Textural Interface Opacity after Descemet Stripping Automated Endothelial
- Slides: 1
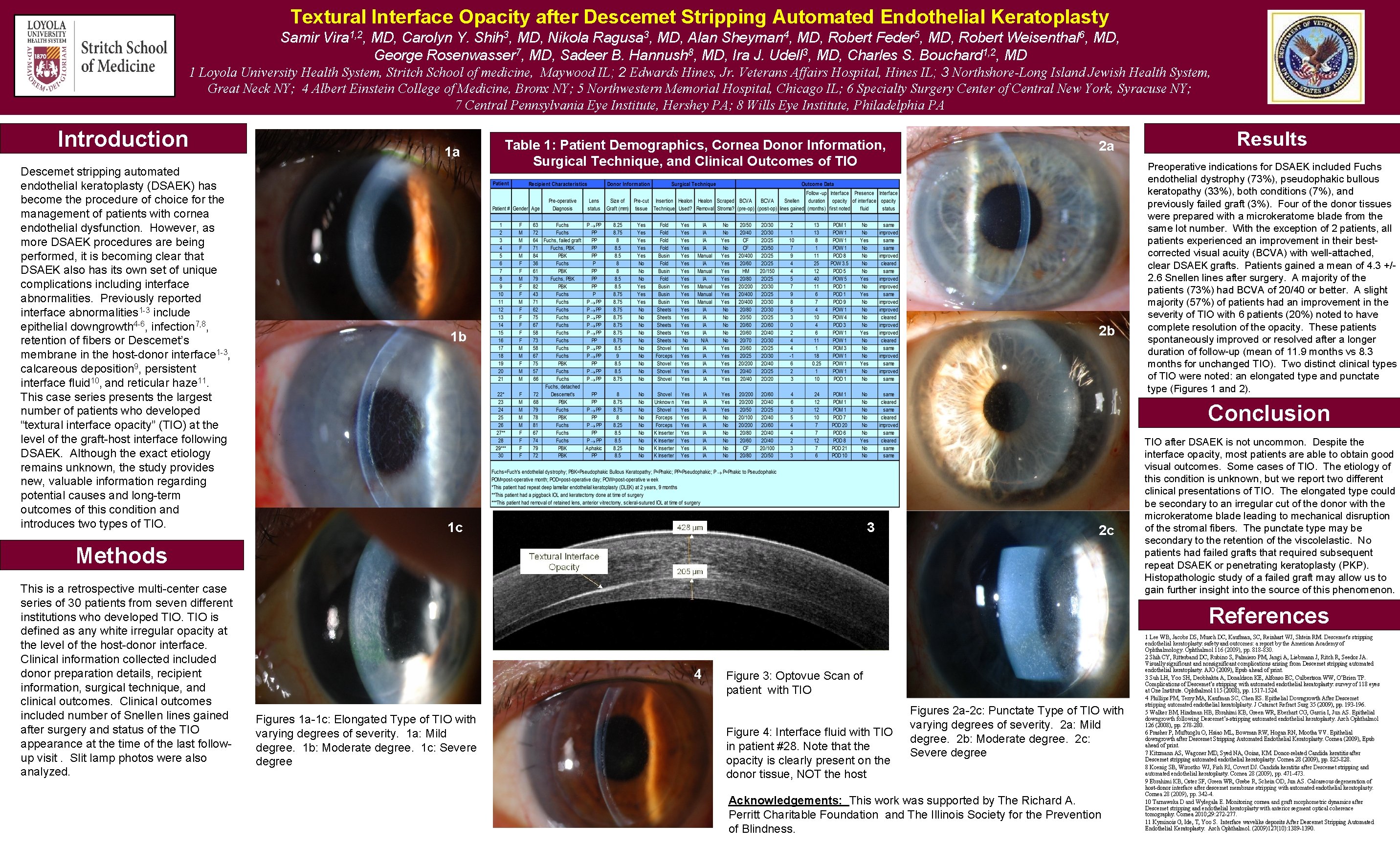
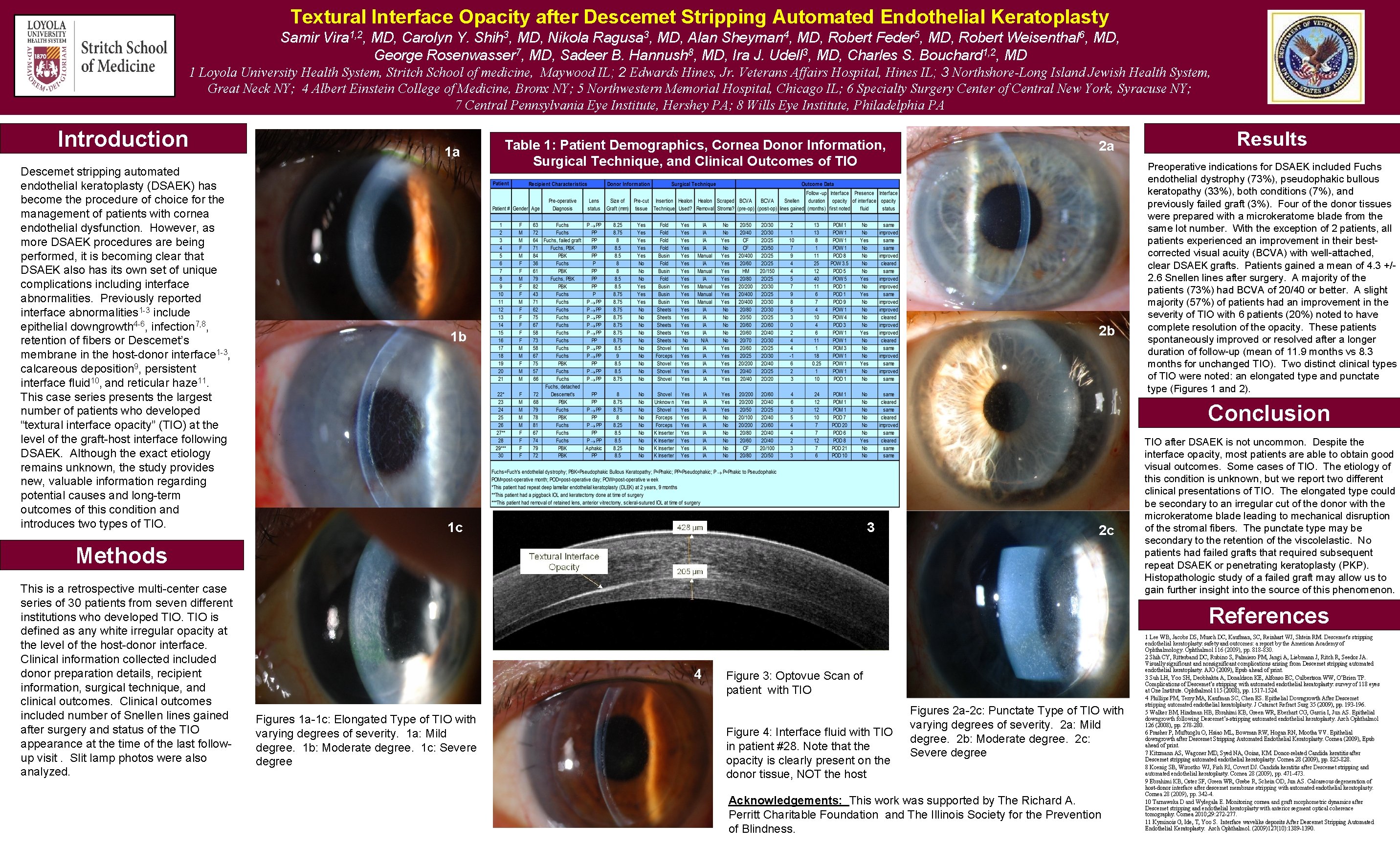
Textural Interface Opacity after Descemet Stripping Automated Endothelial Keratoplasty Samir Vira 1, 2, MD, Carolyn Y. Shih 3, MD, Nikola Ragusa 3, MD, Alan Sheyman 4, MD, Robert Feder 5, MD, Robert Weisenthal 6, MD, George Rosenwasser 7, MD, Sadeer B. Hannush 8, MD, Ira J. Udell 3, MD, Charles S. Bouchard 1, 2, MD 1 Loyola University Health System, Stritch School of medicine, Maywood IL; 2 Edwards Hines, Jr. Veterans Affairs Hospital, Hines IL; 3 Northshore-Long Island Jewish Health System, Great Neck NY; 4 Albert Einstein College of Medicine, Bronx NY; 5 Northwestern Memorial Hospital, Chicago IL; 6 Specialty Surgery Center of Central New York, Syracuse NY; 7 Central Pennsylvania Eye Institute, Hershey PA; 8 Wills Eye Institute, Philadelphia PA Introduction Descemet stripping automated endothelial keratoplasty (DSAEK) has become the procedure of choice for the management of patients with cornea endothelial dysfunction. However, as more DSAEK procedures are being performed, it is becoming clear that DSAEK also has its own set of unique complications including interface abnormalities. Previously reported interface abnormalities 1 -3 include epithelial downgrowth 4 -6, infection 7, 8, retention of fibers or Descemet’s membrane in the host-donor interface 1 -3, calcareous deposition 9, persistent interface fluid 10, and reticular haze 11. This case series presents the largest number of patients who developed “textural interface opacity” (TIO) at the level of the graft-host interface following DSAEK. Although the exact etiology remains unknown, the study provides new, valuable information regarding potential causes and long-term outcomes of this condition and introduces two types of TIO. 1 a Table 1: Patient Demographics, Cornea Donor Information, Surgical Technique, and Clinical Outcomes of TIO 2 a 2 b 1 b Preoperative indications for DSAEK included Fuchs endothelial dystrophy (73%), pseudophakic bullous keratopathy (33%), both conditions (7%), and previously failed graft (3%). Four of the donor tissues were prepared with a microkeratome blade from the same lot number. With the exception of 2 patients, all patients experienced an improvement in their bestcorrected visual acuity (BCVA) with well-attached, clear DSAEK grafts. Patients gained a mean of 4. 3 +/2. 6 Snellen lines after surgery. A majority of the patients (73%) had BCVA of 20/40 or better. A slight majority (57%) of patients had an improvement in the severity of TIO with 6 patients (20%) noted to have complete resolution of the opacity. These patients spontaneously improved or resolved after a longer duration of follow-up (mean of 11. 9 months vs 8. 3 months for unchanged TIO). Two distinct clinical types of TIO were noted: an elongated type and punctate type (Figures 1 and 2). Conclusion 1 c 3 2 c Methods This is a retrospective multi-center case series of 30 patients from seven different institutions who developed TIO is defined as any white irregular opacity at the level of the host-donor interface. Clinical information collected included donor preparation details, recipient information, surgical technique, and clinical outcomes. Clinical outcomes included number of Snellen lines gained after surgery and status of the TIO appearance at the time of the last followup visit. Slit lamp photos were also analyzed. Results TIO after DSAEK is not uncommon. Despite the interface opacity, most patients are able to obtain good visual outcomes. Some cases of TIO. The etiology of this condition is unknown, but we report two different clinical presentations of TIO. The elongated type could be secondary to an irregular cut of the donor with the microkeratome blade leading to mechanical disruption of the stromal fibers. The punctate type may be secondary to the retention of the viscolelastic. No patients had failed grafts that required subsequent repeat DSAEK or penetrating keratoplasty (PKP). Histopathologic study of a failed graft may allow us to gain further insight into the source of this phenomenon. References 4 Figures 1 a-1 c: Elongated Type of TIO with varying degrees of severity. 1 a: Mild degree. 1 b: Moderate degree. 1 c: Severe degree Figure 3: Optovue Scan of patient with TIO Figure 4: Interface fluid with TIO in patient #28. Note that the opacity is clearly present on the donor tissue, NOT the host Figures 2 a-2 c: Punctate Type of TIO with varying degrees of severity. 2 a: Mild degree. 2 b: Moderate degree. 2 c: Severe degree Acknowledgements: This work was supported by The Richard A. Perritt Charitable Foundation and The Illinois Society for the Prevention of Blindness. 1 Lee WB, Jacobs DS, Musch DC, Kaufman, SC, Reinhart WJ, Shtein RM. Descemet's stripping endothelial keratoplasty: safety and outcomes: a report by the American Academy of Ophthalmology. Ophthalmol 116 (2009), pp. 818 -830. 2 Shih CY, Ritterband DC, Rubino S, Palmiero PM, Jangi A, Liebmann J, Ritch R, Seedor JA. Visually significant and nonsignificant complications arising from Descemet stripping automated endothelial keratoplasty. AJO (2009), Epub ahead of print. 3 Suh LH, Yoo SH, Deobhakta A, Donaldson KE, Alfonso EC, Culbertson WW, O’Brien TP. Complications of Descemet’s stripping with automated endothelial keratoplasty: survey of 118 eyes at One Institute. Ophthalmol 115 (2008), pp. 1517 -1524. 4 Phillips PM, Terry MA, Kaufman SC, Chen ES. Epithelial Downgrowth After Descemet stripping automated endothelial keratolplasty. J Cataract Refract Surg 35 (2009), pp. 193 -196. 5 Walker BM, Hindman HB, Ebrahimi KB, Green WR, Eberhart CG, Garcia I, Jun AS. Epithelial downgrowth following Descemet’s-stripping automated endothelial keratoplasty. Arch Ophthalmol 126 (2008), pp. 278 -280. 6 Prasher P, Muftuoglu O, Hsiao ML, Bowman RW, Hogan RN, Mootha VV. Epithelial downgrowth after Descemet Stripping Automated Endothelial Keratoplasty. Cornea (2009), Epub ahead of print. 7 Kitzmann AS, Wagoner MD, Syed NA, Goins, KM. Donor-related Candida keratitis after Descemet stripping automated endothelial keratoplasty. Cornea 28 (2009), pp. 825 -828. 8 Koenig SB, Wirostko WJ, Fish RI, Covert DJ. Candida keratitis after Descemet stripping and automated endothelial keratoplasty. Cornea 28 (2009), pp. 471 -473. 9 Ebrahimi KB, Oster SF, Green WR, Grebe R, Schein OD, Jun AS. Calcareous degeneration of 9 Ebrahimi KB, Oster SF, Green WR, Grebe R, Schein OD, Jun AS. Calcareous degeneration of host-donor interface after descemet membrane stripping with automated endothelial keratoplasty. Cornea 28 (2009), pp. 342 -4. 10 Tarnawska D and Wylegala E. Monitoring cornea and graft morphometric dynamics after Descemet stripping and endothelial keratoplasty with anterior segment optical coherence tomography. Cornea 2010; 29: 272 -277. 11 Kyminois G, Ide, T, Yoo S. Interface wavelike deposits After Descemet Stripping Automated Endothelial Keratoplasty. Arch Ophthalmol. (2009)127(10): 1389 -1390.