The Chronic Disease Prevention model and its use
- Slides: 21
The Chronic Disease Prevention model and its use in the definition of public health policies Jeremy Lauer, Ph. D Health Systems Financing World Health Organization
Generalized Cost-effectiveness Analysis • Acknowledges global budget constraints • Allows the comparison of interventions within and outside the health sector • Identifies the mix of interventions that generates the largest health gain • Improves the transferability of results across similar settings
When is cost-effectiveness analysis useful? • Outside health sector: – When the finance minister says, "So what's your plan? " – To support strategies with operationalizable actions • Inside health sector: Inside health sector Outside health sector – To assist establishing priorities for action. – To set norms and standards – To plan for health system development
Background: WHO-CHOICE work on cancer • WHO-CHOICE has focused on cancers for which there are both treatment and preventive interventions. • In addition, interventions to prevent or reduce tobacco use, responsible for about one-quarter of the total cancer burden. • Other high-burden cancers such as stomach (about 11% of cancer burden) and liver (about 9% of cancer burden) lack efficacious treatments options at present. • breast, cervical and colorectal cancer.
WHO-CHOICE work on cancer • 10 -country study financed by the Komen Foundation to use cost-effectiveness analysis to support policy development in breast cancer control; participating are: – Mexico – Costa Rica – Colombia and – Brazil. • Our work on the CDP model was motivated by the desire to embed this analysis inside a broader NCD framework.
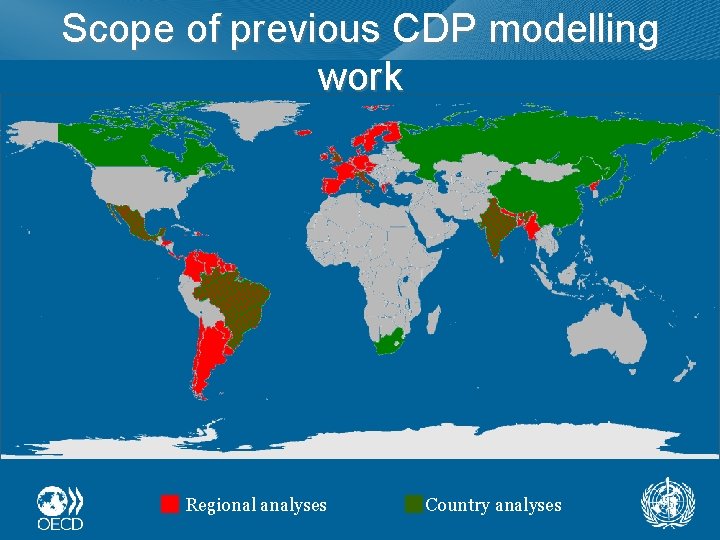
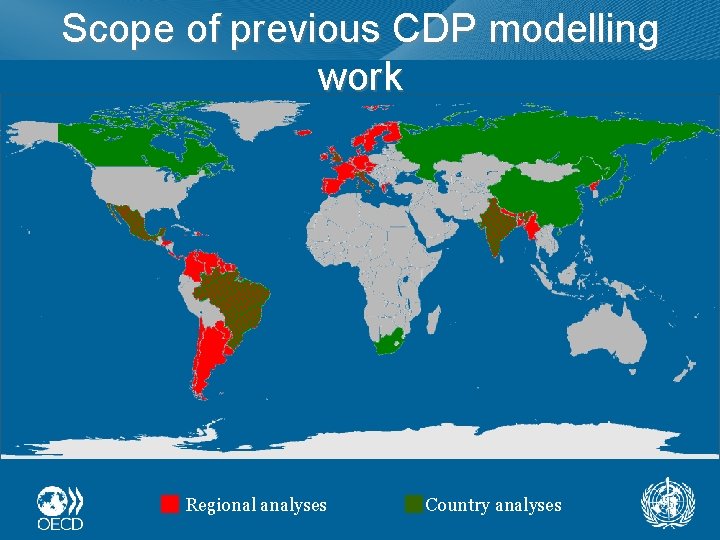
Scope of previous CDP modelling work Regional analyses Country analyses
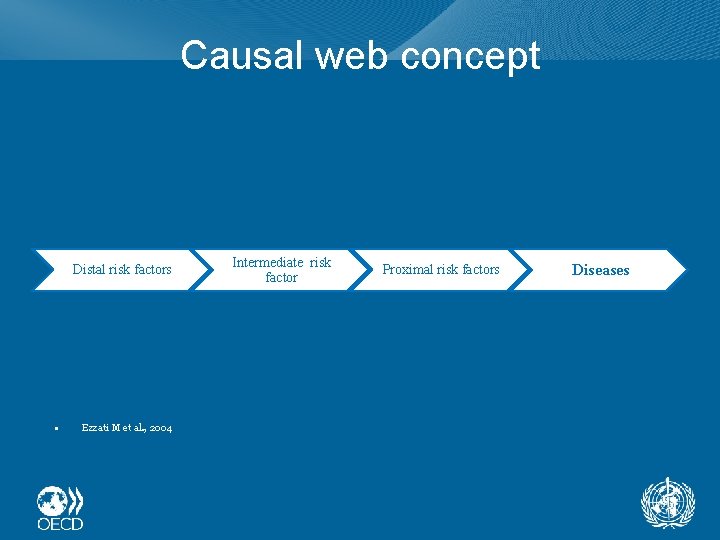
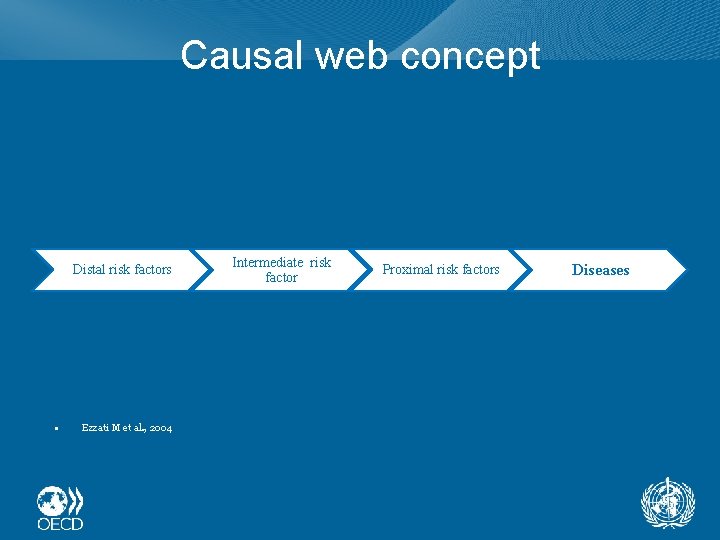
Causal web concept Distal risk factors • Ezzati M et al. , 2004 Intermediate risk factor Proximal risk factors Diseases
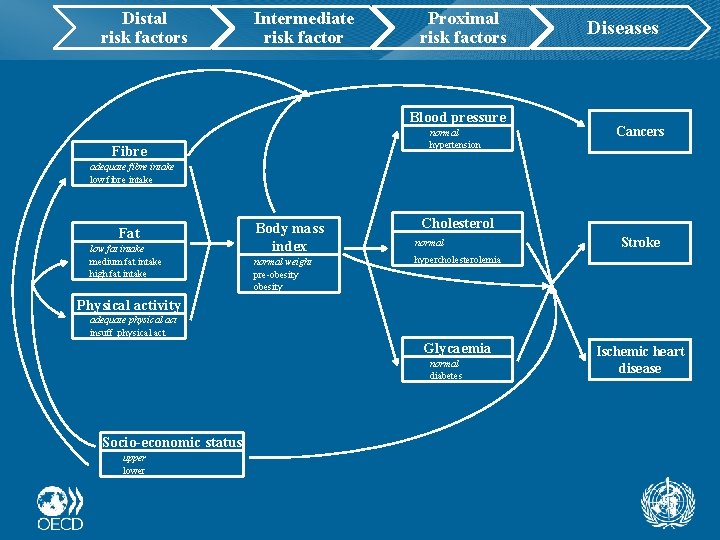
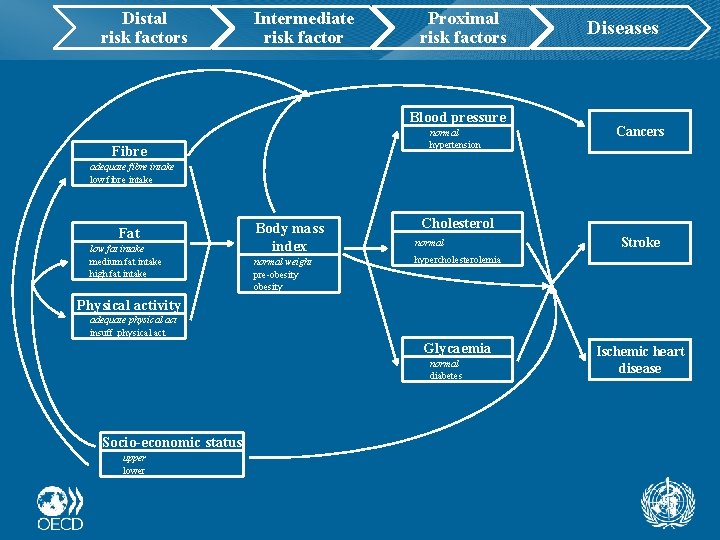
Distal risk factors Intermediate risk factor Proximal risk factors Blood pressure normal hypertension Fibre Diseases Cancers adequate fibre intake low fibre intake Fat low fat intake medium fat intake high fat intake Body mass index normal weight pre-obesity Cholesterol normal Stroke hypercholesterolemia Physical activity adequate physical act insuff. physical act Glycaemia normal diabetes Socio-economic status upper lower Ischemic heart disease
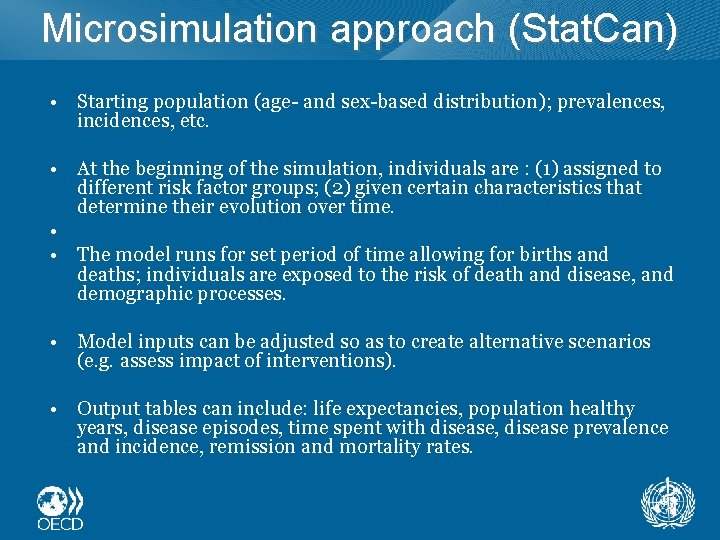
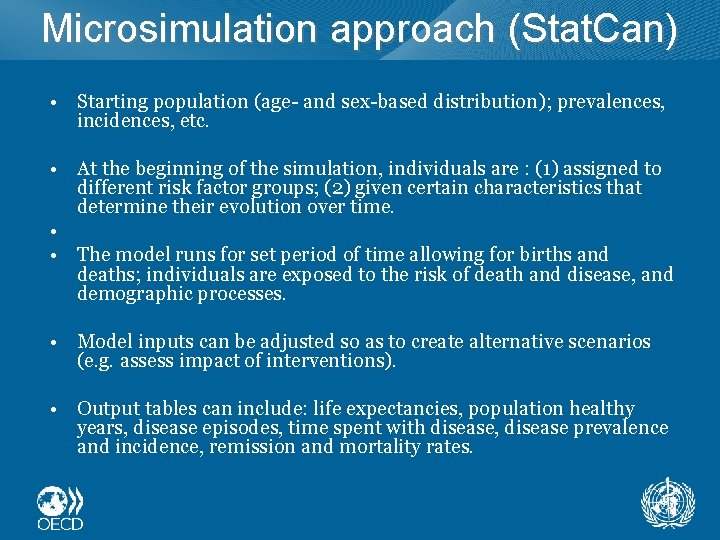
Microsimulation approach (Stat. Can) • Starting population (age- and sex-based distribution); prevalences, incidences, etc. • At the beginning of the simulation, individuals are : (1) assigned to different risk factor groups; (2) given certain characteristics that determine their evolution over time. • • The model runs for set period of time allowing for births and deaths; individuals are exposed to the risk of death and disease, and demographic processes. • Model inputs can be adjusted so as to create alternative scenarios (e. g. assess impact of interventions). • Output tables can include: life expectancies, population healthy years, disease episodes, time spent with disease, disease prevalence and incidence, remission and mortality rates.
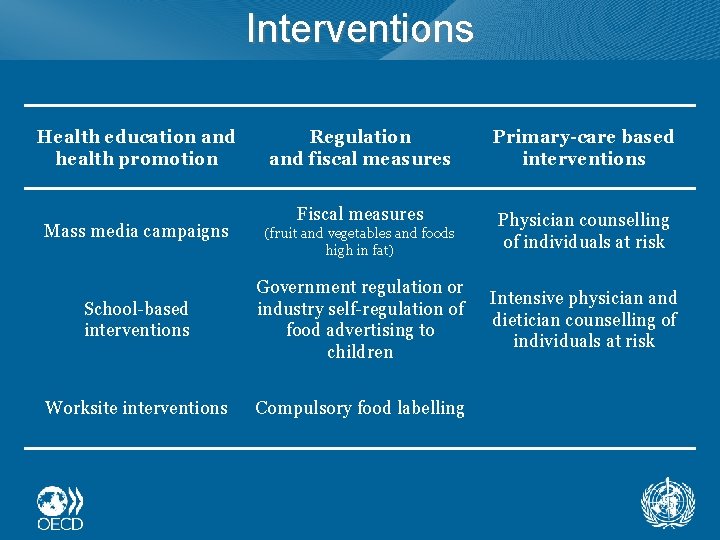
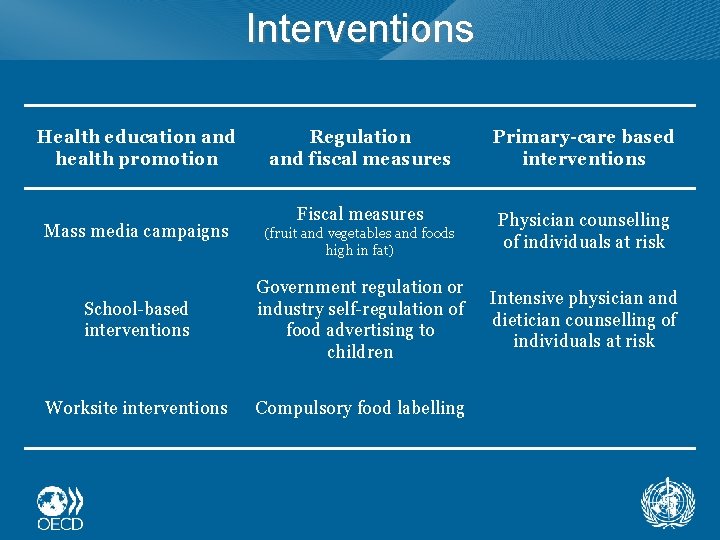
Interventions Health education and health promotion Mass media campaigns Regulation and fiscal measures Primary-care based interventions Fiscal measures Physician counselling of individuals at risk (fruit and vegetables and foods high in fat) School-based interventions Government regulation or industry self-regulation of food advertising to children Worksite interventions Compulsory food labelling Intensive physician and dietician counselling of individuals at risk
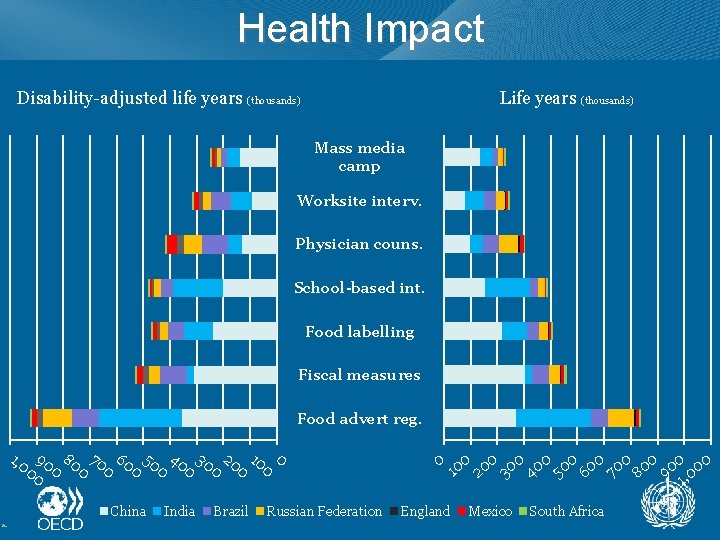
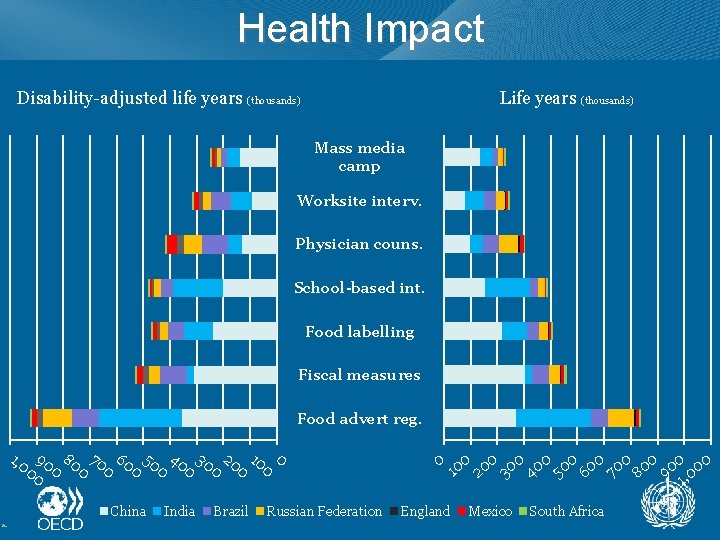
Health Impact Disability-adjusted life years (thousands) Life years (thousands) Mass media camp Worksite interv. Physician couns. School-based int. Food labelling Fiscal measures Food advert reg. 1, 0 90 80 70 60 50 40 30 20 10 0 0 0 China India Brazil Russian Federation 0 00 00 00 1 2 3 4 5 6 7 8 9 , 0 1 England Mexico South Africa
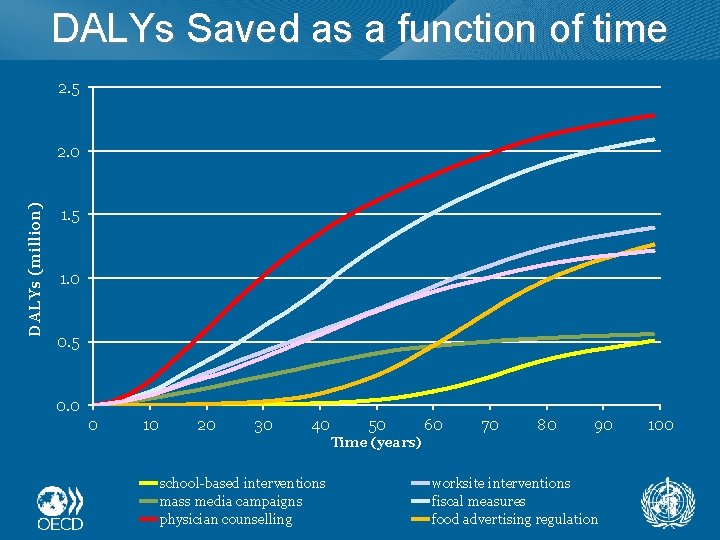
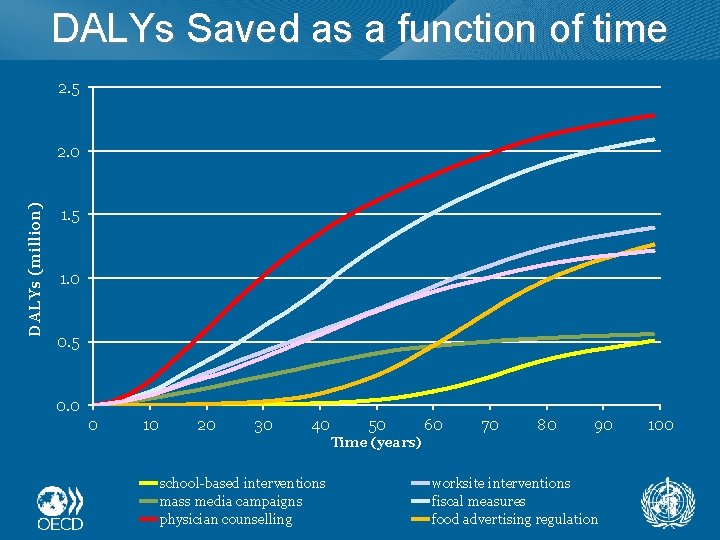
DALYs Saved as a function of time 2. 5 DALYs (million) 2. 0 1. 5 1. 0 0. 5 0. 0 0 10 20 30 40 50 60 70 80 90 Time (years) school-based interventions mass media campaigns physician counselling worksite interventions fiscal measures food advertising regulation 100
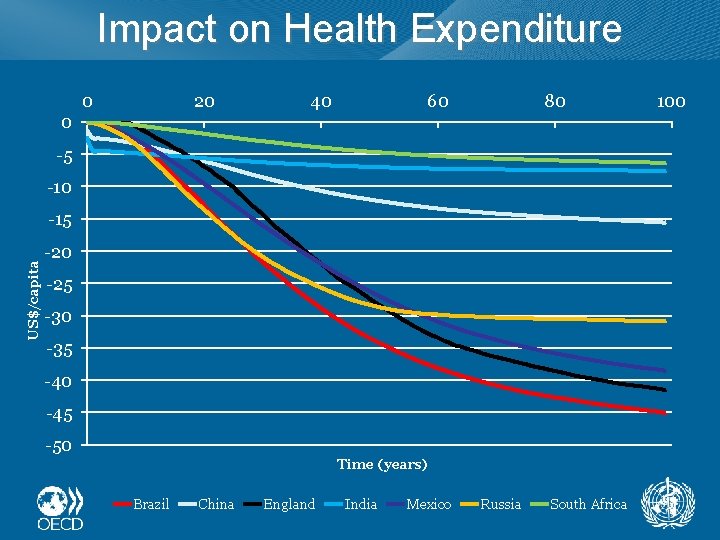
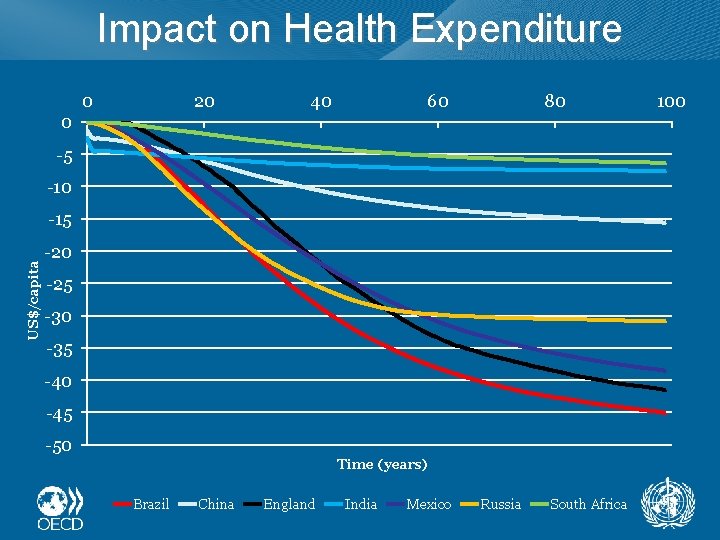
Impact on Health Expenditure 0 20 40 60 80 0 -5 -10 US$/capita -15 -20 -25 -30 -35 -40 -45 -50 Time (years) Brazil China England India Mexico Russia South Africa 100
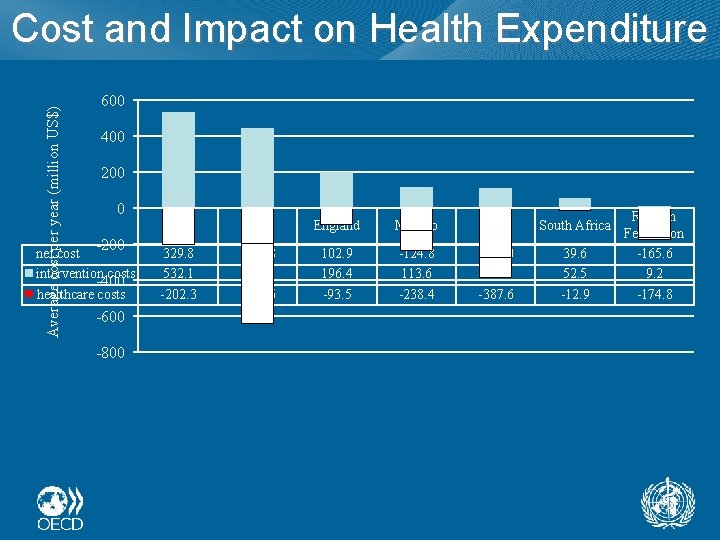
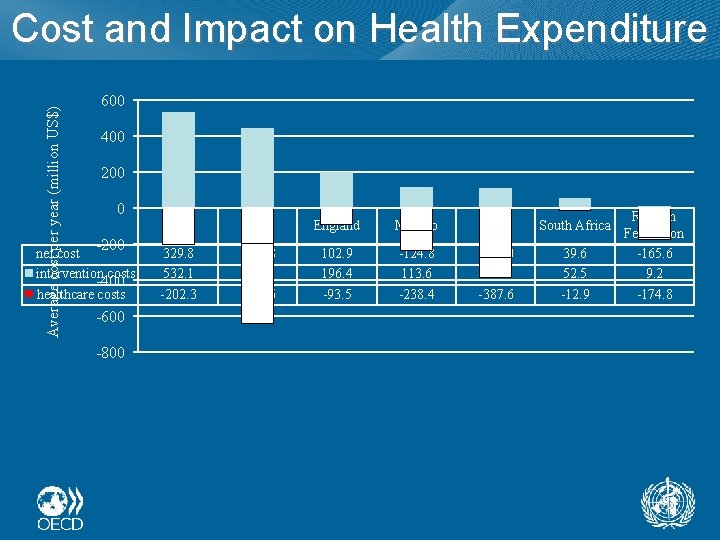
Average cost per year (million US$) Cost and Impact on Health Expenditure 600 400 200 0 -200 net cost intervention costs -400 healthcare costs -600 -800 India China England Mexico Brazil South Africa 329. 8 532. 1 -202. 3 -195. 8 444. 8 -640. 6 102. 9 196. 4 -93. 5 -124. 8 113. 6 -238. 4 -278. 0 109. 6 -387. 6 39. 6 52. 5 -12. 9 Russian Federation -165. 6 9. 2 -174. 8
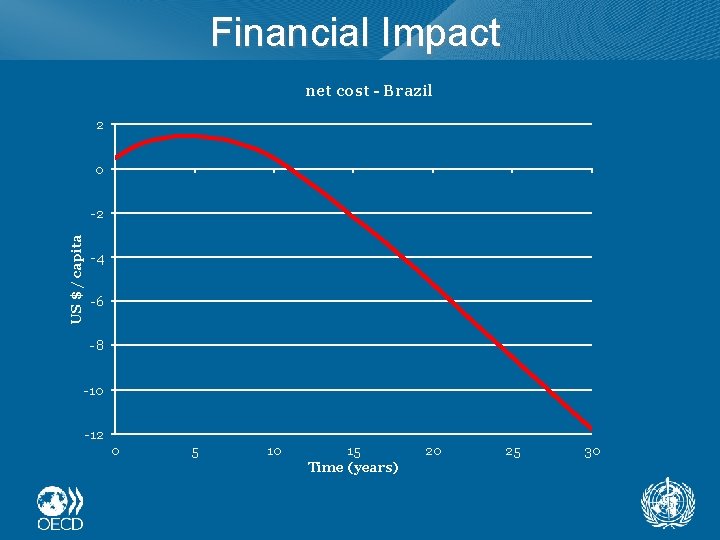
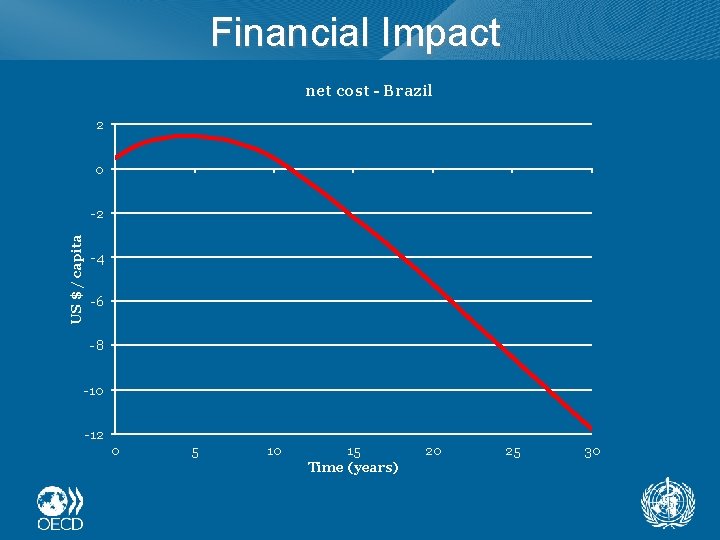
Financial Impact net cost - Brazil 2 0 US $ / capita -2 -4 -6 -8 -10 -12 0 5 10 15 Time (years) 20 25 30
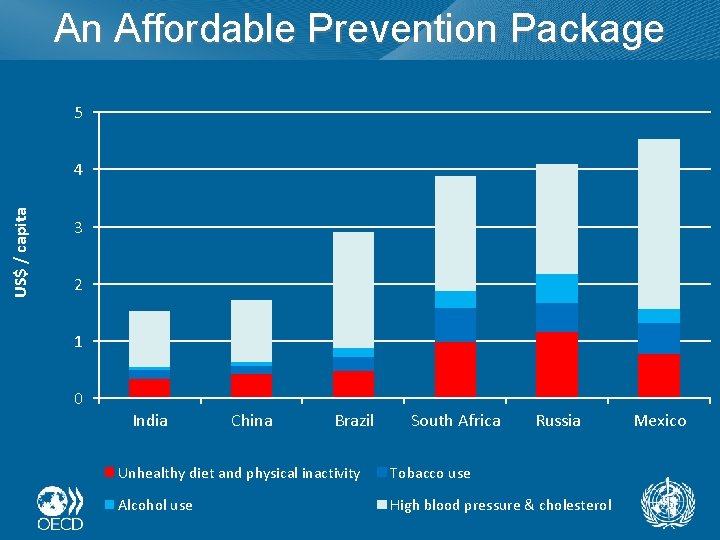
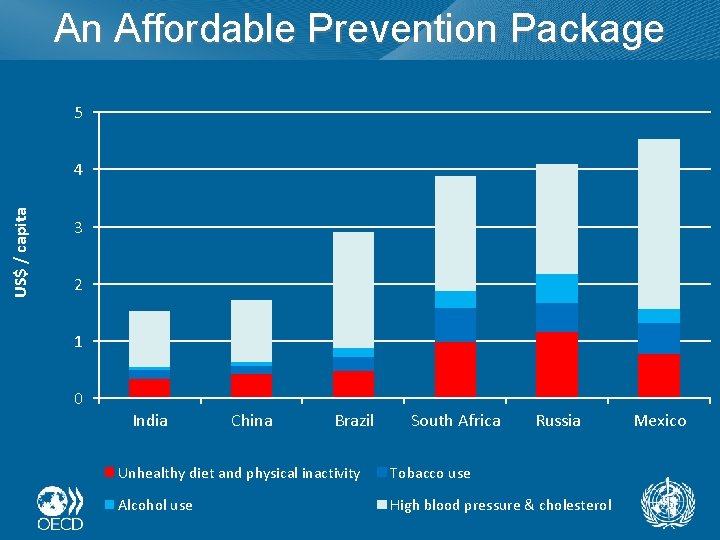
An Affordable Prevention Package 5 US$ / capita 4 3 2 1 0 India China Brazil South Africa Russia Unhealthy diet and physical inactivity Tobacco use Alcohol use High blood pressure & cholesterol Mexico
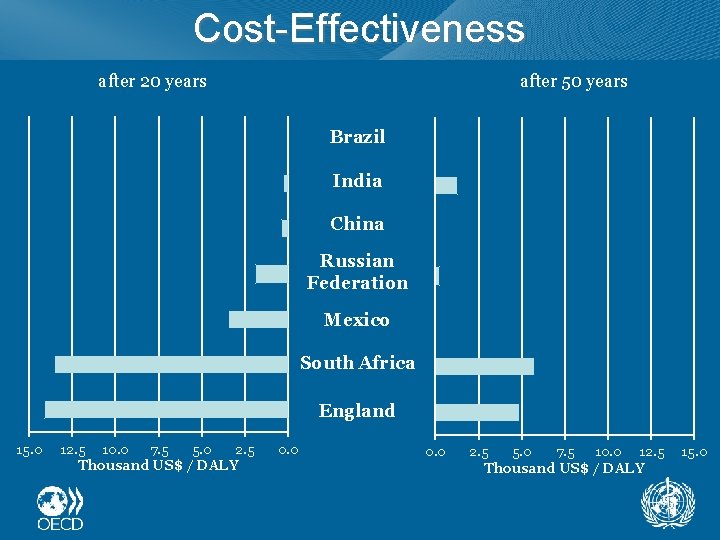
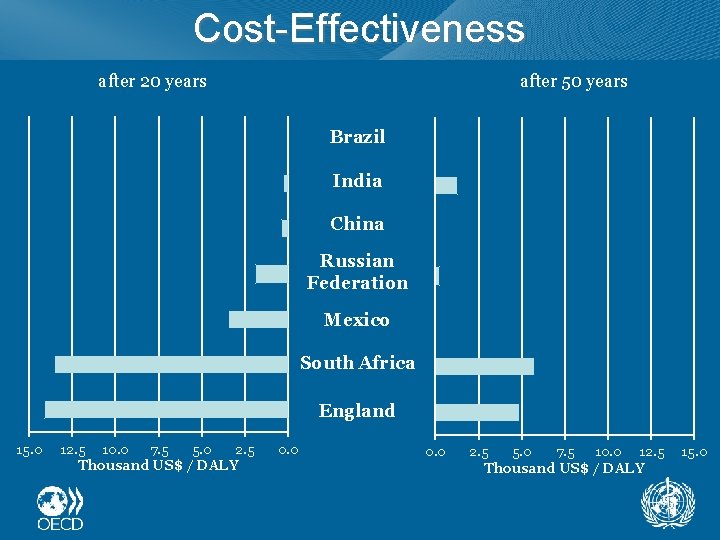
Cost-Effectiveness after 50 years after 20 years Brazil India China Russian Federation Mexico South Africa England 15. 0 12. 5 10. 0 7. 5 5. 0 2. 5 Thousand US$ / DALY 0. 0 2. 5 5. 0 7. 5 10. 0 12. 5 Thousand US$ / DALY 15. 0
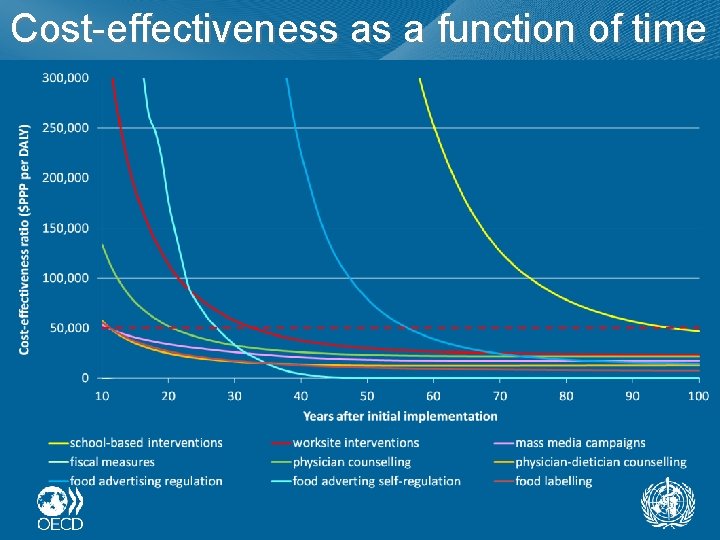
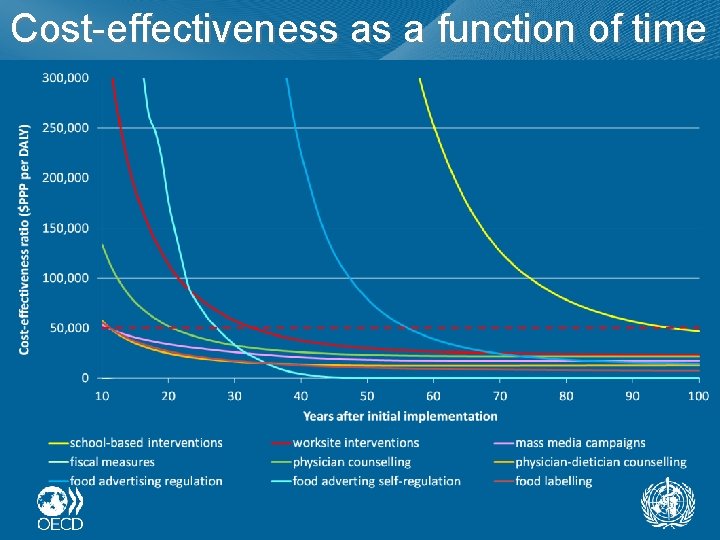
Cost-effectiveness as a function of time
Impact on Inequalities Worksite interventions Fiscal measures
What matters most for health policy? • Does prevention improve health? • Does it reduce health expenditure? • Does it improve health inequalities? • Is it cost-effective?
References Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V, Chisholm D. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and costeffectiveness Lancet. 2010 Nov 20; 376(9754): 1775 -84