The approach to the critically ill patient Assessment



- Slides: 56
The approach to the critically ill patient Assessment of the Critically Ill Patient Nick Smith Clinical Skills Khaled M. Hassan MD; 2011
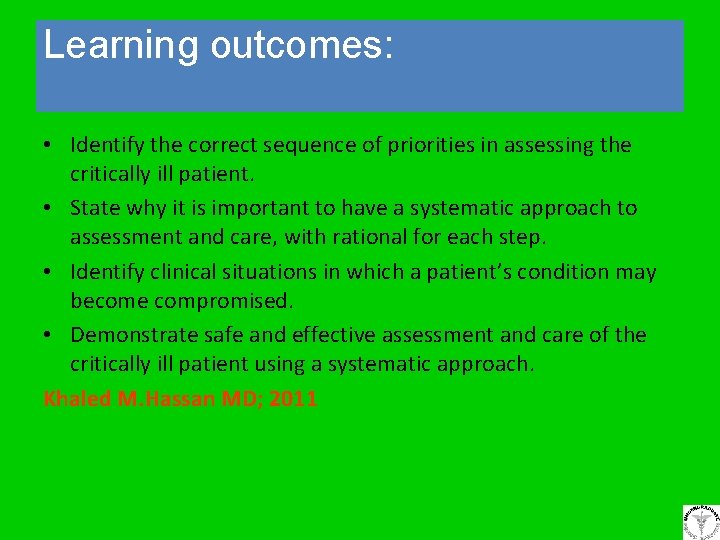
Learning outcomes: • Identify the correct sequence of priorities in assessing the critically ill patient. • State why it is important to have a systematic approach to assessment and care, with rational for each step. • Identify clinical situations in which a patient’s condition may become compromised. • Demonstrate safe and effective assessment and care of the critically ill patient using a systematic approach. Khaled M. Hassan MD; 2011
IS IT IMPORTANT TO ASSESS? • Assessment is the first step in Caring for a patient, and assessing the critically ill patient is an essential part of their care. • Careful assessment is fundamental in order to recognise when a patient is becoming compromised. • The nurse acts as patient advocate, monitoring, anticipating potential problems, planning, implementing and constantly evaluating care, and communicating with other MDT; multidisciplinary team; staff involved in the patient care. Khaled M. Hassan MD; 2011

The Multidisciplinary Team )MDT( • The MDT brings together people who are experts in different areas of medicine and care, and usually meet every week to discuss the diagnosis, treatment and care of individual patients. The Team is responsible for : • Working out your treatment plan • Deciding on further tests • Making appropriate referrals to specialist services • Making sure the team has all the necessary members • Collecting information and keeping good records. Khaled M. Hassan MD. 2011
Patient Assessment Systems • Basic Life support (BLS) • Advanced Life Support (ALS) • Acute Life-threatening Events, Recognition and Treatment (ALERT) • The Advanced Trauma Life Support (ATLS) Khaled M. Hassan MD; 2011
All of these assessment systems use a systematic approach in a strict order: • • • A: airway (with C-spine protection in trauma) B: breathing C: circulation D: deficits in neurological status E: environment (exposure) Khaled M. Hassan MD; 2011
Objectives • • • The rational of ABCDE The process of primary & secondary survey Recognition of life threatening events Treatment of life-threatening conditions Handover Khaled M. Hassan MD; 2011
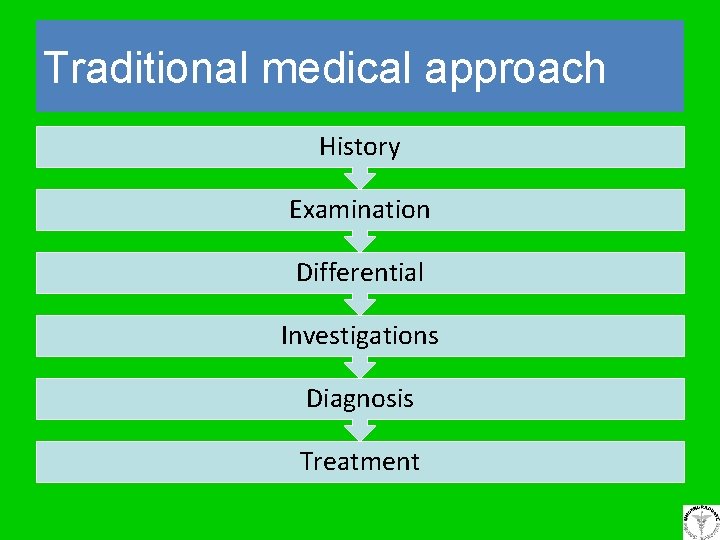
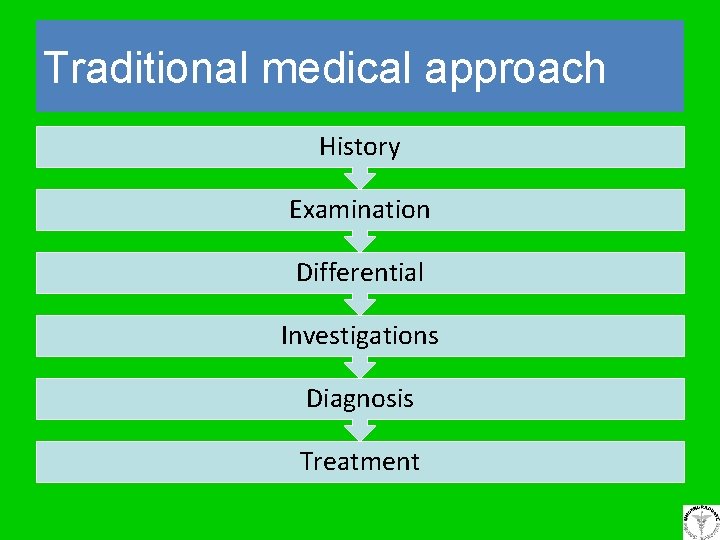
Traditional medical approach History Examination Differential Investigations Diagnosis Treatment
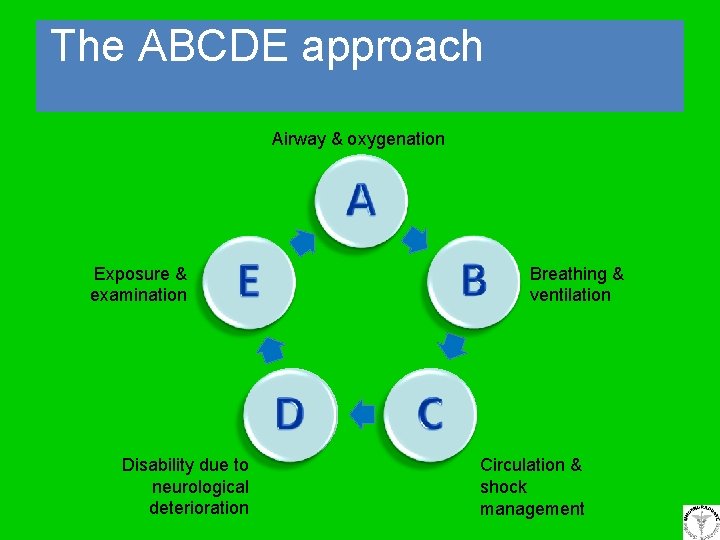
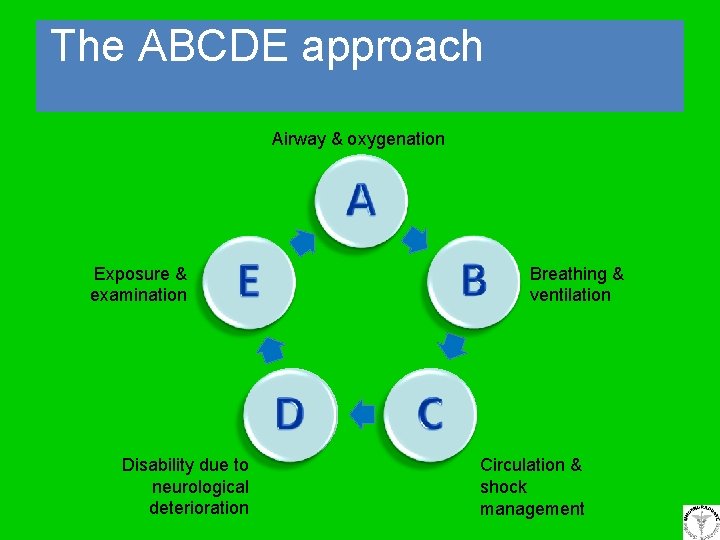
The ABCDE approach Airway & oxygenation A Exposure & examination E B D Disability due to neurological deterioration Breathing & ventilation C Circulation & shock management
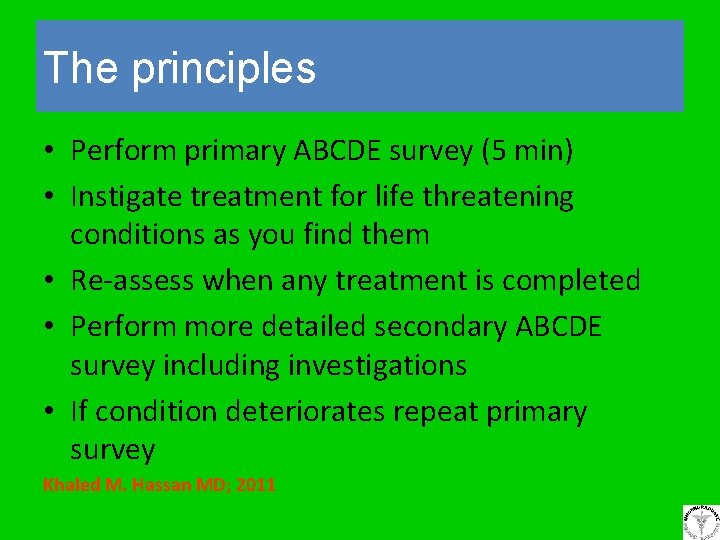
The principles • Perform primary ABCDE survey (5 min) • Instigate treatment for life threatening conditions as you find them • Re-assess when any treatment is completed • Perform more detailed secondary ABCDE survey including investigations • If condition deteriorates repeat primary survey Khaled M. Hassan MD; 2011
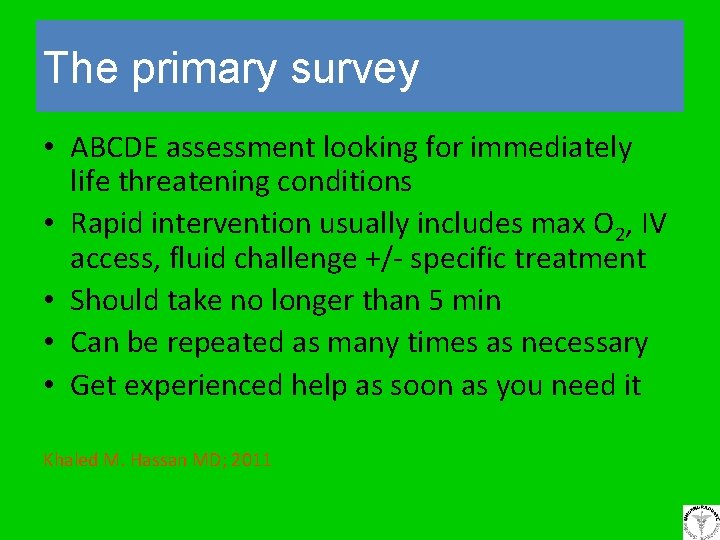
The primary survey • ABCDE assessment looking for immediately life threatening conditions • Rapid intervention usually includes max O 2, IV access, fluid challenge +/- specific treatment • Should take no longer than 5 min • Can be repeated as many times as necessary • Get experienced help as soon as you need it Khaled M. Hassan MD; 2011
The secondary survey • • Performed when patient more stable More detailed examination of patient (ABCDE) Order investigations to aid diagnosis IF PATIENT DETERIORATES RETURN TO PRIMARY SURVEY Khaled M. Hassan MD; 2011
Airway • How do we assess airway and why? Khaled M. Hassan MD; 2011
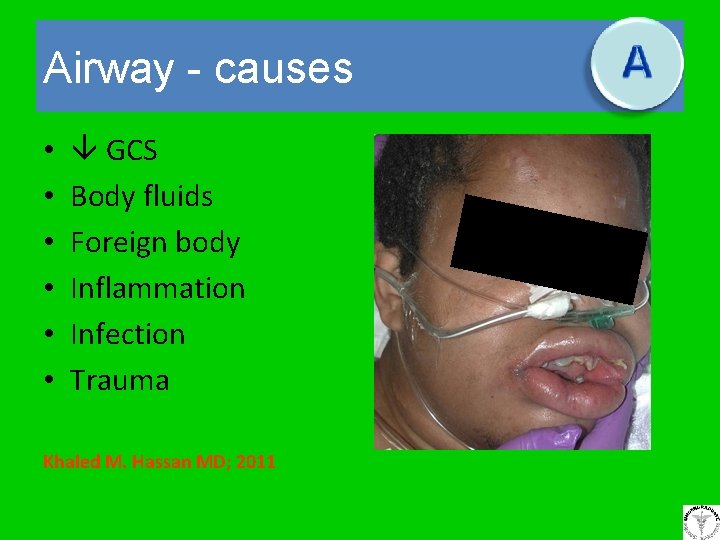
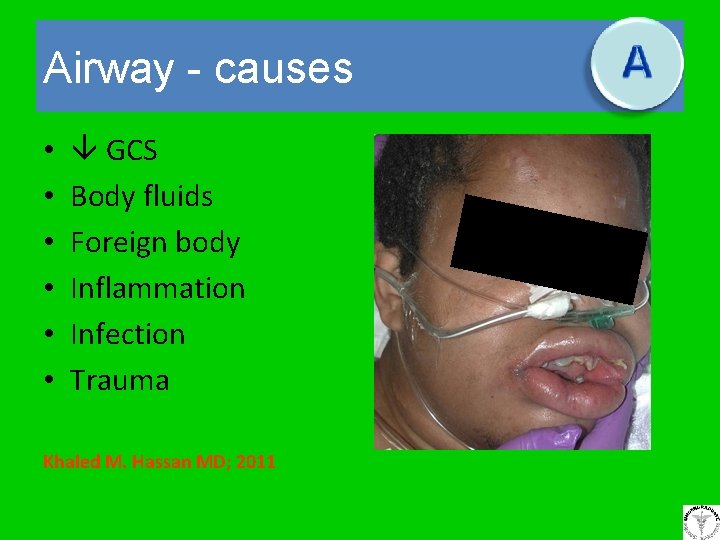
Airway - causes • • • GCS Body fluids Foreign body Inflammation Infection Trauma Khaled M. Hassan MD; 2011
Airway - assessment • Unresponsive • Added sounds – Snoring, gurgling, wheeze, stridor • Tracheal tug • Accessory muscles • See-saw respiratory pattern Khaled M. Hassan MD; 2011
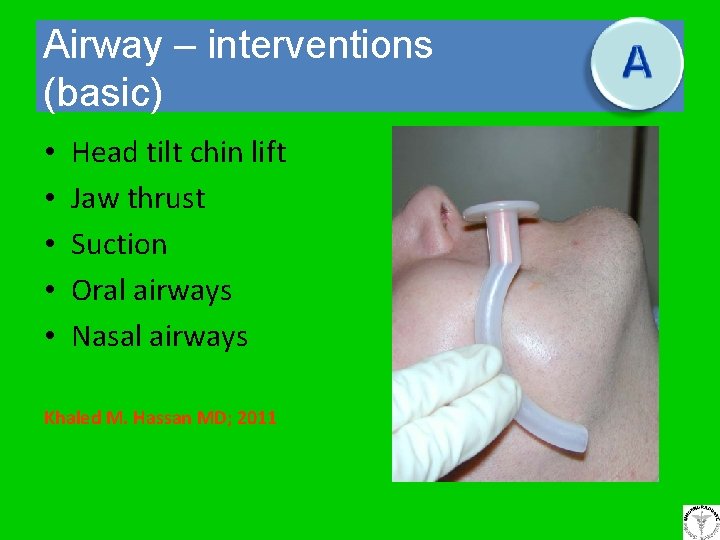
Airway – interventions (basic) • • • Head tilt chin lift Jaw thrust Suction Oral airways Nasal airways Khaled M. Hassan MD; 2011
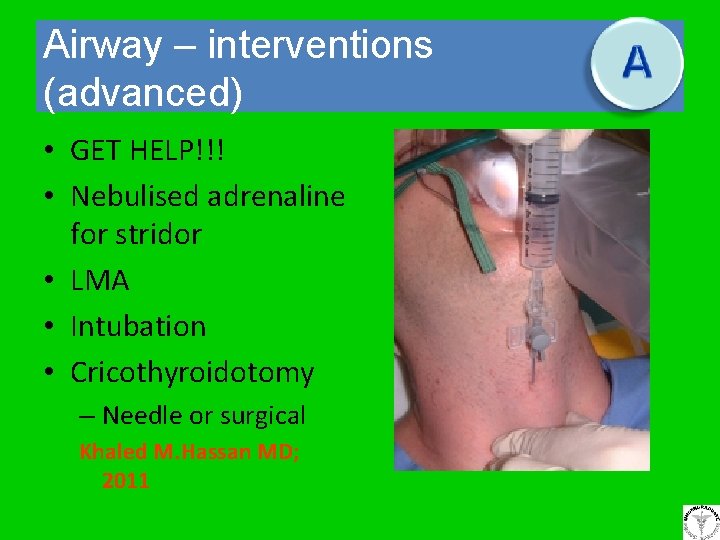
Airway – interventions (advanced) • GET HELP!!! • Nebulised adrenaline for stridor • LMA • Intubation • Cricothyroidotomy – Needle or surgical Khaled M. Hassan MD; 2011
Once airway open. . . • Give 15 litres of oxygen to all patients via a nonrebreathing mask • For COPD patients re -assess after the primary survey has been complete & keep Sats 90 -93% Khaled M. Hassan MD; 2011
Breathing • Why do we assess breathing and how do we carry out a comprehensive respiratory assessment? Khaled M. Hassan MD; 2011
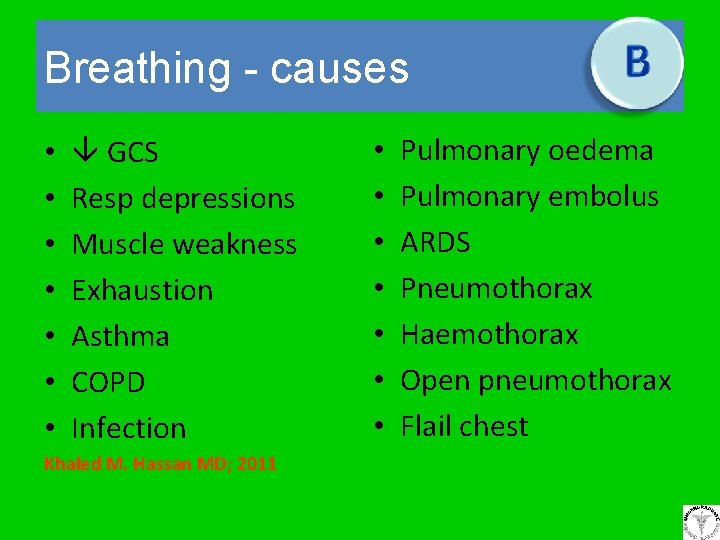
Breathing - causes • • GCS Resp depressions Muscle weakness Exhaustion Asthma COPD Infection Khaled M. Hassan MD; 2011 • • Pulmonary oedema Pulmonary embolus ARDS Pneumothorax Haemothorax Open pneumothorax Flail chest
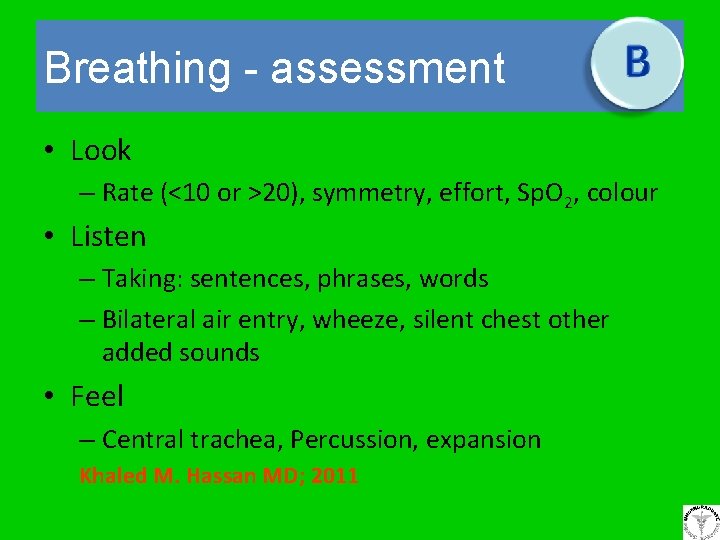
Breathing - assessment • Look – Rate (<10 or >20), symmetry, effort, Sp. O 2, colour • Listen – Taking: sentences, phrases, words – Bilateral air entry, wheeze, silent chest other added sounds • Feel – Central trachea, Percussion, expansion Khaled M. Hassan MD; 2011
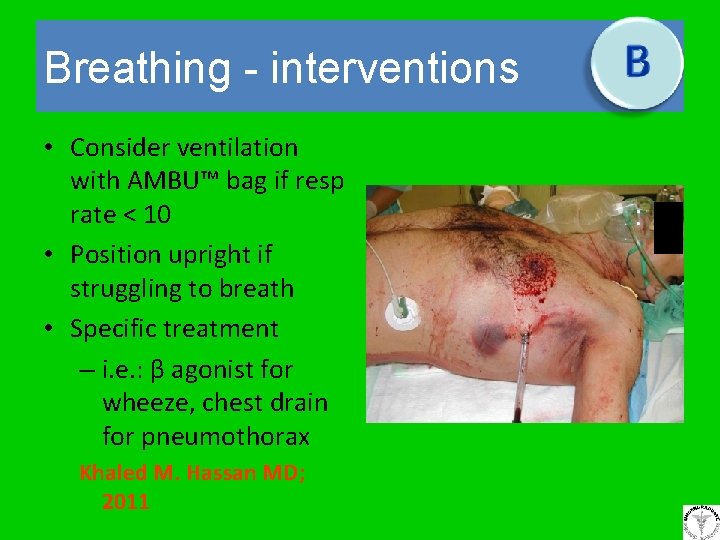
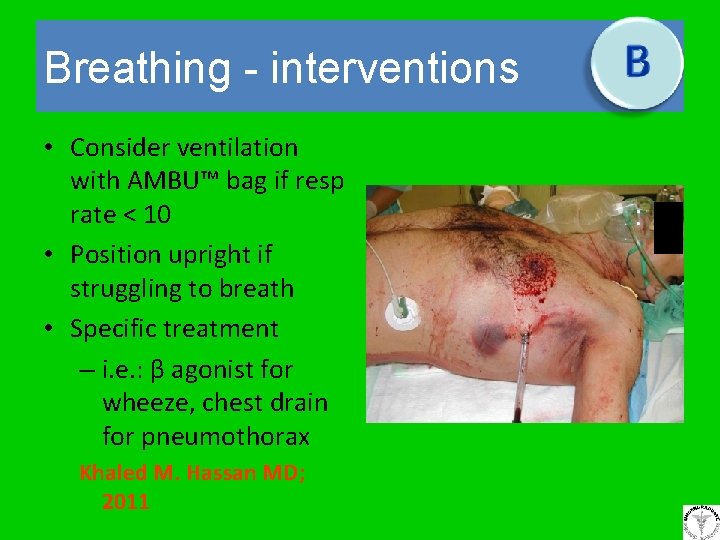
Breathing - interventions • Consider ventilation with AMBU™ bag if resp rate < 10 • Position upright if struggling to breath • Specific treatment – i. e. : β agonist for wheeze, chest drain for pneumothorax Khaled M. Hassan MD; 2011
Circulation • What is the significance of circulation and how do we assess the patient? Khaled M. Hassan MD; 2011
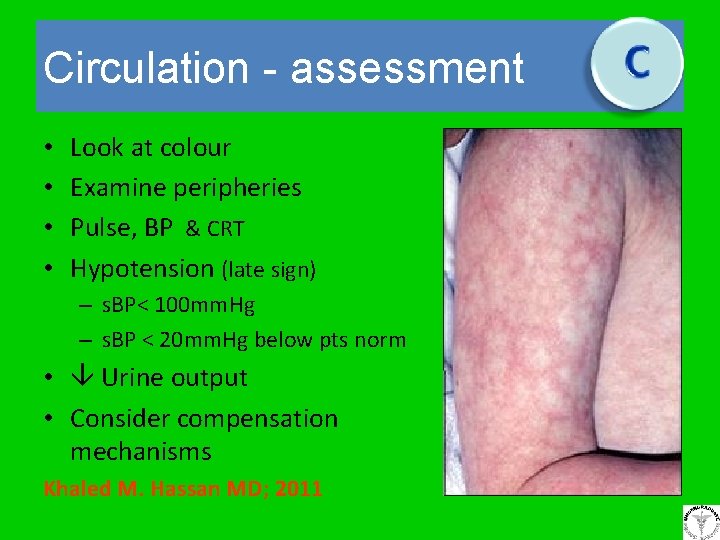
Circulation - assessment • • Look at colour Examine peripheries Pulse, BP & CRT Hypotension (late sign) – s. BP< 100 mm. Hg – s. BP < 20 mm. Hg below pts norm • Urine output • Consider compensation mechanisms Khaled M. Hassan MD; 2011
Circulation – shock Inadequate tissue perfusion • Loss of volume – Hypovolaemia • Pump failure – Myocardial & nonmyocardial causes • Vasodilatation – Sepsis, anaphylaxis, neurogenic BP = HR x SVR Khaled M. Hassan MD; 2011
Circulation - interventions • Position supine with legs raised – Left lateral tilt in pregnancy • IV access - 16 G or larger x 2 – +/- bloods if new cannula • Fluid challenge – colloid or crystalloid? • ECG Monitoring • Specific treatment Khaled M. Hassan MD; 2011
Central Venous Pressure • Involves insertion of a line to a major vein e. g. subclavian, internal jugular under full aseptic technique. • Patient is placed in supine or Trendelenburg position – promotes venous filling, aids catheter placement and reduces risk of air embolism. • Following insertion a check x-ray is required to confirm position and absence of pneumothorax. Khaled M. Hassan MD; 2011
CVP (contd. ) • It is a direct measurement of pressure within the right atrium. • Readings should not be used in isolation, but as part of full haemodynamic assessment. • Used as a guide in fluid replacement. • Used to establish deficits in blood volume. • Used for drug administration, maintaining nutrition (TPN) Khaled M. Hassan MD; 2011
CVP (contd. ) • What is the nursing management of CVP lines Khaled M. Hassan MD; 2011
Deficits in neurological status & environment (exposure) • How will you assess neurological status and environment? Khaled M. Hassan MD; 2011
Disability - causes • • • Inadequate perfusion of the brain Sedative side effects of drugs BM Toxins and poisons CVA ICP Khaled M. Hassan MD; 2011
Disability - assessment • AVPU (or GCS) – Alert, responds to Voice, responds to Pain, Unresponsive • • Pupil size/response Posture BM Pain relief Khaled M. Hassan MD; 2011
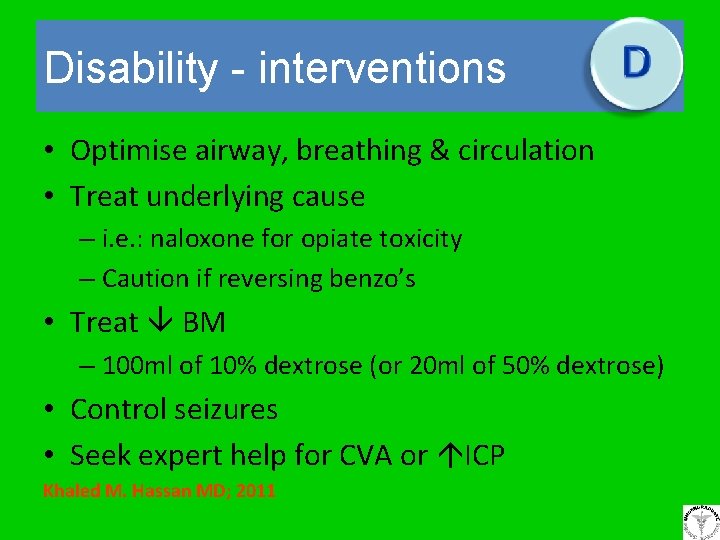
Disability - interventions • Optimise airway, breathing & circulation • Treat underlying cause – i. e. : naloxone for opiate toxicity – Caution if reversing benzo’s • Treat BM – 100 ml of 10% dextrose (or 20 ml of 50% dextrose) • Control seizures • Seek expert help for CVA or ICP Khaled M. Hassan MD; 2011
Exposure • Remove clothes and examine head to toe front and back – Haemorrhage (inc concealed), rashes, swelling etc • Keep warm (unless post cardiac arrest) • Maintain dignity Khaled M. Hassan MD; 2011
Secondary survey • Repeat ABCDE in more detail • History • Order investigations – ABG, CXR, 12 lead ECG, Specific bloods • Management plan • Referral • Handover Khaled M. Hassan MD; 2011
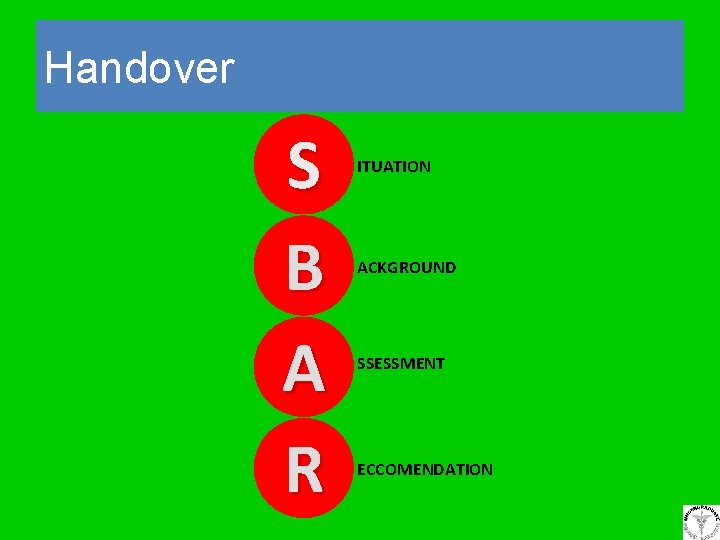
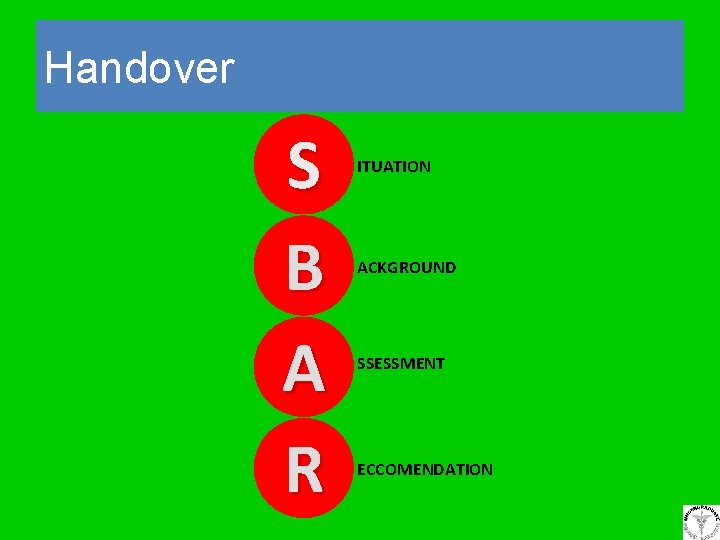
Handover S B A R ITUATION ACKGROUND SSESSMENT ECCOMENDATION
Situation • • Check you are talking o the right person State your name & department I am calling about. . . (patient) The reason I am calling is. . . Khaled M. Hassan MD; 2011 S

Background B • Admission diagnosis and date of admission • Relevant medical history • Brief summary of treatment to date Khaled M. Hassan MD; 2011
Assessment • The assessment of the patient using the ABCDE approach Khaled M. Hassan MD; 2011 A
Current practice in critical care services • Development of outreach services from critical care specialists to support ward staff in managing patients at risk. • Improved patient monitoring through the use of early warning scores (EWS) or modified early warning scores (MEWS) Khaled M. Hassan MD; 2011
Recommendation • • R I would like you to. . . Determine the time scale Is there anything else I should do? Record the name and contact number of your contact Khaled M. Hassan MD; 2011
Questions ?
Summary • Assess ABCDE in turn • Instigate treatments for life-threatening problems as you find them • Reassess following treatment • If anything changes go back to A Khaled M. Hassan MD; 2011
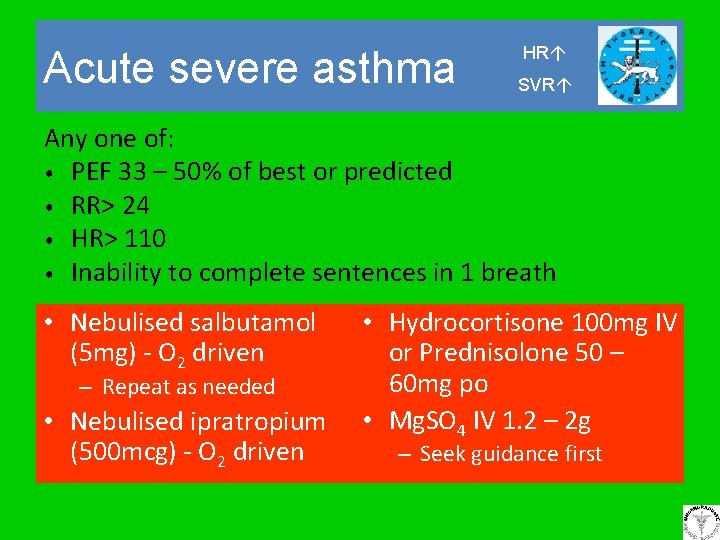
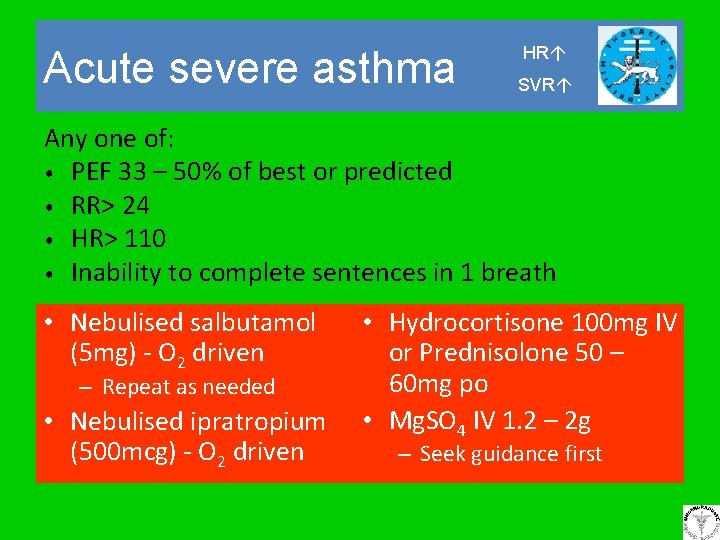
Acute severe asthma HR SVR Any one of: • PEF 33 – 50% of best or predicted • RR> 24 • HR> 110 • Inability to complete sentences in 1 breath • Nebulised salbutamol (5 mg) - O 2 driven – Repeat as needed • Nebulised ipratropium (500 mcg) - O 2 driven • Hydrocortisone 100 mg IV or Prednisolone 50 – 60 mg po • Mg. SO 4 IV 1. 2 – 2 g – Seek guidance first
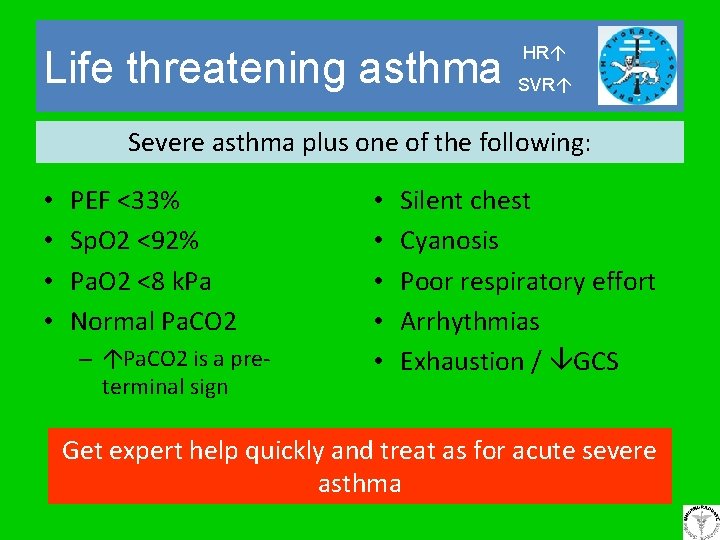
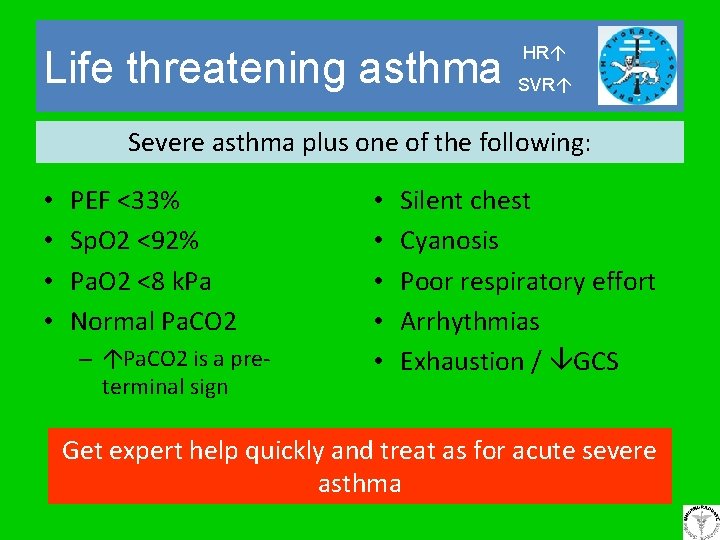
Life threatening asthma HR SVR Severe asthma plus one of the following: • • PEF <33% Sp. O 2 <92% Pa. O 2 <8 k. Pa Normal Pa. CO 2 – Pa. CO 2 is a preterminal sign • • • Silent chest Cyanosis Poor respiratory effort Arrhythmias Exhaustion / GCS Get expert help quickly and treat as for acute severe asthma
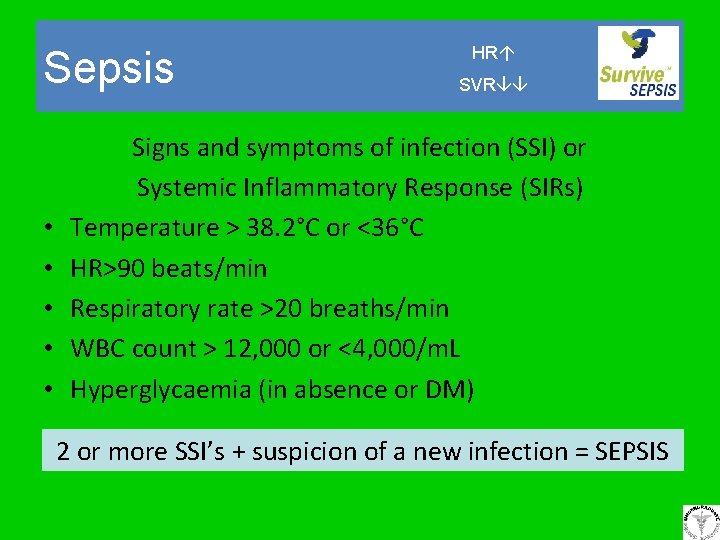
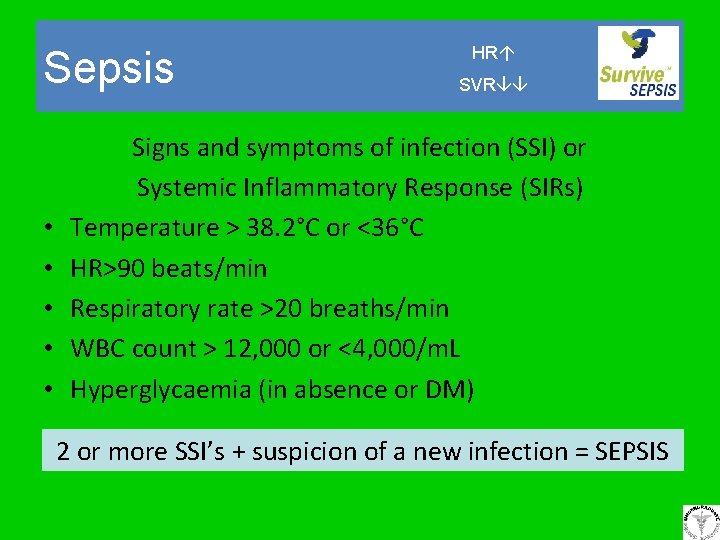
Sepsis • • • HR SVR Signs and symptoms of infection (SSI) or Systemic Inflammatory Response (SIRs) Temperature > 38. 2°C or <36°C HR>90 beats/min Respiratory rate >20 breaths/min WBC count > 12, 000 or <4, 000/m. L Hyperglycaemia (in absence or DM) 2 or more SSI’s + suspicion of a new infection = SEPSIS
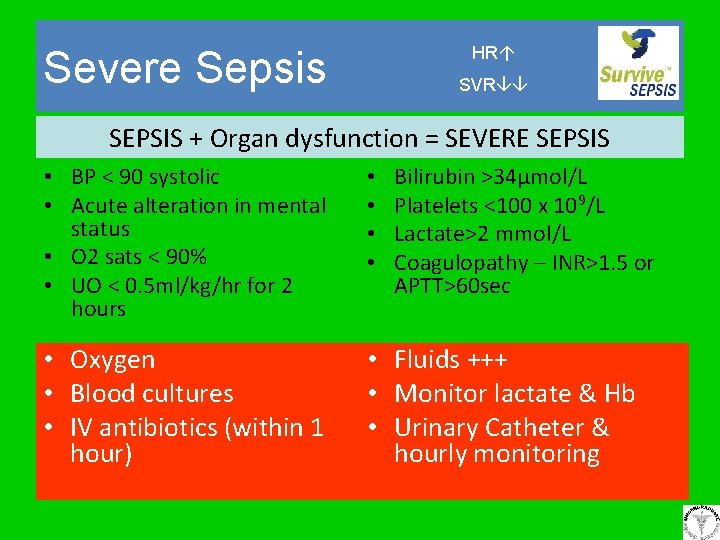
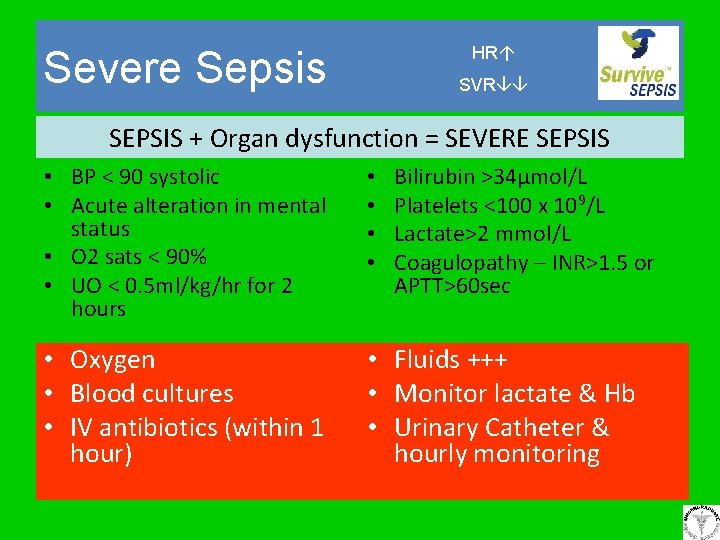
HR Severe Sepsis SVR SEPSIS + Organ dysfunction = SEVERE SEPSIS • BP < 90 systolic • Acute alteration in mental status • O 2 sats < 90% • UO < 0. 5 ml/kg/hr for 2 hours • • Bilirubin >34µmol/L Platelets <100 x 109/L Lactate>2 mmol/L Coagulopathy – INR>1. 5 or APTT>60 sec • Oxygen • Blood cultures • IV antibiotics (within 1 hour) • Fluids +++ • Monitor lactate & Hb • Urinary Catheter & hourly monitoring
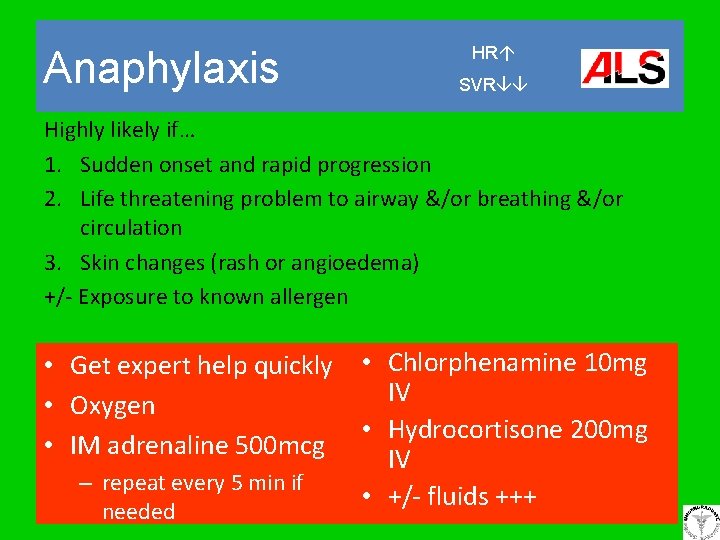
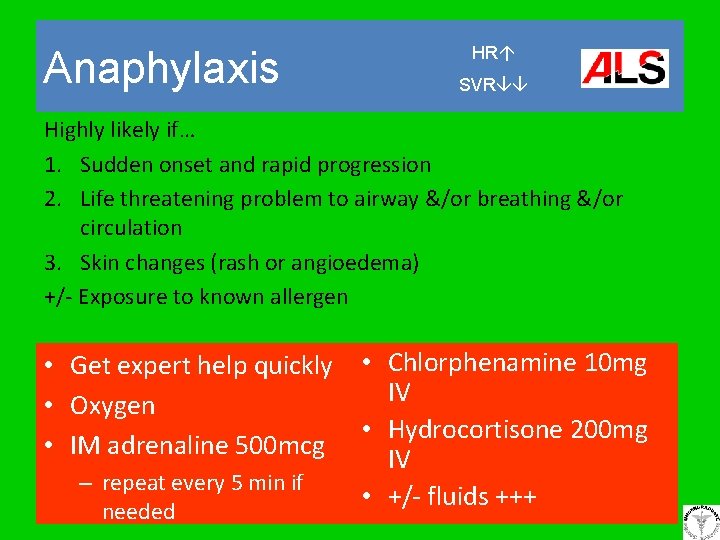
Anaphylaxis HR SVR Highly likely if… 1. Sudden onset and rapid progression 2. Life threatening problem to airway &/or breathing &/or circulation 3. Skin changes (rash or angioedema) +/- Exposure to known allergen • Get expert help quickly • Chlorphenamine 10 mg IV • Oxygen • Hydrocortisone 200 mg • IM adrenaline 500 mcg IV – repeat every 5 min if • +/- fluids +++ needed
Patterns of Traumatic Injury • Penetrating injury – ongoing significant blood loss is expected • Blunt injury – blood loss may be occult or contained and significant or limited • Head injury – maintenance of cerebral perfusion pressure • Others: pediatric and obstetric trauma
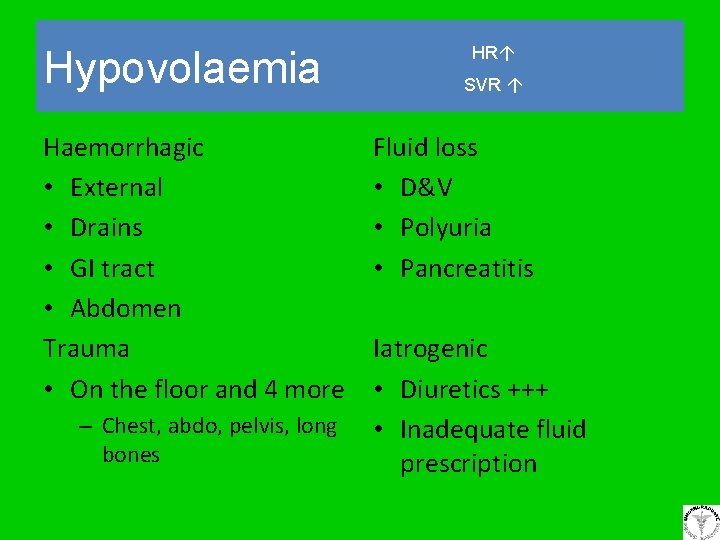
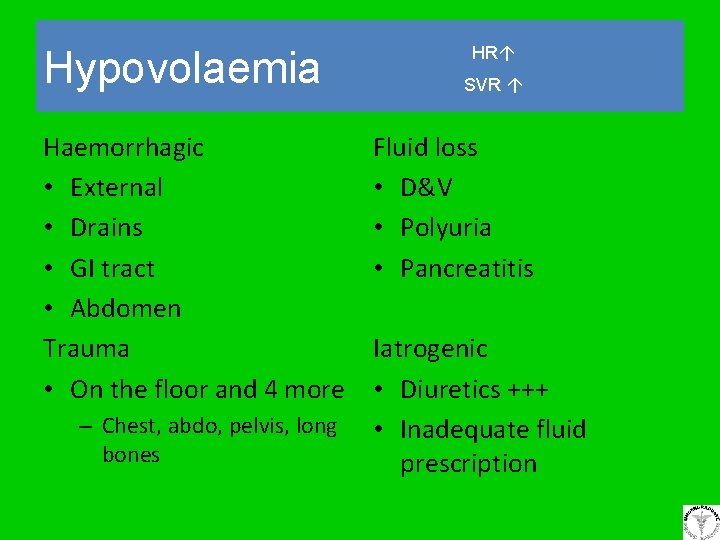
Hypovolaemia Haemorrhagic • External • Drains • GI tract • Abdomen Trauma • On the floor and 4 more – Chest, abdo, pelvis, long bones HR SVR Fluid loss • D&V • Polyuria • Pancreatitis Iatrogenic • Diuretics +++ • Inadequate fluid prescription
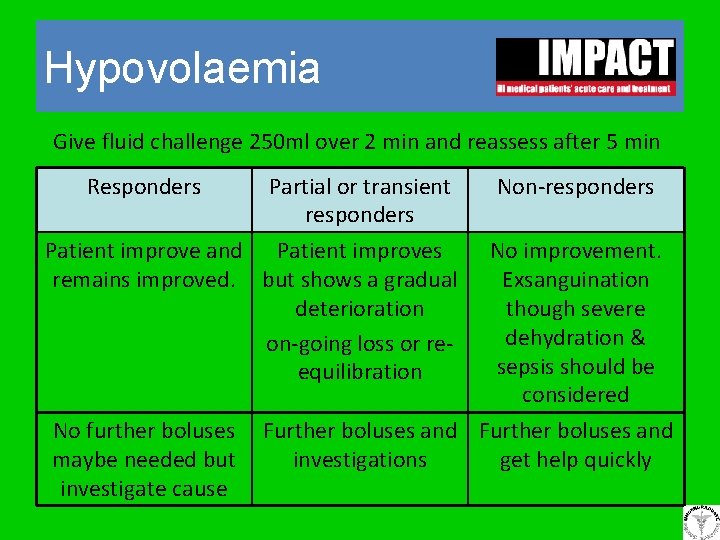
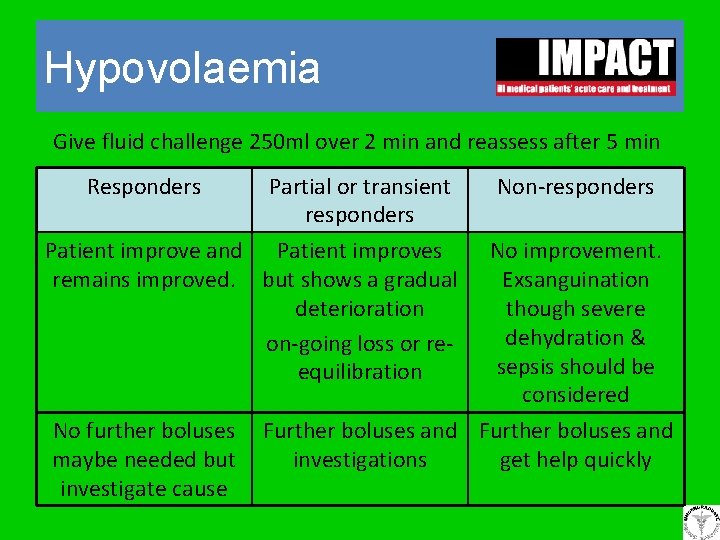
Hypovolaemia Give fluid challenge 250 ml over 2 min and reassess after 5 min Responders Partial or transient responders Non-responders Patient improve and Patient improves remains improved. but shows a gradual deterioration on-going loss or reequilibration No improvement. Exsanguination though severe dehydration & sepsis should be considered No further boluses maybe needed but investigate cause Further boluses and investigations get help quickly
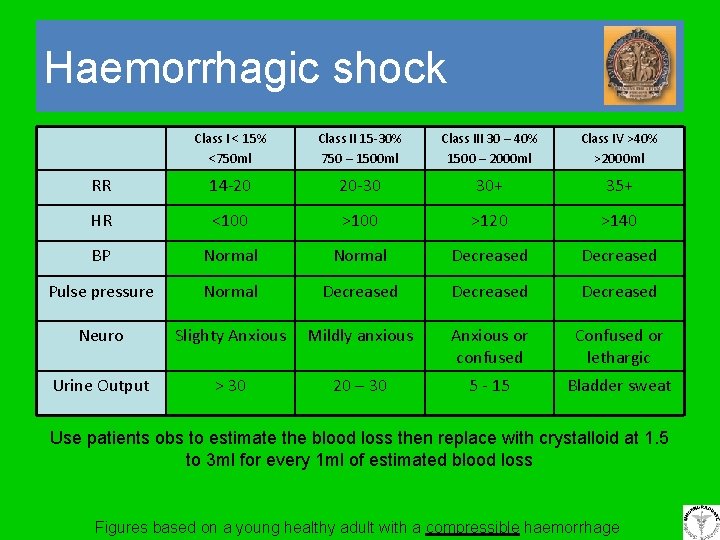
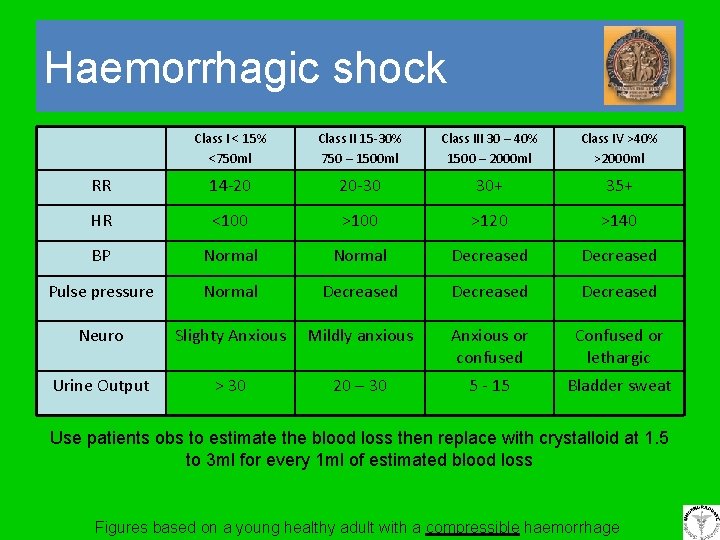
Haemorrhagic shock Class I < 15% <750 ml Class II 15 -30% 750 – 1500 ml Class III 30 – 40% 1500 – 2000 ml Class IV >40% >2000 ml RR 14 -20 20 -30 30+ 35+ HR <100 >120 >140 BP Normal Decreased Pulse pressure Normal Decreased Neuro Slighty Anxious Mildly anxious Anxious or confused Confused or lethargic Urine Output > 30 20 – 30 5 - 15 Bladder sweat Use patients obs to estimate the blood loss then replace with crystalloid at 1. 5 to 3 ml for every 1 ml of estimated blood loss Figures based on a young healthy adult with a compressible haemorrhage
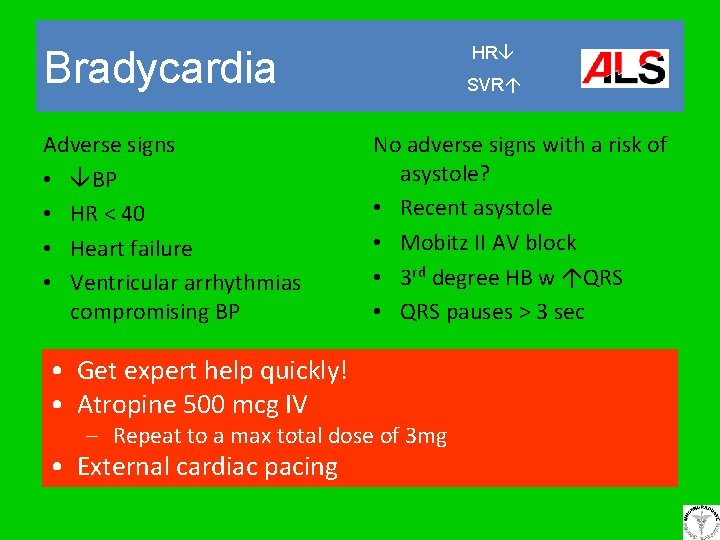
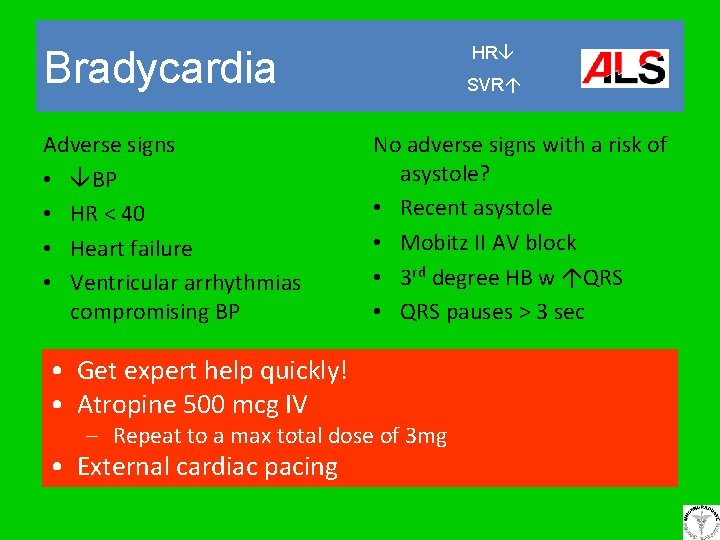
HR Bradycardia Adverse signs • BP • HR < 40 • Heart failure • Ventricular arrhythmias compromising BP • Get expert help quickly! • Atropine 500 mcg IV SVR No adverse signs with a risk of asystole? • Recent asystole • Mobitz II AV block • 3 rd degree HB w QRS • QRS pauses > 3 sec – Repeat to a max total dose of 3 mg • External cardiac pacing
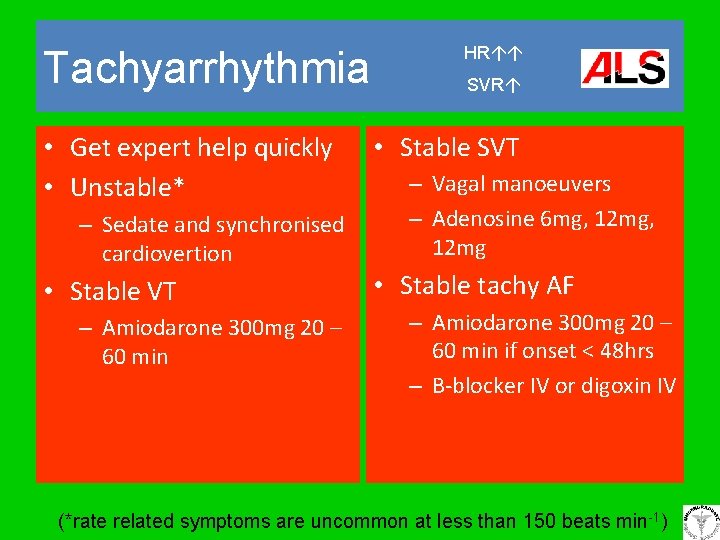
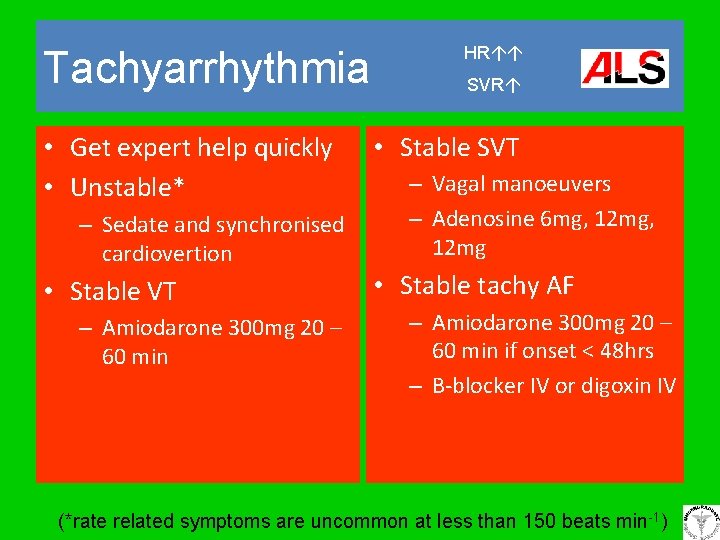
Tachyarrhythmia • Get expert help quickly • Unstable* – Sedate and synchronised cardiovertion • Stable VT – Amiodarone 300 mg 20 – 60 min HR SVR • Stable SVT – Vagal manoeuvers – Adenosine 6 mg, 12 mg • Stable tachy AF – Amiodarone 300 mg 20 – 60 min if onset < 48 hrs – Β-blocker IV or digoxin IV (*rate related symptoms are uncommon at less than 150 beats min-1)
