The anaesthetist restrictive interventions restraint teams Dr Liam







- Slides: 23

The anaesthetist, restrictive interventions & restraint teams Dr Liam Brennan Consultant Anaesthetist, Cambridge University Hospitals
Winterbourne View scandal (2011) • Punitive use of restraint in hospital for adults with learning disabilities; 11 staff charged with criminal offences; 6 jailed • Prompted national debate about use of restrictive interventions in all health & social care settings • DH published guidance on use of restrictive interventions (2014) • Potential implications for anaesthetic & critical care practice https: //www. gov. uk/government/uploads/system/uploads/attachment_data/file/300293/J RA_Do. H_Guidance_on_RP_web_accessible. pdf
Content • • • Overview of restrictive interventions (RIs) Key principles of RI practice Legal perspectives Physical & chemical restraint Training implications Restraint response teams
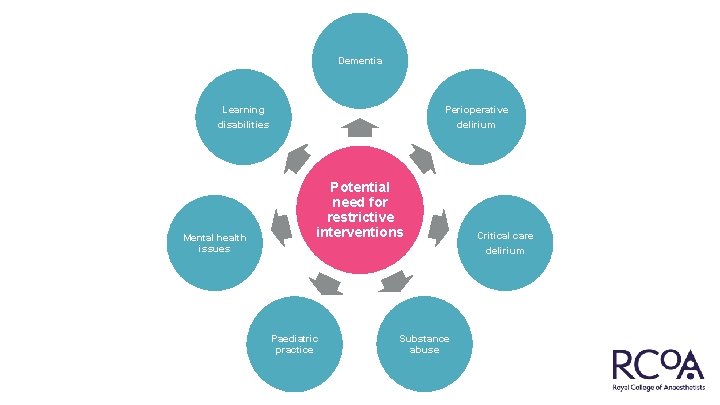
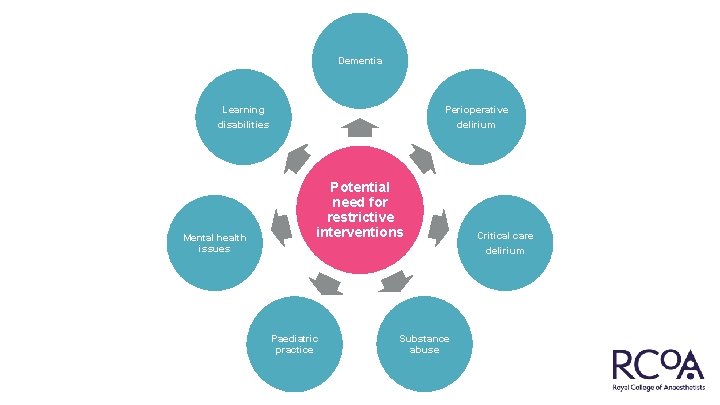
Dementia Learning disabilities Mental health issues Perioperative delirium Potential need for restrictive interventions Paediatric practice Substance abuse Critical care delirium
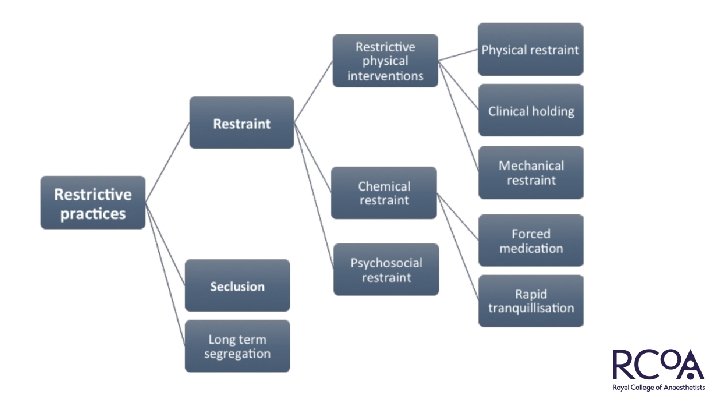
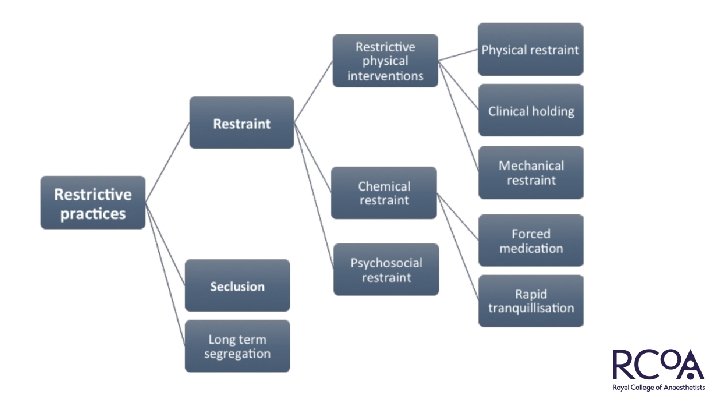
What is a restrictive intervention? • Deliberate acts on the part of other person(s) that restrict an individual’s movement, liberty and/or freedom to act independently in order to: – take immediate control of a dangerous situation where there is a real possibility of harm to the person or others if no action is undertaken; and – end or reduce significantly the danger to the person or others; and – contain or limit the person’s freedom for no longer than is necessary.
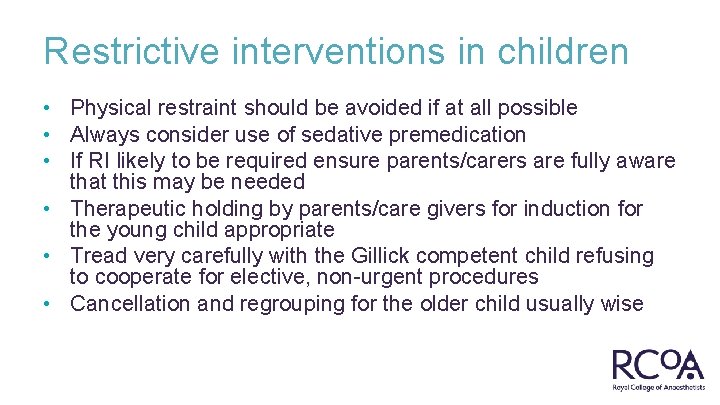
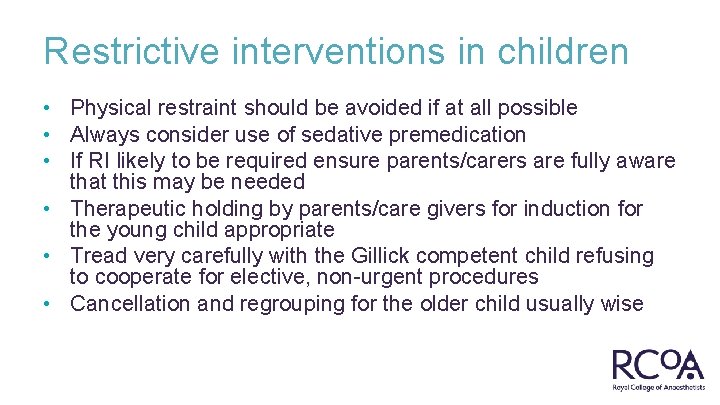
Restrictive interventions in children • Physical restraint should be avoided if at all possible • Always consider use of sedative premedication • If RI likely to be required ensure parents/carers are fully aware that this may be needed • Therapeutic holding by parents/care givers for induction for the young child appropriate • Tread very carefully with the Gillick competent child refusing to cooperate for elective, non-urgent procedures • Cancellation and regrouping for the older child usually wise

Need to learn more? Positive Outcome and Experience Management Strategy • • • One day course Strategies to ↓ child anxiety http: //www. poemsforchildren. co. uk
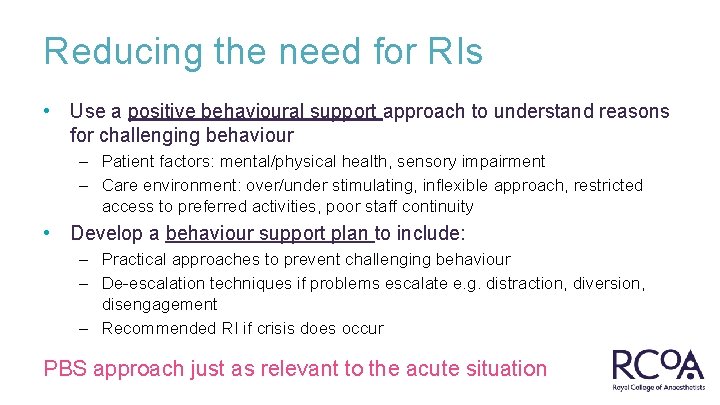
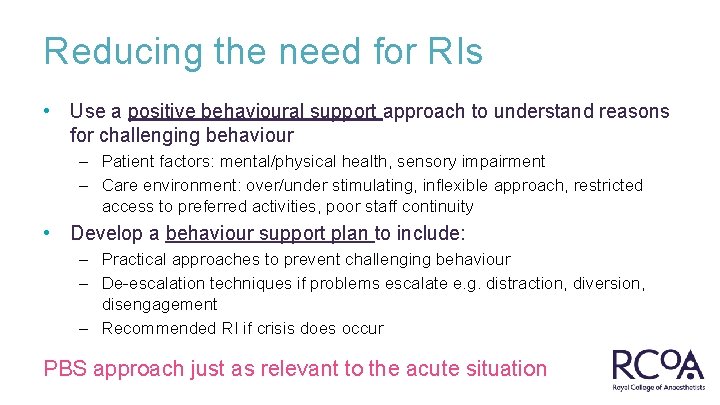
Reducing the need for RIs • Use a positive behavioural support approach to understand reasons for challenging behaviour – Patient factors: mental/physical health, sensory impairment – Care environment: over/under stimulating, inflexible approach, restricted access to preferred activities, poor staff continuity • Develop a behaviour support plan to include: – Practical approaches to prevent challenging behaviour – De-escalation techniques if problems escalate e. g. distraction, diversion, disengagement – Recommended RI if crisis does occur PBS approach just as relevant to the acute situation

Causes of confusion, delirium & agitation • • • Hypoxaemia Shock Advanced age is a risk factor not a cause Sepsis Glycaemic derangement Substance abuse NB Alcohol withdrawal Brain trauma/stroke/dementia/other CNS disorders Chronic renal/hepatic/cardiac dysfunction Anxiety/fear/stress Under sedation Drug reactions/interactions General discomfort e. g. urinary retention, prolonged starvation Environmental factors Noise Inexperienced staff Overcrowding Lack of continuity Lack of privacy Staff shortages

Physical restraint
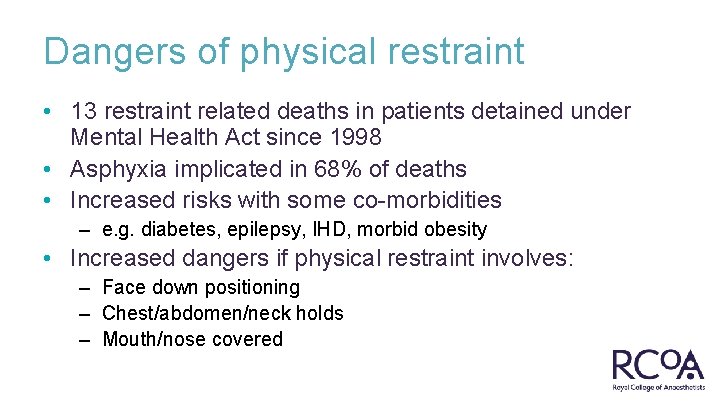
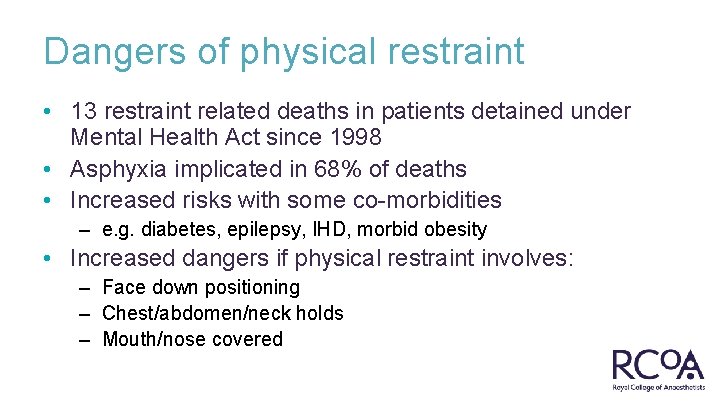
Dangers of physical restraint • 13 restraint related deaths in patients detained under Mental Health Act since 1998 • Asphyxia implicated in 68% of deaths • Increased risks with some co-morbidities – e. g. diabetes, epilepsy, IHD, morbid obesity • Increased dangers if physical restraint involves: – Face down positioning – Chest/abdomen/neck holds – Mouth/nose covered
Key principles in use of RIs • • Least restrictive intervention possible Only use RI for the shortest period of time Must not include deliberate application of pain RIs only used by staff trained in their safe usage Staff safety high priority Liaise with family/carers whenever possible Follow local protocols
Key principles in use of RIs (continued) • Refer to BSP whenever possible to choose most appropriate RI • Physical restraint must not impact on ABC • Chemical restraint should use oral route whenever possible NB: co-morbidities & other medication • Vital signs must be monitored during and after RI • Post incident reviews & debrief essential • Regular audit and reporting essential
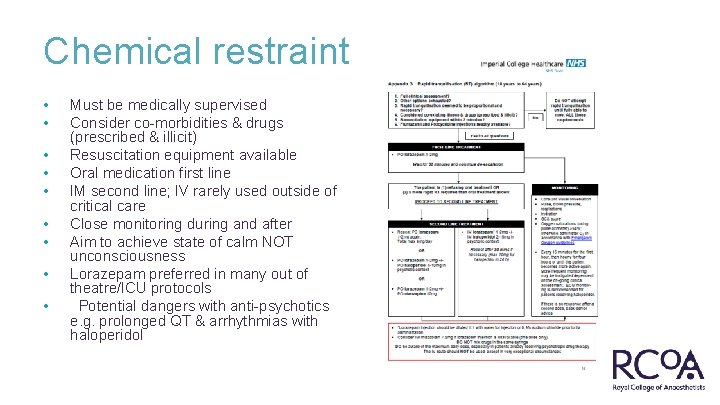
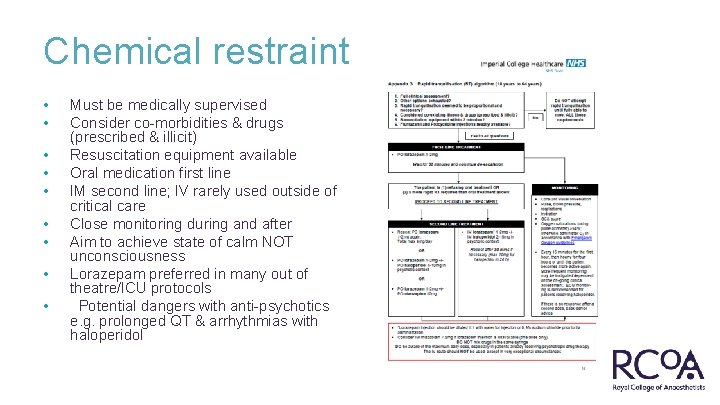
Chemical restraint • • • Must be medically supervised Consider co-morbidities & drugs (prescribed & illicit) Resuscitation equipment available Oral medication first line IM second line; IV rarely used outside of critical care Close monitoring during and after Aim to achieve state of calm NOT unconsciousness Lorazepam preferred in many out of theatre/ICU protocols Potential dangers with anti-psychotics e. g. prolonged QT & arrhythmias with haloperidol
Legal perspectives • Various key pieces of legislation are relevant: • • Mental Health Act 1983 Mental Capacity Act 2005 Human Rights Act 1998 Health & Safety at Work Act 1974 • Use of RIs only justified if patient lacks capacity • Using RIs in situations where patients have capacity risks accusation of assault or ‘deprivation of liberty • Use of RIs is not justified solely on the grounds that a patient makes an unwise decision • The safety of staff involved is paramount
Principles of the Mental Capacity Act (2005) • Understands the information (explained appropriately) • Retains the information (for long enough to decide) • Uses the information in their decision making • Communicates their decision in any way
Training • All staff involved in providing RIs must receive training which should be regularly updated • Current packages focus on mental health professionals • Perioperative care staff rarely receive training • DH and NICE guidance likely to recommend more widespread training • Concern that training resources will not be able to cope with potential demand

Training content • • Building therapeutic relationships Principles of positive behavioural support Causes of challenging behaviours Legal framework Risks associated with RIs De-escalation techniques Safe implementation of RIs Post incident de-briefing

Restraint response teams • Multidisciplinary teams to provide rapid response for acutely agitated or aggressive patients with mental health issues • Some Trusts have included anaesthetists as members of these teams • RCo. A with RCPsych has published guidance on anaesthetic involvement
RCo. A/RCPsych guidance on involvement of anaesthetists in restraint teams (2014) • • Anaesthetists should only act as part of a multi-disciplinary team including a psychiatrist Trainee anaesthetists should not be routinely involved in initiating chemical restraint except in an emergency Anaesthetists should receive appropriate training If rapid tranquillisation is required the minimum intervention possible according to local protocols CPR equipment & skilled assistance must be available Post sedation management & monitoring should be in a suitable venue by appropriately trained staff Post incident reflection & de-briefing to maximise learning http: //www. rcoa. ac. uk/news-and-bulletin/rcoa-news-andstatements/position-statement-the-involvement-of-anaesthetists
Summary • Public increasingly aware of the use and abuse of restrictive practices across all health & social care • Anaesthetists/intensivists face difficult situations requiring RIs in their traditional working environments and beyond • Need to increase awareness and training in all aspects of restrictive interventions to ensure safe and compassionate practice

Questions?