THE ADDITIONAL LATERAL TENODESIS OF THE KNEE EARLY
















- Slides: 71
THE ADDITIONAL LATERAL TENODESIS OF THE KNEE : EARLY RESULTS IN SOCCER PLAYERS Karachalios G. G. , Tamviskos A. , Krinas G. , Pavlides E. , Milionis G. Arthroscopic Surgery and Sports Injury dpt Metropolitan Hospital , Piraeus , Hellas Laertion Rehabilitation Center , Piraeus , Hellas
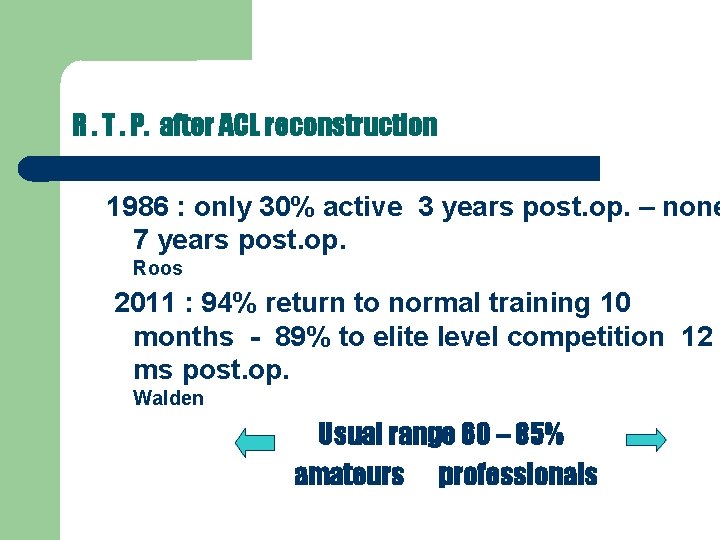
R. T. P. after ACL reconstruction 1986 : only 30% active 3 years post. op. – none 7 years post. op. Roos 2011 : 94% return to normal training 10 months - 89% to elite level competition 12 ms post. op. Walden Usual range 60 – 85% amateurs professionals
Which factors can explain these differences ?
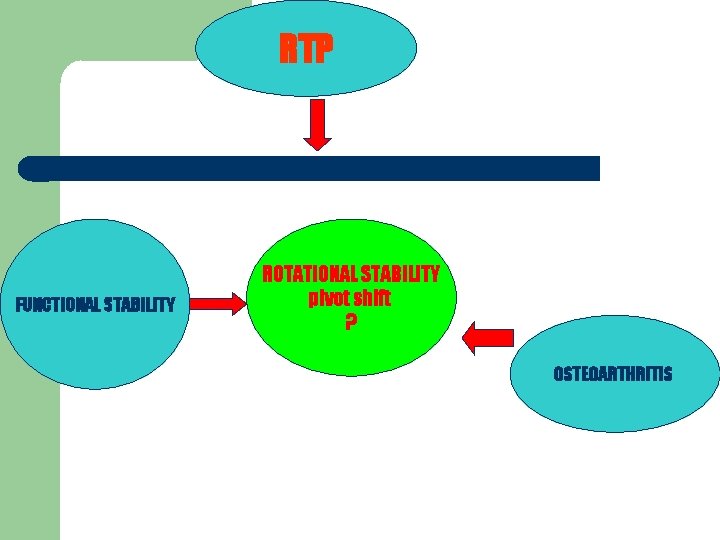
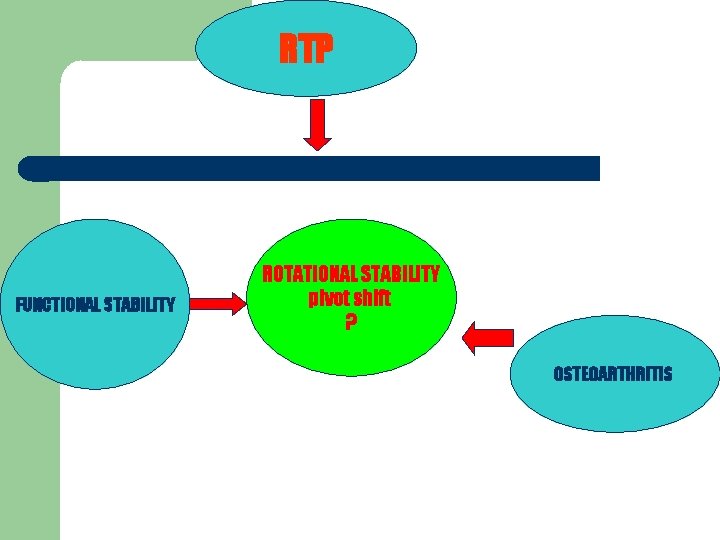
RTP FUNCTIONAL STABILITY ROTATIONAL STABILITY pivot shift ? OSTEOARTHRITIS
Recent studies correlate residual rotatory instability with decreased patient satisfaction , increase functional instability , chondromalacia and the development of osteoarthritis. . . Ayeni Tanaka positive pivot sign after ACL reconstruction is prognostic of o/a in the future. . . Jonsson restoring rotational kinematics during dynamic pivoting activities after ACL reconstruction is predictive of functional outcome. . . Zampeli , Pappas , Giotis , Hantes , Georgoulis 2012
But. . . ACL reconstruction , with graft either hamstrings or BTB , and with the recent techniques , can not restore the rotation of the tibia to the previous physiological levels during activities with increased rotational loading of the knee , although the abnormal anteroposterior tanslation of the tibia has been restablished Prof An. Georgoulis

Improved techniques ?
“ posterolateralization ” ? a more horizontal placement of the femoral tunnel , close to 10 o΄clock , which is anatomically closer to the insertion of the p/l bundle , can improve rotational stability , without full restoration Lucchetti
Double – bundle technique ? the anatomical double-bundle reconstruction can decrease the translation and rotation of the tibia during pivot-shift Zaffagnini there are no studies showing any major clinical advantages in terms of using the double-bundle surgical technique Meredick , Sammuelson technically demanding dependent on individual anatomical factors revision ?
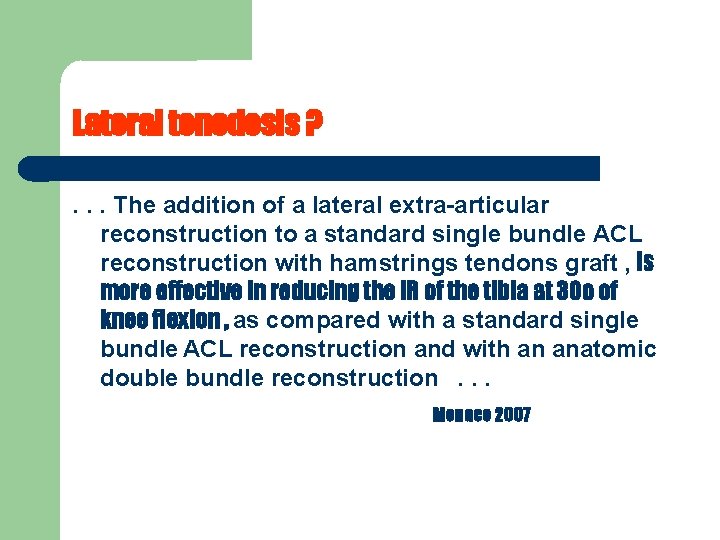
Lateral tenodesis ? . . . The addition of a lateral extra-articular reconstruction to a standard single bundle ACL reconstruction with hamstrings tendons graft , is more effective in reducing the IR of the tibia at 30 o of knee flexion , as compared with a standard single bundle ACL reconstruction and with an anatomic double bundle reconstruction. . . Monaco 2007
Results Isolated extra-articular tenodesis : only 50% of patients reported good to excellent results is no longer recommended ACL reconstruction and extra-articular tenodesis : 80 -90% good to excellent results Dodds ( review )

THE AIM OF THIS STUDY IS. . . To present our experience with this combined procedure regarding. . . The procedure itself The time of return to play The special issues ( if any ) during rehabilitation The stability of the knee and An early follow-up

MATERIAL 37 male soccer players Recent ( < 30 days ) ACL rupture 2014 : at least 12 months follow-up ( 12 – 21 ) 16 – 34 years old Level : 3 first division 16 second/third division 18 amateurs

CONCOMITANT INJURIES 20 meniscal injury 14 lateral 6 medial 8 chondral injuries 7 ICRS < II 1 ICRS III
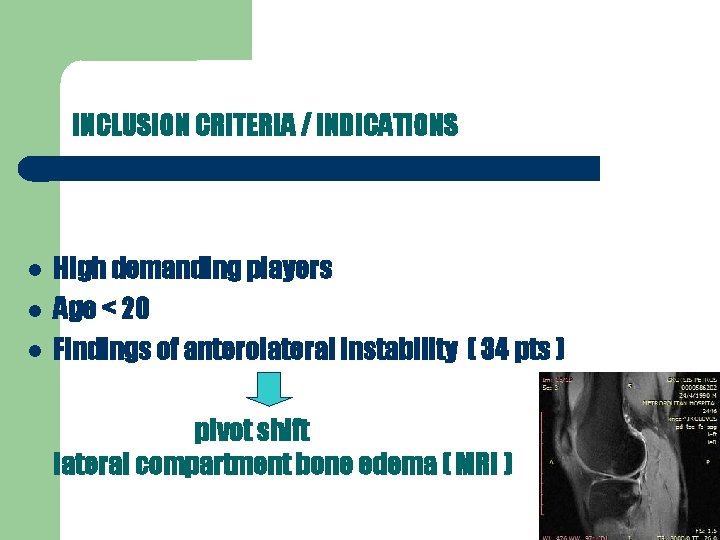
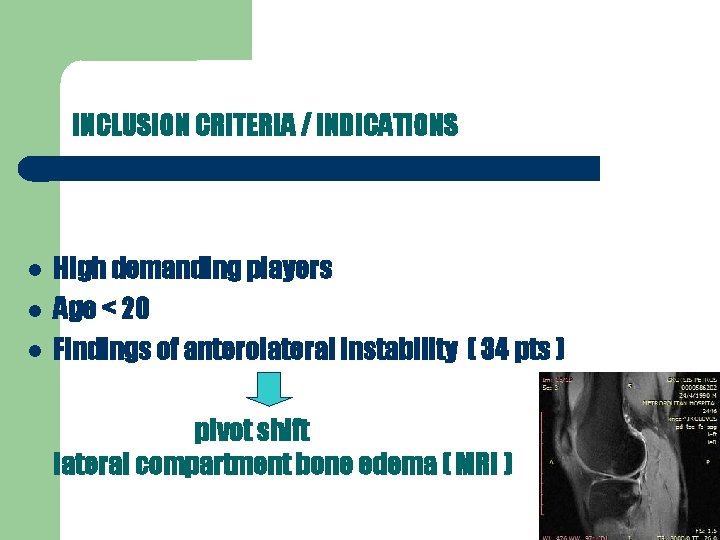
INCLUSION CRITERIA / INDICATIONS High demanding players Age < 20 Findings of anterolateral instability ( 34 pts ) pivot shift lateral compartment bone edema ( MRI )

SURGICAL TECHNIQUE : 4 - strand autologus ST/G tendon graft Retain and pull-out the torn ligament’s remnants Notchplasty “ monoloop ” lateral tenodesis knee in 20 -30 o fl ( initially 90 o ) and ex. rot. of the tibia 8 meniscal repair , 7 trimming and 5 partial meniscectomies. No any special treatment for the chondral injuries
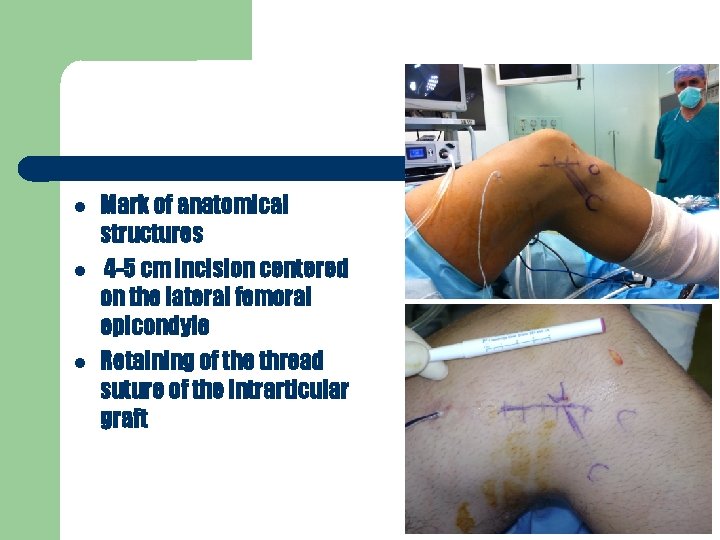
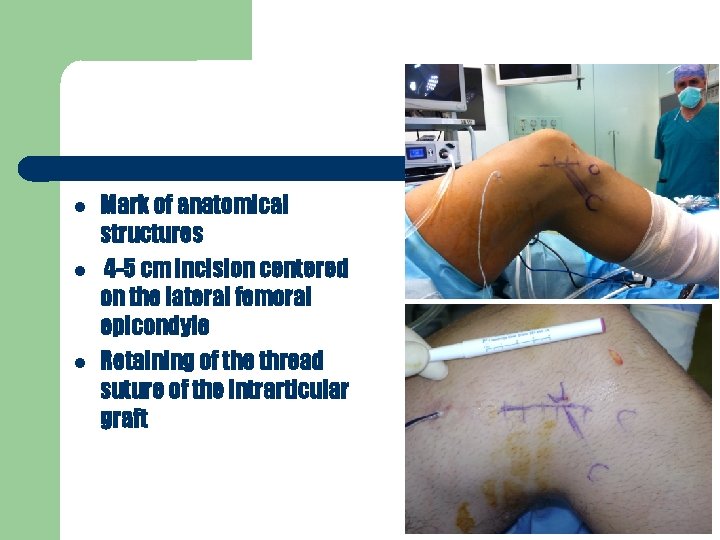
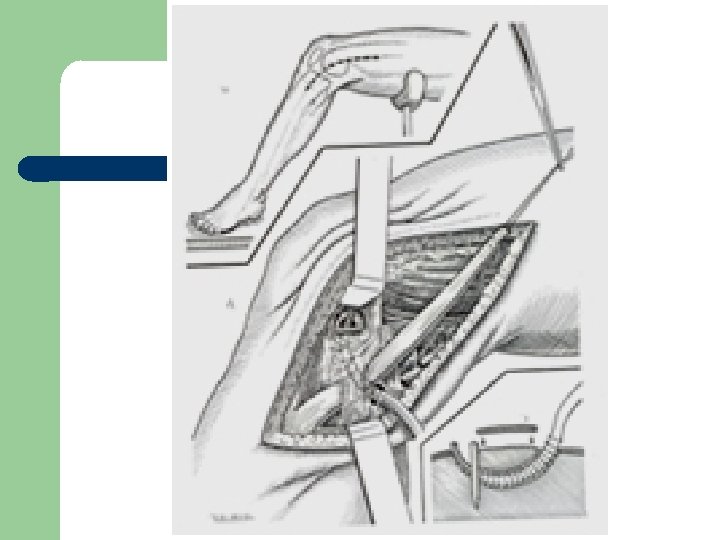
Mark of anatomical structures 4 -5 cm incision centered on the lateral femoral epicondyle Retaining of the thread suture of the intrarticular graft
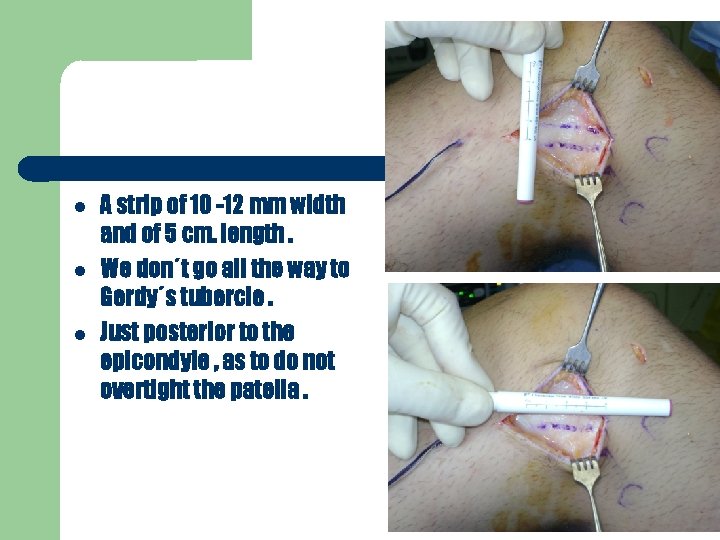
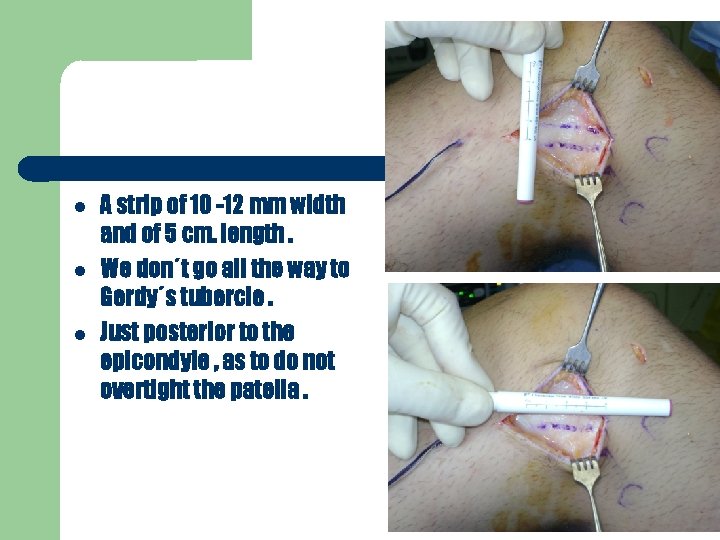
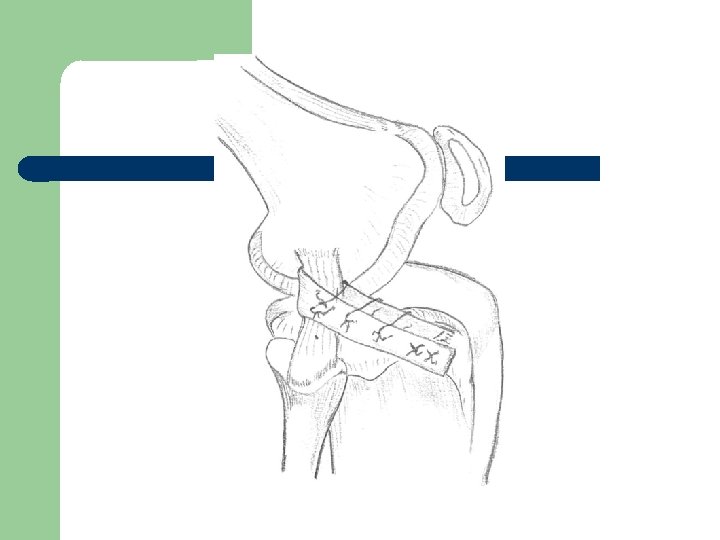
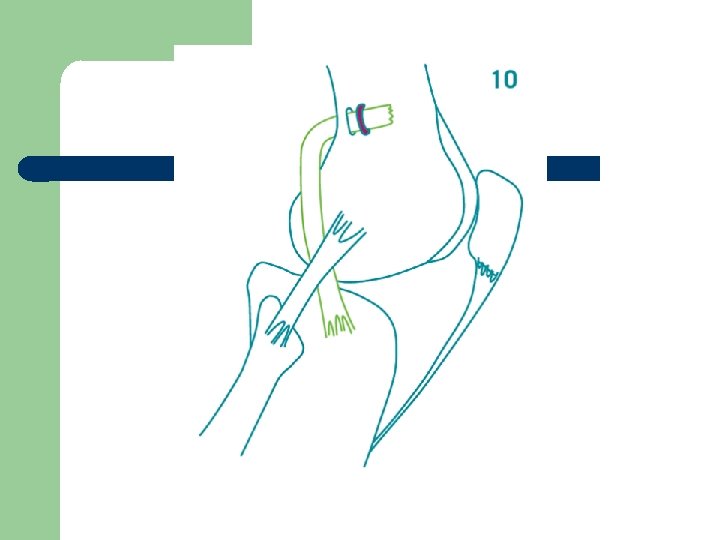
A strip of 10 -12 mm width and of 5 cm. length. We don΄t go all the way to Gerdy΄s tubercle. Just posterior to the epicondyle , as to do not overtight the patella.

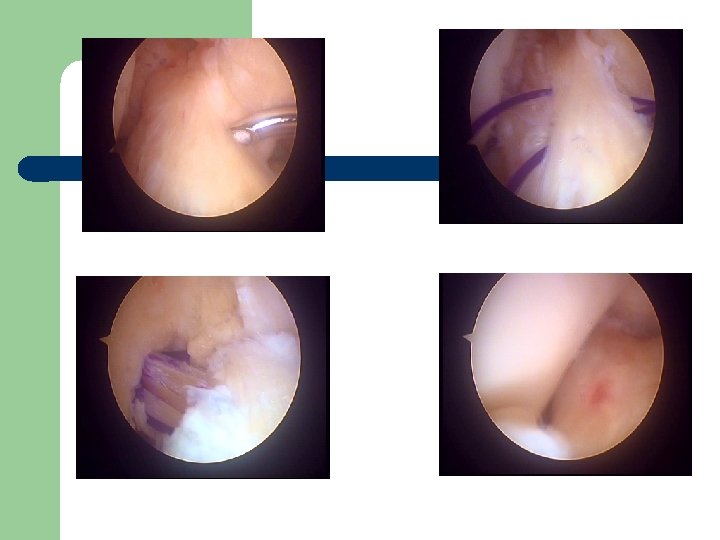
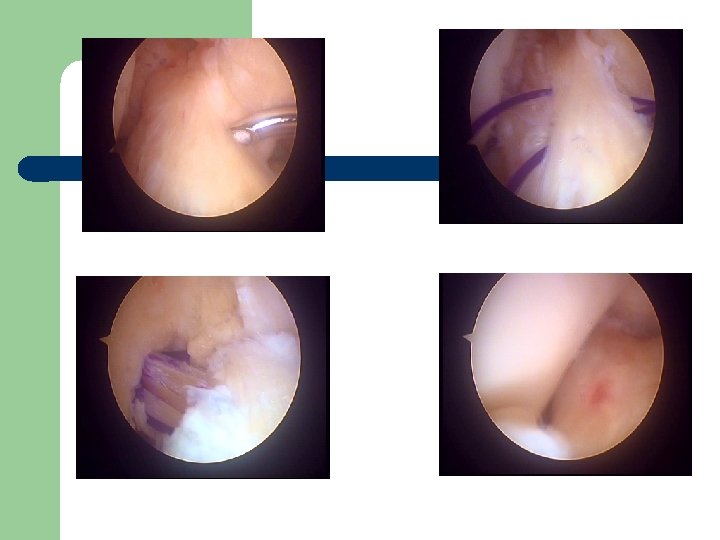
Find the lateral colateral ligament
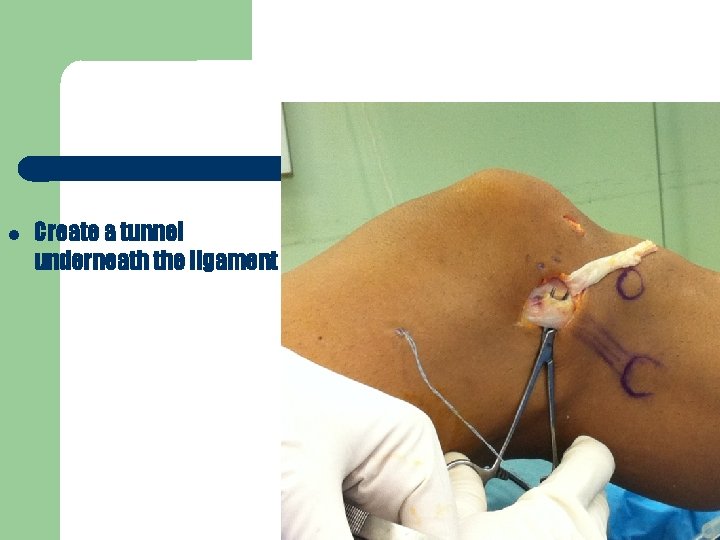
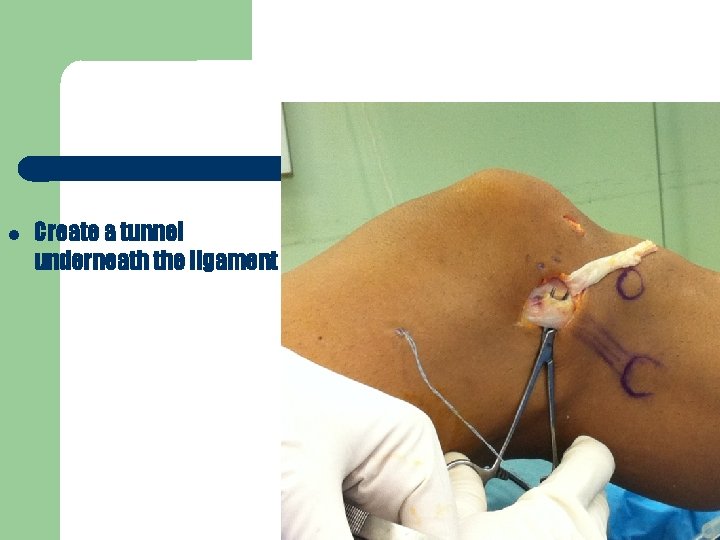
Create a tunnel underneath the ligament

Suturing of the end of the strip.
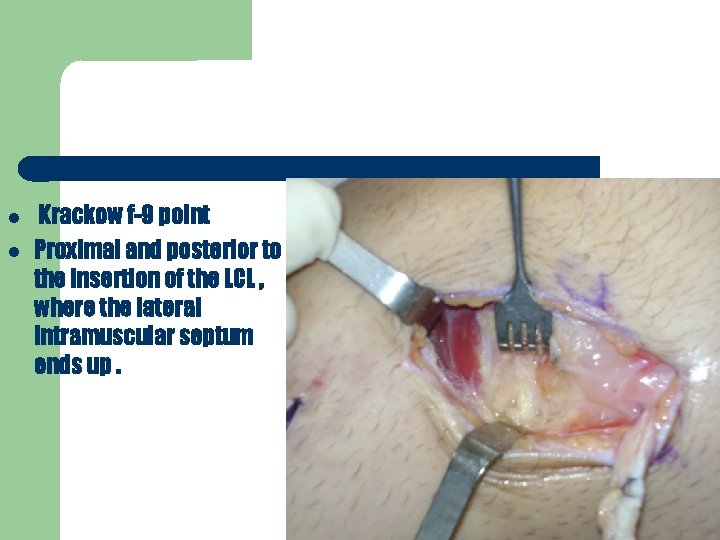
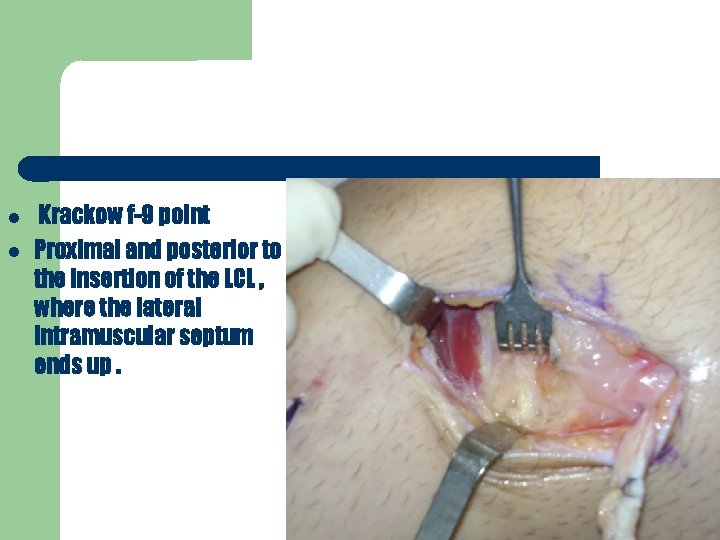
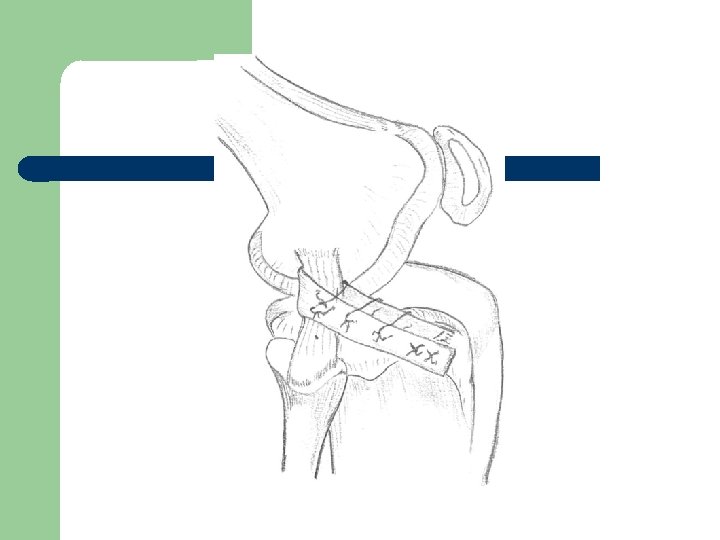
Krackow f-9 point Proximal and posterior to the insertion of the LCL , where the lateral intramuscular septum ends up.
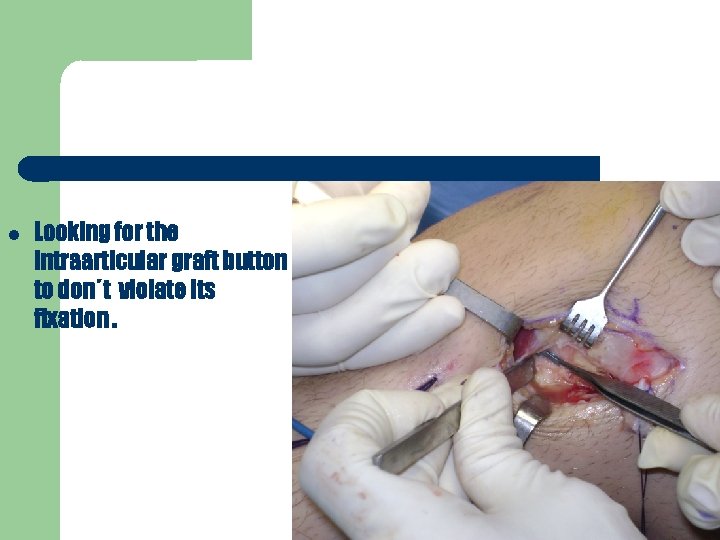
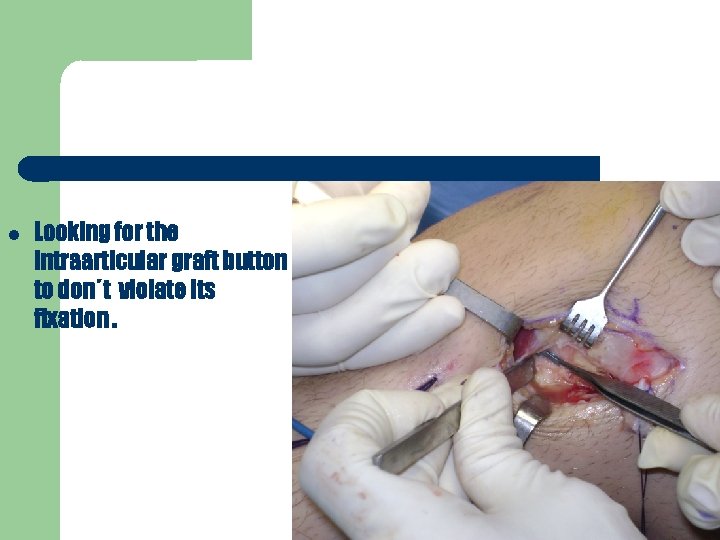
Looking for the intraarticular graft button to don΄t violate its fixation.
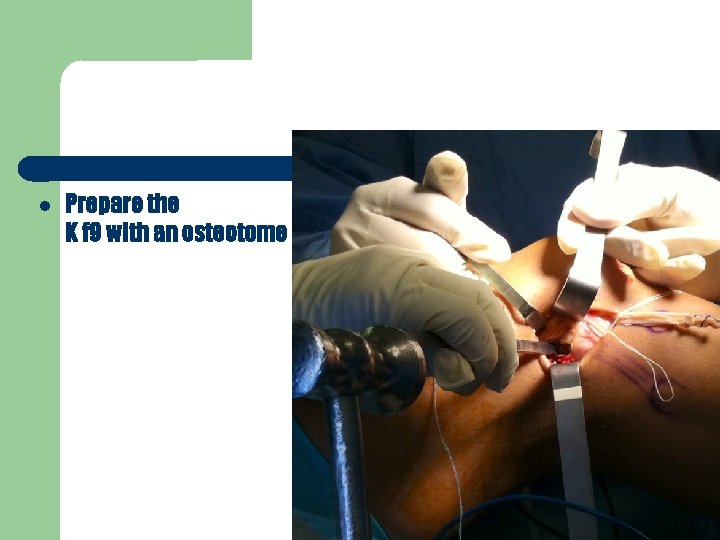
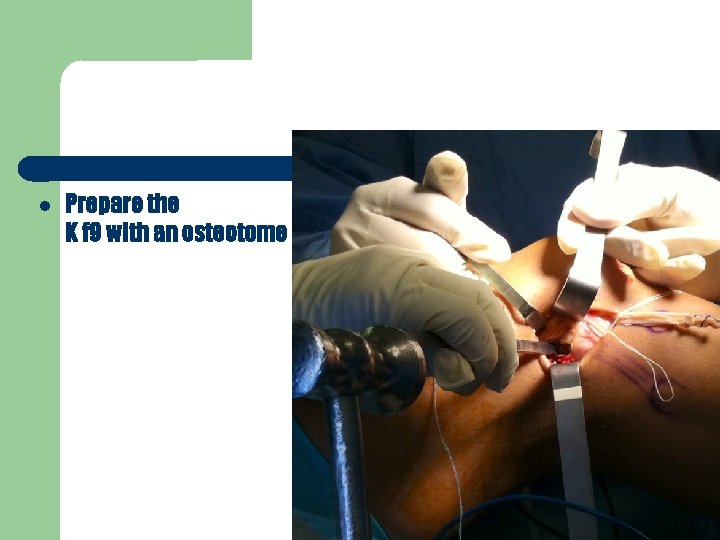
Prepare the K f 9 with an osteotome
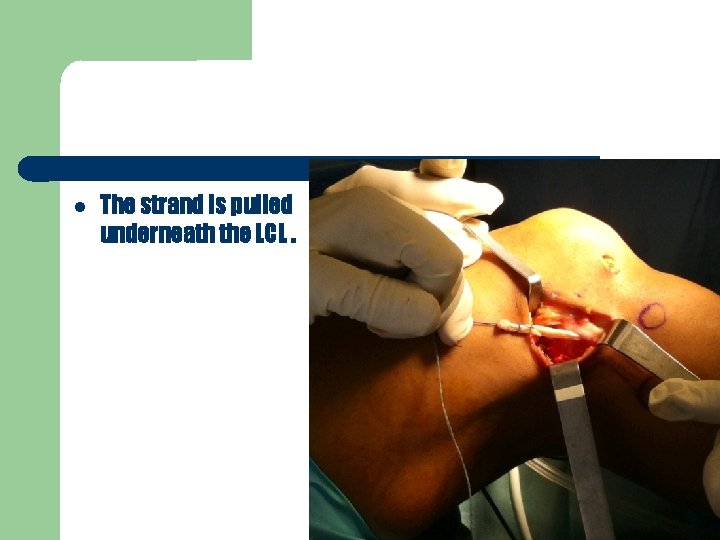
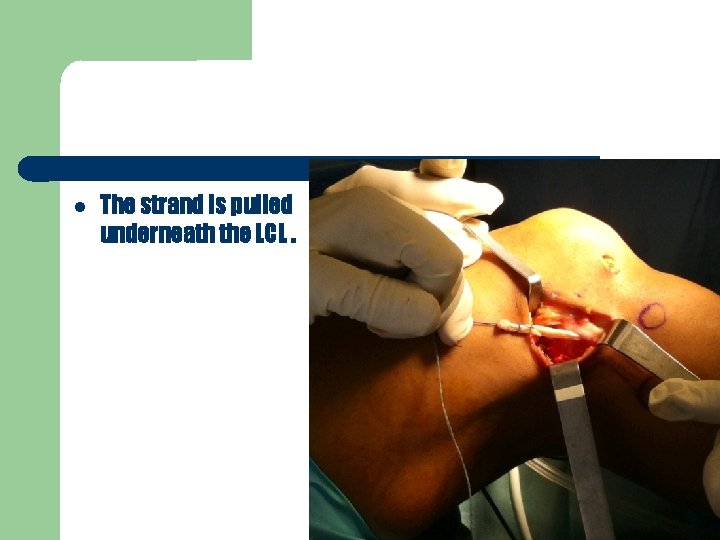
The strand is pulled underneath the LCL.
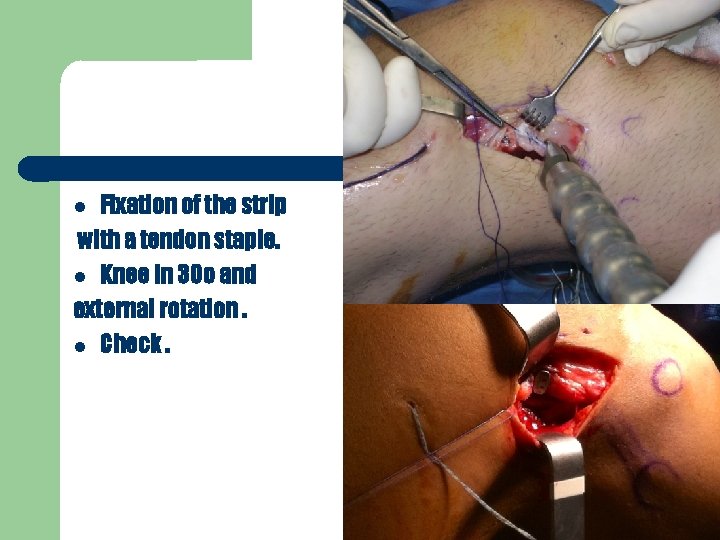
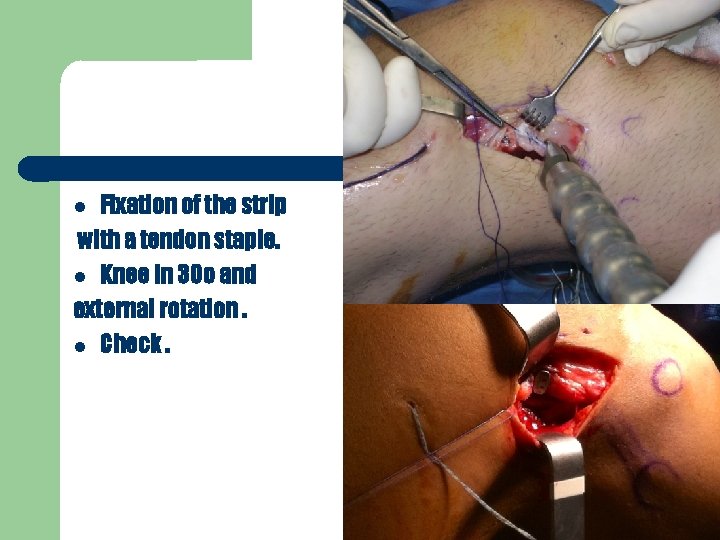
Fixation of the strip with a tendon staple. Knee in 30 o and external rotation. Check.
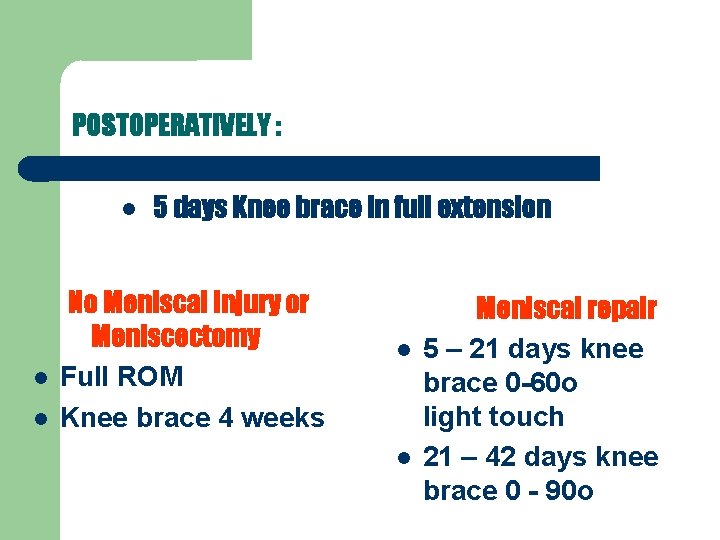
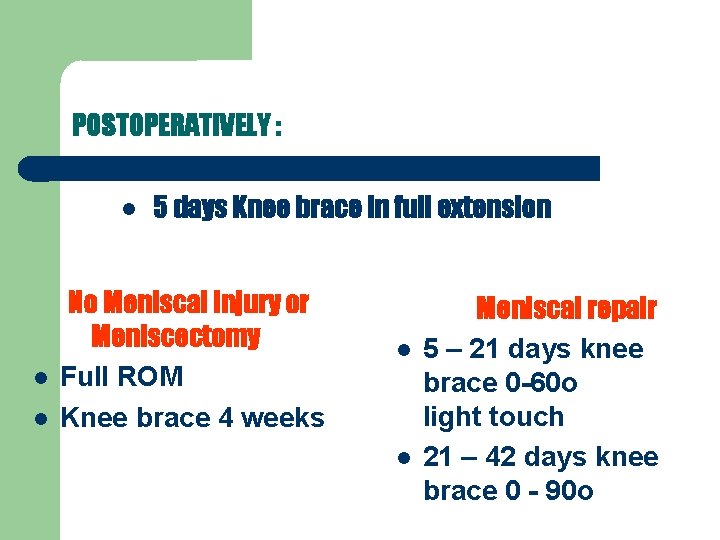
POSTOPERATIVELY : 5 days Knee brace in full extension No Meniscal injury or Meniscectomy Full ROM Knee brace 4 weeks Meniscal repair 5 – 21 days knee brace 0 -60 o light touch 21 – 42 days knee brace 0 - 90 o
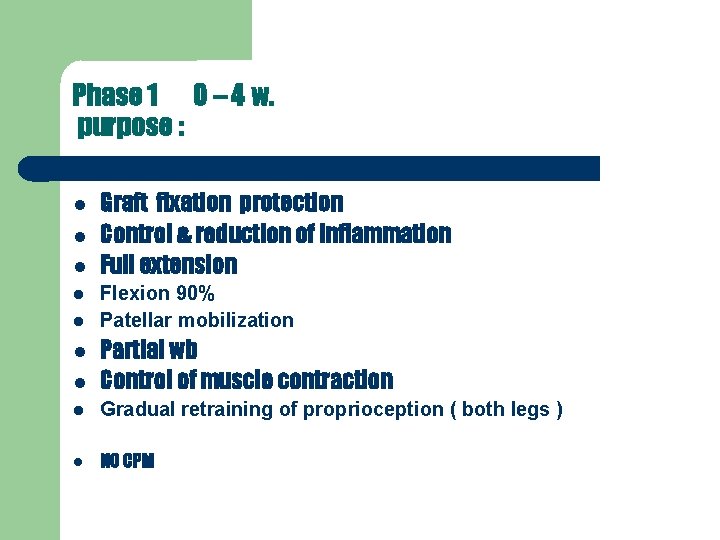
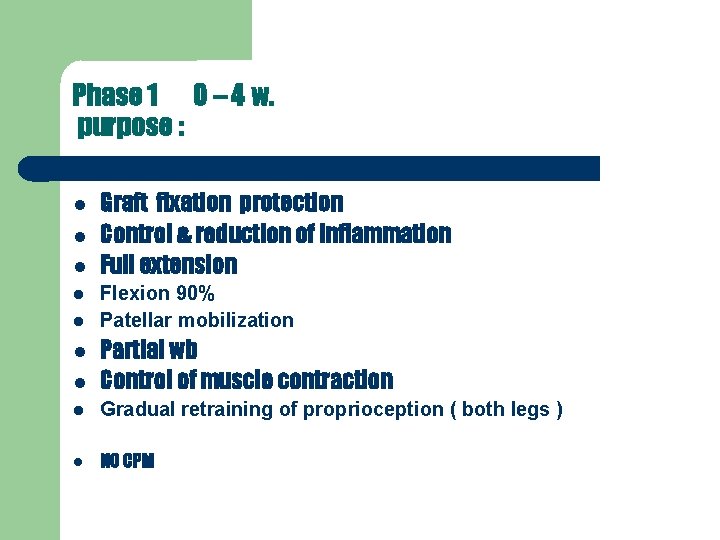
Phase 1 0 – 4 w. purpose : Graft fixation protection Control & reduction of inflammation Full extension Flexion 90% Patellar mobilization Partial wb Control of muscle contraction Gradual retraining of proprioception ( both legs ) NO CPM
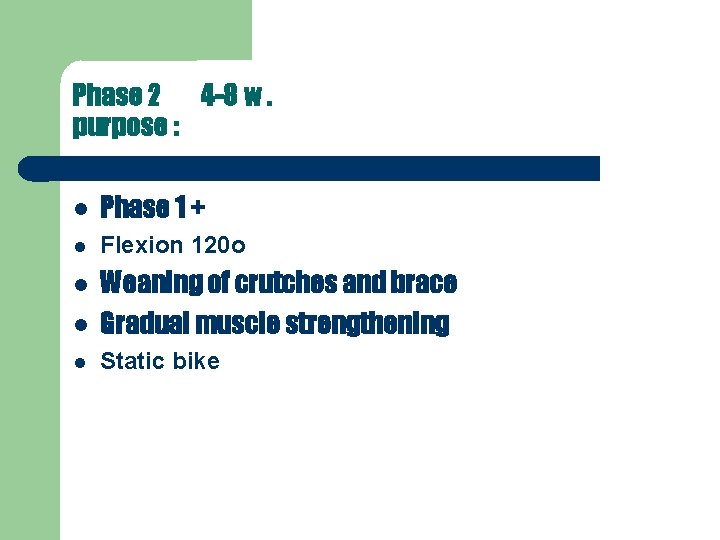
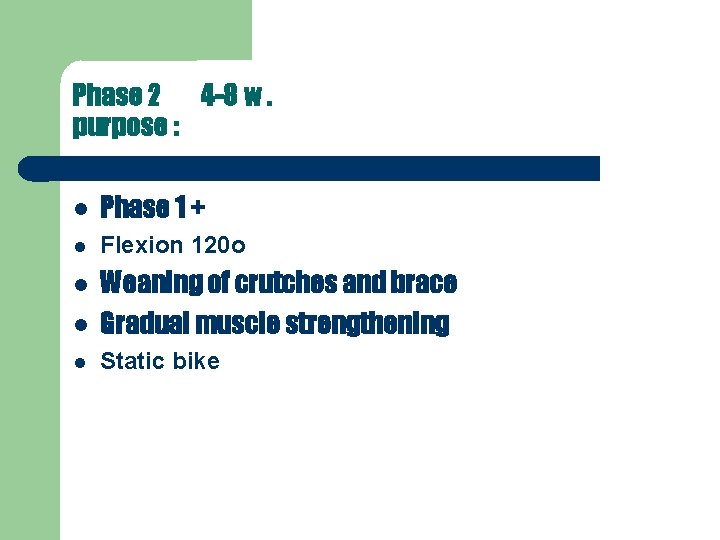
Phase 2 4 -8 w. purpose : Phase 1 + Flexion 120 o Weaning of crutches and brace Gradual muscle strengthening Static bike
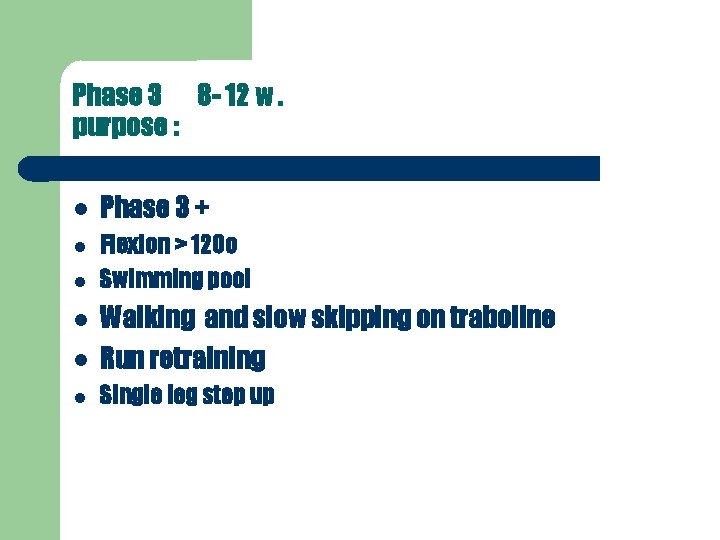
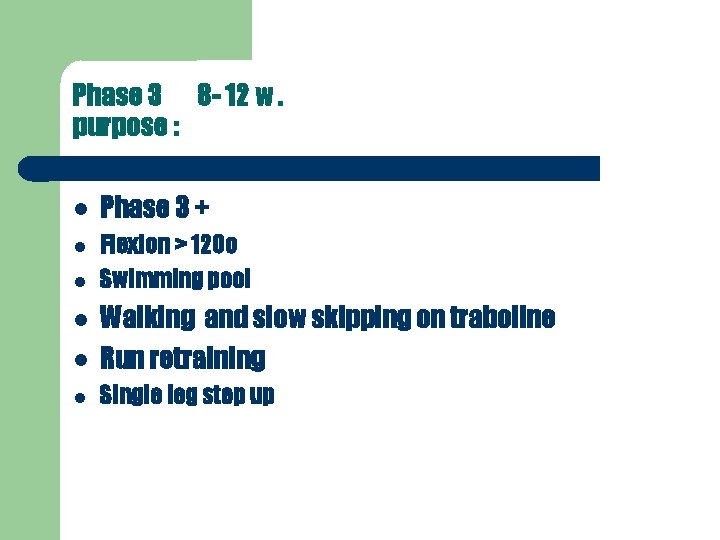
Phase 3 8 - 12 w. purpose : Phase 3 + Flexion > 120 o Swimming pool Walking and slow skipping on traboline Run retraining Single leg step up
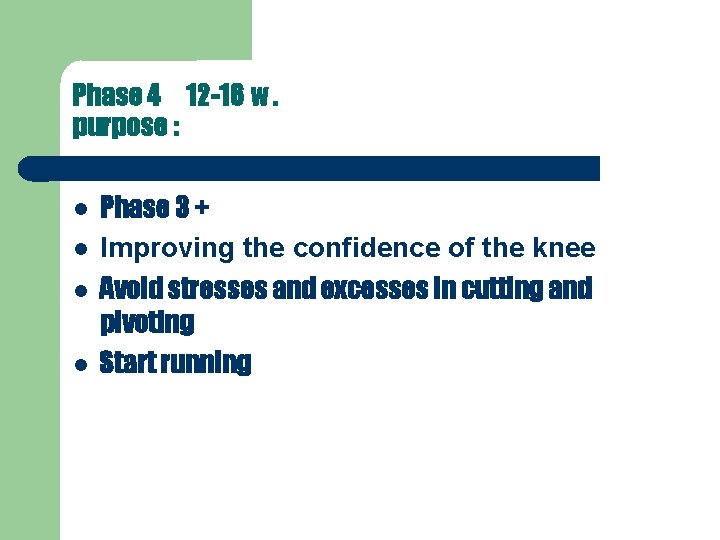
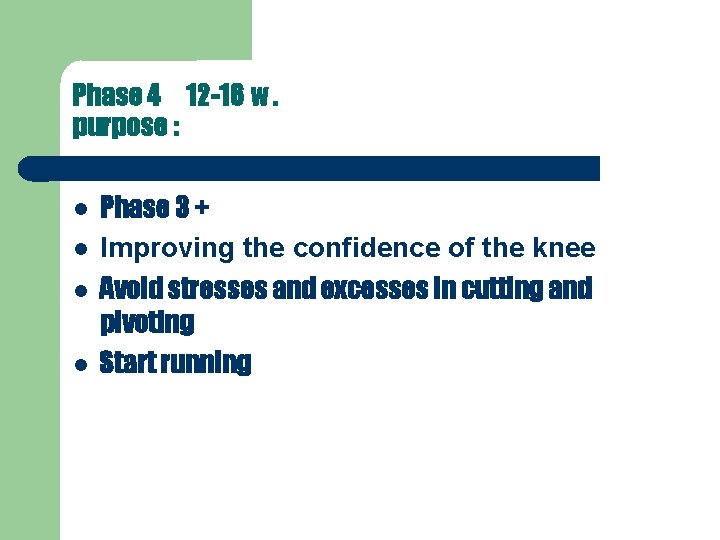
Phase 4 12 -16 w. purpose : Phase 3 + Improving the confidence of the knee Avoid stresses and excesses in cutting and pivoting Start running
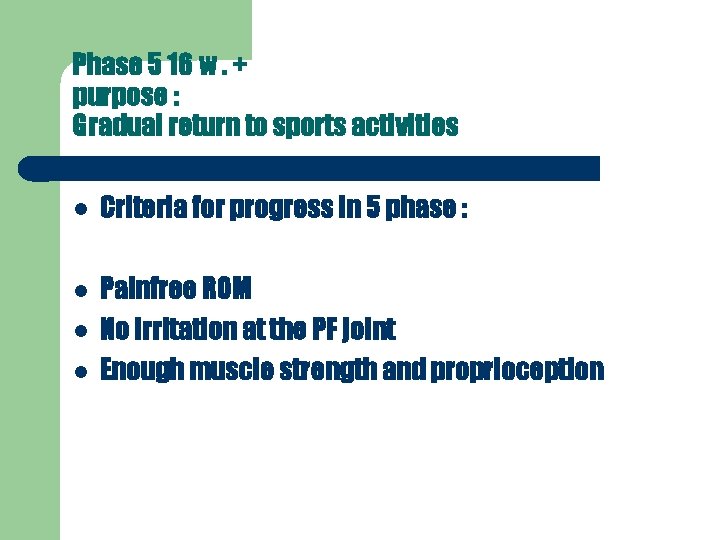
Phase 5 16 w. + purpose : Gradual return to sports activities Criteria for progress in 5 phase : Painfree ROM No irritation at the PF joint Enough muscle strength and proprioception

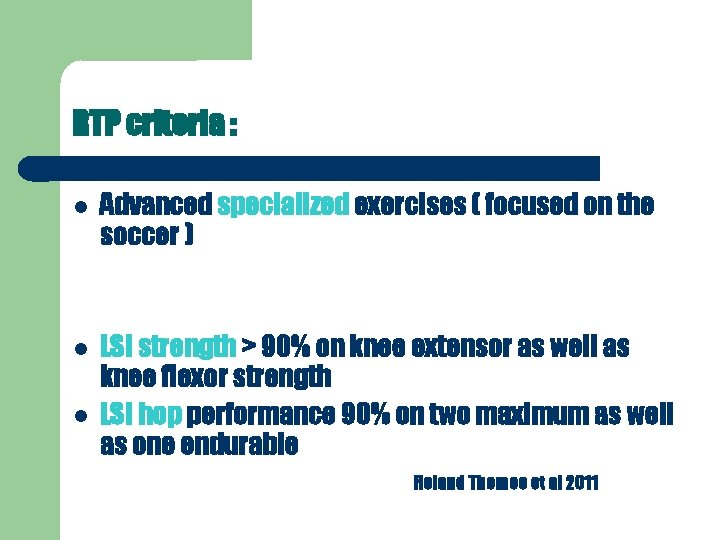
RTP criteria : Advanced specialized exercises ( focused on the soccer ) LSI strength > 90% on knee extensor as well as knee flexor strength LSI hop performance 90% on two maximum as well as one endurable Roland Thomee et al 2011

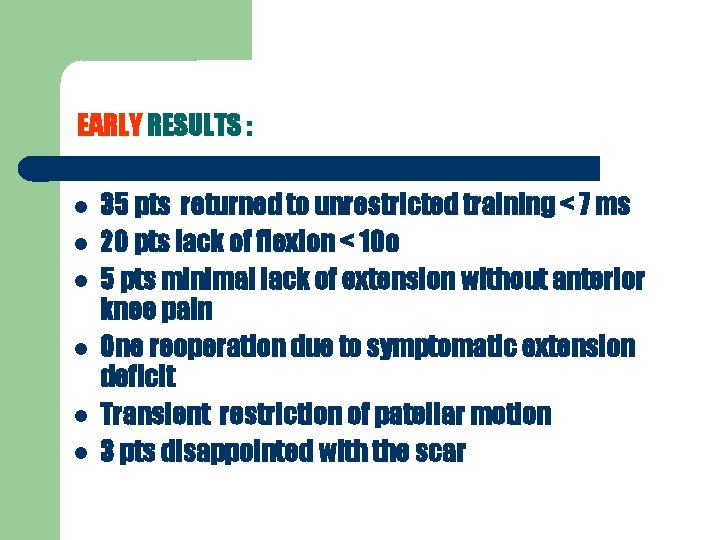
EARLY RESULTS : 35 pts returned to unrestricted training < 7 ms 20 pts lack of flexion < 10 o 5 pts minimal lack of extension without anterior knee pain One reoperation due to symptomatic extension deficit Transient restriction of patellar motion 3 pts disappointed with the scar
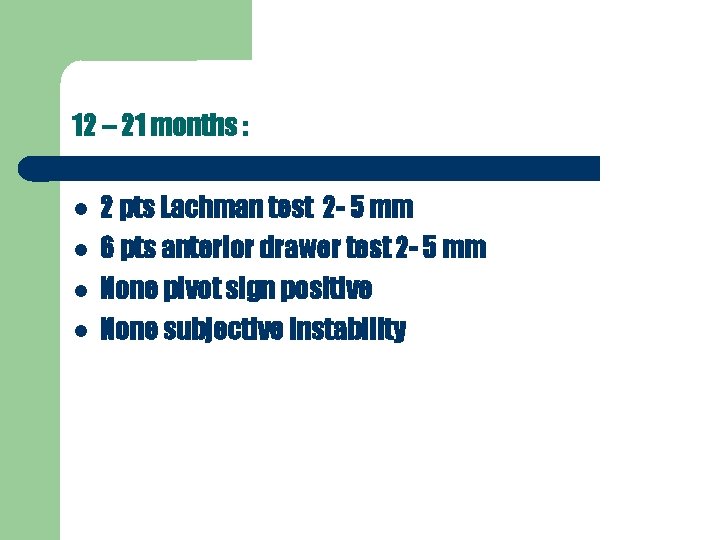
12 – 21 months : 2 pts Lachman test 2 - 5 mm 6 pts anterior drawer test 2 - 5 mm None pivot sign positive None subjective instability

12 – 21 months : No rerupture No meniscal repair failure No secondary chondral injury 21 footballers same team 11 same division 5 lower division
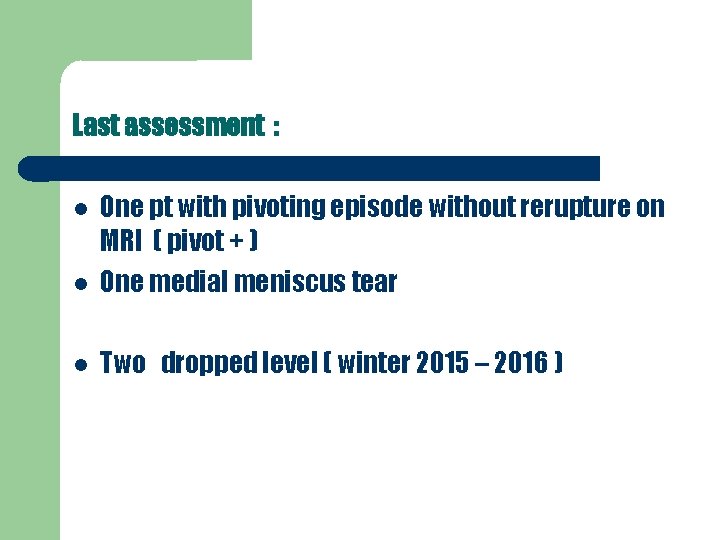
Last assessment : One pt with pivoting episode without rerupture on MRI ( pivot + ) One medial meniscus tear Two dropped level ( winter 2015 – 2016 )
In summary our EARLY results showed : Improved stability ( mainly in the last degrees of extension ) and protection of the knee Without elongation of the recovery time Slight delay in achieving full ROM Without any special demands Particularly for athletes with high demanding pivot and cutting activities ( such as footballers ) , the addition of lateral tenodesis provides a more stable knee and offers an unrestricted return to

Thank you and have a nice day
phase 3 purpose 4 -6 Phase 2 + Flexion 90 -120 o Weaning of crutches and brace Static bike
Phase 5 8 -12 Phase 4 + Gradual run retraining Slow skipping on the trampoline Single leg step up
… tibial rotation is not restored after ACL reconstruction with a hamstring allograft. . . Georgoulis et al. 2007
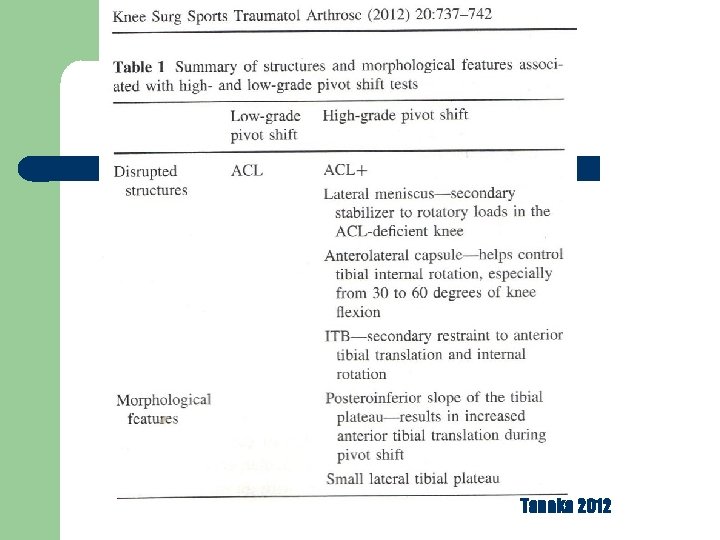
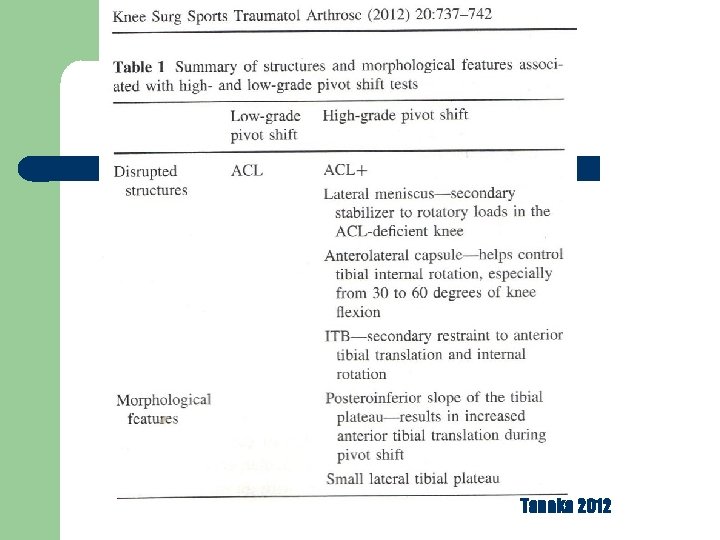
Tanaka 2012
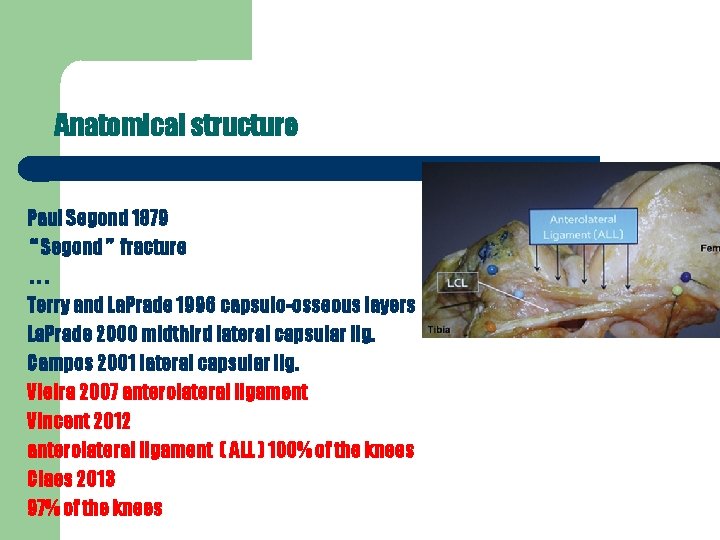
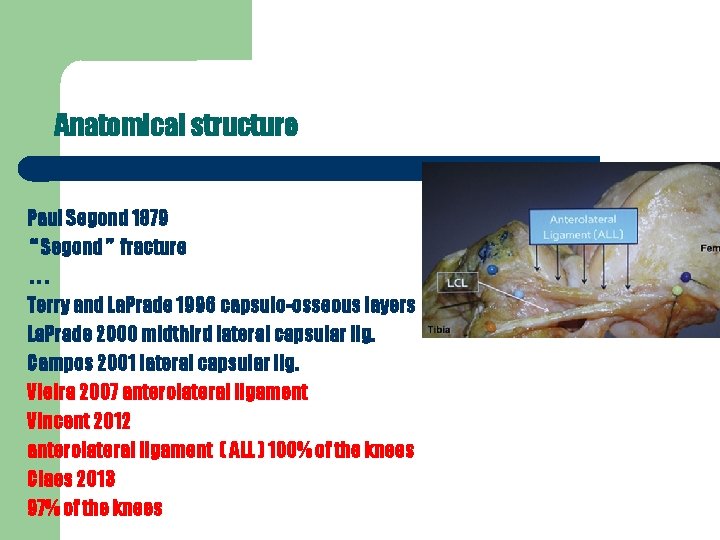
Anatomical structure Paul Segond 1879 “ Segond ” fracture. . . Terry and La. Prade 1996 capsulo-osseous layers La. Prade 2000 midthird lateral capsular lig. Campos 2001 lateral capsular lig. Vieira 2007 anterolateral ligament Vincent 2012 anterolateral ligament ( ΑLL ) 100% of the knees Claes 2013 97% of the knees

Biomechanical and anatomical reconstruction
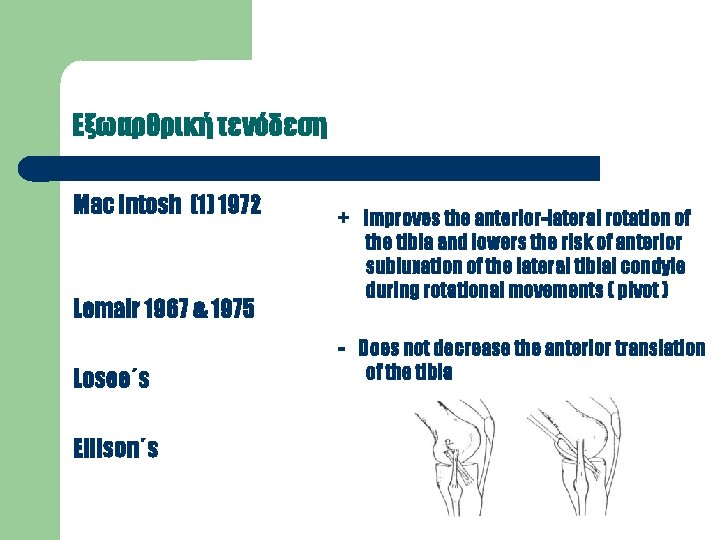
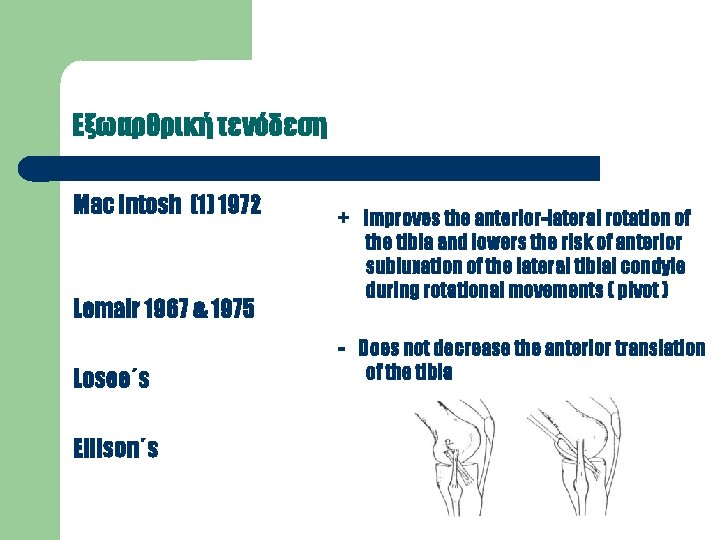
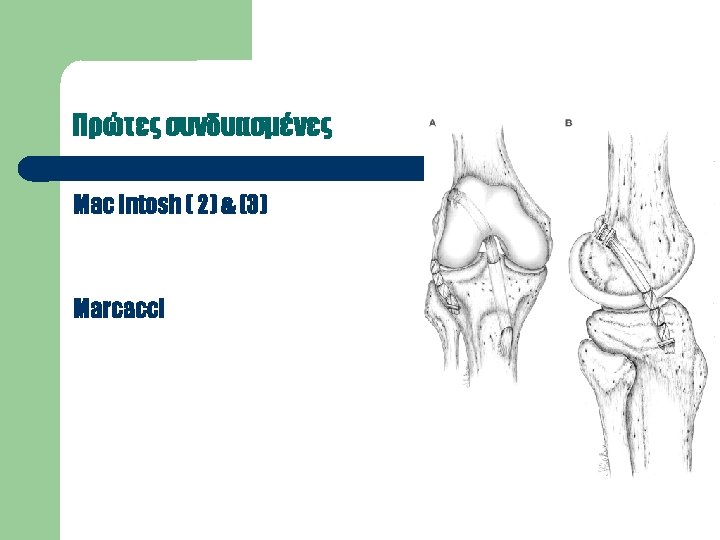
Εξωαρθρική τενόδεση Mac Intosh (1) 1972 Lemair 1967 & 1975 Losee΄s Ellison΄s + improves the anterior-lateral rotation of the tibia and lowers the risk of anterior subluxation of the lateral tibial condyle during rotational movements ( pivot ) - Does not decrease the anterior translation of the tibia
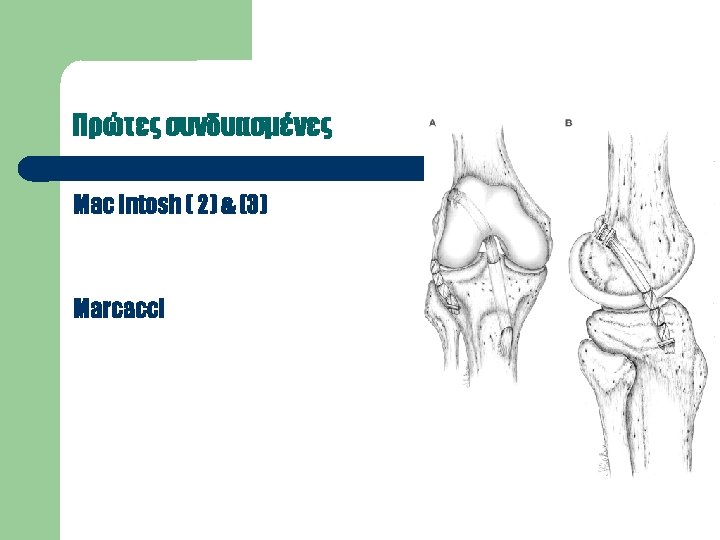
Combined techniques ( intra- and extra- ) Additional rotatory stability Improved control of the IR of the tibia « protection » of the intraarticular graft Engebretsen
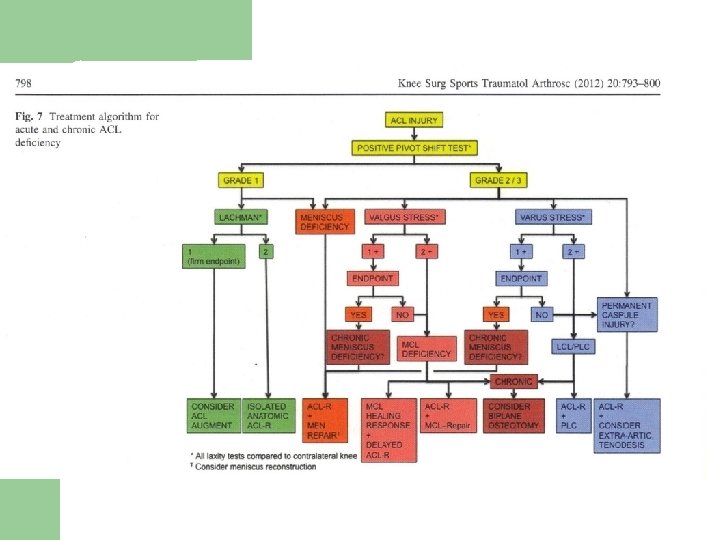
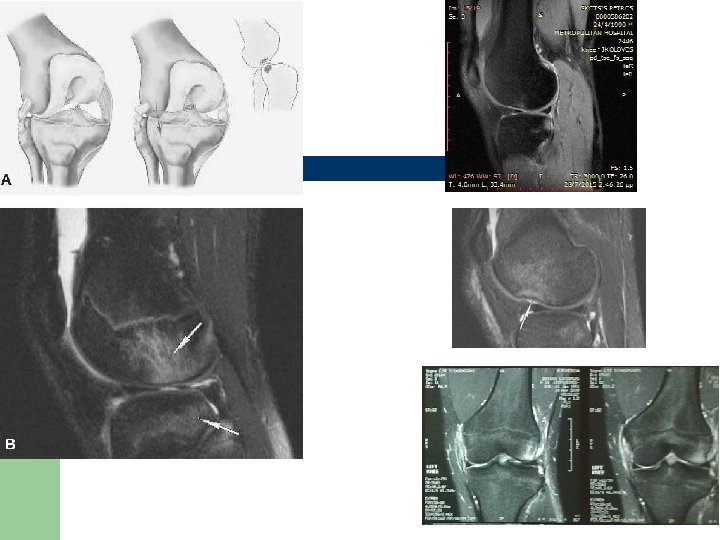
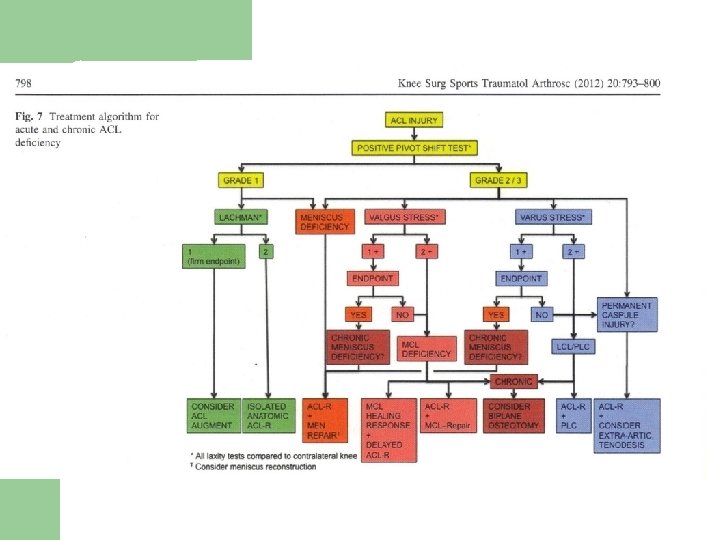
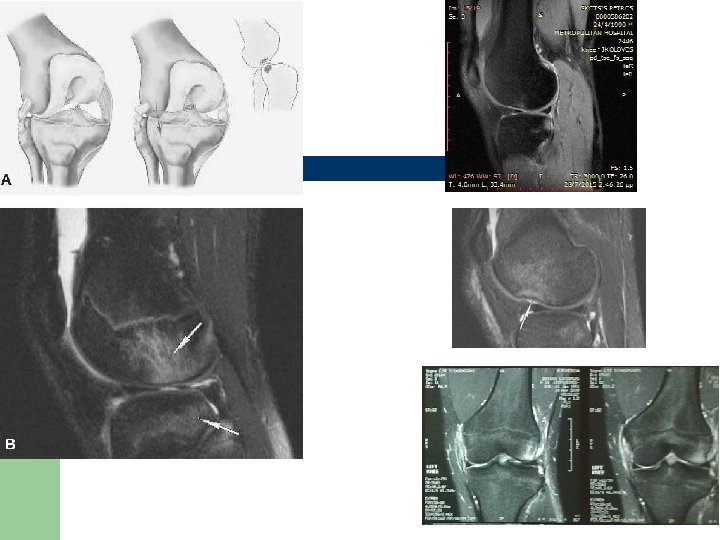
Criteria clinically High positive pivot sign imaging MRI bone bruising of the anterior-lateral femoral and posterior – lateral tibial condyle. X-Ray fracture Segond
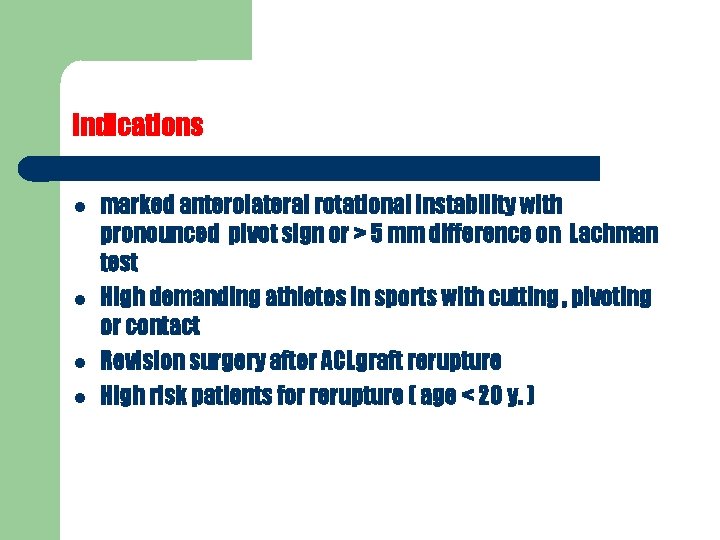
indications marked anterolateral rotational instability with pronounced pivot sign or > 5 mm difference on Lachman test High demanding athletes in sports with cutting , pivoting or contact Revision surgery after ACLgraft rerupture High risk patients for rerupture ( age < 20 y. )

In cases of using cadaveric allograft , particularly in revision surgery in combination with osteotomies and coexistant instability Patients with generalized joint laxity Women with valgus knee
Τechnique Strip of ITT with restoration of the distal insertion at Gerdy΄s tubercle 10 -12 mm width and 12 -18 cm of length Fixation : posterior and proximal of the insertion of the LCL – at the end of the lateral intramuscular septum ( Krakow f 9 point ) Monoloop ( shorter graft ) , doubleloop , tripleloop. fixaton in 30ο or 90ο flexion and the tibia in neutral position or external rotation The ITT strip is twisted 180 o

Results ACL Single-bundle and extra-articular tenodesis VS Double-bundle Reconstruction Slightly superior with combined procedure Monaco Similar , but better pivot and dynamic behavior with D-B. Zaffagnini
Results revision cases Addition of a lateral extra-articular tenodesis increases knee stability Trojani ( multicenter )
Conclusion The addition of a lateral tenodesis to a standard ACL S-B reconstruction improves rotational stability in high demands patients , in patients with marked pivot shift and in cases of revision ACL reconstruction.

Playing level Post. op. rehabilitation Time difference surgical technique ? Probably improvement of but. . . There are no studies showing a long – term difference in functional outcome between different surgical techniques such as the use of hamstring – or patellar tendon as grafts Ekstrand
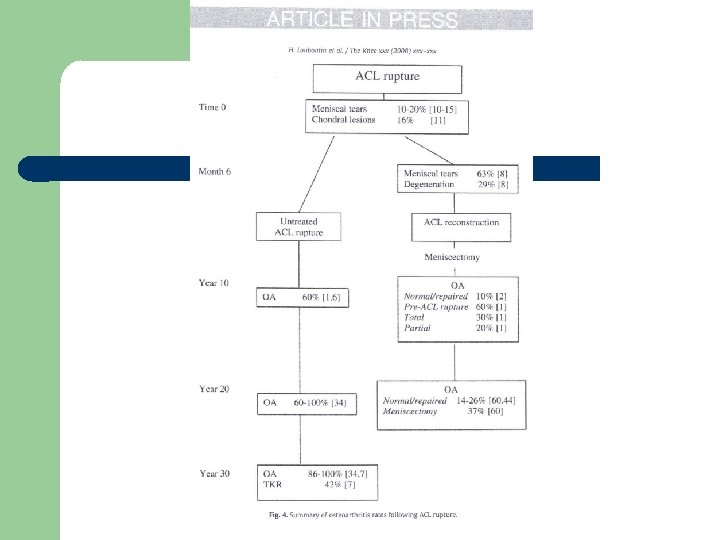
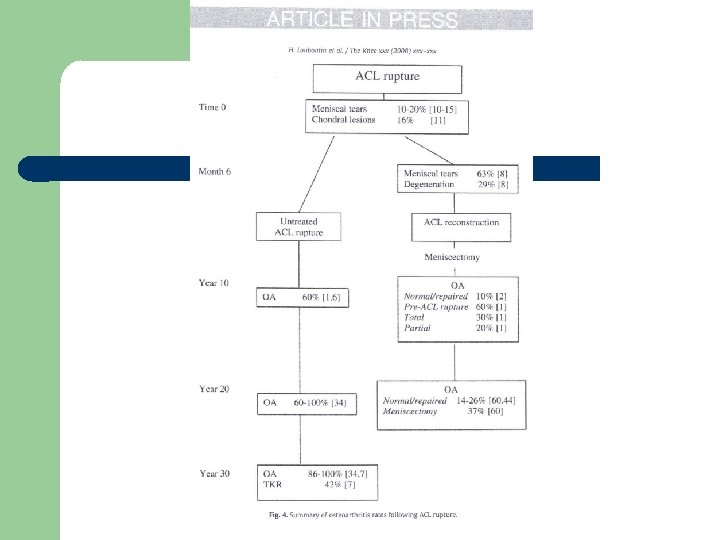
DEGENERATIVE CHANGES – O/A ACL reconstruction VS conservative treatment Risk factors : age sex BMI post injury time meniscectomy chondral lesions Type of graft technique

double – bundle technique ? improved control rotational stability through independent reconstruction and tensioning of the posterior – lateral bundle technically demanding dependent on individual anatomical factors