The Acetabular Labrum BLAIRE CHANDLER VIRGINIA COMMONWEALTH UNIVERSITY
The Acetabular Labrum BLAIRE CHANDLER VIRGINIA COMMONWEALTH UNIVERSITY PHYSICAL THERAPY DECEMBER 1, 2015
Prevalence § 2010 Review 8: § “Unprecedented growth” in the number of hip arthroscopies over the last decade § Acetabular labral tears are the leading indication for hip arthroscopy
Anatomy & Function
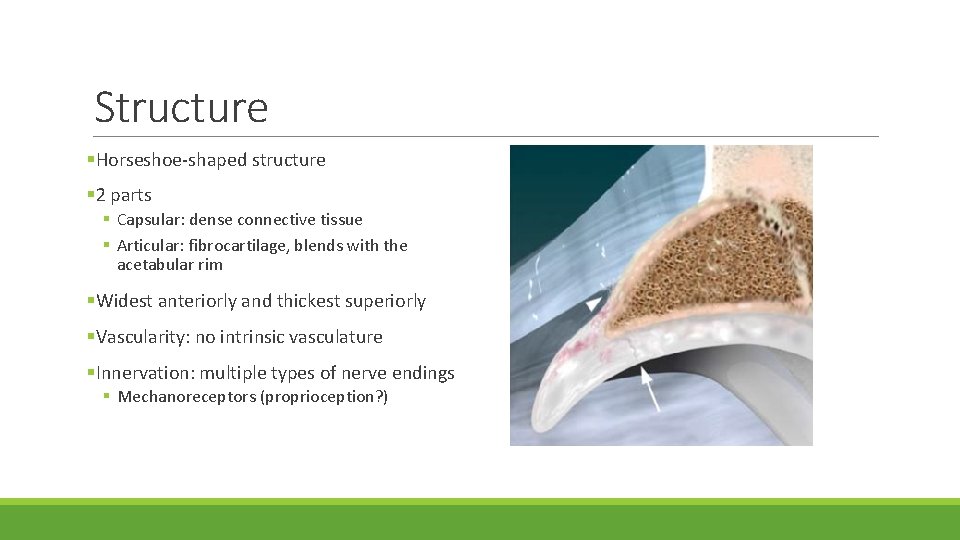
Structure §Horseshoe-shaped structure § 2 parts § Capsular: dense connective tissue § Articular: fibrocartilage, blends with the acetabular rim §Widest anteriorly and thickest superiorly §Vascularity: no intrinsic vasculature §Innervation: multiple types of nerve endings § Mechanoreceptors (proprioception? )
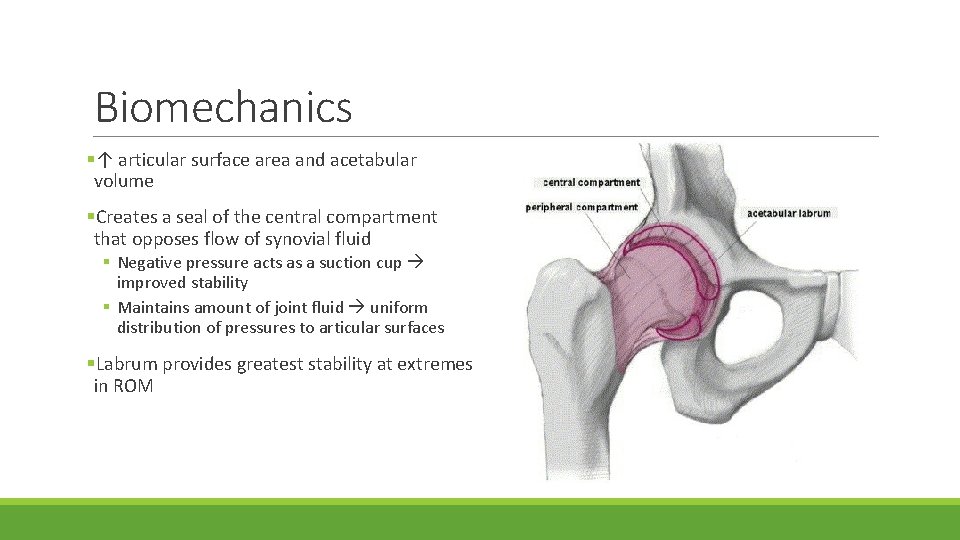
Biomechanics §↑ articular surface area and acetabular volume §Creates a seal of the central compartment that opposes flow of synovial fluid § Negative pressure acts as a suction cup improved stability § Maintains amount of joint fluid uniform distribution of pressures to articular surfaces §Labrum provides greatest stability at extremes in ROM

Labral Tears
Etiologies §Traumatic Injuries §Femoral acetabular impingement (FAI) § North America – anterosuperior tears associated §Capsular laxity with sudden twisting or pivoting motions § Asia – posterior tears associated with hyperflexion §Dysplasia § Shallow acetabular socket § Decrease coverage of femoral head anteriorly and laterally increased stress on anterior capsule and labrum §Reported 74. 1% of tears are not associated with a known event or cause 7
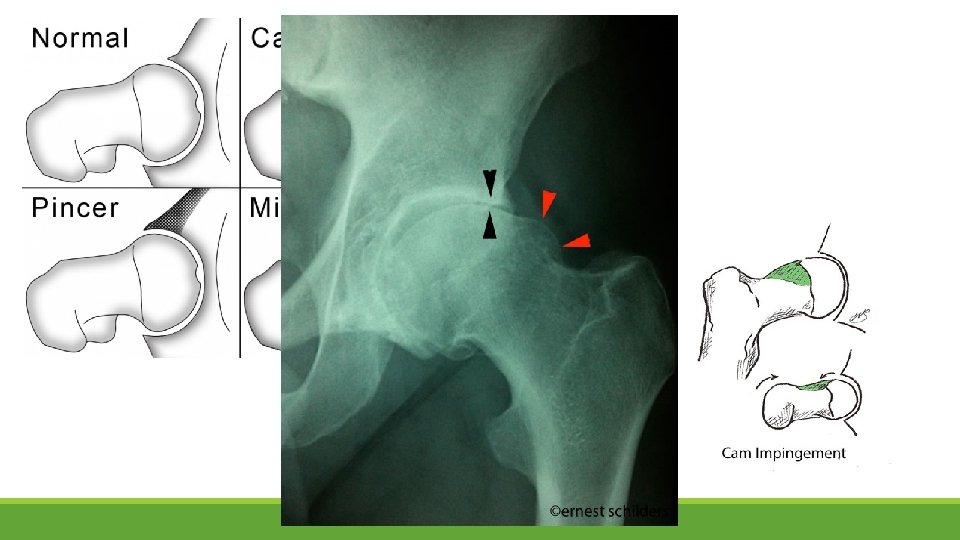
Femoral Acetabular Impingement (FAI) §FAI = ↓joint clearance between the acetabulum and femur § 2 types – Cam and Pincer §Cam impingement: § Abnormally large radius of femoral head § Abnormal contact with acetabulum, especially in flexion with adduction and IR § More common in young, athletic males §Pincer impingement: § Abnormal acetabulum with overcoverage § More common in middle-aged, active women
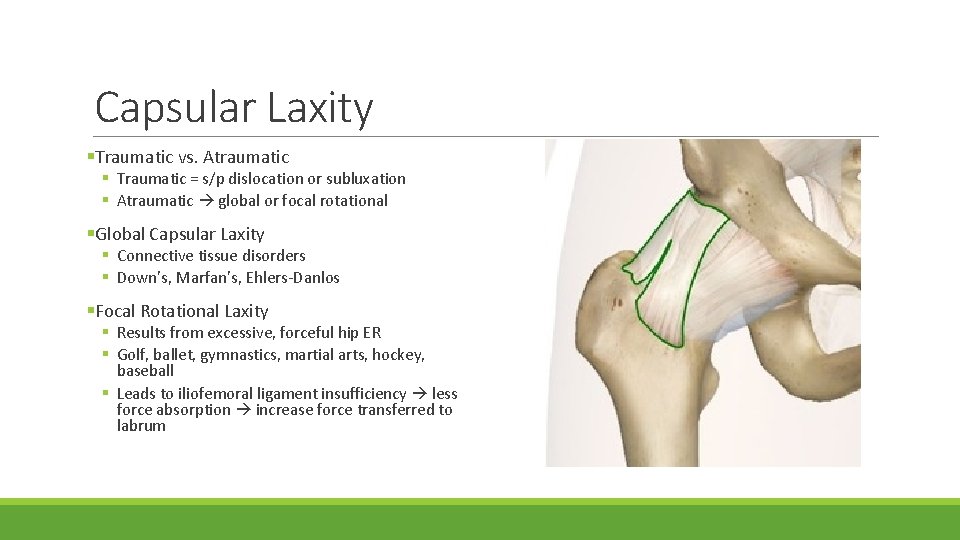
Capsular Laxity §Traumatic vs. Atraumatic § Traumatic = s/p dislocation or subluxation § Atraumatic global or focal rotational §Global Capsular Laxity § Connective tissue disorders § Down’s, Marfan’s, Ehlers-Danlos §Focal Rotational Laxity § Results from excessive, forceful hip ER § Golf, ballet, gymnastics, martial arts, hockey, baseball § Leads to iliofemoral ligament insufficiency less force absorption increase force transferred to labrum
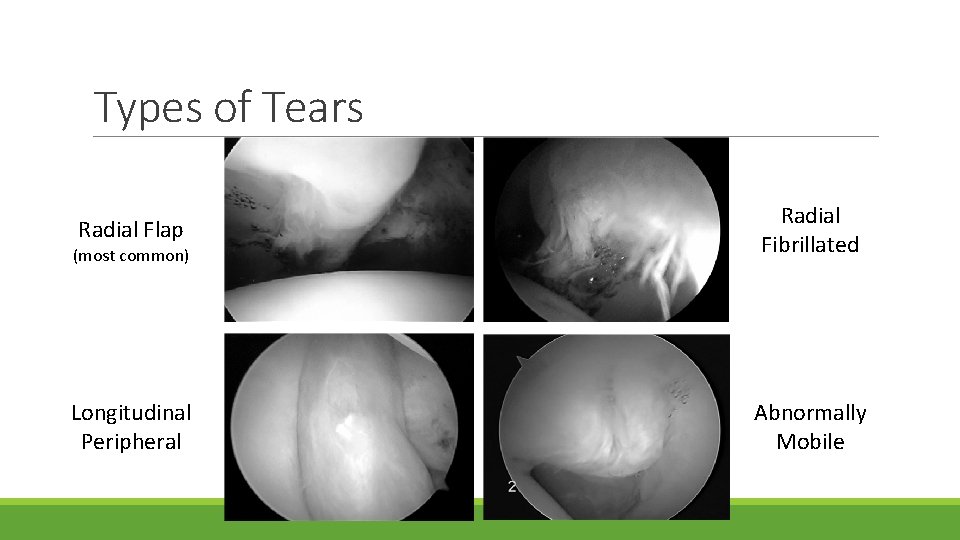
Types of Tears Radial Flap (most common) Radial Fibrillated Longitudinal Peripheral Abnormally Mobile

Location of Tears §Dependent on geographic region §Prevalence of anterior tears: § ? Poorer vascular supply § Mechanically weaker tissue § Higher localized forces Most common
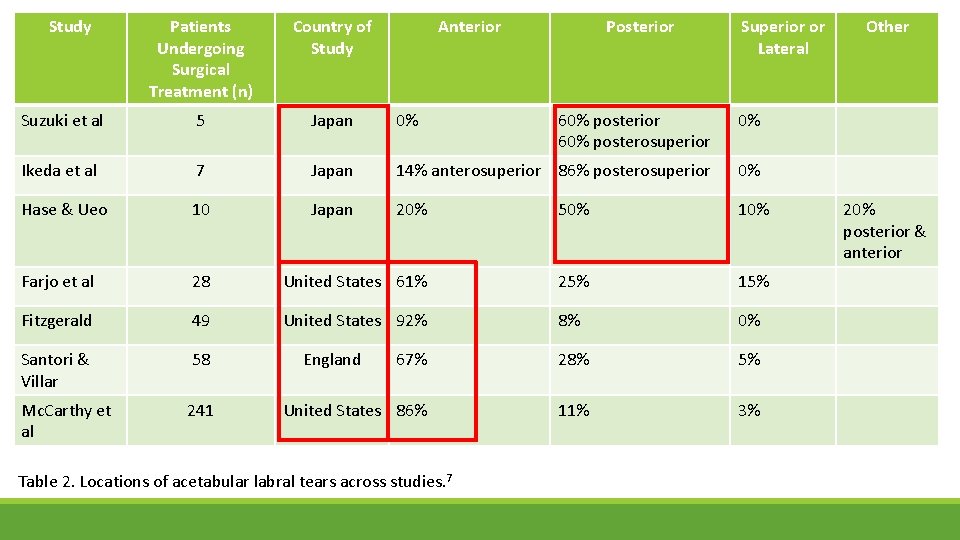
Study Patients Undergoing Surgical Treatment (n) Country of Study Suzuki et al 5 Japan 0% 60% posterior 60% posterosuperior 0% Ikeda et al 7 Japan 14% anterosuperior 86% posterosuperior 0% Hase & Ueo 10 Japan 20% 50% 10% Farjo et al 28 United States 61% 25% 15% Fitzgerald 49 United States 92% 8% 0% Santori & Villar 58 67% 28% 5% Mc. Carthy et al 241 United States 86% 11% 3% England Anterior Table 2. Locations of acetabular labral tears across studies. 7 Posterior Superior or Lateral Other 20% posterior & anterior
Clinical Assessment
History & Symptoms §Most common traumatic MOI = ER force in a hyperextended position §Symptoms – pain, clicking, locking, catching, instability, giving way, stiffness § Pain location = anterior groin, buttock, greater trochanter, thigh, and/or medial knee § Anterior groin pain is NOT specific to labral tear §Symptom localization – C-sign
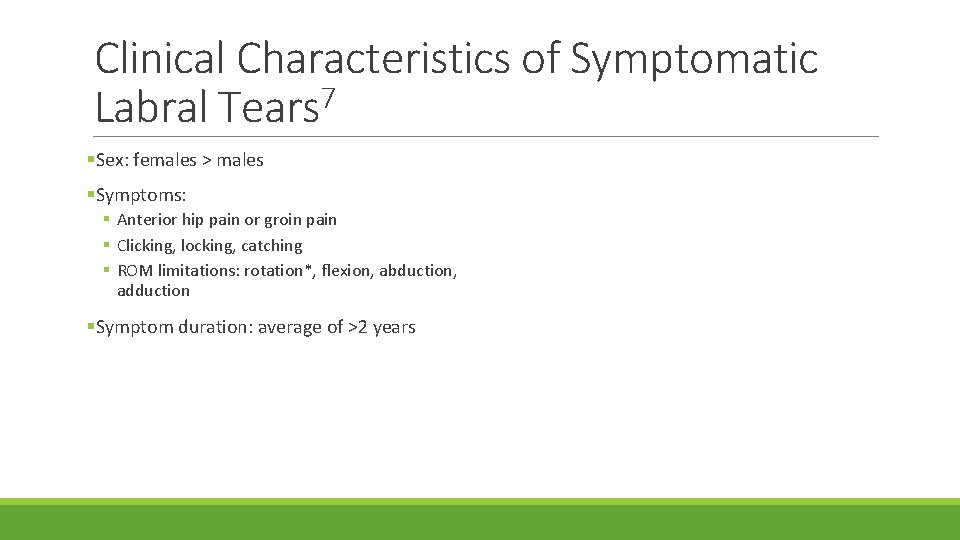
Clinical Characteristics of Symptomatic Labral Tears 7 §Sex: females > males §Symptoms: § Anterior hip pain or groin pain § Clicking, locking, catching § ROM limitations: rotation*, flexion, abduction, adduction §Symptom duration: average of >2 years
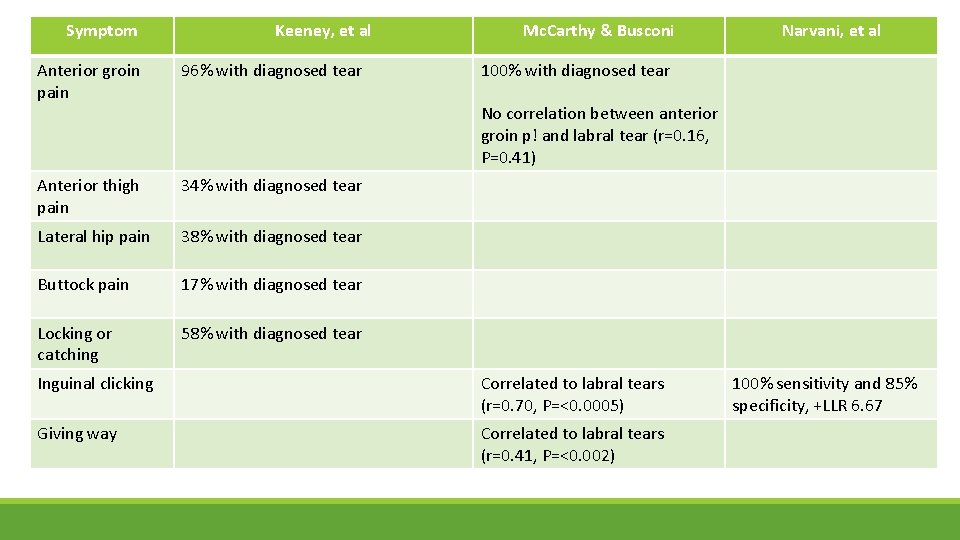
Symptom Keeney, et al Anterior groin pain 96% with diagnosed tear Anterior thigh pain 34% with diagnosed tear Lateral hip pain 38% with diagnosed tear Buttock pain 17% with diagnosed tear Locking or catching 58% with diagnosed tear Mc. Carthy & Busconi Narvani, et al 100% with diagnosed tear No correlation between anterior groin p! and labral tear (r=0. 16, P=0. 41) Inguinal clicking Correlated to labral tears (r=0. 70, P=<0. 0005) Giving way Correlated to labral tears (r=0. 41, P=<0. 002) 100% sensitivity and 85% specificity, +LLR 6. 67
Physical Examination §Inspection § Standing posture § Sitting posture § Gait §Palpation – usually to rule out other disorders
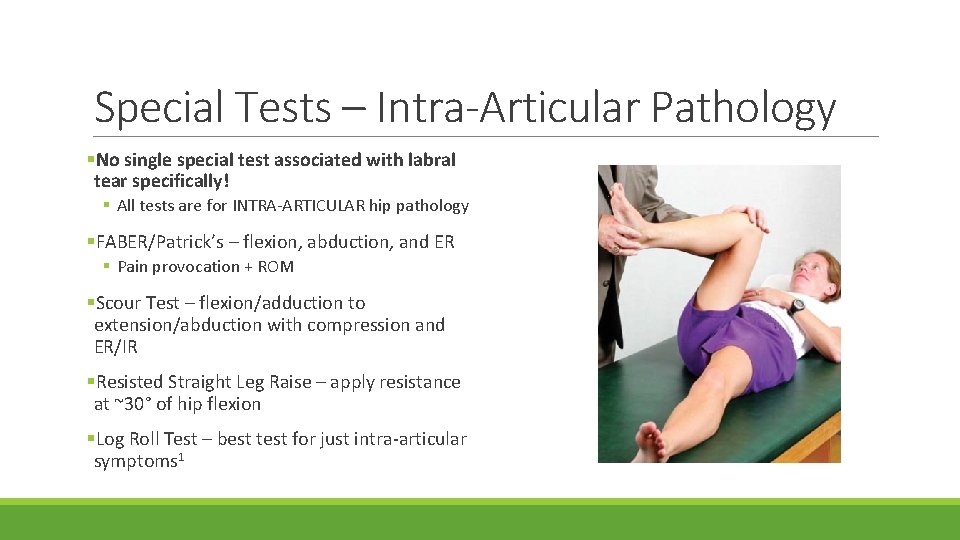
Special Tests – Intra-Articular Pathology §No single special test associated with labral tear specifically! § All tests are for INTRA-ARTICULAR hip pathology §FABER/Patrick’s – flexion, abduction, and ER § Pain provocation + ROM §Scour Test – flexion/adduction to extension/abduction with compression and ER/IR §Resisted Straight Leg Raise – apply resistance at ~30° of hip flexion §Log Roll Test – best test for just intra-articular symptoms 1
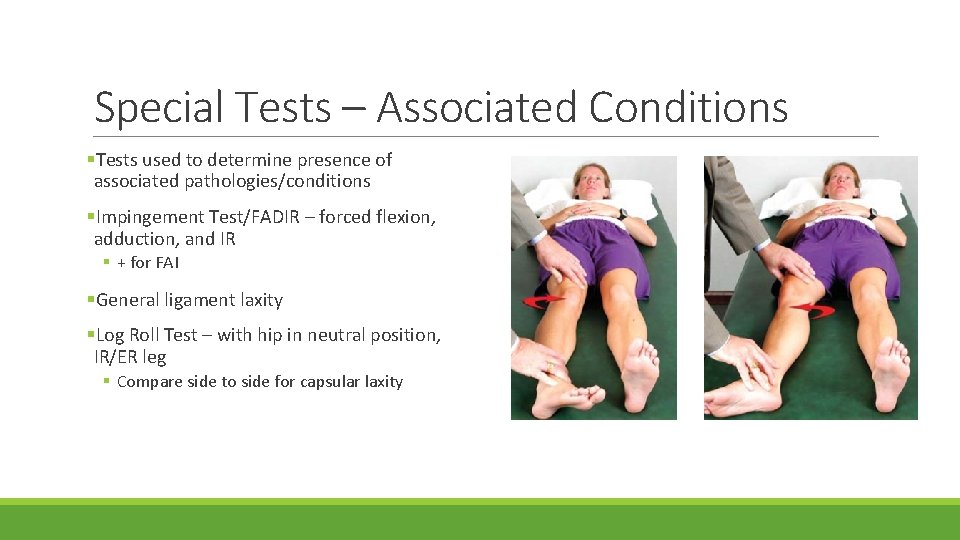
Special Tests – Associated Conditions §Tests used to determine presence of associated pathologies/conditions §Impingement Test/FADIR – forced flexion, adduction, and IR § + for FAI §General ligament laxity §Log Roll Test – with hip in neutral position, IR/ER leg § Compare side to side for capsular laxity
JOSPT Key Examination Elements 7 1) Positions and movement tests § § § Standing alignment, esp. hip hyperextension Precision of active and passive hip flexion Precision of active hip extension (contribution of hamstrings vs. gluteals) Pattern and range of hip IR/ER in prone Quadruped – effect on symptoms, alignment 2) Muscle strength and pattern of control 3) Muscle length and stiffness 4) Gait assessment – esp. lack of appropriate knee flexion, excessive time in foot flat, hip hyperextension 5) Modification of functional activities – sitting mechanics
Hip Pain “Red Flags” §Acute hip pain with: § § § § Fever Malaise Night sweats Weight lost Night pain IV drug use History of cancer Compromised immune system §Could indicate tumor, infection, septic arthritis, osteomyelitis, or an inflammatory condition §Corticosteroid or alcohol use = risk of avascular necrosis §Potential indicators of fracture: § § Significant trauma Pain with any/all movement Inability to walk/bear weight Shortened, externally rotated lower extremity
Diagnosis §Diagnosed via MRI with arthrogram §Kahlenberg et al: § Average number of healthcare providers: 4 ($315. 05) § Average number of diagnostic tests: 3. 4 ($837. 01) § Average number of conservative treatments: 3. 1 ($1375. 44)
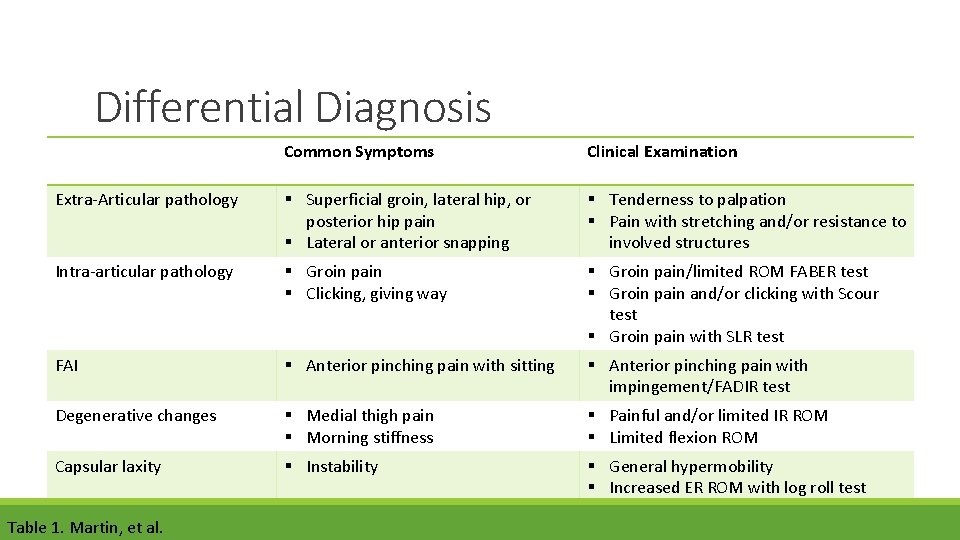
Differential Diagnosis Common Symptoms Clinical Examination Extra-Articular pathology § Superficial groin, lateral hip, or posterior hip pain § Lateral or anterior snapping § Tenderness to palpation § Pain with stretching and/or resistance to involved structures Intra-articular pathology § Groin pain § Clicking, giving way § Groin pain/limited ROM FABER test § Groin pain and/or clicking with Scour test § Groin pain with SLR test FAI § Anterior pinching pain with sitting § Anterior pinching pain with impingement/FADIR test Degenerative changes § Medial thigh pain § Morning stiffness § Painful and/or limited IR ROM § Limited flexion ROM Capsular laxity § Instability § General hypermobility § Increased ER ROM with log roll test Table 1. Martin, et al.
Treatment
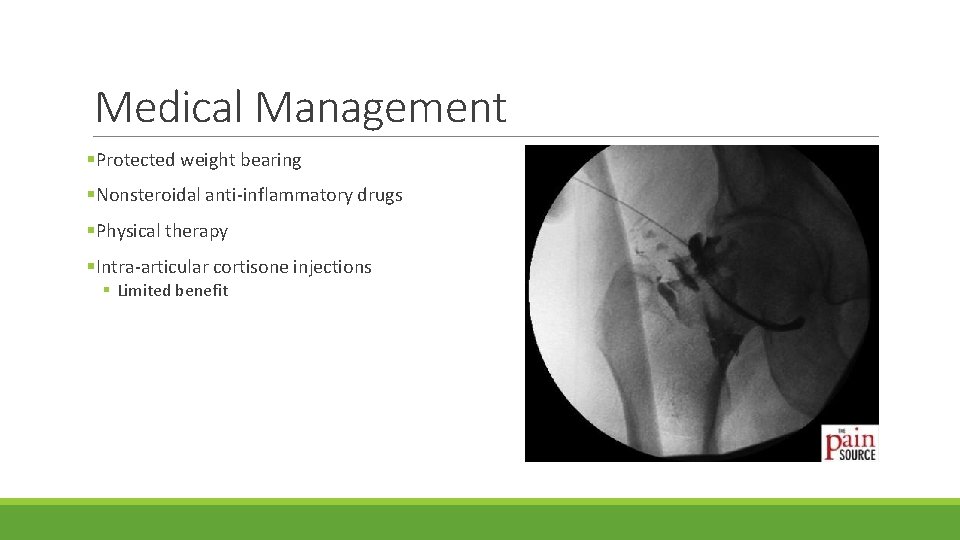
Medical Management §Protected weight bearing §Nonsteroidal anti-inflammatory drugs §Physical therapy §Intra-articular cortisone injections § Limited benefit
Physical Therapy (Pre-Op) §“Physical therapy has not proved to be of significant benefit and is not recommended for patients with a labral tear” §Goal: reducing anteriorly directed forces on the hip § Address patterns of recruitment of muscles that control hip motion § Correct movement patterns § Education re: provocative positions, etc. §Key muscles to target: § § Hip abductors Deep external rotators Gluteus maximus Iliopsoas
Surgical Management §Goal: “anatomically restore labral function in order to preserve or restore stability of the joint, decrease joint contact pressure on the articular cartilage, and ultimately restore painfree function” 10 § 3 options: § Debridement or excision § Repair § Reconstruction §Other pathology often corrected simultaneously

Post-Op Rehabilitation
Rehabilitation After Hip Arthroscopy §No evidence exists to support §Generally broken down into 3 -4 specific post-op rehab guidelines phases: §Lots of variability § MD dependent § Different surgical components §*Protocols should be tailored to the individual patient § Phase I – Initial Exercises § Phase II – Intermediate Exercises § Phase III – Advanced Exercises § Phase IV – Sport-Specific Exercises
General Guidelines §Protected weight bearing § 50% WB x 4 weeks § TTWB x 3 weeks § WBAT with use of crutches x 4 weeks § Variable… §ROM limitations (~6 weeks) § No hip flexion past 90° § Avoid external rotation § No hip extension past 0 -10° (most variable) § Limited abduction §Avoid hip flexor activity §Limit ROM based on pain initially §Gentle circumduction should be started early to maintain joint mobility and decrease the likelihood of adhesions
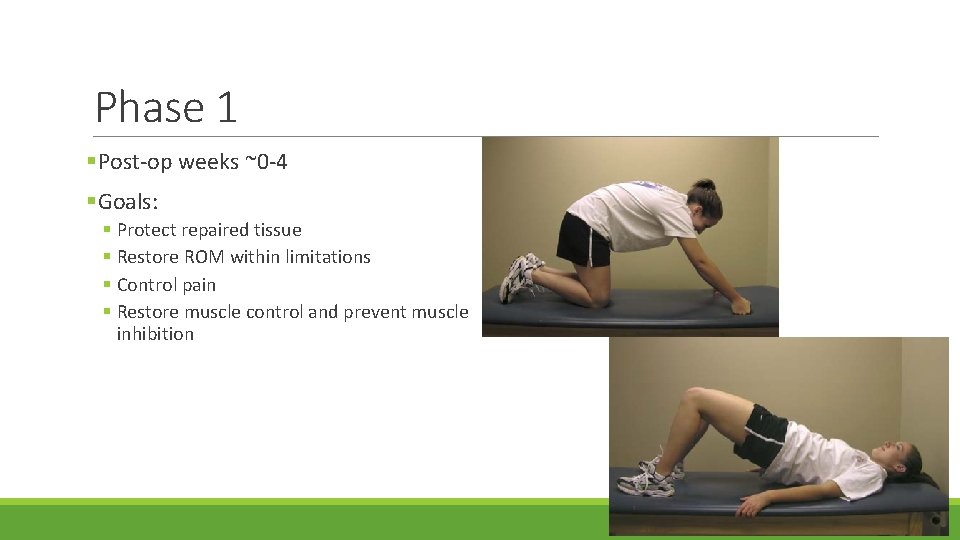
Phase 1 §Post-op weeks ~0 -4 §Goals: § Protect repaired tissue § Restore ROM within limitations § Control pain § Restore muscle control and prevent muscle inhibition
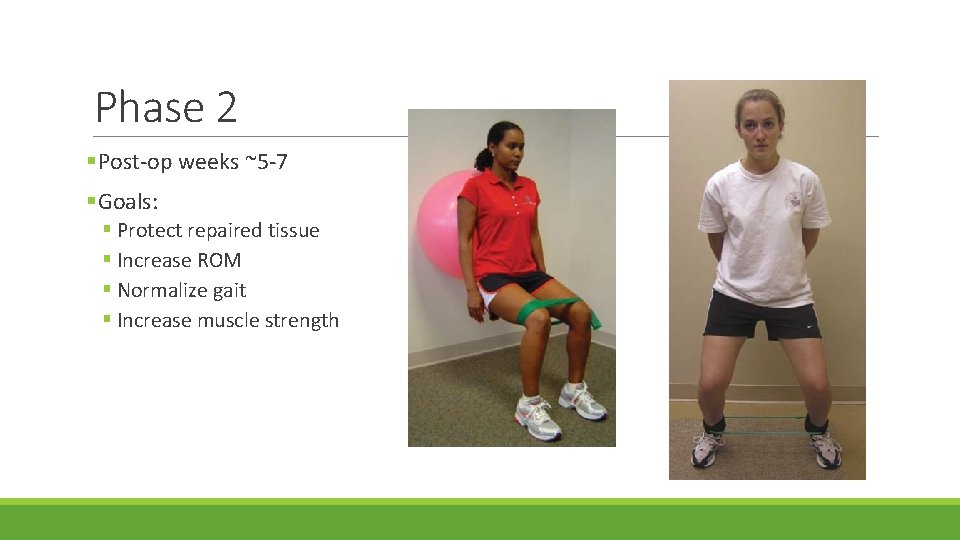
Phase 2 §Post-op weeks ~5 -7 §Goals: § Protect repaired tissue § Increase ROM § Normalize gait § Increase muscle strength
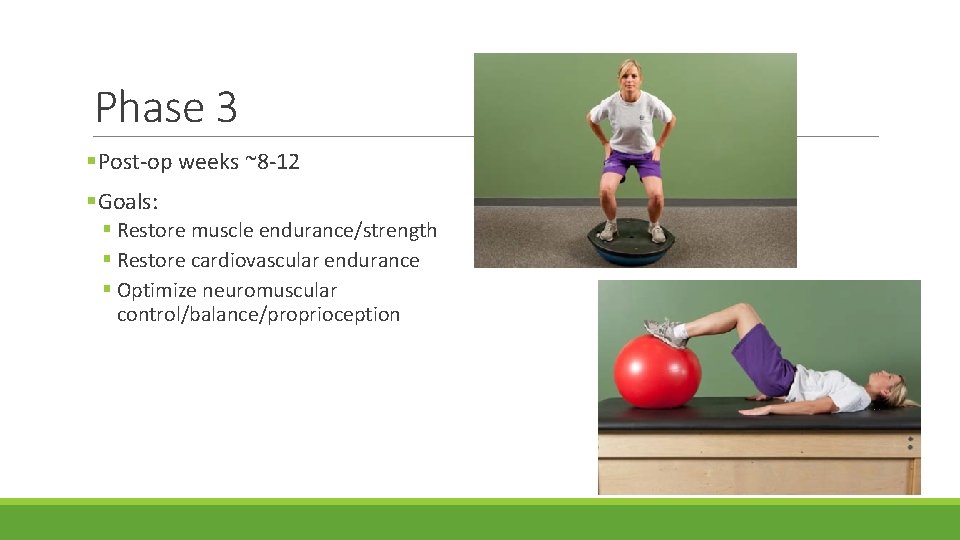
Phase 3 §Post-op weeks ~8 -12 §Goals: § Restore muscle endurance/strength § Restore cardiovascular endurance § Optimize neuromuscular control/balance/proprioception
Phase 4 §Post-op weeks ~12+ §Goals: § Running progression § Sport-specific drills § Return to sport
References 1) Byrd, T. (2007). Evaluation of the Hip: History and Physical Examination. North American Journal of Sports Physical Therapy, 2(4), 231 -240. 2) Edelstein, J. , Ranawat, A. , Enseki, K. , Yun, R. , & Draovitch, P. (2012). Post-operative guidelines following hip arthroscopy. Current Review of Musculoskeletal Medicine, 5, 15 -23. 3) Garrison, J. , Osler, M. , & Singleton, S. (2007). Rehabilitation After Arthroscopy of an Acetabular Labral Tear. North American Journal of Sports Physical Therapy, 2(4), 241 -250. 4) Kahlenberg, C. , Han, B. , Patel, R. , Deshmane, P. , & Terry, M. (2014). Time and Cost of Diagnosis for Symptomatic Femoroacetabular Impingement. Orthopaedic Journal of Sports Medicine, 2(3). 5) Krych, A. , Griffith, T. , Hudgens, J. , Kuzma, S. , Sierra, R. , & Levy, B. (2014). Limited therapeutic benefits of intra-articular cortisone injection for patients with femoro-acetabular impingement and labral tear. Knee Surgery, Sports Traumatology, Arthroscopy, 22, 750 -755. 6) Lewis, C. , & Sahrmann, S. (2006). Acetabular Labral Tears. Physical Therapy, 86(1), 110 -121. 7) Martin, R. , Enseki, K. , Draovitch, P. , Trapuzzano, T. , & Philippon, M. (2006). Acetabular Labral Tears of the Hip: Examination and Diagnostic Challenges. Journal of Orthopedic & Sports Physical Therapy, 36(7), 503 -515. doi: 10. 2519/jospt. 2006. 2135 8) Safran, M. (2010). The Acetabular Labrum: Anatomic and Functional Characteristics and Rationale for Surgical Intervention. Journal of the American Academy of Orthopaedic Surgeons, 18(6), 338 -345. 9) Edelstein, J. , Ranawat, A. , Enseki, K. , Yun, R. , & Draovitch, P. (2012). Post-operative guidelines following hip arthroscopy. Current Review of Musculoskeletal Medicine, 5, 15 -23. 10) Wolff AB. Mantell M. Gerscovich D. Haines C. “Arthroscopic Management of the Labrum: Debridement, Repair, and Stitch Configurations” Chapter 11 with accompanying video in *The Hip: Arthroscopy Association of North America Advanced Arthroscopic Surgical Techniques. In Press.
- Slides: 37