The Cardiovascular System Ch 13 Vessels Artery Strong




- Slides: 45
The Cardiovascular System Ch. 13
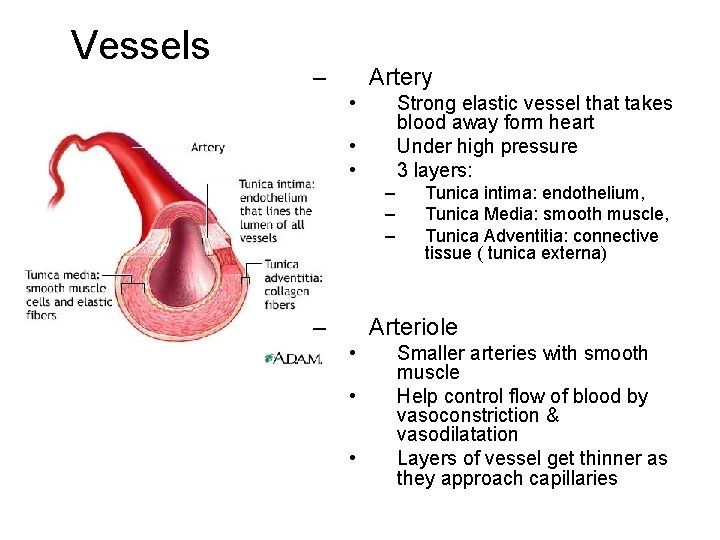
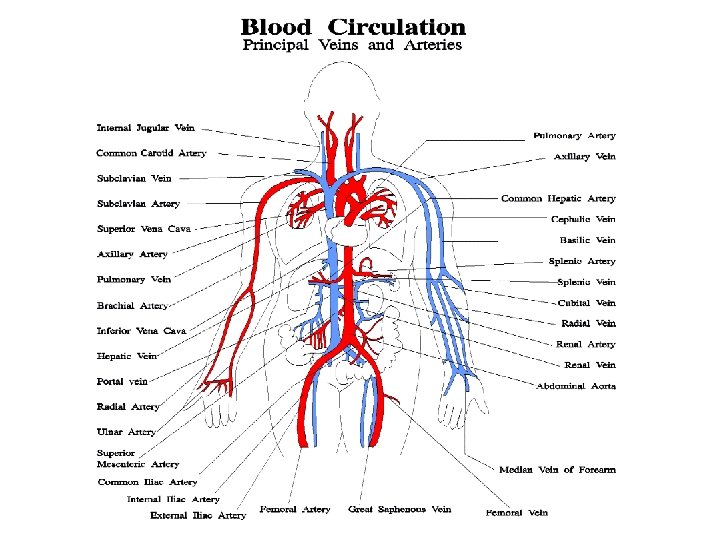
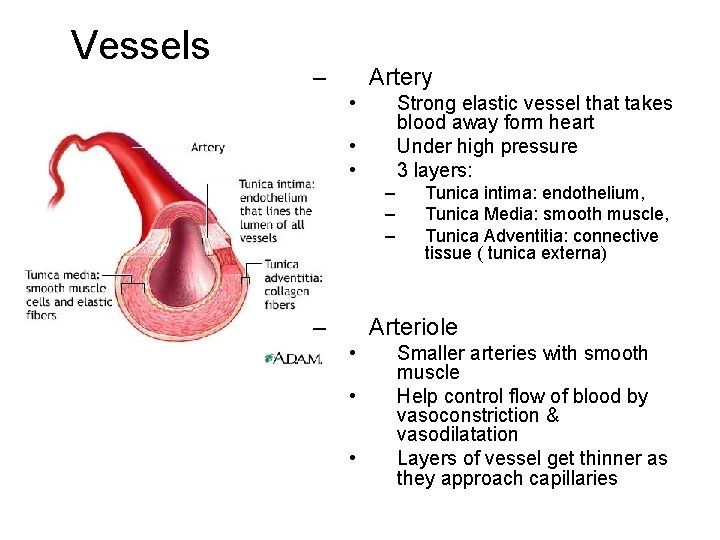
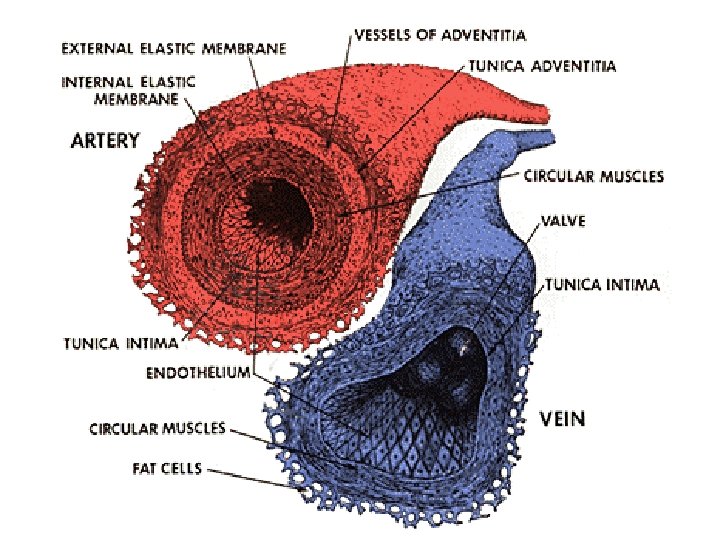
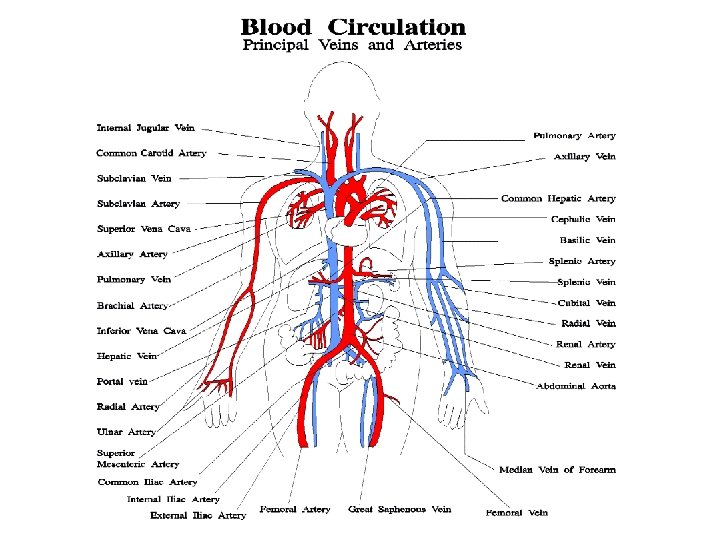
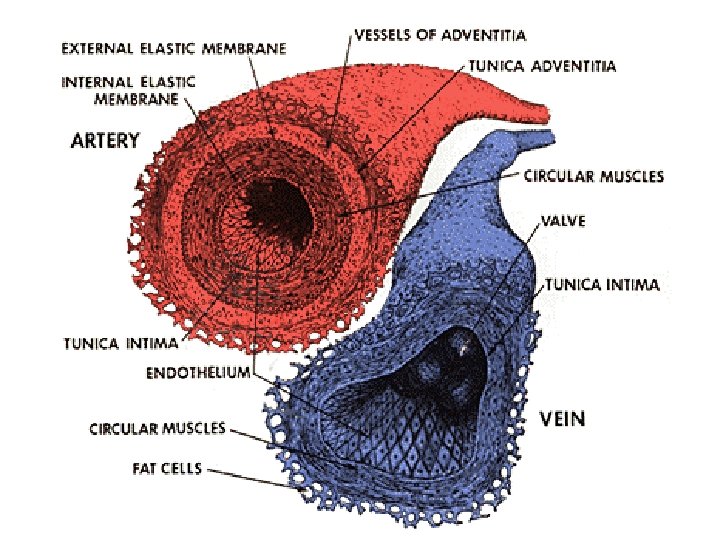
Vessels – Artery • Strong elastic vessel that takes blood away form heart Under high pressure 3 layers: • • – – Tunica intima: endothelium, Tunica Media: smooth muscle, Tunica Adventitia: connective tissue ( tunica externa) Arteriole • • • Smaller arteries with smooth muscle Help control flow of blood by vasoconstriction & vasodilatation Layers of vessel get thinner as they approach capillaries
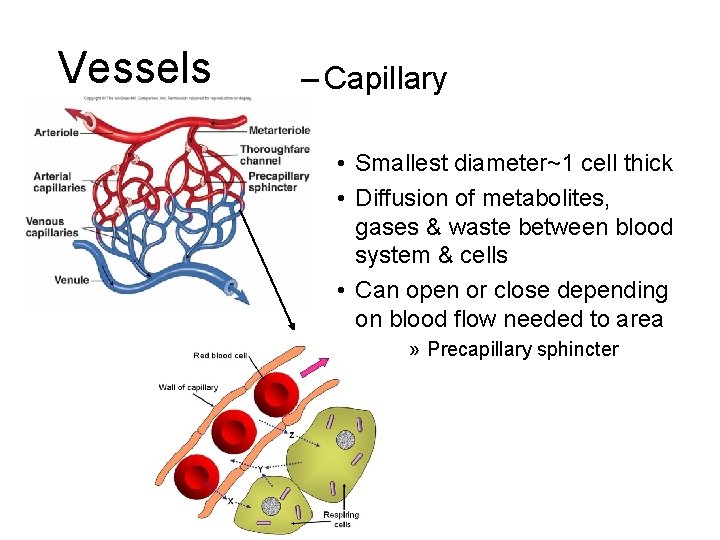
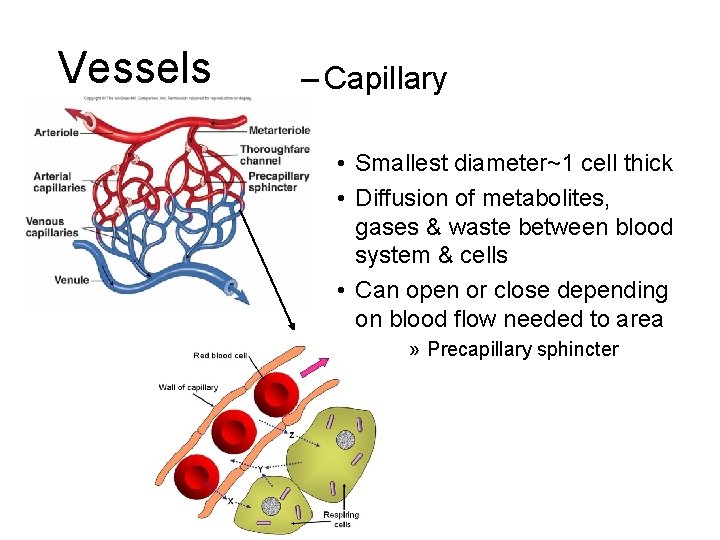
Vessels – Capillary • Smallest diameter~1 cell thick • Diffusion of metabolites, gases & waste between blood system & cells • Can open or close depending on blood flow needed to area » Precapillary sphincter
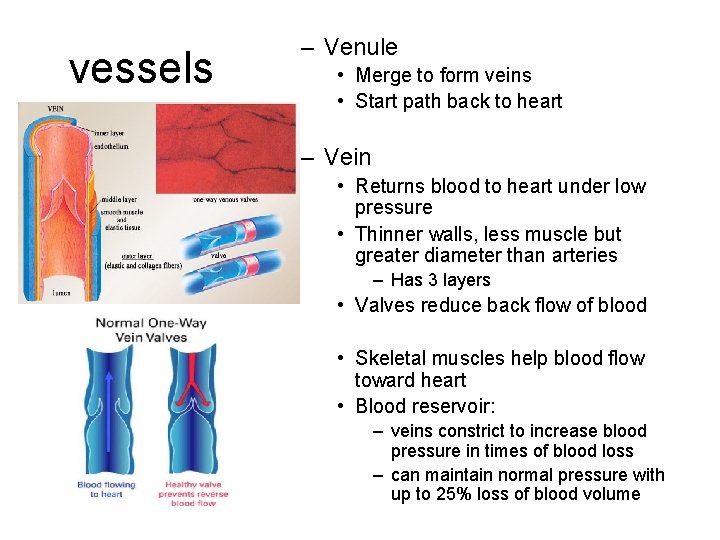
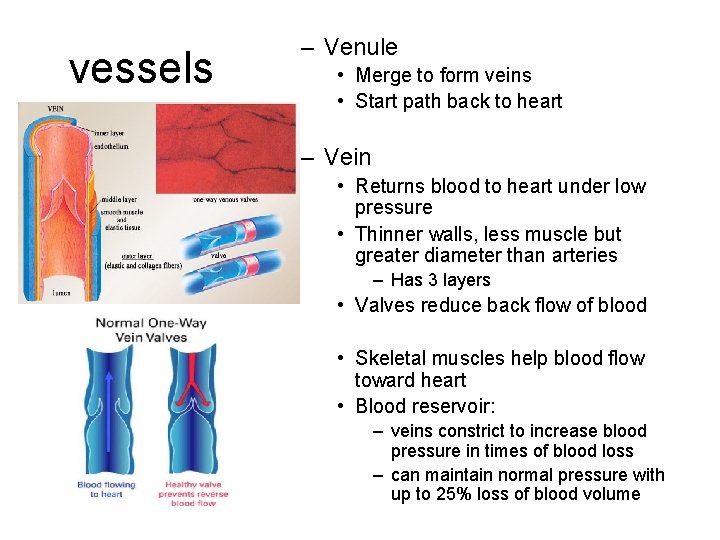
vessels – Venule • Merge to form veins • Start path back to heart – Vein • Returns blood to heart under low pressure • Thinner walls, less muscle but greater diameter than arteries – Has 3 layers • Valves reduce back flow of blood • Skeletal muscles help blood flow toward heart • Blood reservoir: – veins constrict to increase blood pressure in times of blood loss – can maintain normal pressure with up to 25% loss of blood volume
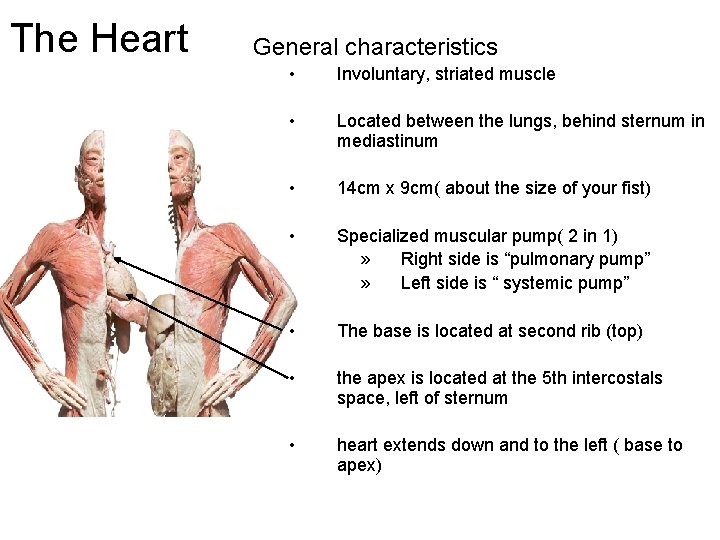
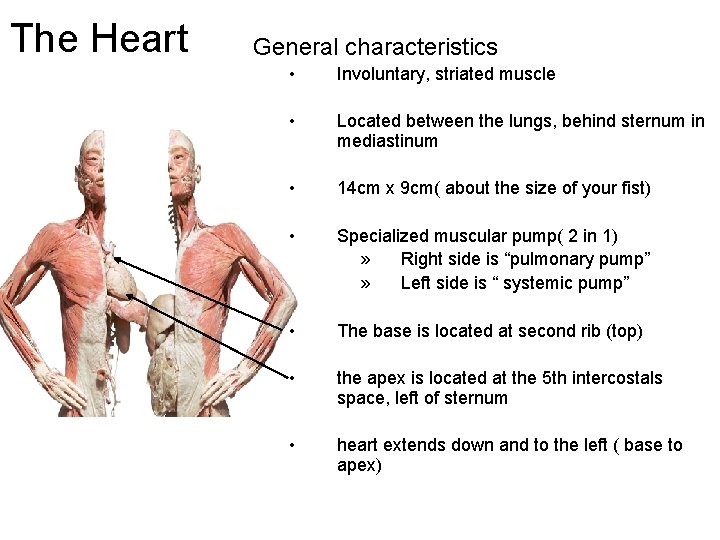
The Heart General characteristics • Involuntary, striated muscle • Located between the lungs, behind sternum in mediastinum • 14 cm x 9 cm( about the size of your fist) • Specialized muscular pump( 2 in 1) » Right side is “pulmonary pump” » Left side is “ systemic pump” • The base is located at second rib (top) • the apex is located at the 5 th intercostals space, left of sternum • heart extends down and to the left ( base to apex)
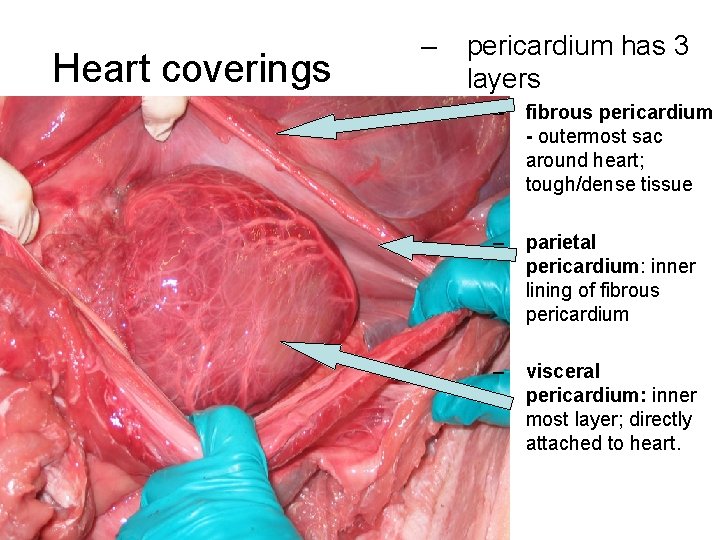
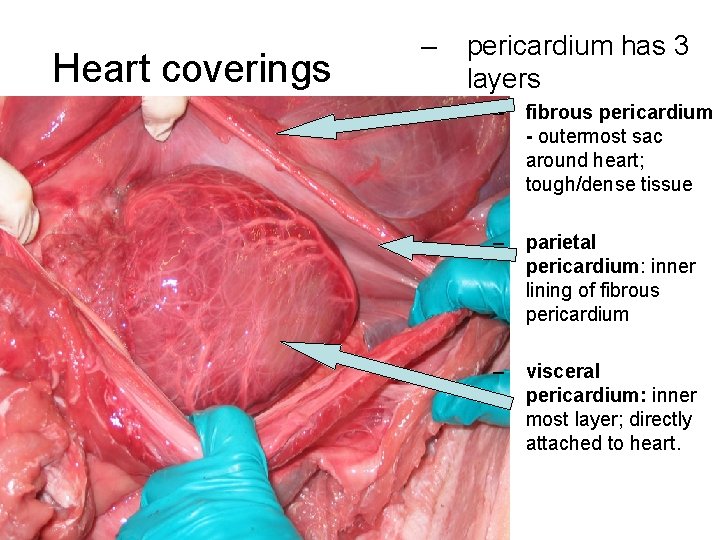
Heart coverings – pericardium has 3 layers – fibrous pericardium - outermost sac around heart; tough/dense tissue – parietal pericardium: inner lining of fibrous pericardium – visceral pericardium: inner most layer; directly attached to heart.
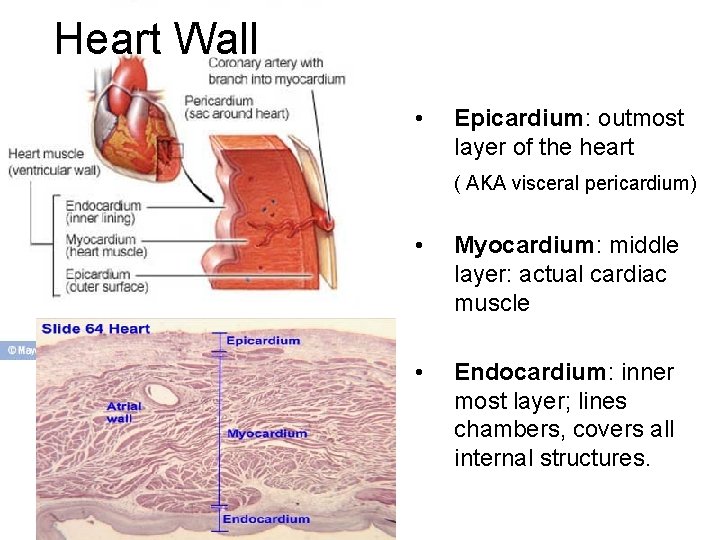
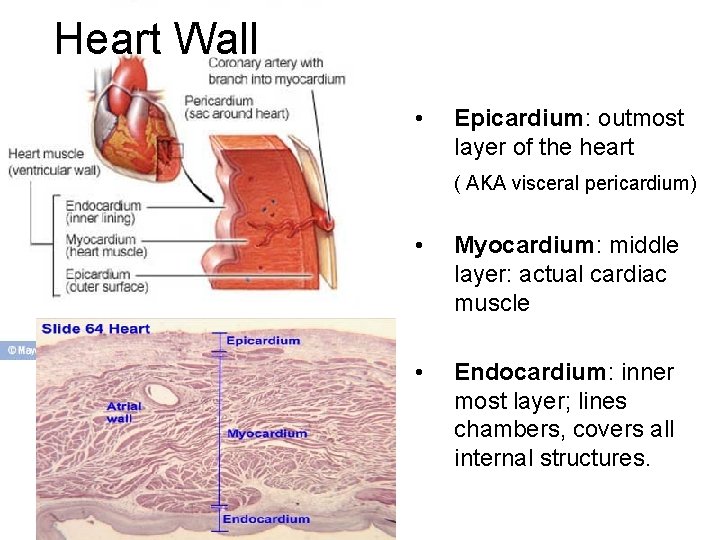
Heart Wall • Epicardium: outmost layer of the heart ( AKA visceral pericardium) • Myocardium: middle layer: actual cardiac muscle • Endocardium: inner most layer; lines chambers, covers all internal structures.
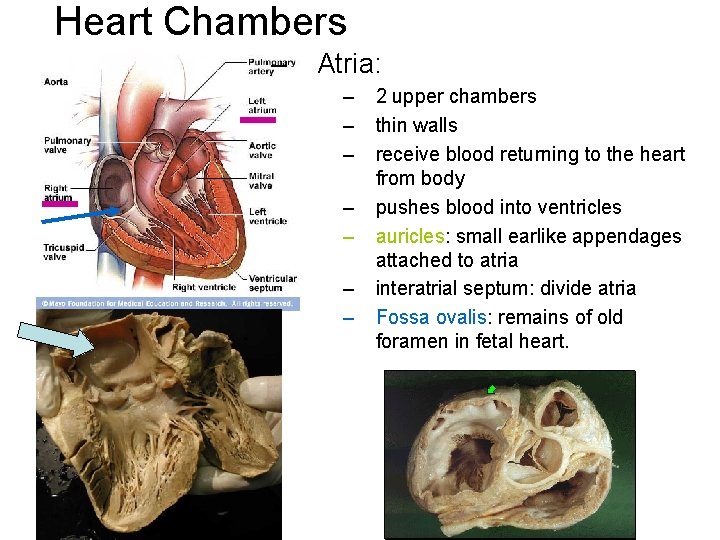
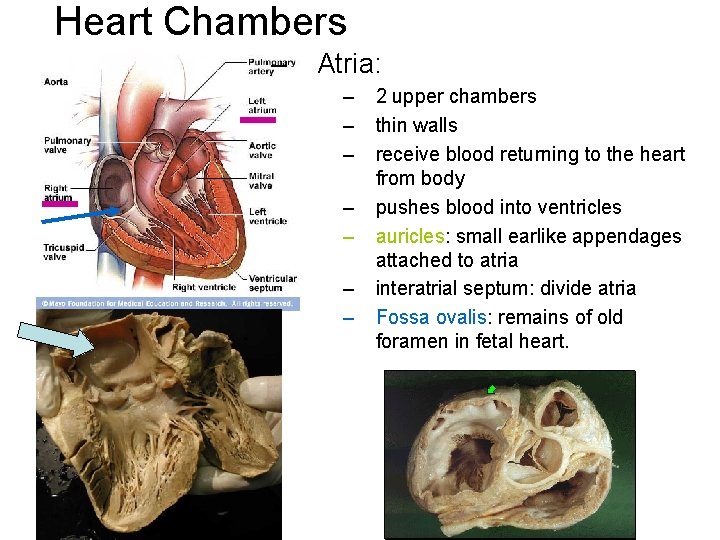
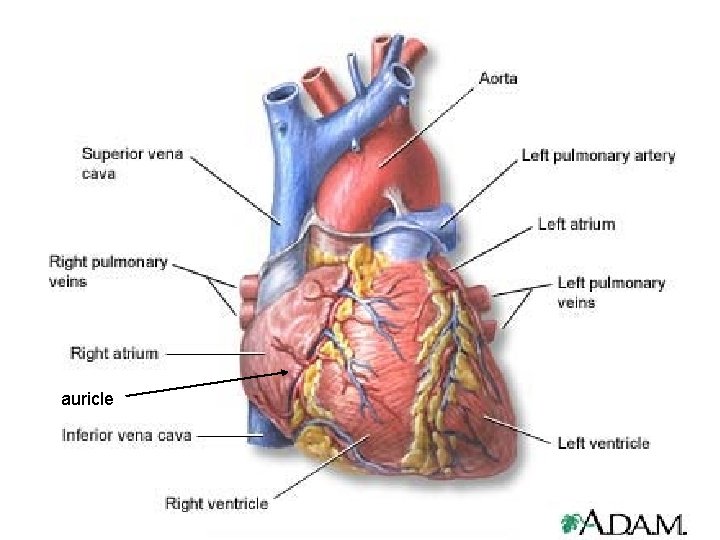
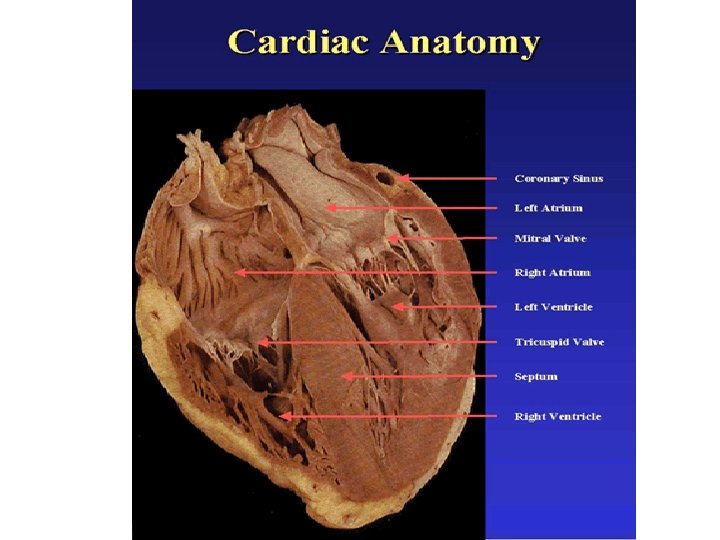
Heart Chambers – Atria: – – – – 2 upper chambers thin walls receive blood returning to the heart from body pushes blood into ventricles auricles: small earlike appendages attached to atria interatrial septum: divide atria Fossa ovalis: remains of old foramen in fetal heart.
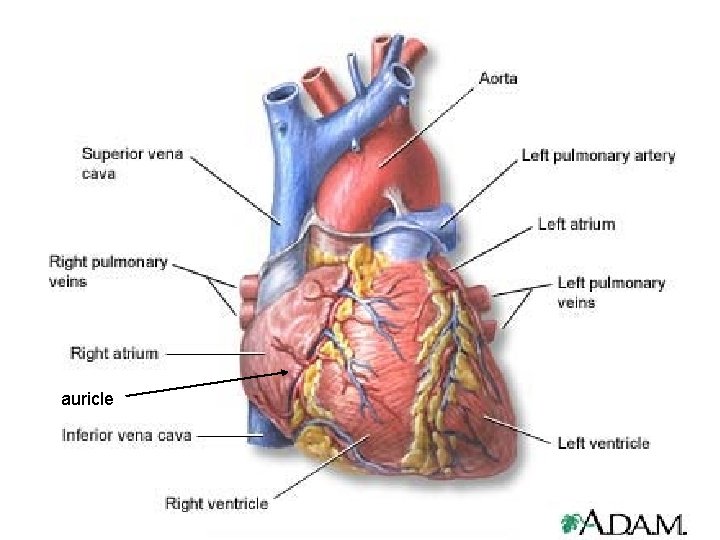
auricle
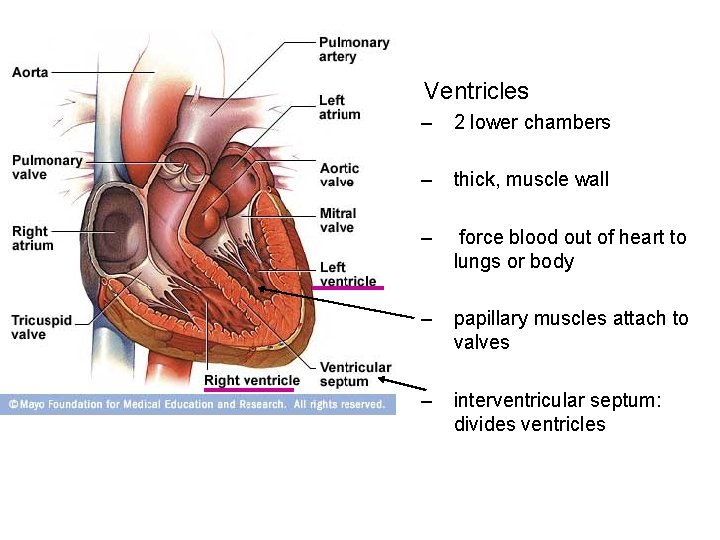
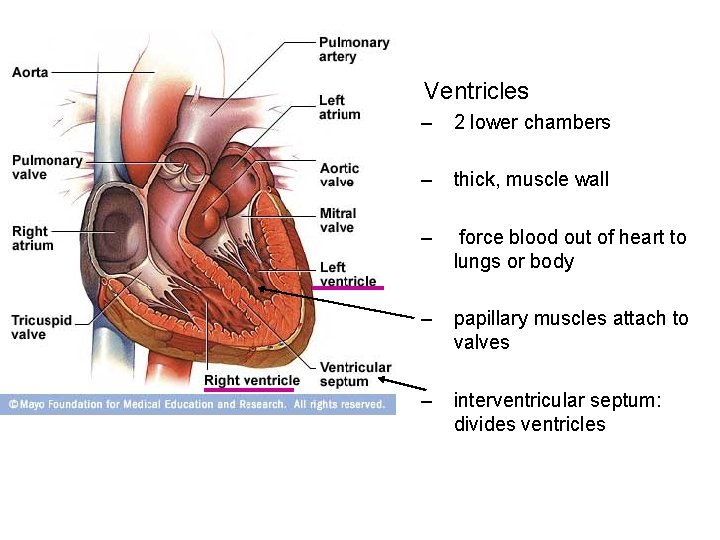
• Ventricles – 2 lower chambers – thick, muscle wall – force blood out of heart to lungs or body – papillary muscles attach to valves – interventricular septum: divides ventricles
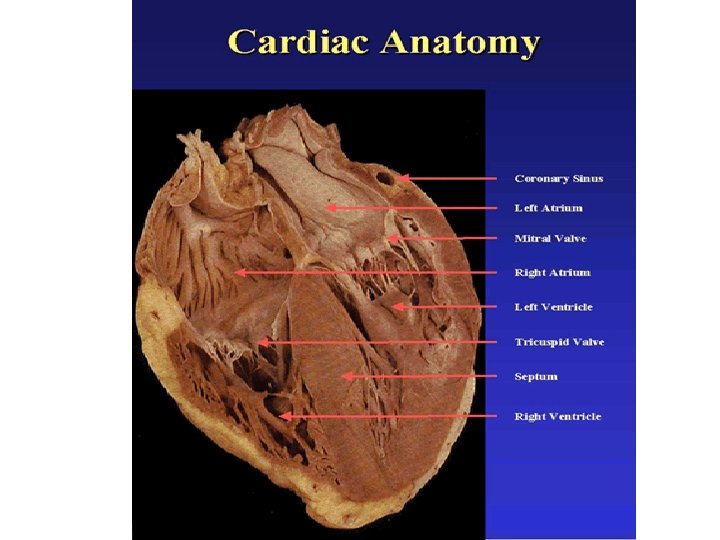
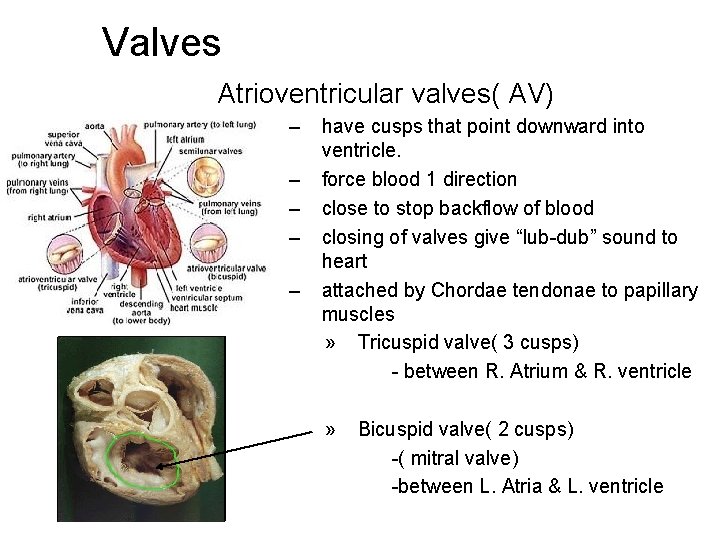
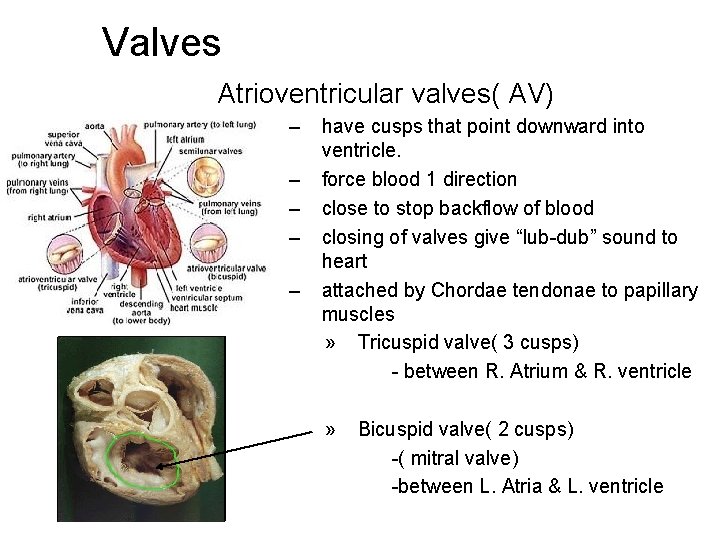
Valves Atrioventricular valves( AV) – – – have cusps that point downward into ventricle. force blood 1 direction close to stop backflow of blood closing of valves give “lub-dub” sound to heart attached by Chordae tendonae to papillary muscles » Tricuspid valve( 3 cusps) - between R. Atrium & R. ventricle » Bicuspid valve( 2 cusps) -( mitral valve) -between L. Atria & L. ventricle
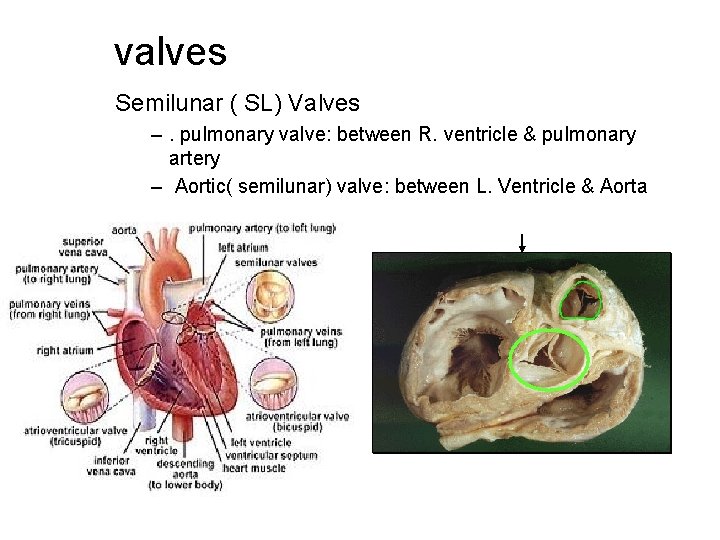
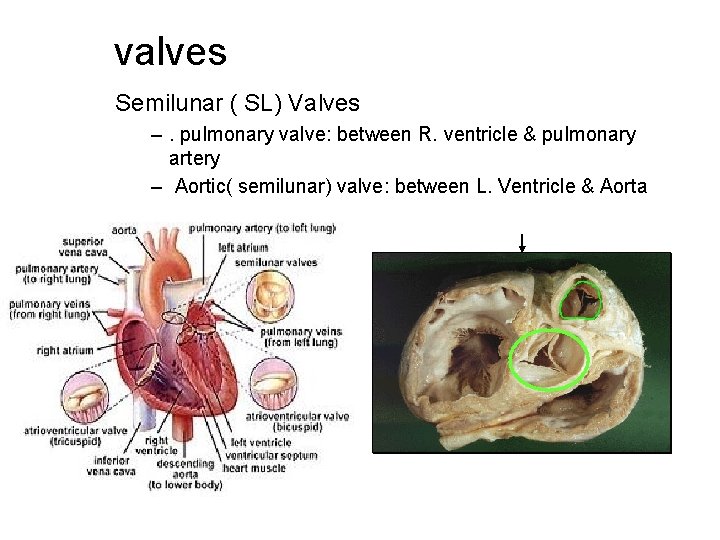
valves Semilunar ( SL) Valves –. pulmonary valve: between R. ventricle & pulmonary artery – Aortic( semilunar) valve: between L. Ventricle & Aorta
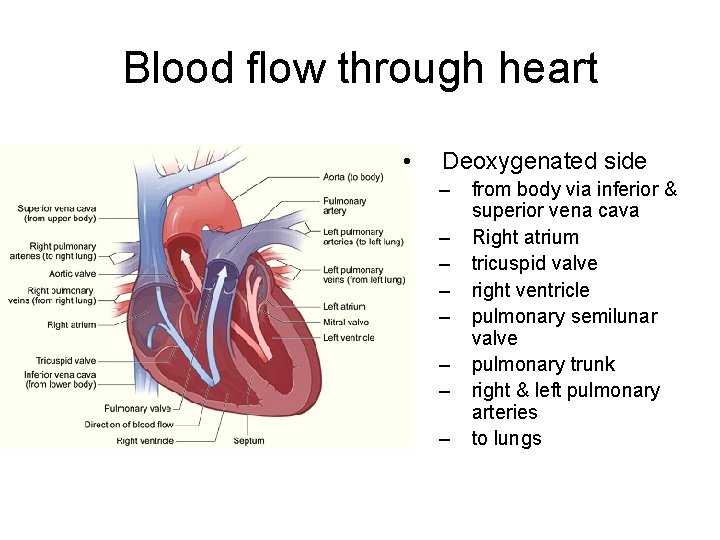
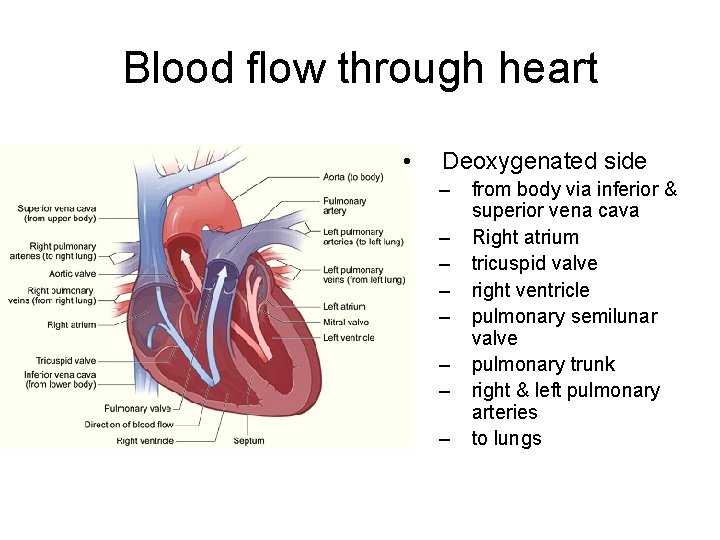
Blood flow through heart • Deoxygenated side – – – – from body via inferior & superior vena cava Right atrium tricuspid valve right ventricle pulmonary semilunar valve pulmonary trunk right & left pulmonary arteries to lungs
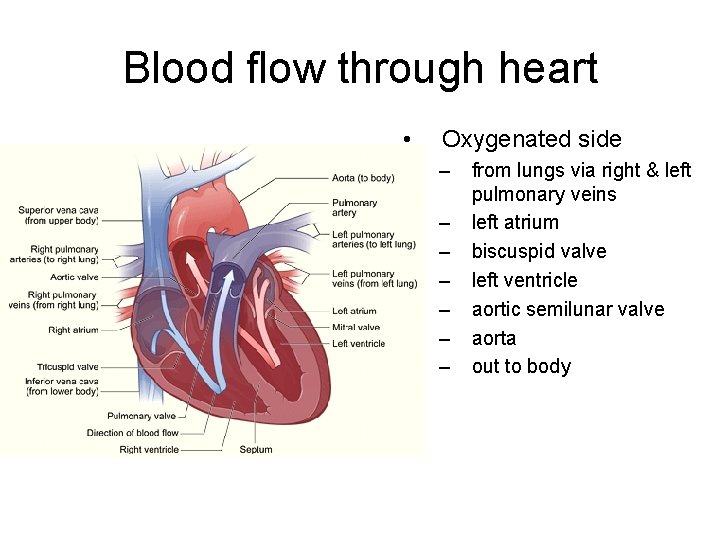
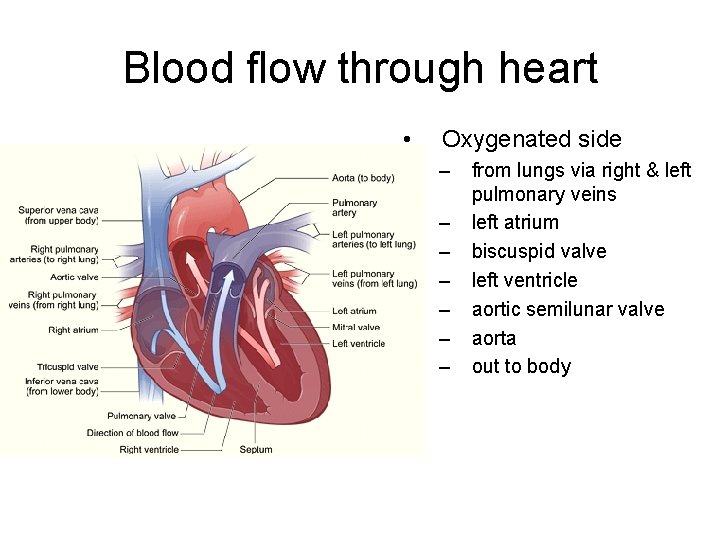
Blood flow through heart • Oxygenated side – – – – from lungs via right & left pulmonary veins left atrium biscuspid valve left ventricle aortic semilunar valve aorta out to body

Queue up the music • http: //www. youtube. com/watch? v=D 8 LK 34 ho. Vp. U • http: //www. youtube. com/watch? v=j. Cpha 8 Z -vjw • http: //www. youtube. com/watch? v=OMXxv e. Zgx 0 M


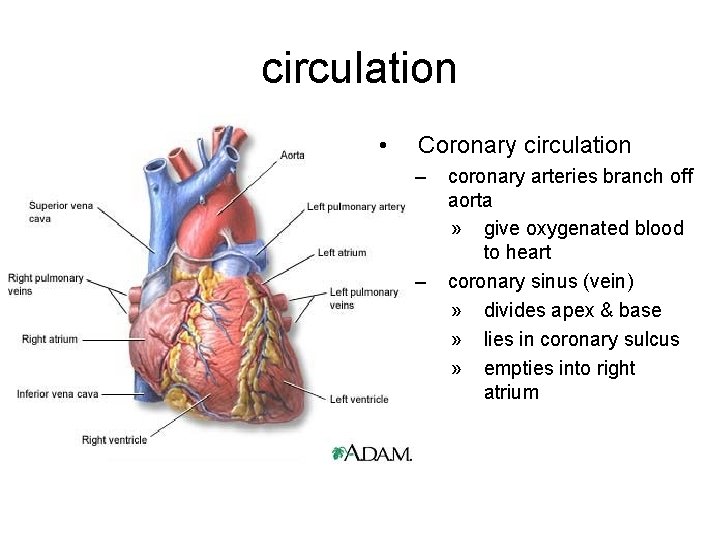
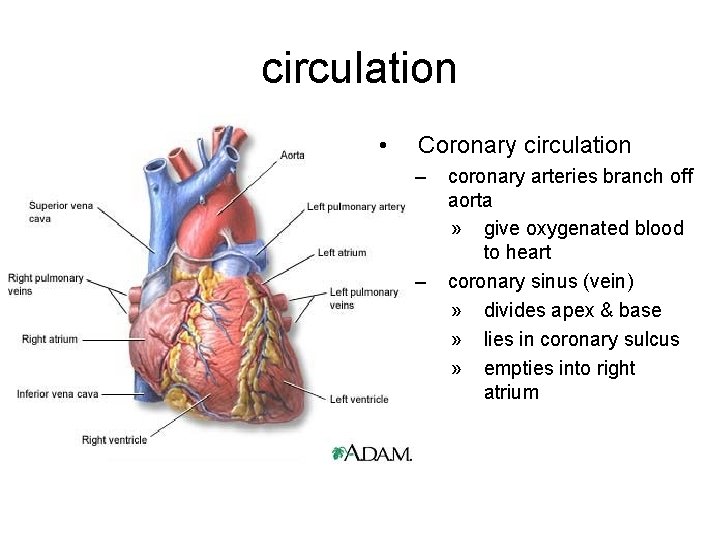
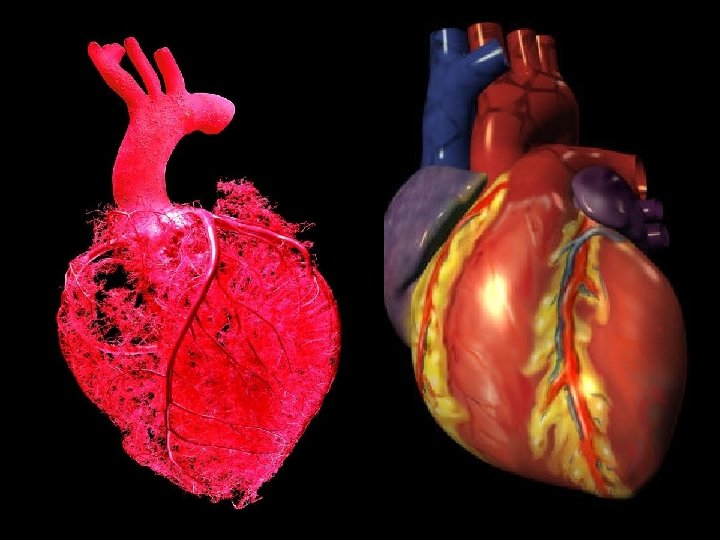
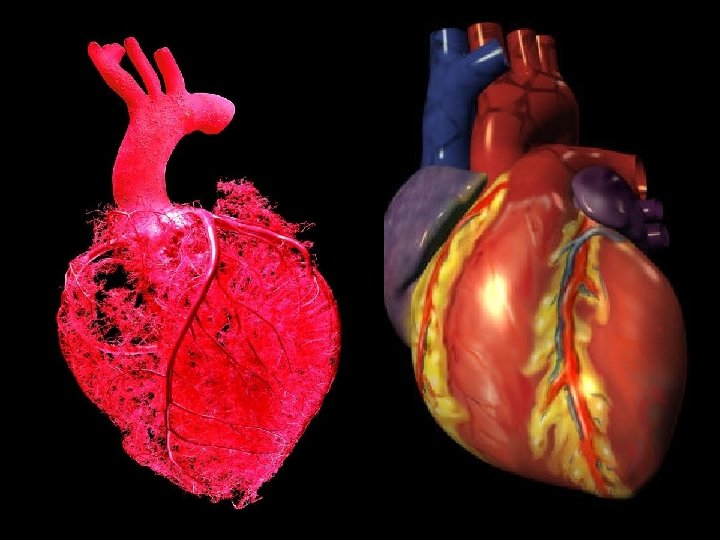
circulation • Coronary circulation – – coronary arteries branch off aorta » give oxygenated blood to heart coronary sinus (vein) » divides apex & base » lies in coronary sulcus » empties into right atrium
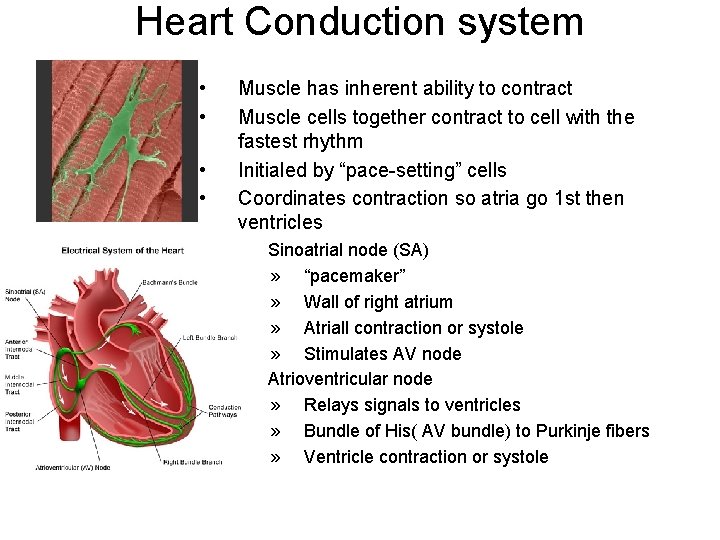
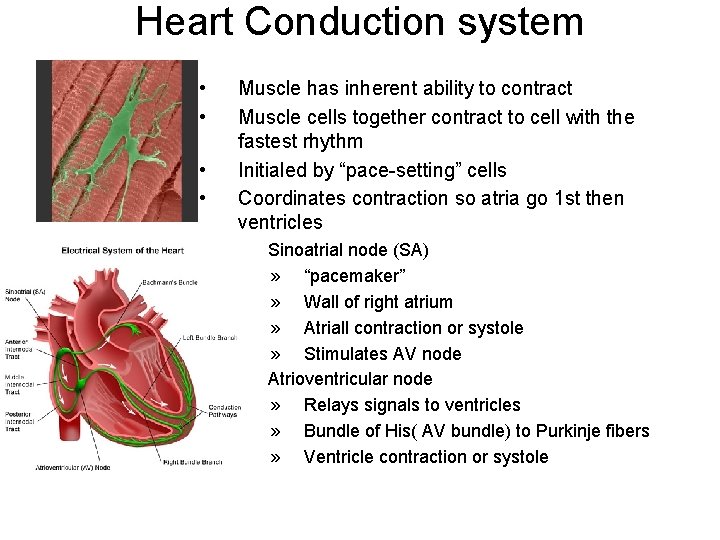
Heart Conduction system • • Muscle has inherent ability to contract Muscle cells together contract to cell with the fastest rhythm Initialed by “pace-setting” cells Coordinates contraction so atria go 1 st then ventricles – – Sinoatrial node (SA) » “pacemaker” » Wall of right atrium » Atriall contraction or systole » Stimulates AV node Atrioventricular node » Relays signals to ventricles » Bundle of His( AV bundle) to Purkinje fibers » Ventricle contraction or systole
Conducting System of the Heart
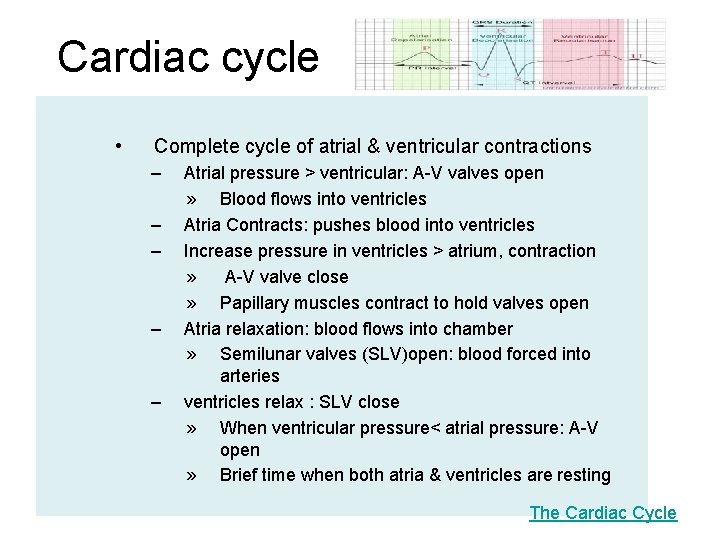
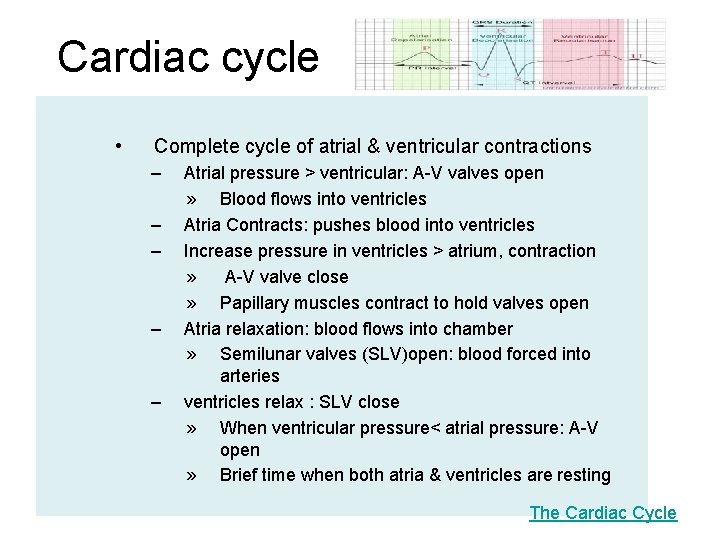
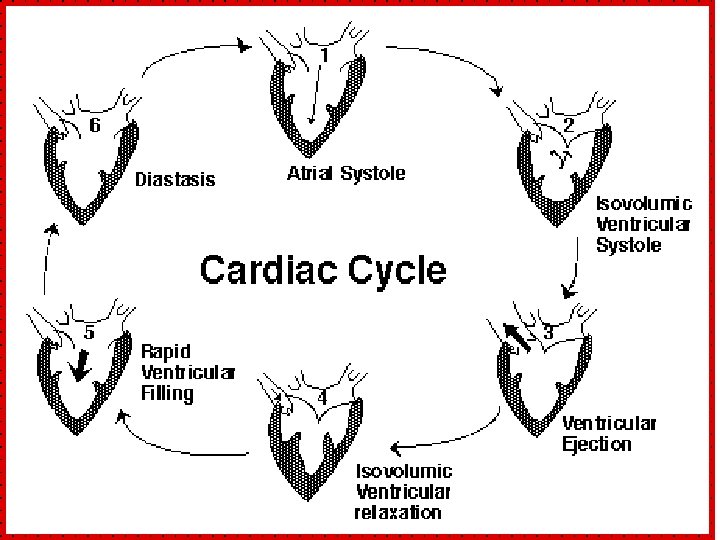
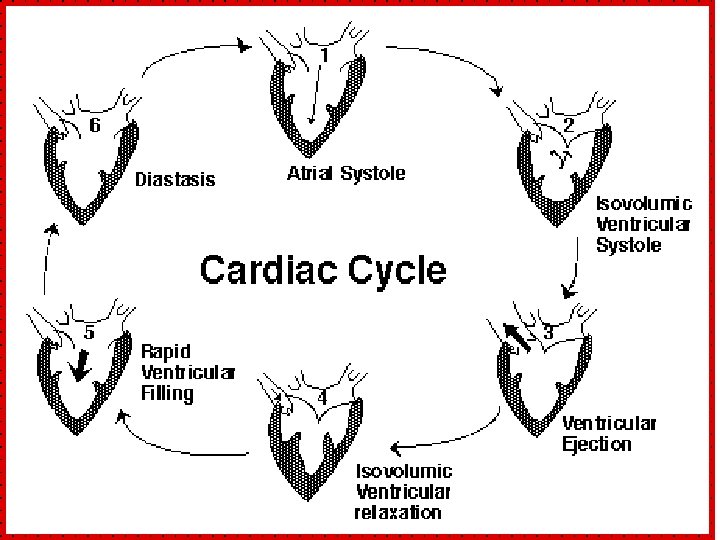
Cardiac cycle • Complete cycle of atrial & ventricular contractions – – – Atrial pressure > ventricular: A-V valves open » Blood flows into ventricles Atria Contracts: pushes blood into ventricles Increase pressure in ventricles > atrium, contraction » A-V valve close » Papillary muscles contract to hold valves open Atria relaxation: blood flows into chamber » Semilunar valves (SLV)open: blood forced into arteries ventricles relax : SLV close » When ventricular pressure< atrial pressure: A-V open » Brief time when both atria & ventricles are resting The Cardiac Cycle
Cardiac cycle http: //www. youtube. com/watch? v=rguzt. Y 8 aqpk
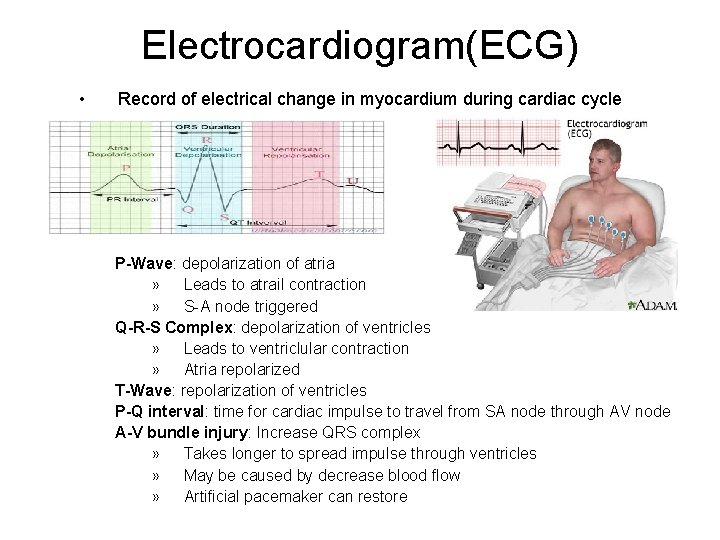
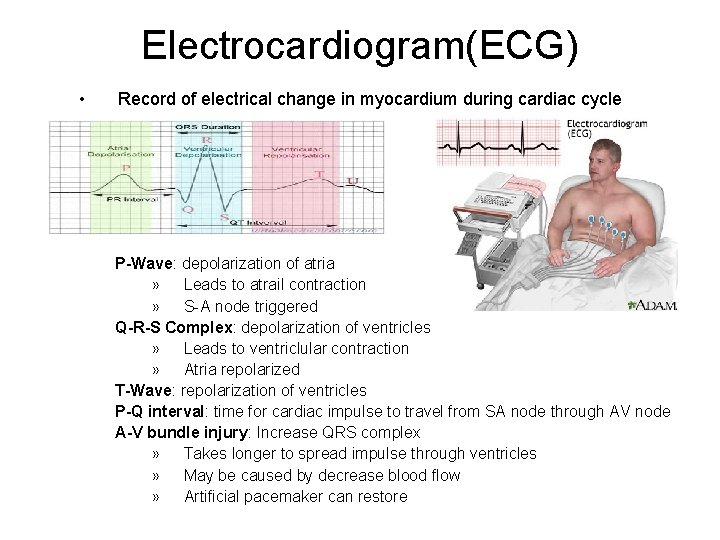
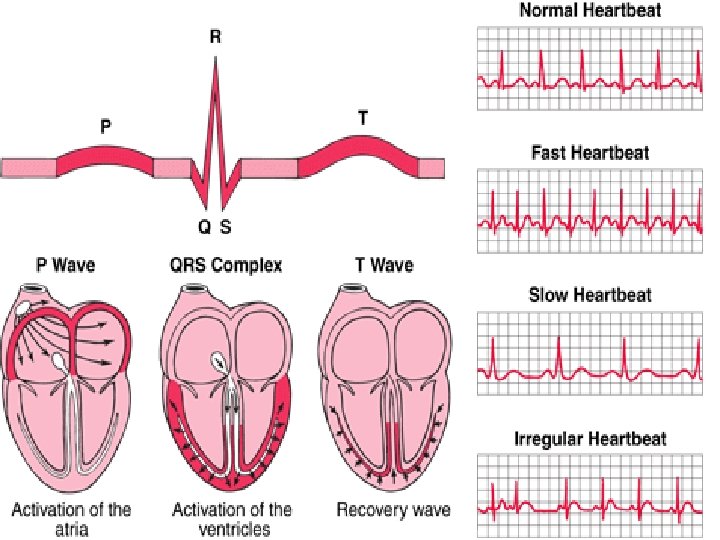
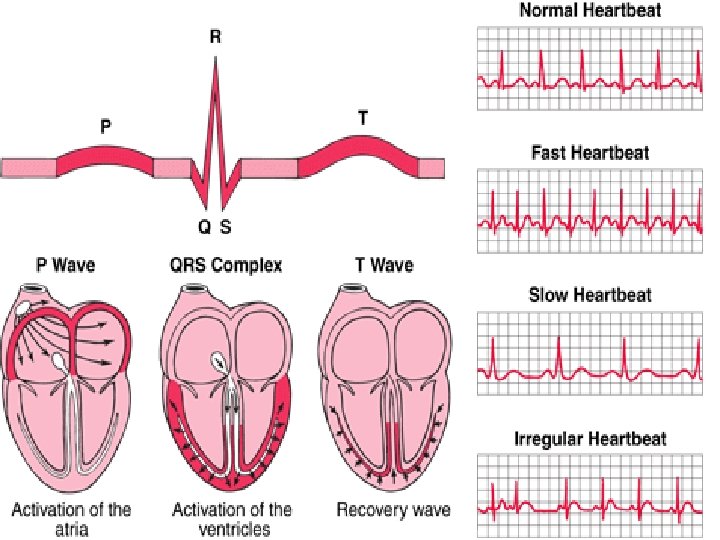
Electrocardiogram(ECG) • Record of electrical change in myocardium during cardiac cycle P-Wave: depolarization of atria » Leads to atrail contraction » S-A node triggered Q-R-S Complex: depolarization of ventricles » Leads to ventriclular contraction » Atria repolarized T-Wave: repolarization of ventricles P-Q interval: time for cardiac impulse to travel from SA node through AV node A-V bundle injury: Increase QRS complex » Takes longer to spread impulse through ventricles » May be caused by decrease blood flow » Artificial pacemaker can restore
ECG • http: //www. youtube. com/watch? v=n. K 0_28 q 6 Wo. M
Heart Sounds • Lubb-Dupp – – Lubb- ventricular contraction; A-V valves close » 5 th intercostals space @ nipple line » Left side=bicuspid » Right side= tricuspid Dupp- Ventricular relaxation; SL Valves close » 2 nd intercostals space
Heart Action • Cardiac output (CO): blood pushed / minute ~5, 250 ml/min or 5. 25 L/min. • Stroke Volume (SV): how much blood pushed /beat ~70 ml/min • Heart rate( HR): how fast heart beats/min ~ 75 bpm – – CO = SV x HR Starling’s law of the heart: explains how CO changes with levels of exercise & blood flow
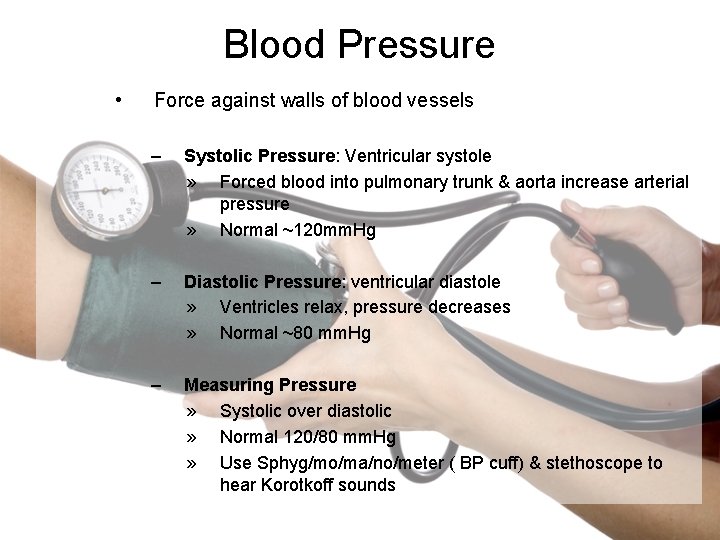
Blood Pressure • Force against walls of blood vessels – Systolic Pressure: Ventricular systole » Forced blood into pulmonary trunk & aorta increase arterial pressure » Normal ~120 mm. Hg – Diastolic Pressure: ventricular diastole » Ventricles relax, pressure decreases » Normal ~80 mm. Hg – Measuring Pressure » Systolic over diastolic » Normal 120/80 mm. Hg » Use Sphyg/mo/ma/no/meter ( BP cuff) & stethoscope to hear Korotkoff sounds

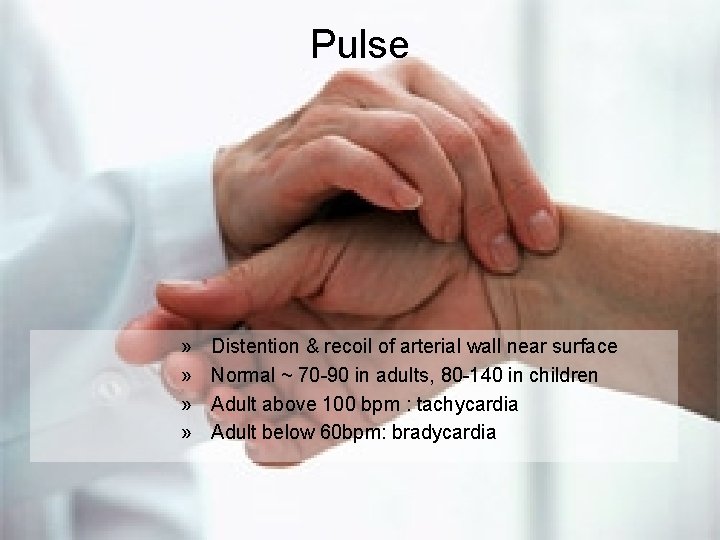
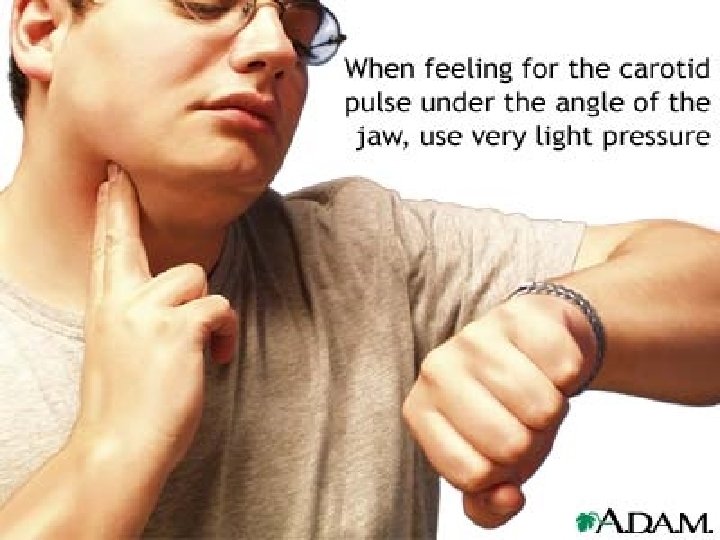
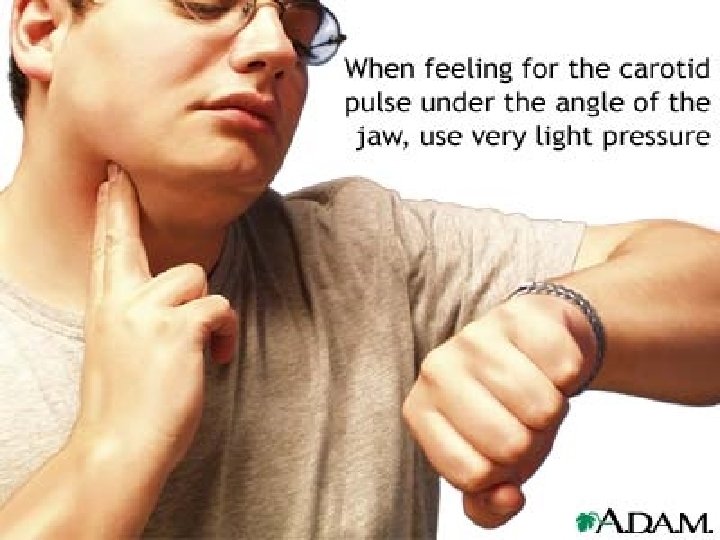
Pulse » » Distention & recoil of arterial wall near surface Normal ~ 70 -90 in adults, 80 -140 in children Adult above 100 bpm : tachycardia Adult below 60 bpm: bradycardia
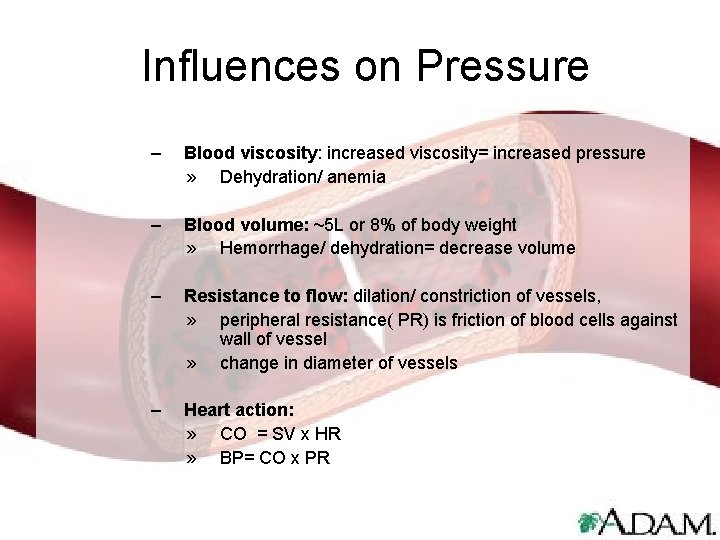
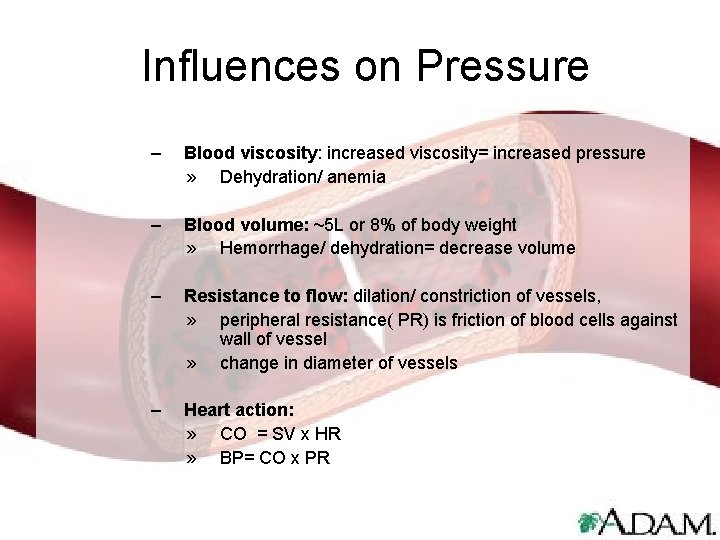
Influences on Pressure – Blood viscosity: increased viscosity= increased pressure » Dehydration/ anemia – Blood volume: ~5 L or 8% of body weight » Hemorrhage/ dehydration= decrease volume – Resistance to flow: dilation/ constriction of vessels, » peripheral resistance( PR) is friction of blood cells against wall of vessel » change in diameter of vessels – Heart action: » CO = SV x HR » BP= CO x PR
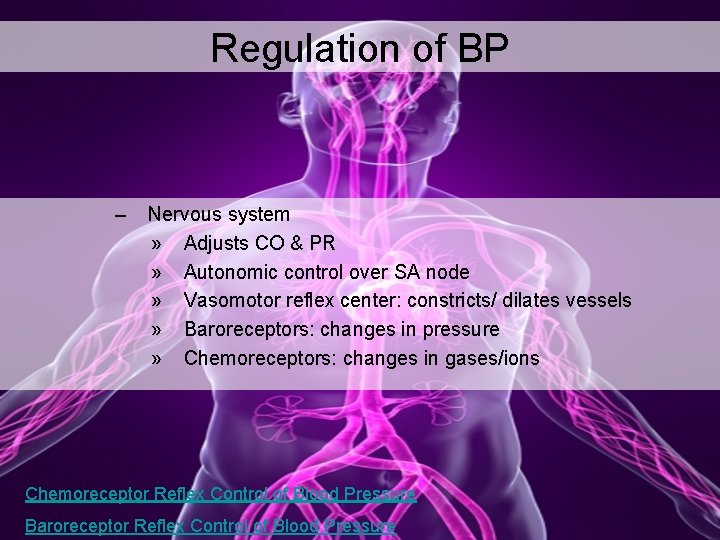
Regulation of BP – Nervous system » Adjusts CO & PR » Autonomic control over SA node » Vasomotor reflex center: constricts/ dilates vessels » Baroreceptors: changes in pressure » Chemoreceptors: changes in gases/ions Chemoreceptor Reflex Control of Blood Pressure Baroreceptor Reflex Control of Blood Pressure
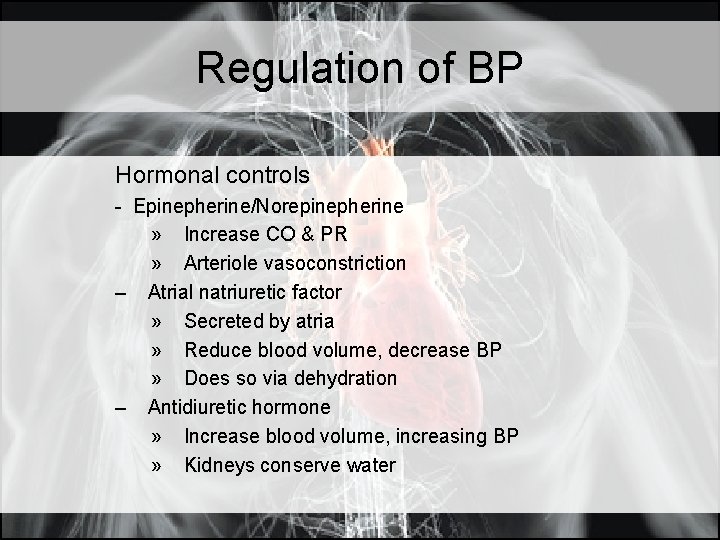
Regulation of BP Hormonal controls - Epinepherine/Norepinepherine » Increase CO & PR » Arteriole vasoconstriction – Atrial natriuretic factor » Secreted by atria » Reduce blood volume, decrease BP » Does so via dehydration – Antidiuretic hormone » Increase blood volume, increasing BP » Kidneys conserve water
Regulation of BP • Kidney’s – Maintain long term BP controls » Regulate water excretion rate – Release of Renin » Triggers angiotensin: vasoconstrictor » Triggers aldosterone: reabsorb Na+/water follows » Increases BP by increasing BV & PR
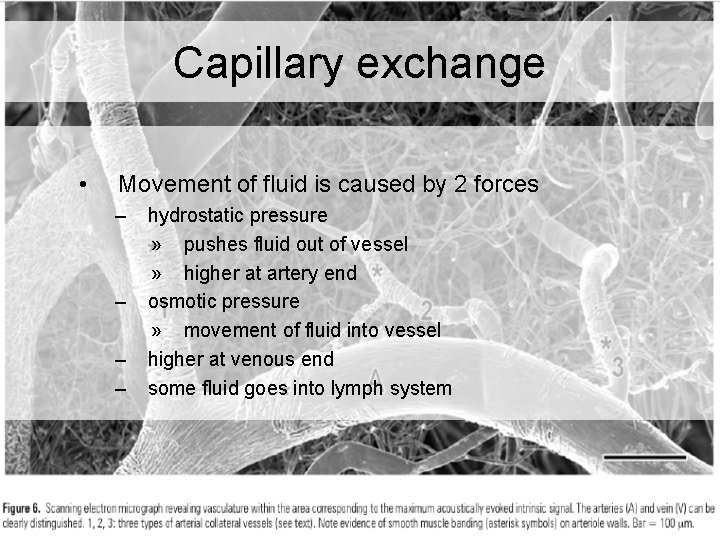
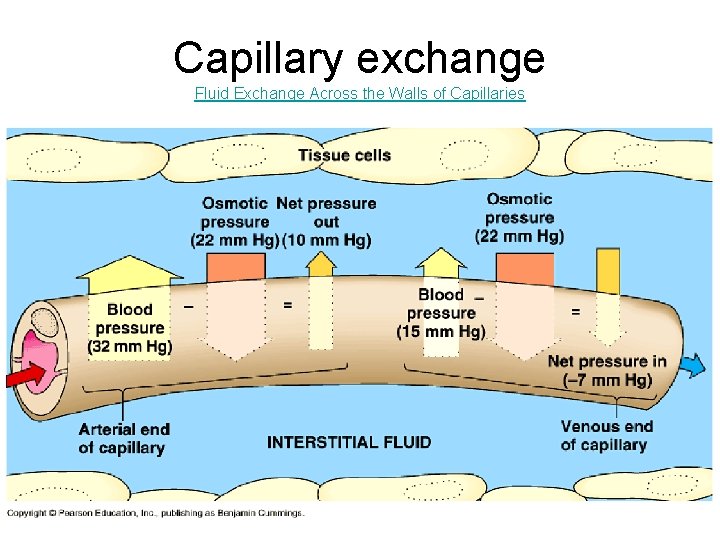
Capillary exchange • Movement of fluid is caused by 2 forces – – hydrostatic pressure » pushes fluid out of vessel » higher at artery end osmotic pressure » movement of fluid into vessel higher at venous end some fluid goes into lymph system
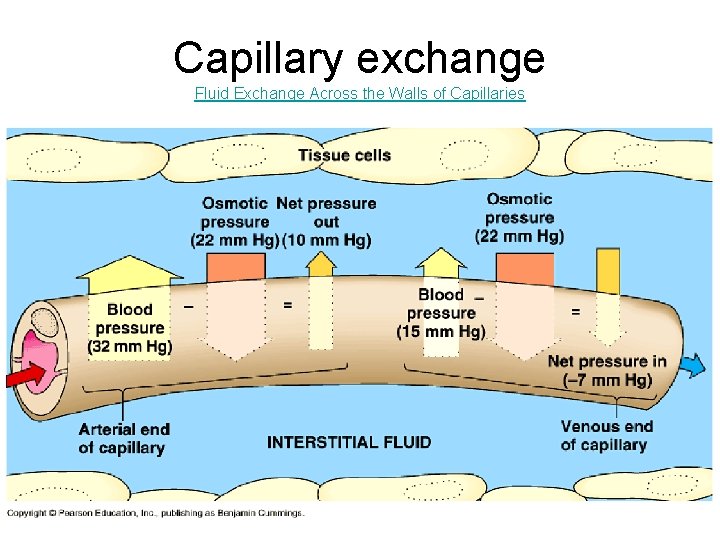
Capillary exchange Fluid Exchange Across the Walls of Capillaries
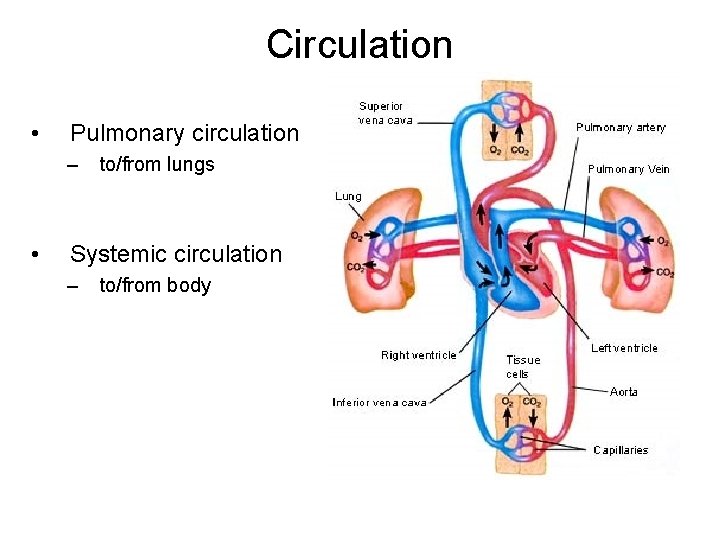
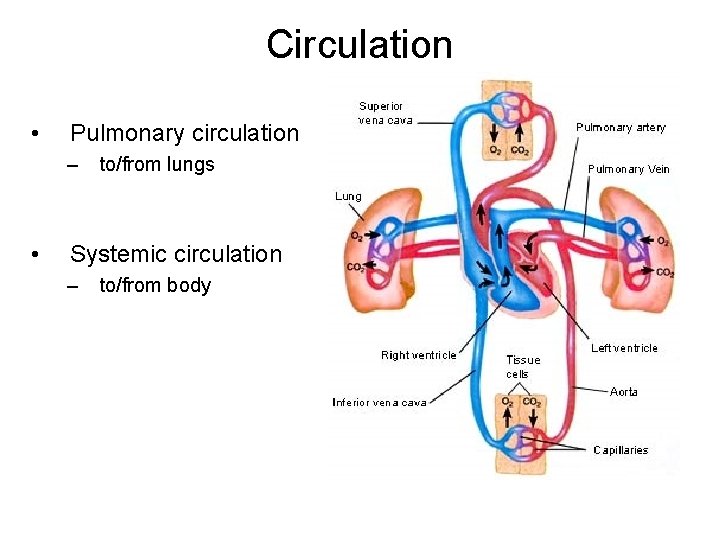
Circulation • Pulmonary circulation – • to/from lungs Systemic circulation – to/from body