The Changing Patterns of Aortic Stenosis Increased Frequency

- Slides: 60
The Changing Patterns of Aortic Stenosis: Increased Frequency in an Aging Population and the Impact on Treatment Options Martin B. Leon, MD Columbia University Medical Center Cardiovascular Research Foundation New York City CRT 2010 Washington, DC; February 21, 2010
Presenter Disclosure Information for CRT 2010; February 21, 2010 Martin B. Leon, M. D. NON-PAID Consultant: Edwards Lifesciences, Medtronic
Aortic Stenosis: Diagnostic Patterns Severe AS without AVR Severe AS without Symptoms Low Flow/Low Gradient AS AS + CAD
Aortic Stenosis: Diagnostic Patterns Severe AS without AVR Severe AS without Symptoms Low Flow/Low Gradient AS AS + CAD
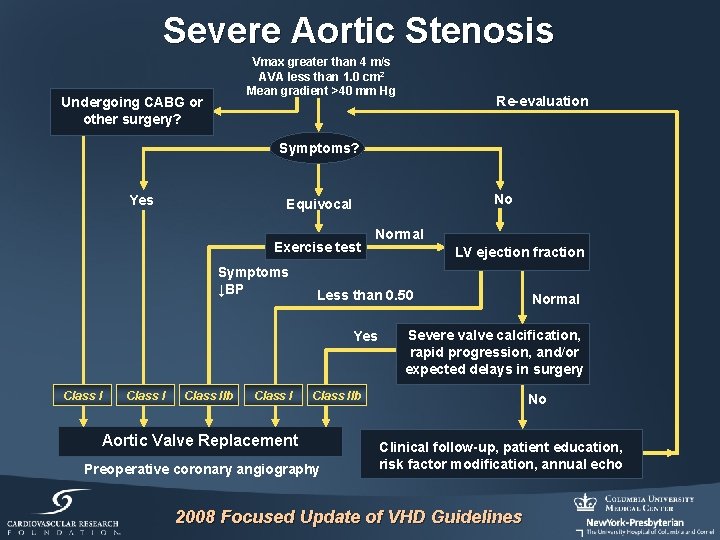
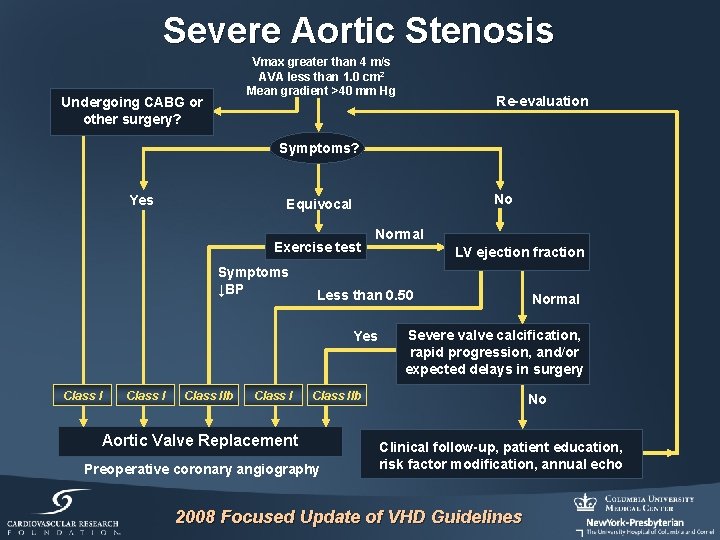
Severe Aortic Stenosis Vmax greater than 4 m/s AVA less than 1. 0 cm 2 Mean gradient >40 mm Hg Undergoing CABG or other surgery? Re-evaluation Symptoms? Yes No Equivocal Exercise test Symptoms ↓BP Normal Less than 0. 50 Yes Class IIb Class I LV ejection fraction Severe valve calcification, rapid progression, and/or expected delays in surgery Class IIb Aortic Valve Replacement Preoperative coronary angiography Normal No Clinical follow-up, patient education, risk factor modification, annual echo 2008 Focused Update of VHD Guidelines
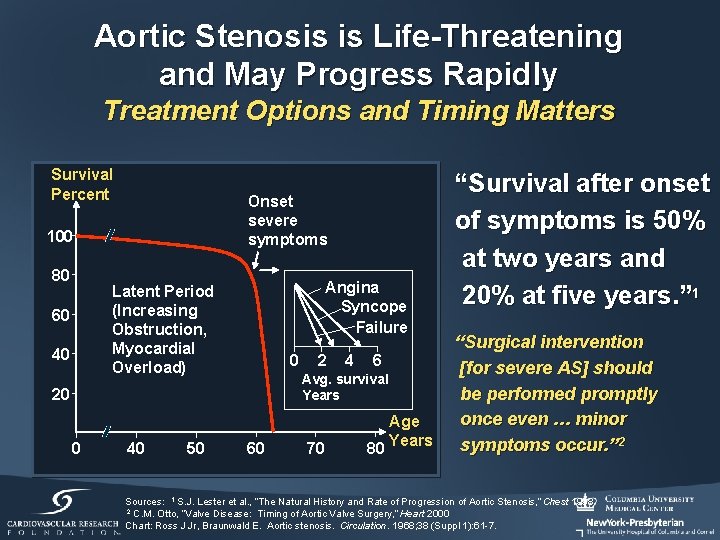
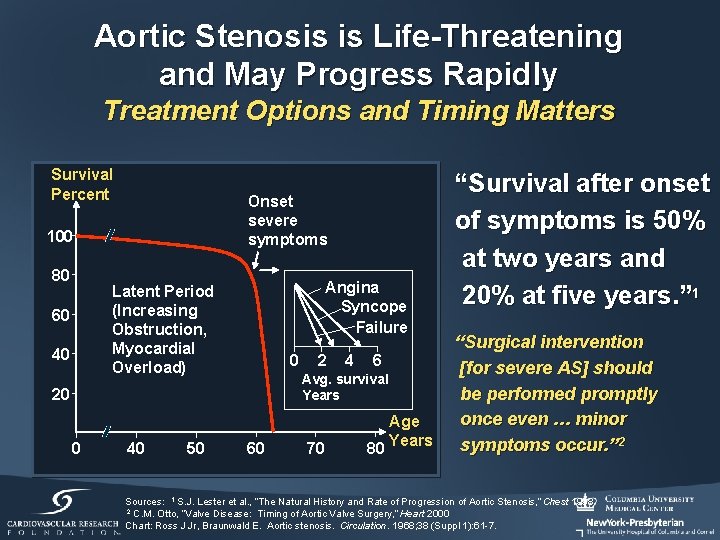
Aortic Stenosis is Life-Threatening and May Progress Rapidly Treatment Options and Timing Matters Survival Percent Onset severe symptoms 100 80 Angina Syncope Failure Latent Period (Increasing Obstruction, Myocardial Overload) 60 40 50 4 6 Avg. survival Years 20 0 2 60 70 Age 80 Years “Survival after onset of symptoms is 50% at two years and 20% at five years. ” 1 “Surgical intervention [for severe AS] should be performed promptly once even … minor symptoms occur. ” 2 Sources: 1 S. J. Lester et al. , “The Natural History and Rate of Progression of Aortic Stenosis, ” Chest 1998 2 C. M. Otto, “Valve Disease: Timing of Aortic Valve Surgery, ” Heart 2000 Chart: Ross J Jr, Braunwald E. Aortic stenosis. Circulation. 1968; 38 (Suppl 1): 61 -7.
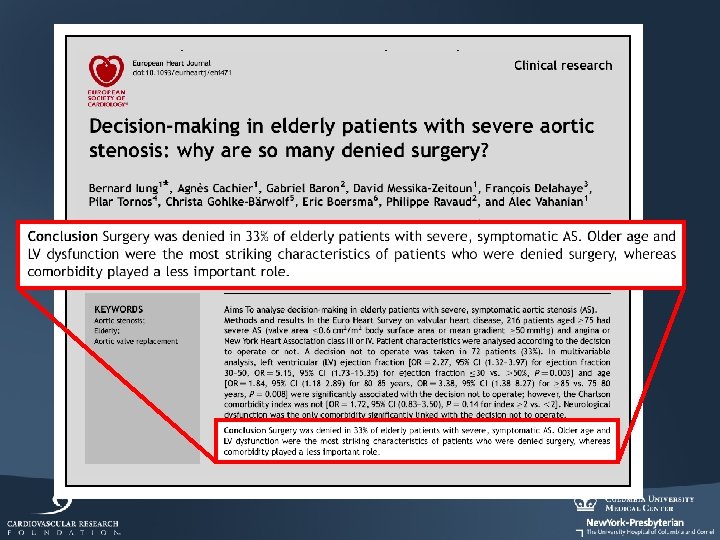
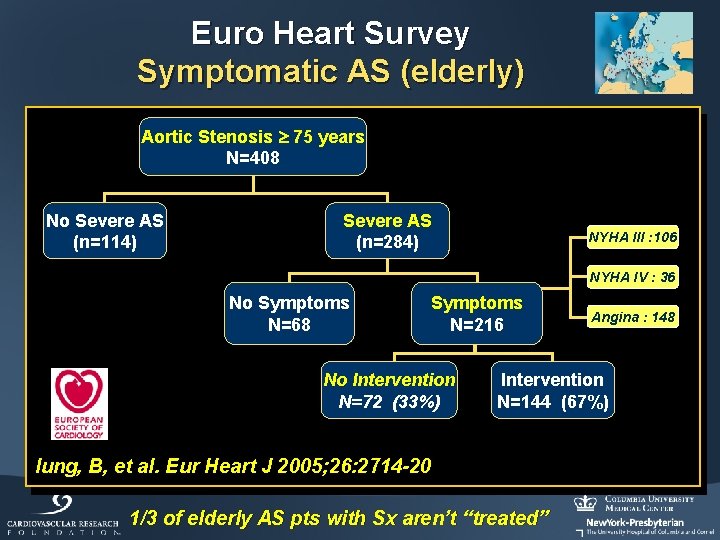
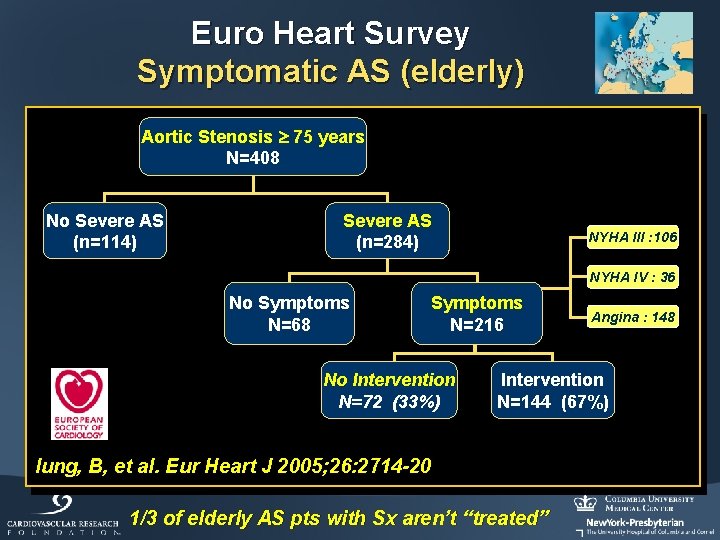
Euro Heart Survey Symptomatic AS (elderly) Aortic Stenosis 75 years N=408 No Severe AS (n=114) Severe AS (n=284) NYHA III : 106 NYHA IV : 36 No Symptoms N=68 Symptoms N=216 No Intervention N=72 (33%) Angina : 148 Intervention N=144 (67%) Iung, B, et al. Eur Heart J 2005; 26: 2714 -20 1/3 of elderly AS pts with Sx aren’t “treated”
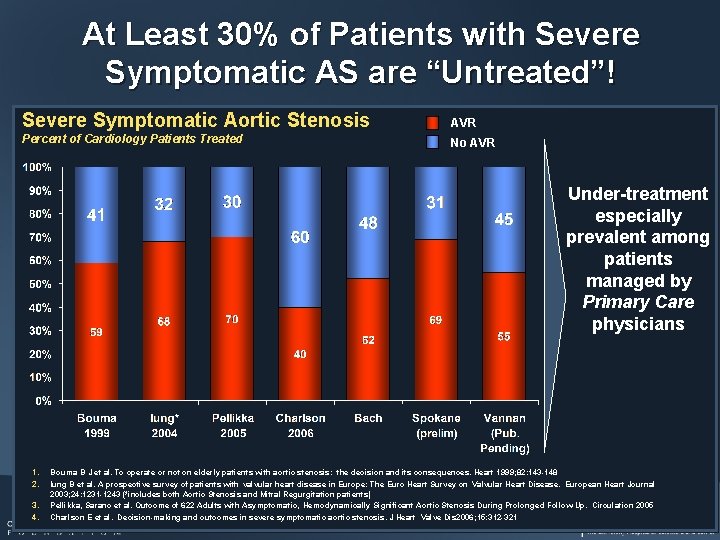
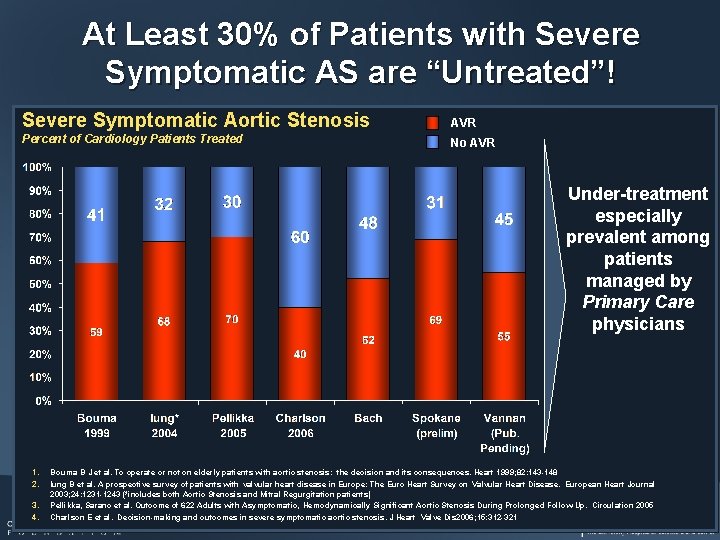
At Least 30% of Patients with Severe Symptomatic AS are “Untreated”! Severe Symptomatic Aortic Stenosis AVR Percent of Cardiology Patients Treated No AVR Under-treatment especially prevalent among patients managed by Primary Care physicians 1. 2. 3. 4. Bouma B J et al. To operate or not on elderly patients with aortic stenosis: the decision and its consequences. Heart 1999; 82: 143 -148 Iung B et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. European Heart Journal 2003; 24: 1231 -1243 (*includes both Aortic Stenosis and Mitral Regurgitation patients) Pellikka, Sarano et al. Outcome of 622 Adults with Asymptomatic, Hemodynamically Significant Aortic Stenosis During Prolonged Follow-Up. Circulation 2005 Charlson E et al. Decision-making and outcomes in severe symptomatic aortic stenosis. J Heart Valve Dis 2006; 15: 312 -321
Severe AS without AVR Bach DS, et al. Circ Cardiovasc Qual Outcomes. 2009; 2: 533 -539
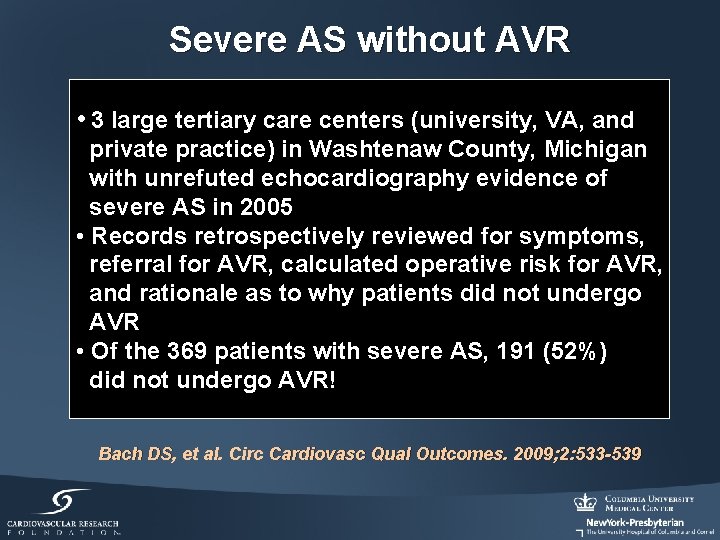
Severe AS without AVR • 3 large tertiary care centers (university, VA, and private practice) in Washtenaw County, Michigan with unrefuted echocardiography evidence of severe AS in 2005 • Records retrospectively reviewed for symptoms, referral for AVR, calculated operative risk for AVR, and rationale as to why patients did not undergo AVR • Of the 369 patients with severe AS, 191 (52%) did not undergo AVR! Bach DS, et al. Circ Cardiovasc Qual Outcomes. 2009; 2: 533 -539
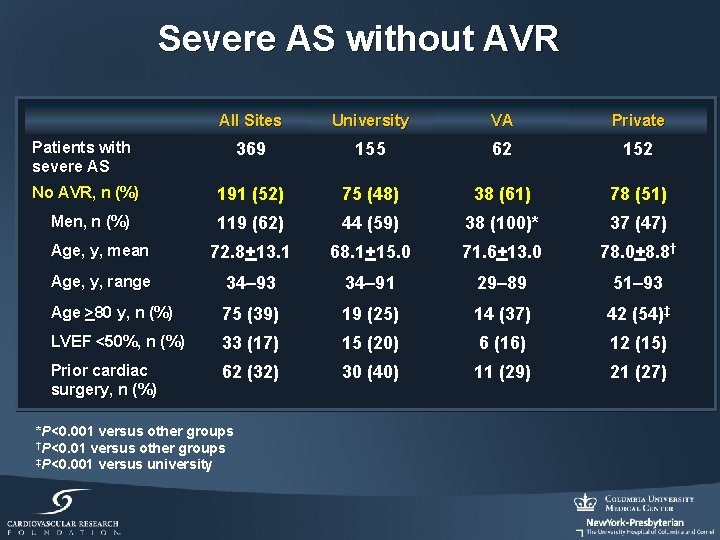
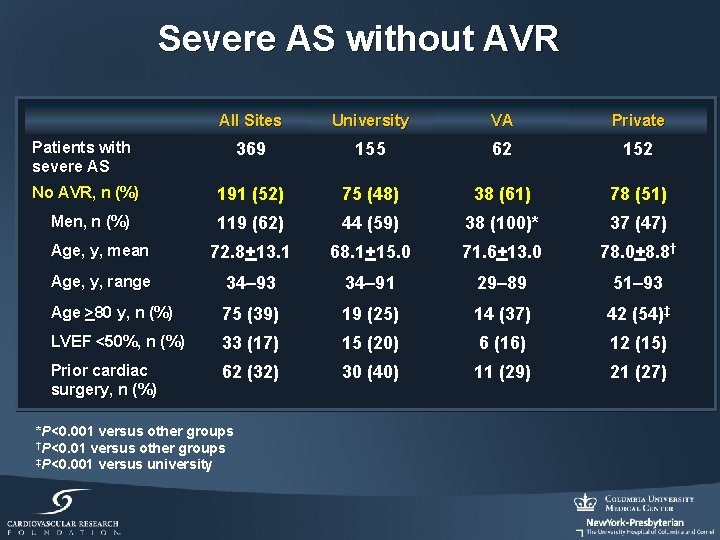
Severe AS without AVR All Sites University VA Private Patients with severe AS 369 155 62 152 No AVR, n (%) 191 (52) 75 (48) 38 (61) 78 (51) Men, n (%) 119 (62) 44 (59) 38 (100)* 37 (47) Age, y, mean 72. 8+13. 1 68. 1+15. 0 71. 6+13. 0 78. 0+8. 8† Age, y, range 34– 93 34– 91 29– 89 51– 93 Age >80 y, n (%) 75 (39) 19 (25) 14 (37) 42 (54)‡ LVEF <50%, n (%) 33 (17) 15 (20) 6 (16) 12 (15) Prior cardiac surgery, n (%) 62 (32) 30 (40) 11 (29) 21 (27) *P<0. 001 versus other groups †P<0. 01 versus other groups ‡P<0. 001 versus university
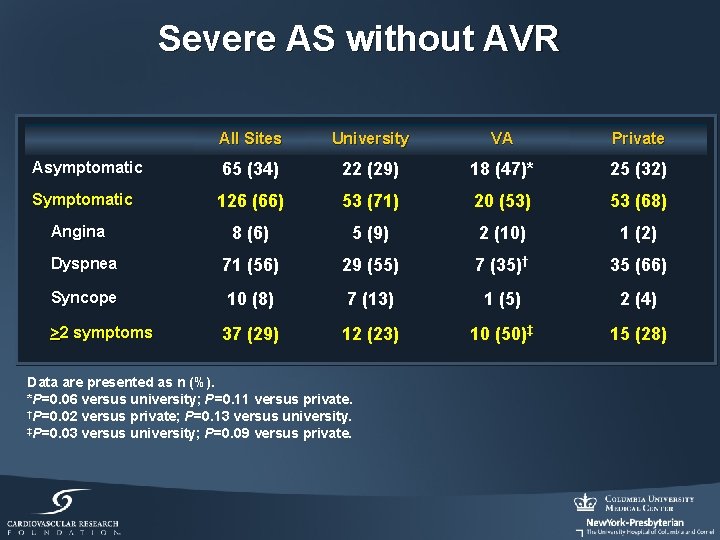
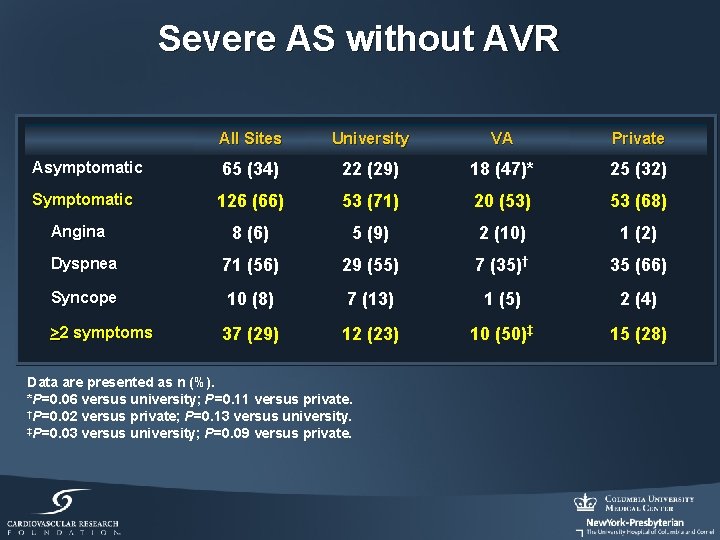
Severe AS without AVR All Sites University VA Private Asymptomatic 65 (34) 22 (29) 18 (47)* 25 (32) Symptomatic 126 (66) 53 (71) 20 (53) 53 (68) 8 (6) 5 (9) 2 (10) 1 (2) Dyspnea 71 (56) 29 (55) 7 (35)† 35 (66) Syncope 10 (8) 7 (13) 1 (5) 2 (4) 37 (29) 12 (23) 10 (50)‡ 15 (28) Angina >2 symptoms Data are presented as n (%). *P=0. 06 versus university; P=0. 11 versus private. †P=0. 02 versus private; P=0. 13 versus university. ‡P=0. 03 versus university; P=0. 09 versus private.
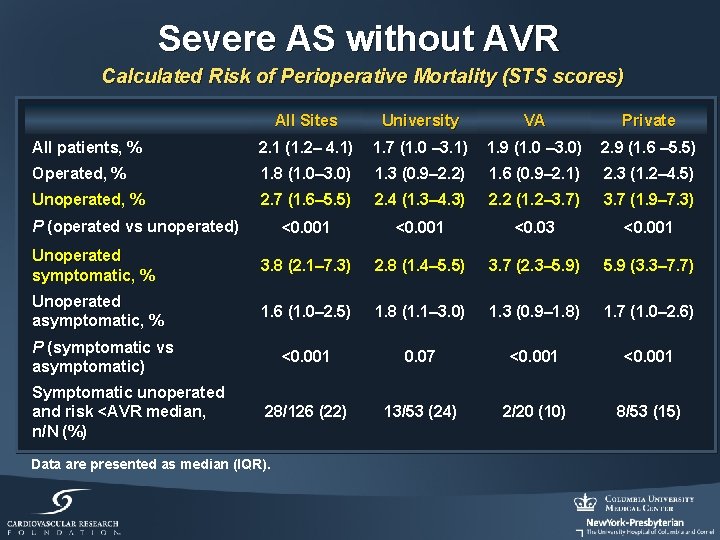
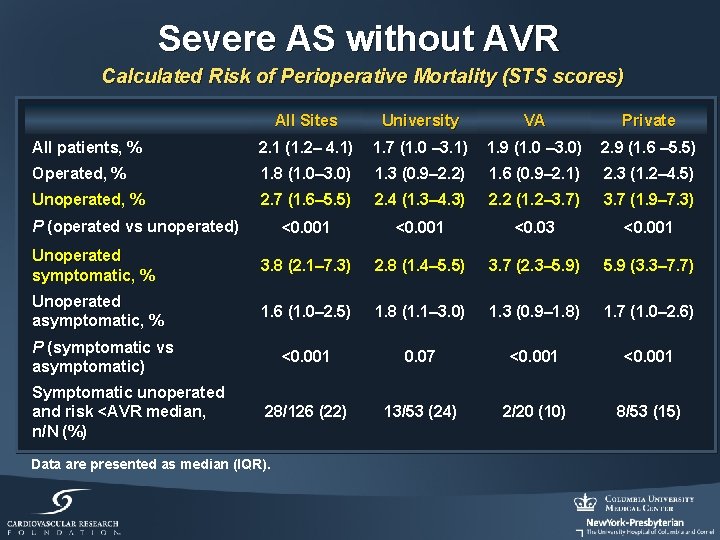
Severe AS without AVR Calculated Risk of Perioperative Mortality (STS scores) All Sites University VA Private All patients, % 2. 1 (1. 2– 4. 1) 1. 7 (1. 0 – 3. 1) 1. 9 (1. 0 – 3. 0) 2. 9 (1. 6 – 5. 5) Operated, % 1. 8 (1. 0– 3. 0) 1. 3 (0. 9– 2. 2) 1. 6 (0. 9– 2. 1) 2. 3 (1. 2– 4. 5) Unoperated, % 2. 7 (1. 6– 5. 5) 2. 4 (1. 3– 4. 3) 2. 2 (1. 2– 3. 7) 3. 7 (1. 9– 7. 3) <0. 001 <0. 03 <0. 001 Unoperated symptomatic, % 3. 8 (2. 1– 7. 3) 2. 8 (1. 4– 5. 5) 3. 7 (2. 3– 5. 9) 5. 9 (3. 3– 7. 7) Unoperated asymptomatic, % 1. 6 (1. 0– 2. 5) 1. 8 (1. 1– 3. 0) 1. 3 (0. 9– 1. 8) 1. 7 (1. 0– 2. 6) <0. 001 0. 07 <0. 001 28/126 (22) 13/53 (24) 2/20 (10) 8/53 (15) P (operated vs unoperated) P (symptomatic vs asymptomatic) Symptomatic unoperated and risk <AVR median, n/N (%) Data are presented as median (IQR).
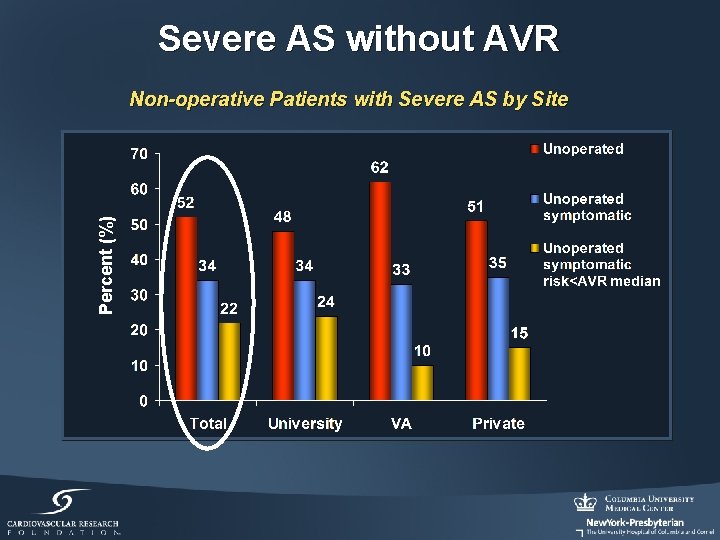
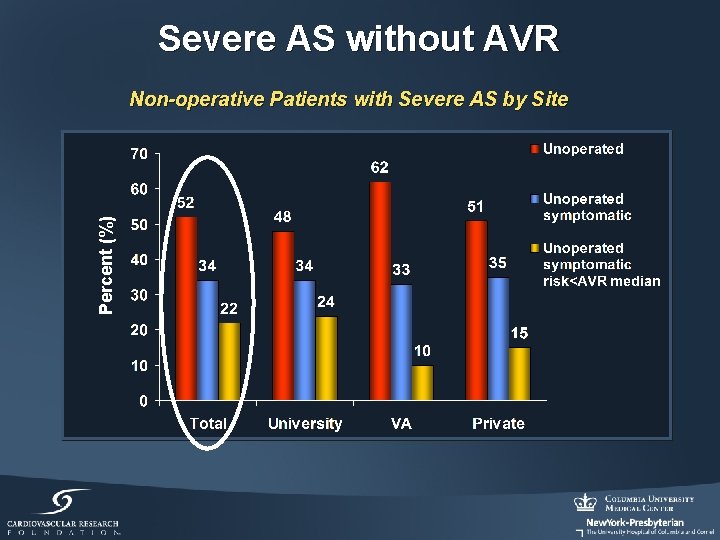
Severe AS without AVR Percent (%) Non-operative Patients with Severe AS by Site
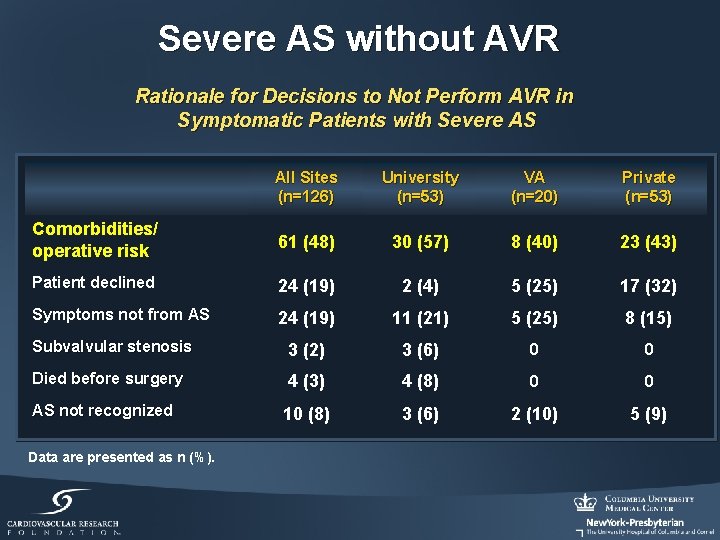
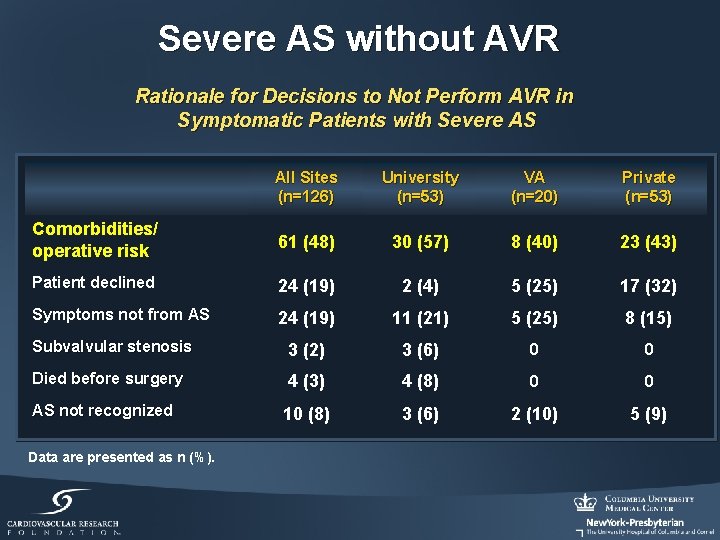
Severe AS without AVR Rationale for Decisions to Not Perform AVR in Symptomatic Patients with Severe AS All Sites (n=126) University (n=53) VA (n=20) Private (n=53) Comorbidities/ operative risk 61 (48) 30 (57) 8 (40) 23 (43) Patient declined 24 (19) 2 (4) 5 (25) 17 (32) Symptoms not from AS 24 (19) 11 (21) 5 (25) 8 (15) Subvalvular stenosis 3 (2) 3 (6) 0 0 Died before surgery 4 (3) 4 (8) 0 0 10 (8) 3 (6) 2 (10) 5 (9) AS not recognized Data are presented as n (%).
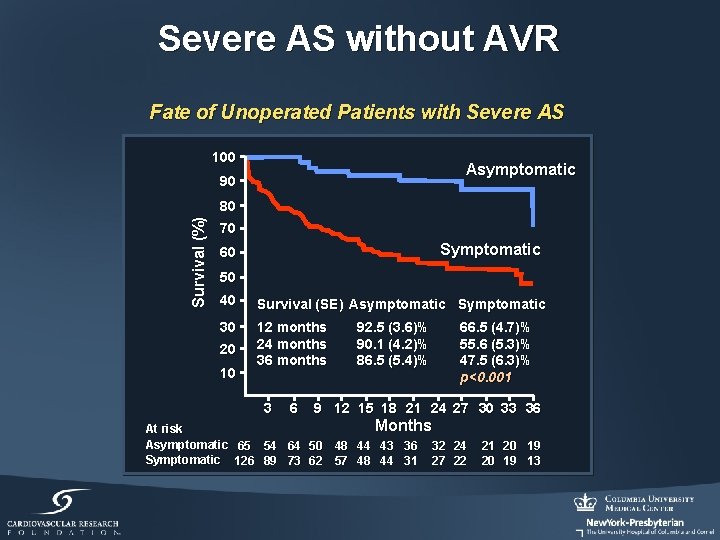
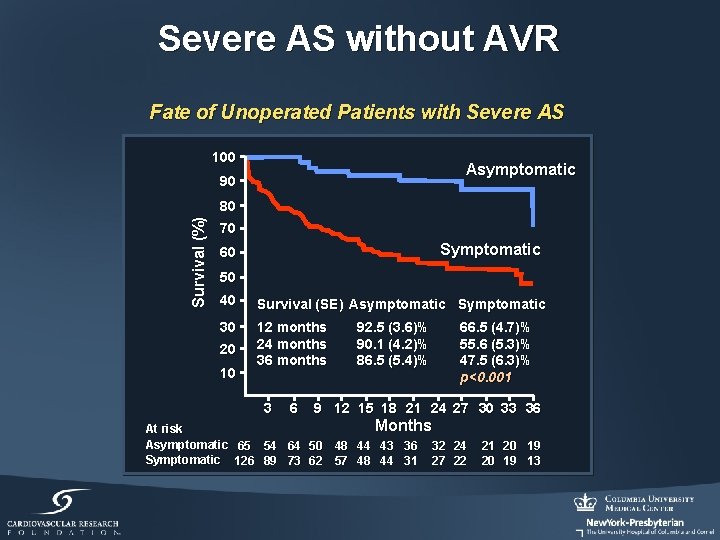
Severe AS without AVR Fate of Unoperated Patients with Severe AS 100 Asymptomatic 90 Survival (%) 80 70 Symptomatic 60 50 40 Survival (SE) Asymptomatic Symptomatic 30 12 months 24 months 36 months 20 10 3 6 92. 5 (3. 6)% 90. 1 (4. 2)% 86. 5 (5. 4)% 66. 5 (4. 7)% 55. 6 (5. 3)% 47. 5 (6. 3)% p<0. 001 9 12 15 18 21 24 27 30 33 36 Months At risk Asymptomatic 65 54 64 50 48 44 43 36 32 24 Symptomatic 126 89 73 62 57 48 44 31 27 22 21 20 19 13
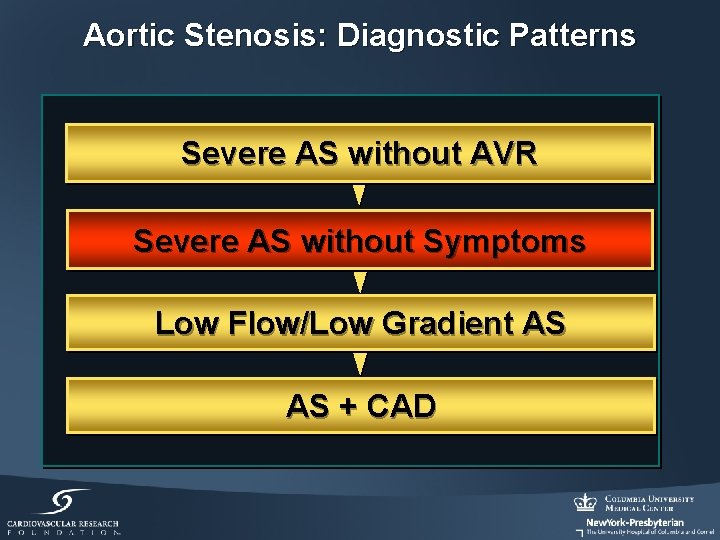
Aortic Stenosis: Diagnostic Patterns Severe AS without AVR Severe AS without Symptoms Low Flow/Low Gradient AS AS + CAD
Aortic Stenosis Should asymptomatic patients with severe AS undergo AVR? ?
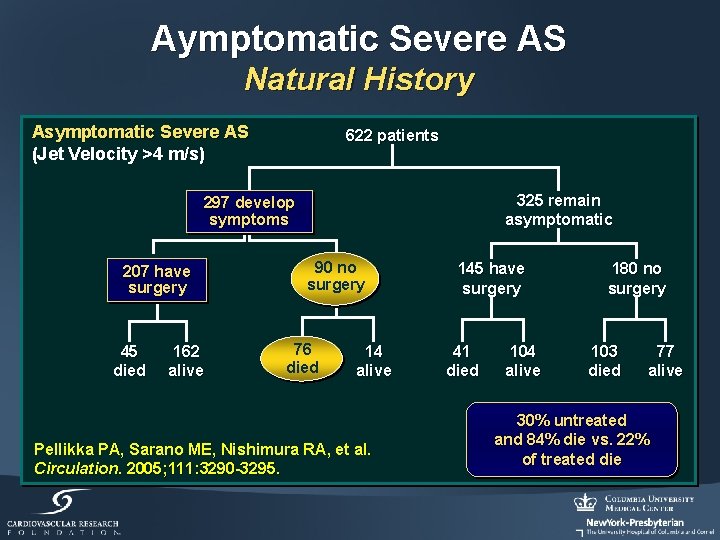
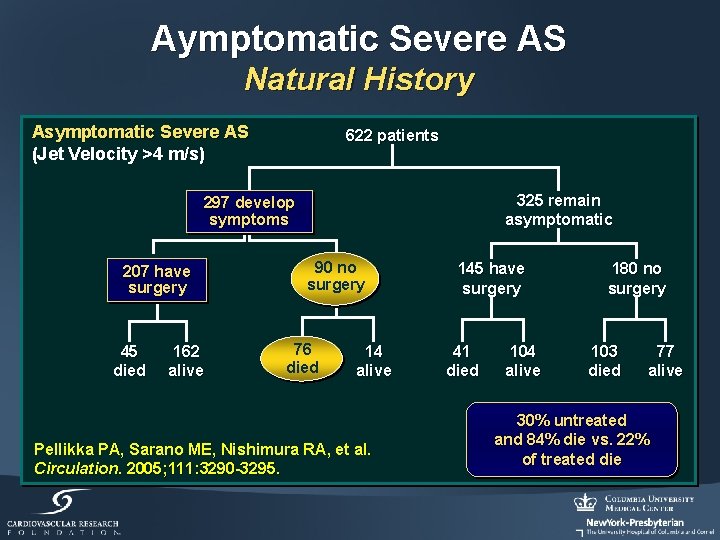
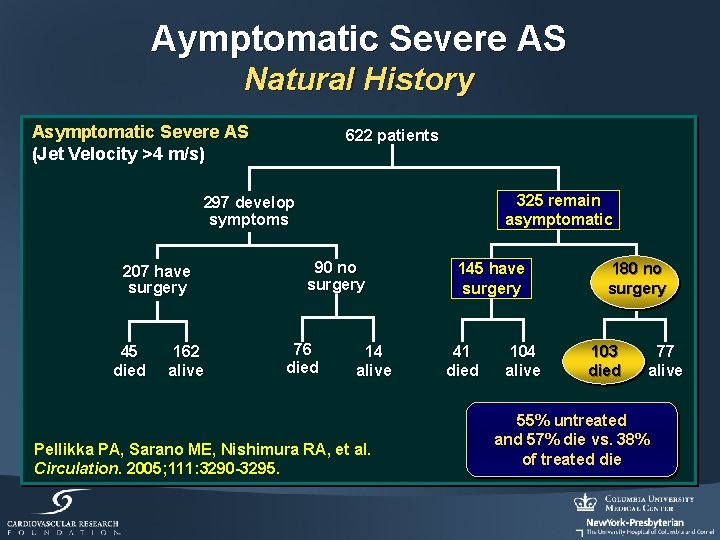
Aymptomatic Severe AS Natural History Asymptomatic Severe AS (Jet Velocity >4 m/s) 622 patients 325 remain asymptomatic 297 develop symptoms 207 have surgery 45 died 162 alive 90 no surgery 76 died 14 alive Pellikka PA, Sarano ME, Nishimura RA, et al. Circulation. 2005; 111: 3290 -3295. 145 have surgery 41 died 104 alive 180 no surgery 103 died 77 alive 30% untreated and 84% die vs. 22% of treated die
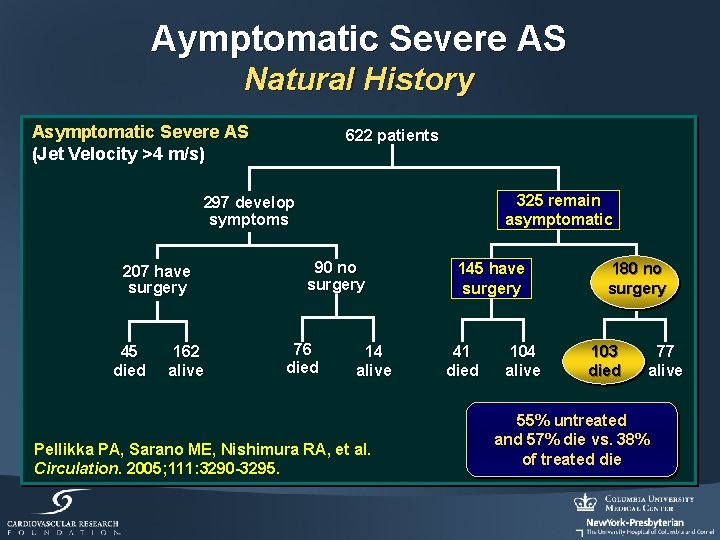
Aymptomatic Severe AS Natural History Asymptomatic Severe AS (Jet Velocity >4 m/s) 622 patients 325 remain asymptomatic 297 develop symptoms 207 have surgery 45 died 162 alive 90 no surgery 76 died 14 alive Pellikka PA, Sarano ME, Nishimura RA, et al. Circulation. 2005; 111: 3290 -3295. 145 have surgery 41 died 104 alive 180 no surgery 103 died 77 alive 55% untreated and 57% die vs. 38% of treated die
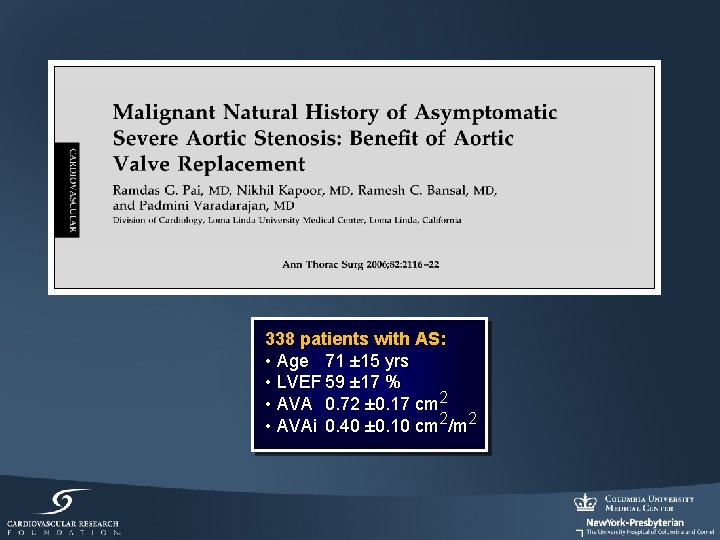
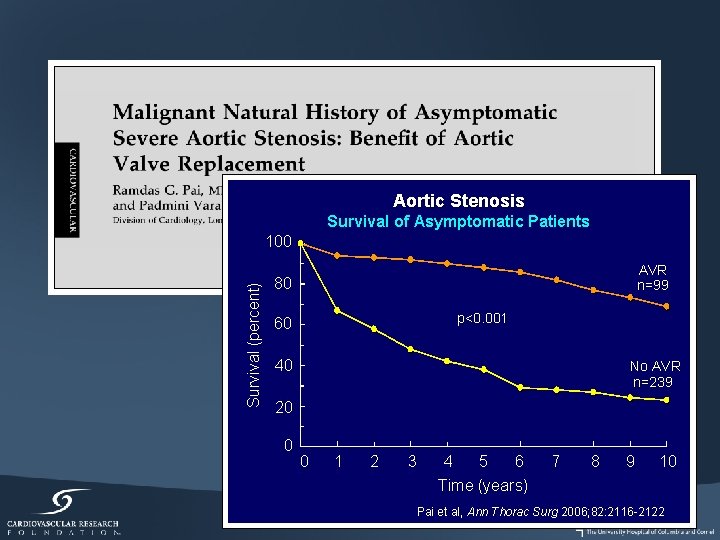
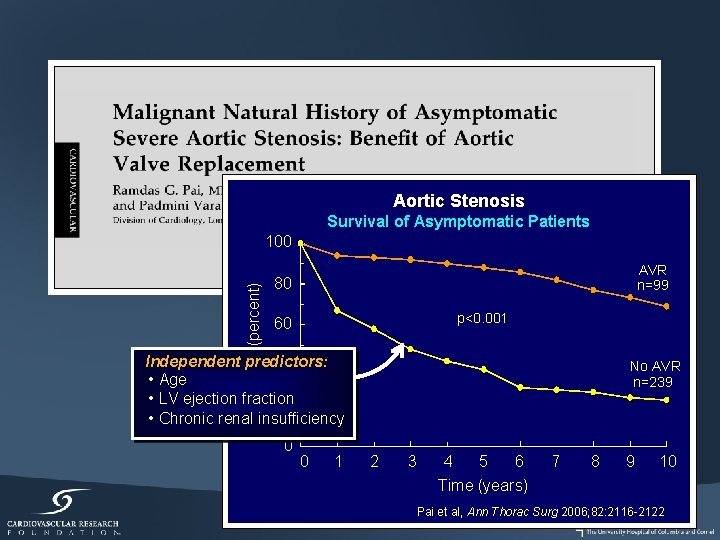
338 patients with AS: • Age 71 ± 15 yrs • LVEF 59 ± 17 % • AVA 0. 72 ± 0. 17 cm 2 • AVAi 0. 40 ± 0. 10 cm 2/m 2
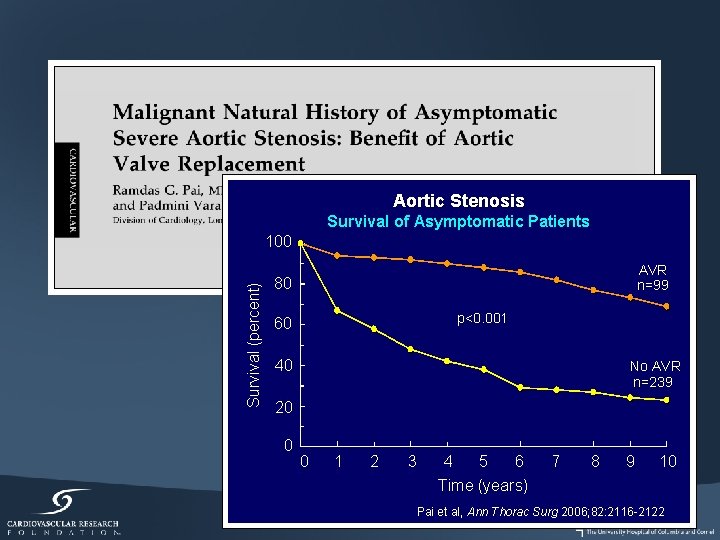
Aortic Stenosis Survival of Asymptomatic Patients Survival (percent) 100 AVR n=99 80 p<0. 001 60 40 No AVR n=239 20 0 0 1 2 3 4 5 6 Time (years) 7 8 9 10 Pai et al, Ann Thorac Surg 2006; 82: 2116 -2122
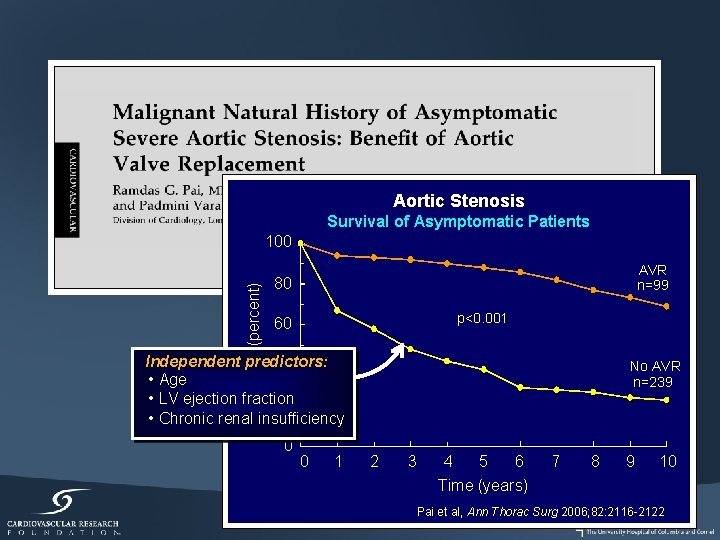
Aortic Stenosis Survival of Asymptomatic Patients Survival (percent) 100 AVR n=99 80 p<0. 001 60 Independent predictors: 40 • Age • LV ejection fraction 20 • Chronic renal insufficiency 0 0 1 No AVR n=239 2 3 4 5 6 Time (years) 7 8 9 10 Pai et al, Ann Thorac Surg 2006; 82: 2116 -2122
Aortic Stenosis Are asymptomatic patients with severe AS really asymptomatic? ?
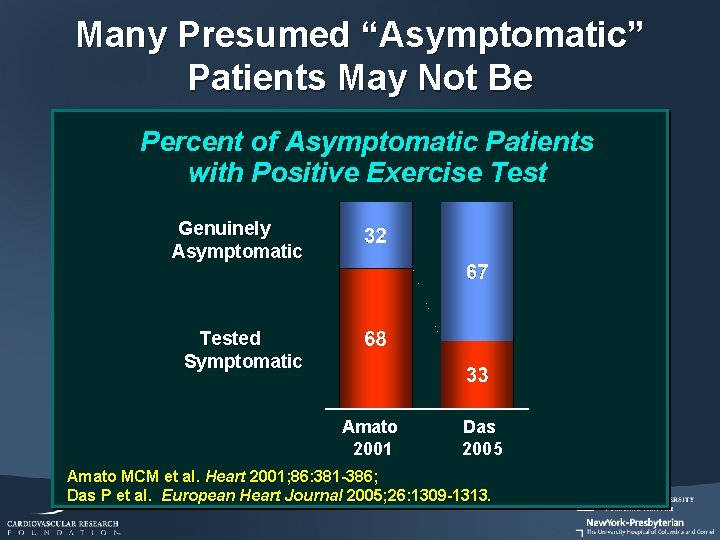
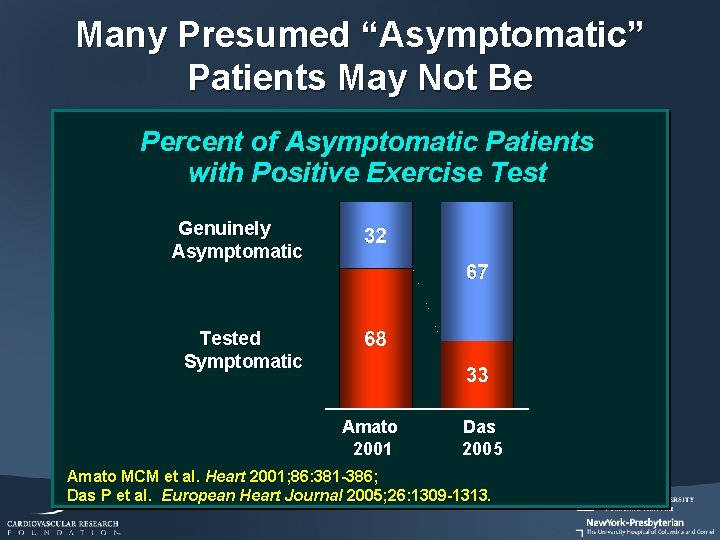
Many Presumed “Asymptomatic” Patients May Not Be Percent of Asymptomatic Patients with Positive Exercise Test Genuinely Asymptomatic Tested Symptomatic Amato 2001 Das 2005 Amato MCM et al. Heart 2001; 86: 381 -386; Das P et al. European Heart Journal 2005; 26: 1309 -1313.
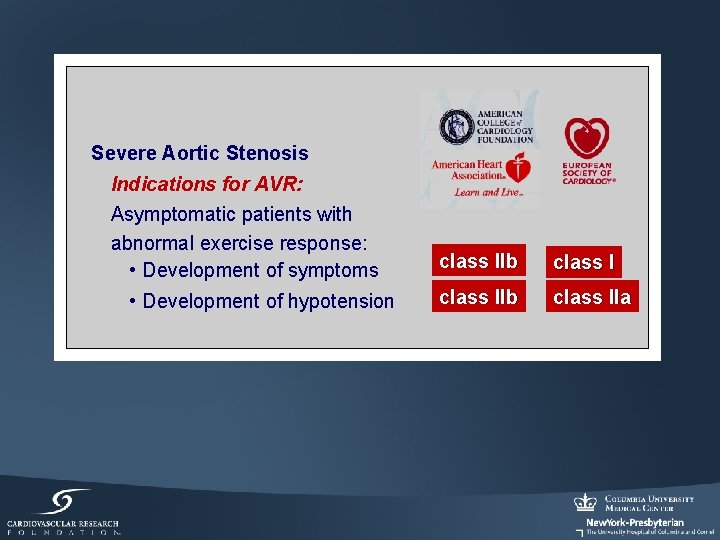
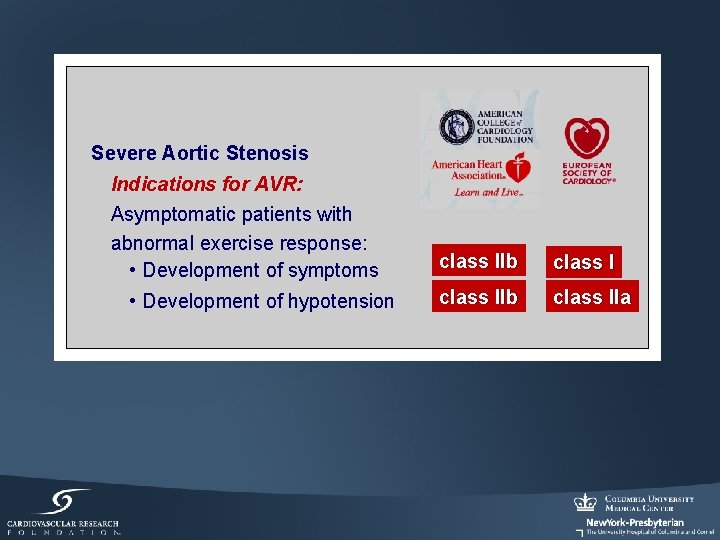
Severe Aortic Stenosis Indications for AVR: Asymptomatic patients with abnormal exercise response: • Development of symptoms • Development of hypotension class IIb class IIa
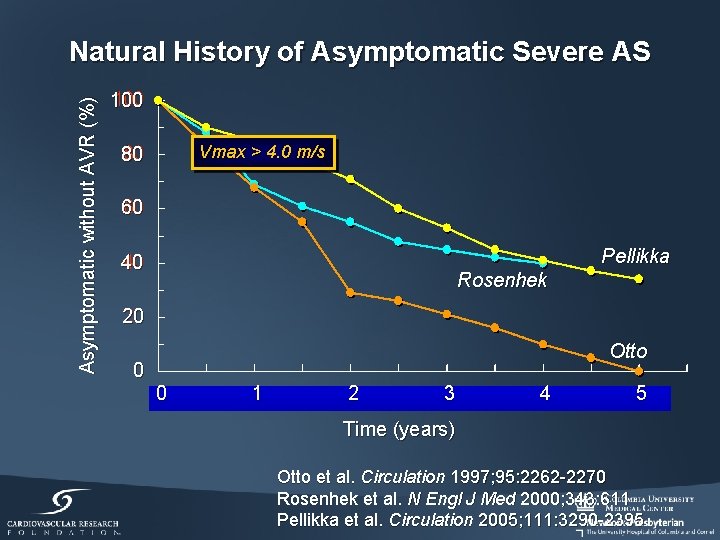
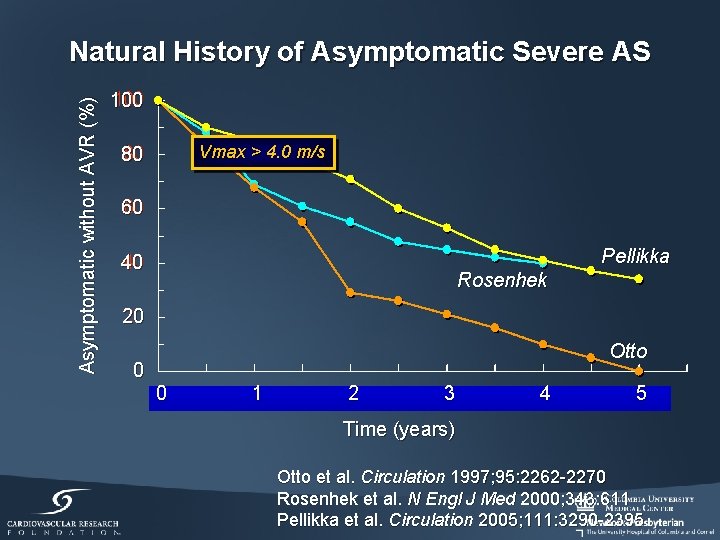
Asymptomatic without AVR (%) Natural History of Asymptomatic Severe AS 100 Vmax > 4. 0 m/s 80 60 Pellikka 40 Rosenhek 20 0 Otto 0 1 2 3 4 5 Time (years) Otto et al. Circulation 1997; 95: 2262 -2270 Rosenhek et al. N Engl J Med 2000; 343: 611 Pellikka et al. Circulation 2005; 111: 3290 -2395
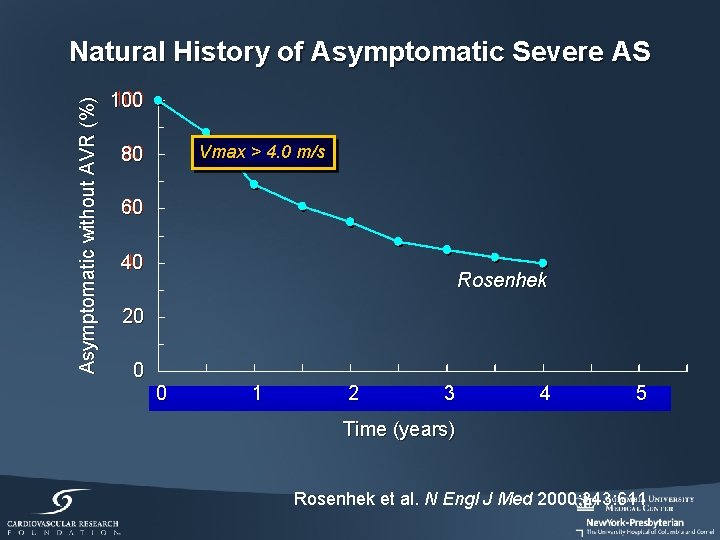
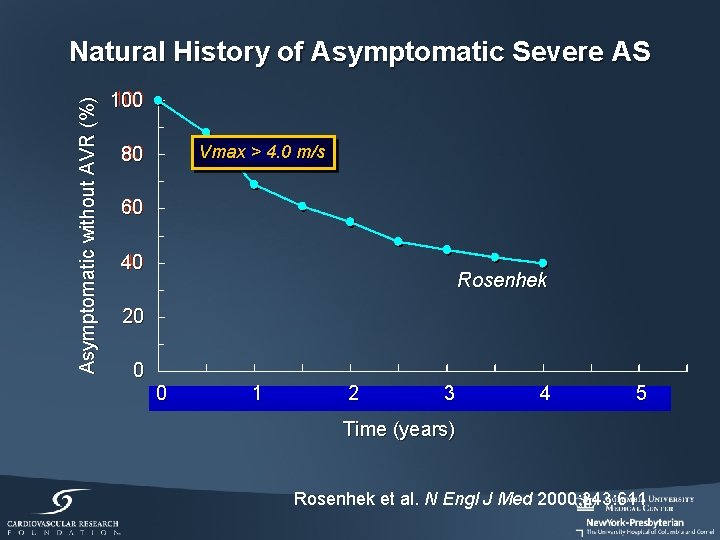
Asymptomatic without AVR (%) Natural History of Asymptomatic Severe AS 100 Vmax > 4. 0 m/s 80 60 40 Rosenhek 20 0 0 1 2 3 4 5 Time (years) Rosenhek et al. N Engl J Med 2000; 343: 611
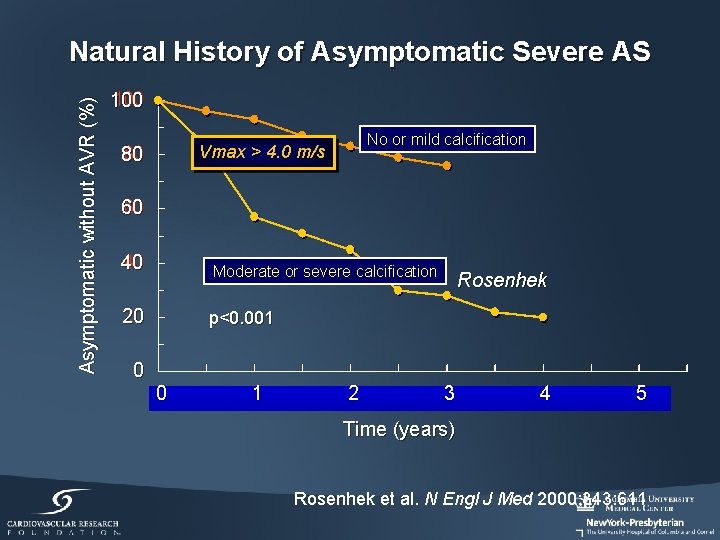
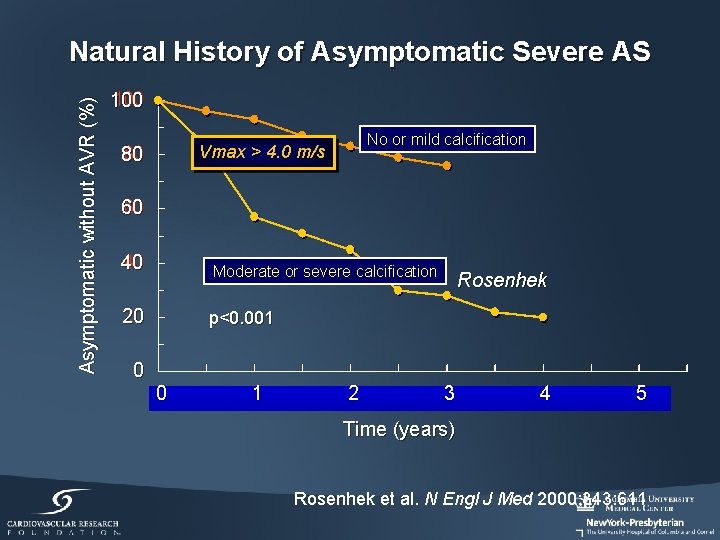
Asymptomatic without AVR (%) Natural History of Asymptomatic Severe AS 100 No or mild calcification Vmax > 4. 0 m/s 80 60 40 Moderate or severe calcification 20 p<0. 001 0 0 1 2 Rosenhek 3 4 5 Time (years) Rosenhek et al. N Engl J Med 2000; 343: 611
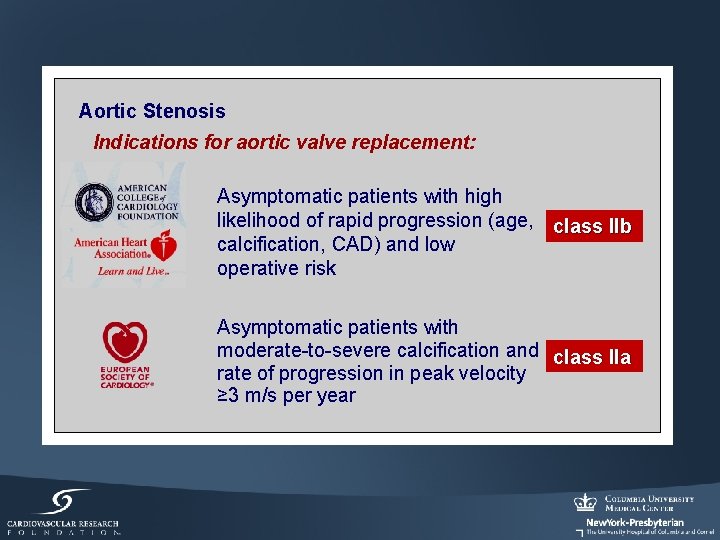
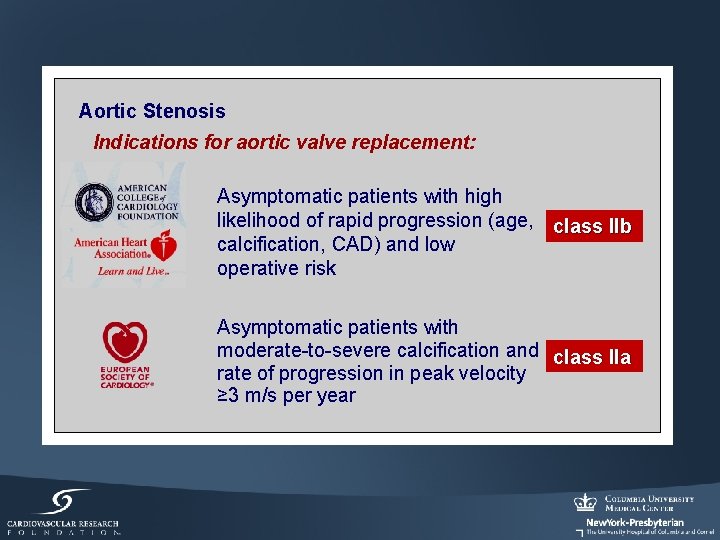
Aortic Stenosis Indications for aortic valve replacement: Asymptomatic patients with high likelihood of rapid progression (age, class IIb calcification, CAD) and low operative risk Asymptomatic patients with moderate-to-severe calcification and class IIa rate of progression in peak velocity ≥ 3 m/s per year
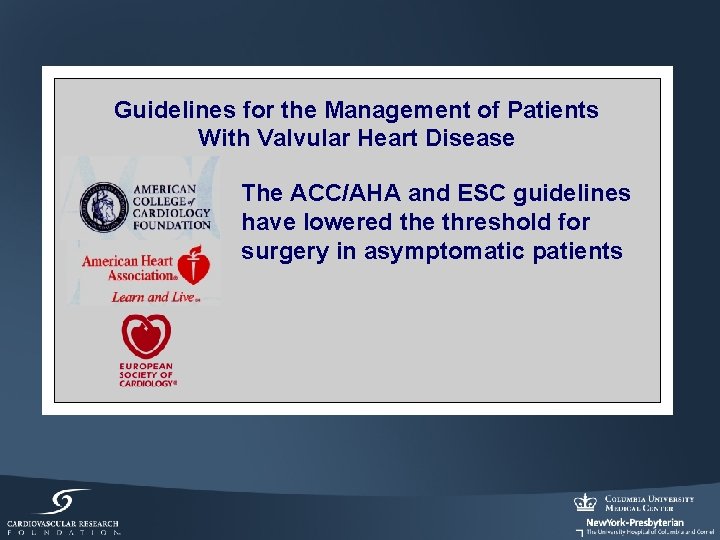
Guidelines for the Management of Patients With Valvular Heart Disease The ACC/AHA and ESC guidelines have lowered the threshold for surgery in asymptomatic patients
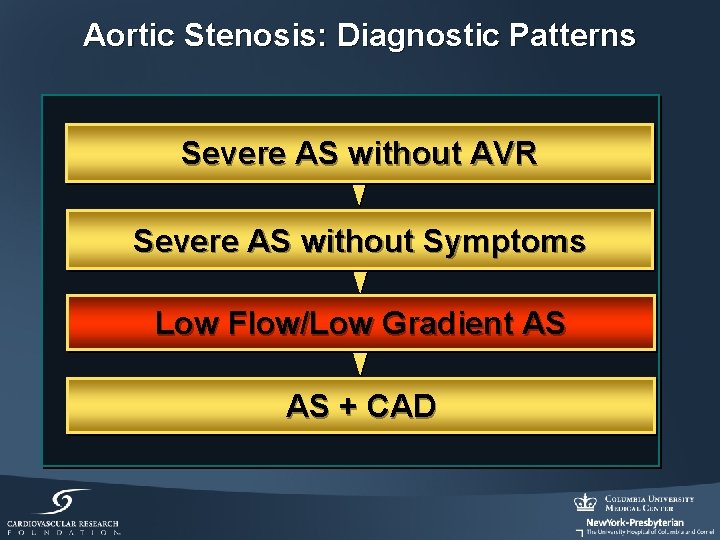
Aortic Stenosis: Diagnostic Patterns Severe AS without AVR Severe AS without Symptoms Low Flow/Low Gradient AS AS + CAD
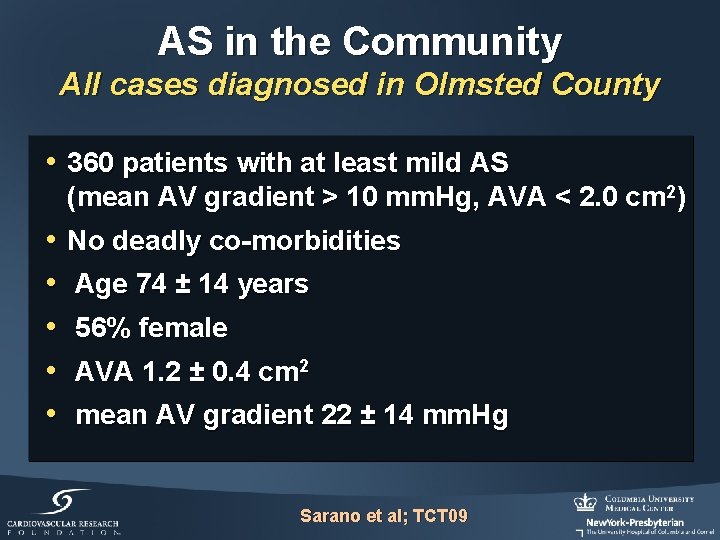
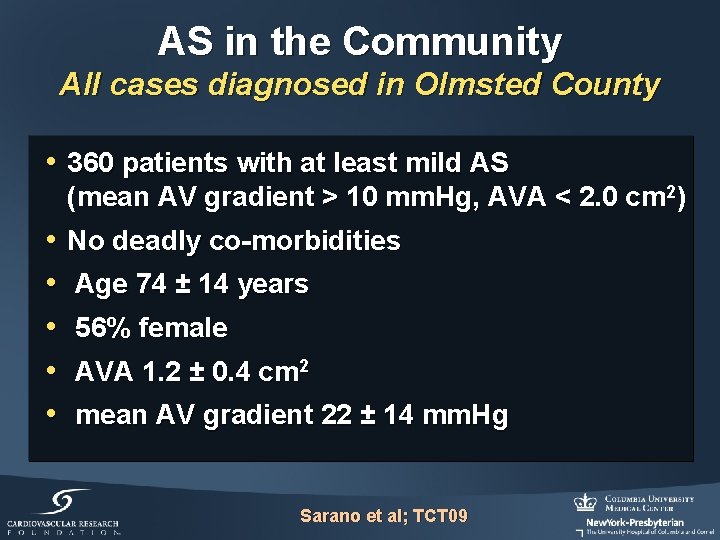
AS in the Community All cases diagnosed in Olmsted County • 360 patients with at least mild AS (mean AV gradient > 10 mm. Hg, AVA < 2. 0 cm 2) • • • No deadly co-morbidities Age 74 ± 14 years 56% female AVA 1. 2 ± 0. 4 cm 2 mean AV gradient 22 ± 14 mm. Hg Sarano et al; TCT 09
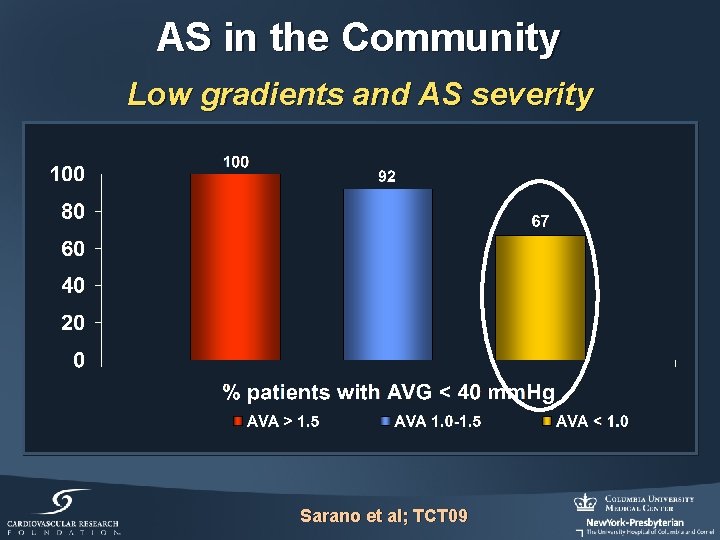
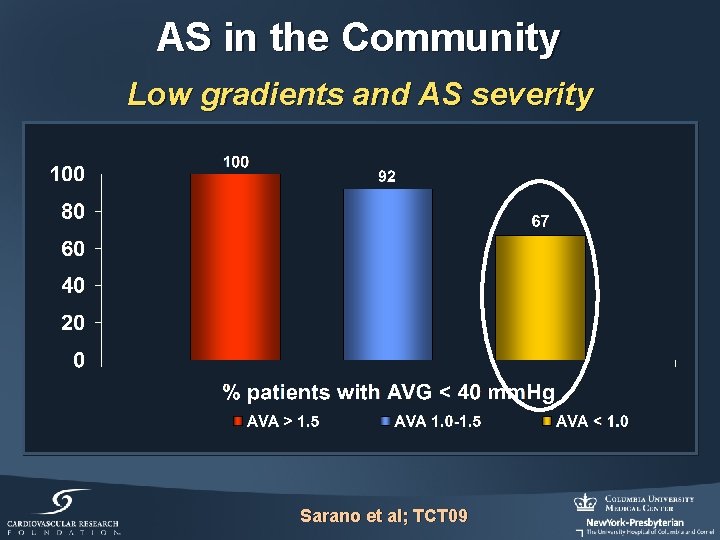
AS in the Community Low gradients and AS severity Sarano et al; TCT 09
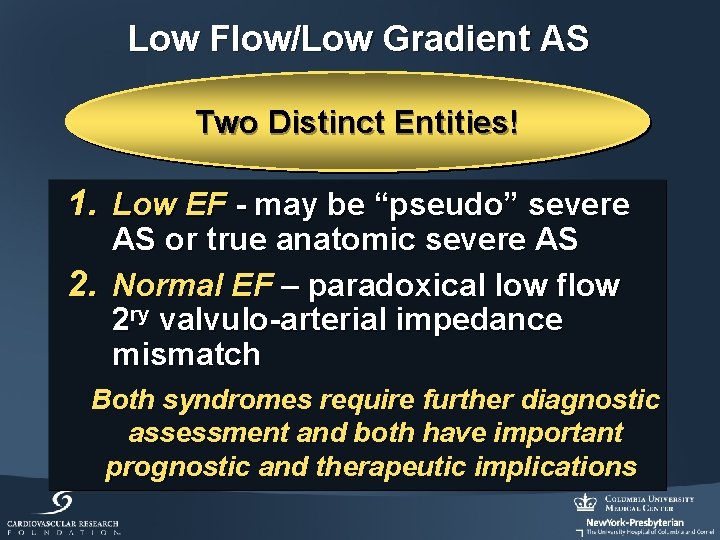
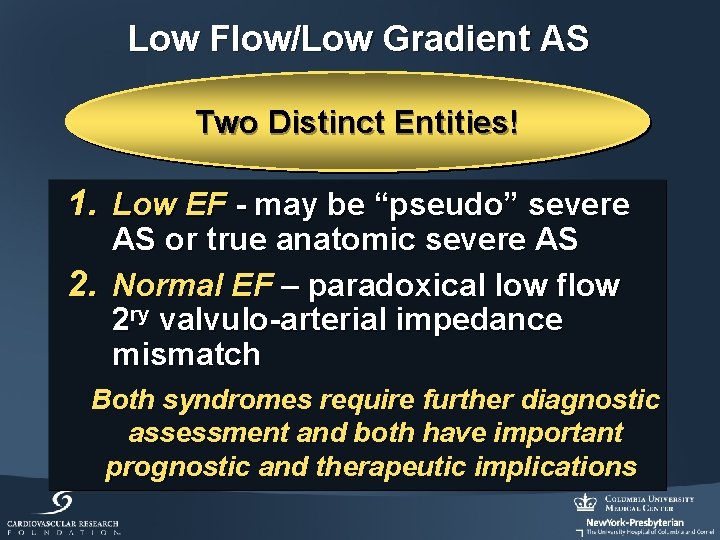
Low Flow/Low Gradient AS Two Distinct Entities! 1. Low EF - may be “pseudo” severe AS or true anatomic severe AS 2. Normal EF – paradoxical low flow 2 ry valvulo-arterial impedance mismatch Both syndromes require further diagnostic assessment and both have important prognostic and therapeutic implications
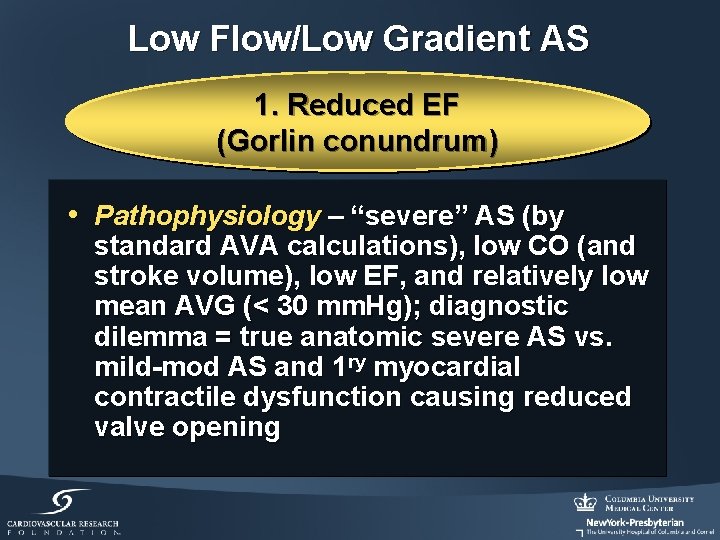
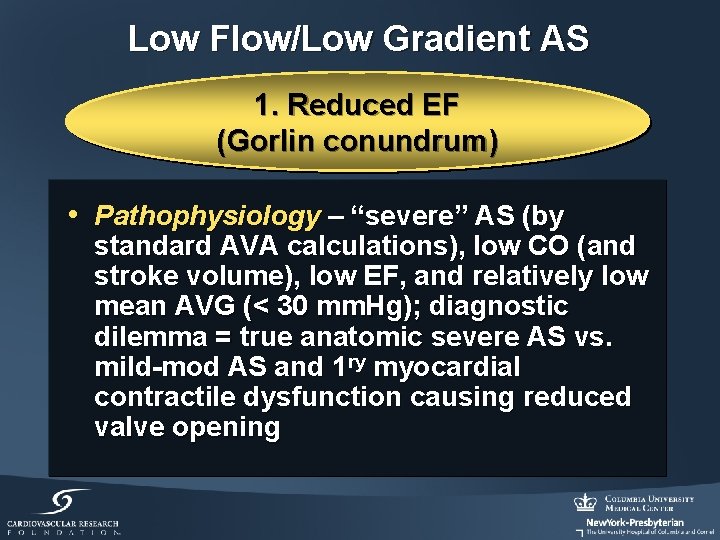
Low Flow/Low Gradient AS 1. Reduced EF (Gorlin conundrum) • Pathophysiology – “severe” AS (by standard AVA calculations), low CO (and stroke volume), low EF, and relatively low mean AVG (< 30 mm. Hg); diagnostic dilemma = true anatomic severe AS vs. mild-mod AS and 1 ry myocardial contractile dysfunction causing reduced valve opening
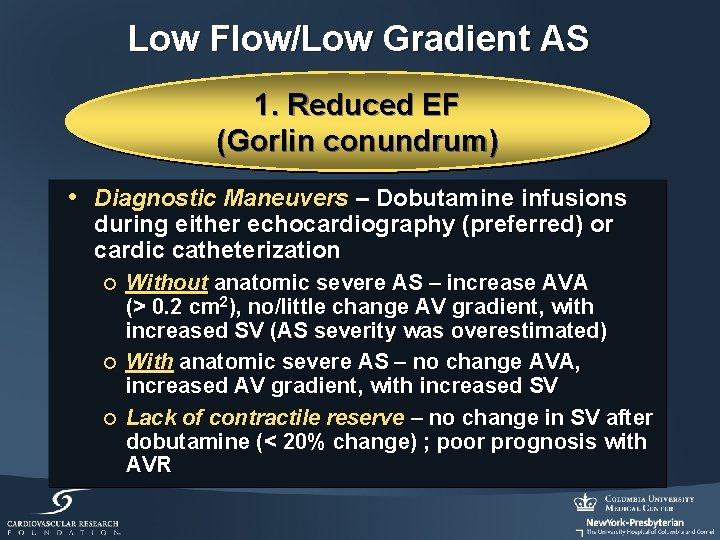
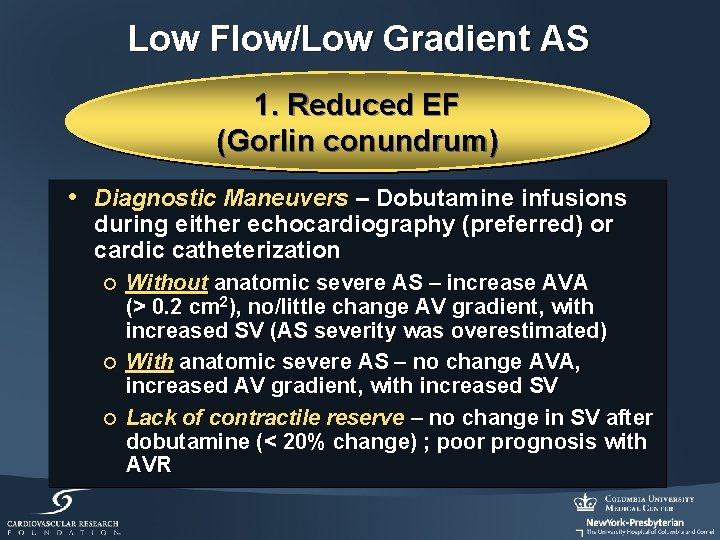
Low Flow/Low Gradient AS 1. Reduced EF (Gorlin conundrum) • Diagnostic Maneuvers – Dobutamine infusions during either echocardiography (preferred) or cardic catheterization ¡ ¡ ¡ Without anatomic severe AS – increase AVA (> 0. 2 cm 2), no/little change AV gradient, with increased SV (AS severity was overestimated) With anatomic severe AS – no change AVA, increased AV gradient, with increased SV Lack of contractile reserve – no change in SV after dobutamine (< 20% change) ; poor prognosis with AVR
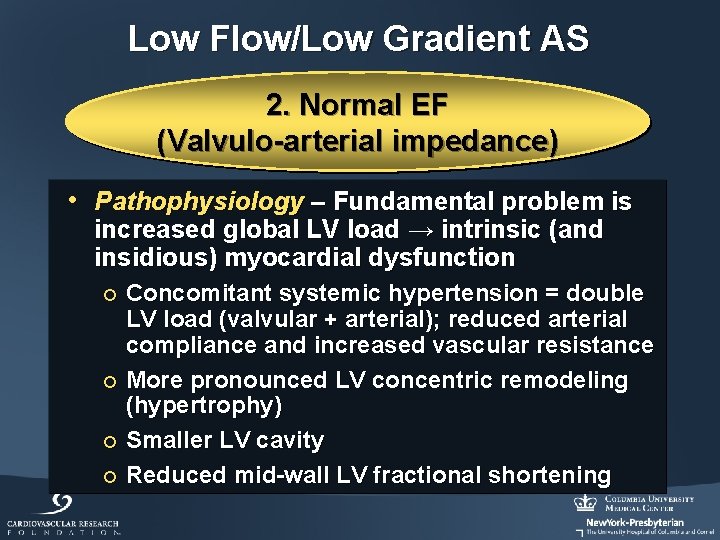
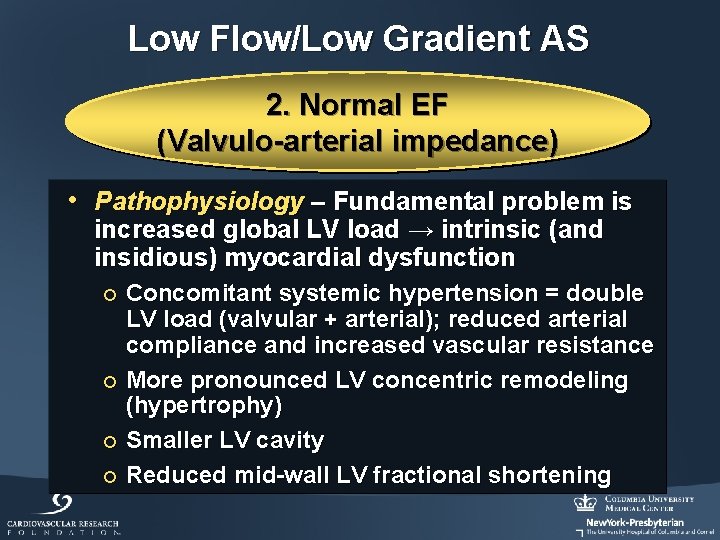
Low Flow/Low Gradient AS 2. Normal EF (Valvulo-arterial impedance) • Pathophysiology – Fundamental problem is increased global LV load → intrinsic (and insidious) myocardial dysfunction Concomitant systemic hypertension = double LV load (valvular + arterial); reduced arterial compliance and increased vascular resistance ¡ More pronounced LV concentric remodeling (hypertrophy) ¡ Smaller LV cavity ¡ Reduced mid-wall LV fractional shortening ¡
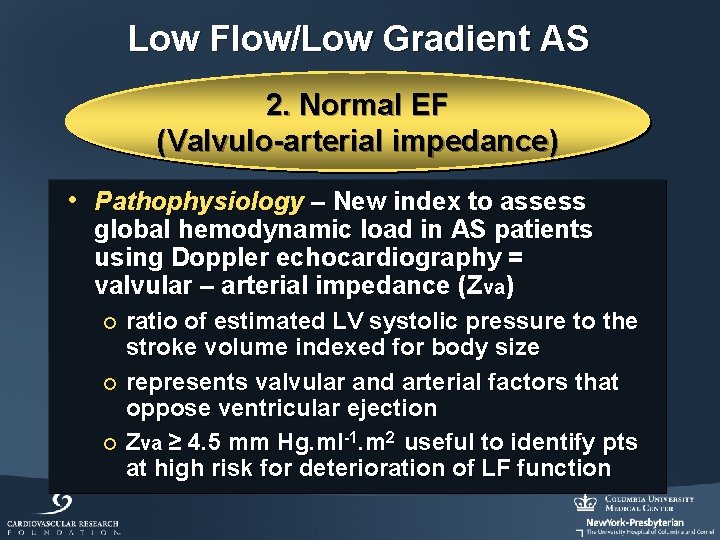
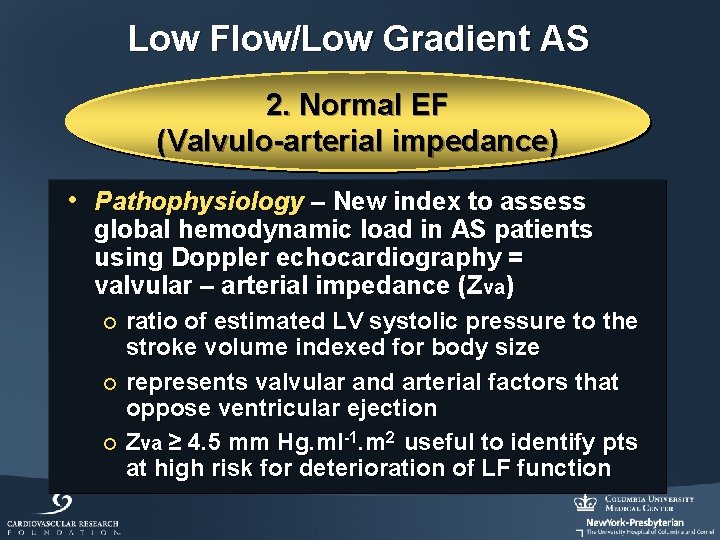
Low Flow/Low Gradient AS 2. Normal EF (Valvulo-arterial impedance) • Pathophysiology – New index to assess global hemodynamic load in AS patients using Doppler echocardiography = valvular – arterial impedance (Zva) ratio of estimated LV systolic pressure to the stroke volume indexed for body size ¡ represents valvular and arterial factors that oppose ventricular ejection ¡ Zva ≥ 4. 5 mm Hg. ml-1. m 2 useful to identify pts at high risk for deterioration of LF function ¡
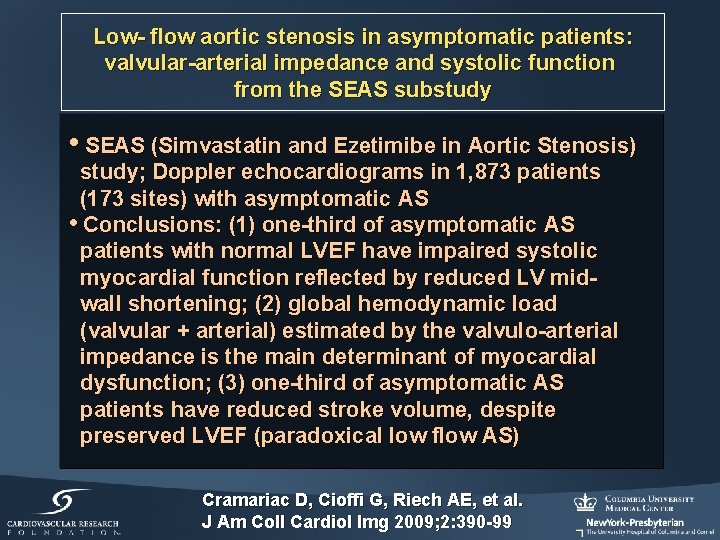
Low- flow aortic stenosis in asymptomatic patients: valvular-arterial impedance and systolic function from the SEAS substudy • SEAS (Simvastatin and Ezetimibe in Aortic Stenosis) study; Doppler echocardiograms in 1, 873 patients (173 sites) with asymptomatic AS • Conclusions: (1) one-third of asymptomatic AS patients with normal LVEF have impaired systolic myocardial function reflected by reduced LV midwall shortening; (2) global hemodynamic load (valvular + arterial) estimated by the valvulo-arterial impedance is the main determinant of myocardial dysfunction; (3) one-third of asymptomatic AS patients have reduced stroke volume, despite preserved LVEF (paradoxical low flow AS) Cramariac D, Cioffi G, Riech AE, et al. J Am Coll Cardiol Img 2009; 2: 390 -99
Paradoxical Low Flow/Low Gradient Severe AS
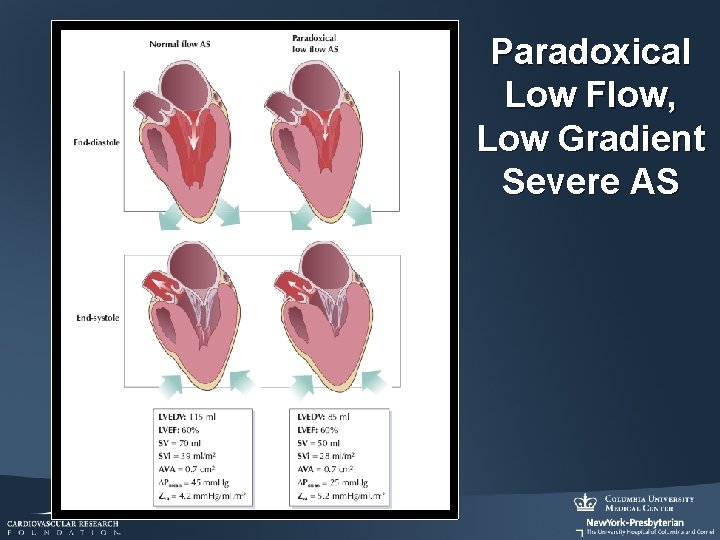
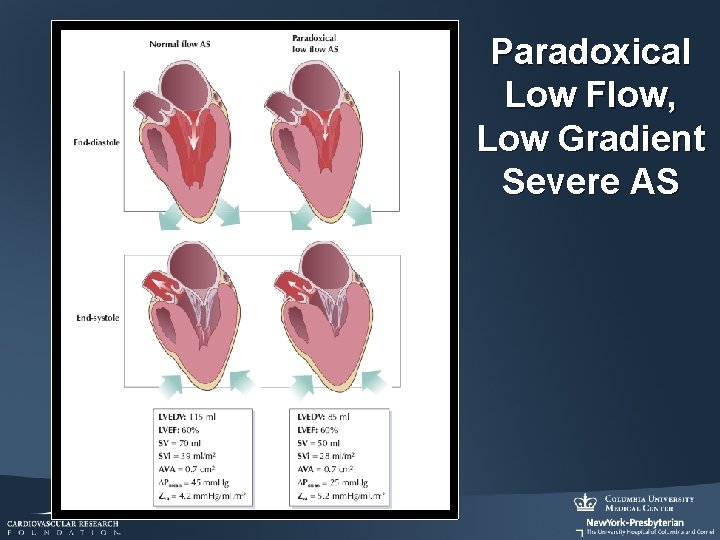
Paradoxical Low Flow, Low Gradient Severe AS
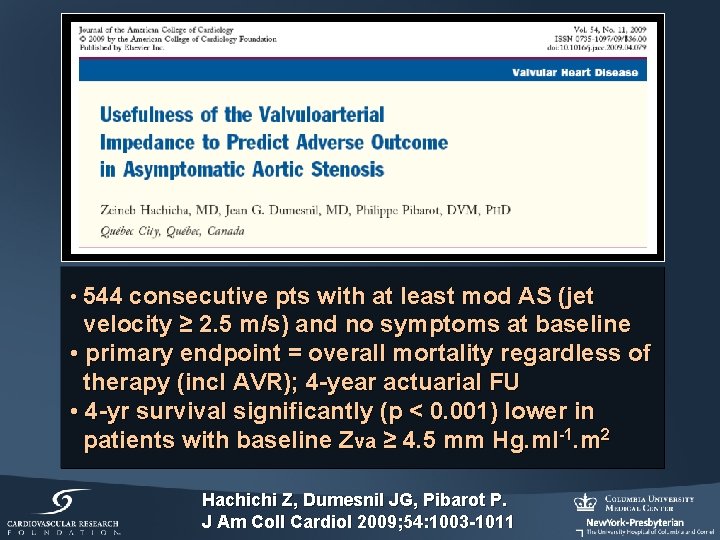
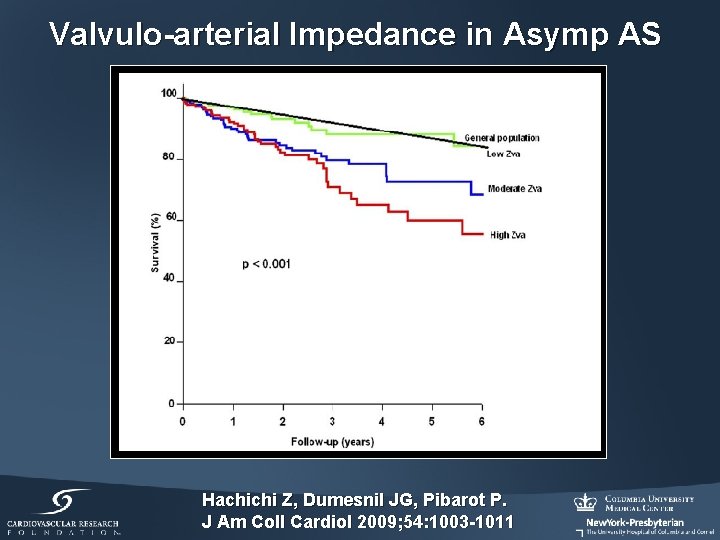
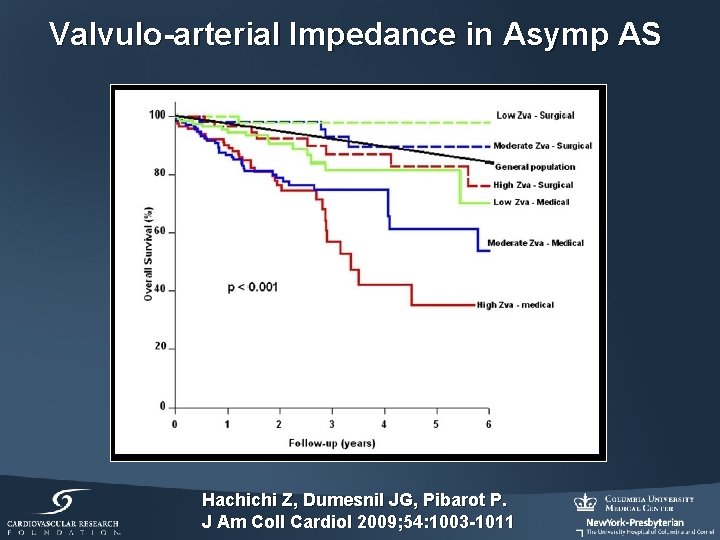
• 544 consecutive pts with at least mod AS (jet velocity ≥ 2. 5 m/s) and no symptoms at baseline • primary endpoint = overall mortality regardless of therapy (incl AVR); 4 -year actuarial FU • 4 -yr survival significantly (p < 0. 001) lower in patients with baseline Zva ≥ 4. 5 mm Hg. ml-1. m 2 Hachichi Z, Dumesnil JG, Pibarot P. J Am Coll Cardiol 2009; 54: 1003 -1011
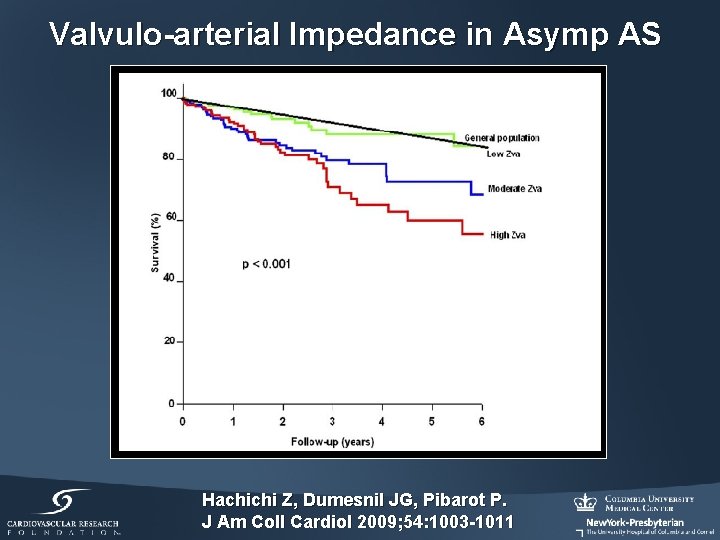
Valvulo-arterial Impedance in Asymp AS Hachichi Z, Dumesnil JG, Pibarot P. J Am Coll Cardiol 2009; 54: 1003 -1011
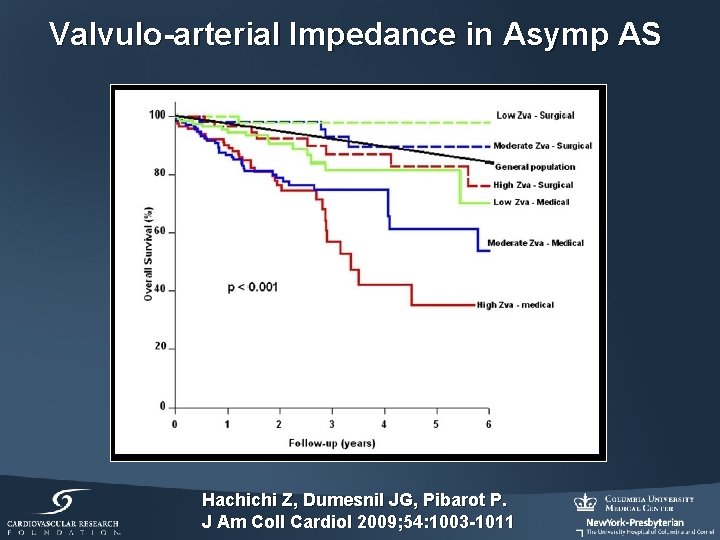
Valvulo-arterial Impedance in Asymp AS Hachichi Z, Dumesnil JG, Pibarot P. J Am Coll Cardiol 2009; 54: 1003 -1011
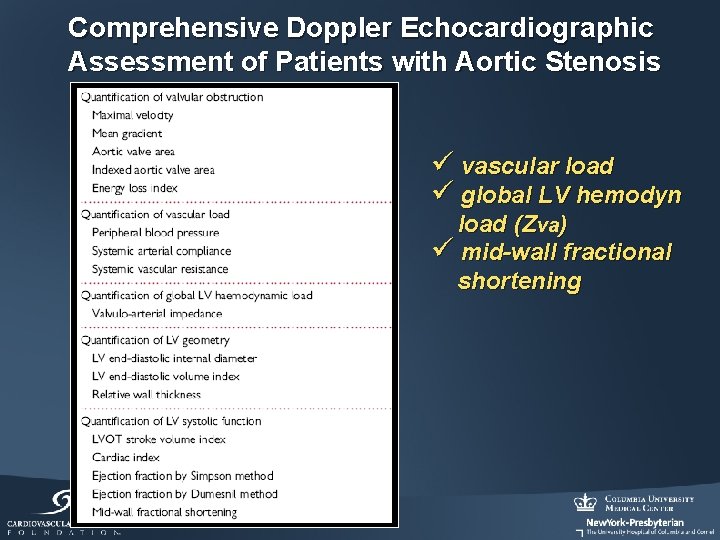
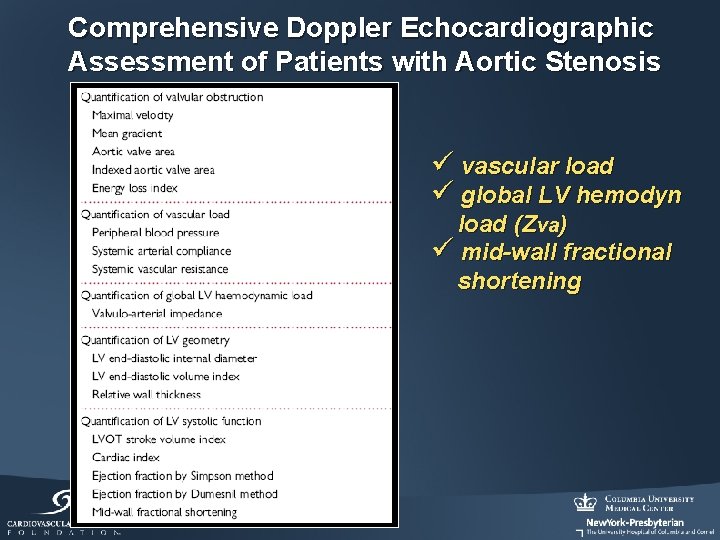
Comprehensive Doppler Echocardiographic Assessment of Patients with Aortic Stenosis ü vascular load ü global LV hemodyn load (Zva) ü mid-wall fractional shortening
Aortic Stenosis: Diagnostic Patterns Severe AS without AVR Severe AS without Symptoms Low Flow/Low Gradient AS AS + CAD
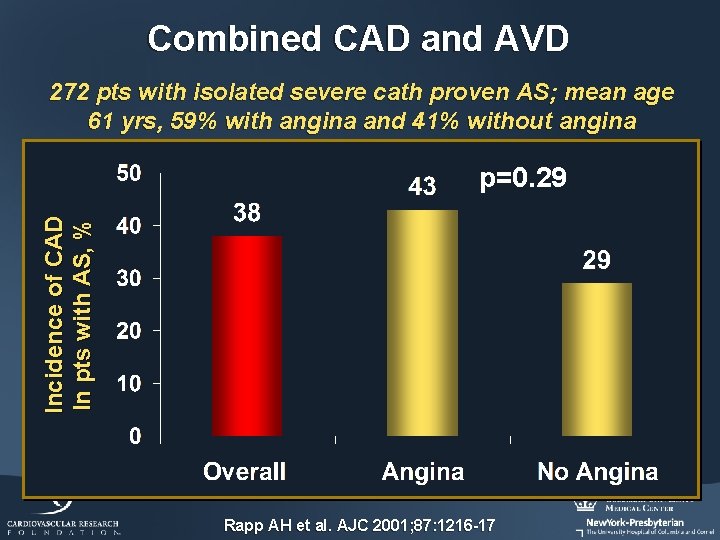
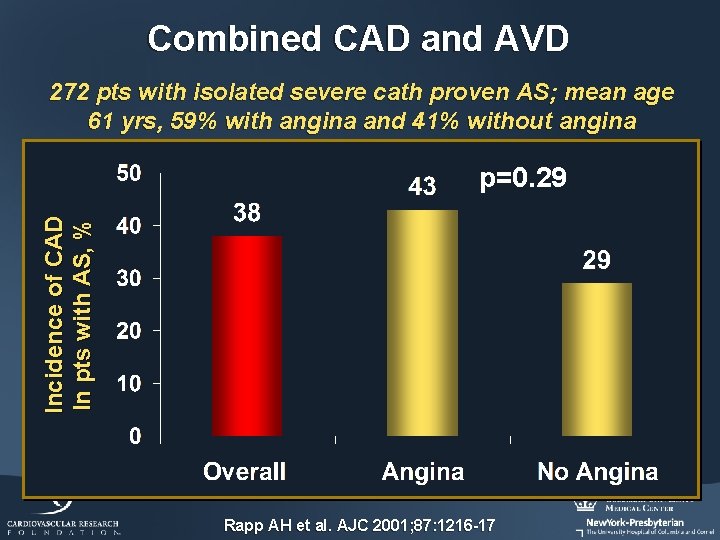
Combined CAD and AVD 272 pts with isolated severe cath proven AS; mean age 61 yrs, 59% with angina and 41% without angina Incidence of CAD In pts with AS, % p=0. 29 Rapp AH et al. AJC 2001; 87: 1216 -17
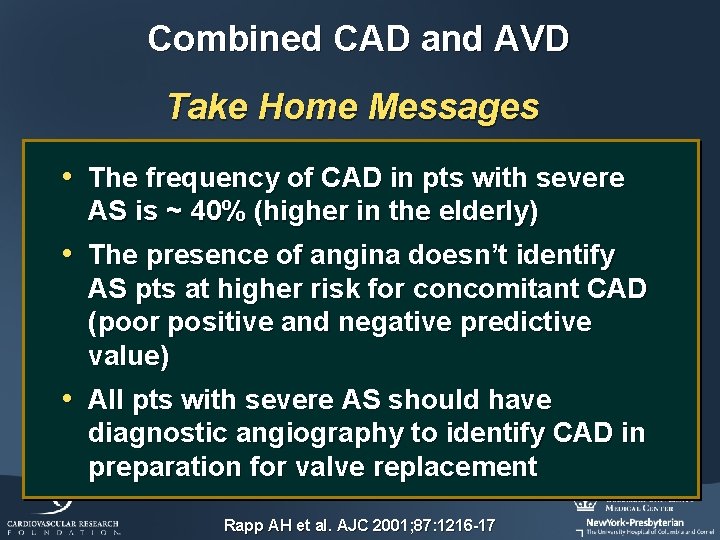
Combined CAD and AVD Take Home Messages • The frequency of CAD in pts with severe AS is ~ 40% (higher in the elderly) • The presence of angina doesn’t identify AS pts at higher risk for concomitant CAD (poor positive and negative predictive value) • All pts with severe AS should have diagnostic angiography to identify CAD in preparation for valve replacement Rapp AH et al. AJC 2001; 87: 1216 -17
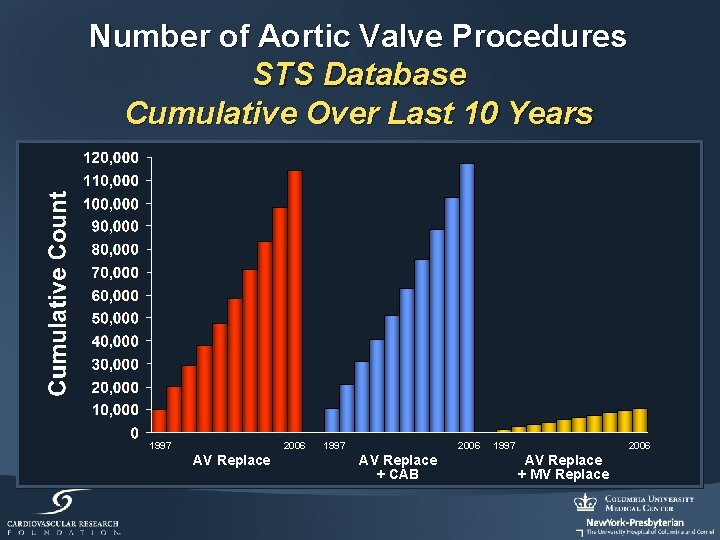
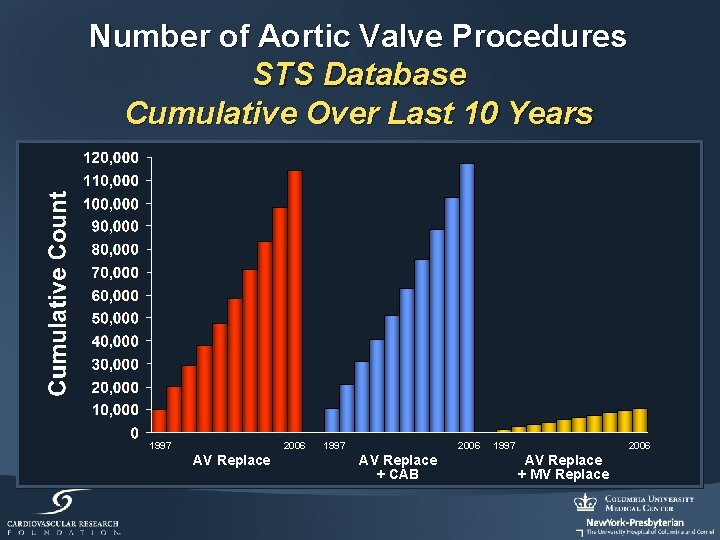
Number of Aortic Valve Procedures STS Database Cumulative Over Last 10 Years 1997 2006 AV Replace + CAB 1997 2006 AV Replace + MV Replace
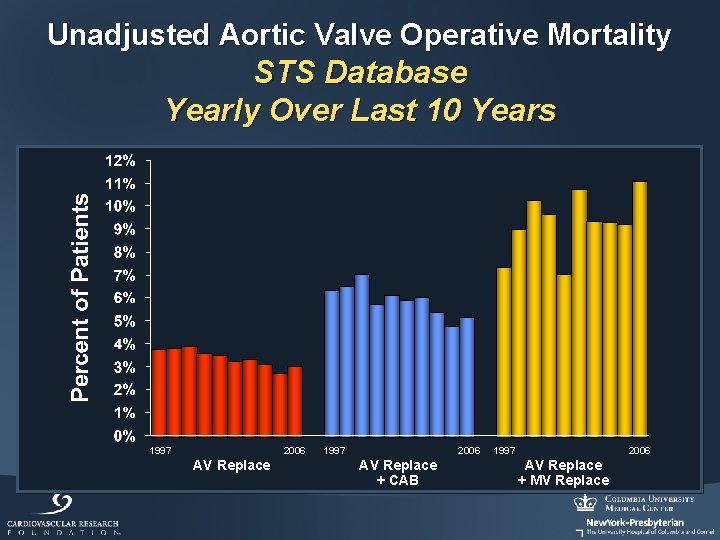
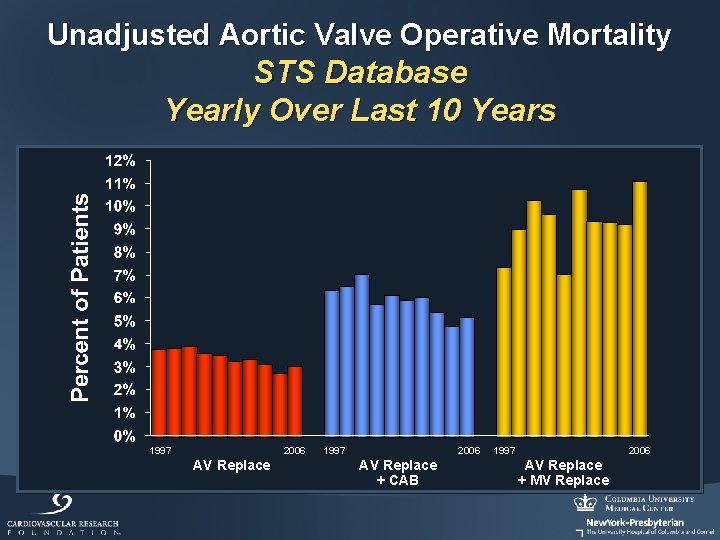
Unadjusted Aortic Valve Operative Mortality STS Database Yearly Over Last 10 Years 1997 2006 AV Replace + CAB 1997 2006 AV Replace + MV Replace
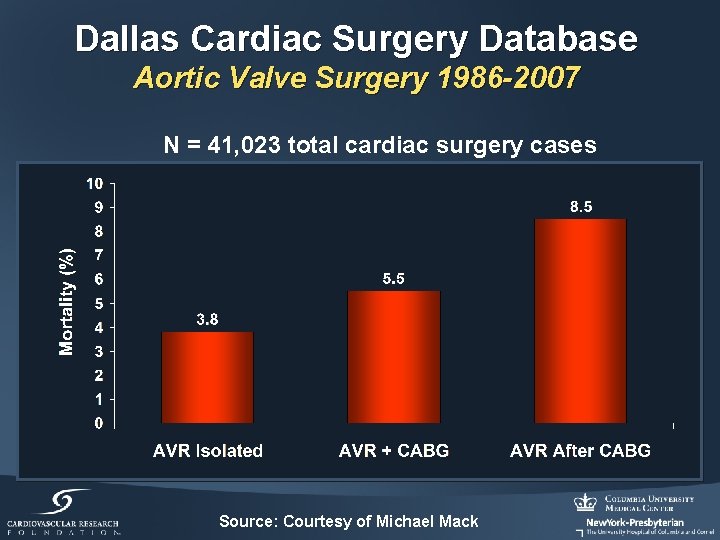
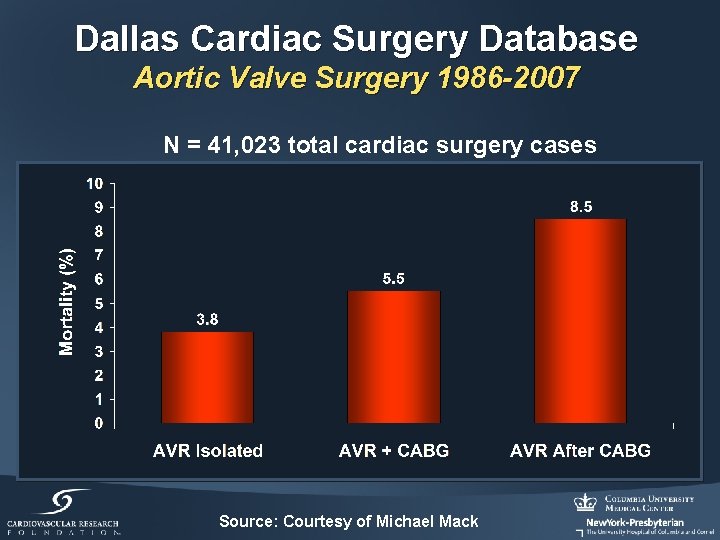
Dallas Cardiac Surgery Database Aortic Valve Surgery 1986 -2007 N = 41, 023 total cardiac surgery cases Source: Courtesy of Michael Mack
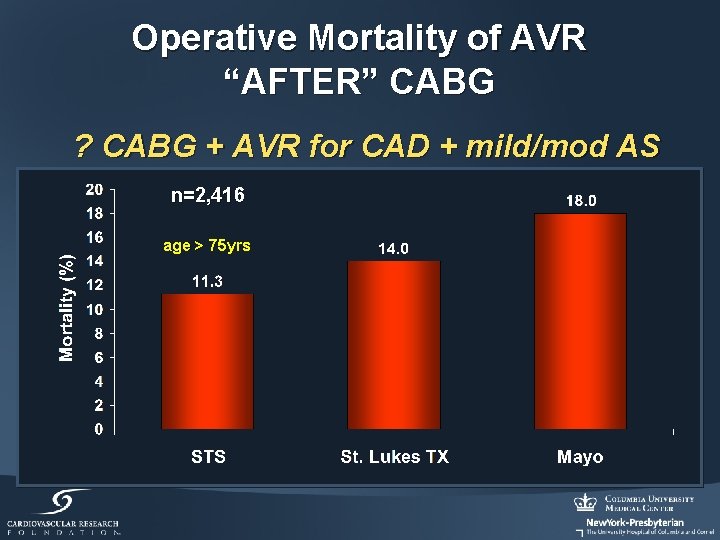
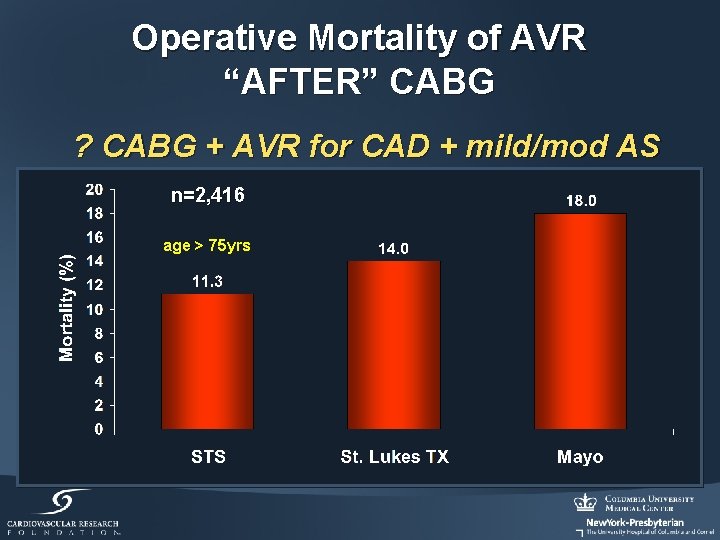
Operative Mortality of AVR “AFTER” CABG ? CABG + AVR for CAD + mild/mod AS n=2, 416 age > 75 yrs

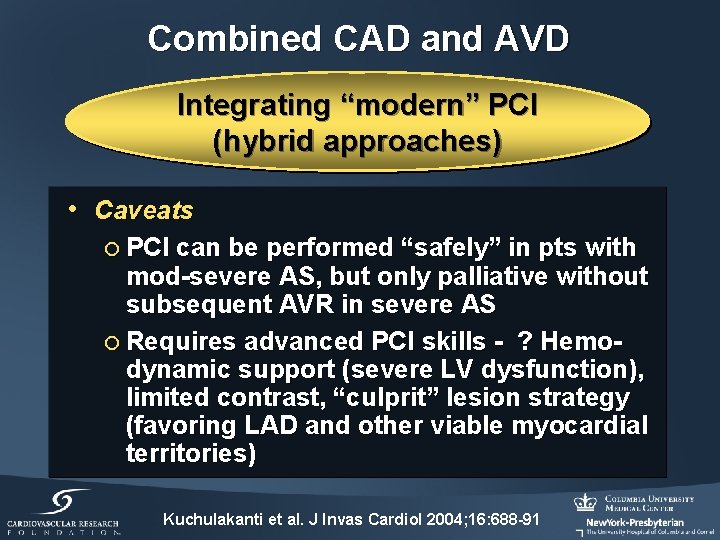
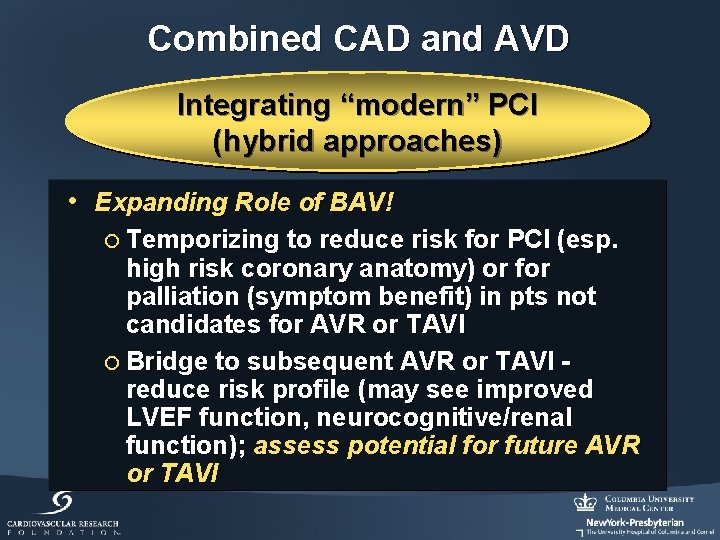
Combined CAD and AVD Integrating “modern” PCI (hybrid approaches) • Reasons – in high surgical risk or “inoperable” pts, pre-treatment with PCI may defer AVR (esp. in mod AS pts) or reduce subsequent risk of surgical AVR • Caveats ¡ Not a “replacement” for surgical AVR in normal risk pts ¡ Clinical presentation (esp. ACS a/o AMI) and coronary anatomy important
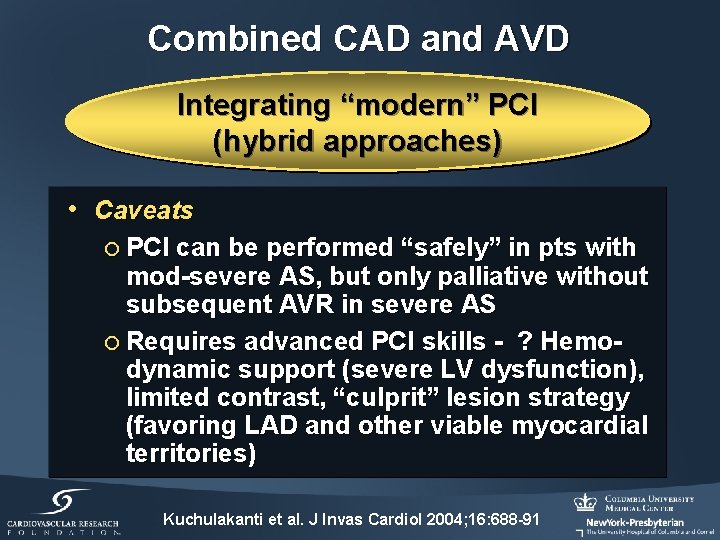
Combined CAD and AVD Integrating “modern” PCI (hybrid approaches) • Caveats ¡ PCI can be performed “safely” in pts with mod-severe AS, but only palliative without subsequent AVR in severe AS ¡ Requires advanced PCI skills - ? Hemodynamic support (severe LV dysfunction), limited contrast, “culprit” lesion strategy (favoring LAD and other viable myocardial territories) Kuchulakanti et al. J Invas Cardiol 2004; 16: 688 -91
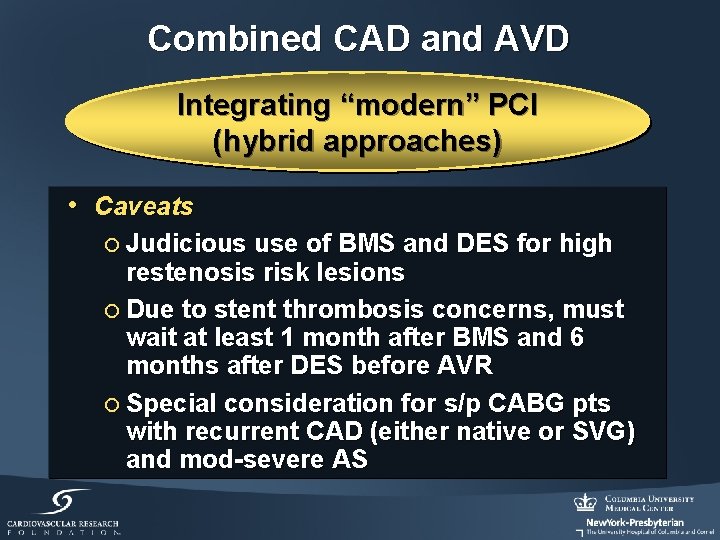
Combined CAD and AVD Integrating “modern” PCI (hybrid approaches) • Caveats ¡ Judicious use of BMS and DES for high restenosis risk lesions ¡ Due to stent thrombosis concerns, must wait at least 1 month after BMS and 6 months after DES before AVR ¡ Special consideration for s/p CABG pts with recurrent CAD (either native or SVG) and mod-severe AS
Combined CAD and AVD Integrating “modern” PCI (hybrid approaches) • Expanding Role of BAV! ¡ Temporizing to reduce risk for PCI (esp. high risk coronary anatomy) or for palliation (symptom benefit) in pts not candidates for AVR or TAVI ¡ Bridge to subsequent AVR or TAVI reduce risk profile (may see improved LVEF function, neurocognitive/renal function); assess potential for future AVR or TAVI
“There is no treatment for aortic valve disease”
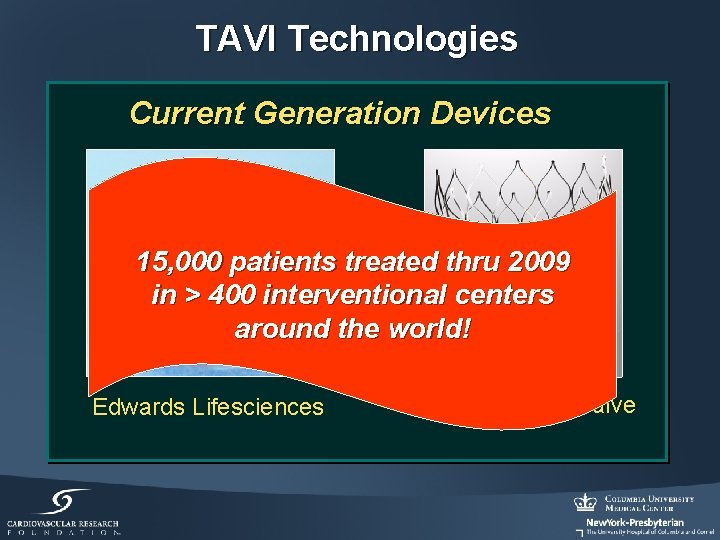
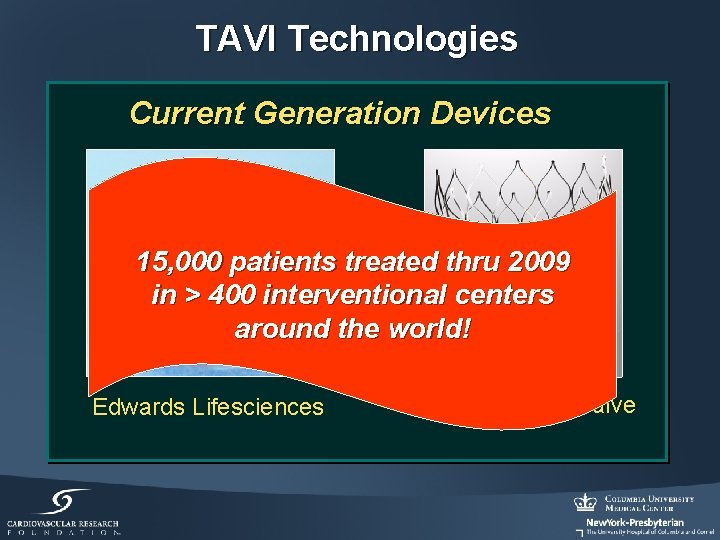
TAVI Technologies Current Generation Devices 15, 000 patients treated thru 2009 in > 400 interventional centers around the world! Edwards Lifesciences Medtronic Core. Valve