The Cardiac Cycle Heart Murmur Sounds produced by

The Cardiac Cycle • Heart Murmur – Sounds produced by regurgitation through valves
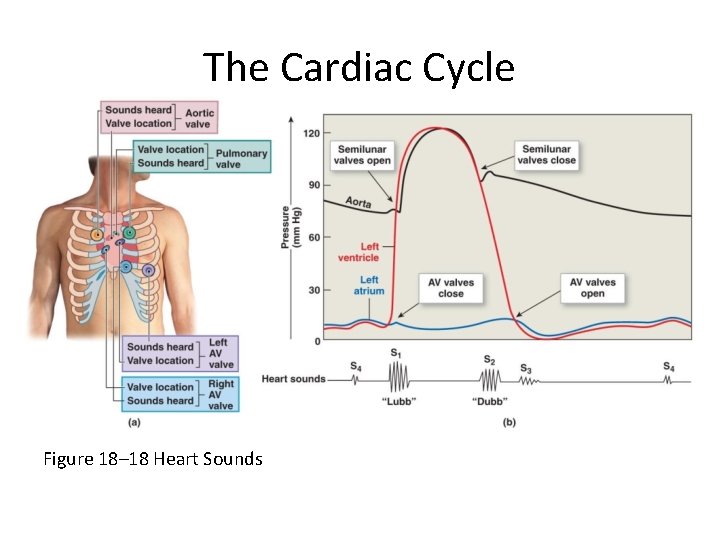
The Cardiac Cycle Figure 18– 18 Heart Sounds
Cardiodynamics • The movement and force generated by cardiac contractions – End-diastolic volume (EDV) – End-systolic volume (ESV) – Stroke volume (SV) • SV = EDV – ESV – Ejection fraction • The percentage of EDV represented by SV – Cardiac output (CO) • The volume pumped by left ventricle in 1 minute
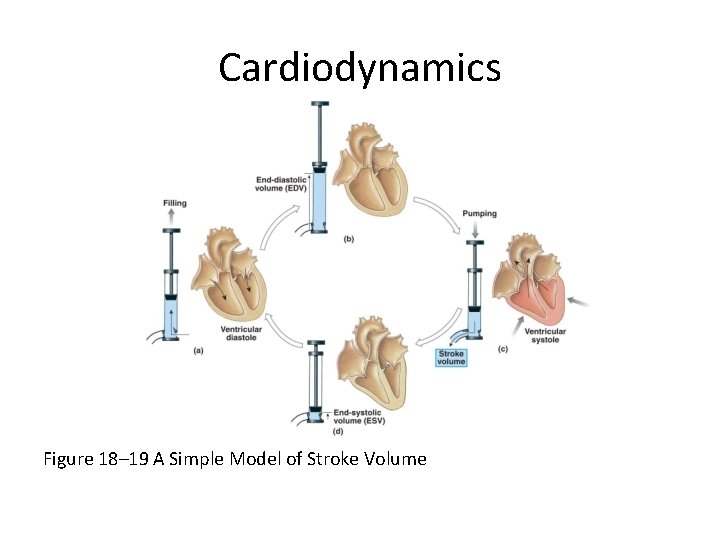
Cardiodynamics Figure 18– 19 A Simple Model of Stroke Volume
Cardiodynamics • Cardiac Output • CO = HR X SV • CO = cardiac output (m. L/min) • HR = heart rate (beats/min) • SV = stroke volume (m. L/beat)
Cardiodynamics • Factors Affecting Cardiac Output – Cardiac output • Adjusted by changes in heart rate or stroke volume – Heart rate • Adjusted by autonomic nervous system or hormones – Stroke volume • Adjusted by changing EDV or ESV
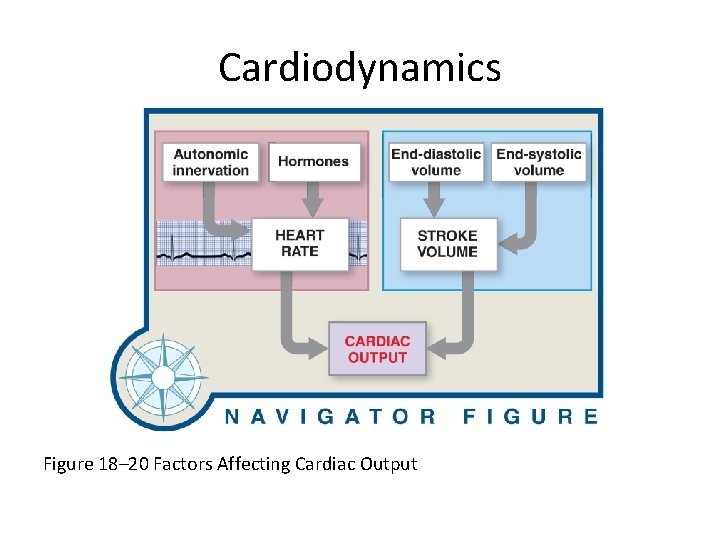
Cardiodynamics Figure 18– 20 Factors Affecting Cardiac Output
Cardiodynamics • Factors Affecting the Heart Rate – Autonomic innervation • Cardiac plexuses: innervate heart • Vagus nerves (X): carry parasympathetic preganglionic fibers to small ganglia in cardiac plexus • Cardiac centers of medulla oblongata: – cardioacceleratory center controls sympathetic neurons (increases heart rate) – cardioinhibitory center controls parasympathetic neurons (slows heart rate)
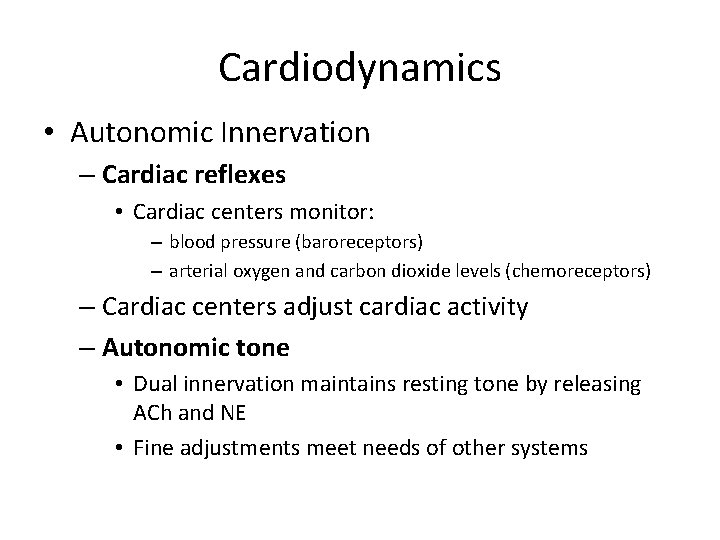
Cardiodynamics • Autonomic Innervation – Cardiac reflexes • Cardiac centers monitor: – blood pressure (baroreceptors) – arterial oxygen and carbon dioxide levels (chemoreceptors) – Cardiac centers adjust cardiac activity – Autonomic tone • Dual innervation maintains resting tone by releasing ACh and NE • Fine adjustments meet needs of other systems
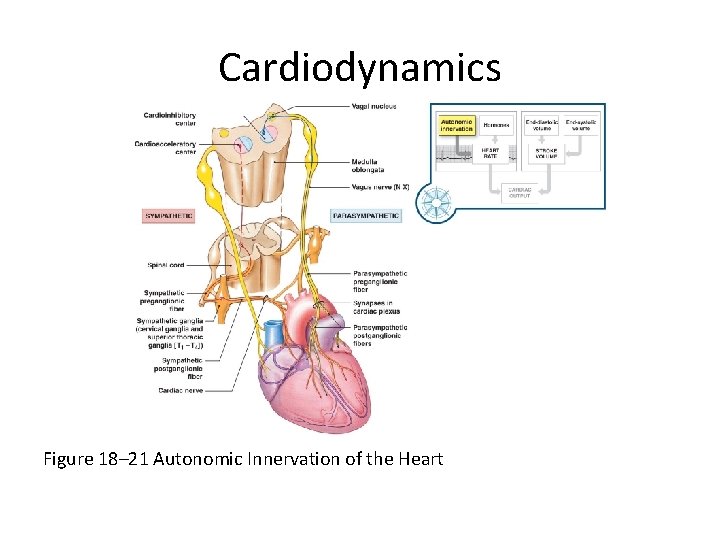
Cardiodynamics Figure 18– 21 Autonomic Innervation of the Heart
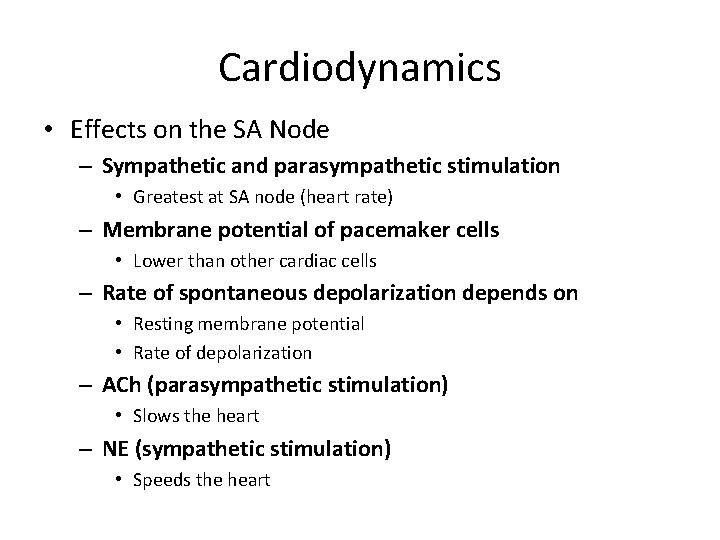
Cardiodynamics • Effects on the SA Node – Sympathetic and parasympathetic stimulation • Greatest at SA node (heart rate) – Membrane potential of pacemaker cells • Lower than other cardiac cells – Rate of spontaneous depolarization depends on • Resting membrane potential • Rate of depolarization – ACh (parasympathetic stimulation) • Slows the heart – NE (sympathetic stimulation) • Speeds the heart
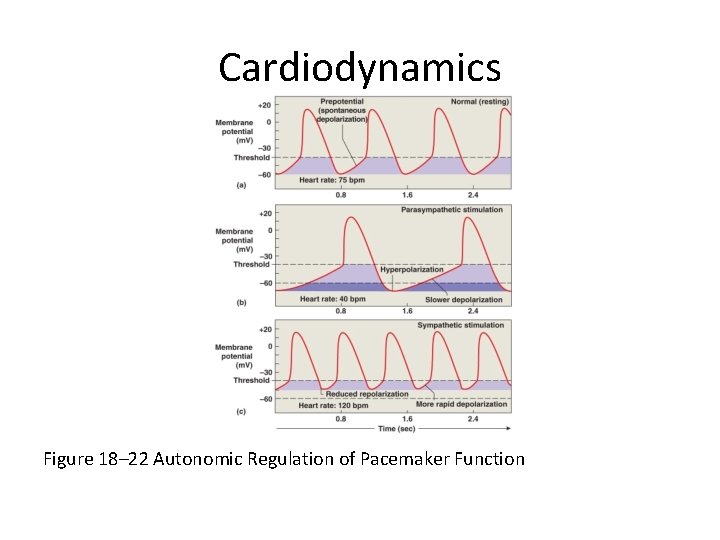
Cardiodynamics Figure 18– 22 Autonomic Regulation of Pacemaker Function
Cardiodynamics • Atrial Reflex – Also called Bainbridge reflex – Adjusts heart rate in response to venous return – Stretch receptors in right atrium • Trigger increase in heart rate • Through increased sympathetic activity
Cardiodynamics • Hormonal Effects on Heart Rate – Increase heart rate (by sympathetic stimulation of SA node) • Epinephrine (E) • Norepinephrine (NE) • Thyroid hormone
Cardiodynamics • Factors Affecting the Stroke Volume – The EDV: amount of blood a ventricle contains at the end of diastole • Filling time: – duration of ventricular diastole • Venous return: – rate of blood flow during ventricular diastole
Cardiodynamics • Preload – The degree of ventricular stretching during ventricular diastole – Directly proportional to EDV – Affects ability of muscle cells to produce tension
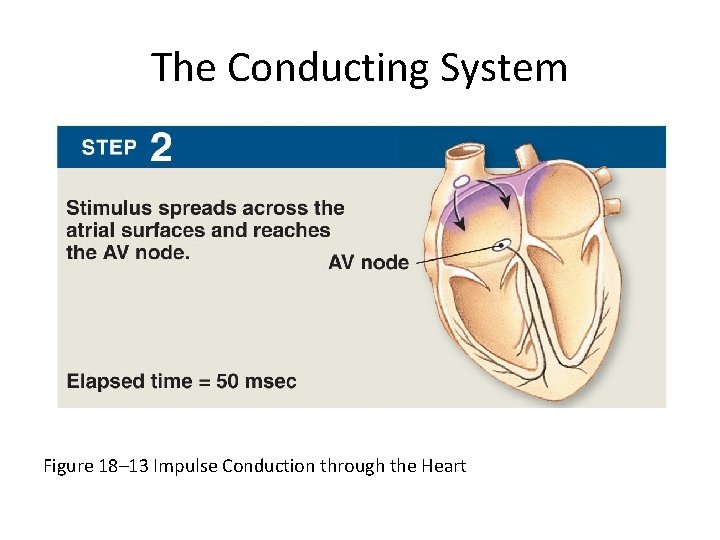
The Conducting System Figure 18– 13 Impulse Conduction through the Heart
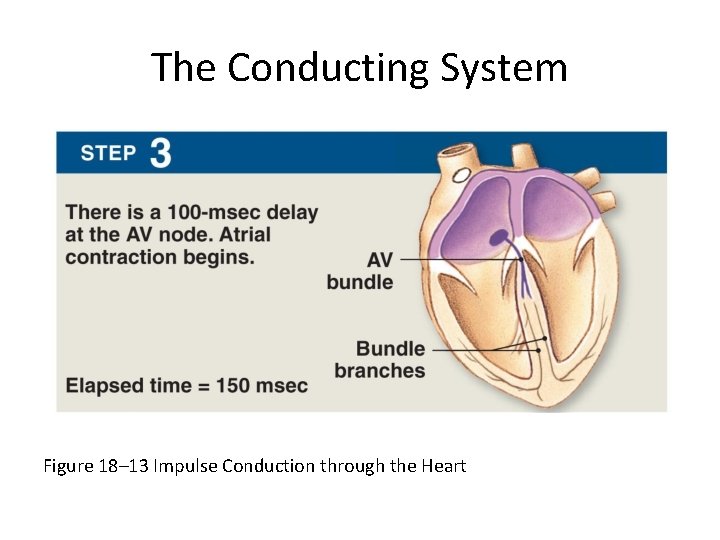
The Conducting System Figure 18– 13 Impulse Conduction through the Heart
The Conducting System • The AV Bundle – In the septum – Carries impulse to left and right bundle branches • Which conduct to Purkinje fibers (Step 4) – And to the moderator band • Which conducts to papillary muscles
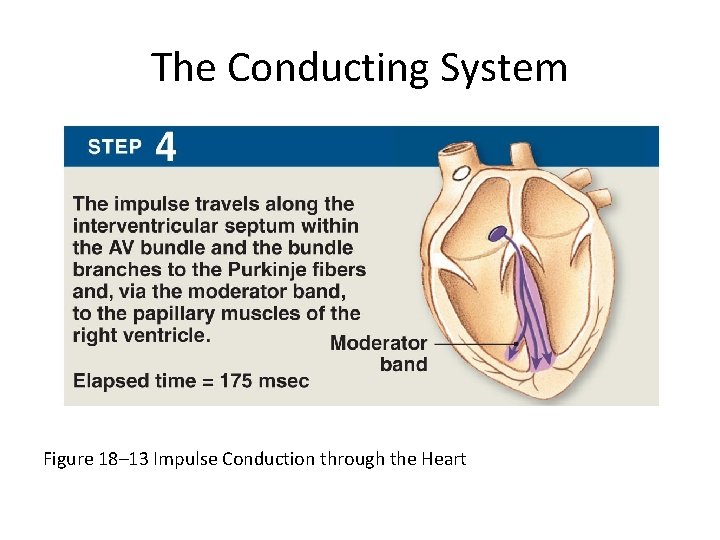
The Conducting System Figure 18– 13 Impulse Conduction through the Heart
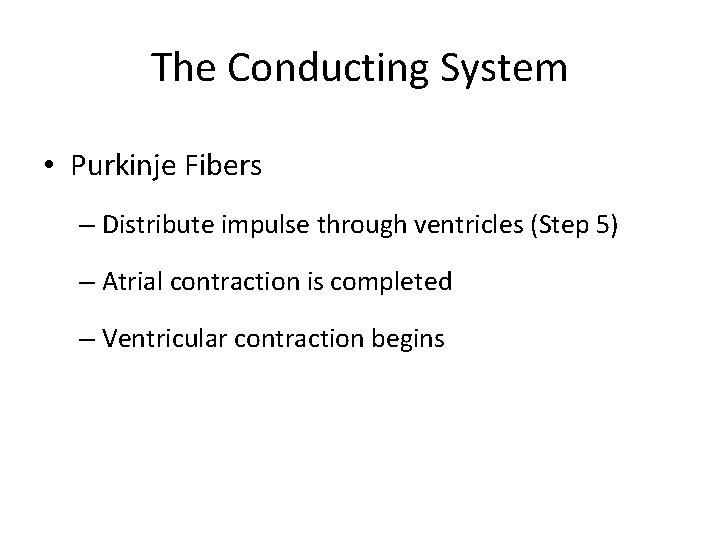
The Conducting System • Purkinje Fibers – Distribute impulse through ventricles (Step 5) – Atrial contraction is completed – Ventricular contraction begins
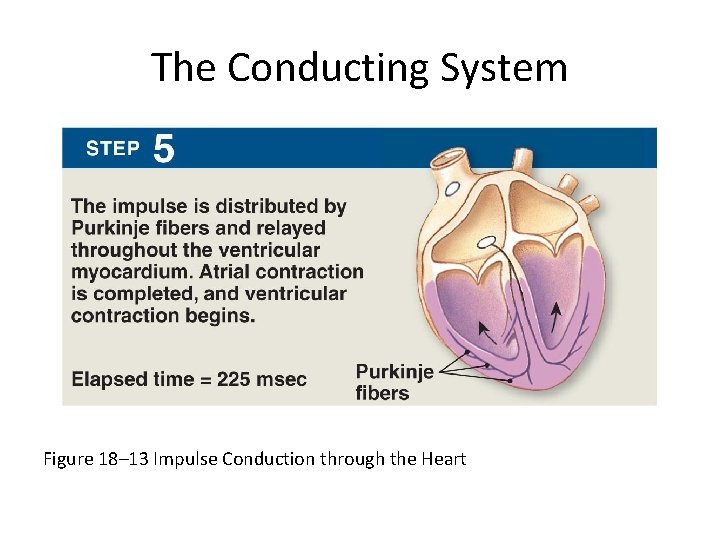
The Conducting System Figure 18– 13 Impulse Conduction through the Heart
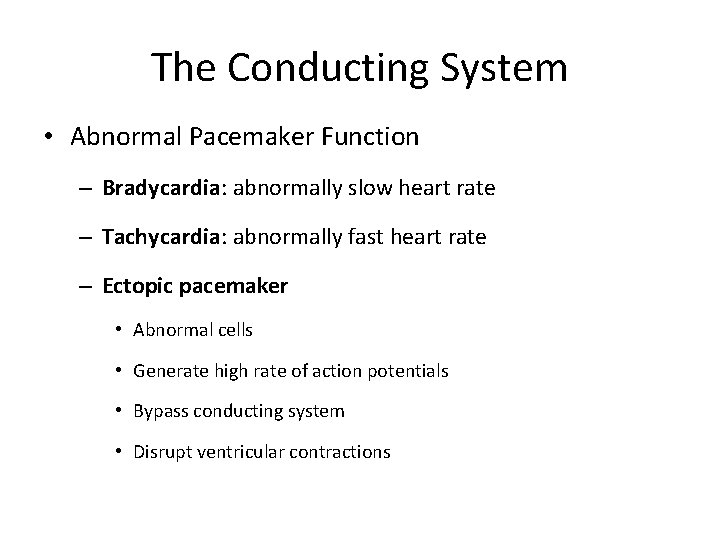
The Conducting System • Abnormal Pacemaker Function – Bradycardia: abnormally slow heart rate – Tachycardia: abnormally fast heart rate – Ectopic pacemaker • Abnormal cells • Generate high rate of action potentials • Bypass conducting system • Disrupt ventricular contractions
The Conducting System • Electrocardiogram (ECG or EKG) – A recording of electrical events in the heart – Obtained by electrodes at specific body locations – Abnormal patterns diagnose damage
The Conducting System • Features of an ECG – P wave • Atria depolarize – QRS complex • Ventricles depolarize – T wave • Ventricles repolarize
The Conducting System • Time Intervals Between ECG Waves – P–R interval • From start of atrial depolarization • To start of QRS complex – Q–T interval • From ventricular depolarization • To ventricular repolarization
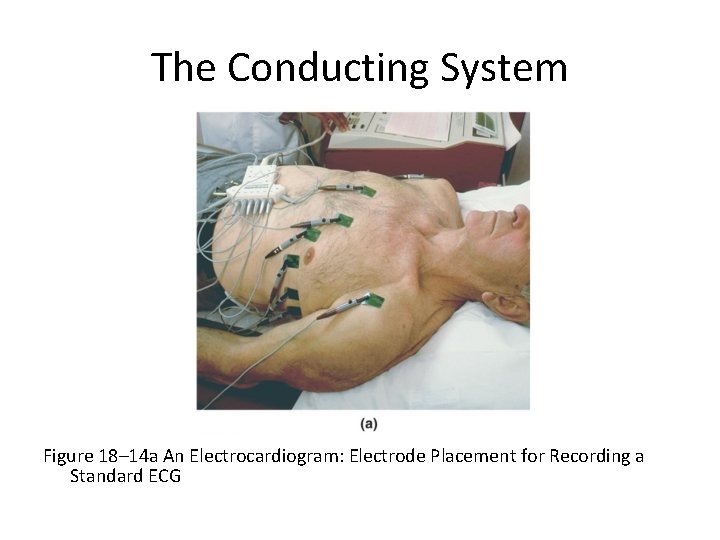
The Conducting System Figure 18– 14 a An Electrocardiogram: Electrode Placement for Recording a Standard ECG
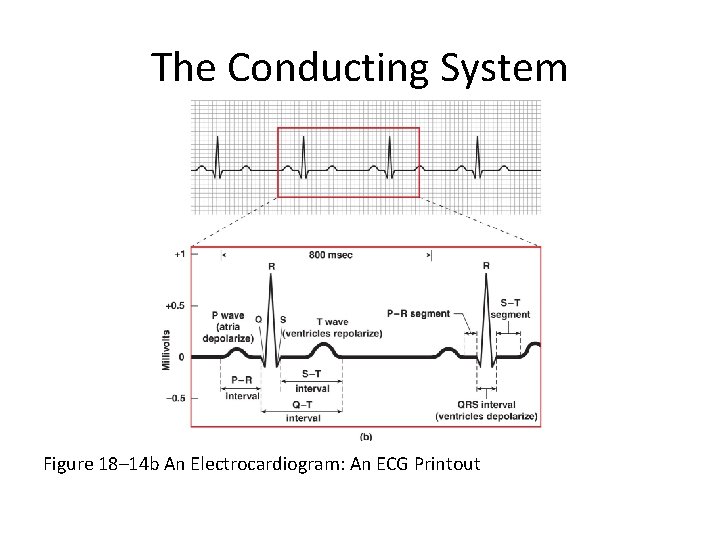
The Conducting System Figure 18– 14 b An Electrocardiogram: An ECG Printout
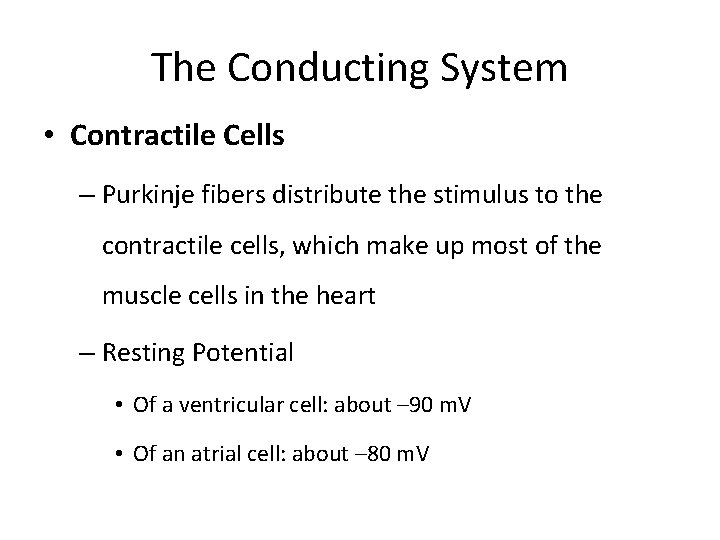
The Conducting System • Contractile Cells – Purkinje fibers distribute the stimulus to the contractile cells, which make up most of the muscle cells in the heart – Resting Potential • Of a ventricular cell: about – 90 m. V • Of an atrial cell: about – 80 m. V
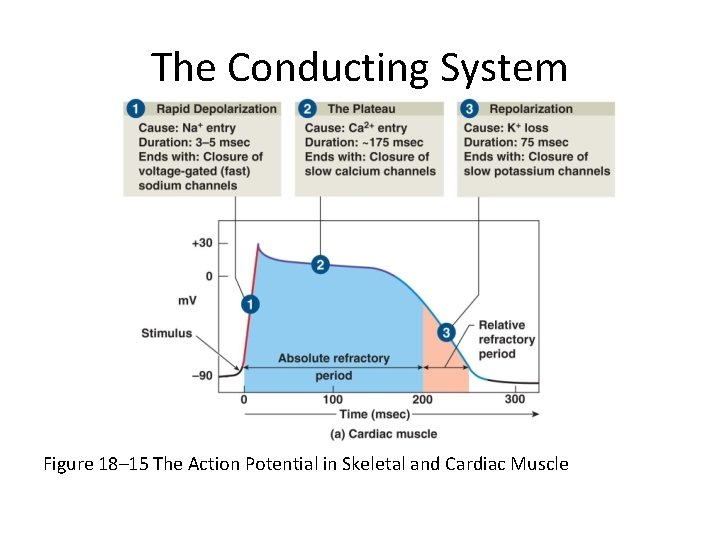
The Conducting System Figure 18– 15 The Action Potential in Skeletal and Cardiac Muscle
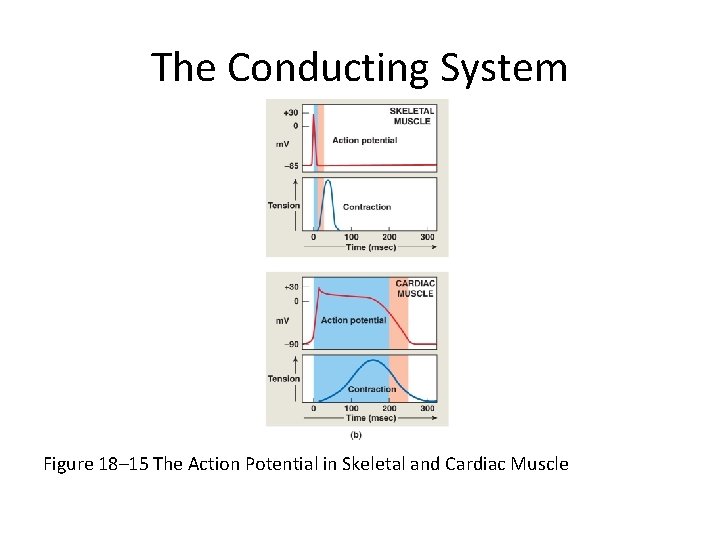
The Conducting System Figure 18– 15 The Action Potential in Skeletal and Cardiac Muscle
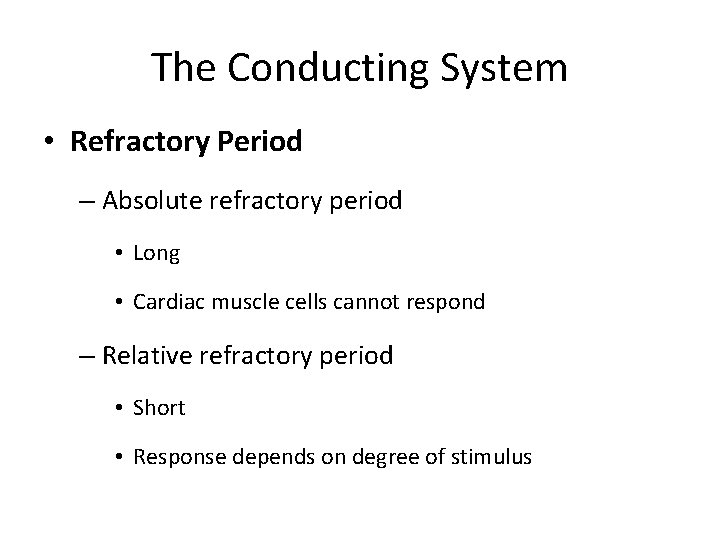
The Conducting System • Refractory Period – Absolute refractory period • Long • Cardiac muscle cells cannot respond – Relative refractory period • Short • Response depends on degree of stimulus
The Conducting System • Timing of Refractory Periods – Length of cardiac action potential in ventricular cell • 250– 300 msecs: – 30 times longer than skeletal muscle fiber – long refractory period prevents summation and tetany
The Conducting System • The Role of Calcium Ions in Cardiac Contractions – Contraction of a cardiac muscle cell is produced by an increase in calcium ion concentration around myofibrils
The Conducting System • The Role of Calcium Ions in Cardiac Contractions – 20% of calcium ions required for a contraction • Calcium ions enter plasma membrane during plateau phase – Arrival of extracellular Ca 2+ • Triggers release of calcium ion reserves from sarcoplasmic reticulum
The Conducting System • The Role of Calcium Ions in Cardiac Contractions – As slow calcium channels close • Intracellular Ca 2+ is absorbed by the SR • Or pumped out of cell – Cardiac muscle tissue • Very sensitive to extracellular Ca 2+ concentrations
The Conducting System • The Energy for Cardiac Contractions – Aerobic energy of heart • From mitochondrial breakdown of fatty acids and glucose • Oxygen from circulating hemoglobin • Cardiac muscles store oxygen in myoglobin
- Slides: 38