THE ADAPTIVE IMMUNE RESPONSE ADAPTIVE IMMUNE SYSTEM The

- Slides: 27

THE ADAPTIVE IMMUNE RESPONSE
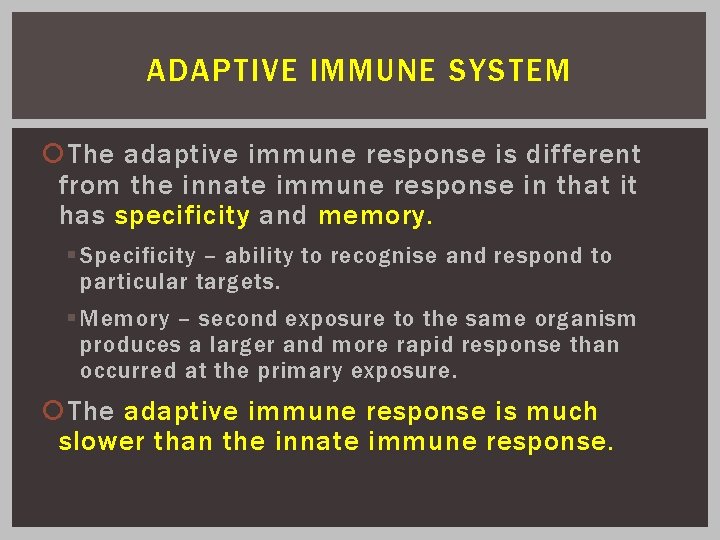
ADAPTIVE IMMUNE SYSTEM The adaptive immune response is different from the innate immune response in that it has specificity and memory. § Specificity – ability to recognise and respond to particular targets. § Memory – second exposure to the same organism produces a larger and more rapid response than occurred at the primary exposure. The adaptive immune response is much slower than the innate immune response.
ADAPTIVE IMMUNE SYSTEM Lymphocytes are the effector cells of the adaptive immune system. They display highly diverse receptors for antigen. Each cell has multiple copies of a receptor for a single antigen only, and thus responds only to one antigen. Antigens are molecules which are recognised by receptors on lymphocytes, and elicit a specific immune response to that antigen. Antigen presenting cells (APCs) collect antigens from infected tissues, and carry to lymphoid tissues to display and activate lymphoid cells. Cytokines act as messengers between cells of the immune system.
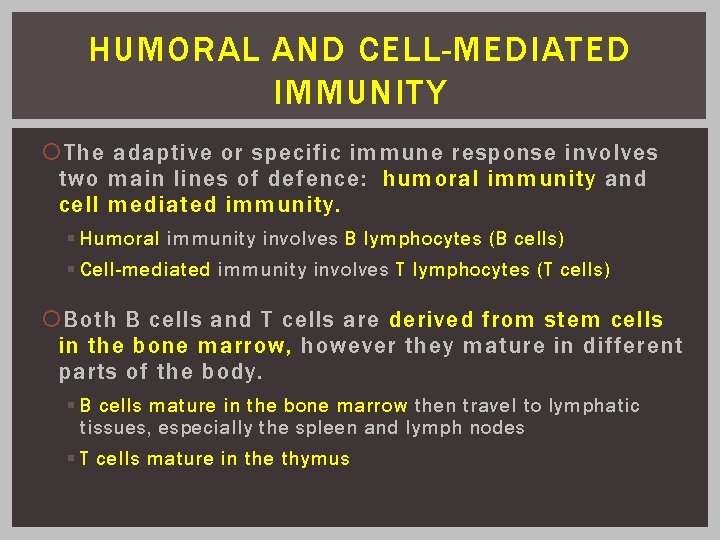
HUMORAL AND CELL-MEDIATED IMMUNITY The adaptive or specific immune response involves two main lines of defence: humoral immunity and cell mediated immunity. § Humoral immunity involves B lymphocytes (B cells) § Cell-mediated immunity involves T lymphocytes (T cells) Both B cells and T cells are derived from stem cells in the bone marrow, however they mature in different parts of the body. § B cells mature in the bone marrow then travel to lymphatic tissues, especially the spleen and lymph nodes § T cells mature in the thymus
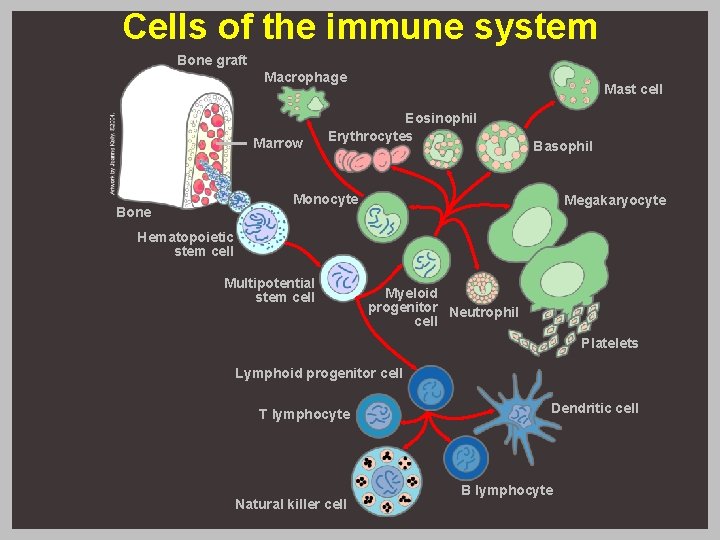
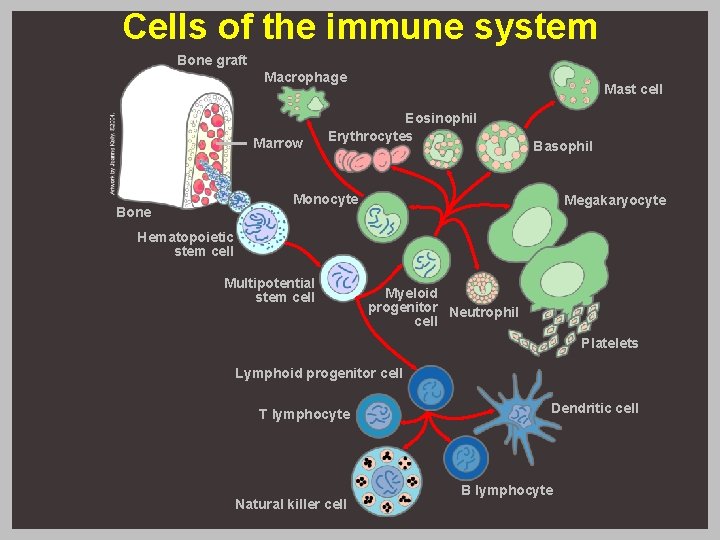
Cells of the immune system Bone graft Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Natural killer cell Dendritic cell B lymphocyte
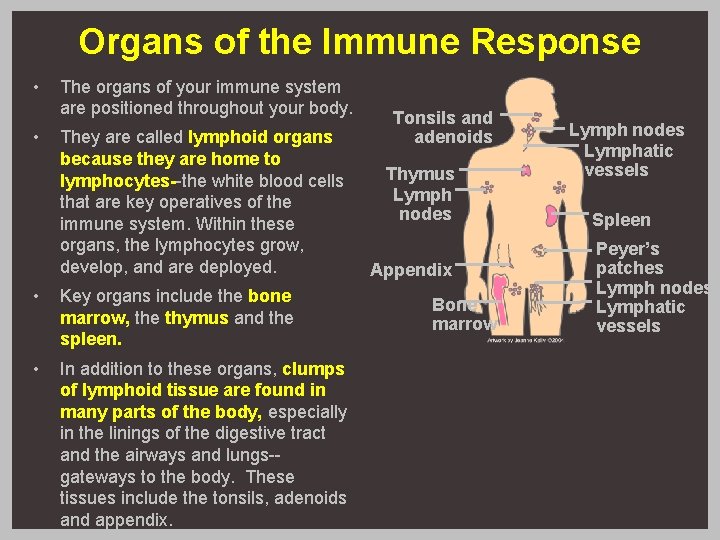
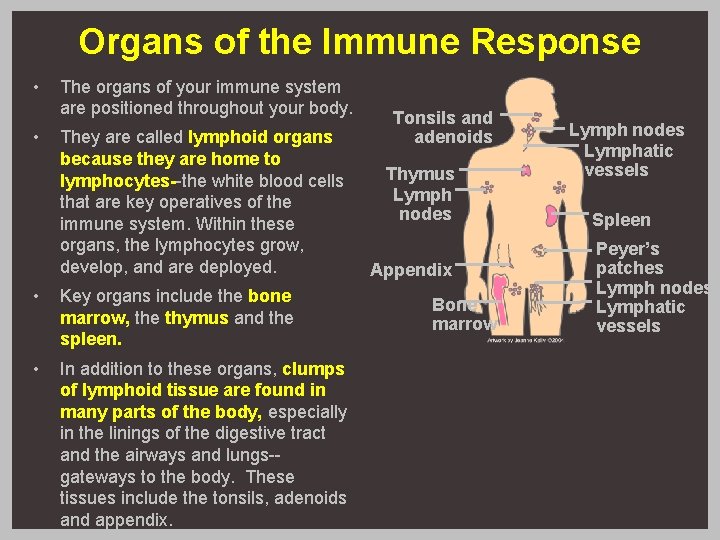
Organs of the Immune Response • • The organs of your immune system are positioned throughout your body. They are called lymphoid organs because they are home to lymphocytes--the white blood cells that are key operatives of the immune system. Within these organs, the lymphocytes grow, develop, and are deployed. • Key organs include the bone marrow, the thymus and the spleen. • In addition to these organs, clumps of lymphoid tissue are found in many parts of the body, especially in the linings of the digestive tract and the airways and lungs-gateways to the body. These tissues include the tonsils, adenoids and appendix. Tonsils and adenoids Thymus Lymph nodes Appendix Bone marrow Lymph nodes Lymphatic vessels Spleen Peyer’s patches Lymph nodes Lymphatic vessels
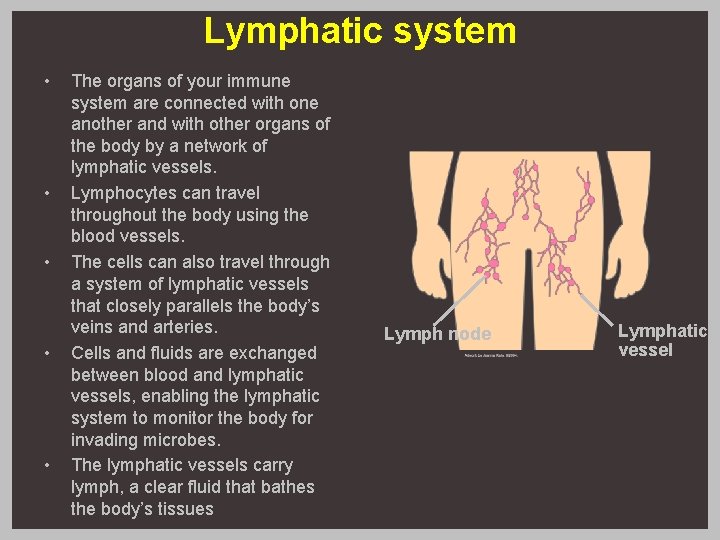
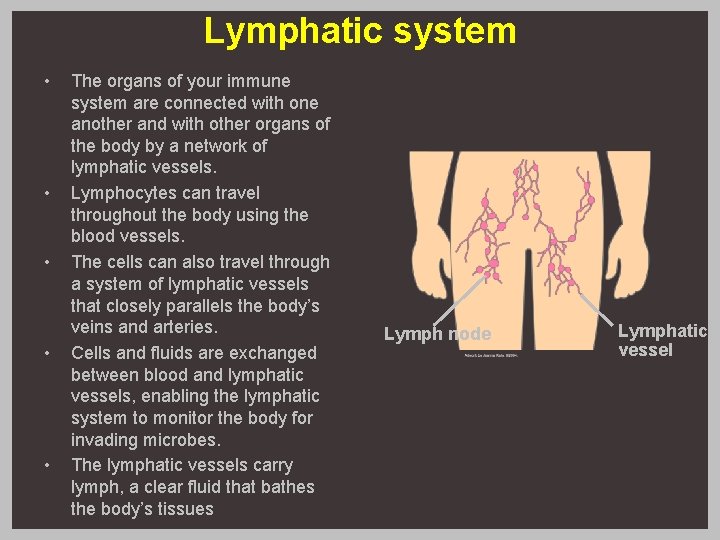
Lymphatic system • • • The organs of your immune system are connected with one another and with other organs of the body by a network of lymphatic vessels. Lymphocytes can travel throughout the body using the blood vessels. The cells can also travel through a system of lymphatic vessels that closely parallels the body’s veins and arteries. Cells and fluids are exchanged between blood and lymphatic vessels, enabling the lymphatic system to monitor the body for invading microbes. The lymphatic vessels carry lymph, a clear fluid that bathes the body’s tissues Lymph node Lymphatic vessel
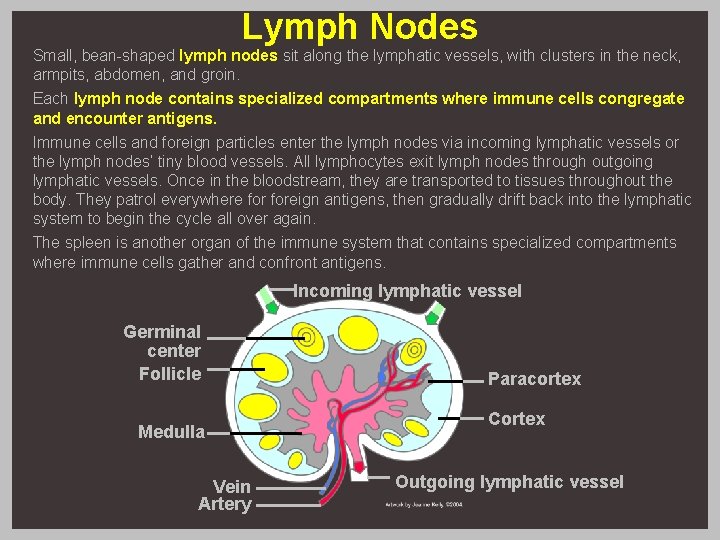
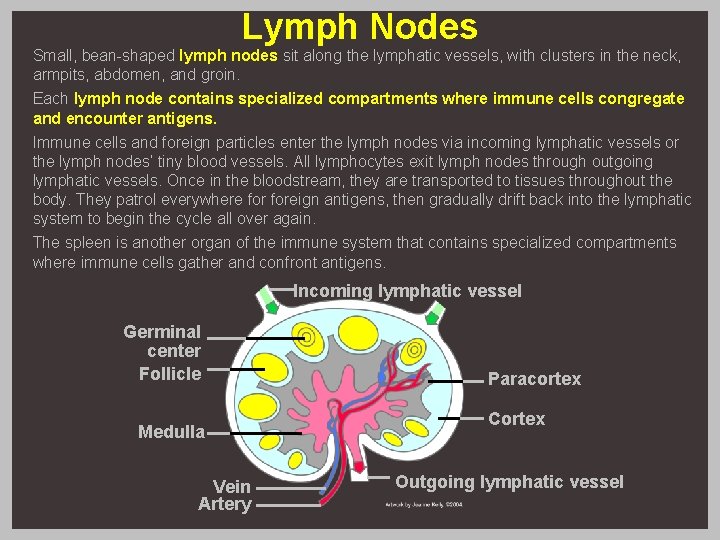
Lymph Nodes Small, bean-shaped lymph nodes sit along the lymphatic vessels, with clusters in the neck, armpits, abdomen, and groin. Each lymph node contains specialized compartments where immune cells congregate and encounter antigens. Immune cells and foreign particles enter the lymph nodes via incoming lymphatic vessels or the lymph nodes’ tiny blood vessels. All lymphocytes exit lymph nodes through outgoing lymphatic vessels. Once in the bloodstream, they are transported to tissues throughout the body. They patrol everywhere foreign antigens, then gradually drift back into the lymphatic system to begin the cycle all over again. The spleen is another organ of the immune system that contains specialized compartments where immune cells gather and confront antigens. Incoming lymphatic vessel Germinal center Follicle Medulla Vein Artery Paracortex Cortex Outgoing lymphatic vessel
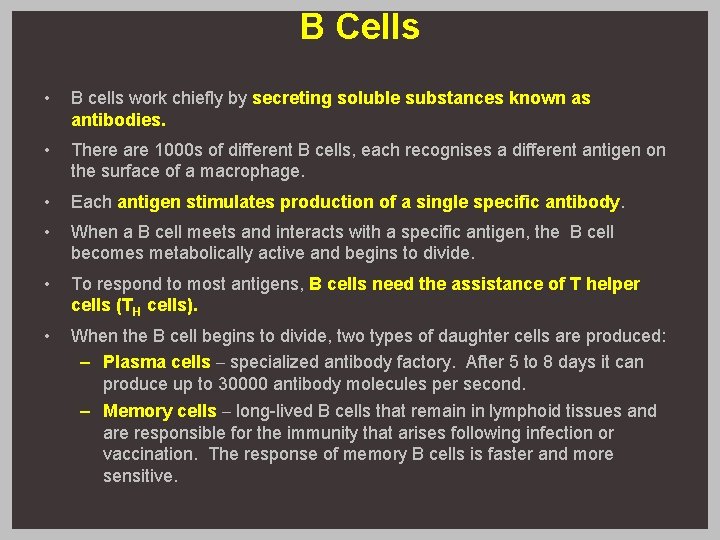
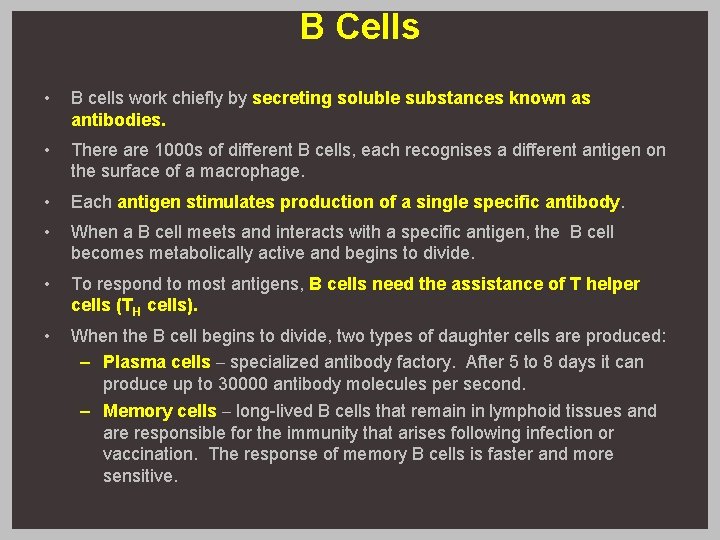
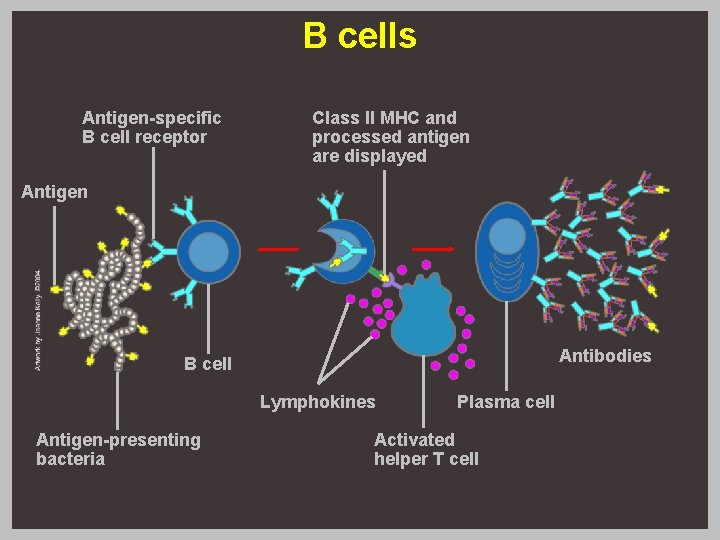
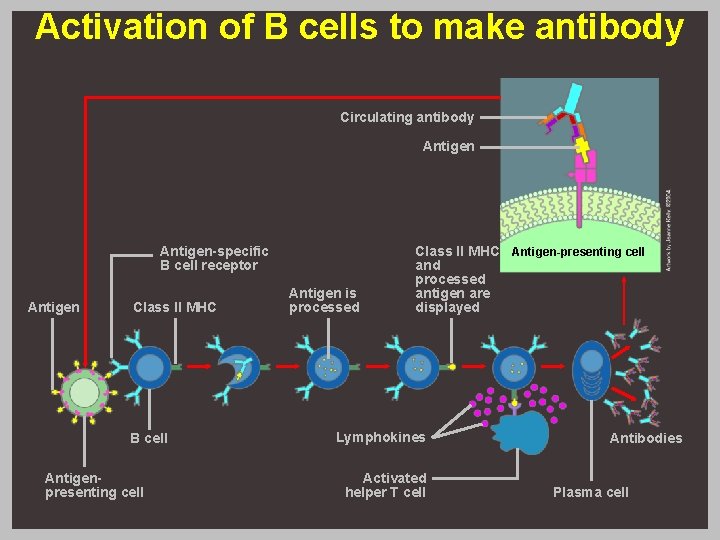
B Cells • B cells work chiefly by secreting soluble substances known as antibodies. • There are 1000 s of different B cells, each recognises a different antigen on the surface of a macrophage. • Each antigen stimulates production of a single specific antibody. • When a B cell meets and interacts with a specific antigen, the B cell becomes metabolically active and begins to divide. • To respond to most antigens, B cells need the assistance of T helper cells (TH cells). • When the B cell begins to divide, two types of daughter cells are produced: – Plasma cells – specialized antibody factory. After 5 to 8 days it can produce up to 30000 antibody molecules per second. – Memory cells – long-lived B cells that remain in lymphoid tissues and are responsible for the immunity that arises following infection or vaccination. The response of memory B cells is faster and more sensitive.
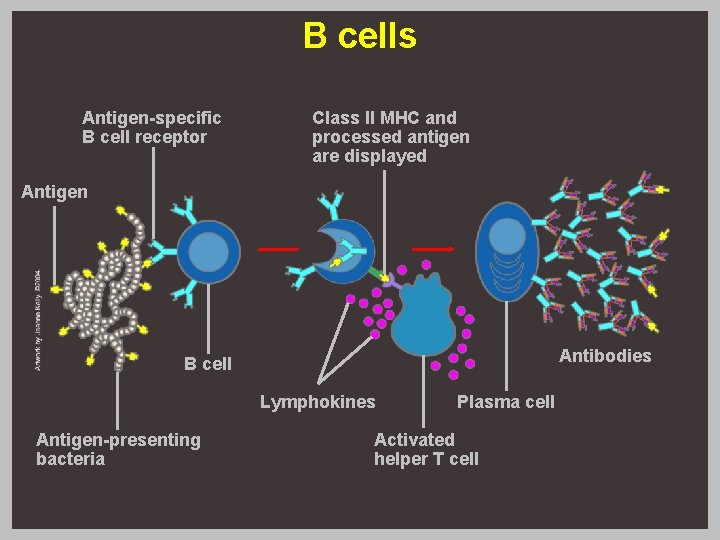
B cells Antigen-specific B cell receptor Class II MHC and processed antigen are displayed Antigen Antibodies B cell Lymphokines Antigen-presenting bacteria Plasma cell Activated helper T cell
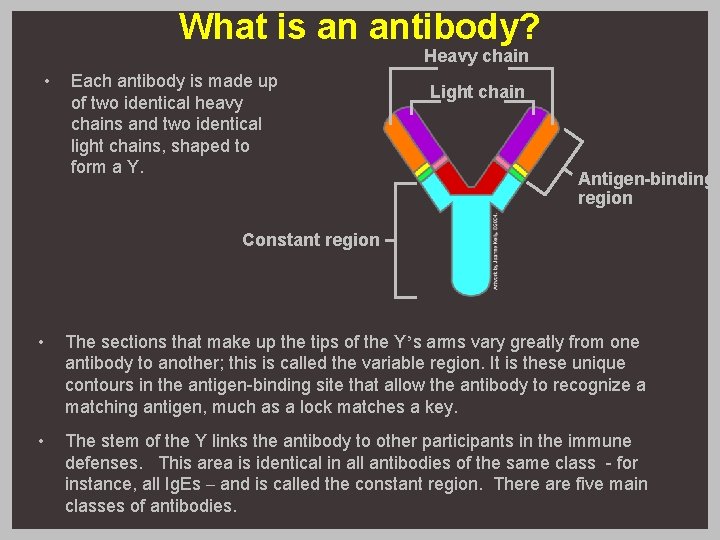
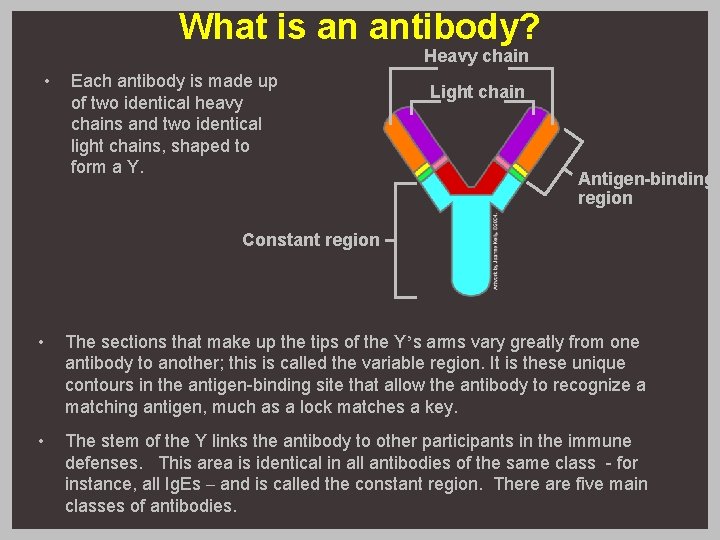
What is an antibody? Heavy chain • Each antibody is made up of two identical heavy chains and two identical light chains, shaped to form a Y. Light chain Antigen-binding region Constant region • The sections that make up the tips of the Y’s arms vary greatly from one antibody to another; this is called the variable region. It is these unique contours in the antigen-binding site that allow the antibody to recognize a matching antigen, much as a lock matches a key. • The stem of the Y links the antibody to other participants in the immune defenses. This area is identical in all antibodies of the same class - for instance, all Ig. Es – and is called the constant region. There are five main classes of antibodies.
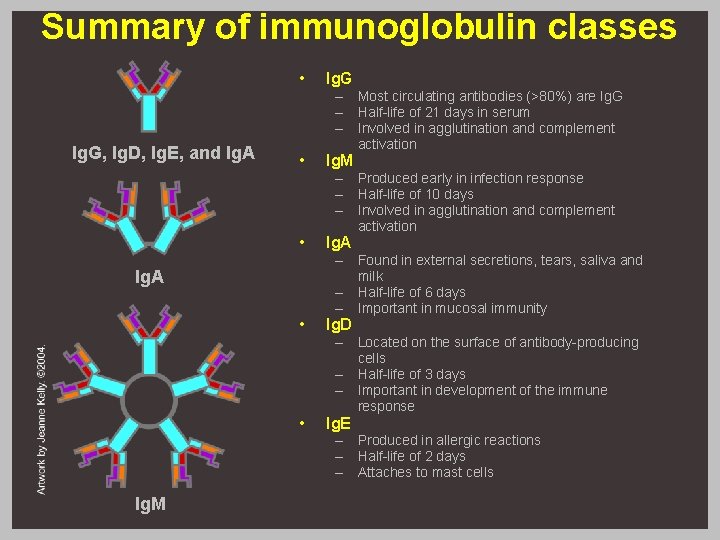
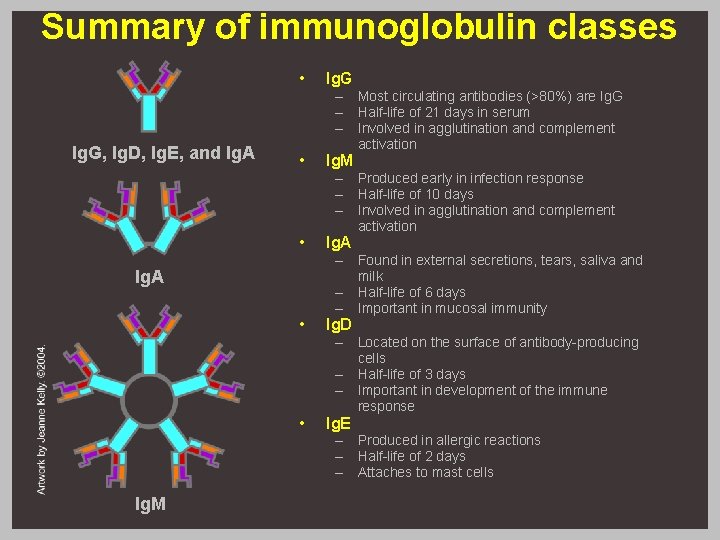
Summary of immunoglobulin classes Ig. G, Ig. D, Ig. E, and Ig. A • Ig. G • Ig. M • Ig. A • Ig. D • Ig. E Ig. A Ig. M – Most circulating antibodies (>80%) are Ig. G – Half-life of 21 days in serum – Involved in agglutination and complement activation – Produced early in infection response – Half-life of 10 days – Involved in agglutination and complement activation – Found in external secretions, tears, saliva and milk – Half-life of 6 days – Important in mucosal immunity – Located on the surface of antibody-producing cells – Half-life of 3 days – Important in development of the immune response – Produced in allergic reactions – Half-life of 2 days – Attaches to mast cells
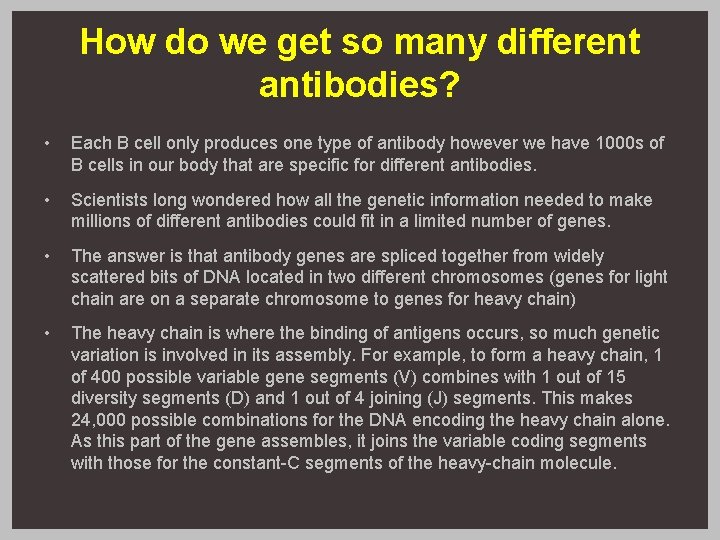
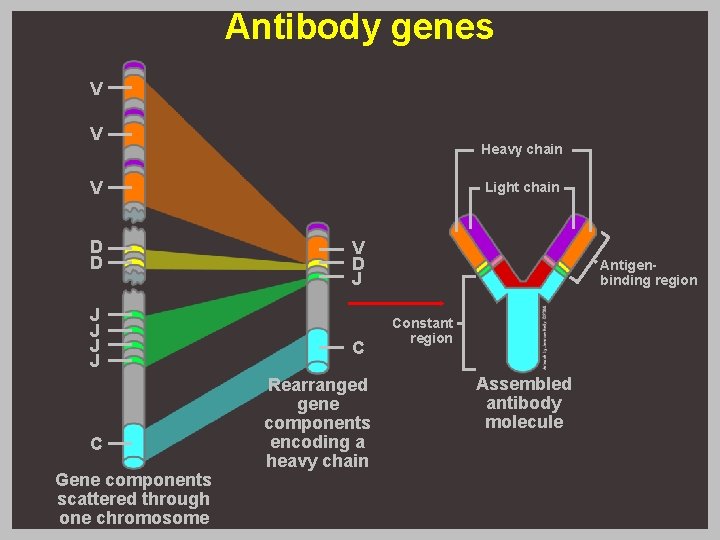
How do we get so many different antibodies? • Each B cell only produces one type of antibody however we have 1000 s of B cells in our body that are specific for different antibodies. • Scientists long wondered how all the genetic information needed to make millions of different antibodies could fit in a limited number of genes. • The answer is that antibody genes are spliced together from widely scattered bits of DNA located in two different chromosomes (genes for light chain are on a separate chromosome to genes for heavy chain) • The heavy chain is where the binding of antigens occurs, so much genetic variation is involved in its assembly. For example, to form a heavy chain, 1 of 400 possible variable gene segments (V) combines with 1 out of 15 diversity segments (D) and 1 out of 4 joining (J) segments. This makes 24, 000 possible combinations for the DNA encoding the heavy chain alone. As this part of the gene assembles, it joins the variable coding segments with those for the constant-C segments of the heavy-chain molecule.
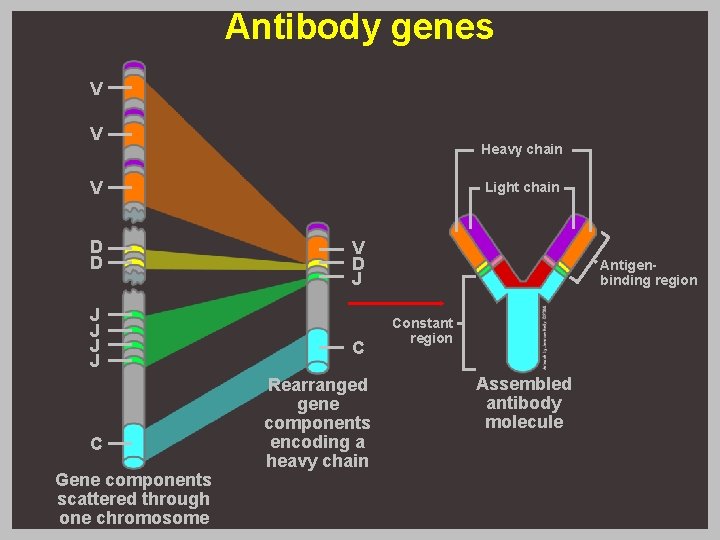
Antibody genes V V Heavy chain V D D J J C Gene components scattered through one chromosome Light chain V D J C Rearranged gene components encoding a heavy chain Antigenbinding region Constant region Assembled antibody molecule
T cells • T cells contribute to your immune defenses in two major ways. Some help regulate the complex workings of the overall immune response, while others are cytotoxic and directly contact infected cells and destroy them. • Four main types of T cells: – Helper T Cells – Killer T cells – Suppressor T cells – Memory T cells
Helper T cells • Recognise antigens on the surface of white blood cells, particularly macrophages. • Enlarge and form a clone of T helper cells. • Secrete interferon and cytokines which stimulate B cells and killer T cells.
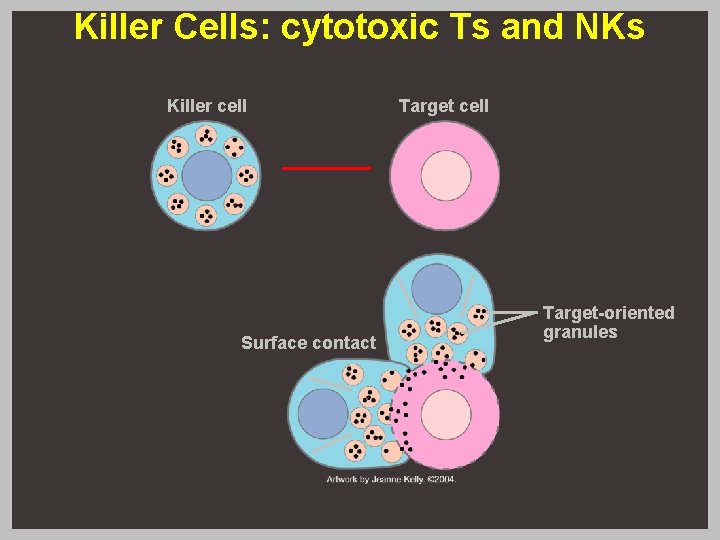
Killer T cells • Also called cytotoxic T cells. • Destroy abnormal body cells e. g. virus infected or cancer cells. • Stimulated by cytokines released by TH cells. • Release perforin which forms pores in target cells – this allows water and ions in and leads to lysis of the target cell. • Natural killer (NK) cells are another type of lymphocyte that acts in a similar manner to cytotoxic T (TC)cells. • Cytotoxic T cells need to recognize a specific antigen bound to self-MHC markers, whereas natural killer (NK) cells will recognize and attack cells lacking these. This gives NK cells the potential to attack many types of foreign cells.
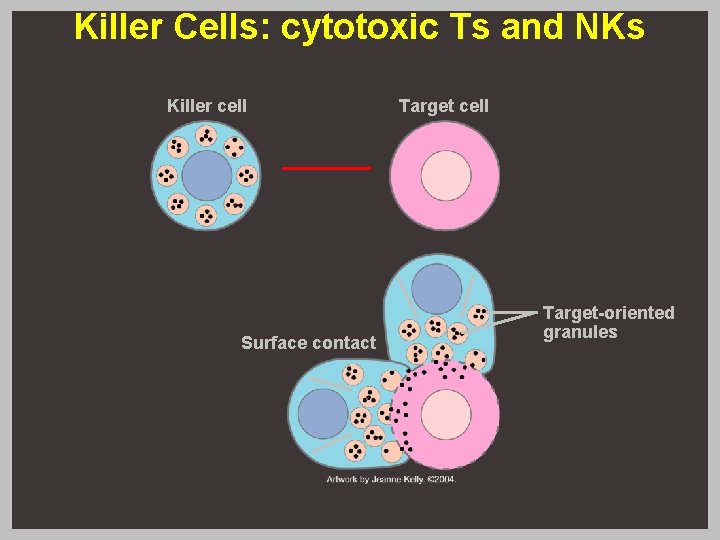
Killer Cells: cytotoxic Ts and NKs Killer cell Surface contact Target cell Target-oriented granules
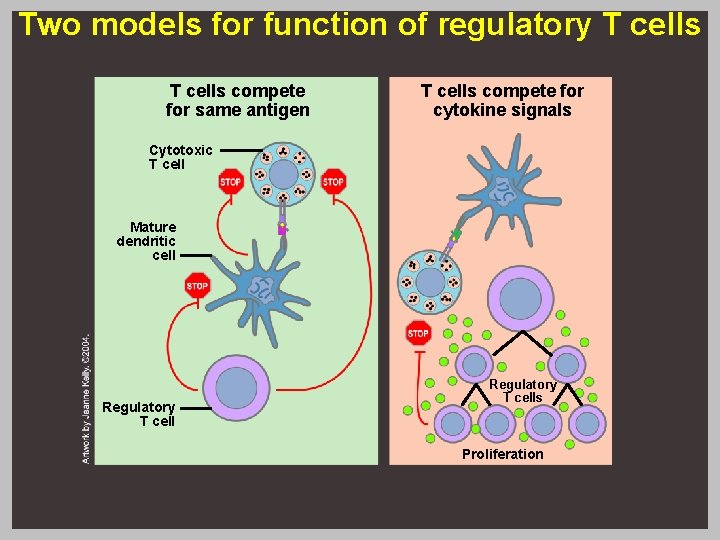
Suppresor/Regulatory T cells • Suppressor T cells or regulatory T cells control the immune system when the antigen/pathogen has been destroyed. • Researchers don’t yet know exactly how regulatory T cells operate. • T cells may recognize and compete for the same antigens as those that activate helper and cytotoxic T cells, but that regulatory T cells zero in on a different epitope. • Another possibility is that cytotoxic or helper T cells only multiply when regulatory T cells are absent.
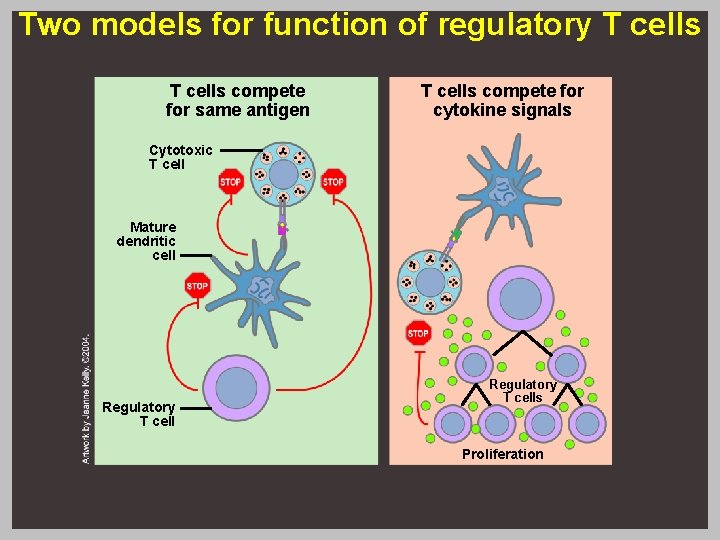
Two models for function of regulatory T cells compete for same antigen T cells compete for cytokine signals Cytotoxic T cell Mature dendritic cell Regulatory T cells Proliferation
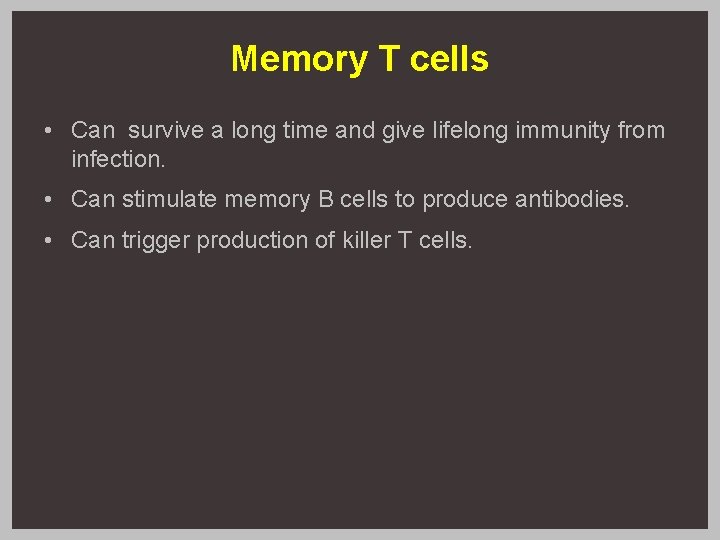
Memory T cells • Can survive a long time and give lifelong immunity from infection. • Can stimulate memory B cells to produce antibodies. • Can trigger production of killer T cells.
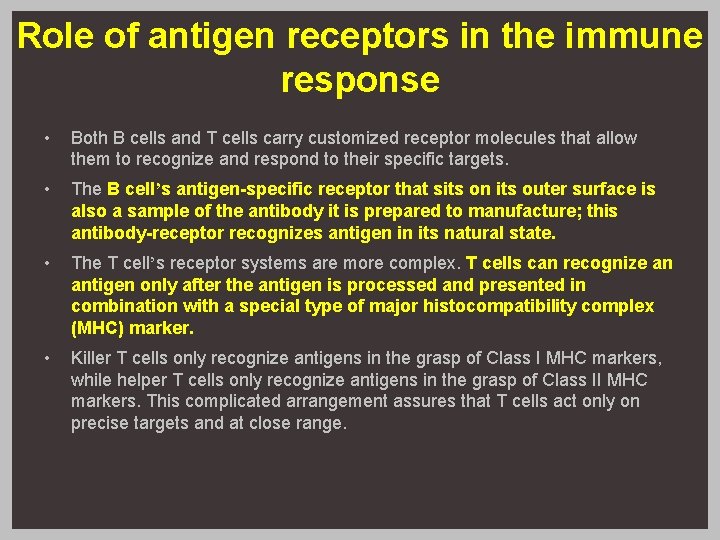
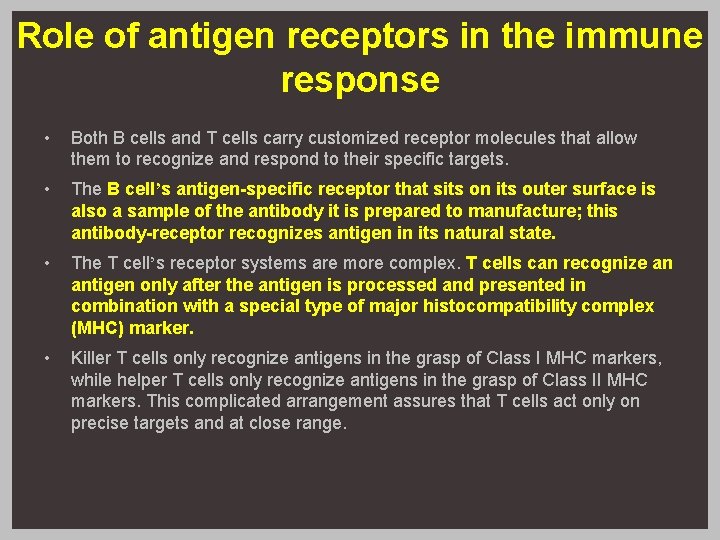
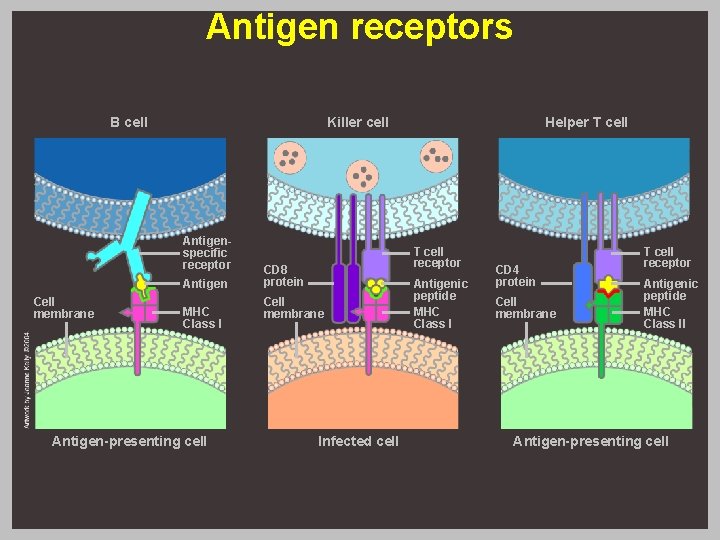
Role of antigen receptors in the immune response • Both B cells and T cells carry customized receptor molecules that allow them to recognize and respond to their specific targets. • The B cell’s antigen-specific receptor that sits on its outer surface is also a sample of the antibody it is prepared to manufacture; this antibody-receptor recognizes antigen in its natural state. • The T cell’s receptor systems are more complex. T cells can recognize an antigen only after the antigen is processed and presented in combination with a special type of major histocompatibility complex (MHC) marker. • Killer T cells only recognize antigens in the grasp of Class I MHC markers, while helper T cells only recognize antigens in the grasp of Class II MHC markers. This complicated arrangement assures that T cells act only on precise targets and at close range.
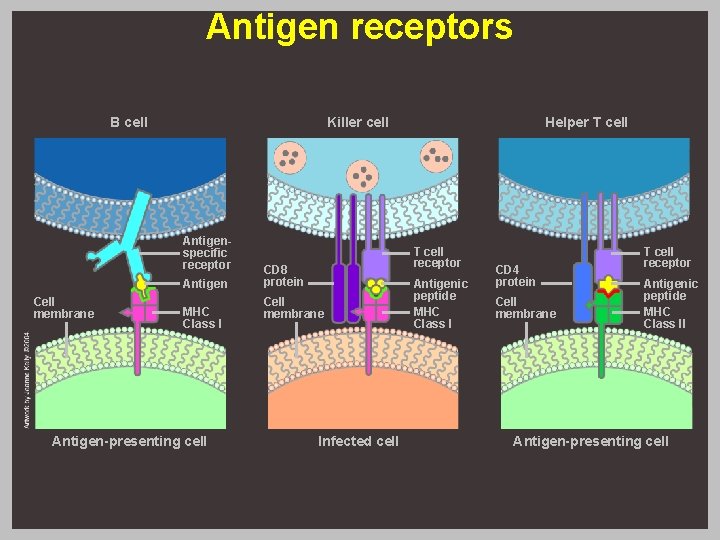
Antigen receptors B cell Killer cell Antigenspecific receptor Antigen Cell membrane MHC Class I Antigen-presenting cell Helper T cell receptor CD 8 protein Cell membrane Infected cell Antigenic peptide MHC Class I CD 4 protein Cell membrane T cell receptor Antigenic peptide MHC Class II Antigen-presenting cell
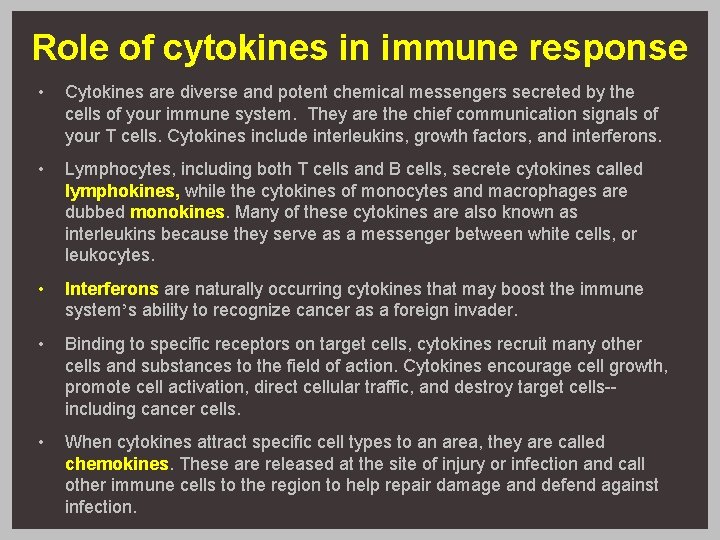
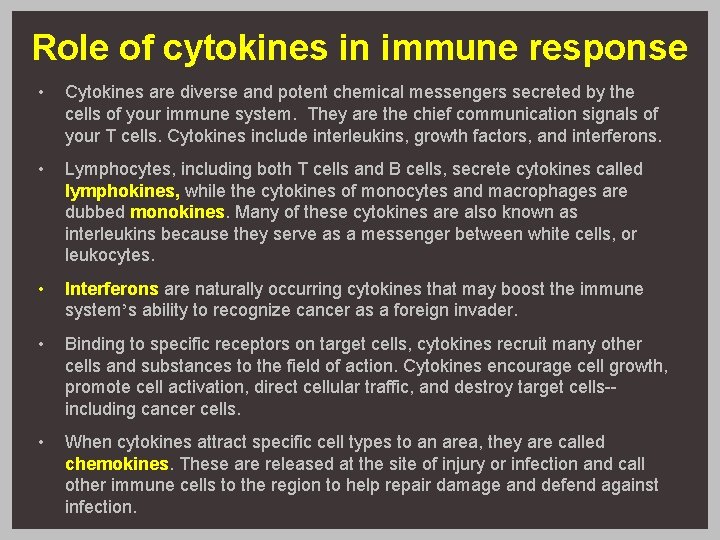
Role of cytokines in immune response • Cytokines are diverse and potent chemical messengers secreted by the cells of your immune system. They are the chief communication signals of your T cells. Cytokines include interleukins, growth factors, and interferons. • Lymphocytes, including both T cells and B cells, secrete cytokines called lymphokines, while the cytokines of monocytes and macrophages are dubbed monokines. Many of these cytokines are also known as interleukins because they serve as a messenger between white cells, or leukocytes. • Interferons are naturally occurring cytokines that may boost the immune system’s ability to recognize cancer as a foreign invader. • Binding to specific receptors on target cells, cytokines recruit many other cells and substances to the field of action. Cytokines encourage cell growth, promote cell activation, direct cellular traffic, and destroy target cells-including cancer cells. • When cytokines attract specific cell types to an area, they are called chemokines. These are released at the site of injury or infection and call other immune cells to the region to help repair damage and defend against infection.
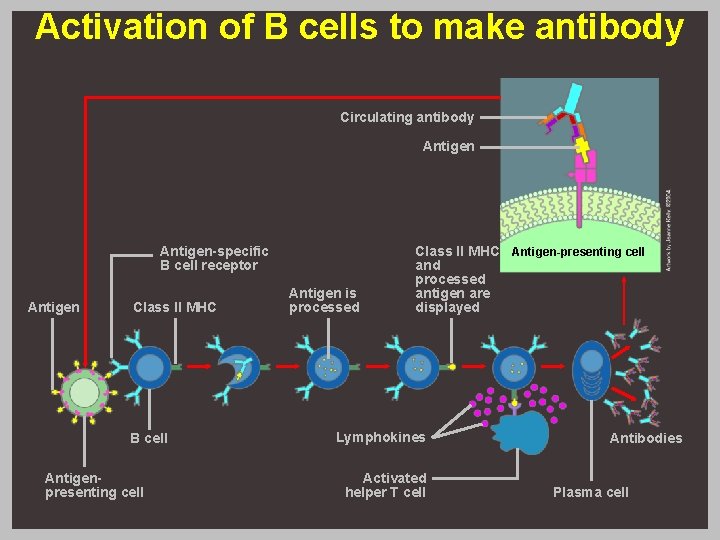
Activation of B cells to make antibody Circulating antibody Antigen-specific B cell receptor Antigen Class II MHC B cell Antigenpresenting cell Antigen is processed Class II MHC Antigen-presenting cell and processed antigen are displayed Lymphokines Activated helper T cell Antibodies Plasma cell
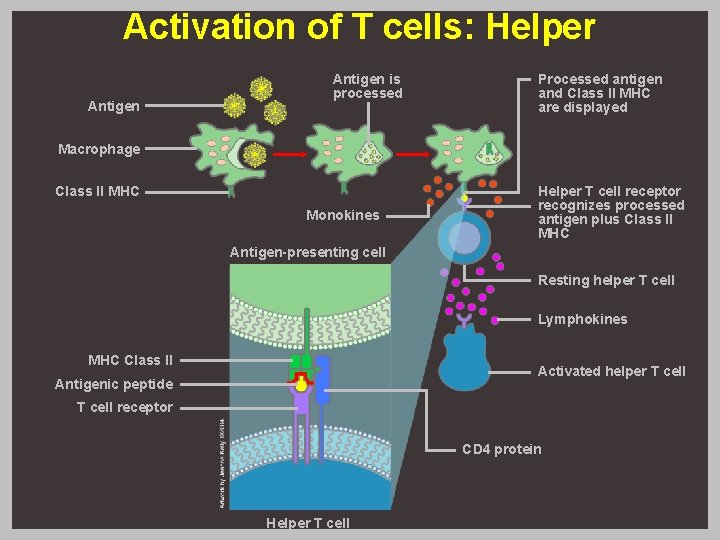
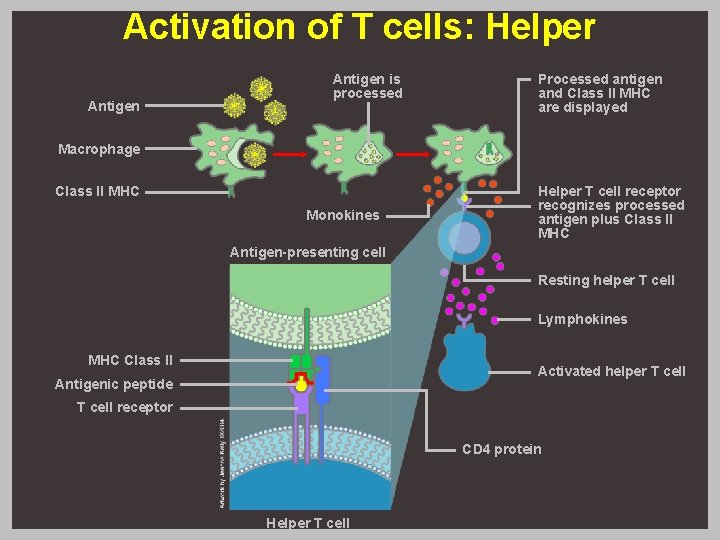
Activation of T cells: Helper Antigen is processed Processed antigen and Class II MHC are displayed Macrophage Class II MHC Monokines Helper T cell receptor recognizes processed antigen plus Class II MHC Antigen-presenting cell Resting helper T cell Lymphokines MHC Class II Activated helper T cell Antigenic peptide T cell receptor CD 4 protein Helper T cell
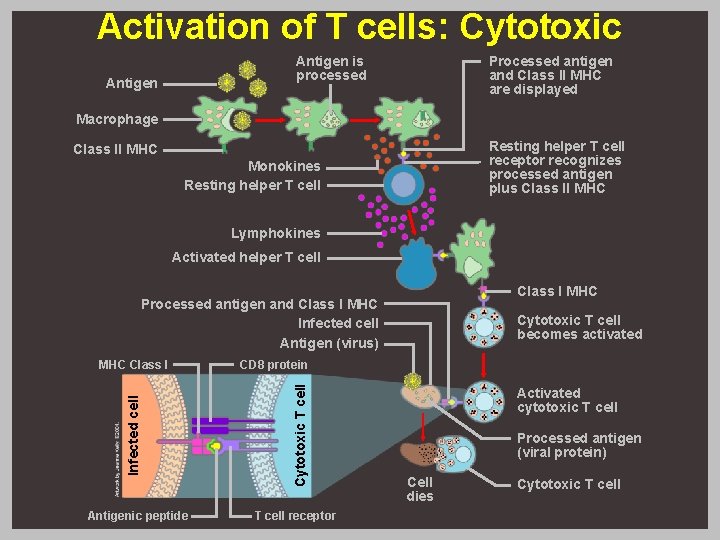
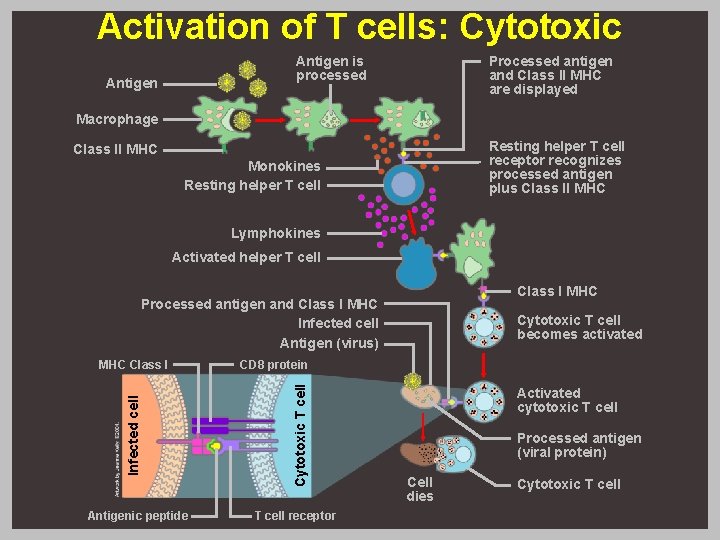
Activation of T cells: Cytotoxic Antigen is processed Antigen Processed antigen and Class II MHC are displayed Macrophage Resting helper T cell receptor recognizes processed antigen plus Class II MHC Monokines Resting helper T cell Lymphokines Activated helper T cell Class I MHC Processed antigen and Class I MHC Infected cell Antigen (virus) Antigenic peptide CD 8 protein Cytotoxic T cell Infected cell MHC Class I Cytotoxic T cell becomes activated T cell receptor Activated cytotoxic T cell Processed antigen (viral protein) Cell dies Cytotoxic T cell