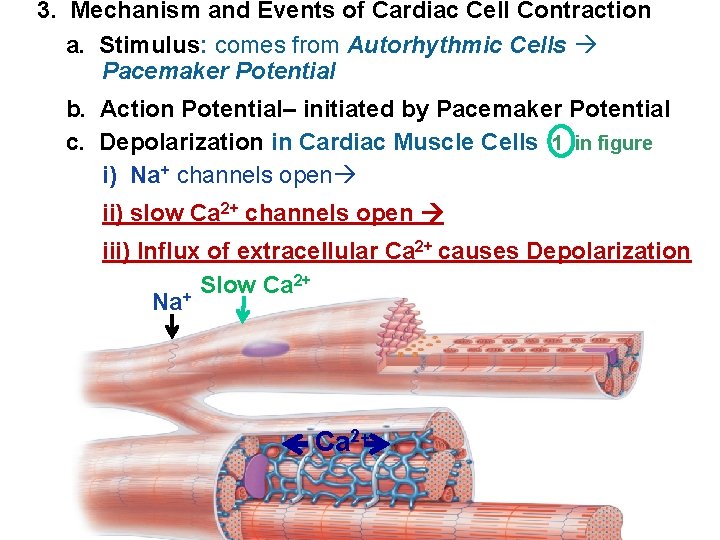
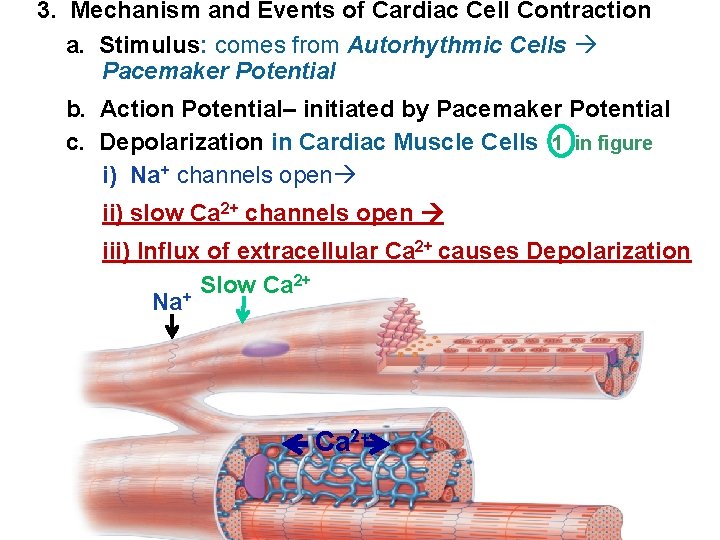
3. Mechanism and Events of Cardiac Cell Contraction a. Stimulus: comes from Autorhythmic Cells Pacemaker Potential b. Action Potential– initiated by Pacemaker Potential c. Depolarization in Cardiac Muscle Cells 1 in figure i) Na+ channels open ii) slow Ca 2+ channels open iii) Influx of extracellular Ca 2+ causes Depolarization 2+ Slow Ca Na+ Ca 2+
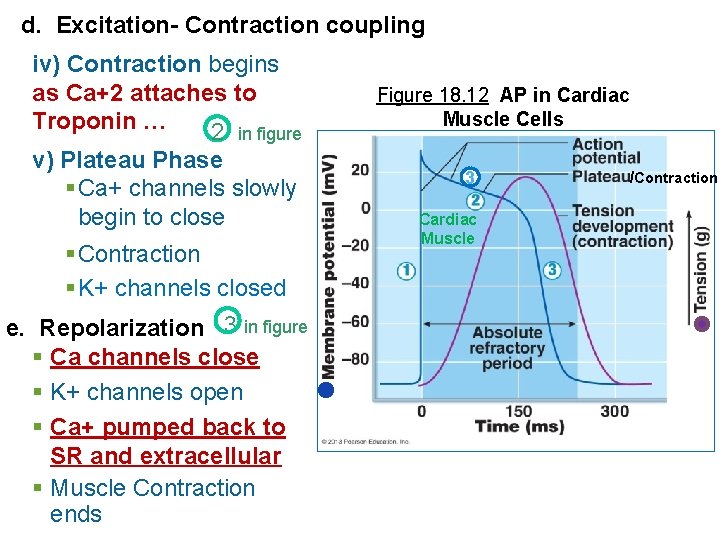
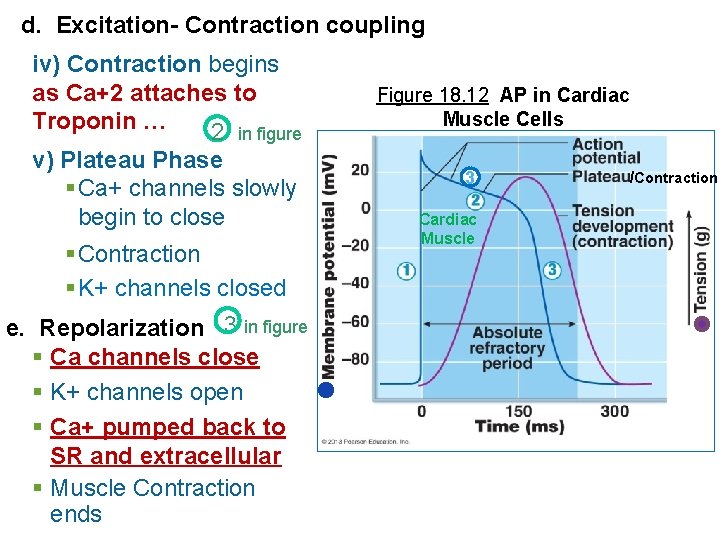
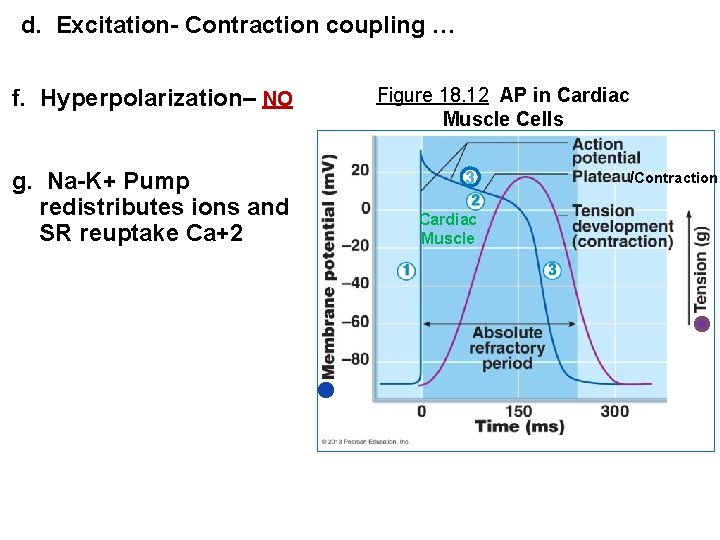
d. Excitation- Contraction coupling iv) Contraction begins as Ca+2 attaches to Troponin … 2 in figure v) Plateau Phase § Ca+ channels slowly begin to close § Contraction § K+ channels closed e. Repolarization 3 in figure § Ca channels close § K+ channels open § Ca+ pumped back to SR and extracellular § Muscle Contraction ends Figure 18. 12 AP in Cardiac Muscle Cells 3 Cardiac Muscle /Contraction
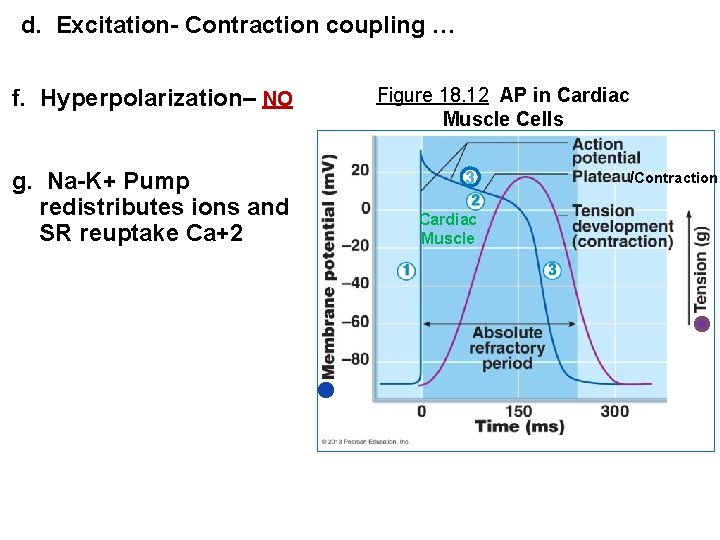
d. Excitation- Contraction coupling … f. Hyperpolarization– NO g. Na-K+ Pump redistributes ions and SR reuptake Ca+2 Figure 18. 12 AP in Cardiac Muscle Cells 3 Cardiac Muscle /Contraction
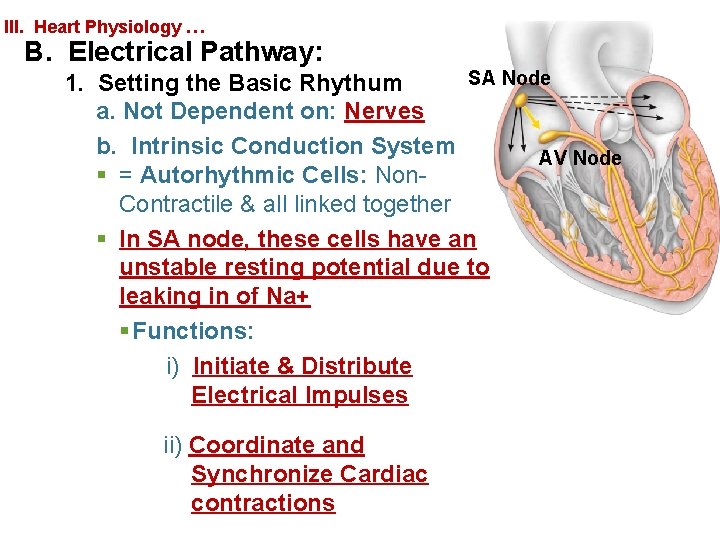
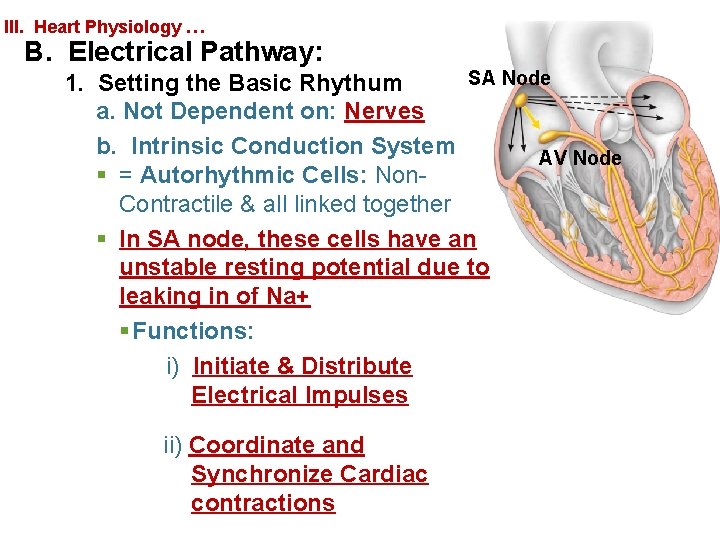
III. Heart Physiology … B. Electrical Pathway: SA Node 1. Setting the Basic Rhythum a. Not Dependent on: Nerves b. Intrinsic Conduction System AV Node § = Autorhythmic Cells: Non. Contractile & all linked together § In SA node, these cells have an unstable resting potential due to leaking in of Na+ § Functions: i) Initiate & Distribute Electrical Impulses ii) Coordinate and Synchronize Cardiac contractions
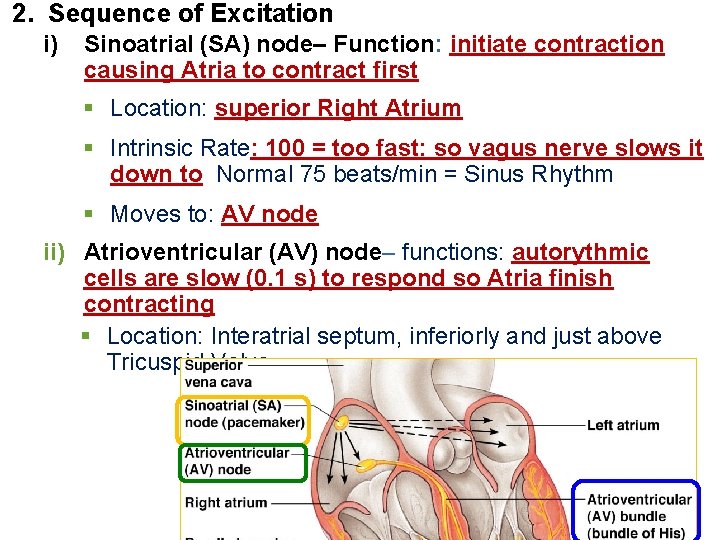
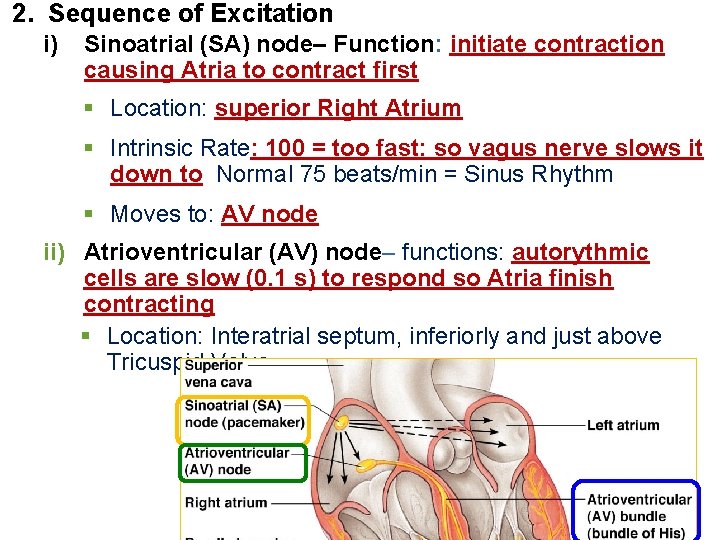
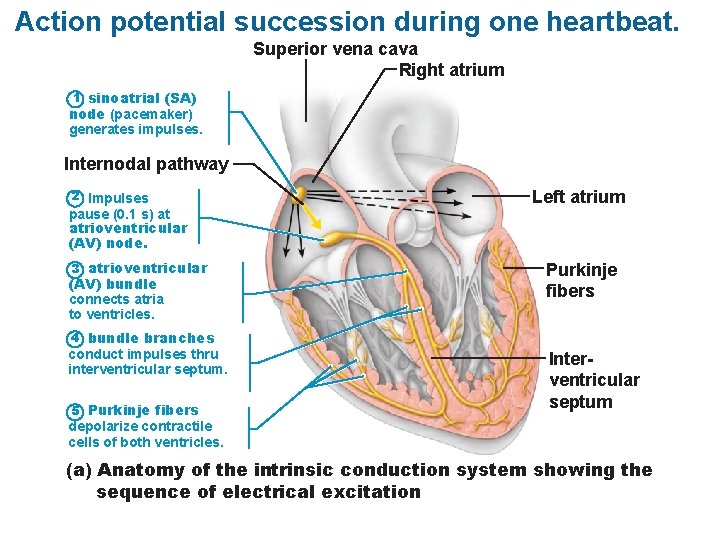
2. Sequence of Excitation i) Sinoatrial (SA) node– Function: initiate contraction causing Atria to contract first § Location: superior Right Atrium § Intrinsic Rate: 100 = too fast: so vagus nerve slows it down to Normal 75 beats/min = Sinus Rhythm § Moves to: AV node ii) Atrioventricular (AV) node– functions: autorythmic cells are slow (0. 1 s) to respond so Atria finish contracting § Location: Interatrial septum, inferiorly and just above Tricuspid Valve
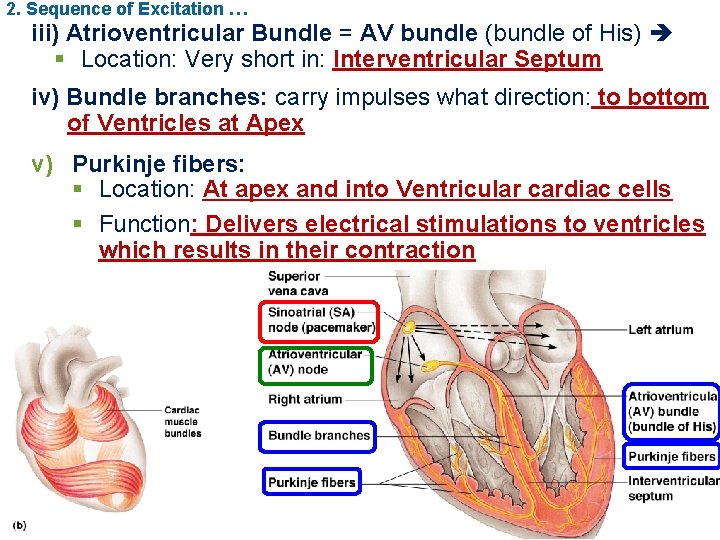
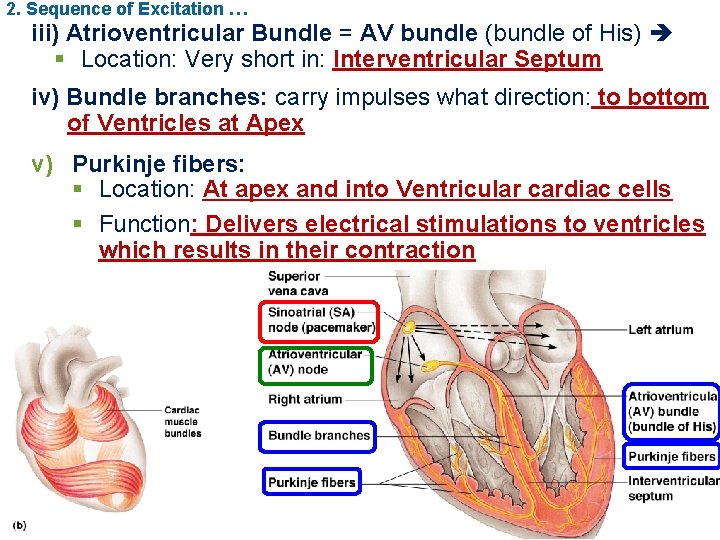
2. Sequence of Excitation … iii) Atrioventricular Bundle = AV bundle (bundle of His) § Location: Very short in: Interventricular Septum iv) Bundle branches: carry impulses what direction: to bottom of Ventricles at Apex v) Purkinje fibers: § Location: At apex and into Ventricular cardiac cells § Function: Delivers electrical stimulations to ventricles which results in their contraction
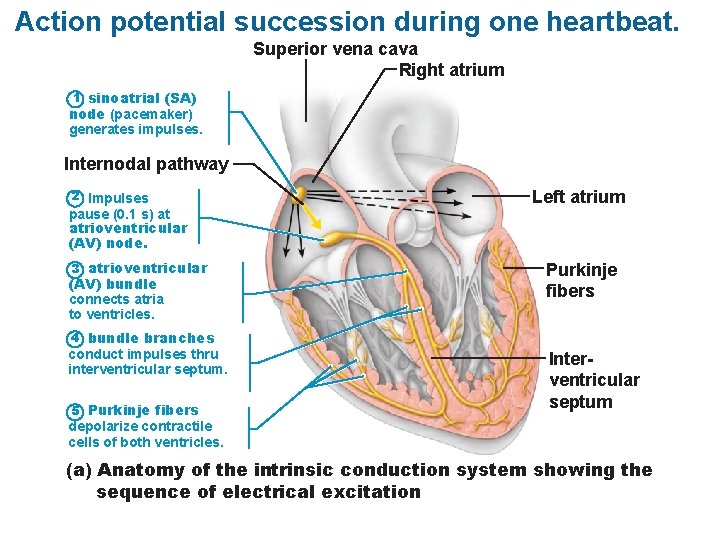
Action potential succession during one heartbeat. Superior vena cava Right atrium 1 sinoatrial (SA) node (pacemaker) generates impulses. Internodal pathway 2 Impulses pause (0. 1 s) at atrioventricular (AV) node. 3 atrioventricular (AV) bundle connects atria to ventricles. Left atrium Purkinje fibers 4 bundle branches conduct impulses thru interventricular septum. 5 Purkinje fibers Interventricular septum depolarize contractile cells of both ventricles. (a) Anatomy of the intrinsic conduction system showing the sequence of electrical excitation
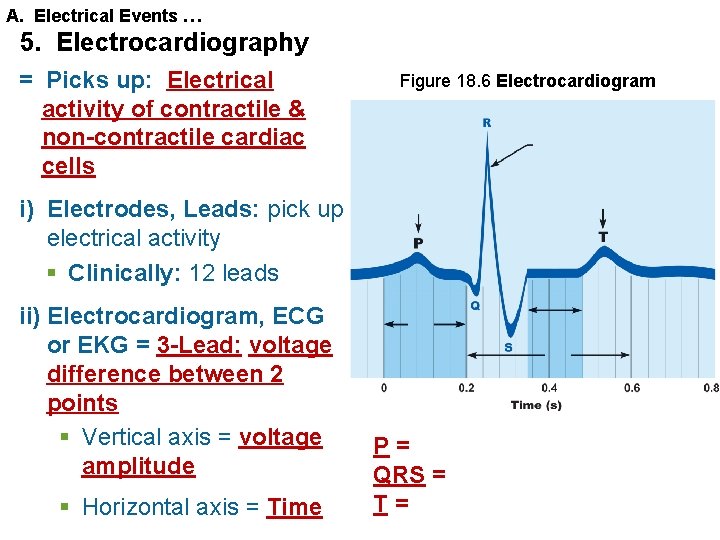
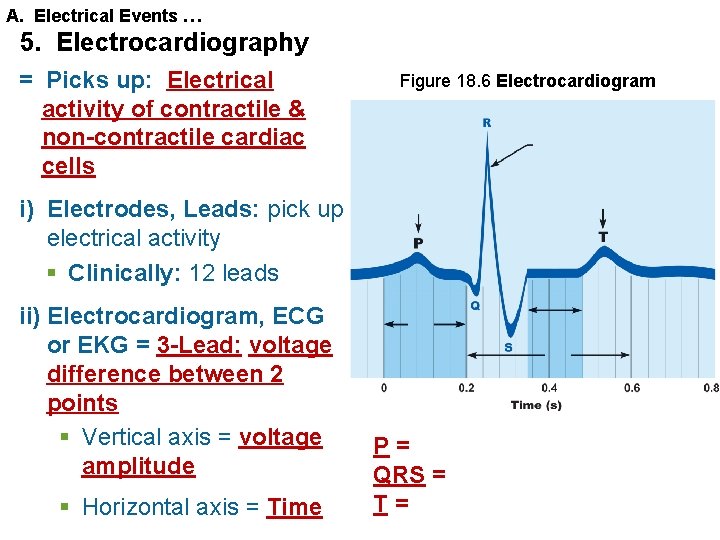
A. Electrical Events … 5. Electrocardiography = Picks up: Electrical activity of contractile & non-contractile cardiac cells Figure 18. 6 Electrocardiogram i) Electrodes, Leads: pick up electrical activity § Clinically: 12 leads ii) Electrocardiogram, ECG or EKG = 3 -Lead: voltage difference between 2 points § Vertical axis = voltage amplitude § Horizontal axis = Time P= QRS = T=
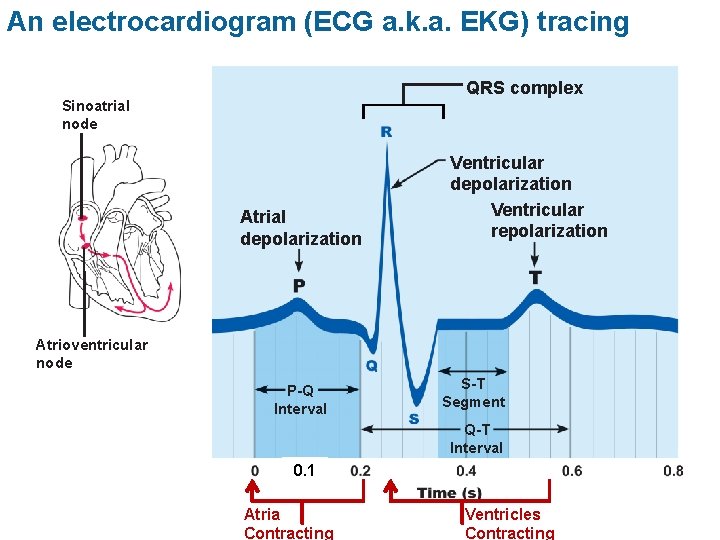
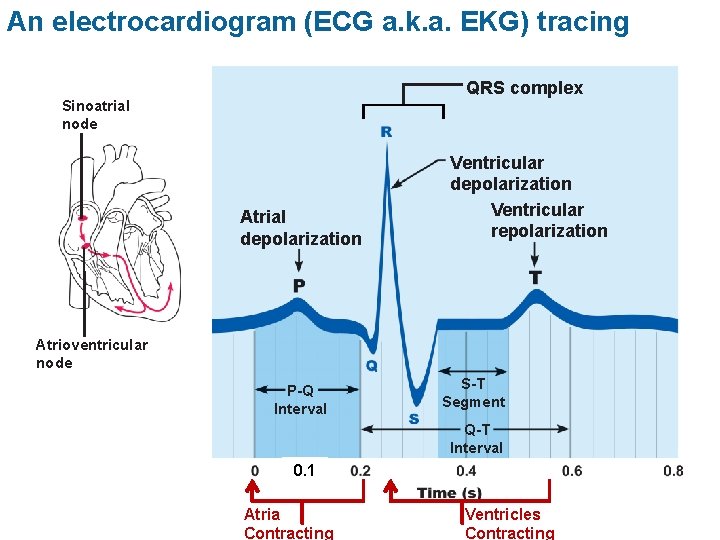
An electrocardiogram (ECG a. k. a. EKG) tracing QRS complex Sinoatrial node Atrial depolarization Ventricular repolarization Atrioventricular node P-Q Interval S-T Segment Q-T Interval 0. 1 Atria Contracting Ventricles Contracting
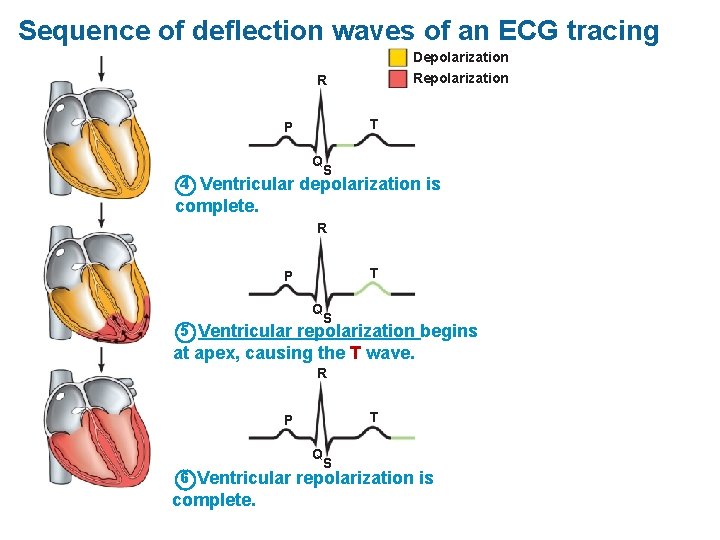
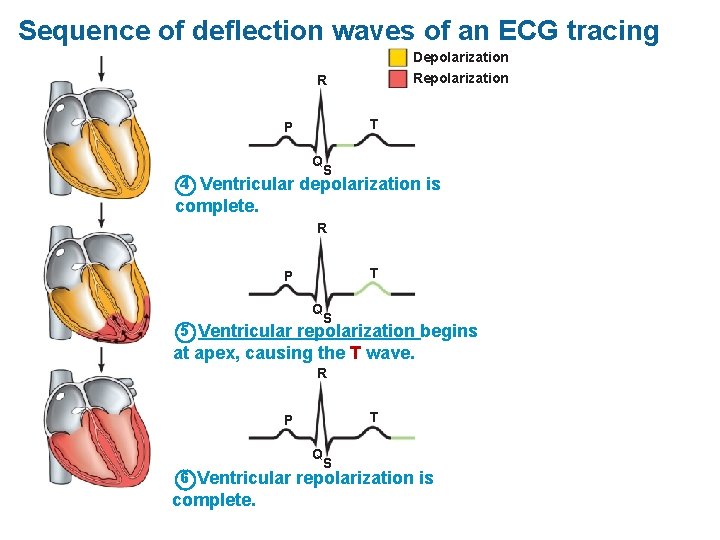
Sequence of deflection waves of an ECG tracing Depolarization R T P Q 4 S Ventricular depolarization is complete. R T P Q 5 S Ventricular repolarization begins at apex, causing the T wave. R T P Q 6 S Ventricular repolarization is complete.
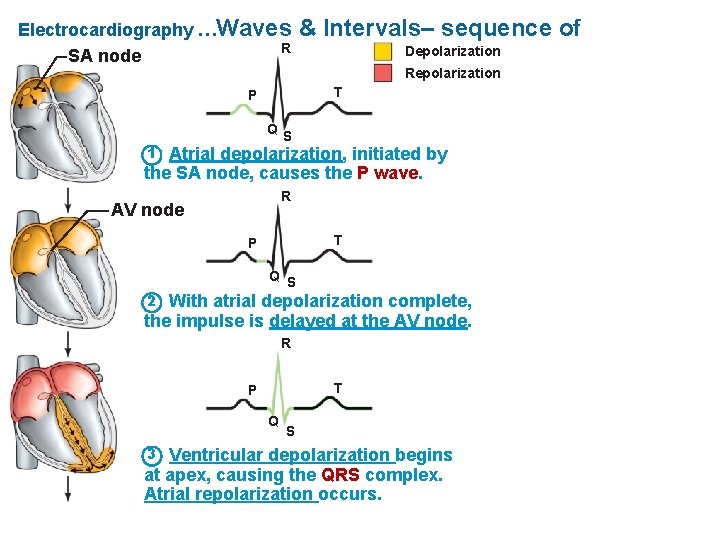
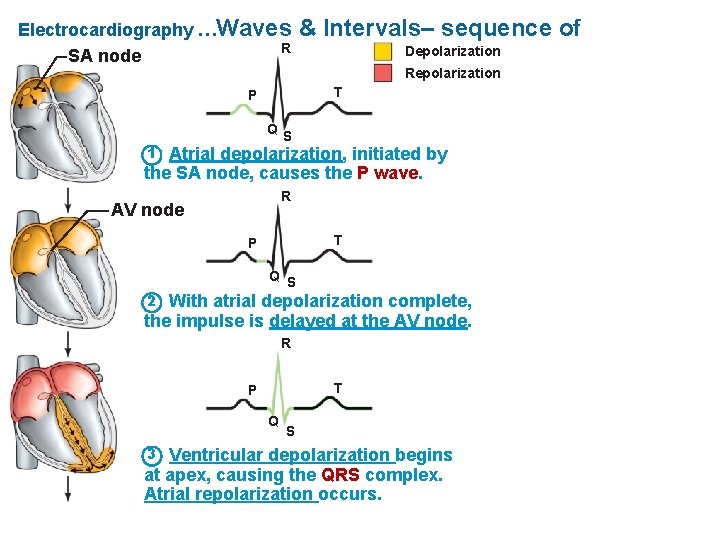
Electrocardiography …Waves R SA node & Intervals– sequence of Depolarization Repolarization T P QS 1 Atrial depolarization, initiated by the SA node, causes the P wave. R AV node T P Q S 2 With atrial depolarization complete, the impulse is delayed at the AV node. R T P Q 3 S Ventricular depolarization begins at apex, causing the QRS complex. Atrial repolarization occurs.
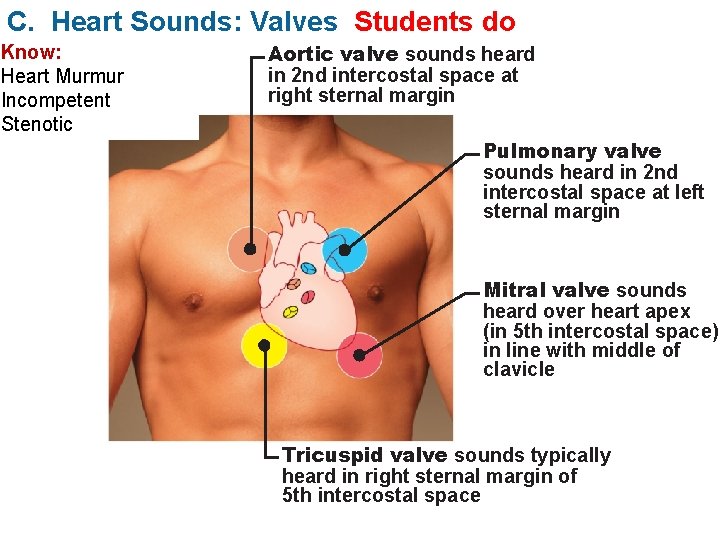
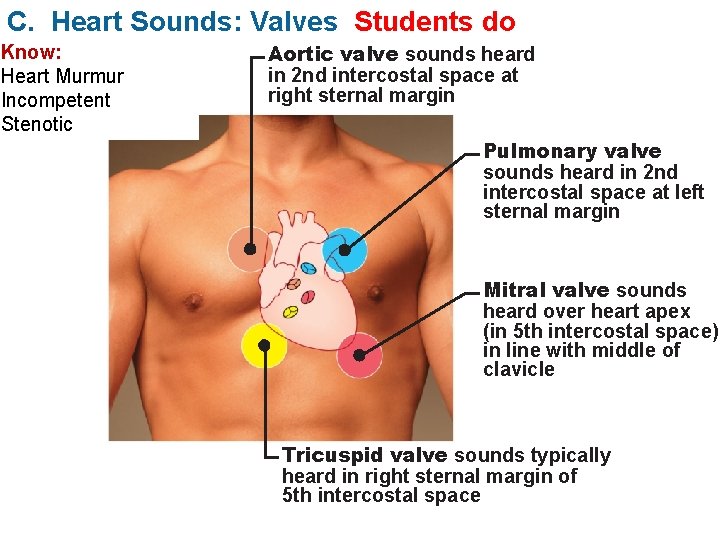
C. Heart Sounds: Valves Students do Know: Heart Murmur Incompetent Stenotic Aortic valve sounds heard in 2 nd intercostal space at right sternal margin Pulmonary valve sounds heard in 2 nd intercostal space at left sternal margin Mitral valve sounds heard over heart apex (in 5 th intercostal space) in line with middle of clavicle Tricuspid valve sounds typically heard in right sternal margin of 5 th intercostal space