The ASA Difficult Airway Algorithm New Thoughts and
- Slides: 23
The ASA Difficult Airway Algorithm: New Thoughts and Considerations Chen, Chien-Yu June 8, 2001
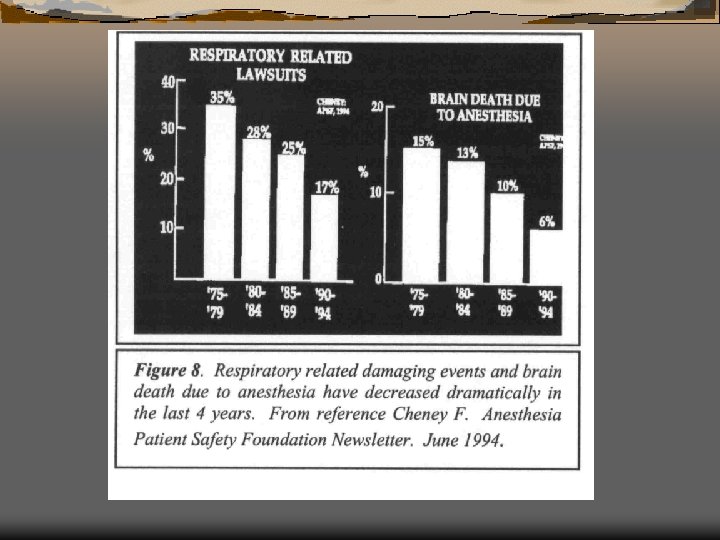
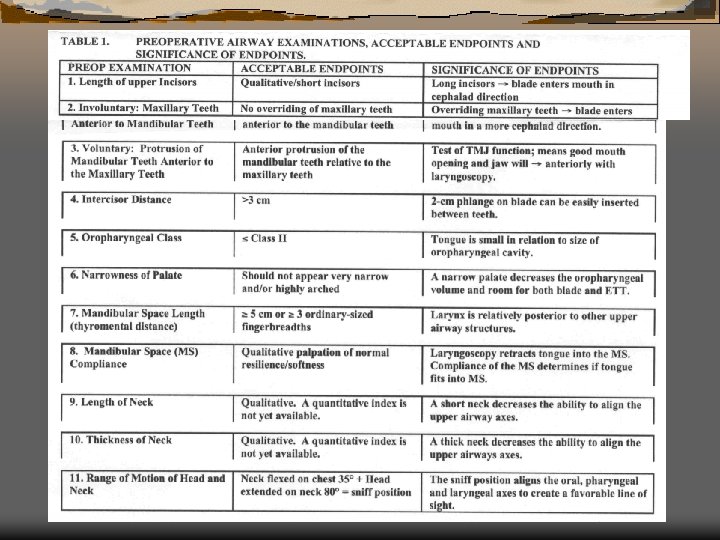
Introduction and Recognition Of A Difficult Airway Ü ASA difficult airway algorithm ( from Anesthesiology 1993, 1996) Ü Pre-op airway evaluation: The more predictors used, the better the prediction
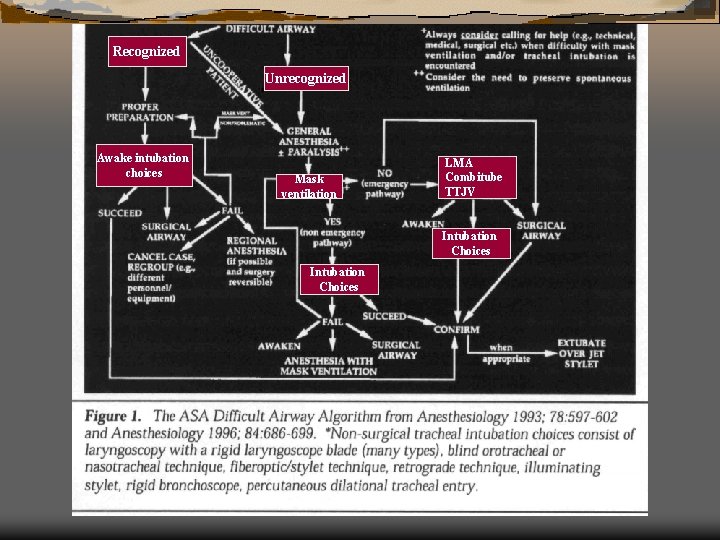
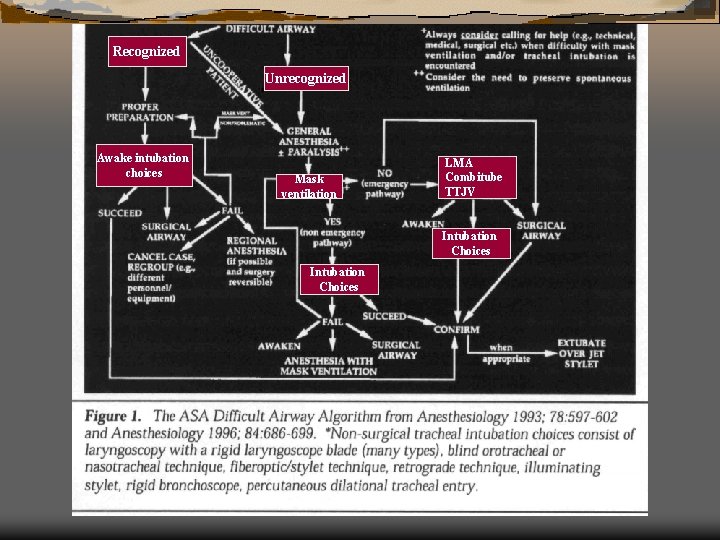
Recognized Unrecognized Awake intubation choices Mask ventilation LMA Combitube TTJV Intubation Choices
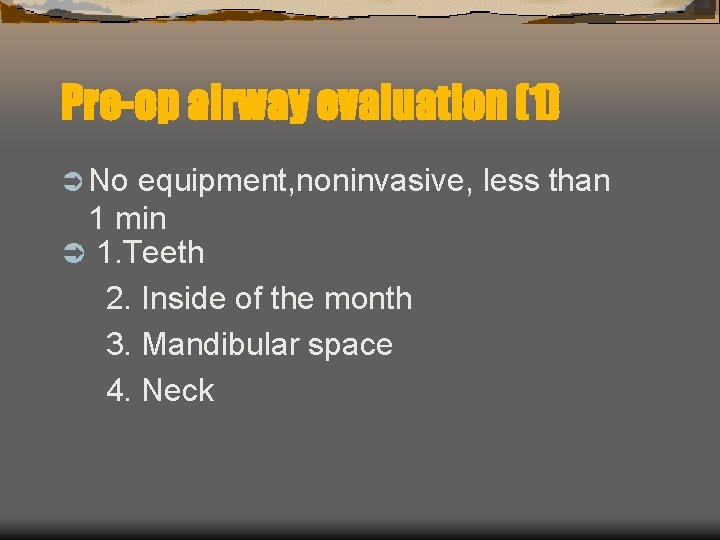
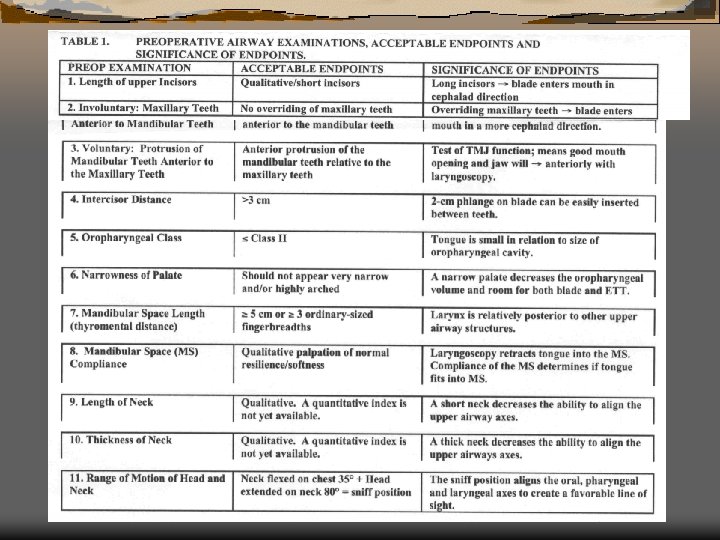
Pre-op airway evaluation (1) Ü No equipment, noninvasive, less than 1 min Ü 1. Teeth 2. Inside of the month 3. Mandibular space 4. Neck
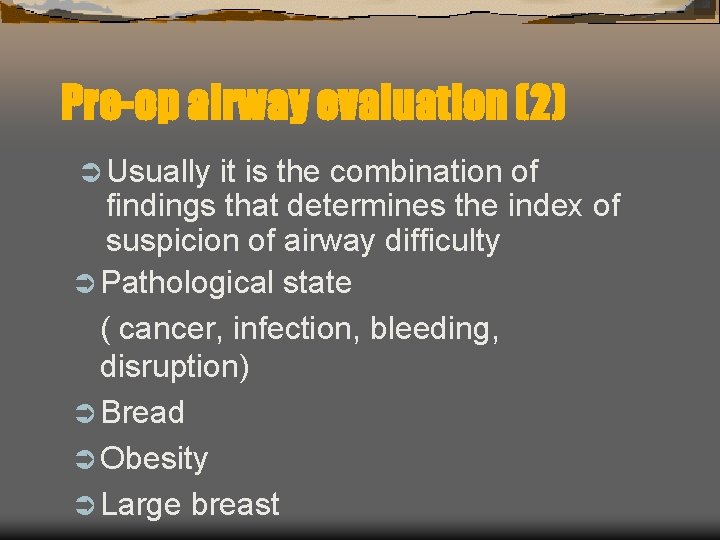
Pre-op airway evaluation (2) Ü Usually it is the combination of findings that determines the index of suspicion of airway difficulty Ü Pathological state ( cancer, infection, bleeding, disruption) Ü Bread Ü Obesity Ü Large breast
Recognized difficult airwayawake limb of algorithm (1) Ü Difficult airway (DA) Awake Intubation
Recognized difficult airwayawake limb of algorithm (2) Ü Proper preparation is the most important determination of the success of an awake intubation Ü Psychological support Ü Use of drying agent Ü Titrated sedation Ü Vasoconstriction Ü Nerve block
Recognized difficult airwayawake limb of algorithm (3) Ü Very occasionally awake intubation may fail due to either lack of p’t cooperation, equipment and operator Ü limitation Fail of awake intubate: Re-prepare Cancel the op GA Regional anesthesia Surgical airway
Recognized difficult airwayawake limb of algorithm (4) Ü Surgical airway first choice Laryngeal/ tracheal disruption Upper airway abscess Mandibular-maxillary fracture
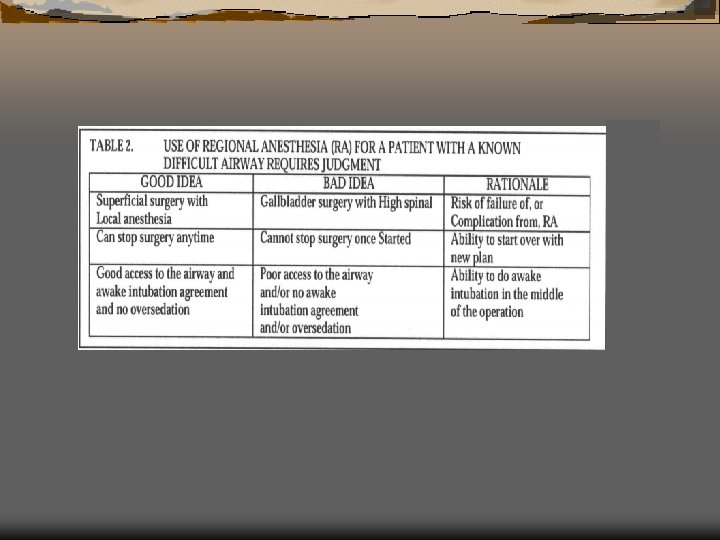
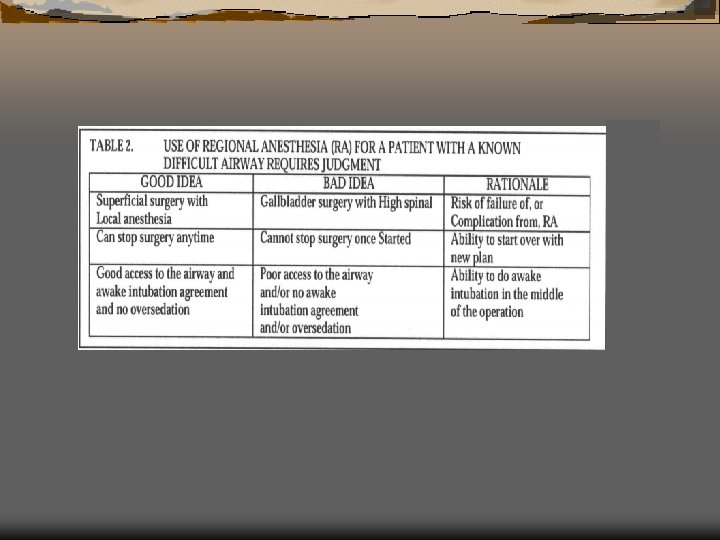
Recognized difficult airwayawake limb of algorithm (5) Ü Use of regional anesthesia in a patient with a known difficult airway requires a high degree of judgment
Unrecognized difficult airway (1) ventilation nonemergency pathway Ü 考慮是否使用conventional laryngoscopy 缺點: edema, bleeding 惡化mask ventilation and intubation CVCI Plan B Ü Mask
Unrecognized difficult airway (2) Ü Definition of optimal intubation attempt reasonably experienced endoscopist: 2 -3 yrs no significant muscle tone optimal sniff position optimal external laryngeal pressure change length of blade*1 change type of blade*1
Unrecognized difficult airway (3) Ü Macintosh blade-small narrow month, palate, oropharynx Ü Miller blade-small mandibular space, large incisors, long floppy epiglottis
Unrecognized difficult airway (4) Ü DA 又可定義 laryngoscope use > 3 attempts and/or > 10 min Ü Laryngoscope fail 後的choices fiberoptic intubation, LMA, airway intubator mask ventilation awaken or surgical airway
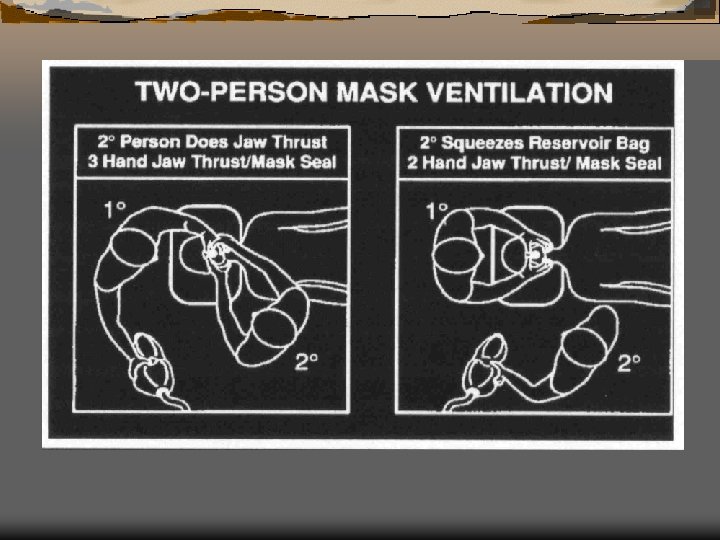
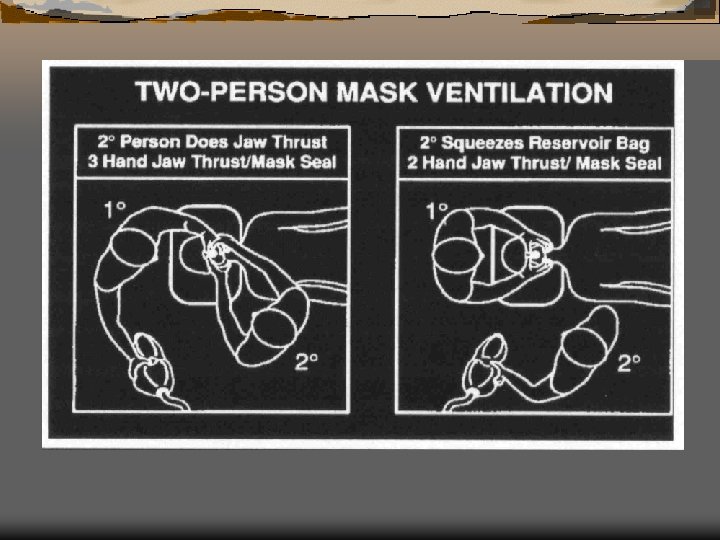
CVCI (1) Ü 2 persons effort: Better mask seal Jaw thrust Better tidal volume Ü Large oral pharyngeal, nasopharyngeal airways
CVCI (2) Ü The decision to abandon mask ventilation should be made after the anesthesiologist has made an optimal/best attempt at mask ventilation
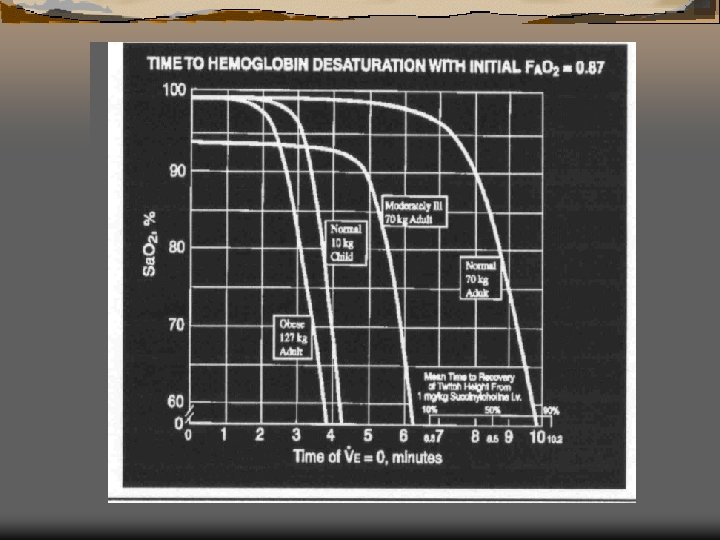
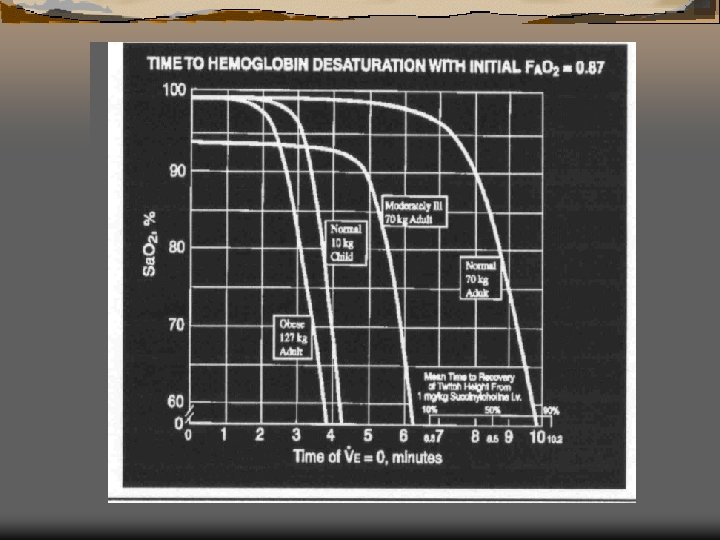
CVCI (3) Ü 8. 5 min fully preoxygenated, p‘t 也會hypoxemic, dead 給 1 mg/kg SCC, 50% recovery Ü P’t will die before SCC wear off Ü awaken option 0. 5 -0. 7 mg/kg
CVCI (4) Ü LMA or Combitube-conduit for fiberscope work as ventilatory mechanism few complications inserted blindly, quickly, low level of skill can’t solve glottic, subglottic problems Ü TTJV-barotrauma