THE ANESTHESIA MACHINE INTRODUCTION Lucie Filteau 2013 Real
![THE ANESTHESIA MACHINE: INTRODUCTION Lucie Filteau (2013), Real GE Aisys Anesthesia Machine [photograpgh]. Retrieved THE ANESTHESIA MACHINE: INTRODUCTION Lucie Filteau (2013), Real GE Aisys Anesthesia Machine [photograpgh]. Retrieved](https://slidetodoc.com/presentation_image/0147663c634f3bbf8f65a4a21c921d3e/image-1.jpg)


![Preventive Maintenance • CO 2 absorber replacement Przemysław Jahr (2012), Drägersorb® Soda Lime [photograph]. Preventive Maintenance • CO 2 absorber replacement Przemysław Jahr (2012), Drägersorb® Soda Lime [photograph].](https://slidetodoc.com/presentation_image/0147663c634f3bbf8f65a4a21c921d3e/image-44.jpg)
- Slides: 44
![THE ANESTHESIA MACHINE INTRODUCTION Lucie Filteau 2013 Real GE Aisys Anesthesia Machine photograpgh Retrieved THE ANESTHESIA MACHINE: INTRODUCTION Lucie Filteau (2013), Real GE Aisys Anesthesia Machine [photograpgh]. Retrieved](https://slidetodoc.com/presentation_image/0147663c634f3bbf8f65a4a21c921d3e/image-1.jpg)
THE ANESTHESIA MACHINE: INTRODUCTION Lucie Filteau (2013), Real GE Aisys Anesthesia Machine [photograpgh]. Retrieved from https: //www. flickr. com/photos/luciefilteau/19843830788/in /album-72157654569908142/ By : Didier Mukama
Objectives • Know the definition of an Anesthesia Machine • Know the different parts of an Anesthesia Machine and their use. • Set up and use of anesthetic machine • System check out • Common Problems and repairs
What is an Anesthetic Machine? • At the minimum an anesthesia machine administers anesthetic gases to a patient in a controlled manner • A medical equipment used to administer anesthesia to patients. • monitors patient and allows the anesthetist/anesthesiologist (user) to make necessary adjustment in order to keep patients under stable state of anesthesia. • gives the patient a mixture of anesthetic gas • Has incorporated devices that monitors vital signs (HR, BP, Temp, SPO 2…) • Has alarm systems to allow failsafe operations. • Has a protection system that prevents the surgeons, anesthetists… to inhale anesthetic gases. (scavenging system)
What is Anesthetic Gas? Gas used to temporarily keep the patient in total unconsciousness. (General anesthesia) 2 types of anesthetic gases are common: 1. 2. Ether Halogenated (most common): e. g. ISOFLURANE, SEVOFLURANE Non-Ether Halogenated hydrocarbons: e. g. HALOTHANE, CHOLOROFORM Non-Ether Halogenated hydrocarbons are no longer used in developed countries because they are toxic, but are very common in Third World. E. g. HALOTHANE is very common in Rwanda. Other types of anesthetic gases: XENON (costly) The Anesthetic gases are stored in liquid state at room temperature but are very volatile. A vaporizer is used to administer the anesthetic gases to patients
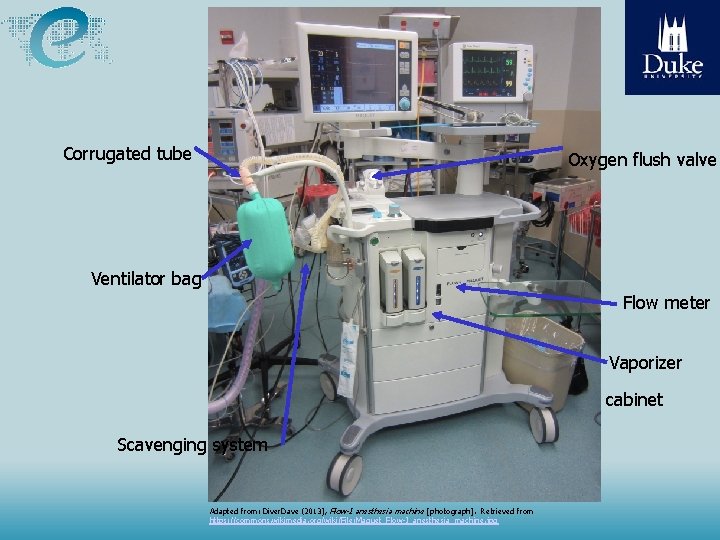
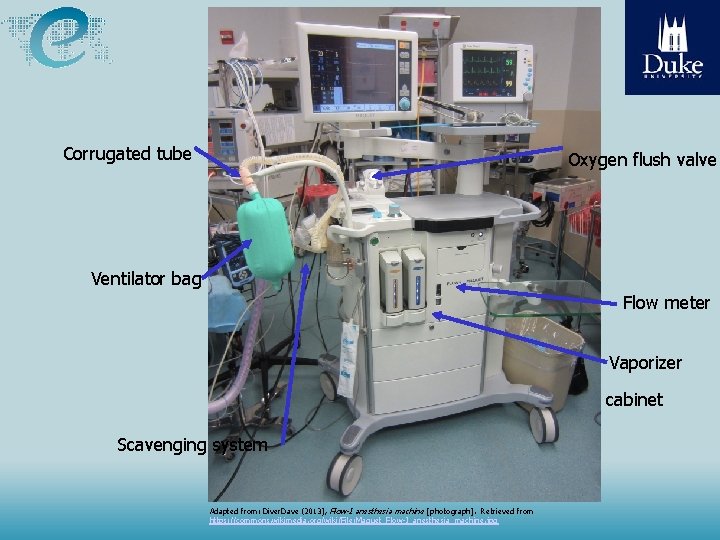
Corrugated tube Oxygen flush valve Ventilator bag Flow meter Vaporizer cabinet Scavenging system Source: Malkin, “Medical Instrumentation in the Developing World” Adapted from: Diver. Dave (2013), Flow-I anesthesia machine [photograph]. Retrieved from https: //commons. wikimedia. org/wiki/File: Maquet_Flow-I_anesthesia_machine. jpg
System Components APL (Adjustable Pressure Limiting) valve: Pressure limiting valve which releases gas over an adjustable range of pressures on purpose to control system pressure and thus intrapulmonary pressure. Scavenging System: An assembly of specific components that collect excessive exhaled gases and exhausts them out of the operating room to avoid accidental anesthesia of staff. Soda lime: A mixture of sodium and calcium hydroxides that absorbs liquids and gases, especially CO 2 from patient exhaled gases Vaporizer: Used to produce an accurate amount of gas from a volatile liquid anesthetic gas. It has a dial or knob to know and to regulate the percentage of anesthetic gases given to the patient.
Homeostasis Control – Manual (bag) or assisted (automatic) ventilation – Circulation (Blood volume, vasopressor drugs) – Neurologic (Autonomous reflex; Anesthetic drugs, relaxant) – Thermal regulation (physical; cover, room temperature)
Side effects • Drug Toxicity • Drug interactions with therapeutic, herbal, abused substances • Post-operation Nausea and vomiting
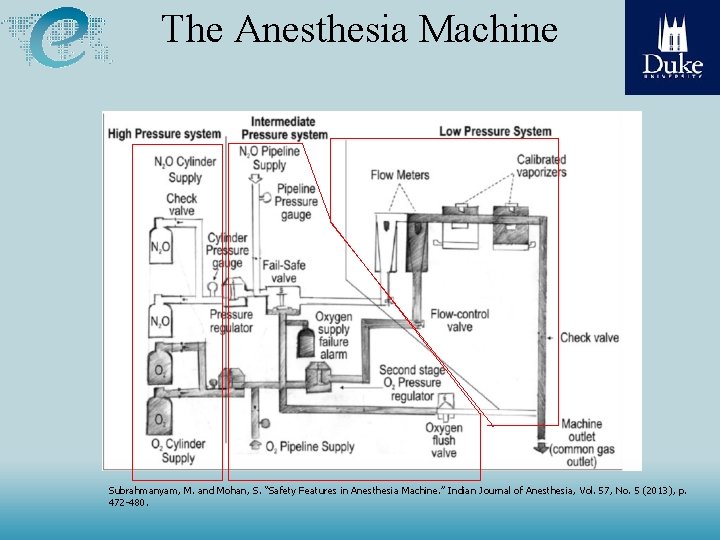
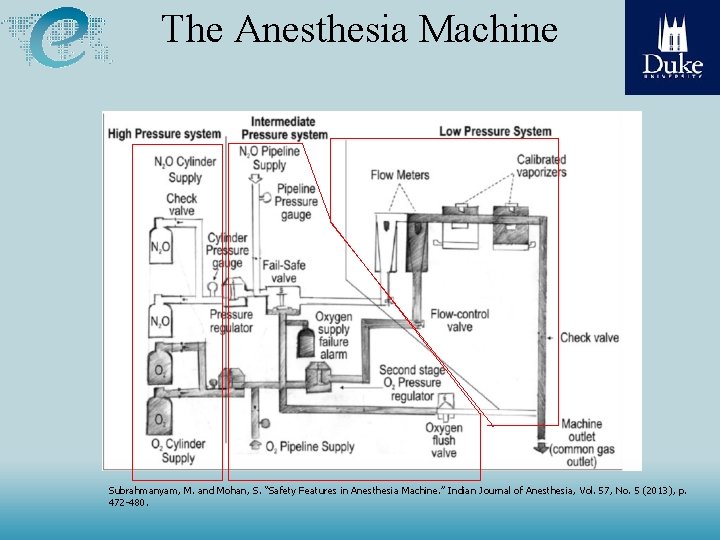
The Anesthesia Machine Subrahmanyam, M. and Mohan, S. “Safety Features in Anesthesia Machine. ” Indian Journal of Anesthesia, Vol. 57, No. 5 (2013), p. 472 -480.
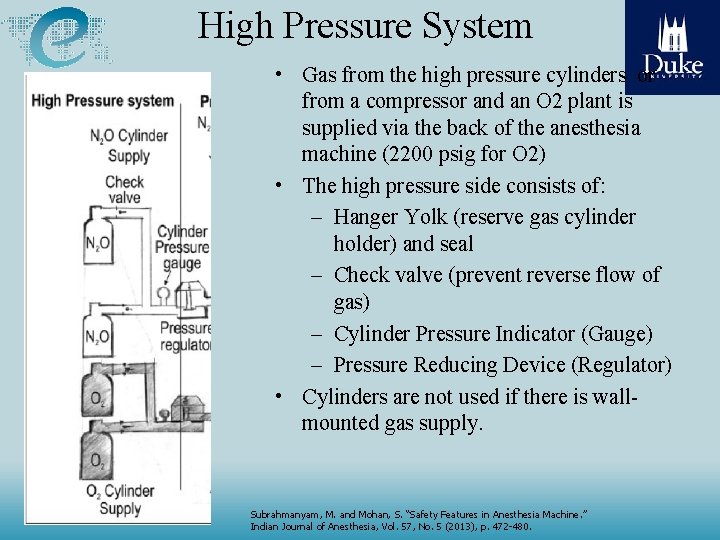
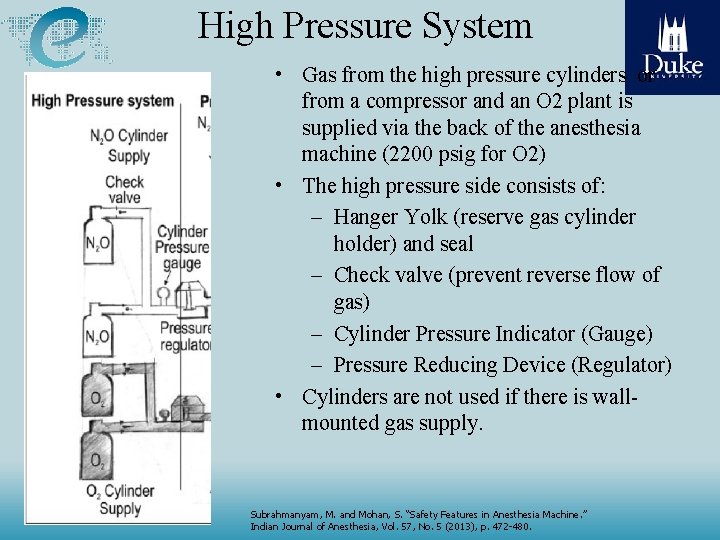
High Pressure System • Gas from the high pressure cylinders or from a compressor and an O 2 plant is supplied via the back of the anesthesia machine (2200 psig for O 2) • The high pressure side consists of: – Hanger Yolk (reserve gas cylinder holder) and seal – Check valve (prevent reverse flow of gas) – Cylinder Pressure Indicator (Gauge) – Pressure Reducing Device (Regulator) • Cylinders are not used if there is wallmounted gas supply. Subrahmanyam, M. and Mohan, S. “Safety Features in Anesthesia Machine. ” Indian Journal of Anesthesia, Vol. 57, No. 5 (2013), p. 472 -480.
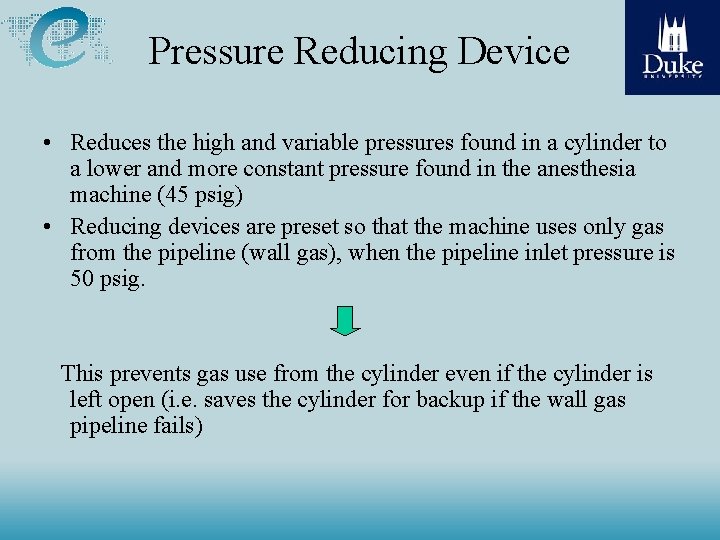
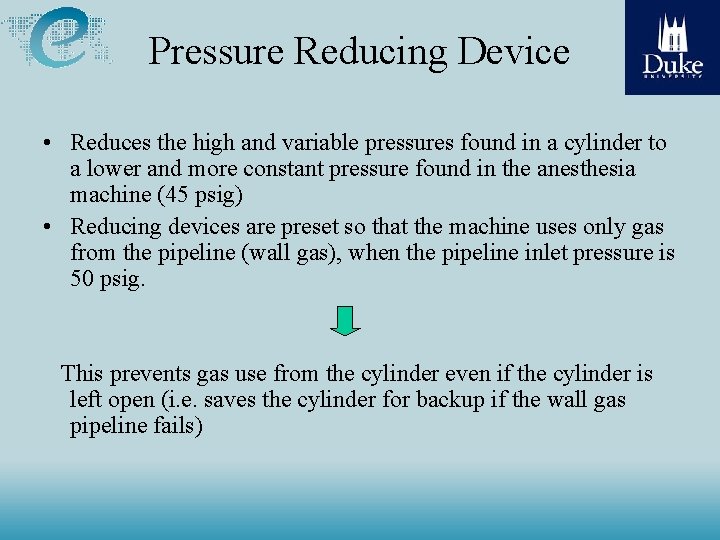
Pressure Reducing Device • Reduces the high and variable pressures found in a cylinder to a lower and more constant pressure found in the anesthesia machine (45 psig) • Reducing devices are preset so that the machine uses only gas from the pipeline (wall gas), when the pipeline inlet pressure is 50 psig. This prevents gas use from the cylinder even if the cylinder is left open (i. e. saves the cylinder for backup if the wall gas pipeline fails)
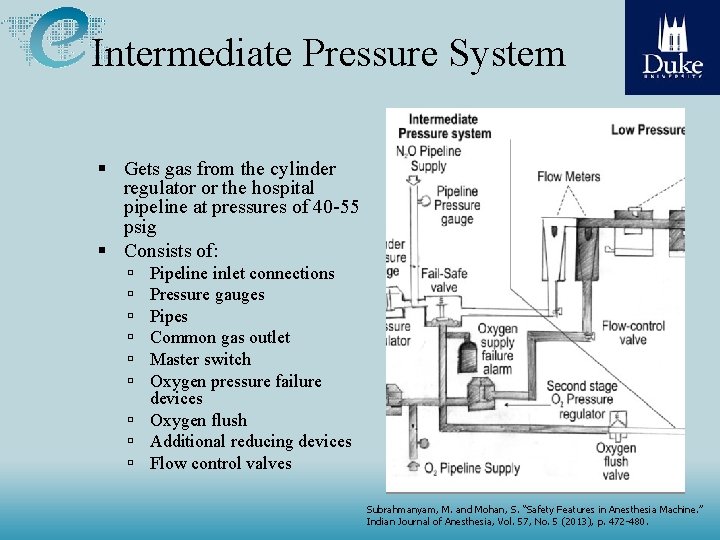
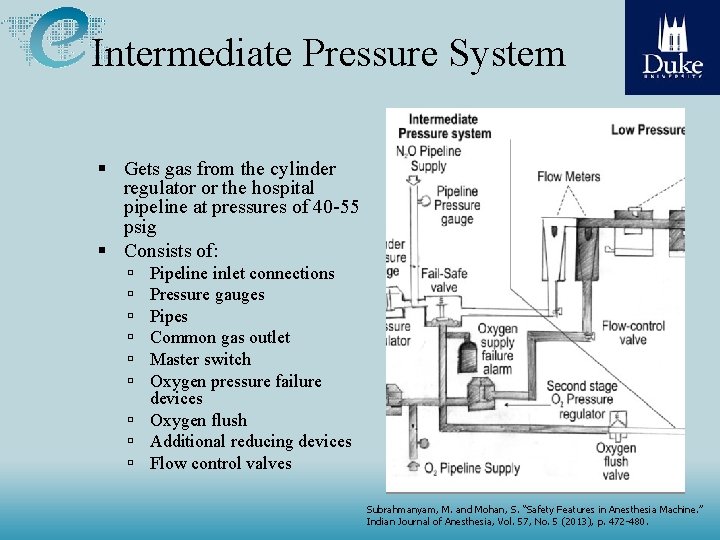
Intermediate Pressure System Gets gas from the cylinder regulator or the hospital pipeline at pressures of 40 -55 psig Consists of: Pipeline inlet connections Pressure gauges Pipes Common gas outlet Master switch Oxygen pressure failure devices Oxygen flush Additional reducing devices Flow control valves Subrahmanyam, M. and Mohan, S. “Safety Features in Anesthesia Machine. ” Indian Journal of Anesthesia, Vol. 57, No. 5 (2013), p. 472 -480.
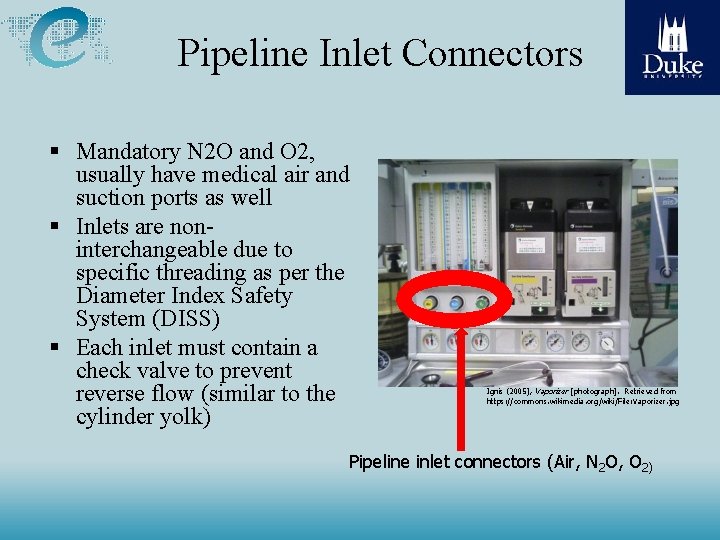
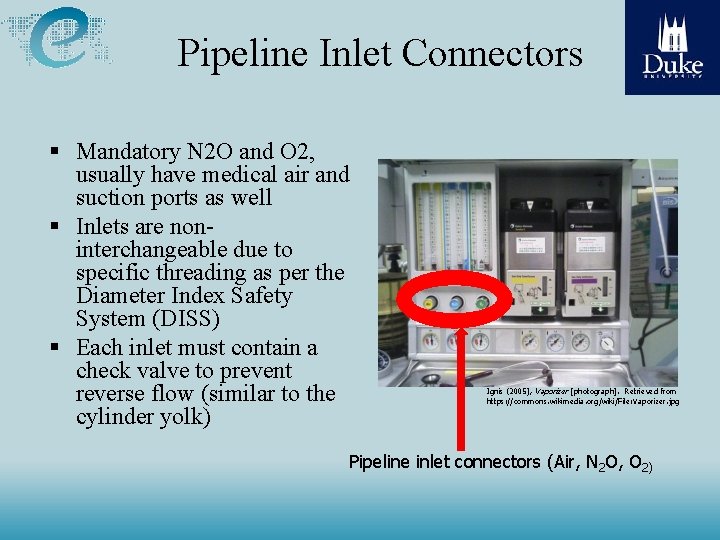
Pipeline Inlet Connectors Mandatory N 2 O and O 2, usually have medical air and suction ports as well Inlets are noninterchangeable due to specific threading as per the Diameter Index Safety System (DISS) Each inlet must contain a check valve to prevent reverse flow (similar to the cylinder yolk) Ignis (2005), Vaporizer [photograph]. Retrieved from https: //commons. wikimedia. org/wiki/File: Vaporizer. jpg Pipeline inlet connectors (Air, N 2 O, O 2)
Oxygen Pressure Monitors • An anesthesia machine is designed such that it sounds an alarm whenever the oxygen supply pressure falls below normal range. (O 2 concentration should not be below 19%) • Some machines have and electronic as well as a mechanical low O 2 supply alarm. In this case one would be a beeper/buzzer and the other would be an air powered whistle
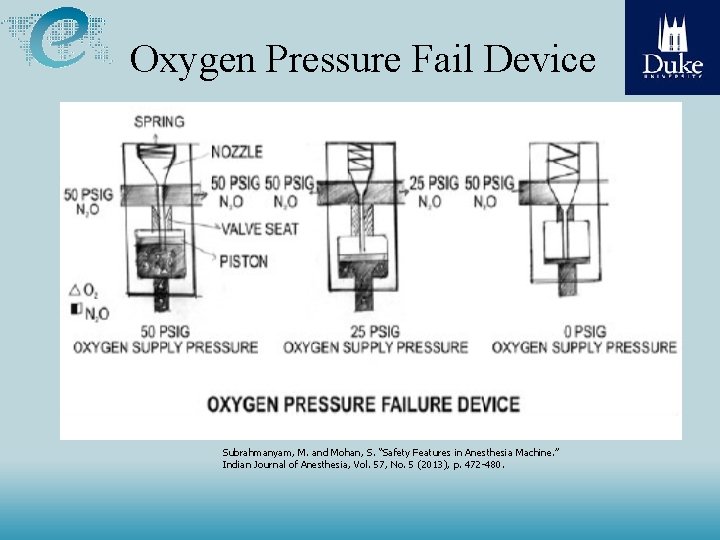
Oxygen Pressure Failure Devices • A Fail-Safe valve is found in each gas line supplying the flow meters. This valve shuts off or proportionately decreases the supply pressure of all other gasses with the decrease in O 2 supply pressure. • 2 kinds of fail-safe valves exist: – Pressure sensor shut-off valve (e. g. Ohmeda) – Oxygen failure protection device (e. g. Drager)
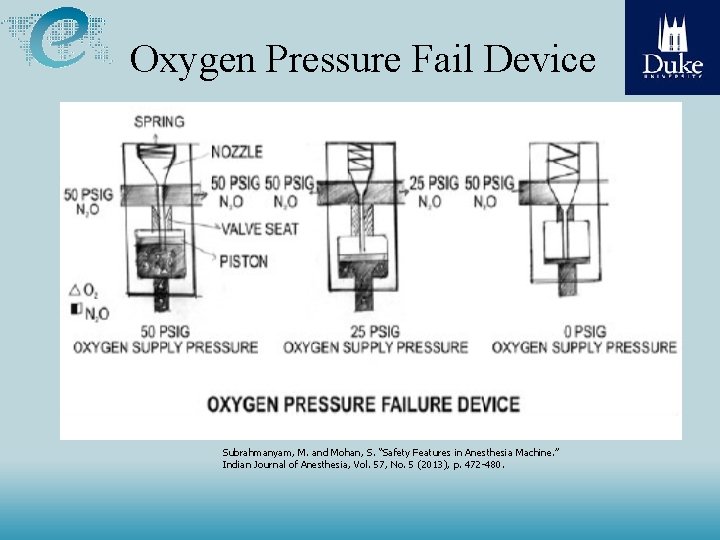
Oxygen Pressure Fail Device Subrahmanyam, M. and Mohan, S. “Safety Features in Anesthesia Machine. ” Indian Journal of Anesthesia, Vol. 57, No. 5 (2013), p. 472 -480.
Pressure Sensor Shut-Off Valve • Oxygen supply pressure opens the valve as long as it is above a pre-set minimum value (e. g. . 20 psig). • If the oxygen supply pressure falls below the threshold value the valve closes and the gas in that limb (e. g. . N 2 O), does not advance to its flowcontrol valve.
Oxygen Failure Protection Device (OFPD) • Based on a proportioning principle rather than a shutoff principle • The pressure of all gases controlled by the OFPD will decrease proportionately with the oxygen pressure
Oxygen Flush Valve • Receives O 2 from pipeline inlet or cylinder reducing device and directs high, unmetered flow directly to the common gas outlet (downstream of the vaporizer) • Machine standard requires that the flow be between 35 and 75 L/min in flush mode • The ability to provide jet ventilation • Hazards – May cause barotrauma
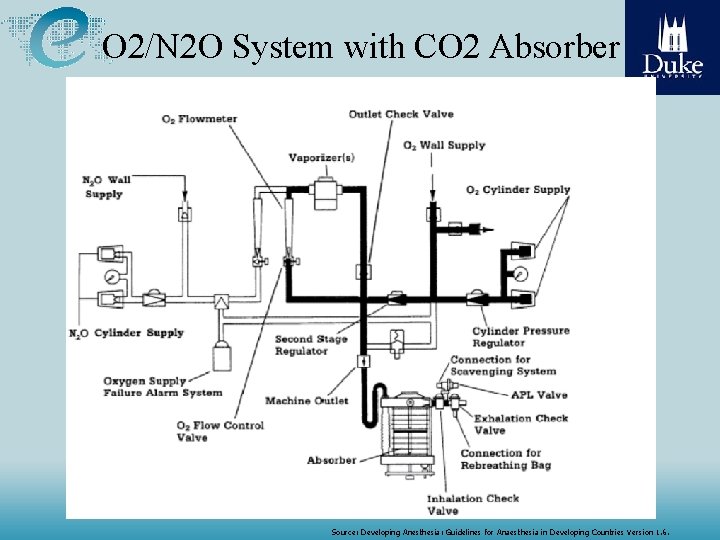
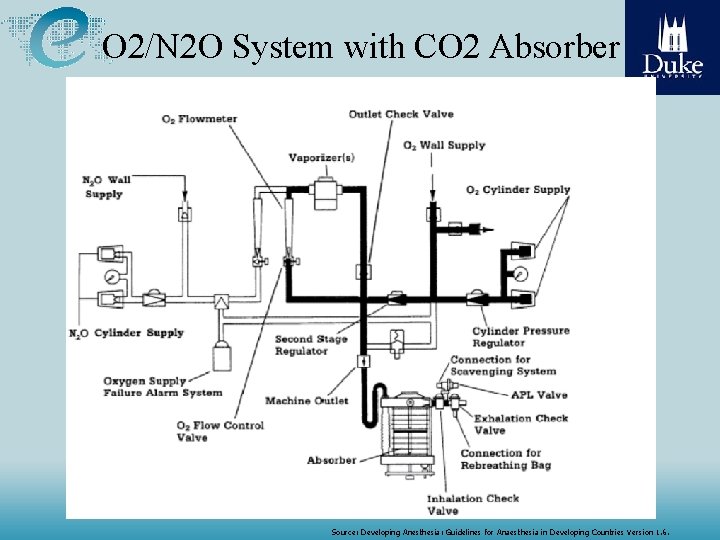
O 2/N 2 O System with CO 2 Absorber Source: Developing Anesthesia: Guidelines for Anaesthesia in Developing Countries Version 1. 6.
Second-Stage Reducing Device • Located just upstream of the flow control valves • Receives gas from the pipeline inlet or the cylinder reducing device and reduces it further to 26 psig for N 2 O and 14 psig for O 2 • Purpose is to eliminate fluctuations in pressure supplied to the flow indicators caused by fluctuations in pipeline pressure
Low Pressure System • It goes from the flow control valves to the gas outlet and consists of: – Flow meters – Vaporizer mounting device – Check valve – Common gas outlet
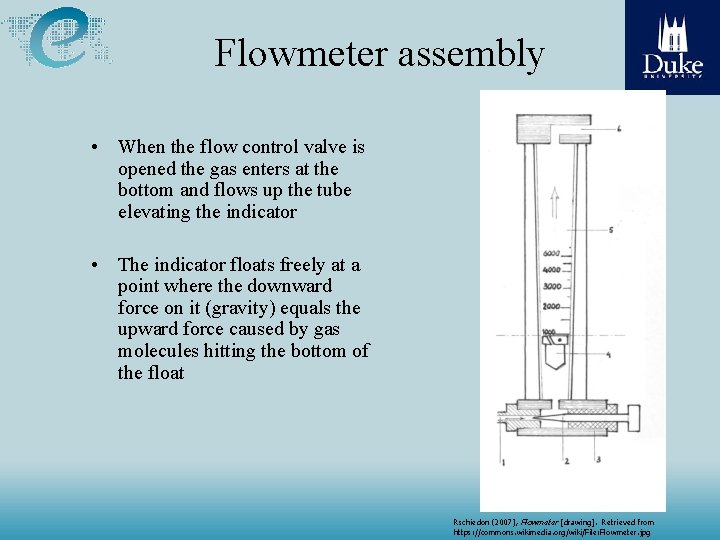
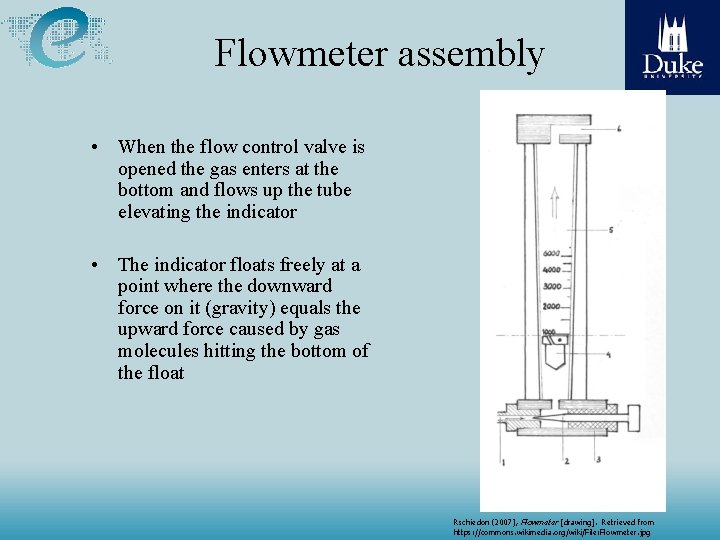
Flowmeter assembly • When the flow control valve is opened the gas enters at the bottom and flows up the tube elevating the indicator • The indicator floats freely at a point where the downward force on it (gravity) equals the upward force caused by gas molecules hitting the bottom of the float Rschiedon (2007), Flowmeter [drawing]. Retrieved from https: //commons. wikimedia. org/wiki/File: Flowmeter. jpg
Proportioning Systems – – Mechanical integration of the N 2 O and O 2 flow-control valves Automatically intercedes to maintain a minimum 25% concentration of oxygen with a maximum N 2 O: O 2 ratio of 3: 1
Limitations of Proportioning Systems • Machines equipped with proportioning systems can still deliver a hypoxic mixture under the following conditions: – Wrong supply gas – Defective pneumatics or mechanics – Leak downstream (e. g. worn/broken o-rings or leaking pipe fittings) – Inert gas administration: Proportioning systems generally link only N 2 O and O 2
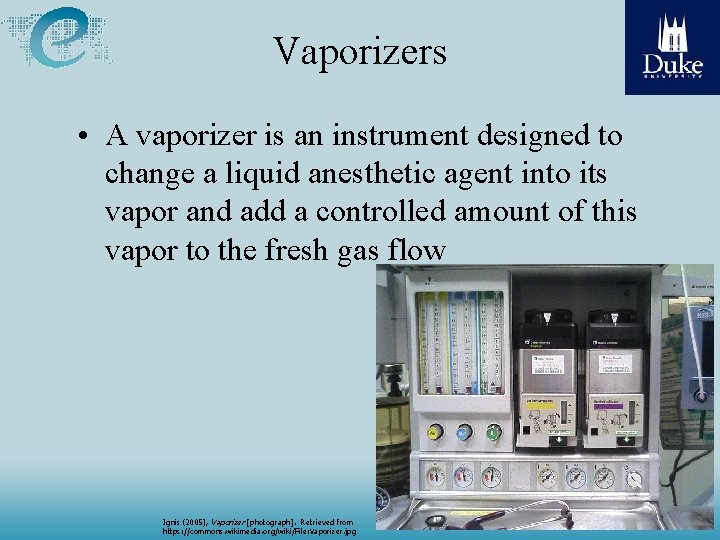
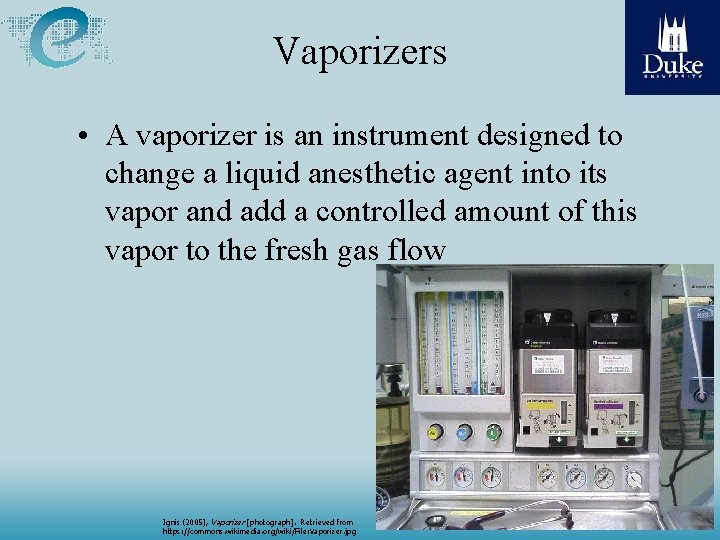
Vaporizers • A vaporizer is an instrument designed to change a liquid anesthetic agent into its vapor and add a controlled amount of this vapor to the fresh gas flow Ignis (2005), Vaporizer [photograph]. Retrieved from https: //commons. wikimedia. org/wiki/File: Vaporizer. jpg
Classification of Vaporizers Methods of regulating output concentration Concentration calibrated (e. g. variable bypass) Measured flow Method of vaporization Flow-over Bubble through Injection Temperature compensation Thermocompensation Supplied heat
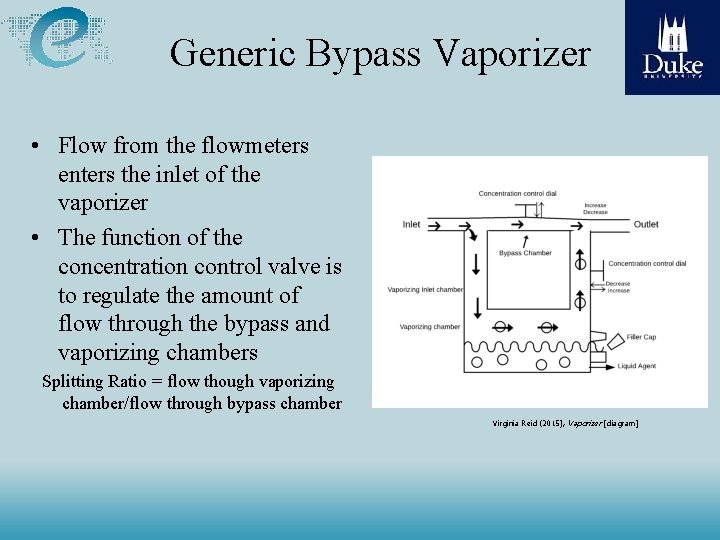
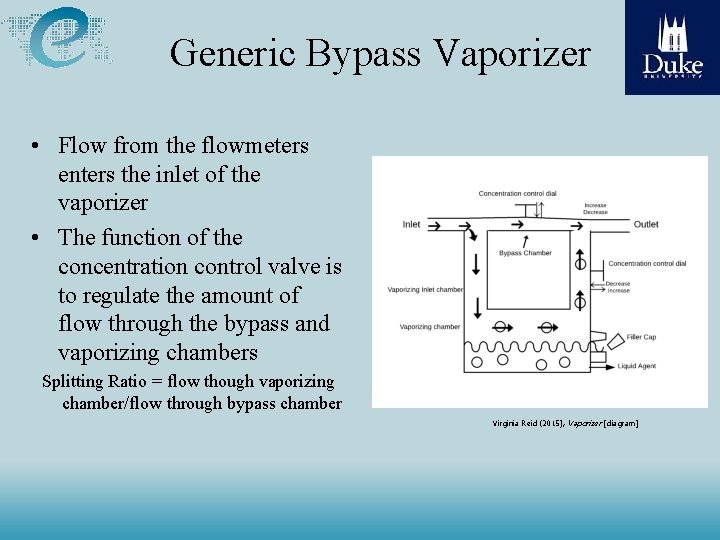
Generic Bypass Vaporizer • Flow from the flowmeters enters the inlet of the vaporizer • The function of the concentration control valve is to regulate the amount of flow through the bypass and vaporizing chambers Splitting Ratio = flow though vaporizing chamber/flow through bypass chamber Virginia Reid (2015), Vaporizer [diagram]
Factors That Influence Vaporizer Output • Flow Rate: The output of the vaporizer is generally less than the dial setting at very low (< 200 ml/min) or very high (> 15 L/min) flows • Temperature: Automatic temperature compensating mechanisms in bypass chambers maintain a constant vaporizer output with varying temperatures • Back Pressure: Intermittent back pressure (e. g. positive pressure ventilation causes a higher vaporizer output than the dial setting)
Factors That Influence Vaporizer Output • Atmospheric Pressure: Changes in atmospheric pressure affect variable bypass vaporizer output as measured by volume % concentration, but not (or very little) as measured by partial pressure (lowering atmospheric pressure increases volume % concentration and vice versa) • Carrier Gas: Vaporizers are calibrated for 100% oxygen. Carrier gases other than this result in decreased vaporizer output.
The Circuit: Circle System • Arrangement is variable, but to prevent re-breathing of CO 2, the following rules must be followed: – Unidirectional valves between the patient and the reservoir bag – Fresh-gas-flow cannot enter the circuit between the expiratory valve and the patient – Adjustable pressure-limiting valve (APL) cannot be located between the patient and the inspiratory valve
Circle System Advantages: Relative stability of inspired concentration Conservation of respiratory moisture and heat Prevention of operating room pollution Pa. CO 2 depends only on ventilation, not fresh gas flow Low fresh gas flows can be used Disadvantages: Complex design = potential for malfunction High resistance (multiple one-way valves) = higher work of breathing
The Adjustable Pressure Limiting (APL) Valve • User adjustable valve that releases gases to the scavenging system and is intended to provide control of the pressure in the breathing system • Bag-mask Ventilation: Valve is usually left partially open. During inspiration the bag is squeezed pushing gas into the inspiratory limb until the pressure relief is reached, opening the APL valve. • Mechanical Ventilation: The APL valve is excluded from the circuit when the selector switch is changed from manual to automatic ventilation

Patient Rebreathing Circuit • Protects the breathing circuit or ventilator from excessive positive or negative pressure. Developing Anesthesia: Guidelines for Anaesthesia in Developing Countries Version 1. 6 (2007). Retrieved from linrary. ewh. com
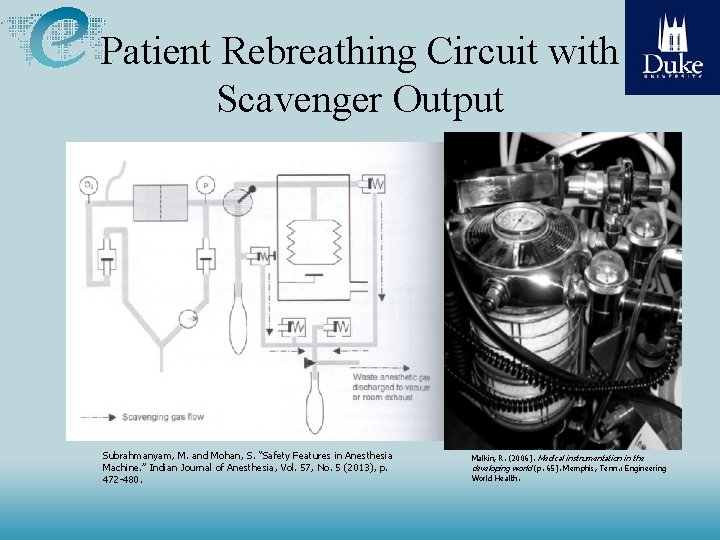
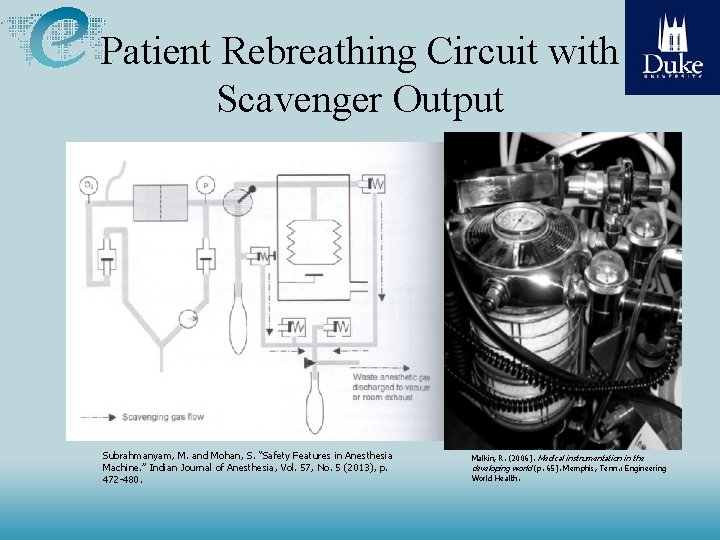
Patient Rebreathing Circuit with Scavenger Output Subrahmanyam, M. and Mohan, S. “Safety Features in Anesthesia Machine. ” Indian Journal of Anesthesia, Vol. 57, No. 5 (2013), p. 472 -480. Malkin, R. (2006). Medical instrumentation in the developing world (p. 65). Memphis, Tenn. : Engineering World Health.
Checking Anesthesia Machines Categories of checks: • Gas supply/High pressure system • Low-Pressure system • APL valve and Scavenging system • Breathing system • Manual and automatic ventilation system • Monitors • Final configurations • Any emergency ventilation equipment located in the OR • Check any gas analysis found on the machine
Patient Monitoring • Clinical Signs – not automatic measured – Movement, Pupil dilation, Sweating, Heart and lung sounds • Anesthesia – Neuromuscular Relaxation- Evoked response - accelerometers, EMG – Sedation, Hypnosis • Blood concentration - Expired inhaled anesthetic agent concentration • Spontaneous EEG - Compressed Spectral, Bi. Spectral analysis; Entropy • Evoked EEG responses -- Somatic, Auditory, Optical – Analgesia (no pain) -- ? ?
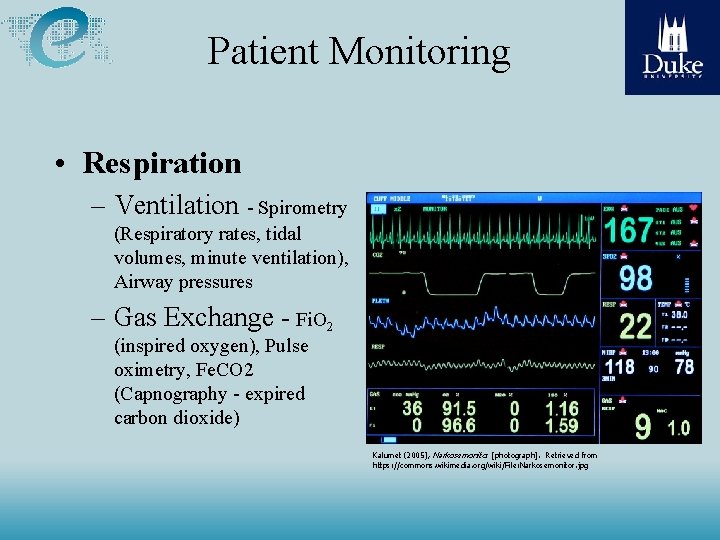
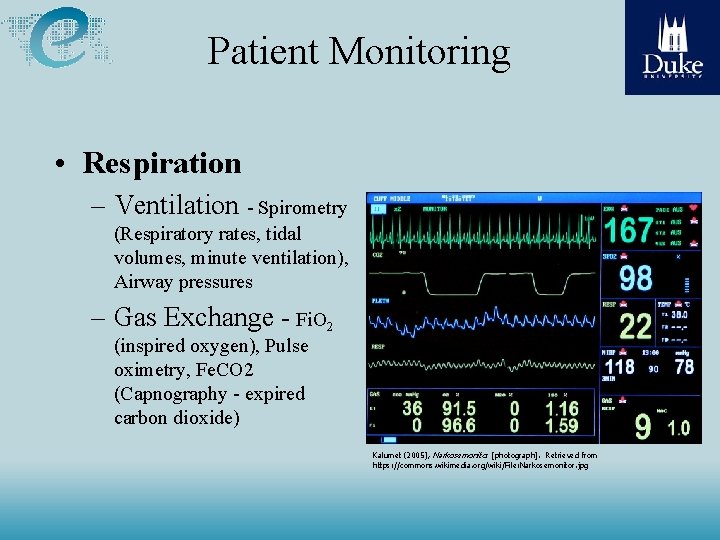
Patient Monitoring • Respiration – Ventilation - Spirometry (Respiratory rates, tidal volumes, minute ventilation), Airway pressures – Gas Exchange - Fi. O 2 (inspired oxygen), Pulse oximetry, Fe. CO 2 (Capnography - expired carbon dioxide) Kalumet (2005), Narkosemonito r [photograph]. Retrieved from https: //commons. wikimedia. org/wiki/File: Narkosemonitor. jpg

Patient Monitoring • Circulation – Electrocardiogram (ECG) – Blood Pressures • Non-invasive blood pressures (NIBP) • Invasive Blood Pressures – Arterial, Venous – Atrial, Ventricle, Pulmonary Artery, Pulmonary pressures – Cardiac Output • Temperature Pflegewiki-User Würfell (2007). , Medical Monitor [photograph]. Retrieved from https: //commons. wikimedia. org/wiki/File: Monitor_(medical). jpg
Patient Safety • Fail Safe Mechanism against – Hypoxia - O 2/N 2 O mechanic connection, O 2 monitor, pulse oximetry – Apnea, Leaks, disconnect, occlusion - low minute ventilation, high/low pressure, CO 2 monitor – Excessive airway pressure - redundant pressure relief valves – Over/Under Anesthetic deliver -Vaporizer interlock, concentration monitor
Patient Safety • Mandatory preanesthesia checkout • Alarm System - a dilemma – Intended for vigilance – Result: Excessive alarms noise
Common Problems • Power supply • User error • Leaks – Gases leak may affect staff and are flammable • Sticky rotameters needle valves – Flush with alcohol Mintz I Flow Meter (2013). Retrieved from https: //en. wikipedia. org/wiki/Anaesthetic_machine
Preventive Maintenance • O 2 sensor contacts cleaning with alcohol Mark. murphy (2005), Diving oxygen analyser [photograph]. Retrieved from https: //commons. wikimedia. org/wiki/File: Diving_oxygen_a nalyser. JPG • Batteries replacement Clckr. Free. Vector. Images (2015), Battery [drawing. Retrieved from Pixabay
![Preventive Maintenance CO 2 absorber replacement Przemysław Jahr 2012 Drägersorb Soda Lime photograph Preventive Maintenance • CO 2 absorber replacement Przemysław Jahr (2012), Drägersorb® Soda Lime [photograph].](https://slidetodoc.com/presentation_image/0147663c634f3bbf8f65a4a21c921d3e/image-44.jpg)
Preventive Maintenance • CO 2 absorber replacement Przemysław Jahr (2012), Drägersorb® Soda Lime [photograph]. Retrieved from https: //commons. wikimedia. org/wiki/File: Dr%C 3%A 4 gersorb_Soda_Lime. jp g