The 4 th CRRT master course CRRT Initiation

- Slides: 30
The 4 th CRRT master course (CRRT Initiation, Dose, Stop) 이상헌

CRRT initiation § Potential advantages of Early RRT § Prevention of the deleterious consequences of § § Fluid overload Electrolyte disturbance Acidosis Uremia § Prevention of further escalation of harmful medical therapies inotropics, fluid loading, diuretics…. . § Immunomodulation from RRT Schetz. 19 th International Vicenza Course on Critical Care Nephrology 2010
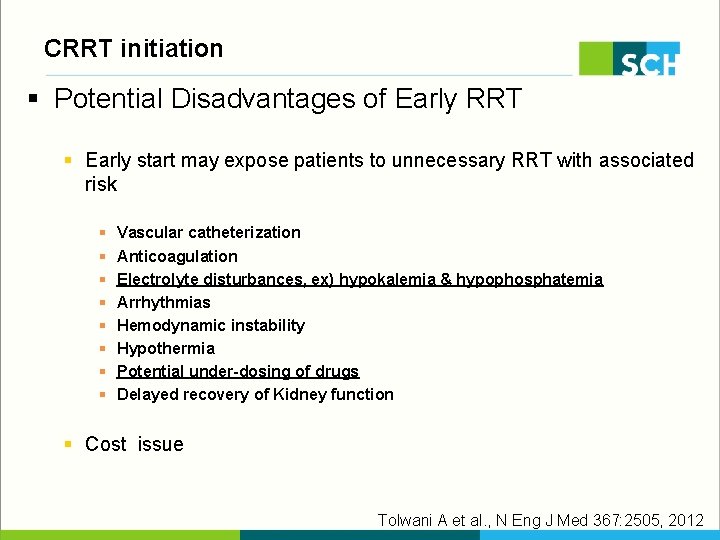
CRRT initiation § Potential Disadvantages of Early RRT § Early start may expose patients to unnecessary RRT with associated risk § § § § Vascular catheterization Anticoagulation Electrolyte disturbances, ex) hypokalemia & hypophosphatemia Arrhythmias Hemodynamic instability Hypothermia Potential under-dosing of drugs Delayed recovery of Kidney function § Cost issue Tolwani A et al. , N Eng J Med 367: 2505, 2012
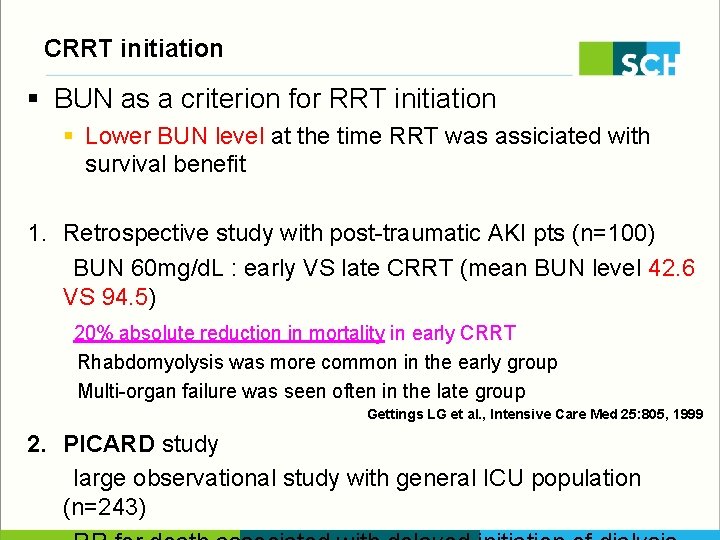
CRRT initiation § BUN as a criterion for RRT initiation § Lower BUN level at the time RRT was assiciated with survival benefit 1. Retrospective study with post-traumatic AKI pts (n=100) BUN 60 mg/d. L : early VS late CRRT (mean BUN level 42. 6 VS 94. 5) 20% absolute reduction in mortality in early CRRT Rhabdomyolysis was more common in the early group Multi-organ failure was seen often in the late group Gettings LG et al. , Intensive Care Med 25: 805, 1999 2. PICARD study large observational study with general ICU population (n=243)
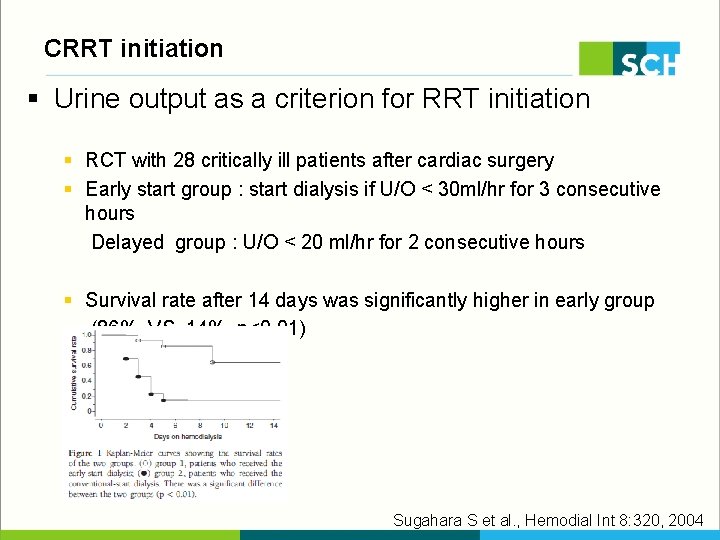
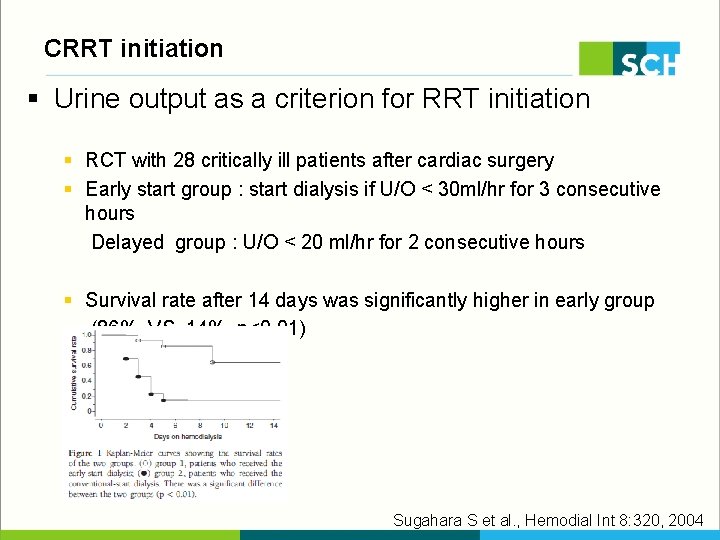
CRRT initiation § Urine output as a criterion for RRT initiation § RCT with 28 critically ill patients after cardiac surgery § Early start group : start dialysis if U/O < 30 ml/hr for 3 consecutive hours Delayed group : U/O < 20 ml/hr for 2 consecutive hours § Survival rate after 14 days was significantly higher in early group (86% VS 14%, p<0. 01) Sugahara S et al. , Hemodial Int 8: 320, 2004
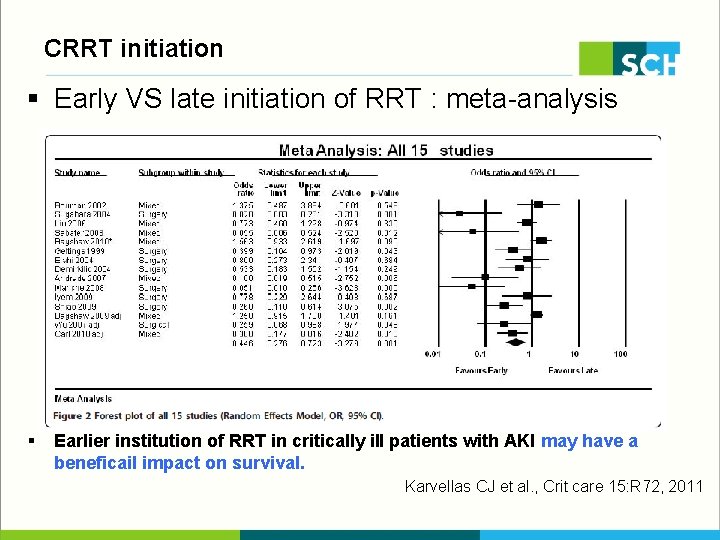
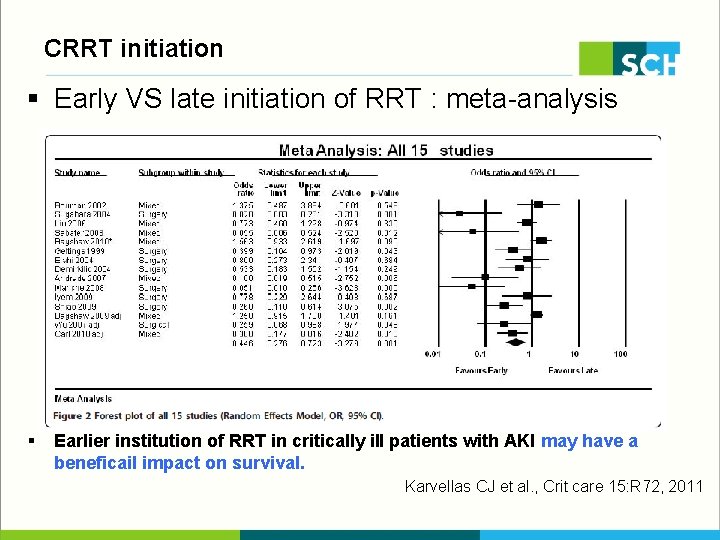
CRRT initiation § Early VS late initiation of RRT : meta-analysis § Survival rate after 14 days was significantly higher in early group (86% VS 14%, p<0. 01) § Earlier institution of RRT in critically ill patients with AKI may have a beneficail impact on survival. Karvellas CJ et al. , Crit care 15: R 72, 2011
CRRT initiation § Problems with previous studies § Variable definition of early RRT : BUN, Cr, Oliguria, Rifle criteria, Time from ICU admission…. § Residual confounding factor : inotropics, fluid loading, diuretics…. § Early group may contain patients who would not receive RRT because of dead or recovery § Appropriate large scale RCT with more accurate predictors of persistent and severe AKI Cystatin C, NGAL, KIM-1….
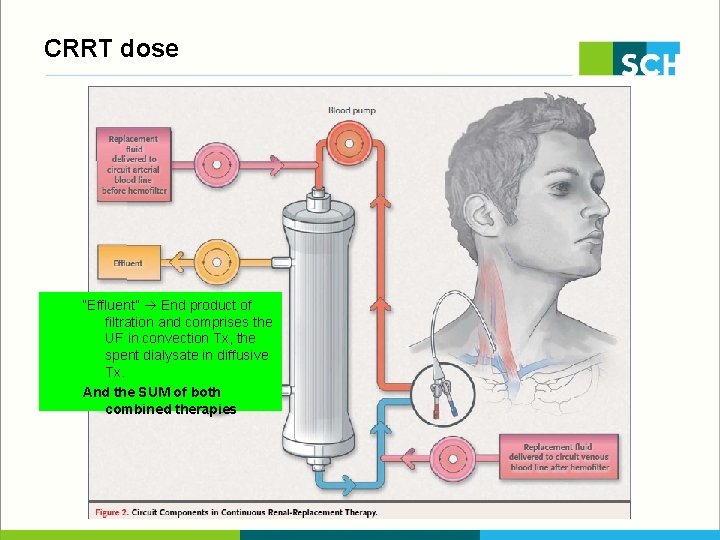
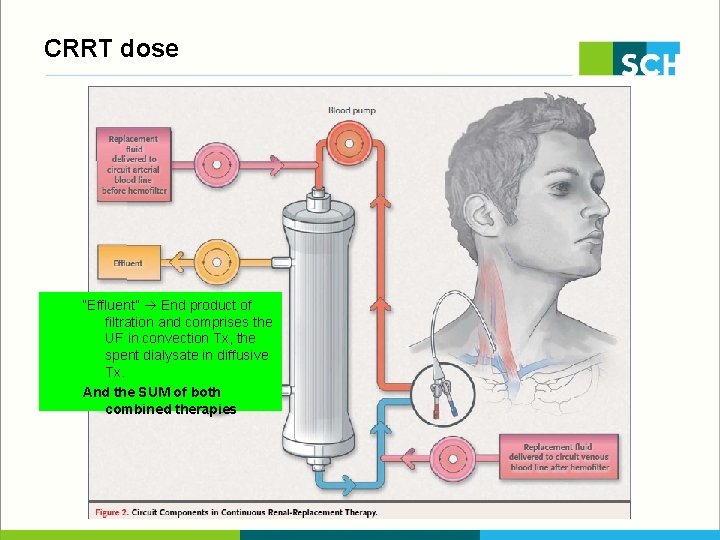
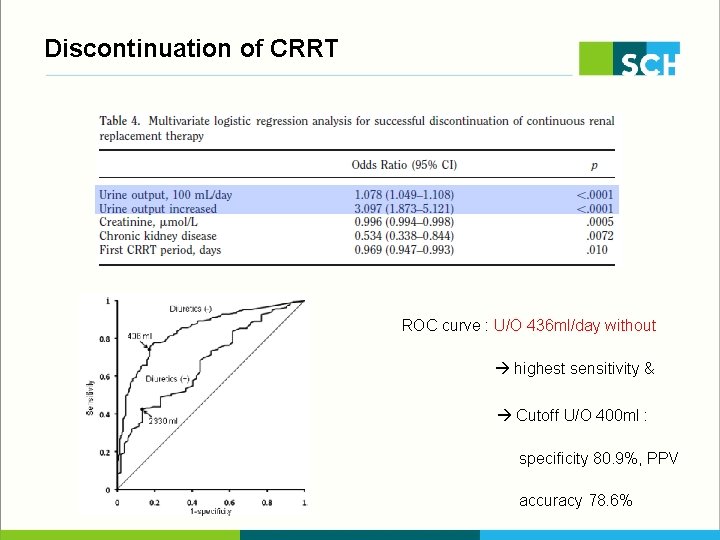
CRRT dose “Effluent” End product of filtration and comprises the UF in convection Tx, the spent dialysate in diffusive Tx. And the SUM of both combined therapies
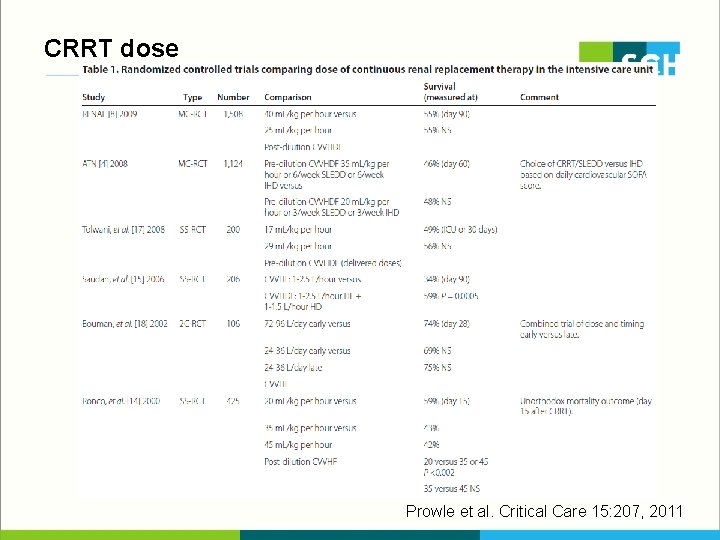
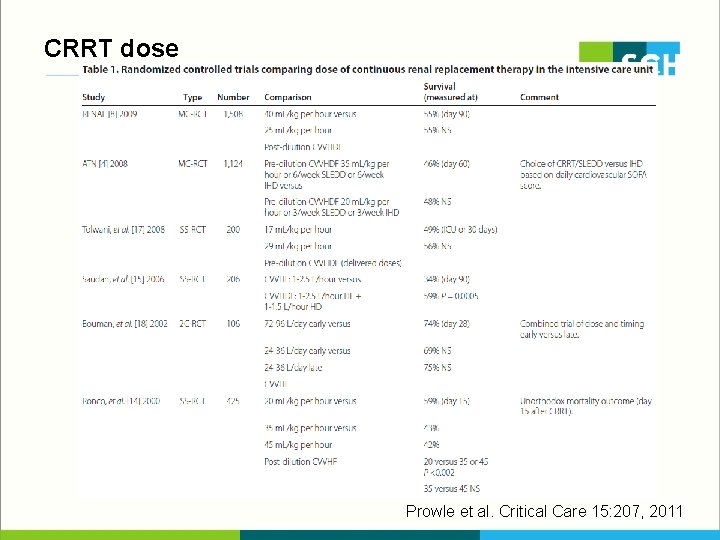
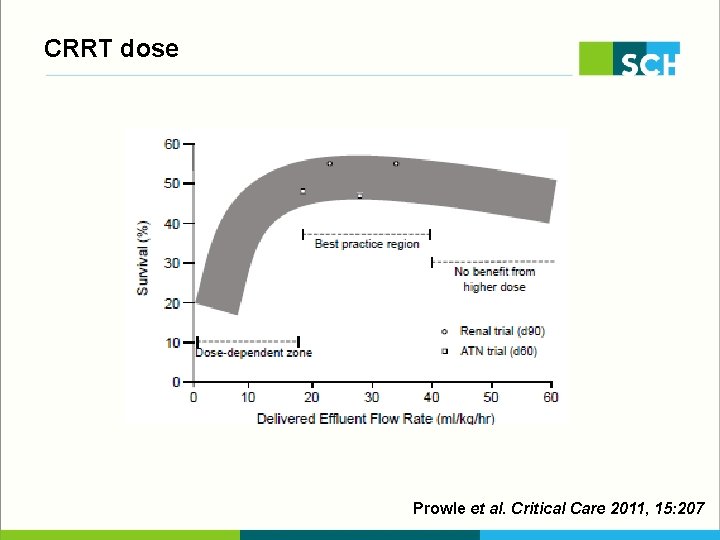
CRRT dose Prowle et al. Critical Care 15: 207, 2011
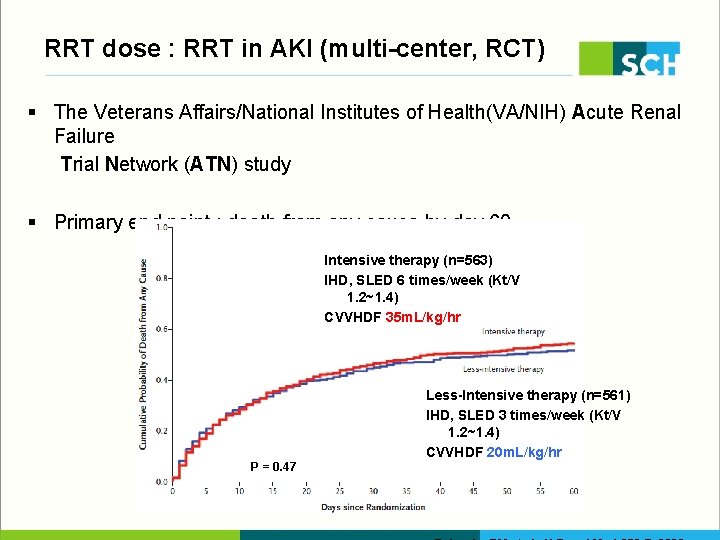
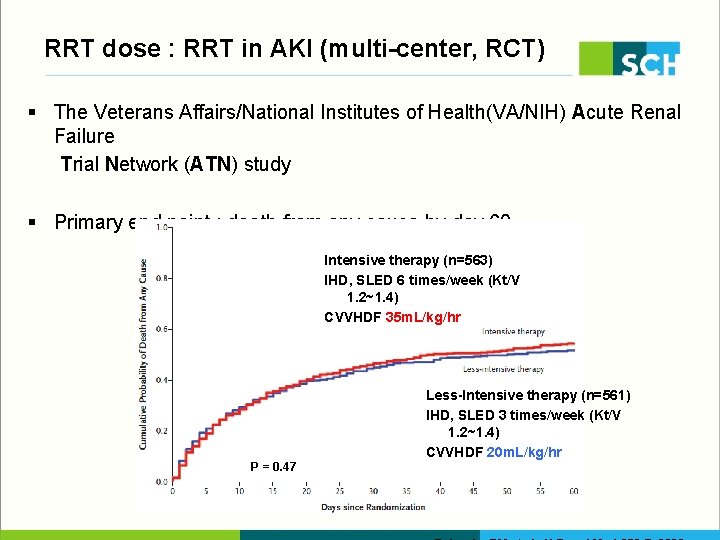
RRT dose : RRT in AKI (multi-center, RCT) § The Veterans Affairs/National Institutes of Health(VA/NIH) Acute Renal Failure Trial Network (ATN) study § Primary end point : death from any cause by day 60 Intensive therapy (n=563) IHD, SLED 6 times/week (Kt/V 1. 2~1. 4) CVVHDF 35 m. L/kg/hr Less-Intensive therapy (n=561) IHD, SLED 3 times/week (Kt/V 1. 2~1. 4) CVVHDF 20 m. L/kg/hr P = 0. 47
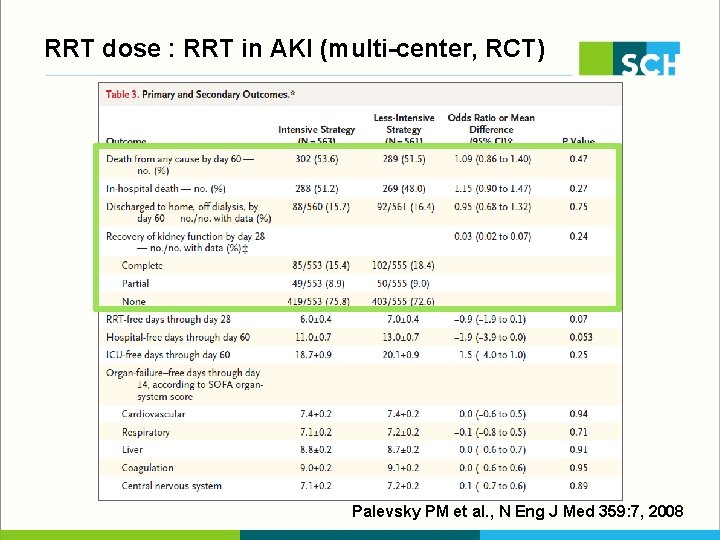
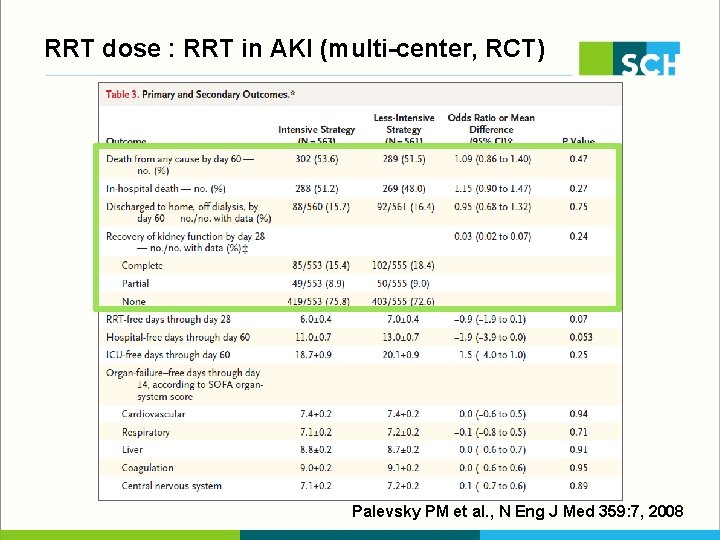
RRT dose : RRT in AKI (multi-center, RCT) Palevsky PM et al. , N Eng J Med 359: 7, 2008
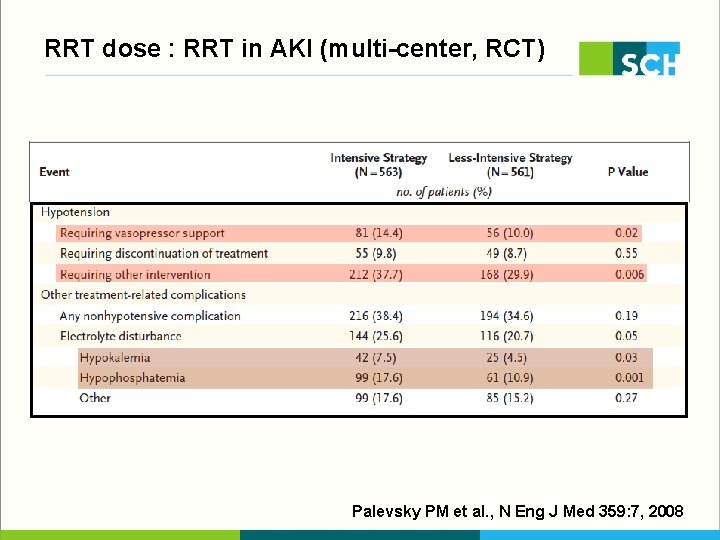
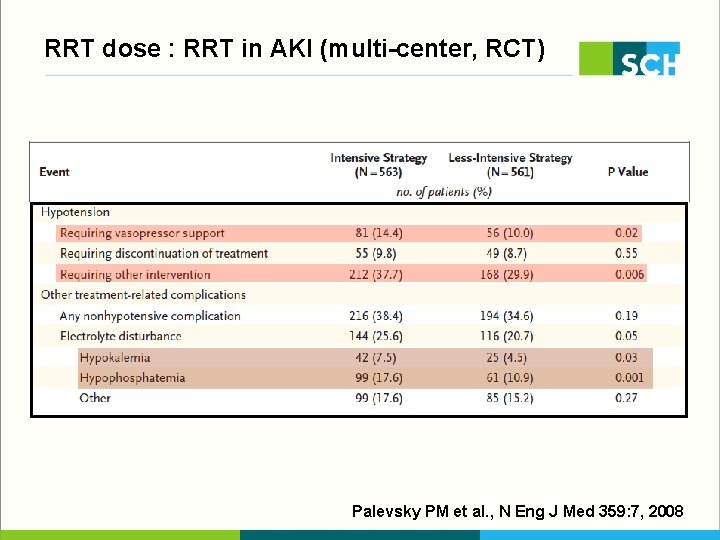
RRT dose : RRT in AKI (multi-center, RCT) Palevsky PM et al. , N Eng J Med 359: 7, 2008
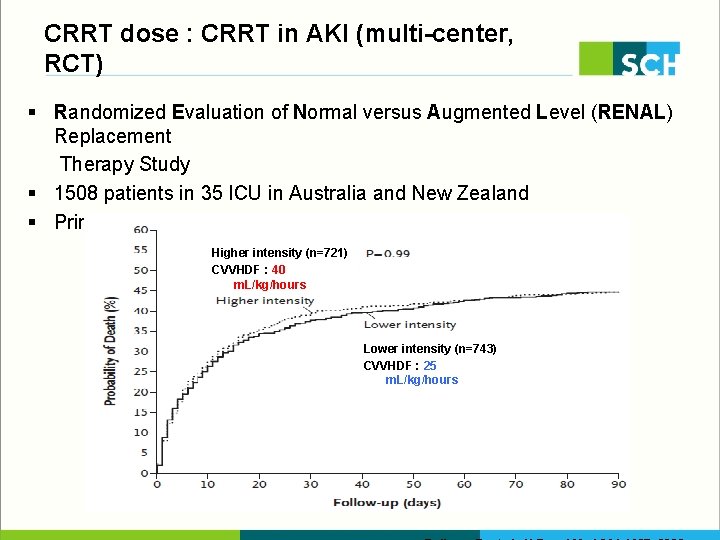
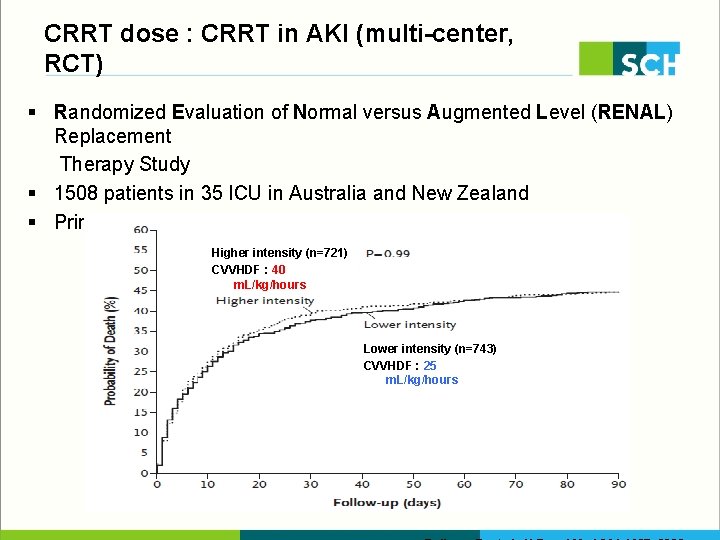
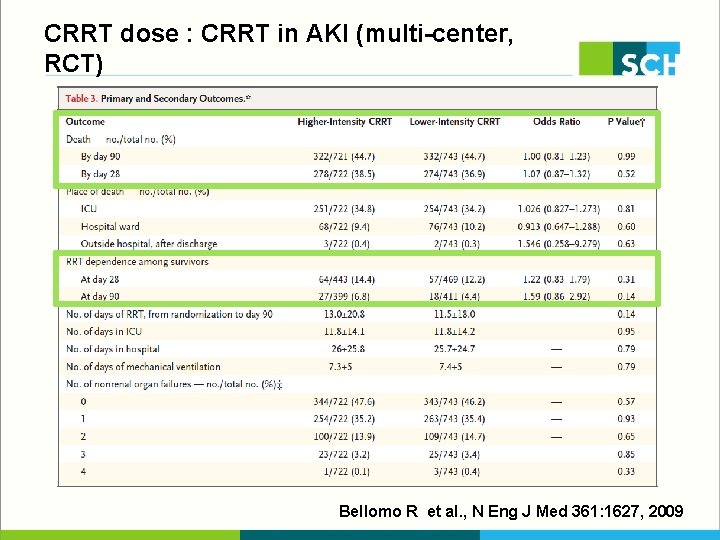
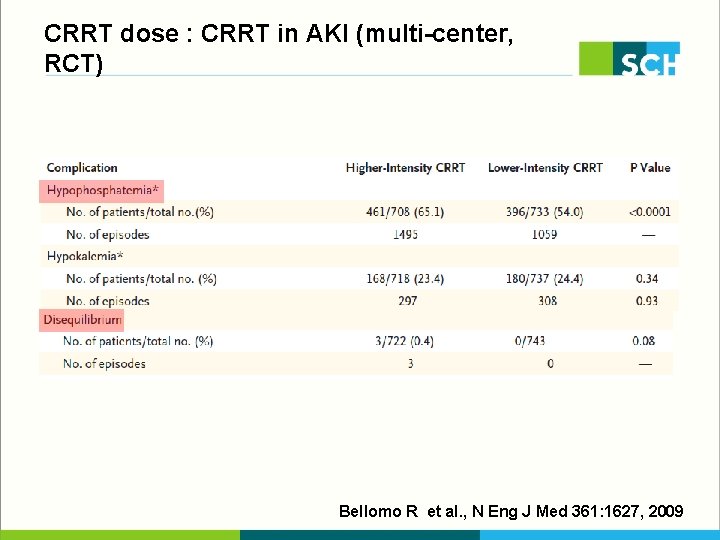
CRRT dose : CRRT in AKI (multi-center, RCT) § Randomized Evaluation of Normal versus Augmented Level (RENAL) Replacement Therapy Study § 1508 patients in 35 ICU in Australia and New Zealand § Primary end point : death within 90 days after randomization Higher intensity (n=721) CVVHDF : 40 m. L/kg/hours Lower intensity (n=743) CVVHDF : 25 m. L/kg/hours
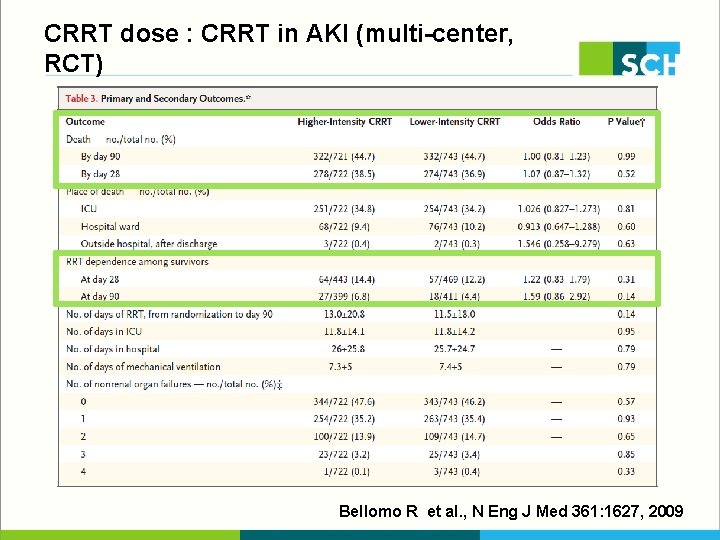
CRRT dose : CRRT in AKI (multi-center, RCT) Bellomo R et al. , N Eng J Med 361: 1627, 2009
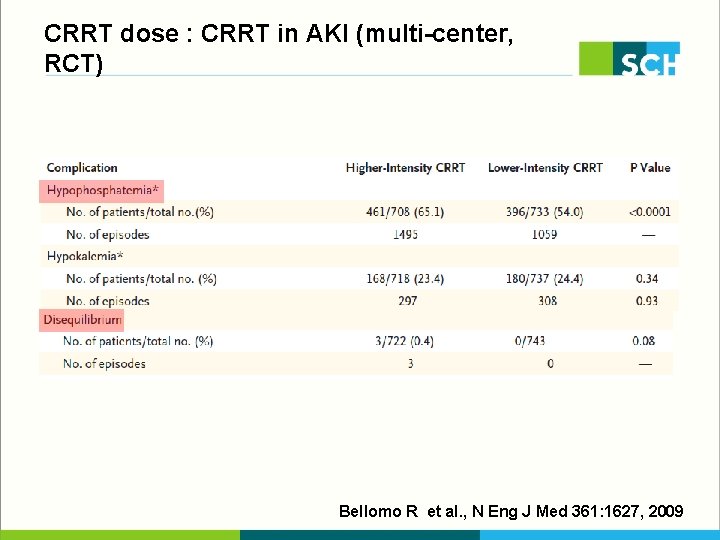
CRRT dose : CRRT in AKI (multi-center, RCT) Bellomo R et al. , N Eng J Med 361: 1627, 2009
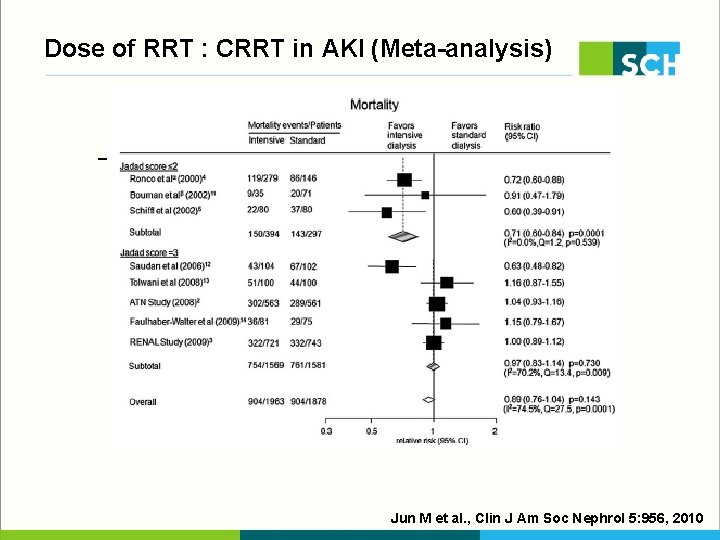
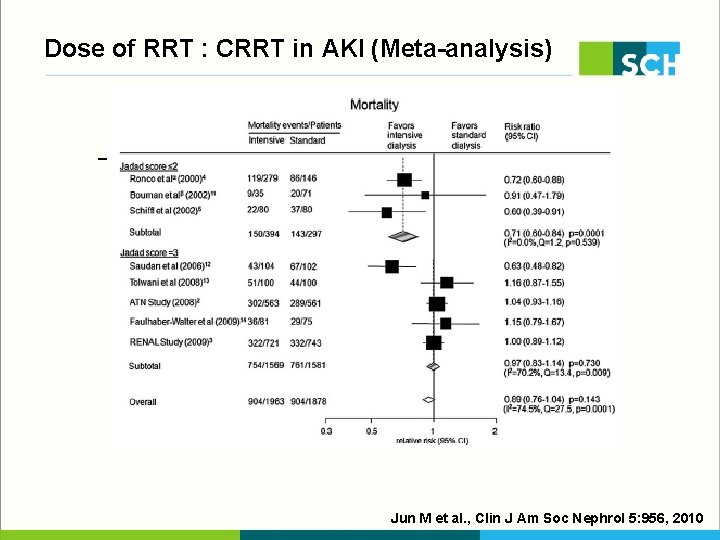
Dose of RRT : CRRT in AKI (Meta-analysis) Jun M et al. , Clin J Am Soc Nephrol 5: 956, 2010
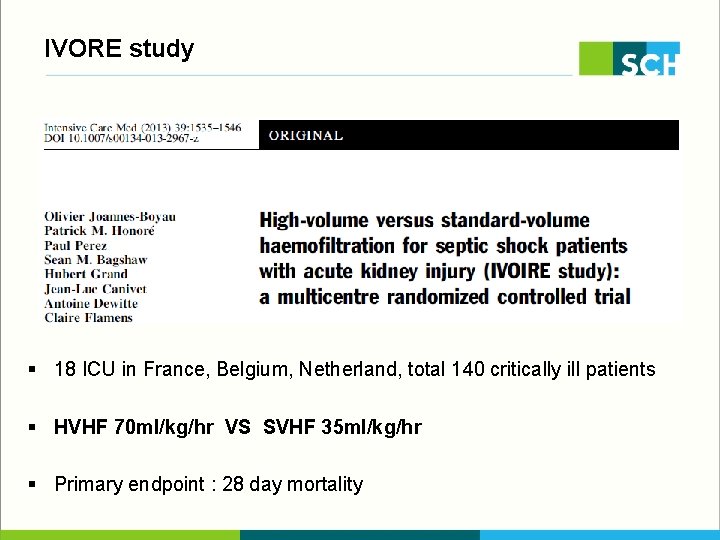
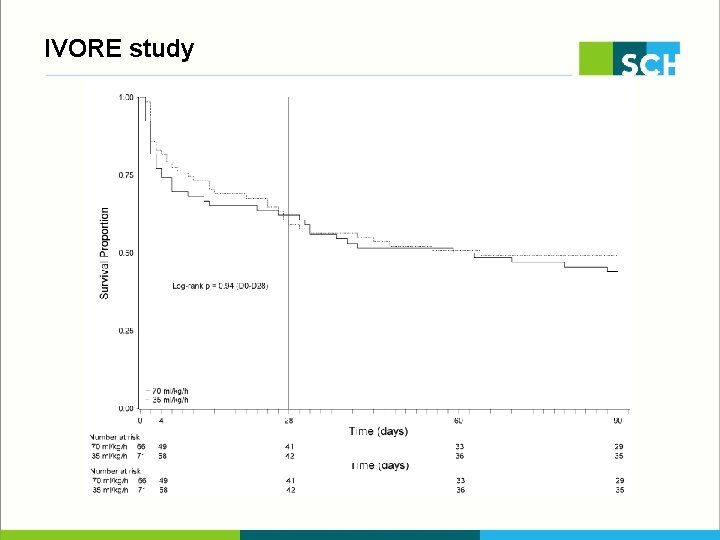
IVORE study § 18 ICU in France, Belgium, Netherland, total 140 critically ill patients § HVHF 70 ml/kg/hr VS SVHF 35 ml/kg/hr § Primary endpoint : 28 day mortality
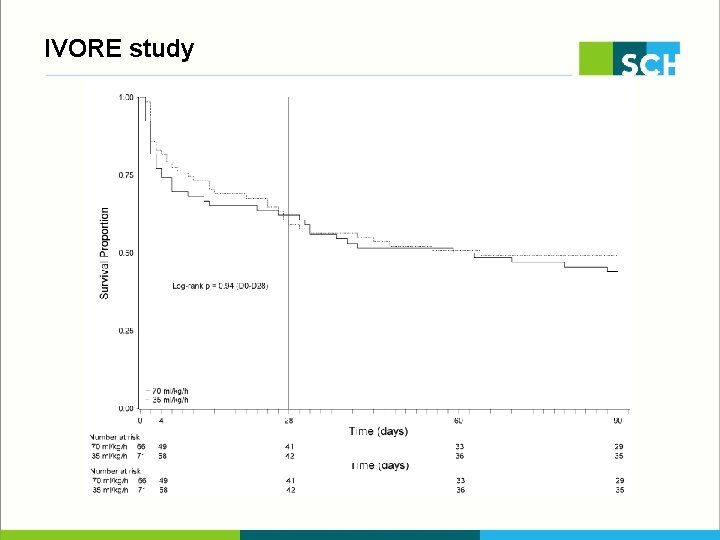
IVORE study
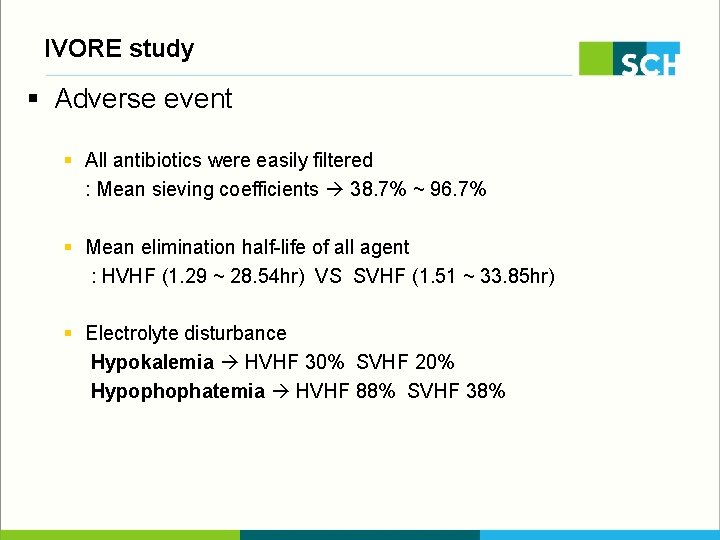
IVORE study § Adverse event § All antibiotics were easily filtered : Mean sieving coefficients 38. 7% ~ 96. 7% § Mean elimination half-life of all agent : HVHF (1. 29 ~ 28. 54 hr) VS SVHF (1. 51 ~ 33. 85 hr) § Electrolyte disturbance Hypokalemia HVHF 30% SVHF 20% Hypophophatemia HVHF 88% SVHF 38%
CRRT dose § Debate of high dose CRRT § Hypophosphatemia / hypokalemia § Higher incidence of hypotension § Effect of pharmacodynamics in antibiotics dosing
Dose of CRRT in AKI § No evidence for superiority of higher CRRT dose Dose threshold below which mortality may increase 35 ml/kg/hr is a reasonable target for prescription > 25 ml/kg/hr should be effectively delivered § KDIGO 2012 Delivering an effluent volume of 20 -25 ml/kg/hr for CRRT in AKI (1 A) We recommend frequent assessment of the actual delivered dose in order to adjust the prescription (1 B)
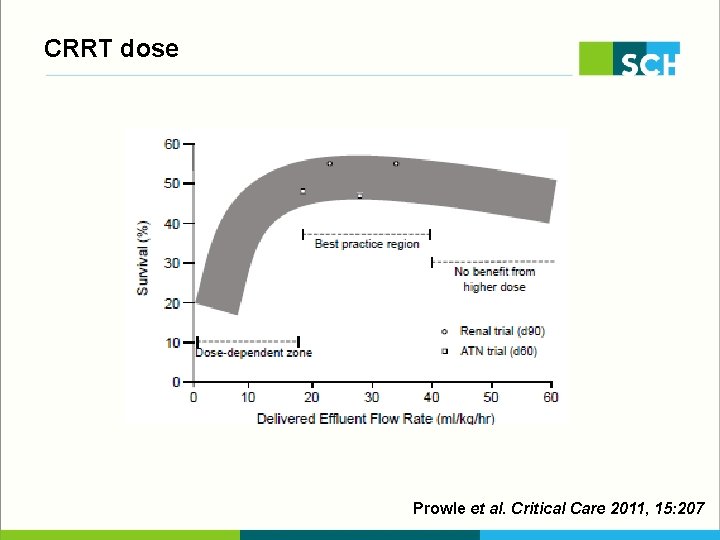
CRRT dose Prowle et al. Critical Care 2011, 15: 207
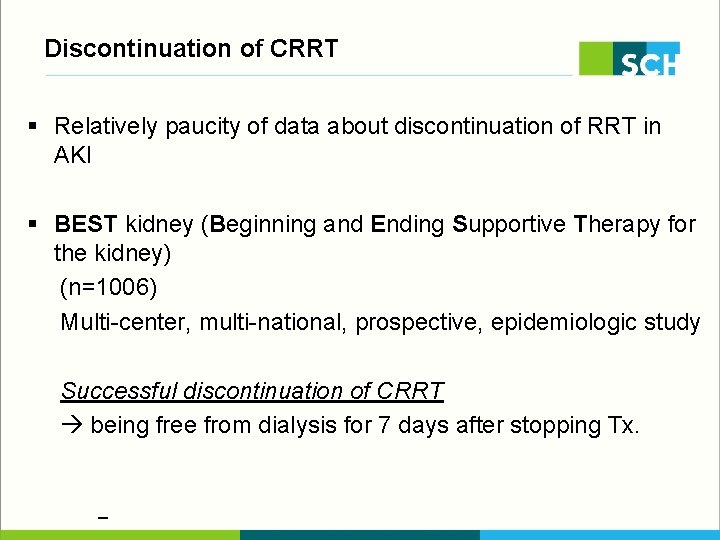
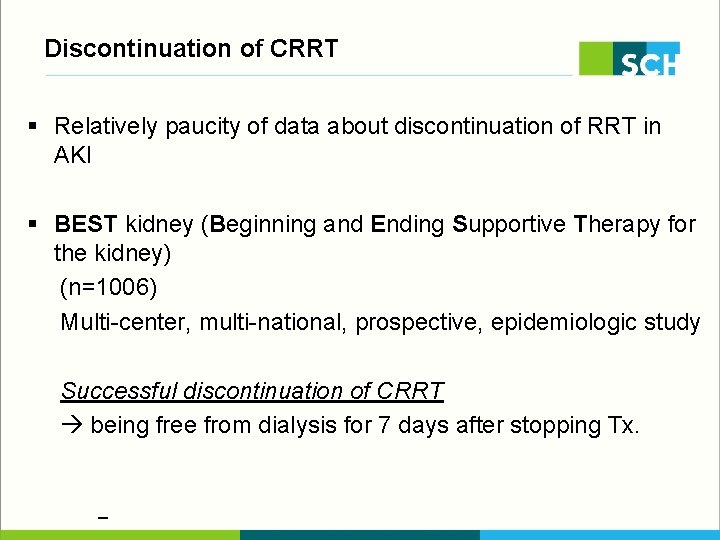
Discontinuation of CRRT § Relatively paucity of data about discontinuation of RRT in AKI § BEST kidney (Beginning and Ending Supportive Therapy for the kidney) (n=1006) Multi-center, multi-national, prospective, epidemiologic study Successful discontinuation of CRRT being free from dialysis for 7 days after stopping Tx.
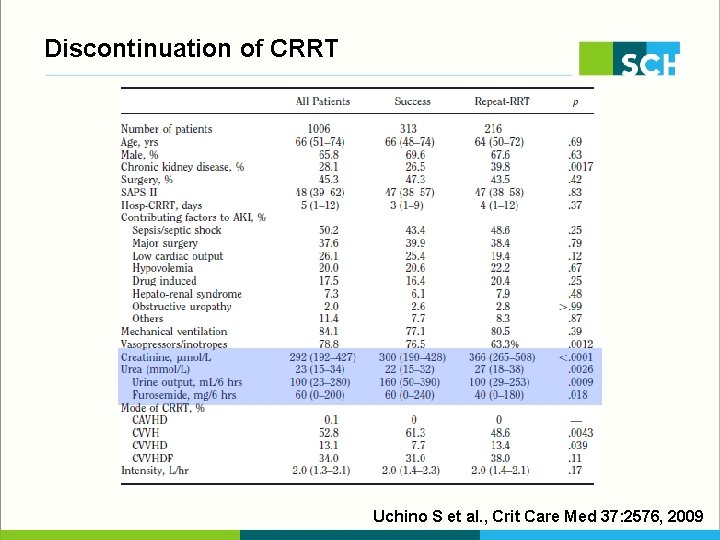
Discontinuation of CRRT Uchino S et al. , Crit Care Med 37: 2576, 2009
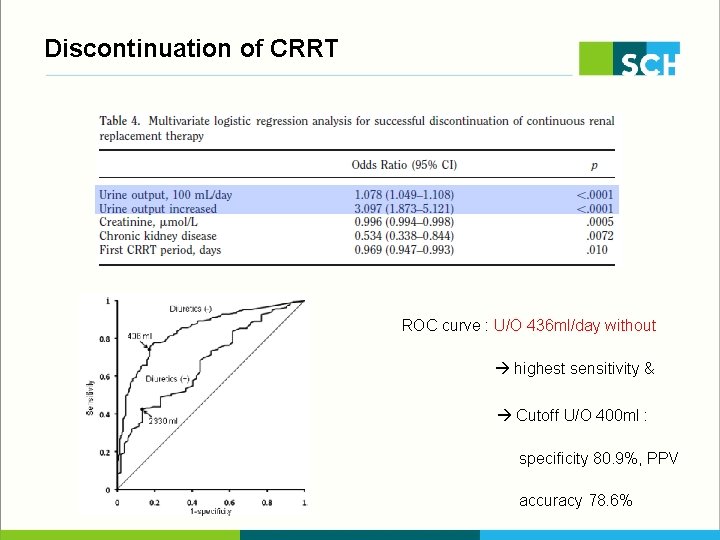
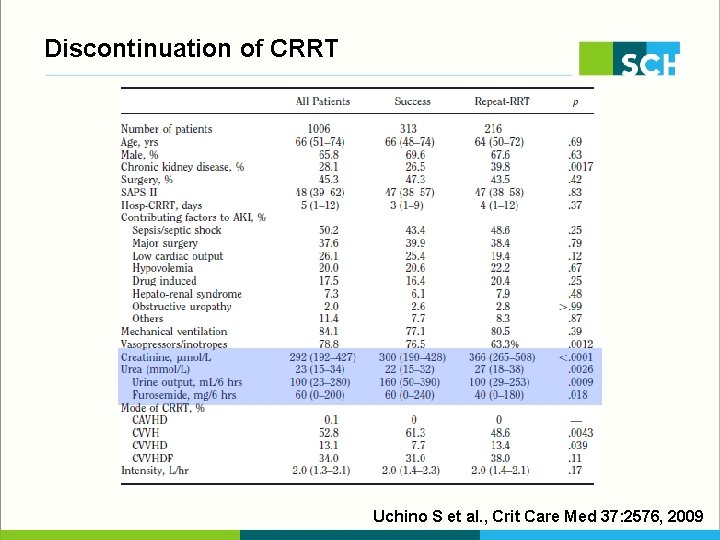
Discontinuation of CRRT ROC curve : U/O 436 ml/day without diuretics highest sensitivity & specificity Cutoff U/O 400 ml : sensitivity 46. 5% specificity 80. 9%, PPV 80. 9%, NPV 76. 5% accuracy 78. 6%
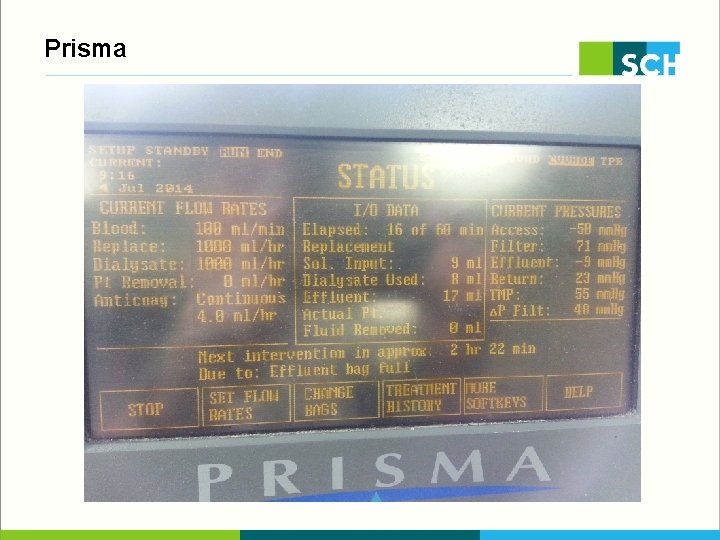
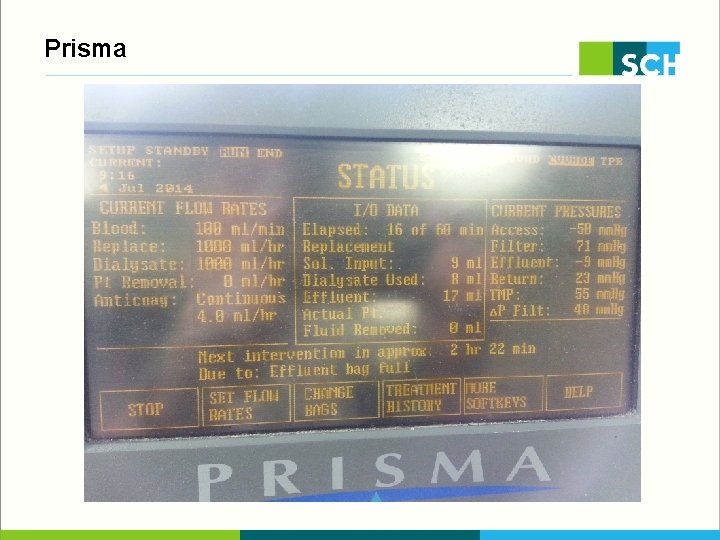
Prisma
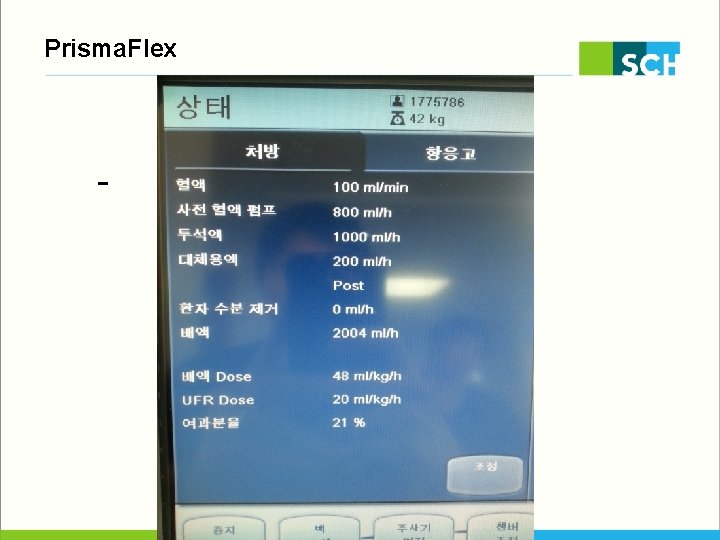
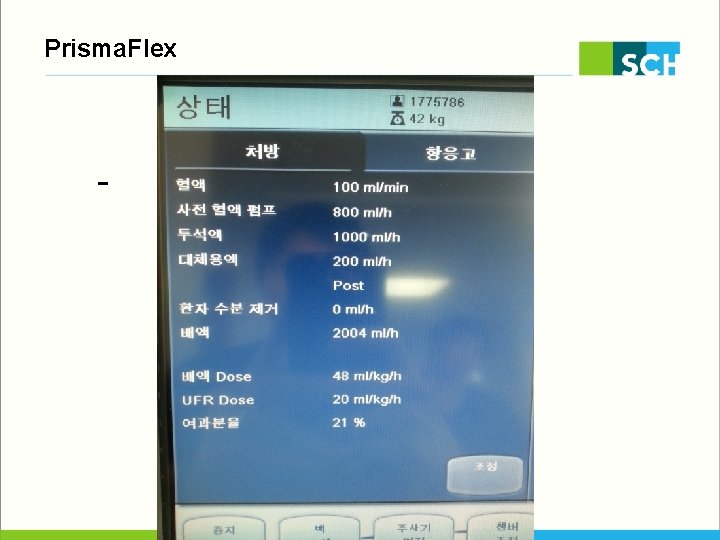
Prisma. Flex
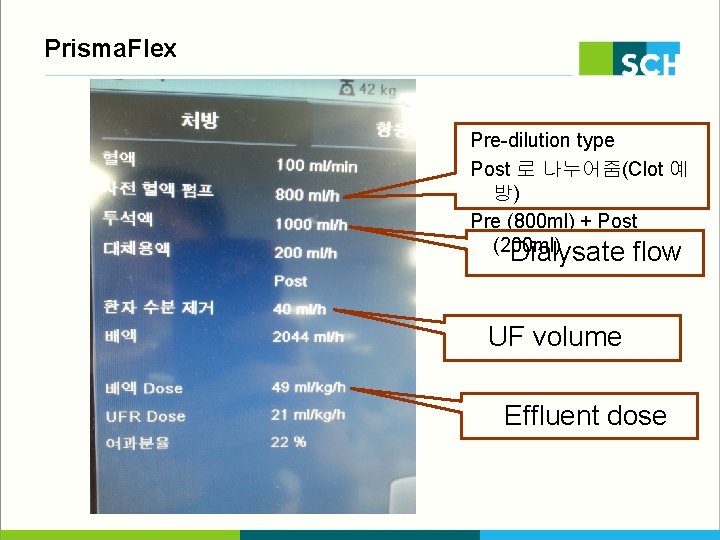
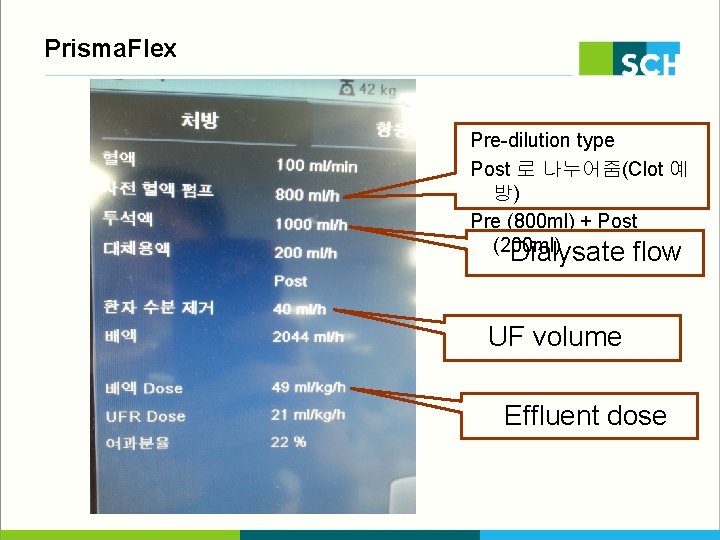
Prisma. Flex Pre-dilution type Post 로 나누어줌(Clot 예 방) Pre (800 ml) + Post (200 ml) Dialysate flow UF volume Effluent dose
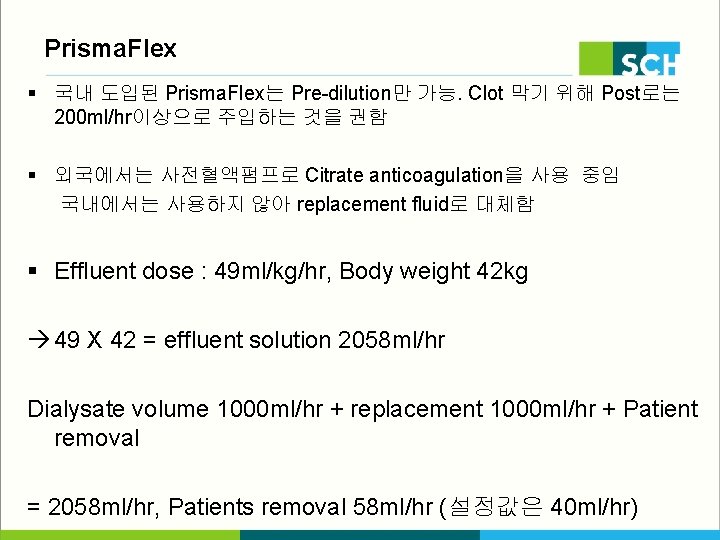
Prisma. Flex § 국내 도입된 Prisma. Flex는 Pre-dilution만 가능. Clot 막기 위해 Post로는 200 ml/hr이상으로 주입하는 것을 권함 § 외국에서는 사전혈액펌프로 Citrate anticoagulation을 사용 중임 국내에서는 사용하지 않아 replacement fluid로 대체함 § Effluent dose : 49 ml/kg/hr, Body weight 42 kg 49 X 42 = effluent solution 2058 ml/hr Dialysate volume 1000 ml/hr + replacement 1000 ml/hr + Patient removal = 2058 ml/hr, Patients removal 58 ml/hr (설정값은 40 ml/hr)
Prisma. Flex § Optimal effluent dose 35 ml/kg/hr 35 X 42 kg = 1470 ml/hr Dialysate : Replacement fluid = 1: 1 로 유지한다면 1470 ml X ½ = 735 ml Dialysate 735 ml, Replacement 735 ml 이렇게 setting 한 후에 UF volume을 정해주면 된다. 현재 본원 setting은 Dialysate 1000 ml/hr, replacement 1000 ml/hr Fix dose로 간호사들이 setting 중임.