The Cardiovascular System Structure of the Heart Blood
The Cardiovascular System
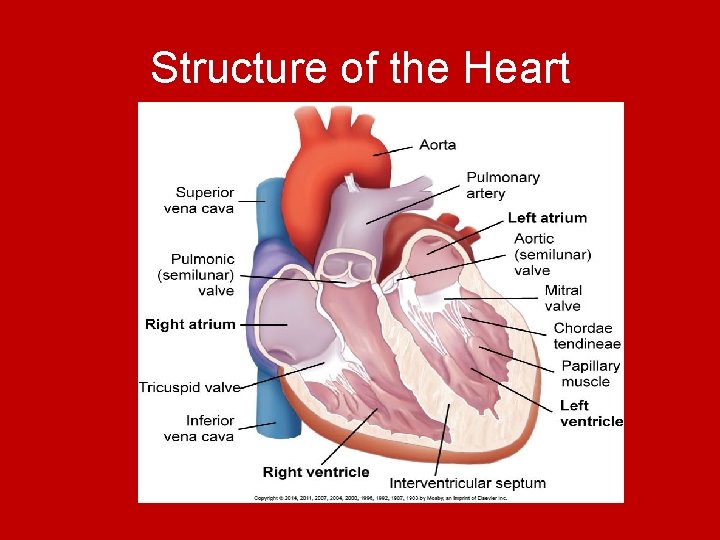
Structure of the Heart
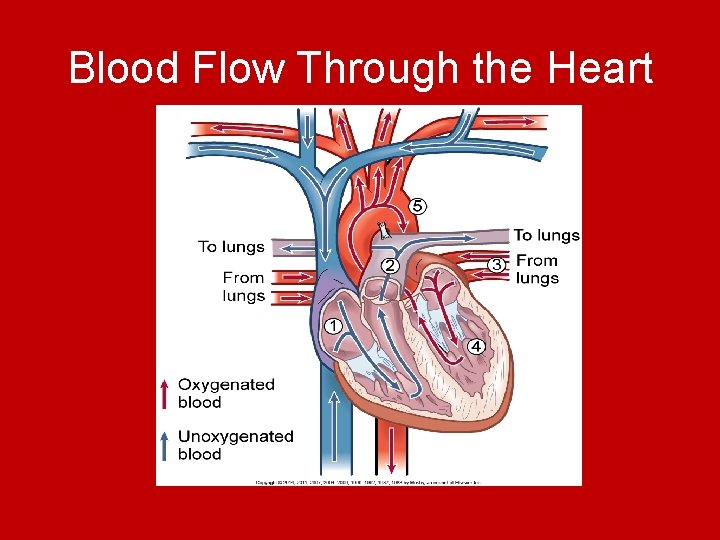
Blood Flow Through the Heart
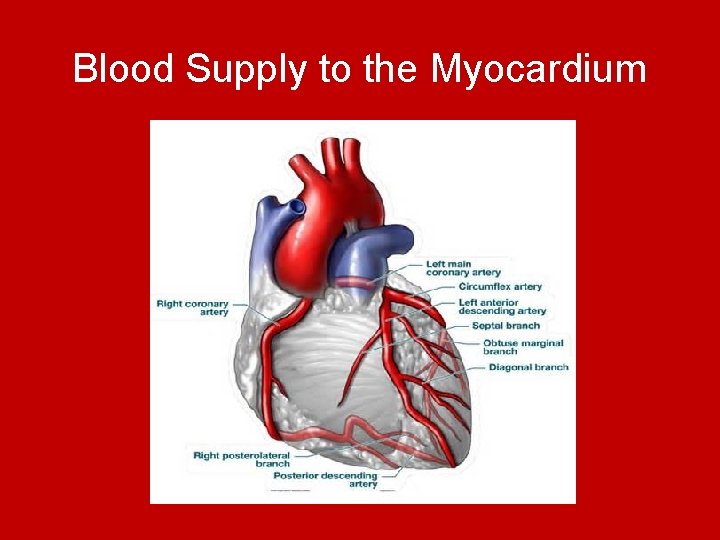
Blood Supply to the Myocardium
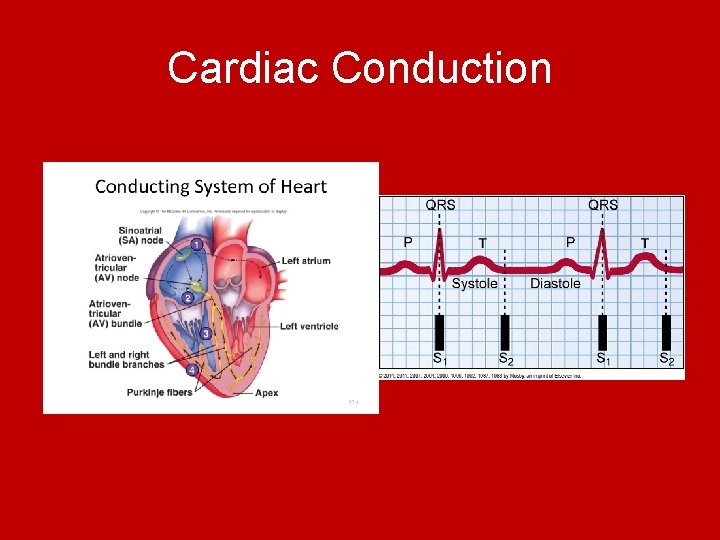
Cardiac Conduction
Cardiac Output • Amount of blood pumped by each ventricle in 1 minute • Stroke volume (SV) = amount of blood ejected from the ventricle with each heart beat • HR (per minute) • CO = SV x HR
Factors affecting Stroke Volume • Preload – volume of blood in the ventricles at the end of diastole (before the next contraction) • Contractility – Force by which ventricles contract • Afterload – Peripheral resistance against which the left ventricle pumps Cardiac Reserve – heart responds to numerous situations/ demands in health and illness (ex: exercise, stress, hypovolemia)
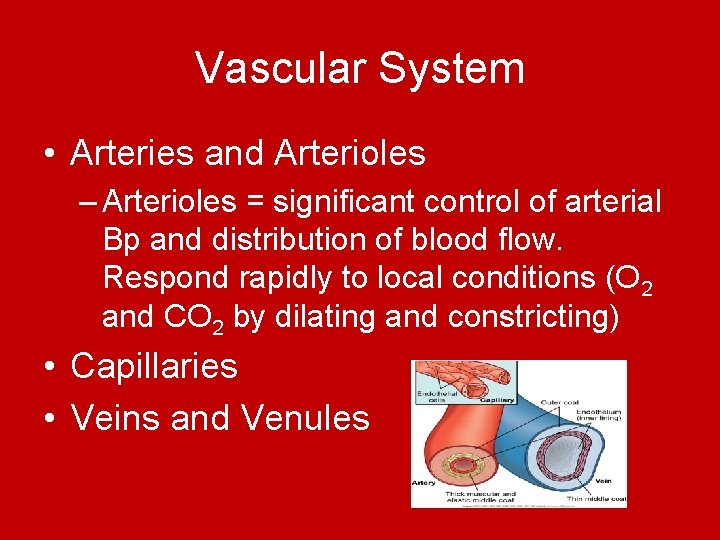
Vascular System • Arteries and Arterioles – Arterioles = significant control of arterial Bp and distribution of blood flow. Respond rapidly to local conditions (O 2 and CO 2 by dilating and constricting) • Capillaries • Veins and Venules
Regulation of the Cardiovascular System • Autonomic Nervous System – Stimulation of sympathetic nervous system ↑ HR, ↑ speed of impulse conduction through the AV node, ↑ force of atrial and ventricular contractions = mediated by specific sites in the heart β – adrenergic receptors (receptors for epinephrine and norepinephrine) α- adrenergic receptors (vasoconstriction)
Regulation of the Cardiovascular System • Parasympathetic Nervous System – Mediated by vagus nerve – Slows the HR by decreasing the impulses from the SA node and thus conduction through the AV node – Parasympathetic nerves have selective distribuion in the blood vessels
• Baroreceptors – in aortic arch and carotid sinus are sensitive to stretch or pressure with the aterial system – Stimulation (volume overload) results in temporary inhibition of sympathetic nervous system and enhancement of parasympathetic influence = ↓ HR and peripheral vasodilation
• Chemoreceptors – located in aortic arch, carotid bodies – Cause changes in RR, BP in response to increased arterial CO 2 pressure and p. H and arterial O 2 pressure – When triggered in the medulla = stimulate vasomotor center to increase BP
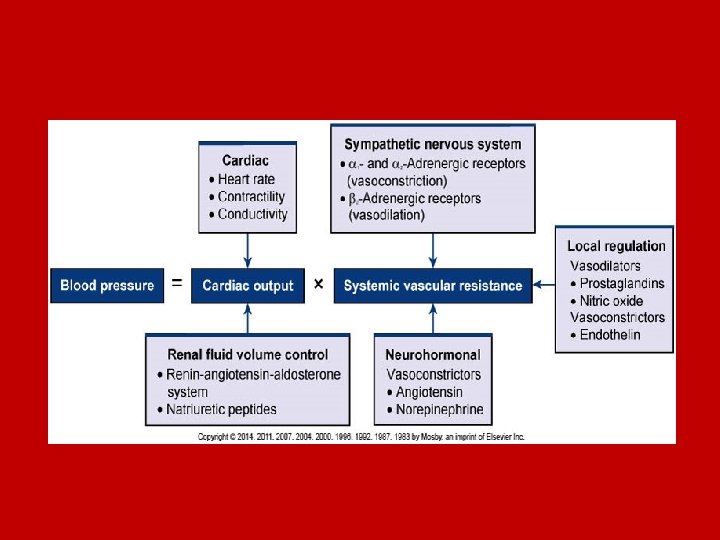
Blood Pressure • Systolic BP – peak pressure exerted by blood against the walls of the arterial system • Diastolic BP – residual pressure in the arterial system during ventricular relaxation (filling) • 2 main factors affecting BP = CO and SVR (systemic vascular resistance) BP = CO x SVR
Pulse Pressure • Pulse pressure = difference between SBP and DBP – Normally about 1/3 of the SBP ↑ pulse pressure = occurs during exercise, those with atherosclerosis of larger arteries
Mean Arterial Pressure (MAP) • Average pressure within the arterial system that is felt by organs in the body ** Not simply the average between SBP and DBP because the length of the diastolic phase is twice as long as the systolic phase • MAP = (SBP + DBP x 2)/ 3 • A MAP > 60 mm. Hg is needed to adequately perfuse and sustain vital organs.
Gerontologic Considerations: Cardiovascular System • • • ↑ collagen and ↓ elastin ↓ response to physical and emotional stress Thicker and stiffer cardiac valves Pacemaker cells in SA node decreases Number and function of β–adrenergic receptors decrease • Arterial and venous blood vessels thicken and become less elastic • Orthostatic hypotension
Hypertension (HTN) • High blood pressure • Direct relationship between HTN and cardiovascular disease • Before age 45 more common in men, after age 65 more common in women (partially attributed to menopause-related factors • African Americans have the highest prevalence of HTN in the world
Normal Regulation of BP • BP is the force exerted by the blood against the walls of the blood vessel – must be adequate to maintain perfusion • CO = SV x HR • Mechanisms that regulate BP affect either CO or SVR (systemic vascular resistance) • Short and long term mechanisms to regulate BP
Sympathetic Nervous System • Increased SNS activity: – ↑ HR – ↑ Cardiac Contractility – Widespread vasoconstriction in the peripheral arterioles – Promotes release of renin from the kidneys BP ↑ secondary to ↑ both CO and SVR
Sympathetic Nervous System • Sympathetic vasomotor center interacts with many areas of the brain to maintain normal BP under various conditions • Causes appropriate increase in CO and BP to adjust to the body’s ↑ O 2 demands – Pain, stress, exercise, postural change (from lying to standing)
Renal System • Kidneys affect BP by controlling Na excretion and extracellular fluid volume – ↑ Blood volume – ↑ volume return to heart thus ↑ stroke volume = ↑ CO and ↑ BP
Renin-angiotensin-aldosterone system • Renin converts angiotensin I to angiotensin II • Angiotensin II ↑ BP through vasoconstriction and stimulates secretion of aldosterone • Aldosterone stimulates kidneys to retain Na and H 2 O = ↑ blood volume and CO
Classification of Hypertension • HTN = persistent SBP >140, DBP >90, or current use of antihypertensive medication • Prehypertension = SBP 120 - 139, or DBP 80 - 89
• Primary HTN – Elevated BP without identified cause (90 -95%) • Secondary HTN – Elevated BP with a specific cause (5 -10%) – Cirrhosis, congenital narrowing of the aorta, drug related (estrogen, oral contraceptives, NSAIDS), endocrine disorders (thyroid disease), neurologic disorders (brain injury), pregnancy induced, renal disorder – Treatment = treat underlying cause
Complications of HTN • • Coronary Artery Disease Left Ventricular Hypertrophy Heart Failure Cerebrovascular disease (Atherosclerosis and plaque = Stroke) • Peripheral vascular disease (circulation), aortic dissection • Nephrosclerosis – narrowing of renal blood vessels = kidney damage • Retinal damage
Risk Factors for Primary Hypertension – Table 33 -4, p. 713 • Age (SBP rises progressively with age) • Alcohol • Diabetes Mellitus • Elevated Serum Lipids • Excess dietary sodium • Gender (Men in young and middle adulthood, women >65) • Family history • Obesity • Ethnicity (African American) • Sedentary lifestyle • Socioeconomic status • Stress
Lifestyle Modifications • • Weight Reduction Dietary approaches (DASH eating plan) Dietary Sodium Reduction Moderation of alcohol consumption Regular physical activity No tobacco Management of psychosocial risk factors (socioeconomic status, social isolation and lack of support, stress at work and in family life and negative emotions – depression and hostility)
DASH Eating Plan • Fruits • Vegetables • Fat-free or lowfat milk and milk products • Whole grains • Fish • Poultry • Beans, seeds and nuts
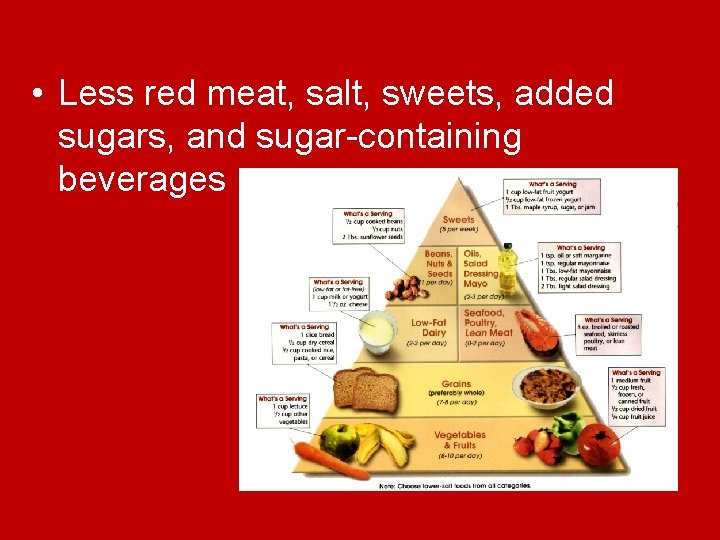
• Less red meat, salt, sweets, added sugars, and sugar-containing beverages
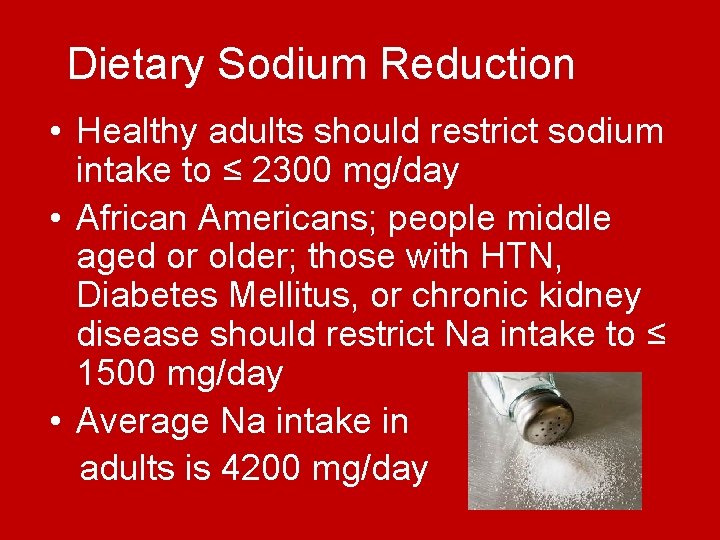
Dietary Sodium Reduction • Healthy adults should restrict sodium intake to ≤ 2300 mg/day • African Americans; people middle aged or older; those with HTN, Diabetes Mellitus, or chronic kidney disease should restrict Na intake to ≤ 1500 mg/day • Average Na intake in adults is 4200 mg/day
Dietary Sodium Reduction • Teach patients to Read labels of over the counter drugs, packaged foods, and health products to look for hidden Na • What are some foods high in Na? – Processed foods, canned products, chips, crackers, luncheon meats, cheese, soda, restaurant food, ketchup, table added salt

Physical Activity Recommendations
Drug Therapy Actions 1. Decrease the volume of circulating blood 2. Reduce Systemic Vascular Resistance Combination therapy for HTN = very effective
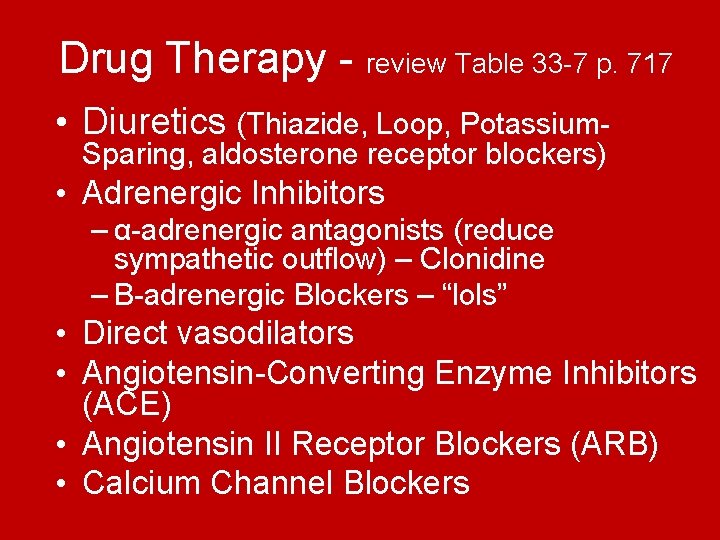
Drug Therapy - review Table 33 -7 p. 717 • Diuretics (Thiazide, Loop, Potassium. Sparing, aldosterone receptor blockers) • Adrenergic Inhibitors – α-adrenergic antagonists (reduce sympathetic outflow) – Clonidine – Β-adrenergic Blockers – “lols” • Direct vasodilators • Angiotensin-Converting Enzyme Inhibitors (ACE) • Angiotensin II Receptor Blockers (ARB) • Calcium Channel Blockers
Drug therapy Common side effects: • Orthostatic hypotension • Sexual problems or ↓ libido = may cause decreased adherence to regimen • Diuretics = frequent voiding • Dry mouth • Side effects of vasodilators and adrenergic inhibitors decrease if taken at night • 24 hour duration drugs should be taken first thing in the morning
Hypertensive Crisis • Hypertensive emergency = BP severely elevated (220/140) – Can cause encephalopathy (headache, nausea, vomiting seizures, coma), intracranial or subarachnoid hemorrhage, acute left ventricular failure, MI, renal failure, dissecting aortic aneurysm, and retinopathy
Hypertensive Crisis • Hypertensive urgency = Develops over days to weeks (180/110 mm. Hg) – Rate of rise of BP is more important than the absolute value (people with chronic HTN can tolerate higher BP)
Hypertensive Crisis • Hospitalization for hypertensive emergencies – Administration of IV antihypertensive medications – have rapid onset Continual monitoring of cardiac and circulatory systems Measure urine output hourly
- Slides: 40