THE BONY PELVIS THE BONY PELVIS a Pelvic
THE BONY PELVIS
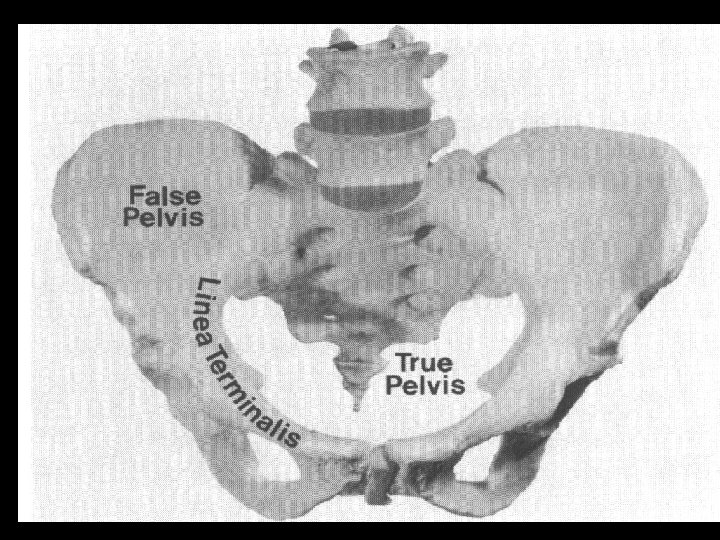
THE BONY PELVIS a. Pelvic anatomy b. Pelvic joints c. Planes & diameters of the pelvis d. Pelvic shapes e. Pelvic size and its clinical estimation
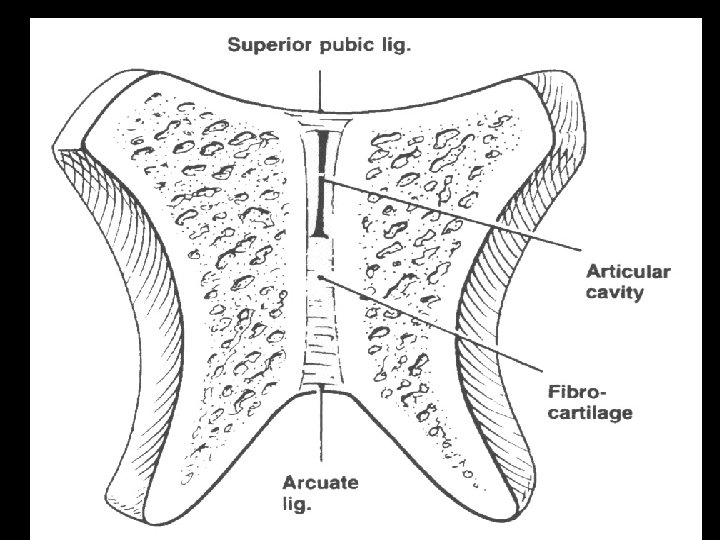
a. PELVIC ANATOMY b. PELVIC JOINTS - Symphysis pubis - Sacroiliac joints - Relaxation of the pelvic joints ( especially during pregnancy)
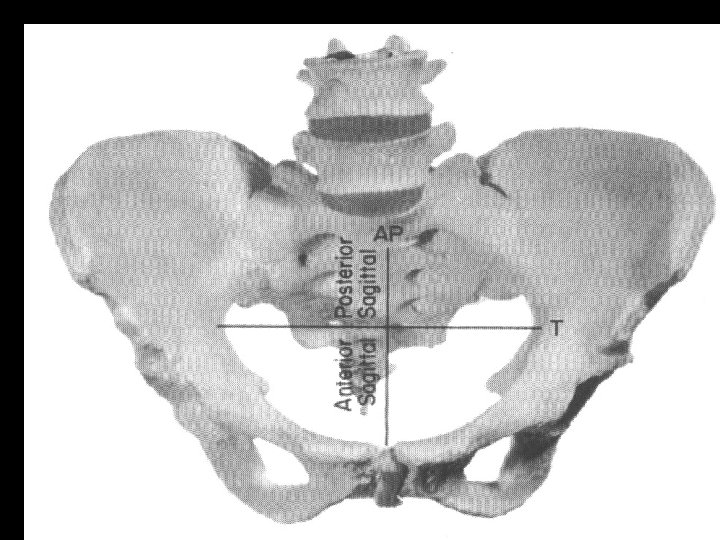
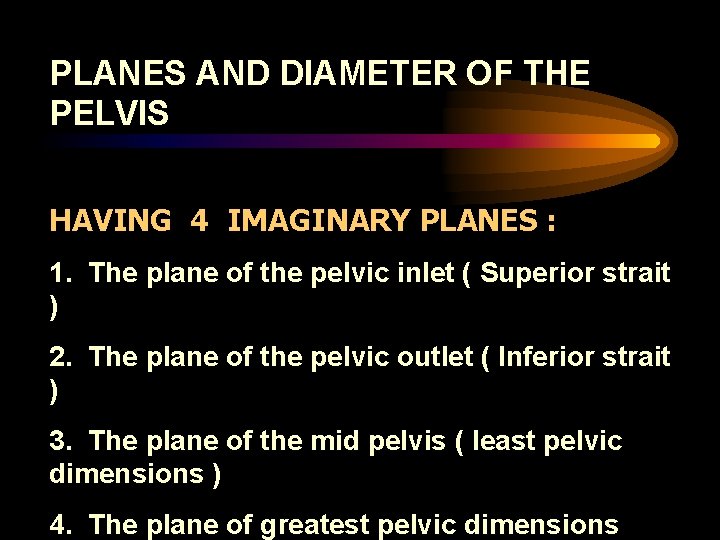
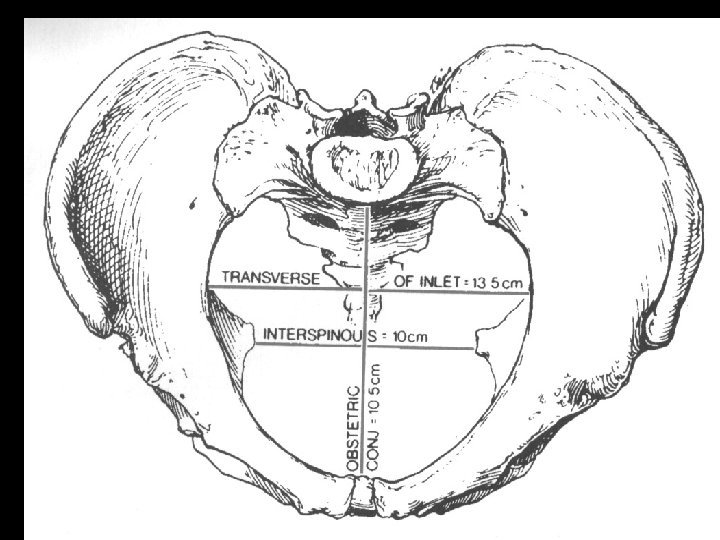
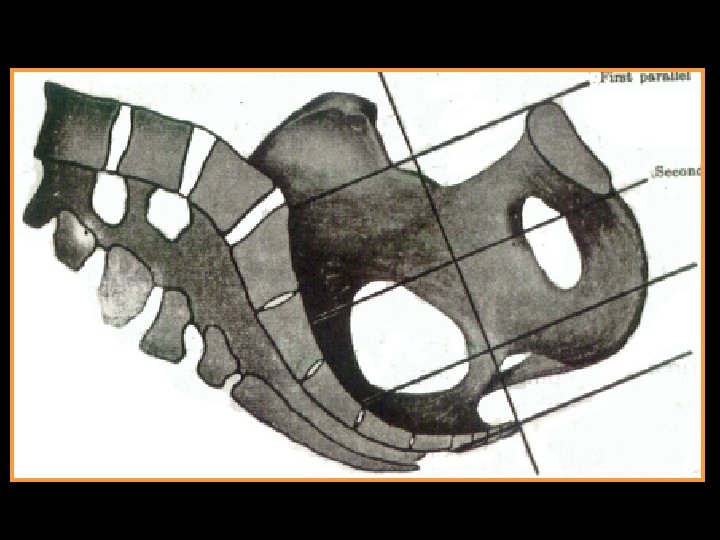
PLANES AND DIAMETER OF THE PELVIS HAVING 4 IMAGINARY PLANES : 1. The plane of the pelvic inlet ( Superior strait ) 2. The plane of the pelvic outlet ( Inferior strait ) 3. The plane of the mid pelvis ( least pelvic dimensions ) 4. The plane of greatest pelvic dimensions
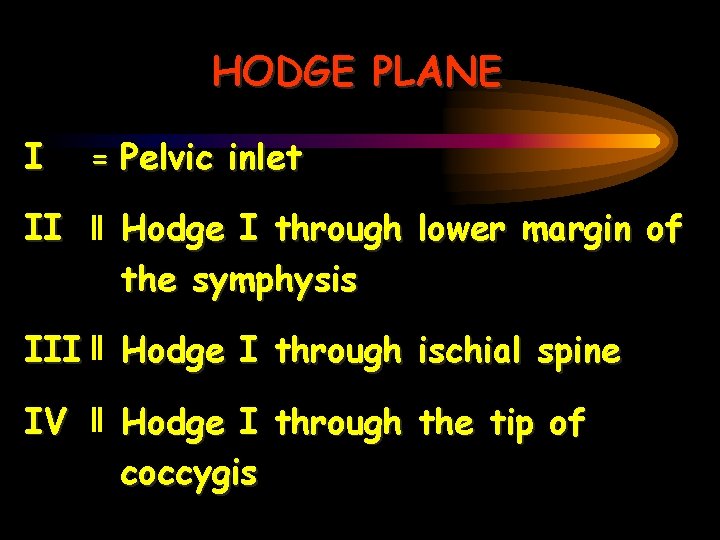
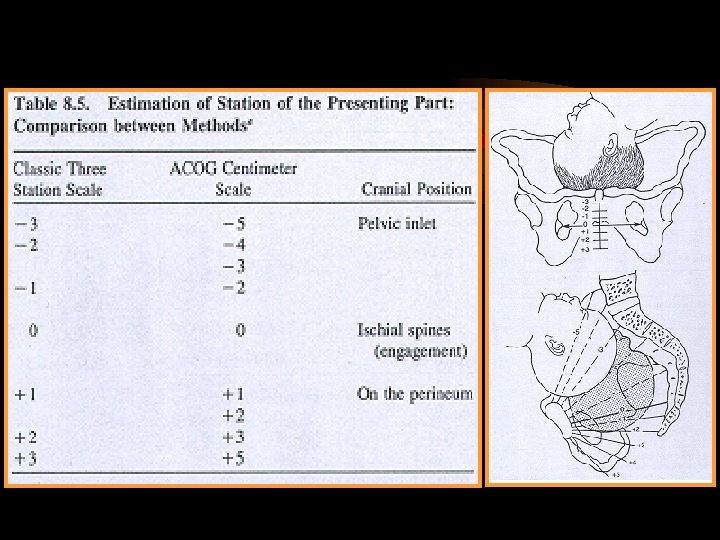
HODGE PLANE I = Pelvic inlet II Hodge I through lower margin of the symphysis III Hodge I through ischial spine IV Hodge I through the tip of coccygis
PELVIC SHAPES CALDWELL - MOLOY CLASSIFICATION (1933 - 34) Gynecoid pelvis Android pelvis Anthropoid pelvis Platypelloid pelvis
GYNECOID PELVIS - Almost 50% of white women (Todd’ Collection study) - Ascertained the frequency of the four parent pelvic types by study of Todd’s Collection ( Caldwell & Co. Workers, 1939) ANDROID PELVIS - 1/3 of pure type pelvis ( white women), 1/6 non white women - The extreme android pelvis presages poor prognosis for vaginal
ANTHROPOID PELVIS - 1/4 pure type pelvis in white women and nearly 1 1/2 of those in non white women PLATYPELLOID PELVIS - Rarest of the pure varieties ( < 3% ) INTERMEDIATE TYPE PELVIS - Mixed type - More frequent than pure types
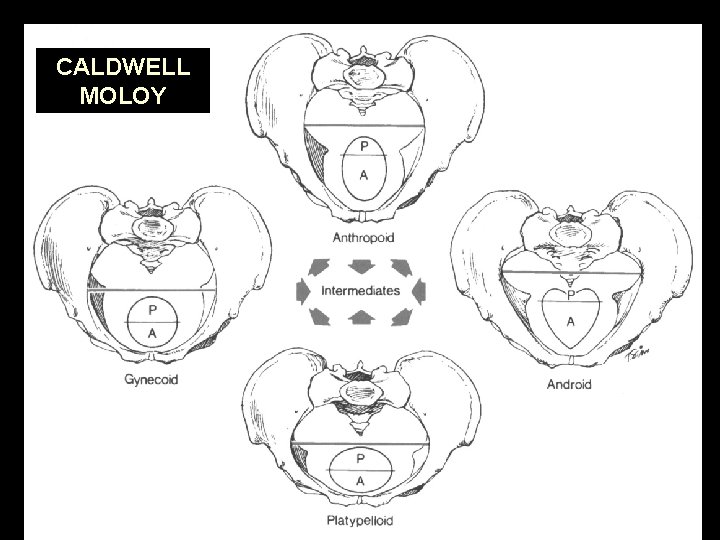
CALDWELL MOLOY
PELVIC SIZE AND ITS CLINICAL ESTIMATION - Pelvic inlet measurements - Diagonal conjugate - Engagerment : - with engagerment, the fetal head serves as an internal pelvimeter to demonstrate that the pelvic inlet is ample for that
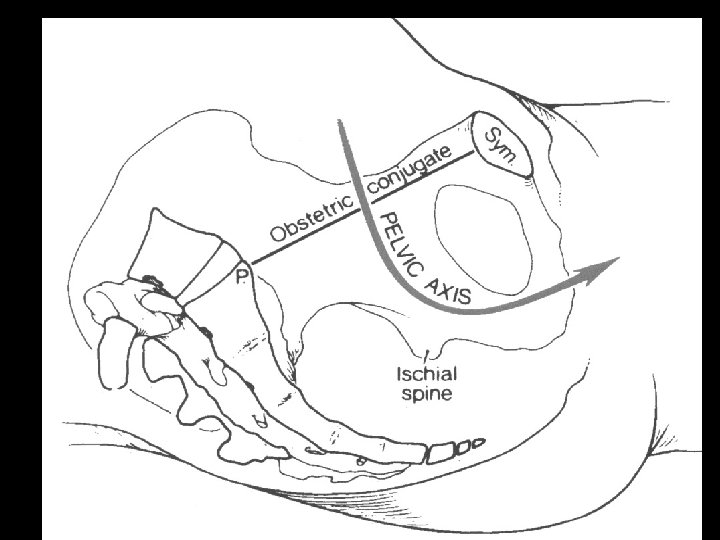
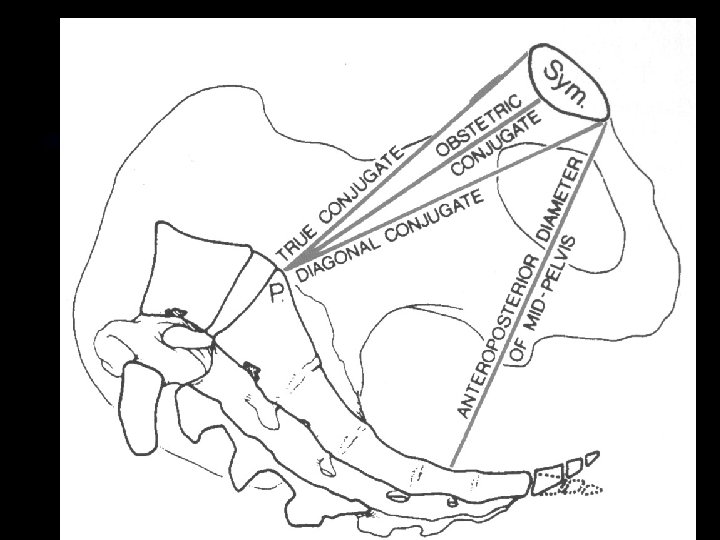
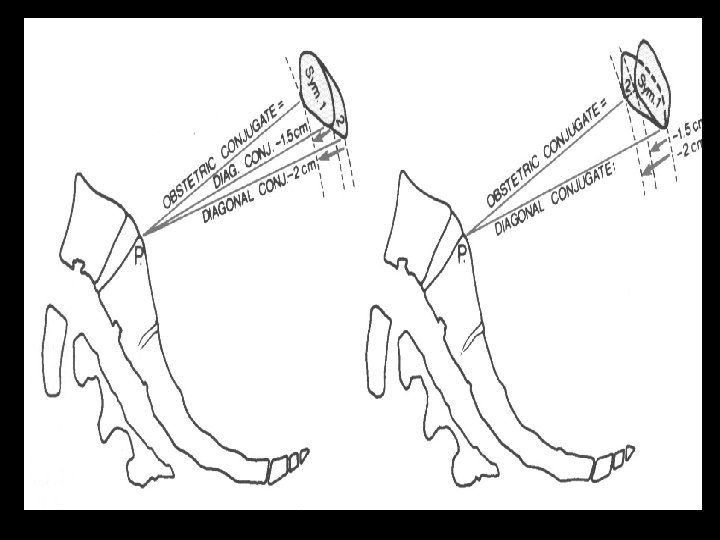
PELVIC INLET - Obstetrical conjugate ( normal > 10 cm) - Diagonal conjugate CD - 1. 5 to 2 cm = True conjugate
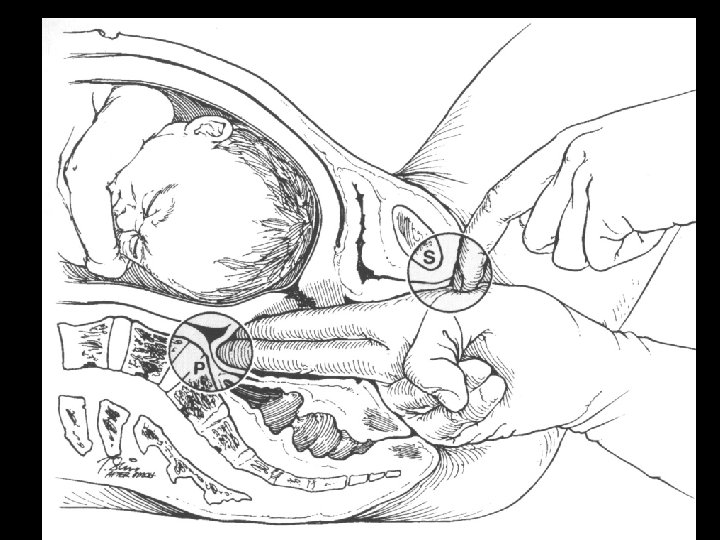
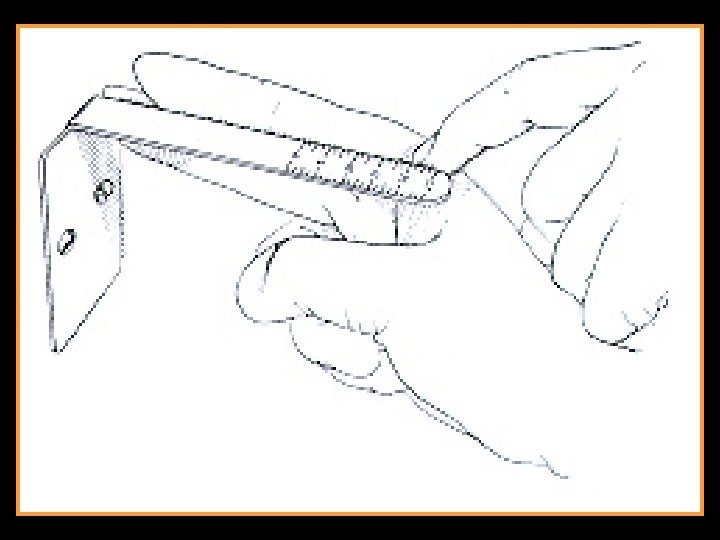
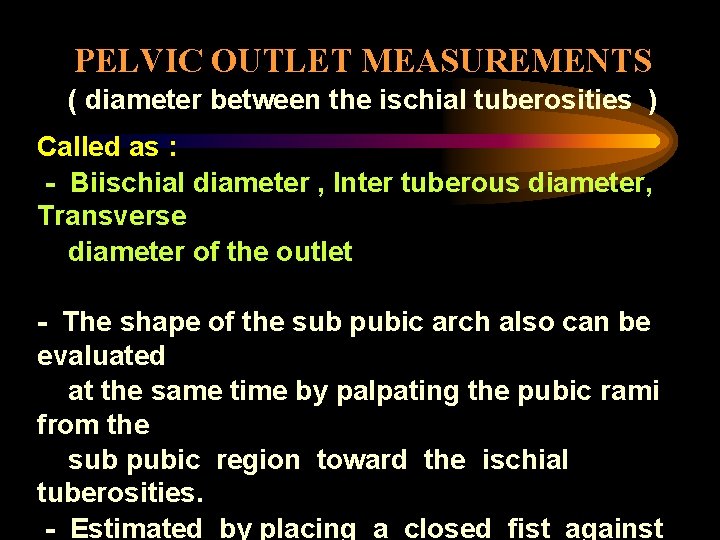
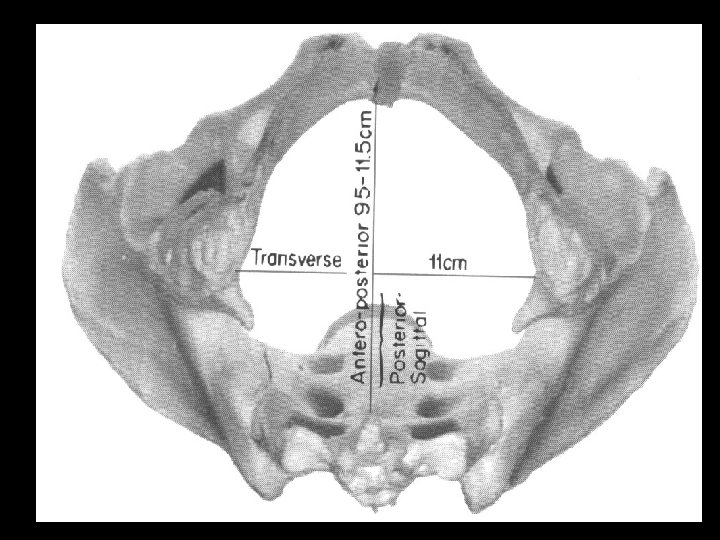
PELVIC OUTLET MEASUREMENTS ( diameter between the ischial tuberosities ) Called as : - Biischial diameter , Inter tuberous diameter, Transverse diameter of the outlet - The shape of the sub pubic arch also can be evaluated at the same time by palpating the pubic rami from the sub pubic region toward the ischial tuberosities. - Estimated by placing a closed fist against
MID PELVIS ESTIMATION - Clinical estimation of mid pelvis capacity by any direct form of measurement is not possible Suspicion contracted pelvis in this region : - Ischial spines are quite prominent - The side walls are felt to converge - The concavity of the sacrum is very shallow - Ischial diameter of the outlet < 8 cm
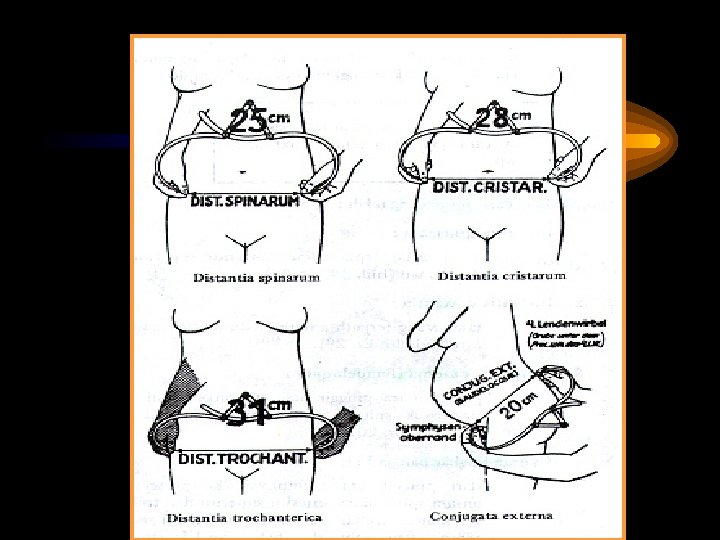
Outer measurement ü Distantia spinarum ü Distantia cristarum ü External conjugate (Baudelaque) Vaginal examination
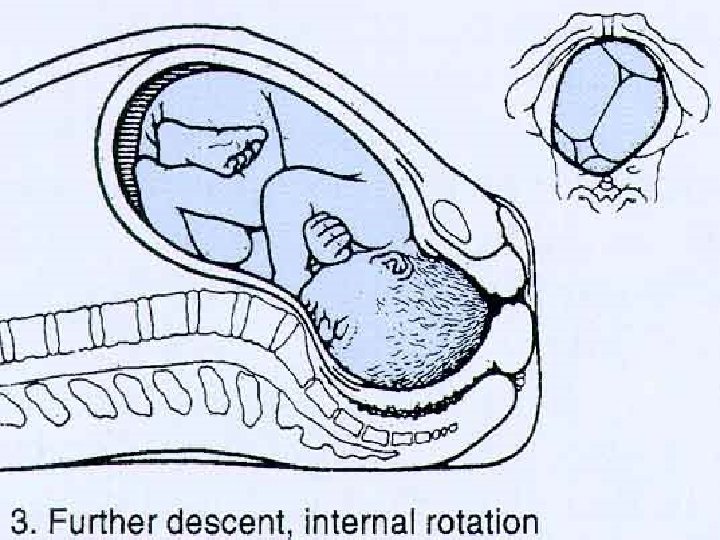
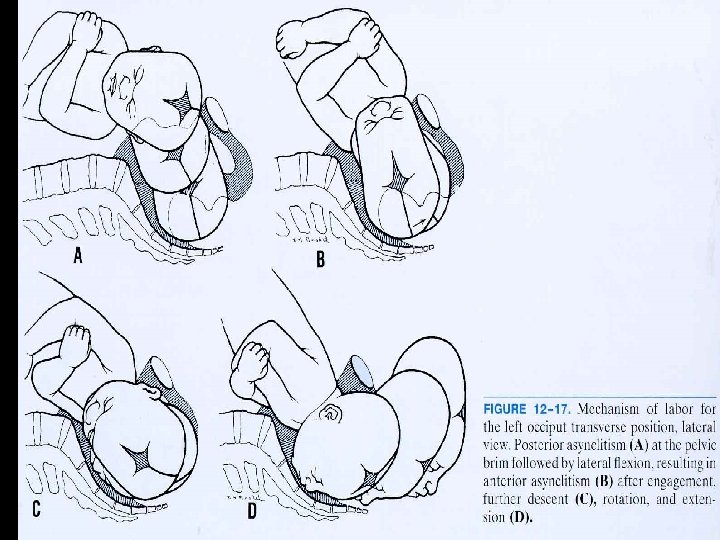
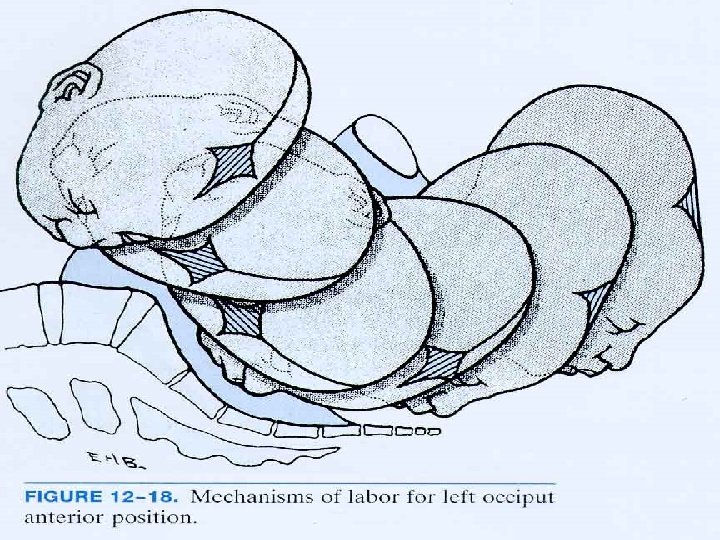
• 95 % of all labors is in vertex presentation and most commonly ascertained by abdominal palpation and confirmed by vaginal examination • Majority of cases the vertex enters the pelvis with the sagittal suture in the transverse pelvic diameter • The fetus enters the pelvis in the Left Occiput Transverse Position / LOT (40% of labors) & 20% ROT. • The head either enters the pelvis with the occiput rotated 45 o anteriorly from the
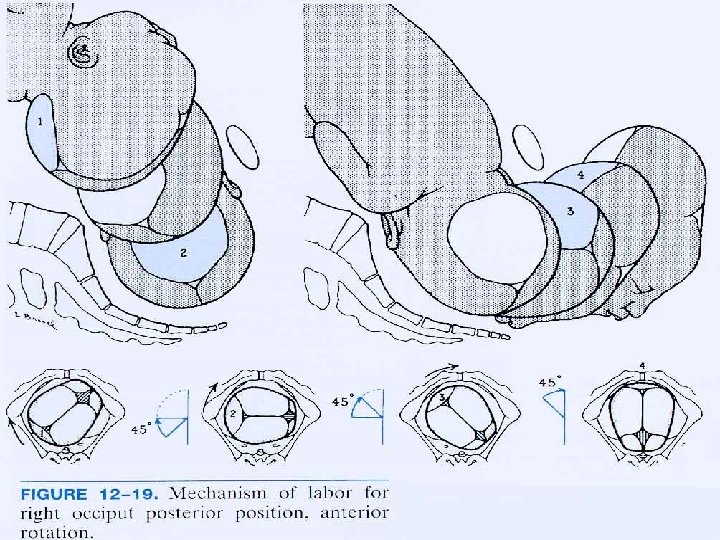
• 20 % of all labors the fetus enters the pelvis in an Occiput Posterior (OP) position. • The ROP is slightly more common than LOP and posterior positions are more often associated with a narrow forepelvis • The head either enters the pelvis with the occiput rotated 45 o anteriorly from the transverse position
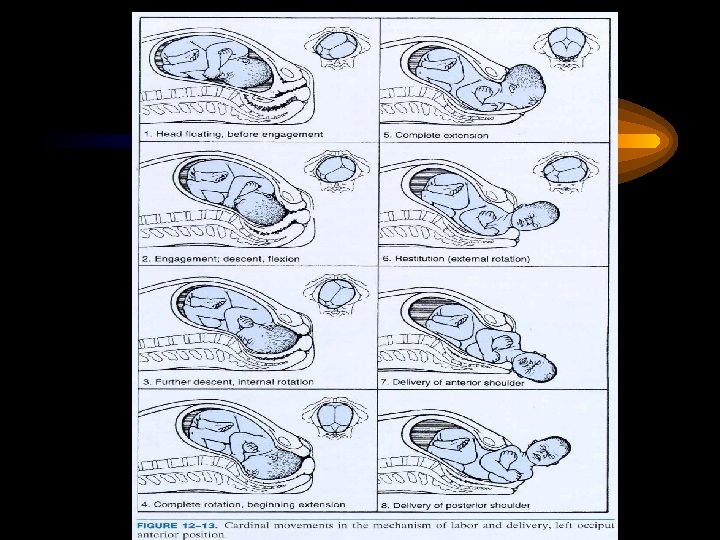
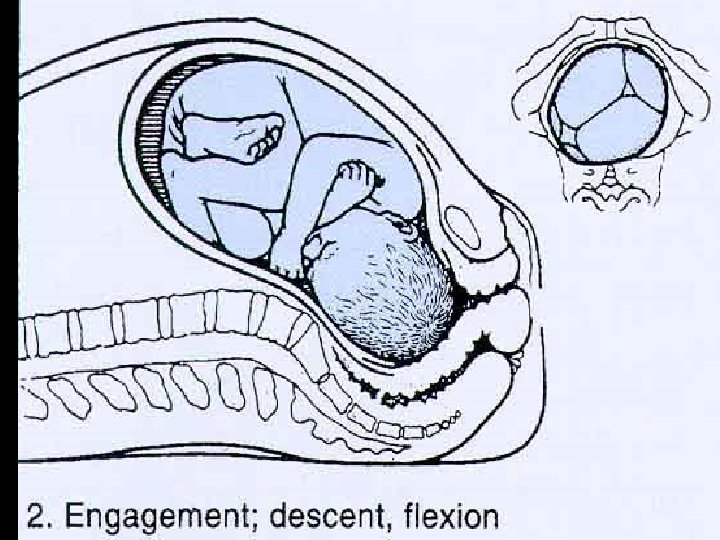
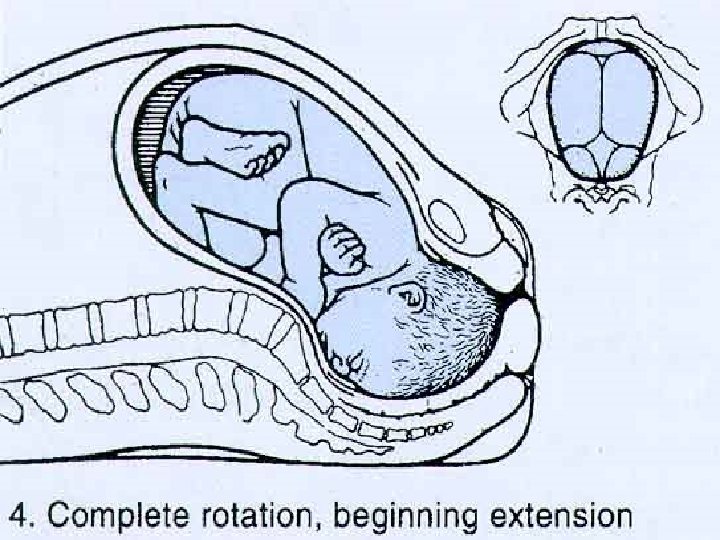
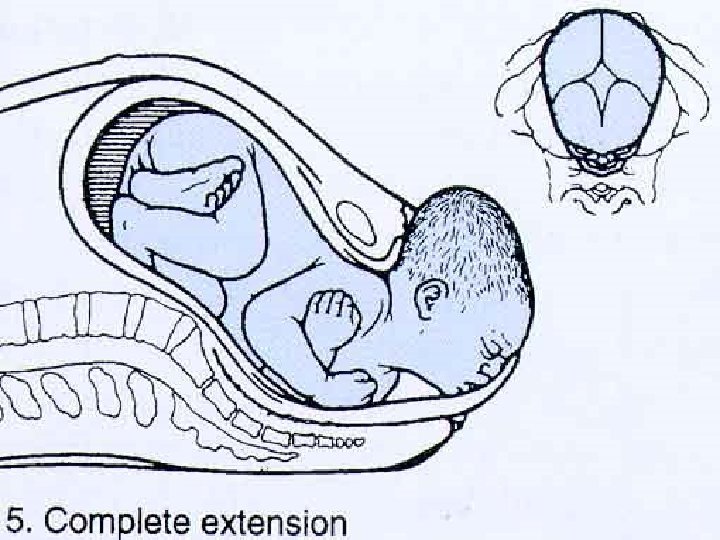
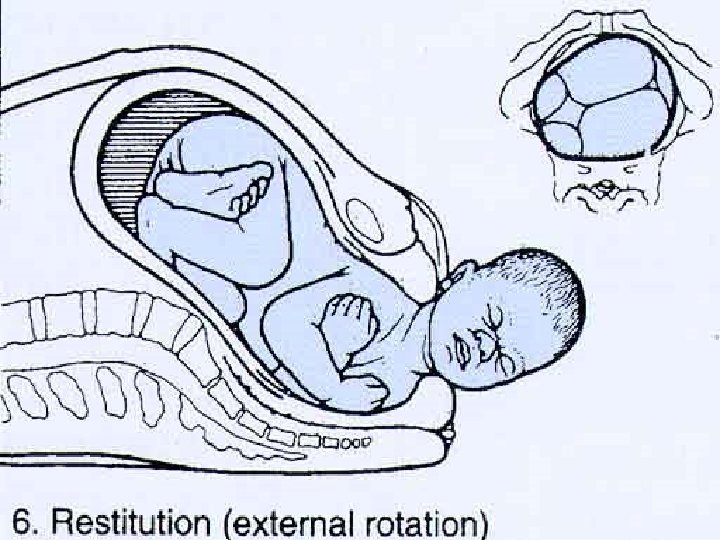
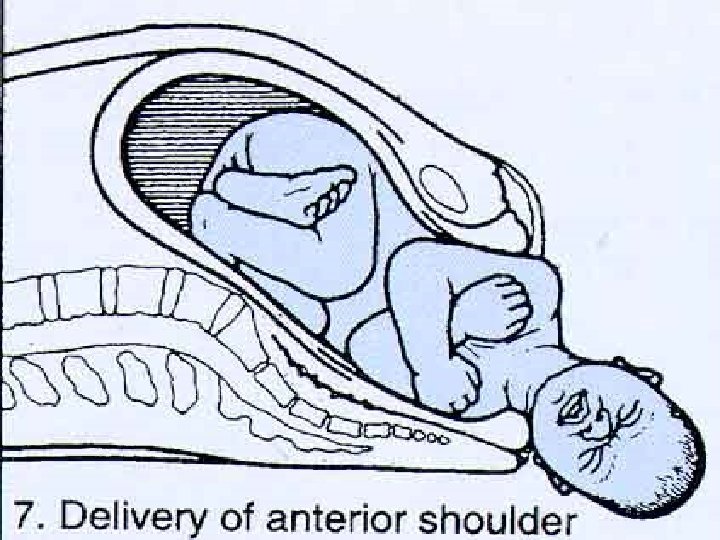
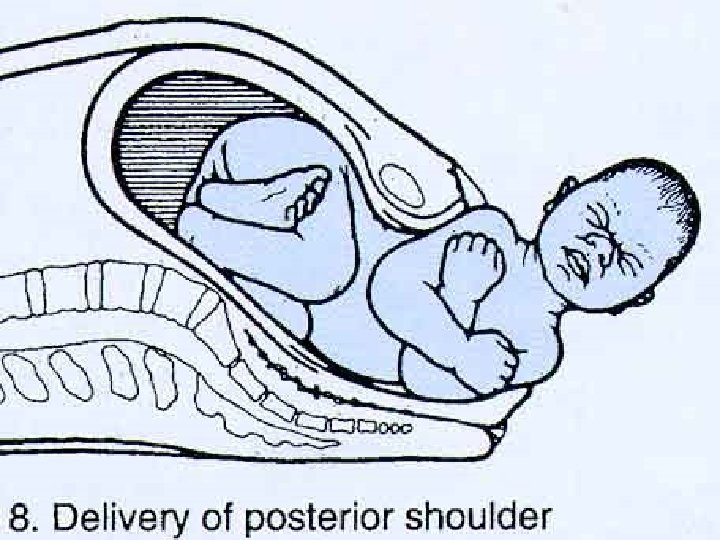
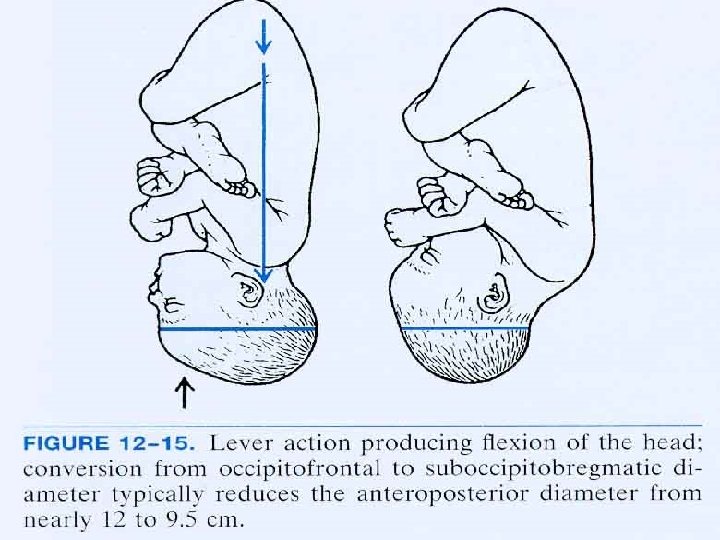
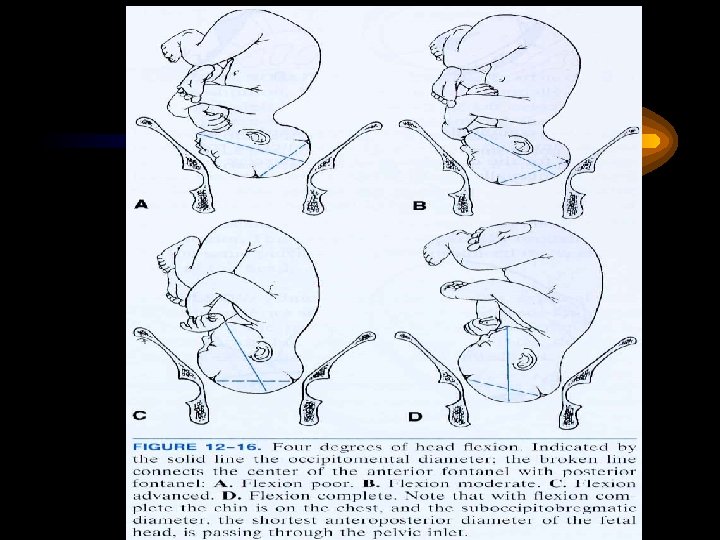
THE CARDINAL MOVEMENTS OF LABOR ARE : • ENGAGEMENT • DESCENT • FLEXION • INTERNAL ROTATION • EXTENSION • EXTERNAL ROTATION • EXPULSION
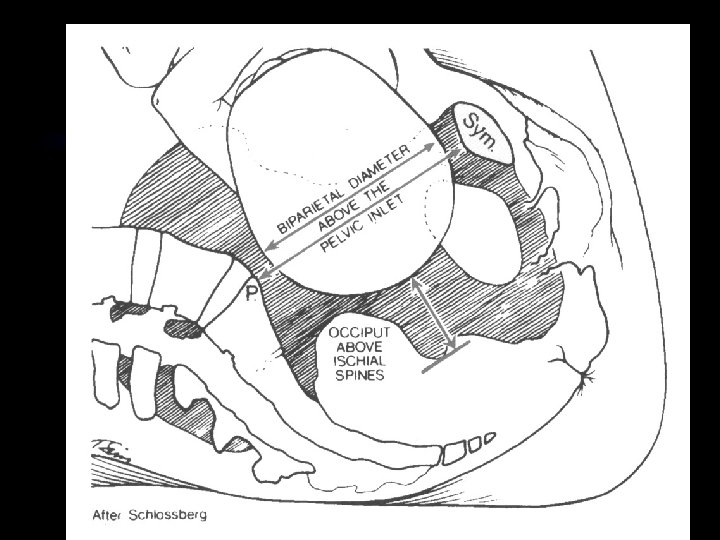
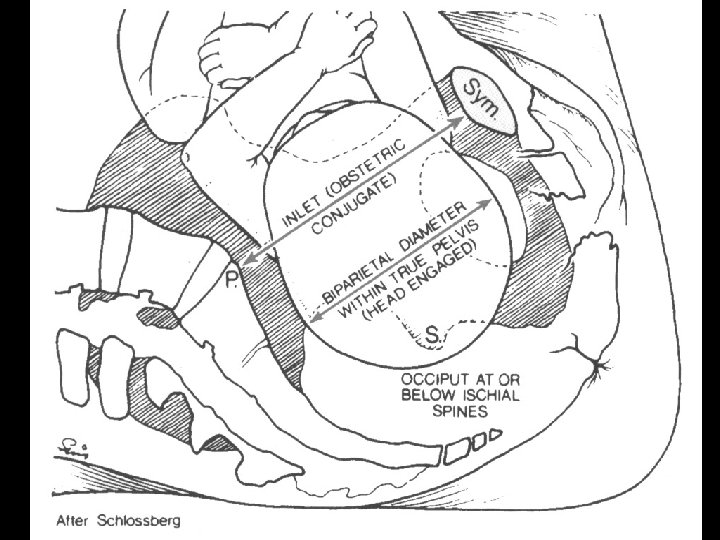
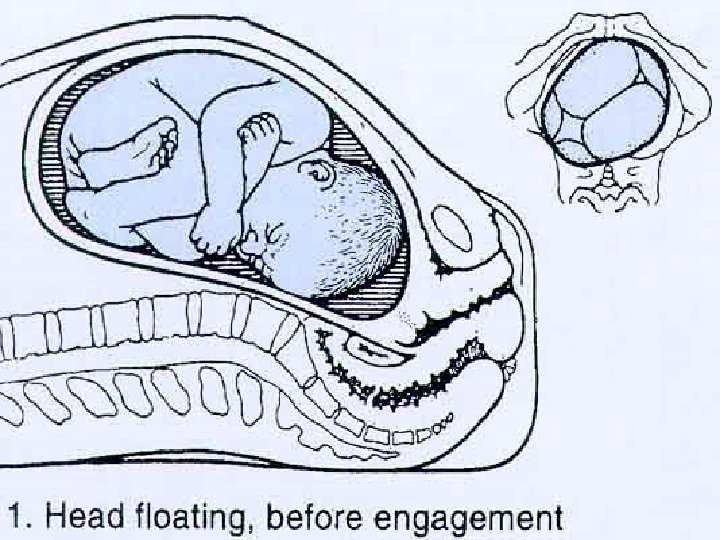
ENGAGEMENT • The biparietal diameter, the greatest transverse diameter of the fetal head in occiput presentations, passes through the pelvic inlet is designated engagement (during the last few weeks of pregnancy) • A normal – sized head usually does not engage with its sagittal suture directed anteroposteriorly. • Instead, the fetal head usually enters the pelvic inlet either in the transverse diameter or in one of the oblique diameters.
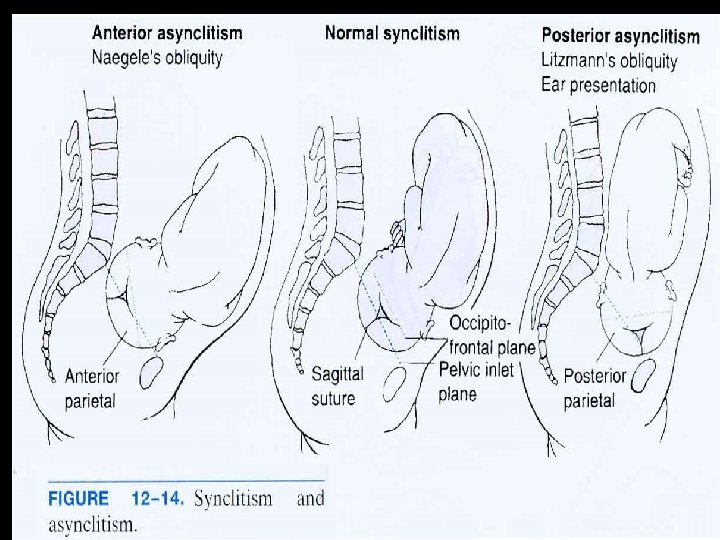
ASYNCLITISM • Although the fetal heads tends to accommodate to the transverse axis of the pelvic inlet, the sagittal suture , while remaining parallel to that axis, may not lie exactly midway between the symphysis and sacral promontory • The sagittal suture frequently is deflected either posteriorly toward the promontory or anteriorly toward the symphysis. • Such lateral deflection of the head to a more anterior or posterior position in the pelvis is called asynclitism • Moderate degrees of asynclitism are the rule in
DESCENT In nulliparas, engagement may take place before the onset of labor and further descent may not follow until the onset of second stage. In multiparous women, descent usually begins with engagement. Descent is brought about by one or more of four forces : • Pressure of the amniotic fluid • Direct pressure of the fundus upon the breech with contractions
- Slides: 50