Thalassaemia DR MEERA MAHAJAN THALASSAEMIA A group of













- Slides: 68
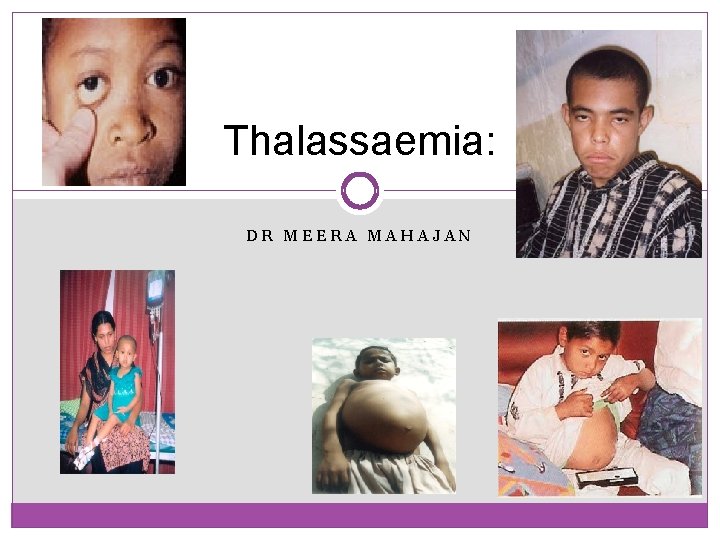
Thalassaemia: DR MEERA MAHAJAN
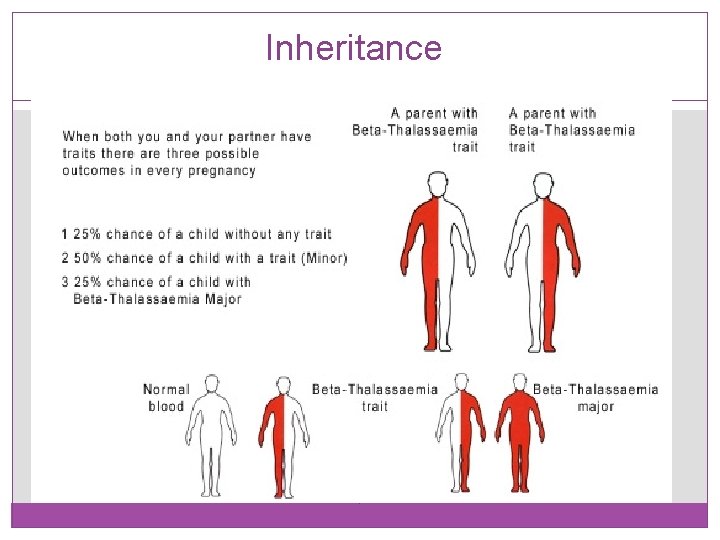
THALASSAEMIA �A group of chronic, inherited anemias characterised by defective Hemoglobin (Hb) synthesis and ineffective erythropoiesis, particularly common in persons of Mediterranean, African and Southeast Asian ancestry. �Thalassaemia results from unbalanced Hb synthesis caused by production of at least one globin polypeptide chain (α, β, γ, δ). There are 2 forms of thalassaemia �Thalassaemia major �Thalassaemia minor (trait)
THALASSAEMIA MAJOR �Thalassaemia major is sometimes known as Cooleys Anaemia, Homozygous, Bete Thalassaemia or Mediterranean Anaemia. Is a serious inherited childhood anaemia. Children with Thalassaemia major cannot make enough haemoglobin. Because of this, their bone marrow cannot produce enough red blood cells. The red blood cells that are produced are nearly empty.
THALASSAEMIA MINOR �People with Thalassaemia Minor, sometimes known as Trait, carry Thalassaemia but they are not ill. They are completely healthy and normal but some of them have slight anaemia. Most people with Thalassaemia Minor do not even know that they have it. It is only discovered if the person has a special blood test or if they have a child with Thalassaemia Major. It is important to know if you have Thalassaemia Minor later in life. The reason for this is that it may cause some problems if the person and their partner wants to start a family. Thalassaemia minors red blood cell are also different from normal blood cells.
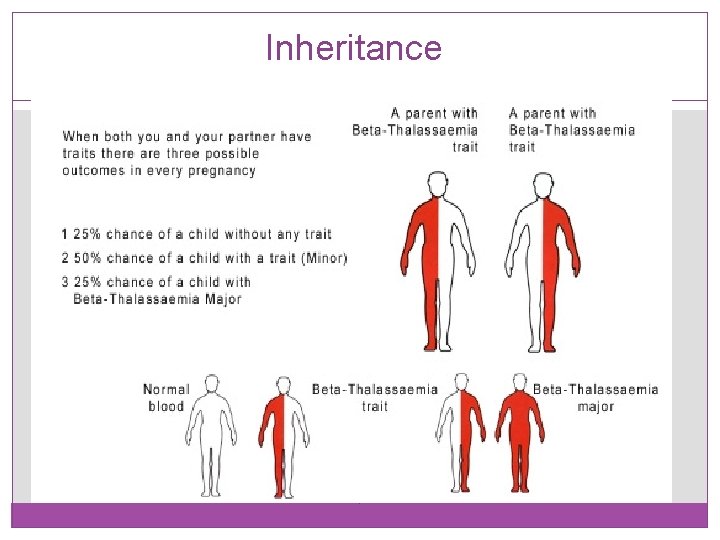
Inheritance


CLINICAL FEATURES MINOR - clinically asymptomatic MAJOR �Severe anemia �Expanded marrow space �Jaundice �Leg ulcers �Cholelithiasis �Splenomegaly �Bone changes and fractures �Growth failure
HAEMOGLOBIN �Hb is most commonly measured to detect anaemia. Low Hb indicates anaemia (various types) and blood loss. �In some relatively rare genetic diseases, the alterations in the structure of the Hb molecule can be detected by electrophoresis.
HAEMOGLOBIN cont… � Hb. A 2 - The haemoglobin is composed of two alpha chains and two delta chains. Hb. A 2 is usually raised in the β thalassaemias, and in unstable haemoglobinopathies where the amino acid substitution is on the β chain. � Hb. F - is the primary hemoglobin produced by the fetus during gestation. The determination of fetal hemoglobin is an aid in evaluating low concentrations of hemoglobin in the blood (anemia). Hb. F may be raised in various haematological conditions among which are thalassemias. � Hb. H inclusions - Performed as part of a haemoglobinopathy/thalassaemia screen. For diagnosis of alpha thalassaemia.
�Hb. A - α 2β 2 �Hb. A 2 - α 2δ 2 �Hb. F – α 2γ 2 Normal Haemoglobin
Beta Thalassemia 12
Classical Syndromes of Beta Thalassemia 13 �Silent carrier state – the mildest form of beta thalassemia. �Beta thalassemia minor - heterozygous disorder resulting in mild hypochromic, microcytic hemolytic anemia. �Beta thalassemia intermedia - Severity lies between the minor and major. �Beta thalassemia major - homozygous disorder resulting in severe transfusion-dependent hemolytic anemia.

Silent Carrier State for β Thalassemia 14 �Are various heterogenous beta mutations that produce only small decrease in production of beta chains. �Patients have nearly normal beta/alpha chain ratio and no hematologic abnormalities. �Have normal levels of Hb A 2.
Beta Thalassemia Minor 1 of 2 15 �Caused by heterogenous mutations that affect beta globin synthesis. �Usually presents as mild, asymptomatic hemolytic anemia unless patient in under stress such as pregnancy, infection, or folic acid deficiency. �Have one normal beta gene and one mutated beta gene. �Hemoglobin level in 10 -13 g/d. L range with normal or slightly elevated RBC count.
Beta Thalassemia Minor 2 of 2 16 �Anemia usually hypochromic and microcytic with slight aniso and poik, including target cells and elliptocytes; May see basophilic stippling. �Rarely see hepatomegaly or splenomegaly. �Have high Hb A 2 levels (3. 5 -8. 0%) and normal to slightly elevated Hb F levels. �Are different variations of this form depending upon which gene has mutated. �Normally require no treatment. �Make sure are not diagnosed with iron deficiency anemia.

Beta Thalassemia Intermedia 1 of 2 17 �Patients able to maintain minimum hemoglobin (7 g/d. L or greater) without transfusions. �Expression of disorder falls between thalassemia minor and thalassemia major. May be either heterozygous for mutations causing mild decrease in beta chain production, or may be homozygous causing a more serious reduction in beta chain production. �See increase in both Hb A 2 production and Hb F production. �Peripheral blood smear picture similar to thalassemia minor.
Beta Thalassemia Intermedia 2 of 2 18 �Have varying symptoms of anemia, jaundice, splenomegaly and hepatomegaly. �Have significant increase in bilirubin levels. �Anemia usually becomes worse with infections, pregnancy, or folic acid deficiencies. �May become transfusion dependent as adults. �Tend to develop iron overloads as result of increased gastrointestinal absorption. �Usually survive into adulthood.
Beta Thalassemia Major 1 of 3 19 �Characterized by severe microcytic, hypochromic anemia. �Detected early in childhood: Infants fail to thrive. Have pallor, variable degree of jaundice, abdominal enlargement, and hepatosplenomegaly. �Hemoglobin level between 4 and 8 gm/d. L. �Severe anemia causes marked bone changes due to expansion of marrow space for increased erythropoiesis. �See characteristic changes in skull, long bones, and hand bones.
Beta Thalassemia Major 2 of 3 20 �Have protrusion upper teeth and Mongoloid facial features. �Physical growth and development delayed. �Peripheral blood shows markedly hypochromic, microcytic erythrocytes with extreme poikilocytosis, such as target cells, teardrop cells and elliptocytes. See marked basophilic stippling and numerous NRBCs. �MCV in range of 50 to 60 f. L. �Low retic count seen (2 -8%). �Most of hemoglobin present is Hb F with slight increase in Hb A 2.
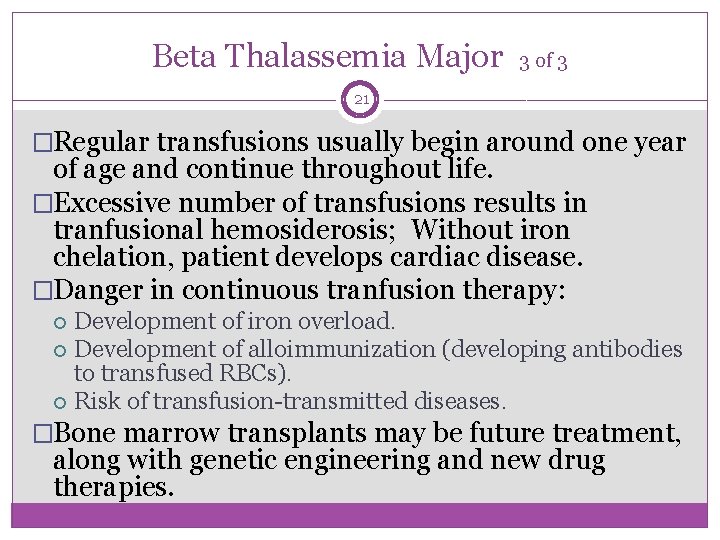
Beta Thalassemia Major 3 of 3 21 �Regular transfusions usually begin around one year of age and continue throughout life. �Excessive number of transfusions results in tranfusional hemosiderosis; Without iron chelation, patient develops cardiac disease. �Danger in continuous tranfusion therapy: Development of iron overload. Development of alloimmunization (developing antibodies to transfused RBCs). Risk of transfusion-transmitted diseases. �Bone marrow transplants may be future treatment, along with genetic engineering and new drug therapies.
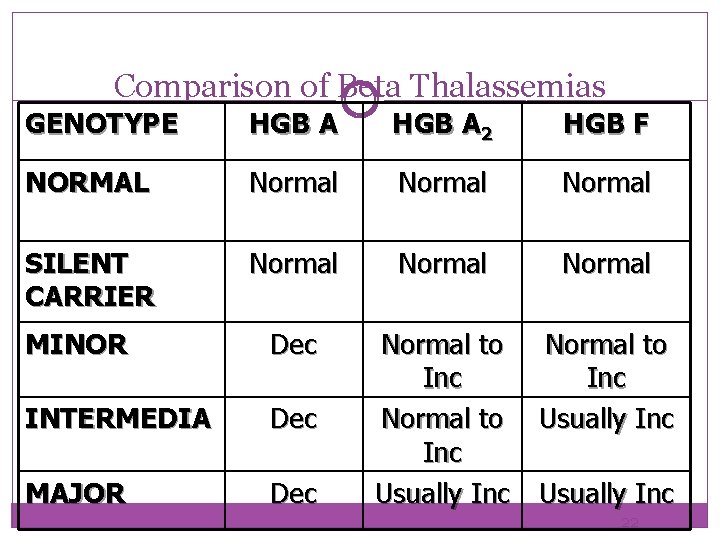
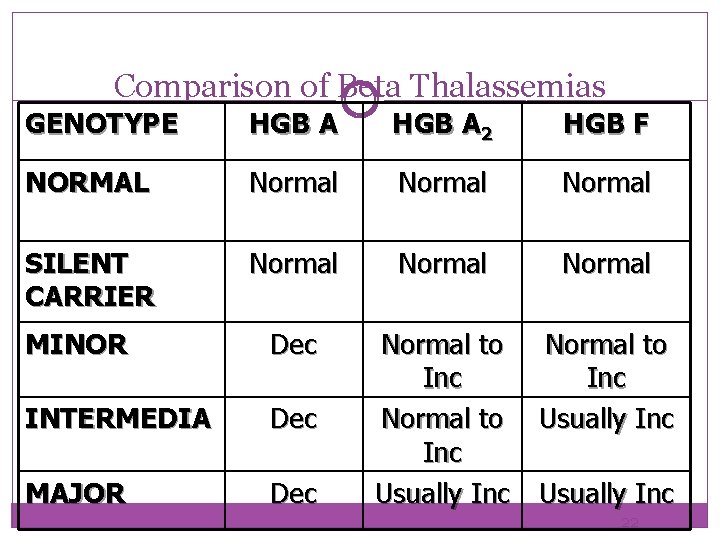
Comparison of Beta Thalassemias GENOTYPE HGB A 2 HGB F NORMAL Normal SILENT CARRIER Normal MINOR Dec INTERMEDIA Dec MAJOR Dec Normal to Inc Normal to Usually Inc 22
Other Thalassemias Caused by Defects in the Beta-Cluster Genes 23 � 1. Delta Beta Thalassemia � 2. Hemoglobin Lepore � 3. Hereditary Persistence of Fetal Hemoglobin (HPFH)
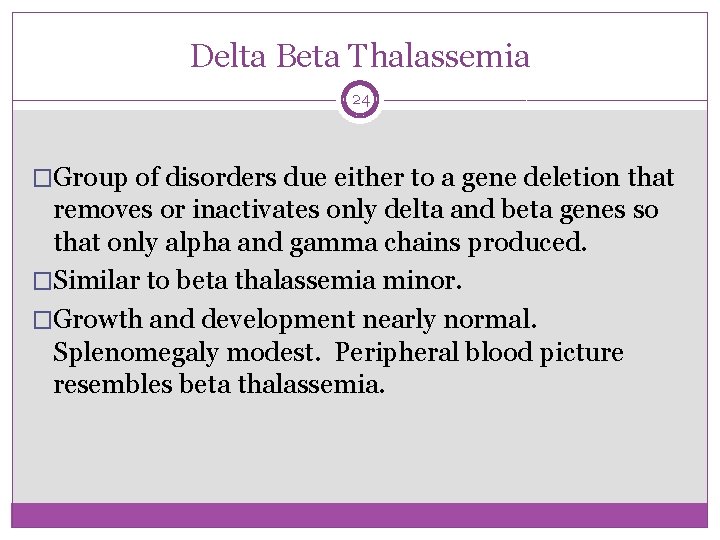
Delta Beta Thalassemia 24 �Group of disorders due either to a gene deletion that removes or inactivates only delta and beta genes so that only alpha and gamma chains produced. �Similar to beta thalassemia minor. �Growth and development nearly normal. Splenomegaly modest. Peripheral blood picture resembles beta thalassemia.
Hemoglobin Lepore 25 �Rare class of delta beta thalassemia. �Caused by gene crossovers between delta locus on one chromosome and beta locus on second chromosome.

Hereditary Persistence of Fetal Hemoglobin (HPFH) 1 of 2 26 �Rare condition characterized by continued synthesis of Hemoglobin F in adult life. �Do not have usual clinical symptoms of thalassemia. �Little significance except when combined with other forms of thalassemia or hemoglobinopathies. �If combined with sickle cell anemia, produces milder form of disease due to presence of Hb F.
Hereditary Persistence of Fetal Hemoglobin (HPFH) 2 of 2 27 �Hb F more resistant to denaturation than Hb A. Can be demonstrated on blood smears using Kleihauer Betke stain. Cells containing Hb F stain. �Classified into two groups according to distribution of Hb F among red cells: Pancellular HPFH - Hemoglobin F uniformly distributed throughout red cells. Heterocellular HPFH - Hemoglobin F found in only small number of cells.

Beta Thalassemia with Hbg S 28 �Inherit gene for Hb S from one parent and gene for Hb A with beta thalassemia from second parent. �Great variety in clinical severity. Usually depend upon severity of thalassemia inherited. Production of Hb A ranges from none produced to varying amounts. If no Hb A produced, see true sickle cell symptoms. If some Hb A produced, have lessening of sickle cell anemia symptoms.
Beta Thalassemia with Hgb C 29 �Shows great variability in clinical and hematologic symptoms. �Symptoms directly related to which type thalassemia inherited. �Usually asymptomatic anemia
Beta Thalassemia with Hgb E 30 �Is unusual because results in more severe disorder than homozygous E disease. �Very severe anemia developing in childhood. �Transfusion therapy required.
Alpha Thalassemia 31
Alpha Thalassemia 1 of 2 32 �Has wide range clinical expressions. �Is difficult to classify alpha thalassemias due to wide variety of possible genetic combinations. �Absence of alpha chains will result in increase of gamma chains during fetal life and excess beta chains later in life; Causes molecules like Bart's Hemoglobin (γ 4) or Hemoglobin H (β 4), which are stable molecules but physiologically useless.
Alpha Thalassemia 2 of 2 33 �Predominant cause of alpha thalassemias is large number of gene deletions in the alpha-globin gene. �Are four clinical syndromes present in alpha thalassemia: Silent Carrier State Alpha Thalassemia Trait (Alpha Thalassemia Minor) Hemoglobin H Disease Bart's Hydrops Fetalis Syndrome
Silent Carrier State 34 �Deletion of one alpha gene, leaving three functional alpha genes. �Alpha/Beta chain ratio nearly normal. �No hematologic abnormalities present. �No reliable way to diagnose silent carriers by hematologic methods; Must be done by genetic mapping. �May see borderline low MCV (78 -80 f. L).
Alpha Thalassemia Trait (Alpha Thalassemia Minor) 35 �Also called Alpha Thalassemia Minor. �Caused by two missing alpha genes. May be homozygous (-a/-a) or heterozygous (--/aa). �Exhibits mild microcytic, hypochromic anemia. �MCV between 70 -75 f. L. �May be confused with iron deficiency anemia. �Although some Bart's hemoglobin (γ 4) present at birth, no Bart's hemoglobin present in adults.
Hemoglobin H Disease 1 of 2 36 �Second most severe form alpha thalassemia. �Usually caused by presence of only one gene producing alpha chains (--/-a). �Results in accumulation of excess unpaired gamma or beta chains. Born with 10 -40% Bart's hemoglobin (γ 4). Gradually replaced with Hemoglobin H (β 4). In adult, have about 30 -50% Hb H. γ 4 β 4
Hemoglobin H Disease 1 of 2 37 �Live normal life; however, infections, pregnancy, exposure to oxidative drugs may trigger hemolytic crisis. �RBCs are microcytic, hypochromic with marked poikilocytosis. Numerous target cells. �Hb H vulnerable to oxidation. Gradually precipitate in vivo to form Heinz-like bodies of denatured hemoglobin. Cells been described has having "golf ball" appearance, especially when stained with brilliant cresyl blue.
Bart’s Hydrops Fetalis Syndrome 38 � Most severe form. Incompatible with life. Have no functioning alpha chain genes (--/--). � Baby born with hydrops fetalis, which is edema and ascites caused by accumulation serous fluid in fetal tissues as result of severe anemia. Also see hepatosplenomegaly and cardiomegaly. � Predominant hemoglobin is Hemoglobin Bart, along with Hemoglobin Portland traces of Hemoglobin H. � Hemoglobin Bart's has high oxygen affinity so cannot carry oxygen to tissues. Fetus dies in utero or shortly after birth. At birth, see severe hypochromic, microcytic anemia with numerous NRBCs. � Pregnancies dangerous to mother. Increased risk of toxemia and severe postpartum hemorrhage.

Comparison of Alpha Thalassemias Genotype Hb A Hb Bart Hb H Normal 97 -98% 0 0 Silent Carrier 96 -98% 0 -2% 0 Alpha Thalassemia Trait 85 -95% 5 -10% 0 Dec 25 -40% 2 -40% 0 80% (with 20% Hgb Portland) 0 -20% Hemoglobin H Disease Hydrops Fetalis 39
Alpha Thalassemia with Hgb S 40 �Alpha thalassemia can occur in combination with hemoglobin S. Is fairly common combination in populations of African descent. �Patient usually asymptomatic. Have less Hb S present than those with sickle cell trait. Have increased presence of Hb F.
Laboratory Diagnosis of Thalassemia 41 �Need to start with patient's individual history and family history. Ethnic background important. �Perform physical examination: Pallor indicating anemia. Jaundice indicating hemolysis. Splenomegaly due to pooling of abnormal cells. Skeletal deformity, especially in beta thalassemia major.

CBC with Differential 1 of 2 43 �See decrease in hemoglobin, hematocrit, mean corpuscular volume (MCV), and mean corpuscular hemoglobin (MCH). See normal to slightly decreased Mean Corpuscular Hemoglobin Concentration (MCHC). Will see microcytic, hypochromic pattern. �Have normal or elevated RBC count with a normal red cell volume distribution (RDW). �Decrease in MCV very noticeable when compared to decrease in Hb and Hct.
CBC with Differential 2 of 2 44 �Elevated RBC count with markedly decreased MCV differentiates thalassemia from iron deficiency anemia. �On differential, see microcytic, hypochromic RBCs (except in carrier states). See mild to moderate poikilocytosis. In more severe cases, see marked number of target cells and elliptocytes. Will see polychromasia, basophilic stippling, and NRBCs.
Causes of Microcytic Anaemia cont… - Non-thalassemic causes of microcytic anaemia include 1) Iron deficiency anaemia 2) Anaemia of chronic disease / inflammation 3) Congenital sideroblastic anaemia
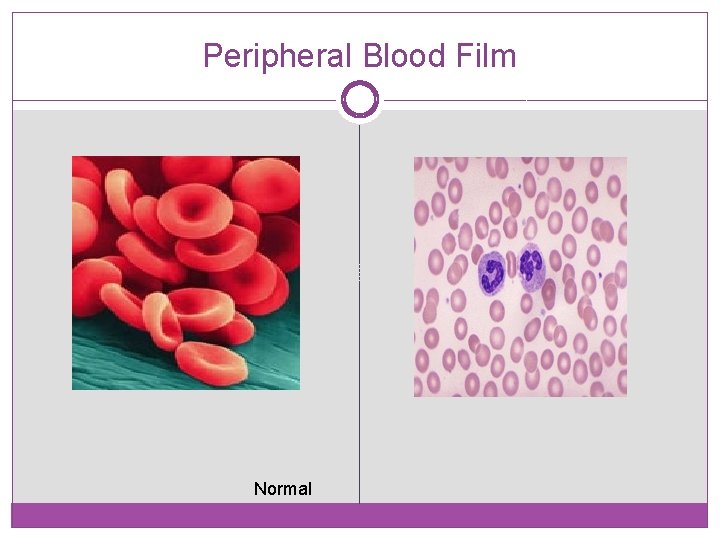
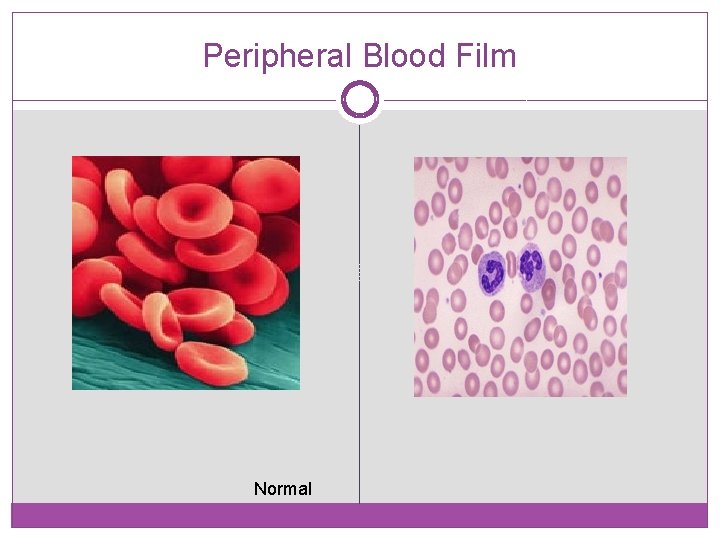
Peripheral Blood Film Normal
Morphology of PBF �RBC Marked anisocytosis, polikilocytosis, microcytosis, frequent target cells, basophilic stippling, fragmented cells or schistocytosis, polychromatic macrocytes and nucleated cells �WBC Whin normal or neutrophilic leucocytosis �Platelets Normal or increased
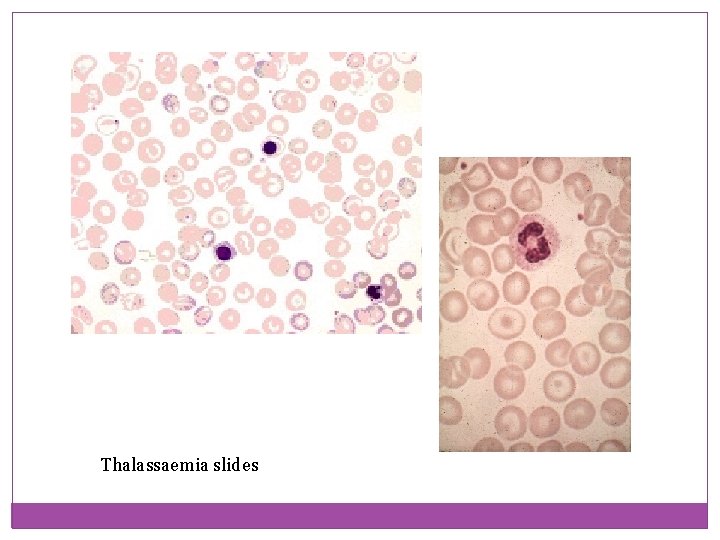
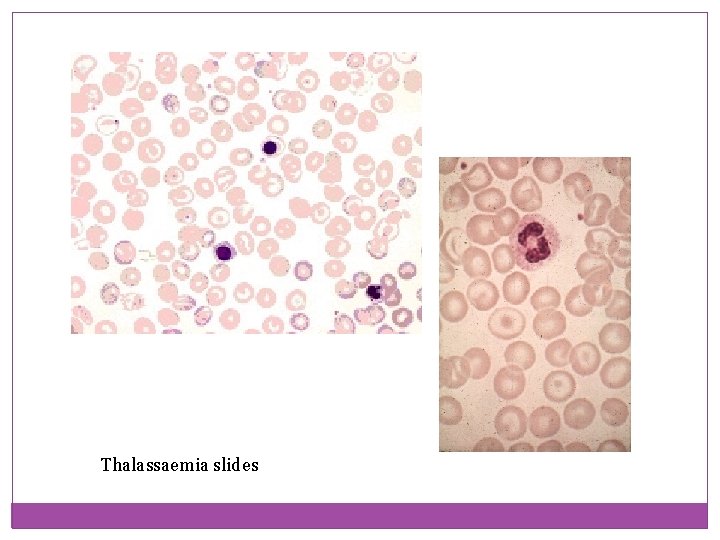
Thalassaemia slides
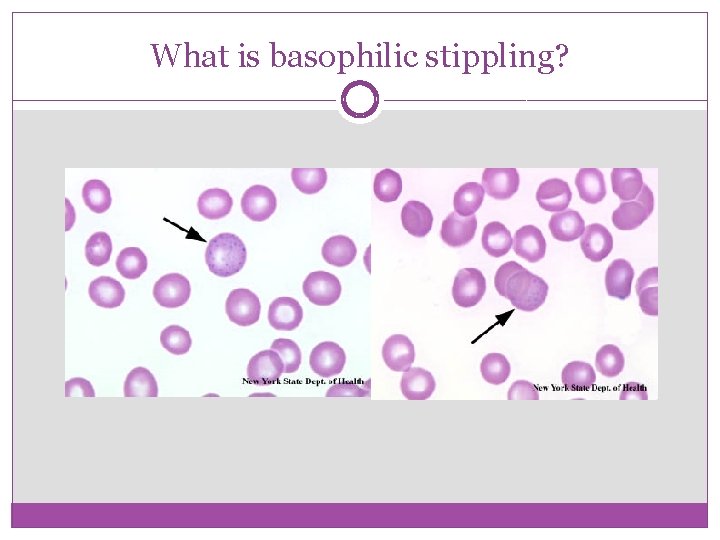
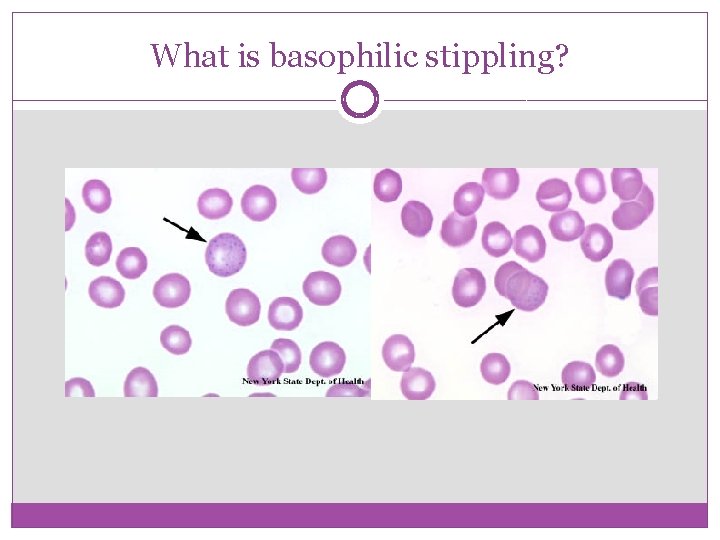
What is basophilic stippling?
HOW DOES IT OCCUR? �Beta thalassemia is caused by mutations in the in haemoglobin beta gene which prevents the production of the beta chains in haemoglobin. �This causes an increased alpha to beta chain ratio and precipitation of alpha ribosomal DNA resulting coarse basophilic stippling. �The stippling effect is aggregations of the ribosomal DNA or protein granulations in the cytoplasm of erythrocytes
IDENTIFICATION �The granulations are usually variable in size and number. An identification technique named the Ramanowsky stain is used to confirm basophilic stippling as it stains the particles a violet blue colour. �The RNA is not blue, it is only the stain required for identification that causes it to appear this way
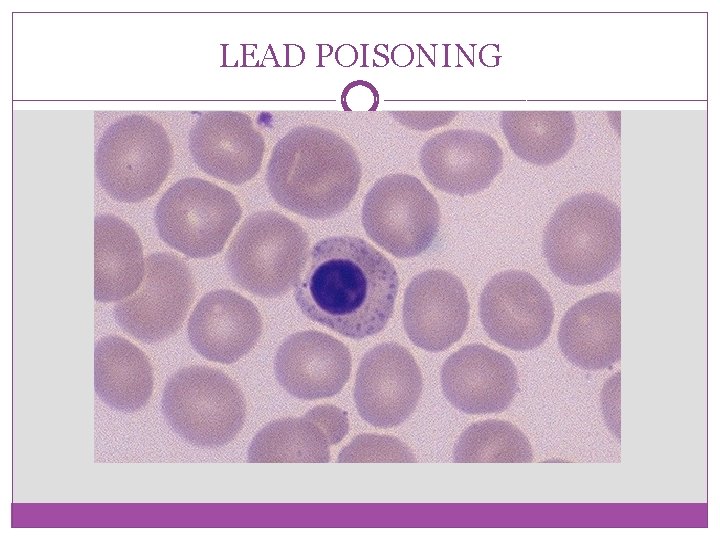
CONDITIONS CAUSING STIPPLING �Coarse stippling is characteristic of lead poisoning and thalassemia. �In thalassemia it is most commonly stippling in the cytoplasm of younger cells. � Lead poisoning often presents as stippling in the cytoplasm of nucleated red blood cells
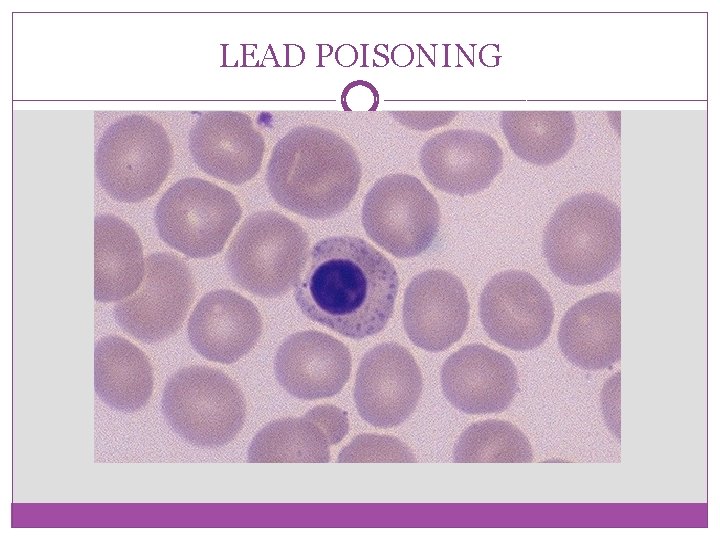
LEAD POISONING

STIPPLING IN THALASSEMIA �Basophilic stippling is not a definitive technique to distinguish between the different forms of thalassemia. It has been found to occur in both beta thalassemia minor and major, although it may be more prevalent in minor.
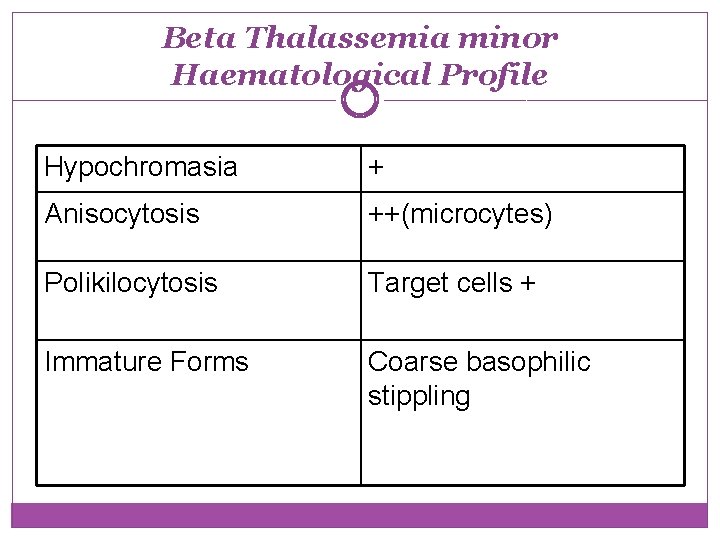
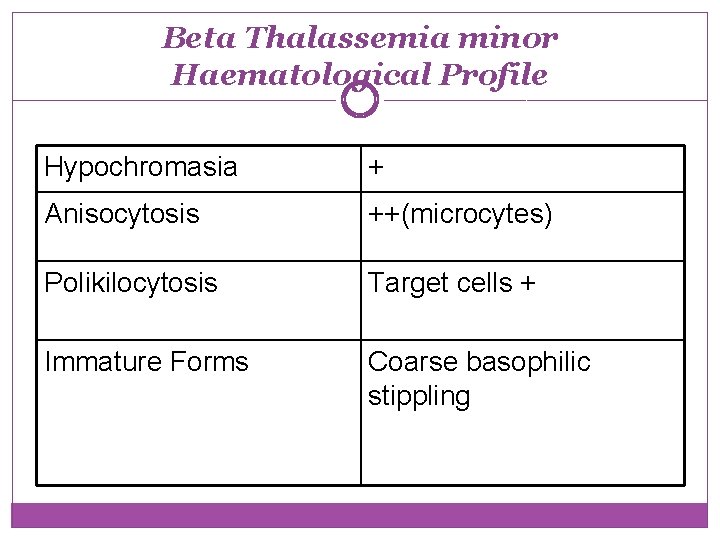
Beta Thalassemia minor Haematological Profile Hypochromasia + Anisocytosis ++(microcytes) Polikilocytosis Target cells + Immature Forms Coarse basophilic stippling
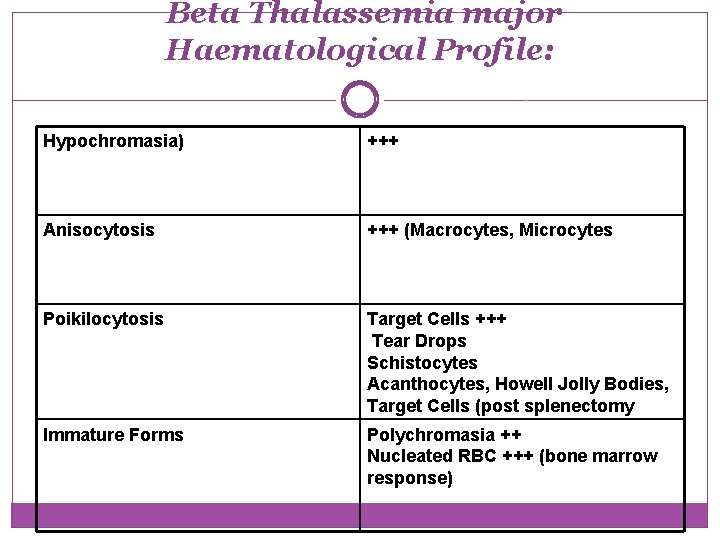
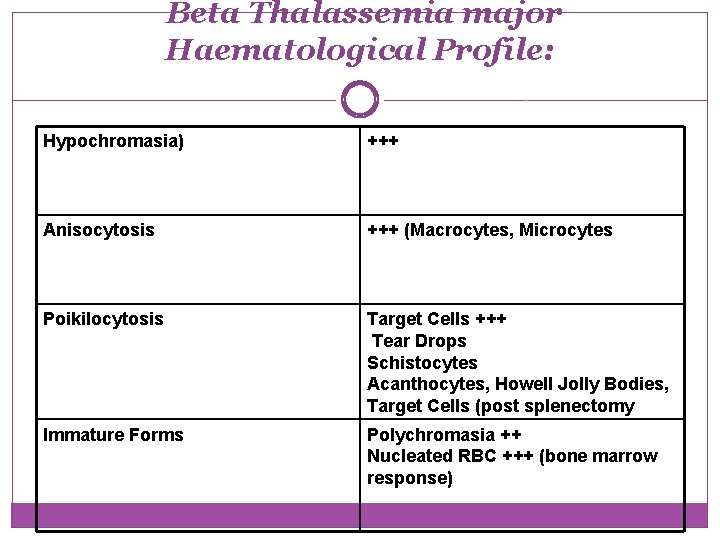
Beta Thalassemia major Haematological Profile: Hypochromasia) +++ Anisocytosis +++ (Macrocytes, Microcytes Poikilocytosis Target Cells +++ Tear Drops Schistocytes Acanthocytes, Howell Jolly Bodies, Target Cells (post splenectomy Immature Forms Polychromasia ++ Nucleated RBC +++ (bone marrow response)
Reticulocyte Count 57 �Usually elevated. Degree of elevation depends upon severity of thalassemia.
Osmotic Fragility 58 �Have decreased osmotic fragility. �Is not very useful fact for diagnosing thalassemia. Is an inexpensive way of screening for carrier states.
Brilliant Cresyl Blue Stain 59 �Incubation with brilliant cresyl blue stain causes Hemoglobin H to precipitate. Results in characteristic appearance of multiple discrete inclusions -golf ball appearance of RBCs. Inclusions smaller than Heinz bodies and are evenly distributed throughout cell.
Acid Elution Stain 60 �Based on Kleihauer-Betke procedure. Acid p. H will dissolve Hemoglobin A from red cells. Hemoglobin F is resistant to denaturation and remains in cell. Stain slide with eosin. Normal adult cells appear as "ghost" cells while cells with Hb F stain varying shades of pink. �Useful way to differentiate between pancellular HPFH and heterocellular HPFH.

Hemoglobin Electrophoresis 61 �Important role in diagnosing and differentiating various forms of thalassemias. �Can differentiate among Hb A, Hb A 2, and Hb F, as well as detect presence of abnormal hemoglobins such as Hemoglobin Lepore, hemoglobin Bart's, or Hemoglobin Constant Spring. �Also aids in detecting combinations of thalassemia and hemoglobinopathies.
Haemoglobin Electrophoresis �Different types of haemoglobins contain different surface charge which determine the elecrtrophoretic mobility and gives a specific bands on the electrophoretic papers when haemolysate is undergone eletrophoresis. �Hb. F, Hb. A 2, Hb. C, Hb. E, Hb. D, Hb. S, Hb. H and Hb Bart can be measured accurately by electrophoresis


Hemoglobin Quantitation 64 �Elevation of Hb A 2 excellent way to detect heterozygote carrier of beta thalassemia. Variations in gene expression in thalassemias results in different amounts of Hb A 2 being produced. �Can also quantitate levels of Hb F.
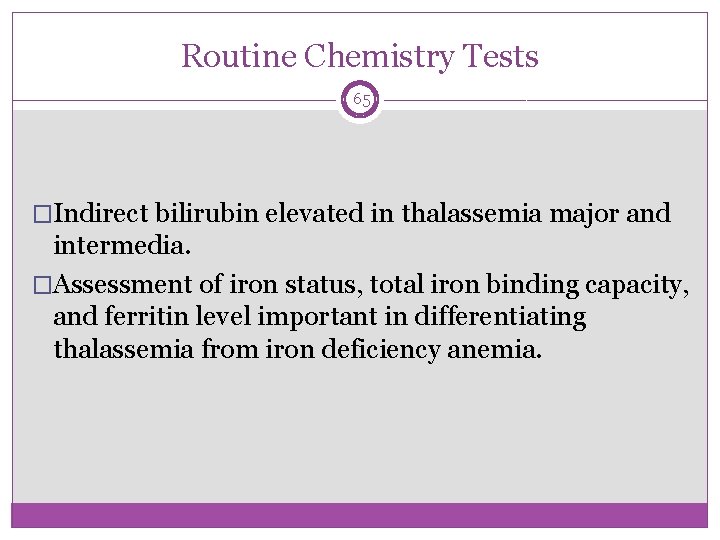
Routine Chemistry Tests 65 �Indirect bilirubin elevated in thalassemia major and intermedia. �Assessment of iron status, total iron binding capacity, and ferritin level important in differentiating thalassemia from iron deficiency anemia.
Other Special Procedures 66 �Globin Chain Testing - determines ratio of globin chains being produced. �DNA Analysis - Determine specific defect at molecular DNA level.
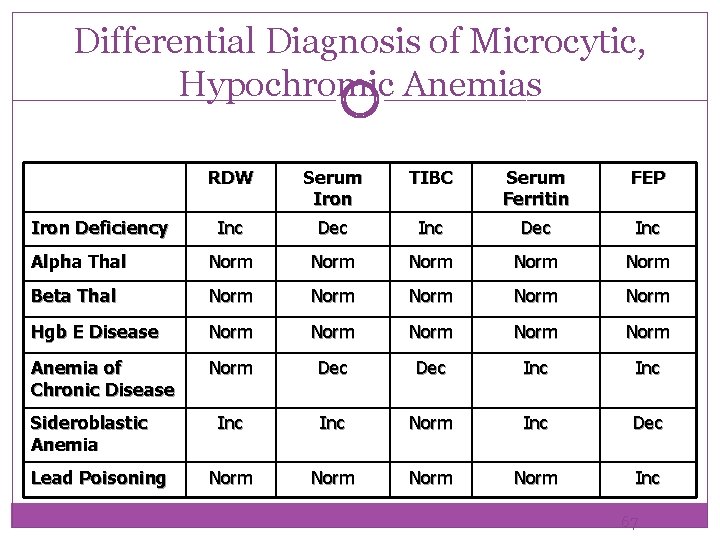
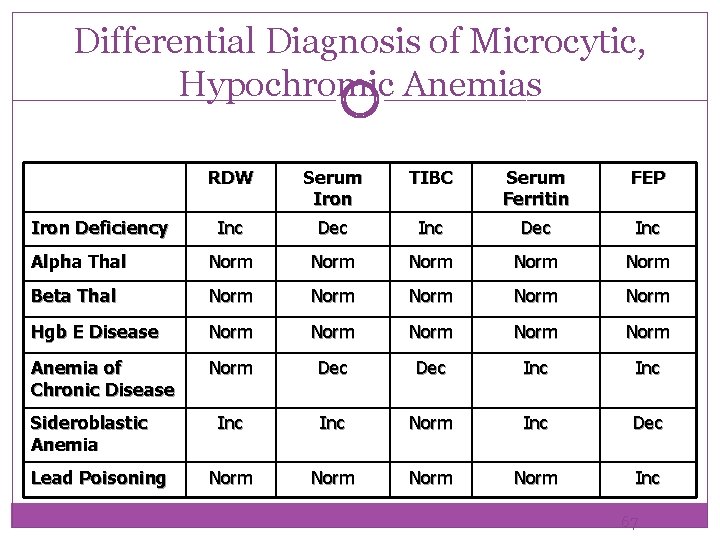
Differential Diagnosis of Microcytic, Hypochromic Anemias RDW Serum Iron TIBC Serum Ferritin FEP Inc Dec Inc Alpha Thal Norm Norm Beta Thal Norm Norm Hgb E Disease Norm Norm Anemia of Chronic Disease Norm Dec Inc Inc Norm Inc Dec Norm Inc Iron Deficiency Sideroblastic Anemia Lead Poisoning 67

 Meera mahajan
Meera mahajan Meera bai poems
Meera bai poems Ratul mahajan
Ratul mahajan Kshiteej mahajan
Kshiteej mahajan Mahajan meaning
Mahajan meaning Ratul mahajan
Ratul mahajan Game loop
Game loop Sunita mahajan
Sunita mahajan Sunita mahajan
Sunita mahajan Mandar mahajan
Mandar mahajan Cedeiser
Cedeiser Dr meera sood
Dr meera sood Meera kaur
Meera kaur Meera warrier
Meera warrier Meera kaur
Meera kaur Meera venkatesh
Meera venkatesh Meera warrier
Meera warrier Meera kaur
Meera kaur Meera gill
Meera gill Cehl:morv::wybf
Cehl:morv::wybf Chargaff rule definition
Chargaff rule definition Sumner's classification of social groups
Sumner's classification of social groups Amino group and carboxyl group
Amino group and carboxyl group Group thinking psychology
Group thinking psychology Group 2 specialties
Group 2 specialties In group out group
In group out group Joining together group theory and group skills
Joining together group theory and group skills Y = a(b)^x
Y = a(b)^x Thermal decomposition of group 1 nitrates
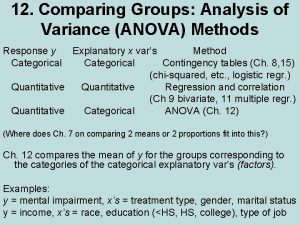
Thermal decomposition of group 1 nitrates Anova within group and between group
Anova within group and between group Group yourselves
Group yourselves Amino group and carboxyl group
Amino group and carboxyl group Voluntary group and involuntary group examples
Voluntary group and involuntary group examples Dylan's mother buys him a sailor's cap
Dylan's mother buys him a sailor's cap Maintenance steering group 3
Maintenance steering group 3 National working group on swiss franc reference rates
National working group on swiss franc reference rates The perceptual tendency to group together stimuli
The perceptual tendency to group together stimuli Power bi user group
Power bi user group The ulysses group
The ulysses group Alkyl group
Alkyl group Bombay phenotype
Bombay phenotype Green world group abu dhabi
Green world group abu dhabi Phenyl structure
Phenyl structure Cahps clinician and group survey
Cahps clinician and group survey What is social interaction
What is social interaction Welcome group
Welcome group Carbon group elements
Carbon group elements Stanford hci group
Stanford hci group Differences between group and team
Differences between group and team Critical thinking in group work
Critical thinking in group work Carbonyl compounds
Carbonyl compounds Tissue is composed of a group of -
Tissue is composed of a group of - Types of group work
Types of group work Ne regional epilepsy group
Ne regional epilepsy group Differences between group and team
Differences between group and team Disjunctive tasks meaning
Disjunctive tasks meaning Diagramming gerund phrases
Diagramming gerund phrases Cochrane musculoskeletal group
Cochrane musculoskeletal group Amino acids groups
Amino acids groups Methyl group ortho para directing
Methyl group ortho para directing Business opportunities in hong kong
Business opportunities in hong kong Alibaba leadership style
Alibaba leadership style Group selection
Group selection 10302020
10302020 International aerospace environmental group
International aerospace environmental group Ir spectrum table
Ir spectrum table Tt power group
Tt power group Humanities group
Humanities group Joseph pratt group therapy
Joseph pratt group therapy