The Abdomen Surface Anatomy Vessels Muscles and Peritoneum
The Abdomen Surface Anatomy, Vessels, Muscles, and Peritoneum Hastaneciyiz. blogspot. com

Abdominopelvic Cavity • Ventral body cavity – Thoracic – Abdominopelvic • Abdominopelvic – Abdominal • Liver • Stomach • Kidneys – Pelvic cavity • Bladder • Some reproductive organs • Rectum

Abdominopelvic Cavity • Surrounded by the abdominal walls and pelvic girdle • The two cavities are continuous • Most organs surrounded by a peritoneal cavity pg 242 – Visceral peritoneum – Serous peritoneum – Peritoneal cavity

Abdominal Quadrants • 9 regions • 4 quadrants – Draw “line” through navel – Right upper quadrant – Left lower quadrant – Right lower quadrant pg 242

Surface Anatomy • Anterior abdominal wall extends from costal margin to inferior boundaries: – – Iliac crest Anterior superior iliac spine Inguinal ligament Pubic crest • Superior boundary – Diaphragm • Central landmark – Umbilicus • Linea alba (white line) pg 345 – Tendinous line – Extends from xiphoid process to pubic symphysis
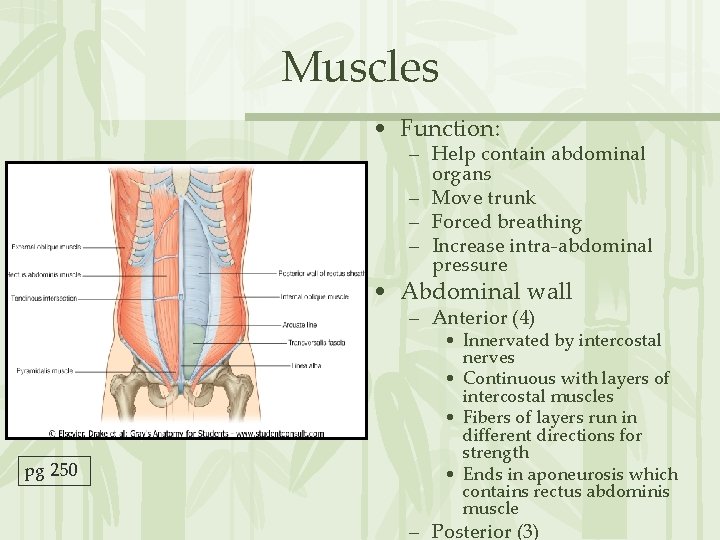
Muscles • Function: – Help contain abdominal organs – Move trunk – Forced breathing – Increase intra-abdominal pressure • Abdominal wall – Anterior (4) pg 250 • Innervated by intercostal nerves • Continuous with layers of intercostal muscles • Fibers of layers run in different directions for strength • Ends in aponeurosis which contains rectus abdominis muscle – Posterior (3)

Anterior Abdominal Wall Muscles Rectus Abdominis – Origin • Pubic crest, symphysis – Insertion • Xiphoid process, costal cartilages of ribs 5 -7 – Function • Flex, rotate trunk, fix and depress ribs, stabilize pelvis, compress abdomen • Internal oblique – Origin • Lumbar fascia, iliac crest, inguinal ligament – Insertion • Linea alba, pubic crest, last 3 -4 ribs, costal margin – Function • Same for external obliques § pg 250, 251
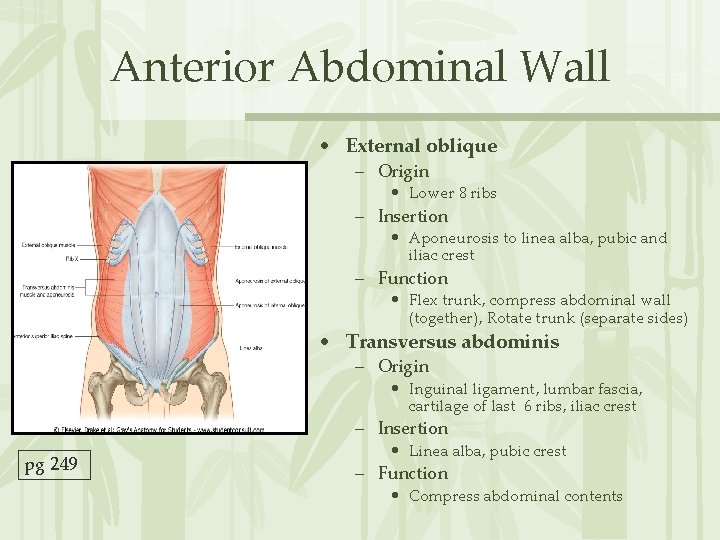
Anterior Abdominal Wall • External oblique – Origin • Lower 8 ribs – Insertion • Aponeurosis to linea alba, pubic and iliac crest – Function • Flex trunk, compress abdominal wall (together), Rotate trunk (separate sides) • Transversus abdominis – Origin • Inguinal ligament, lumbar fascia, cartilage of last 6 ribs, iliac crest – Insertion pg 249 • Linea alba, pubic crest – Function • Compress abdominal contents
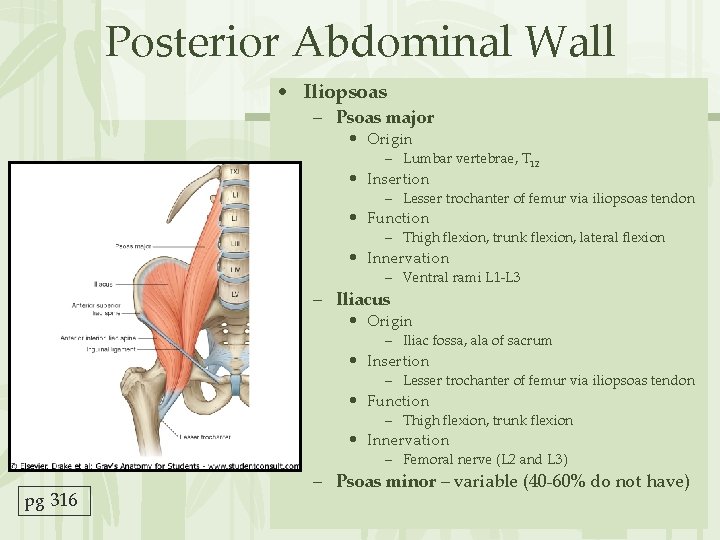
Posterior Abdominal Wall • Iliopsoas – Psoas major • Origin – Lumbar vertebrae, T 12 • Insertion – Lesser trochanter of femur via iliopsoas tendon • Function – Thigh flexion, trunk flexion, lateral flexion • Innervation – Ventral rami L 1 -L 3 – Iliacus • Origin – Iliac fossa, ala of sacrum • Insertion – Lesser trochanter of femur via iliopsoas tendon • Function – Thigh flexion, trunk flexion • Innervation – Femoral nerve (L 2 and L 3) pg 316 – Psoas minor – variable (40 -60% do not have)

Posterior Abdominal Wall • Quadratus lumborum – Origin • Iliac crest and lumbar fascia – Insertion • Transverse process of upper lumbar vertebrae, lower margin of rib 12 – Function • Flex vertebral column, maintains upright posture, assists in inspiration – Innervation: • T 12 and upper lumbar spinal nerves (ventral rami) pg 316

Peritoneum • Mesenteries – Double layer of peritoneum (2 serous membranes fused together) – Extend to the digestive organs from the body wall – Function: • Hold organs in place • Sites of fat storage • Provide a route for vessels and nerves – Dorsal mesenteries: • Lesser omentum and Falciform ligament – Ventral mesenteries: • Greater omentum, Transverse mesocolon, Mesentary, and Sigmoid mesocolon

Dorsal Mesenteries pg 269 pg 291

Ventral Mesenteries pg 271 pg 269
Peritoneum • Peritoneal – Remains surrounded by peritoneal cavity – Liver, stomach, ileum and jejunum • Retroperitoneal – Some organs lay behind/outside peritoneum • Primarily retroperitoneal – Organs NEVER within the cavity – Kidneys, bladder, ureter • Secondarily retroperitoneal – Organs once suspended within the abdominal cavity by mesentery – Migrate posterior to the peritoneum during the course of embryogenesis to become retroperitoneal – Lack mesenteries – Duodenum, ascending and descending colon, rectum, pancreas
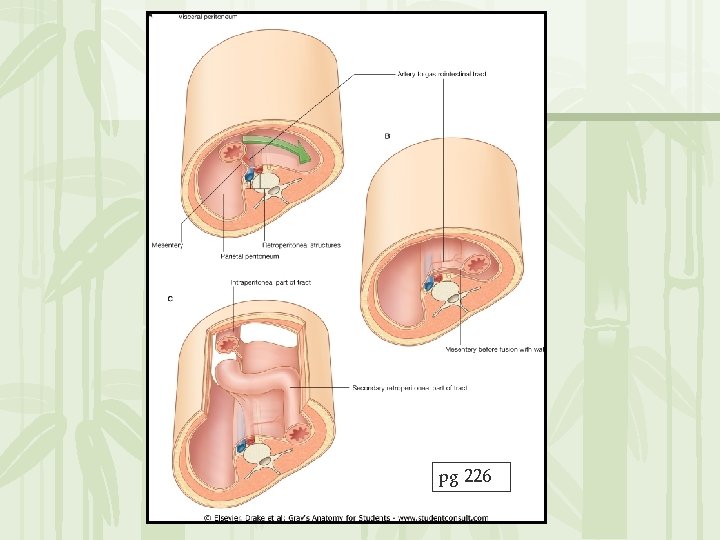
pg 226
Organs of the Abdomen Urinary and Digestive Systems
Urinary System
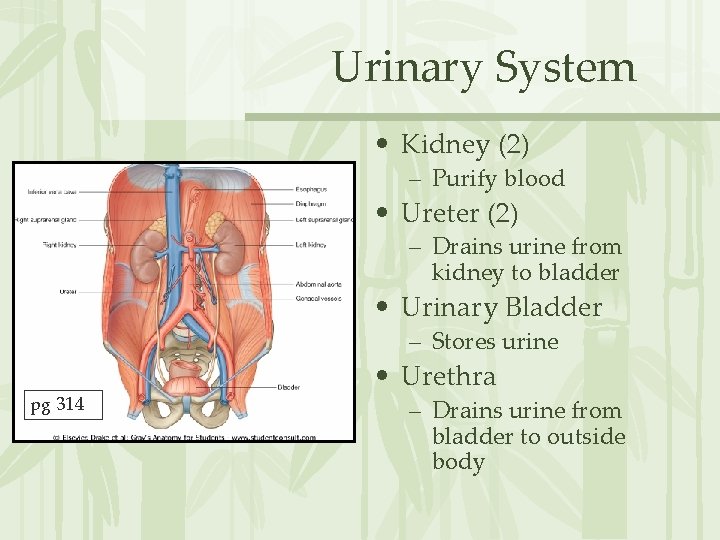
Urinary System • Kidney (2) – Purify blood • Ureter (2) – Drains urine from kidney to bladder • Urinary Bladder – Stores urine pg 314 • Urethra – Drains urine from bladder to outside body
Kidneys • Filter waste from blood – Water, toxins, urea, uric acid, creatinine, metabolic waste, ions • Excretion of waste • Homeostasis – Acid-base balance – Blood pressure – Plasma volume
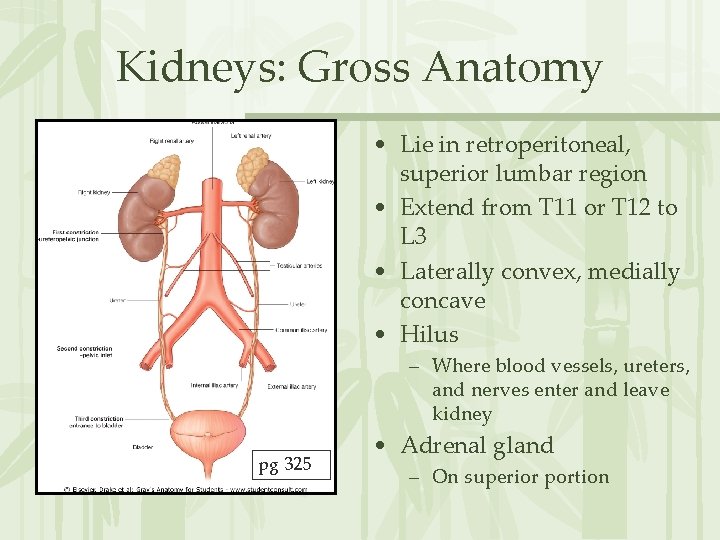
Kidneys: Gross Anatomy • Lie in retroperitoneal, superior lumbar region • Extend from T 11 or T 12 to L 3 • Laterally convex, medially concave • Hilus – Where blood vessels, ureters, and nerves enter and leave kidney pg 325 • Adrenal gland – On superior portion
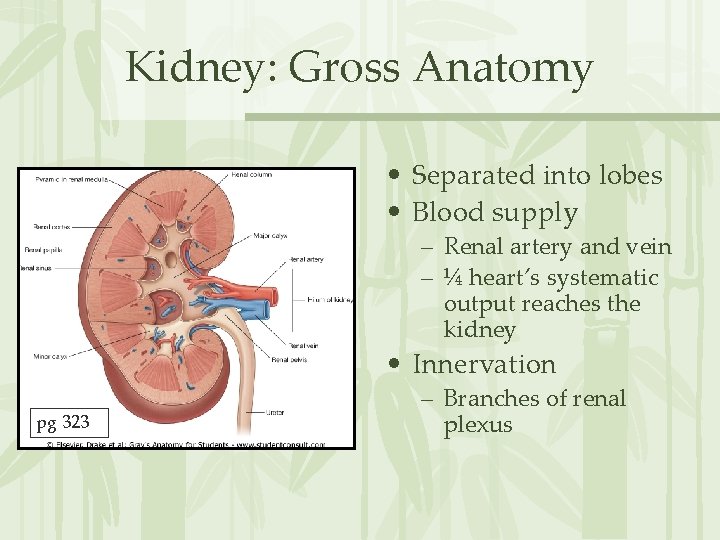
Kidney: Gross Anatomy • Separated into lobes • Blood supply – Renal artery and vein – ¼ heart’s systematic output reaches the kidney • Innervation pg 323 – Branches of renal plexus

Kidney: Gross Anatomy Internal • Supportive tissue – Renal capsule • DCT • Adheres directly to kidney surface • Maintains shape and forms barrier – Adipose capsule • Perirenal fat • Cushions kidney • Keeps kidney in place pg 322 – Renal fascia – Pararenal fat • Cushions kidney • Keeps kidney in place External
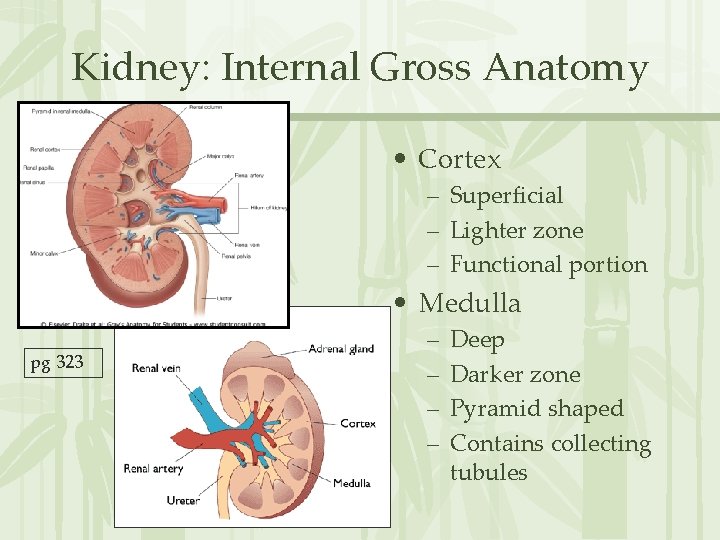
Kidney: Internal Gross Anatomy • Cortex – Superficial – Lighter zone – Functional portion • Medulla pg 323 – – Deep Darker zone Pyramid shaped Contains collecting tubules
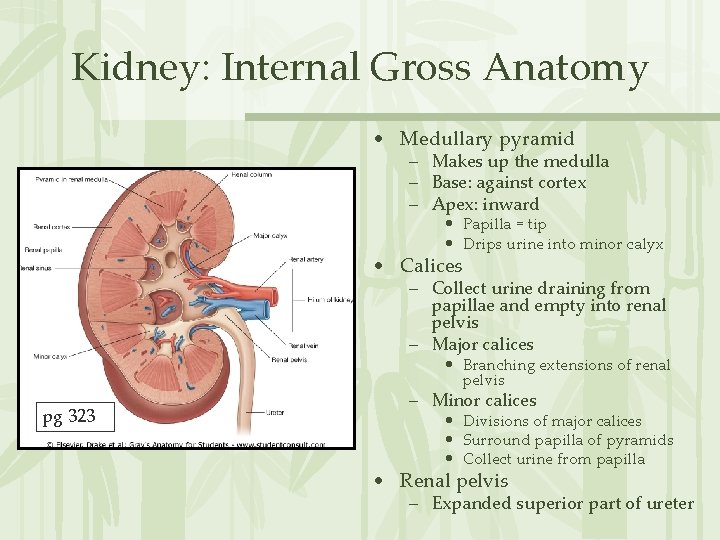
Kidney: Internal Gross Anatomy • Medullary pyramid – Makes up the medulla – Base: against cortex – Apex: inward • Papilla = tip • Drips urine into minor calyx • Calices – Collect urine draining from papillae and empty into renal pelvis – Major calices • Branching extensions of renal pelvis pg 323 – Minor calices • Divisions of major calices • Surround papilla of pyramids • Collect urine from papilla • Renal pelvis – Expanded superior part of ureter

Kidney: Internal Vasculature • Renal arteries • Segmental arteries – Enter through the hilus – Branch into: • Lobar arteries • Interlobar arteries • Arcuate arteries pg 323 – At border of cortex and medulla • Interlobular arteries
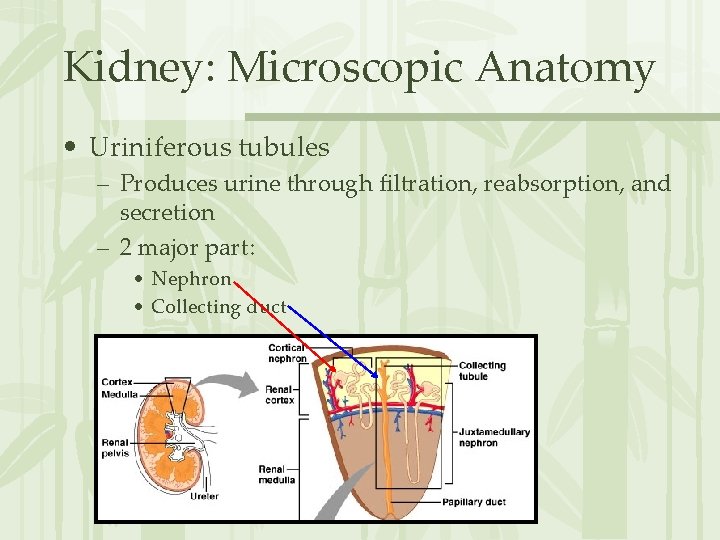
Kidney: Microscopic Anatomy • Uriniferous tubules – Produces urine through filtration, reabsorption, and secretion – 2 major part: • Nephron • Collecting duct
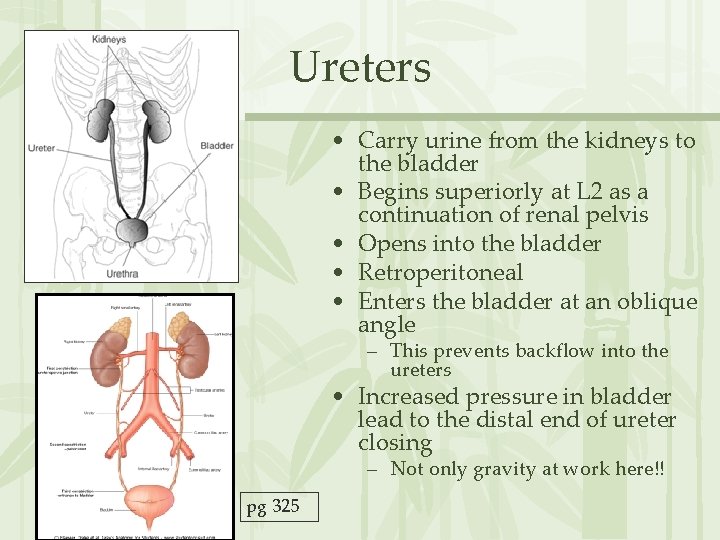
Ureters • Carry urine from the kidneys to the bladder • Begins superiorly at L 2 as a continuation of renal pelvis • Opens into the bladder • Retroperitoneal • Enters the bladder at an oblique angle – This prevents backflow into the ureters • Increased pressure in bladder lead to the distal end of ureter closing – Not only gravity at work here!! pg 325
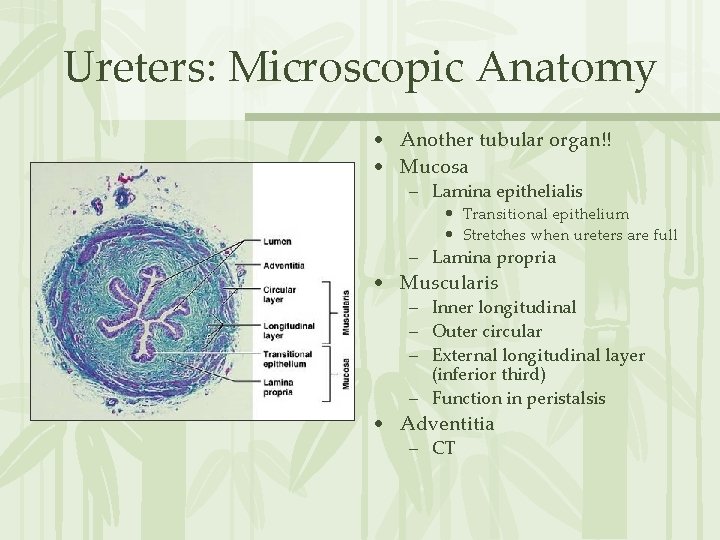
Ureters: Microscopic Anatomy • Another tubular organ!! • Mucosa – Lamina epithelialis • Transitional epithelium • Stretches when ureters are full – Lamina propria • Muscularis – Inner longitudinal – Outer circular – External longitudinal layer (inferior third) – Function in peristalsis • Adventitia – CT

Urinary Bladder • Stores and expels urine • Posterolateral angle receives the ureter • Inferior angle drains into the urethra • Located: – – Inferior to peritoneal cavity On pelvic floor Posterior to pubic symphysis Male: • Anterior to rectum – Female: • Anterior to vagina and uterus pg 400
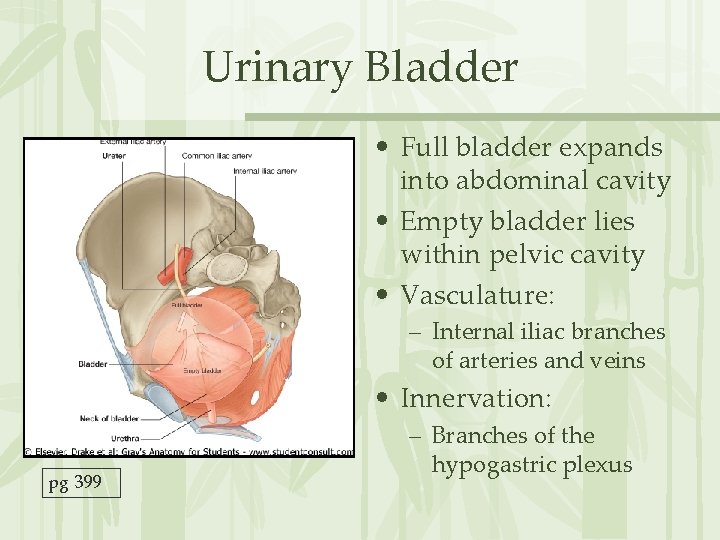
Urinary Bladder • Full bladder expands into abdominal cavity • Empty bladder lies within pelvic cavity • Vasculature: – Internal iliac branches of arteries and veins • Innervation: pg 399 – Branches of the hypogastric plexus
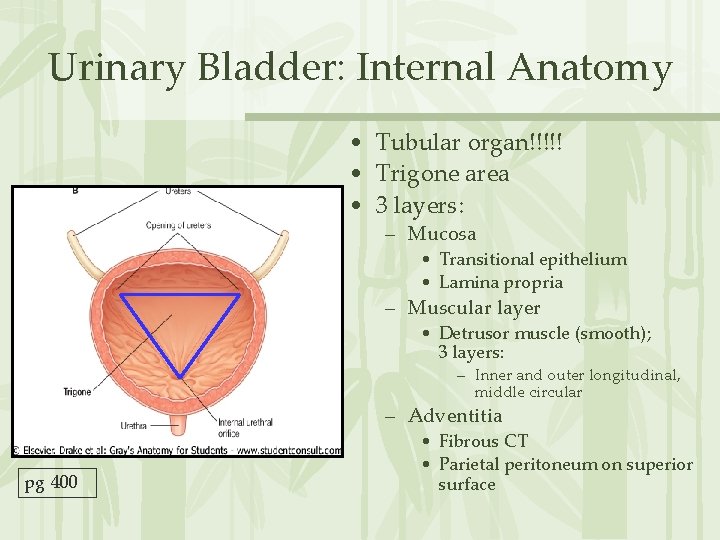
Urinary Bladder: Internal Anatomy • Tubular organ!!!!! • Trigone area • 3 layers: – Mucosa • Transitional epithelium • Lamina propria – Muscular layer • Detrusor muscle (smooth); 3 layers: – Inner and outer longitudinal, middle circular – Adventitia pg 400 • Fibrous CT • Parietal peritoneum on superior surface
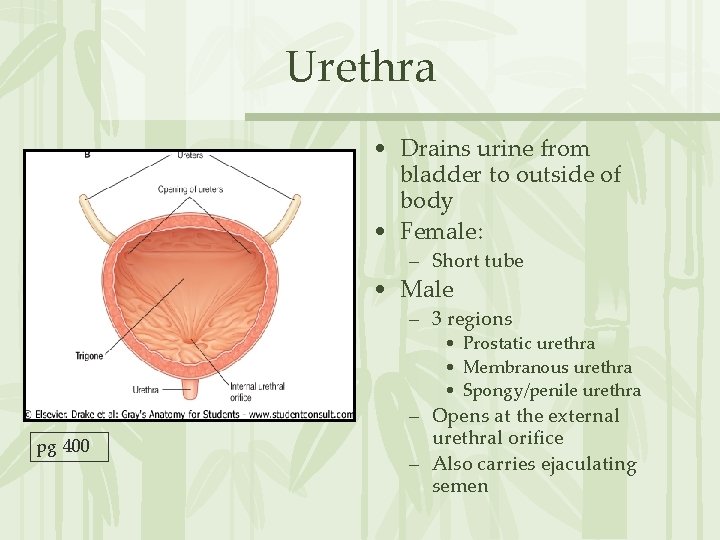
Urethra • Drains urine from bladder to outside of body • Female: – Short tube • Male – 3 regions • Prostatic urethra • Membranous urethra • Spongy/penile urethra pg 400 – Opens at the external urethral orifice – Also carries ejaculating semen
Urethra Landmarks • Internal urethral sphincter – – At bladder/urethral junction Thickening of detrusor muscle Involuntary; keeps urethra closed when urine is not being passed Prevents dribbling! • External urethral sphincter – Surrounds urethra within the urogenital diaphragm – Inhibits voluntary urination until ready • External urethral orifice – Males: • End of the penile urethra – Females: • Anterior to vaginal opening and posterior to clitoris

Males versus Females: pg 403
Micturition = Urination • Contraction of the detrusor muscle to raise intraabdominal pressure • Controlled by the brain • Urine accumulation leads to distention of the bladder – Activates stretch receptors – Send sensory impulses to micturition center (MC) in the pons • MC sends signals to parasympathetic neurons – Stimulate detrusor muscle to contract (involuntary) – Internal urinary sphincter opens (also inhibits sympathetic pathways that would prevent urination)
Micturition = Urination • Other brain receptors (pons, cerebral cortex) can inhibit urination – Relaxing of the detrusor, keeping external urinary sphincter closed • Voluntary contraction of abdominal wall muscles increases abdominal pressure • Voluntary relaxation of external urethral sphincter
Digestive System
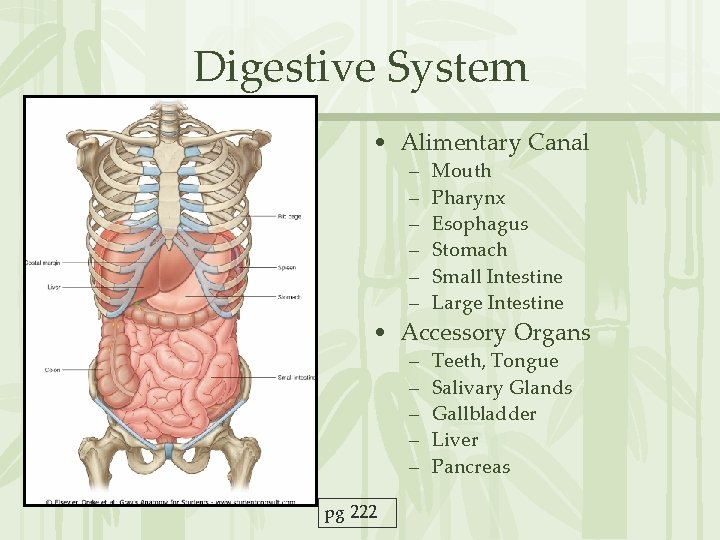
Digestive System • Alimentary Canal – – – Mouth Pharynx Esophagus Stomach Small Intestine Large Intestine – – – Teeth, Tongue Salivary Glands Gallbladder Liver Pancreas • Accessory Organs pg 222
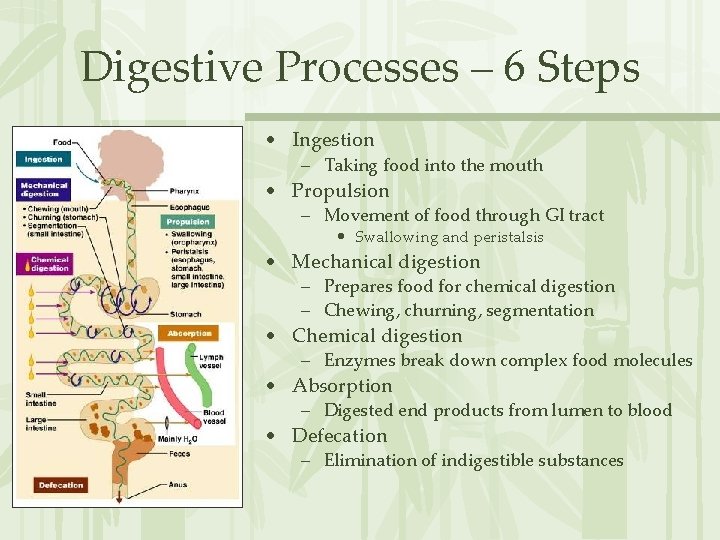
Digestive Processes – 6 Steps • Ingestion – Taking food into the mouth • Propulsion – Movement of food through GI tract • Swallowing and peristalsis • Mechanical digestion – Prepares food for chemical digestion – Chewing, churning, segmentation • Chemical digestion – Enzymes break down complex food molecules • Absorption – Digested end products from lumen to blood • Defecation – Elimination of indigestible substances

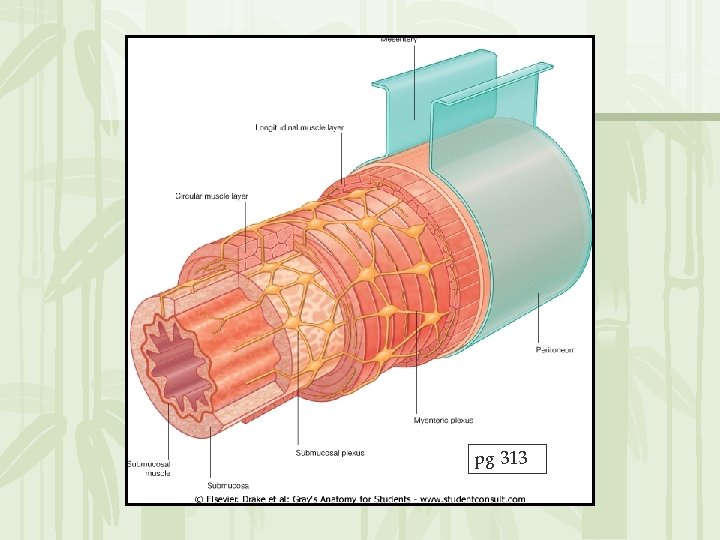
Alimentary Canal Wall • ANOTHER tubular organ! • Layers: – Mucosa • Epithelium • Lamina propria (MALT) • Lamina muscularis mucosa – Submucosa • CT with elastic fibers, nerves, vessels – Muscularis pg 313 • Inner circular • Outer longitudinal • Creates sphincters – Serosa / Adventitia

Peristalsis vs Segmentation • Peristalsis – Propulsion – Adjacent segments of the alimentary canal contract and relax – Moves food distally along the canal • Segmentation – Part of mechanical breakdown – Food-mixing process – Nonadjacent segments of the intestine alternatively contract and relax – Moves food on and back – Mixes rather than propels

Innervation • Nerve plexuses – Occur within wall of alimentary canal – Parasympathetic, Sympathetic, Visceral Sensory fibers – 2 types: • Myenteric nerve plexus – Between 2 muscle layers of the tunica muscularis – Controls segmentation and peristalsis • Submucosal nerve plexus – Between submucosa and muscularis mucosa – Signals glands to secrete and LMM to contract
pg 313
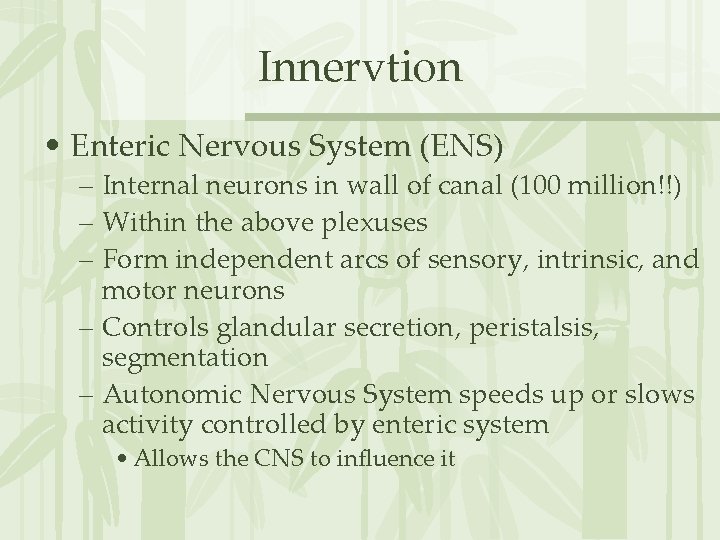
Innervtion • Enteric Nervous System (ENS) – Internal neurons in wall of canal (100 million!!) – Within the above plexuses – Form independent arcs of sensory, intrinsic, and motor neurons – Controls glandular secretion, peristalsis, segmentation – Autonomic Nervous System speeds up or slows activity controlled by enteric system • Allows the CNS to influence it
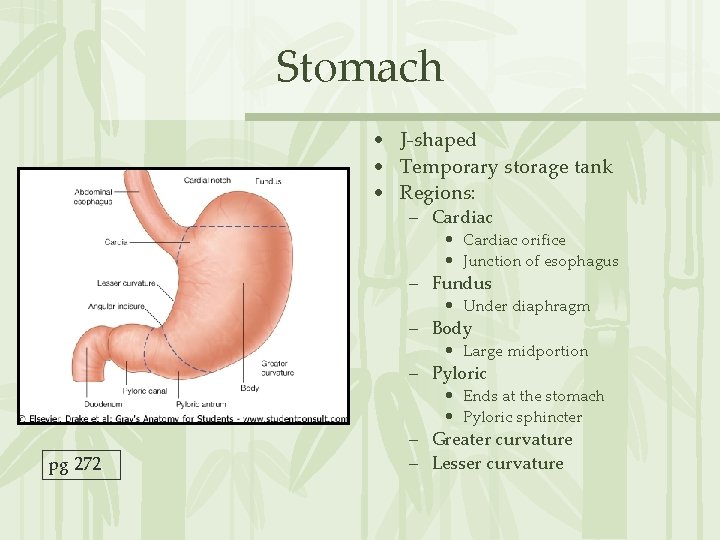
Stomach • J-shaped • Temporary storage tank • Regions: – Cardiac • Cardiac orifice • Junction of esophagus – Fundus • Under diaphragm – Body • Large midportion – Pyloric • Ends at the stomach • Pyloric sphincter pg 272 – Greater curvature – Lesser curvature
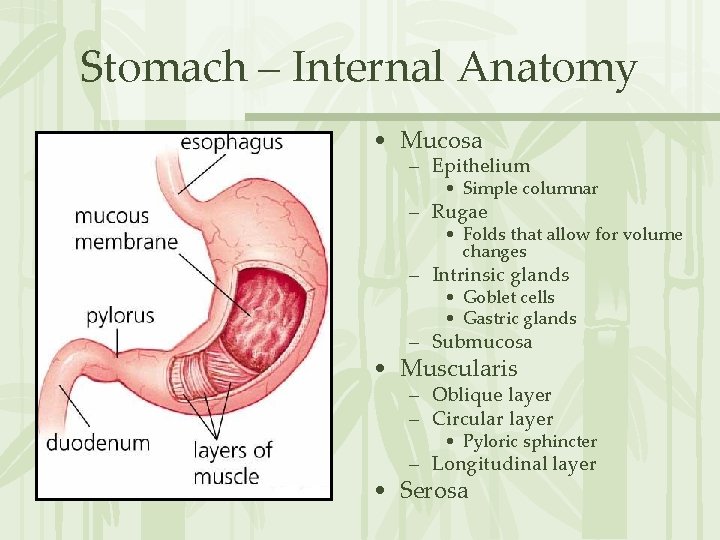
Stomach – Internal Anatomy • Mucosa – Epithelium • Simple columnar – Rugae • Folds that allow for volume changes – Intrinsic glands • Goblet cells • Gastric glands – Submucosa • Muscularis – Oblique layer – Circular layer • Pyloric sphincter – Longitudinal layer • Serosa
Stomach Function • Storage of chyme – Food paste • Breakdown of food proteins – Done by pepsin • Protein-digestion under acidic conditions • Absorption of nutrients – H 2 O, electrolytes – Alcohol, other drugs • Food remains for about 4 hours • Holds from 1. 5 to 4 liters
Small Intestine • Longest portion of GI tract • Site of most enzymatic digestion and absorption of nutrients – Bile: emulsifier (gallbladder, liver) – Enzymes (pancreas) • Undergoes segmentation – Allows for an increase contact with intestinal walls • Peristalsis propels chyme through in about 3 to 6 hours • 2. 6 to 6 meters long!!
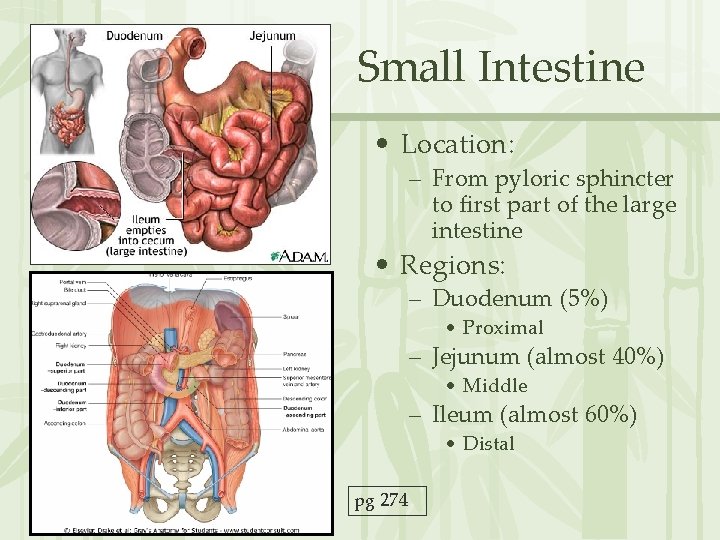
Small Intestine • Location: – From pyloric sphincter to first part of the large intestine • Regions: – Duodenum (5%) • Proximal – Jejunum (almost 40%) • Middle – Ileum (almost 60%) • Distal pg 274
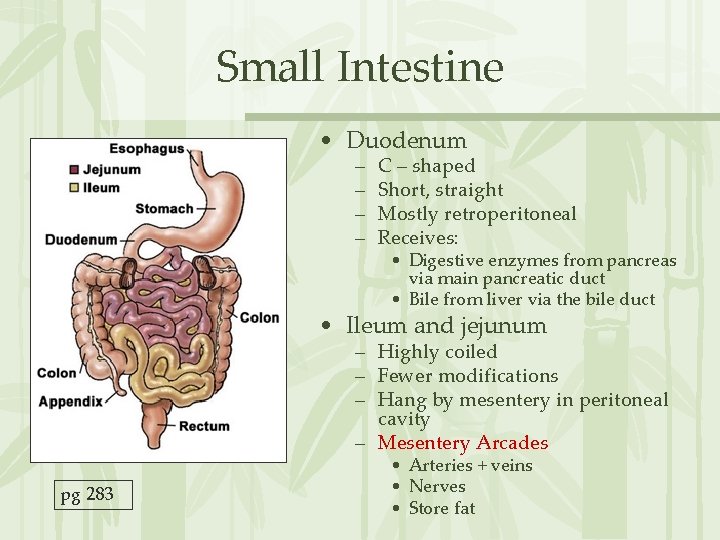
Small Intestine • Duodenum – – C – shaped Short, straight Mostly retroperitoneal Receives: • Digestive enzymes from pancreas via main pancreatic duct • Bile from liver via the bile duct • Ileum and jejunum – Highly coiled – Fewer modifications – Hang by mesentery in peritoneal cavity – Mesentery Arcades pg 283 • Arteries + veins • Nerves • Store fat

Small Intestine Internal Anatomy • Intestinal flora – produces vitamin K • Epithelium: – Simple columnar epithelium with many modifications for absorption • Lymph tissue in submucosa • Muscularis externa has 2 layers • Innervation: – Some parasympathetic innervation from vagus • Arterial supply: – Superior mesenteric – Rt (cranial) pancreaticoduodenal pg 283
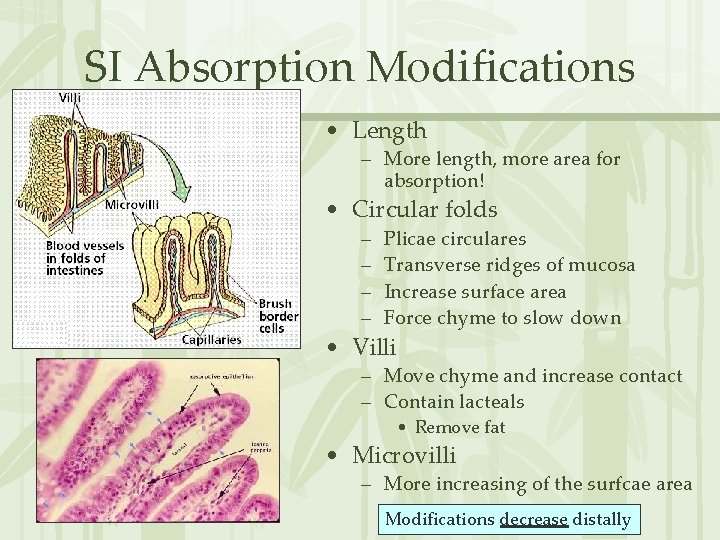
SI Absorption Modifications • Length – More length, more area for absorption! • Circular folds – – Plicae circulares Transverse ridges of mucosa Increase surface area Force chyme to slow down • Villi – Move chyme and increase contact – Contain lacteals • Remove fat • Microvilli – More increasing of the surfcae area Modifications decrease distally

Large Intestine • Regions: – Cecum – Vermiform appendix – Colon • Ascending • Transverse • Descending • Sigmoid – Rectum – Anal Canal pg 279
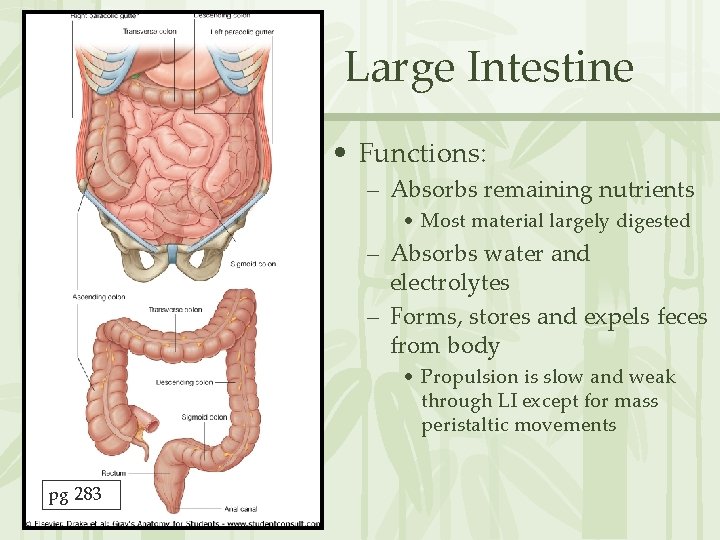
Large Intestine • Functions: – Absorbs remaining nutrients • Most material largely digested – Absorbs water and electrolytes – Forms, stores and expels feces from body • Propulsion is slow and weak through LI except for mass peristaltic movements pg 283
LI: Internal Features • • Intestinal flora No intestinal villi or modifications for absorption Many goblet cells Simple columnar epithelium except lower half of anal canal • Significant lymph tissue in mucosa and submucosa • Muscularis mucosae has 2 layers • Some parasympathetic innervation from vagus
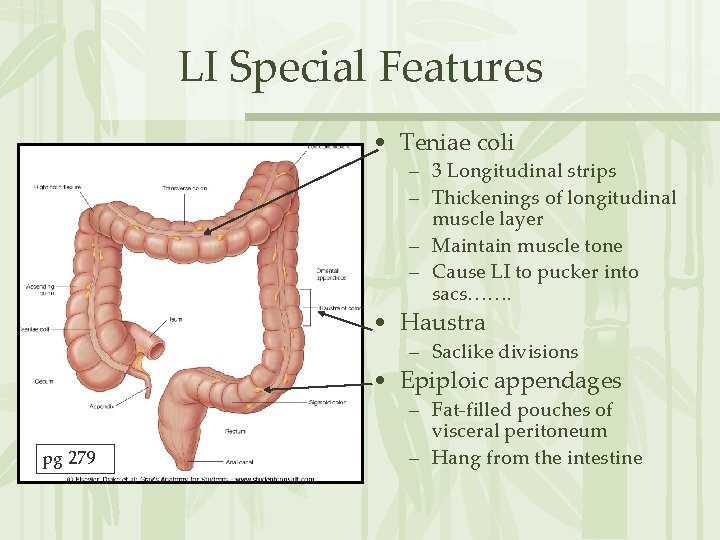
LI Special Features • Teniae coli – 3 Longitudinal strips – Thickenings of longitudinal muscle layer – Maintain muscle tone – Cause LI to pucker into sacs……. • Haustra – Saclike divisions • Epiploic appendages pg 279 – Fat-filled pouches of visceral peritoneum – Hang from the intestine

Cecum and Vermiform Appendix • Cecum – Sac-like pouch (blind pouch) – Ileocecal valve • 2 raised edges of the mucosa • Sphincter keeps closed until food in stomach • Prevents reflux of feces from cecum to ileum • Vermiform Appendix – Blind tube – Opens into cecum – Contains large masses of lymphoid tissue pg 276
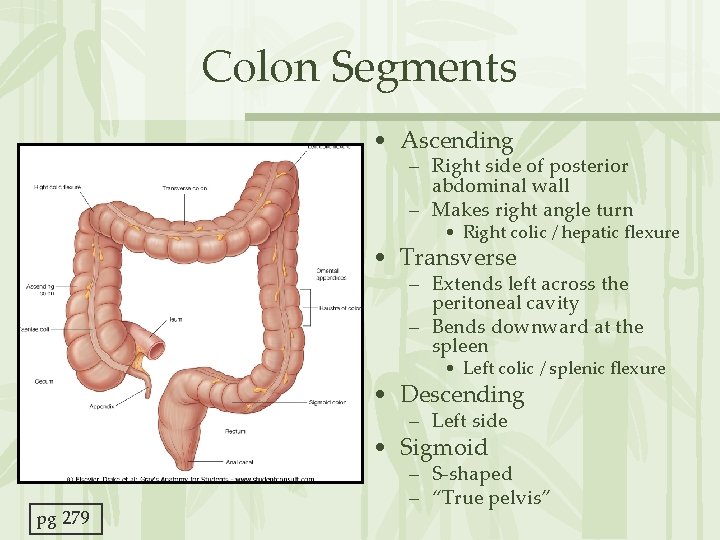
Colon Segments • Ascending – Right side of posterior abdominal wall – Makes right angle turn • Right colic / hepatic flexure • Transverse – Extends left across the peritoneal cavity – Bends downward at the spleen • Left colic / splenic flexure • Descending – Left side • Sigmoid pg 279 – S-shaped – “True pelvis”
Colon Functions • Absorb H 2 O and electrolytes • Some digestion by bacteria • Mass Peristaltic Movements (2 -3 x day) • Moves through in 12 -24 hours • 1. 5 meters
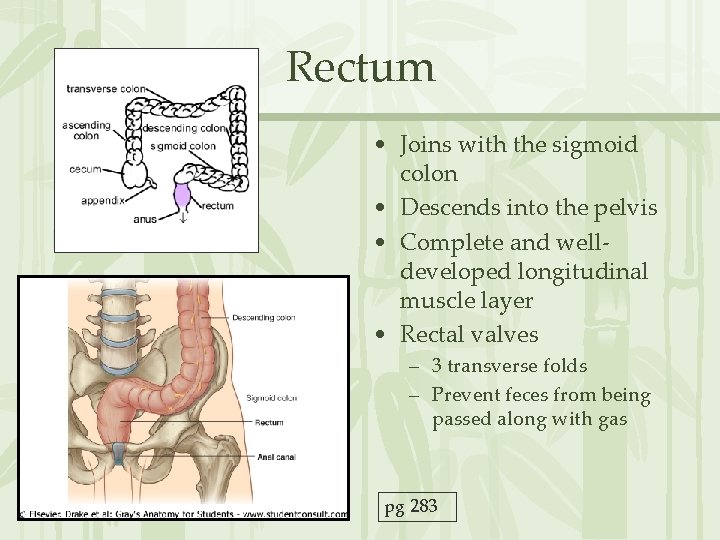
Rectum • Joins with the sigmoid colon • Descends into the pelvis • Complete and welldeveloped longitudinal muscle layer • Rectal valves – 3 transverse folds – Prevent feces from being passed along with gas pg 283

Anal Canal • Begins where rectum passes through the levator ani muscle • Releases mucus to lubricate feces • Internal anal sphincter – Made of smooth muscle – Involuntary • External anal sphincter – Made of skeletal muscle – Voluntary – Toilet training!!! • Stratified squamous epithelium at lower half pg 398

Defecation • Stretching of rectal wall initiates defecation reflex • Mediated by the spinal cord – Parasympathetic reflex signals walls of sigmoid colon and rectum to contract and anal sphincters to relax – Involuntary • If not ready, reflective contraction ends and rectum relaxes – Reflex initiated again until you actually defecate • Contraction of diaphragm, levator ani and abdominal muscles assist – Voluntary
Accessory Digestive Organs
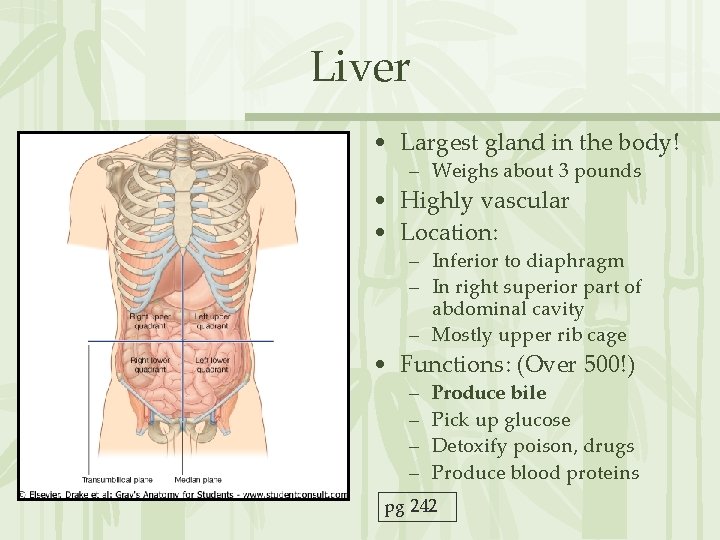
Liver • Largest gland in the body! – Weighs about 3 pounds • Highly vascular • Location: – Inferior to diaphragm – In right superior part of abdominal cavity – Mostly upper rib cage • Functions: (Over 500!) – – Produce bile Pick up glucose Detoxify poison, drugs Produce blood proteins pg 242
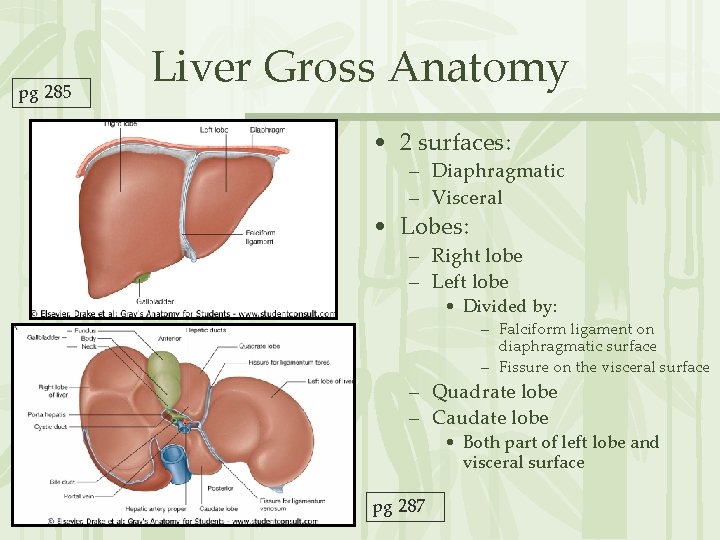
pg 285 Liver Gross Anatomy • 2 surfaces: – Diaphragmatic – Visceral • Lobes: – Right lobe – Left lobe • Divided by: – Falciform ligament on diaphragmatic surface – Fissure on the visceral surface – Quadrate lobe – Caudate lobe • Both part of left lobe and visceral surface pg 287
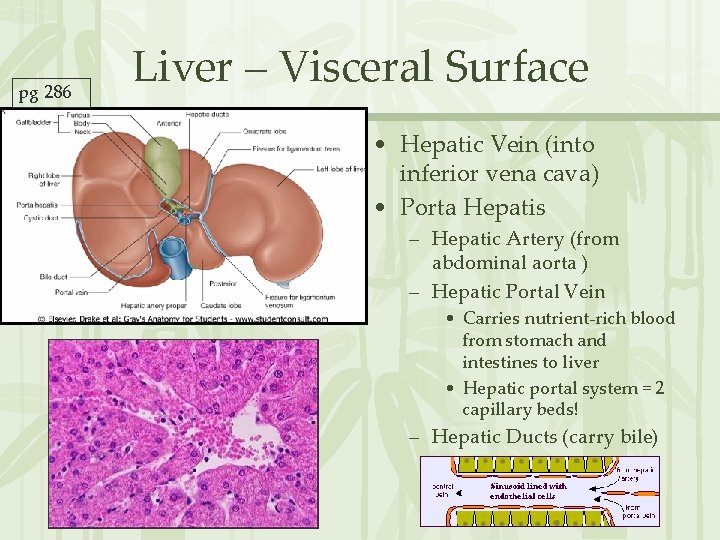
pg 286 Liver – Visceral Surface • Hepatic Vein (into inferior vena cava) • Porta Hepatis – Hepatic Artery (from abdominal aorta ) – Hepatic Portal Vein • Carries nutrient-rich blood from stomach and intestines to liver • Hepatic portal system = 2 capillary beds! – Hepatic Ducts (carry bile)
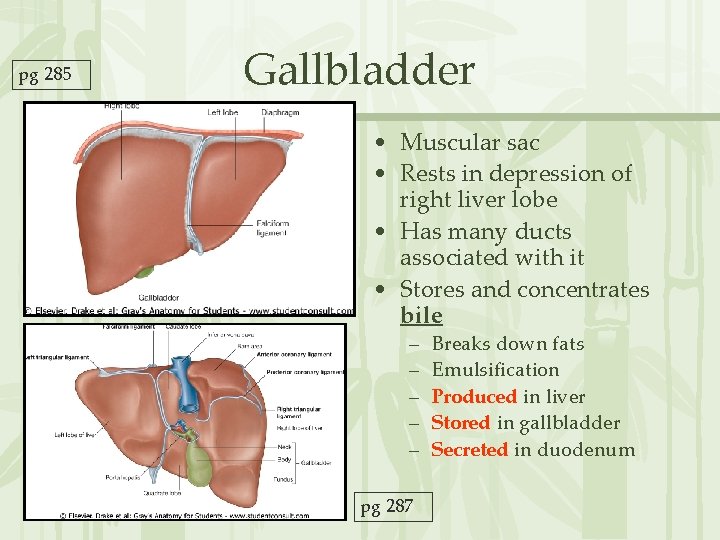
pg 285 Gallbladder • Muscular sac • Rests in depression of right liver lobe • Has many ducts associated with it • Stores and concentrates bile – – – pg 287 Breaks down fats Emulsification Produced in liver Stored in gallbladder Secreted in duodenum
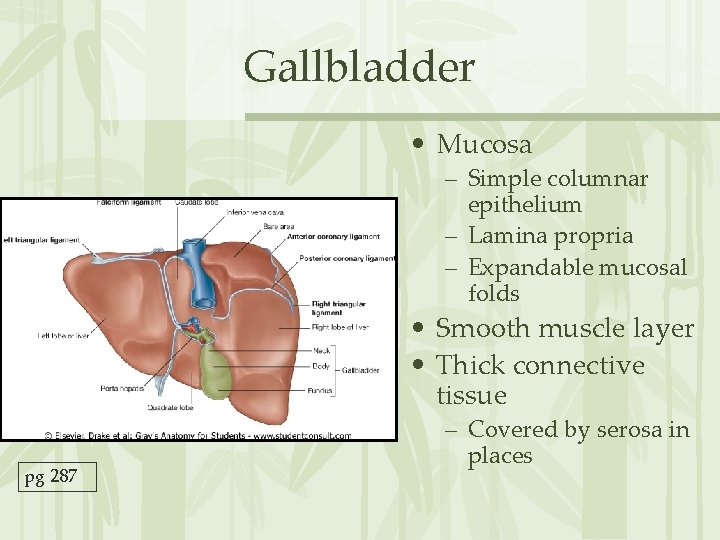
Gallbladder • Mucosa – Simple columnar epithelium – Lamina propria – Expandable mucosal folds • Smooth muscle layer • Thick connective tissue pg 287 – Covered by serosa in places
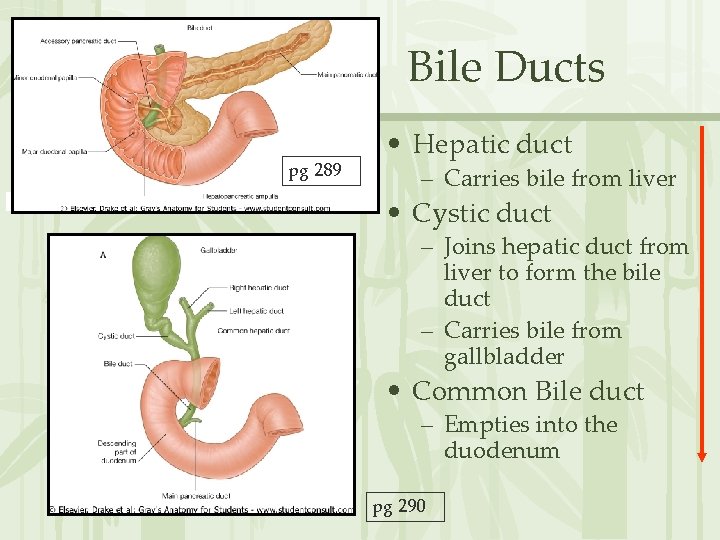
Bile Ducts pg 289 • Hepatic duct – Carries bile from liver • Cystic duct – Joins hepatic duct from liver to form the bile duct – Carries bile from gallbladder • Common Bile duct – Empties into the duodenum pg 290
Movement of Bile • Bile secreted by liver continuously • Hepatopancreatic (Vater) ampulla – common bile + main pancreatic duct meet and enter duodenum – Sphincter of Oddi around it – closed when bile not needed for digestion • Bile then backs up into gallbladder via cystic duct • When needed gallbladder contracts, sphincters open
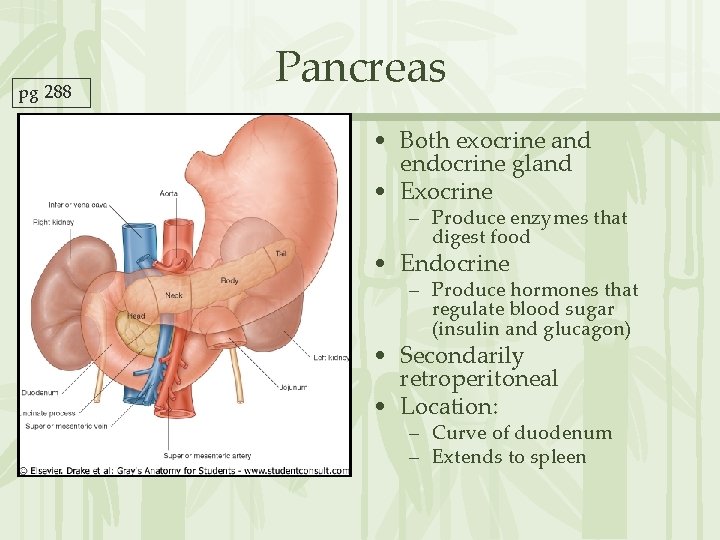
pg 288 Pancreas • Both exocrine and endocrine gland • Exocrine – Produce enzymes that digest food • Endocrine – Produce hormones that regulate blood sugar (insulin and glucagon) • Secondarily retroperitoneal • Location: – Curve of duodenum – Extends to spleen

Pancreatic Ducts • Main pancreatic duct – Extends length of pancreas – Joins bile duct to form the hepatopancreatic ampulla – Empties into duodenum • Accessory pancreatic duct – Lies in head of pancreas – Drains into the main duct – Enters duodenum also pg 289
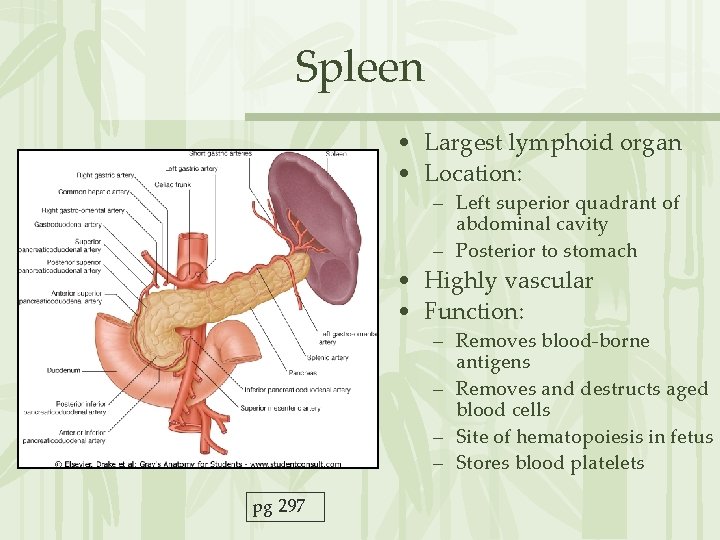
Spleen • Largest lymphoid organ • Location: – Left superior quadrant of abdominal cavity – Posterior to stomach • Highly vascular • Function: – Removes blood-borne antigens – Removes and destructs aged blood cells – Site of hematopoiesis in fetus – Stores blood platelets pg 297
Arterial Blood Supply to Abdominal Viscera • All branches of Abdominal Aorta • Anastomoses – – – Left + Middle colic Left + Right gastroepiploic Cranial + Caudal pancreaticoduodenal Deep Iliac Circumflex + Adrenolumbar • Remember your zoological roots: YOU MUST KNOW WHAT SUPPLIES WHAT!!
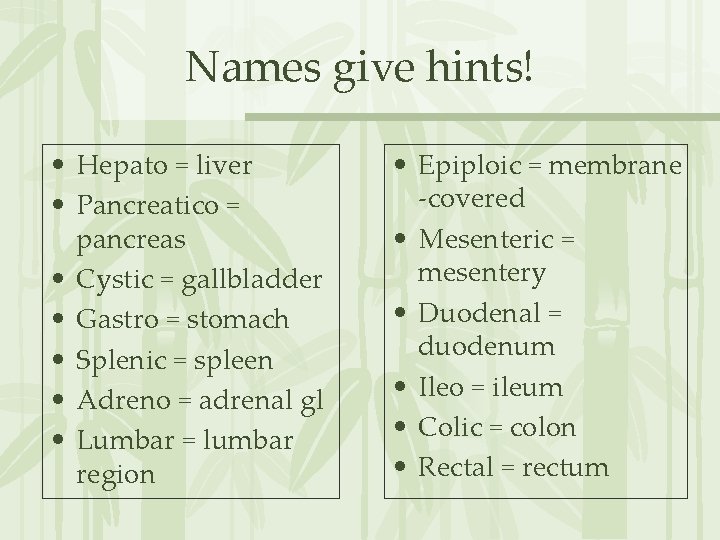
Names give hints! • Hepato = liver • Pancreatico = pancreas • Cystic = gallbladder • Gastro = stomach • Splenic = spleen • Adreno = adrenal gl • Lumbar = lumbar region • Epiploic = membrane -covered • Mesenteric = mesentery • Duodenal = duodenum • Ileo = ileum • Colic = colon • Rectal = rectum
- Slides: 75