THE BIOLOGIC WIDTH INTRODUCTION For restoration to survive
THE BIOLOGIC WIDTH

INTRODUCTION • For restoration to survive long term the periodontium must remain healthy so that teeth are maintained. • For the periodontium to remain healthy restoration must be critically maintained so that they are in harmony with their surrounding periodontal tissue. • To maintain and enhance the patient’s esthetic appearance the tooth-tissue interface must present a healthy natural appearance.
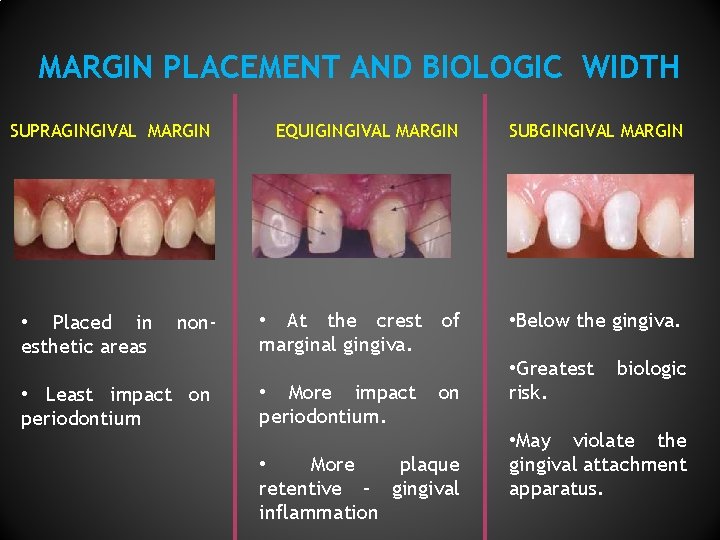
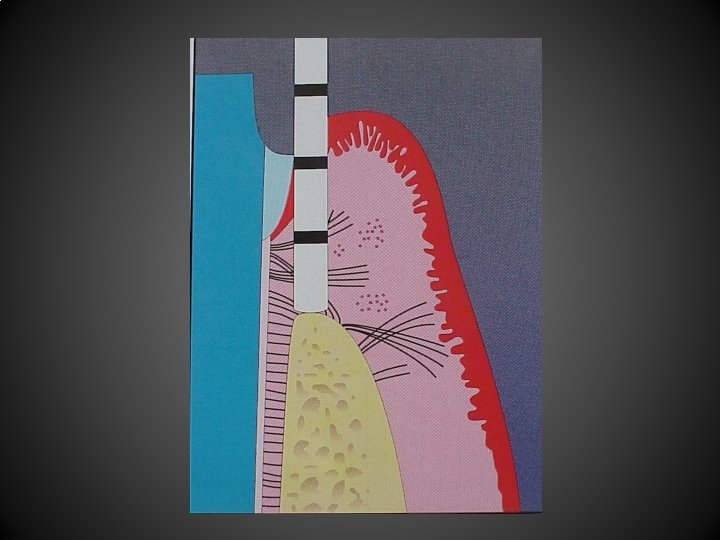
MARGIN PLACEMENT AND BIOLOGIC WIDTH SUPRAGINGIVAL MARGIN • Placed in esthetic areas non- • Least impact on periodontium EQUIGINGIVAL MARGIN SUBGINGIVAL MARGIN • At the crest of marginal gingiva. • Below the gingiva. • More impact periodontium. on • More plaque retentive – gingival inflammation • Greatest risk. biologic • May violate the gingival attachment apparatus.
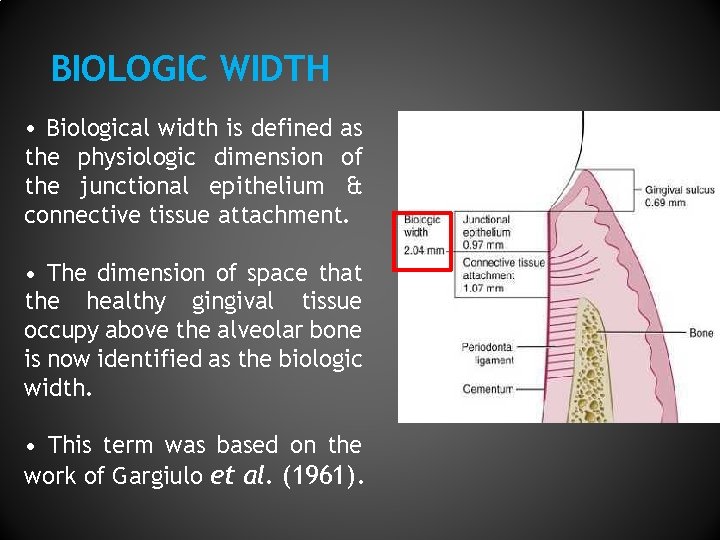
BIOLOGIC WIDTH • Biological width is defined as the physiologic dimension of the junctional epithelium & connective tissue attachment. • The dimension of space that the healthy gingival tissue occupy above the alveolar bone is now identified as the biologic width. • This term was based on the work of Gargiulo et al. (1961).
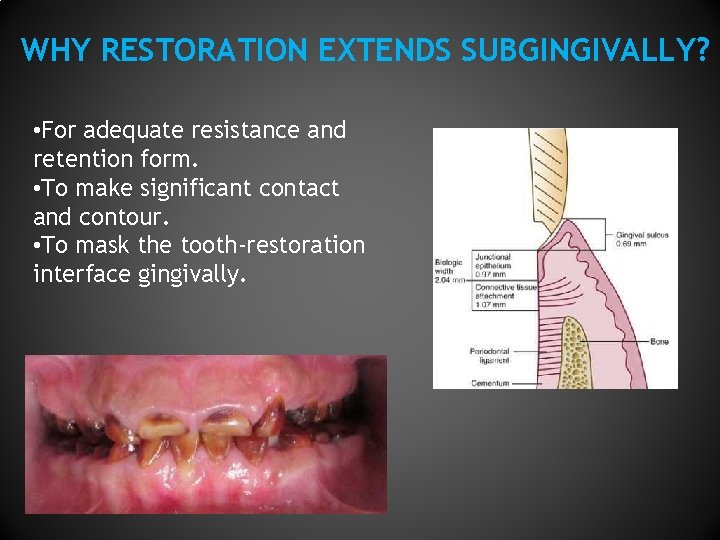
WHY RESTORATION EXTENDS SUBGINGIVALLY? • For adequate resistance and retention form. • To make significant contact and contour. • To mask the tooth-restoration interface gingivally.
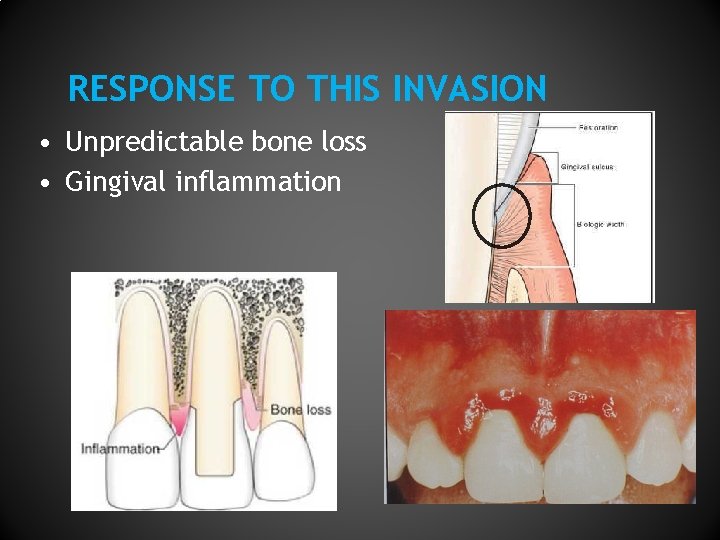
RESPONSE TO THIS INVASION • Unpredictable bone loss • Gingival inflammation
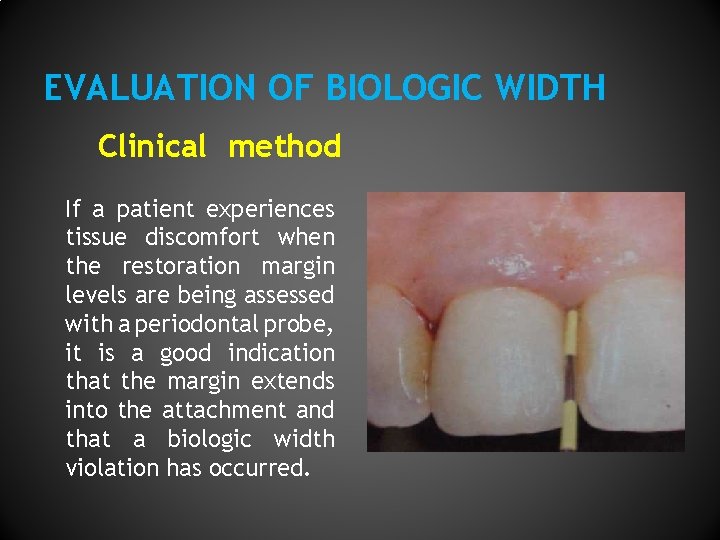
EVALUATION OF BIOLOGIC WIDTH Clinical method If a patient experiences tissue discomfort when the restoration margin levels are being assessed with a periodontal probe, it is a good indication that the margin extends into the attachment and that a biologic width violation has occurred.
Bone sounding The biologic width can be identified by probing under local anesthesia to the bone level (referred to as "sounding to bone") and subtracting the sulcus depth from the resulting measurement. If this distance is less than 2 mm at one or more locations, a diagnosis of biologic width violation can be confirmed. This measurement must be performed on teeth with healthy gingival tissues and should be repeated on more than one tooth to ensure accurate assessment, and reduce individual and site variations.
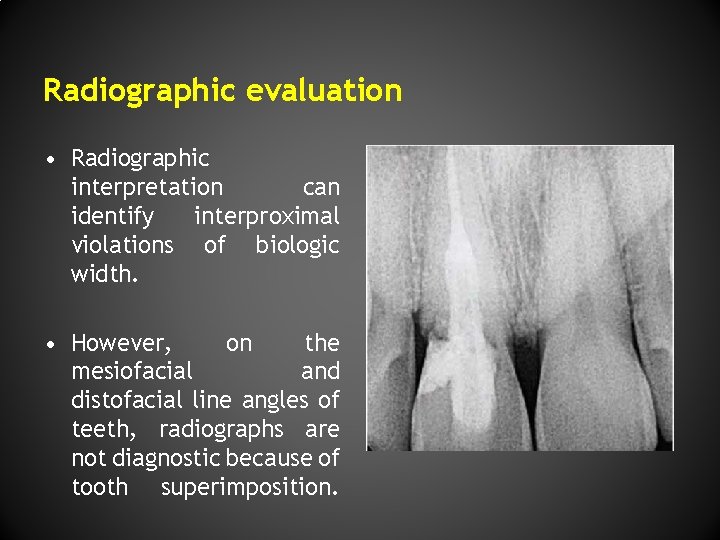
Radiographic evaluation • Radiographic interpretation can identify interproximal violations of biologic width. • However, on the mesiofacial and distofacial line angles of teeth, radiographs are not diagnostic because of tooth superimposition.

METHODS TO CORRECT BIOLOGIC WIDTH VIOLATION Can be corrected by— 1. Surgical crown lengthening 2. Orthodontic technique
SURGICAL CROWN LENGTHENING Indications • Subgingival caries or fracture • Inadequate clinical crown length for retention • Unequal or unesthetic gingival heights Contraindications • Surgery would create an unesthetic outcome. • Deep caries or fracture would require excessive bone removal on contiguous teeth. • The tooth with a poor restorative risk.
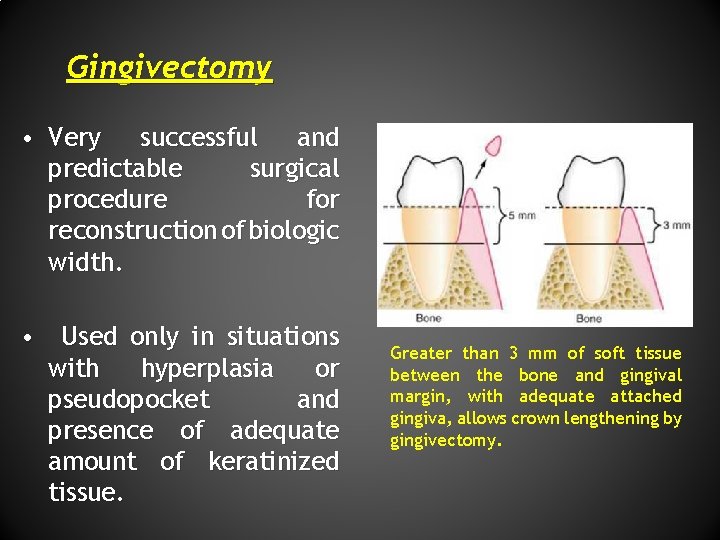
Gingivectomy • Very successful and predictable surgical procedure for reconstruction of biologic width. • Used only in situations with hyperplasia or pseudopocket and presence of adequate amount of keratinized tissue. Greater than 3 mm of soft tissue between the bone and gingival margin, with adequate attached gingiva, allows crown lengthening by gingivectomy.
Apically repositioned flap surgery • Indication Crown lengthening of multiple teeth in a quadrant or sextant of the dentition, root caries, fractures. • Contraindication Apical repositioned flap surgery should not be used during surgical crown lengthening of a single tooth in the esthetic zone.
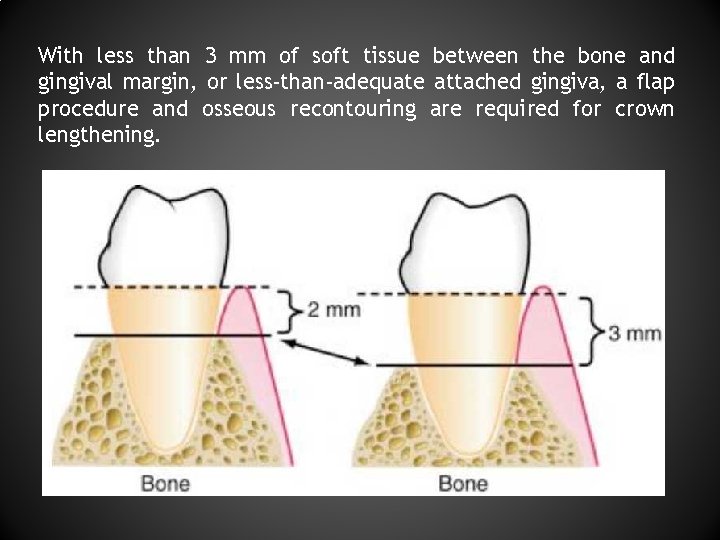
With less than 3 mm of soft tissue between the bone and gingival margin, or less-than-adequate attached gingiva, a flap procedure and osseous recontouring are required for crown lengthening.
Apically repositioned flap without osseous resection Indication: When there is no adequate width of attached gingiva, and there is a biologic width of more than 3 mm on multiple teeth. Apically repositioned flap with osseous reduction Indication: When there is no adequate zone of attached gingiva and the biologic width is less than 3 mm. The alveolar bone is reduced by ostectomy and osteoplasty. As a general rule, at least 4 mm of sound tooth structure must be exposed, so that the soft tissue will proliferate coronally to cover 2 -3 mm of the root, thereby leaving only 12 mm of supragingivally located sound tooth structure.
ORTHODONTIC TECHNIQUES The extrusion can be performed in two ways. 1) Low orthodontic extrusion force: The tooth is erupted slowly, bringing the alveolar bone and gingival tissue with it. The tooth is extruded until the bone level has been carried coronal to the ideal level by the amount that will need to be removed surgically to correct the attachment violation. The tooth is stabilized in this new position and then is treated with surgery to correct the bone and gingival tissue levels.
2) Rapid orthodontic extrusion : The tooth is erupted to the desired amount over several weeks. During this period, a supercrestal fiberotomy is performed weekly in an effort to prevent the tissue and bone from following the tooth. The tooth is then stabilized for at least 12 weeks to confirm the position of the tissue and bone, and any coronal creep can be corrected surgically.
HEALING AFTER CROWN LENGTHENING Restorative procedures must be delayed until new gingival crevice develops after periodontal surgery. In non-esthetic areas : 6 weeks healing period post surgically prior to final restorative procedures is recommended. In esthetic areas: A longer healing period recommended to prevent recession (4 - 6 months). is The margin of the provisional restoration should not hinder healing before the biologic width is established by surgical procedures.
CONCLUSION The health of the periodontal tissues is dependent on properly designed restorations. It is preferable to give supragingival margins in a restoration. But subgingival margin placement is often unavoidable. If restorative margins need to be placed near the alveolar crest, crown-lengthening surgery or orthodontic extrusion should be considered to provide adequate tooth structure while simultaneously assuring the integrity of the biologic width. Although individual variations exist in the soft tissue attachment around teeth, a minimum of 3 mm should exist from the restorative margin to the alveolar bone, allowing for 2 mm of biologic width space and 1 mm for sulcus depth.

Thank You
- Slides: 21