Testing for Coronary Artery Disease John L Tan















- Slides: 70
Testing for Coronary Artery Disease John L. Tan, MD, Ph. D North Texas Heart Center Presbyterian Hospital of Dallas
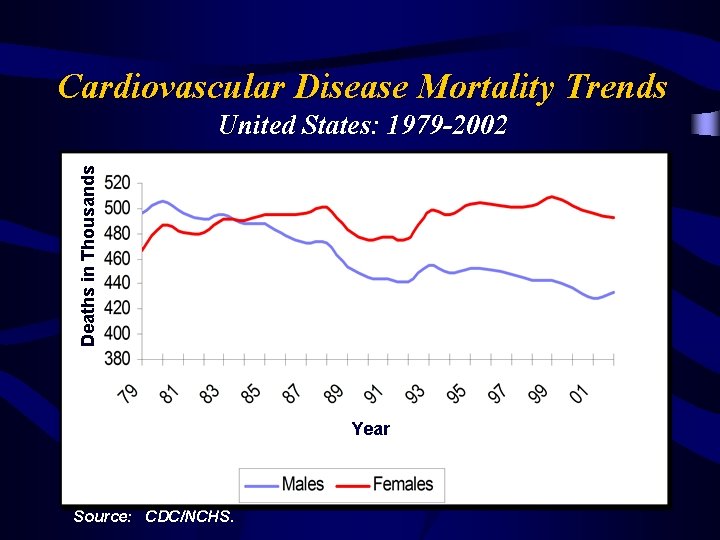
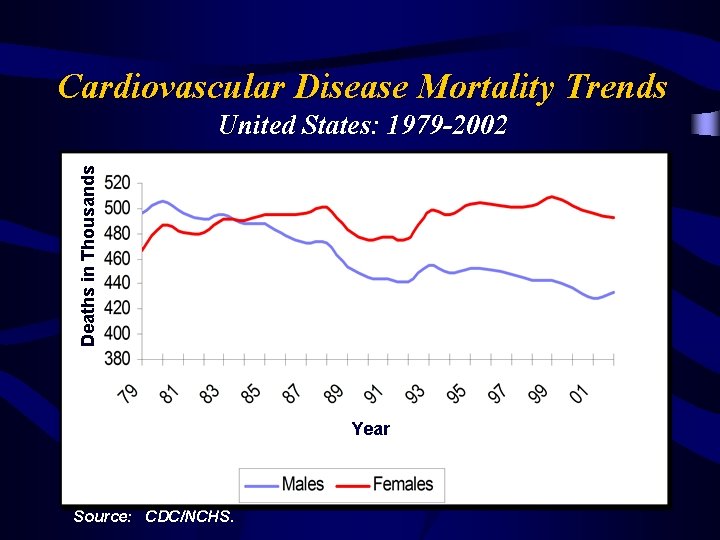
Cardiovascular Disease Mortality Trends Deaths in Thousands United States: 1979 -2002 Year Source: CDC/NCHS.
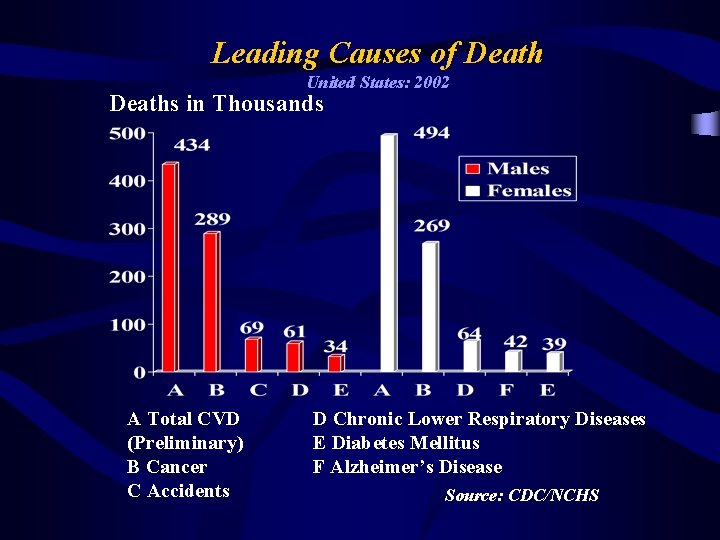
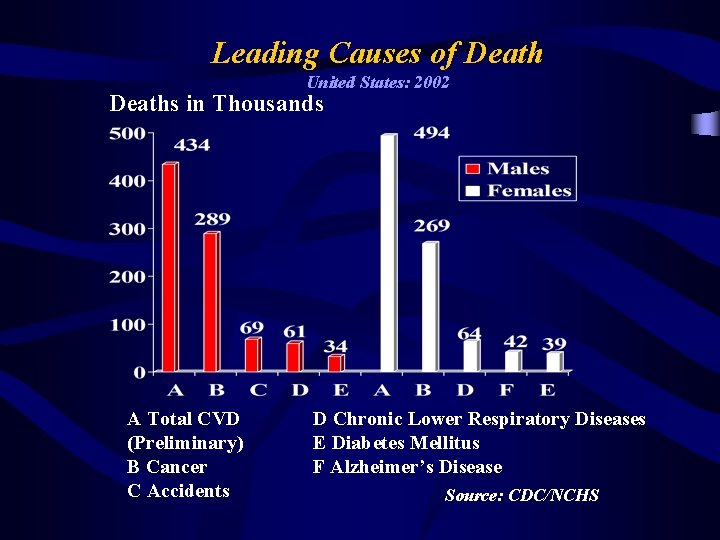
Leading Causes of Death United States: 2002 Deaths in Thousands A Total CVD (Preliminary) B Cancer C Accidents D Chronic Lower Respiratory Diseases E Diabetes Mellitus F Alzheimer’s Disease Source: CDC/NCHS
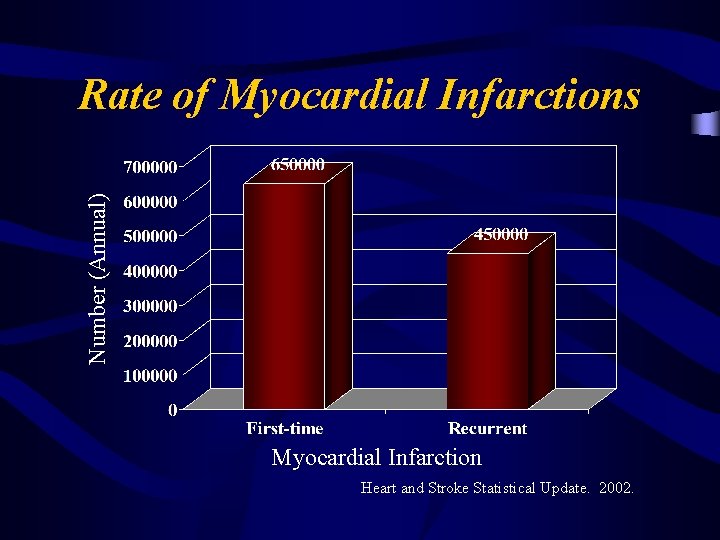
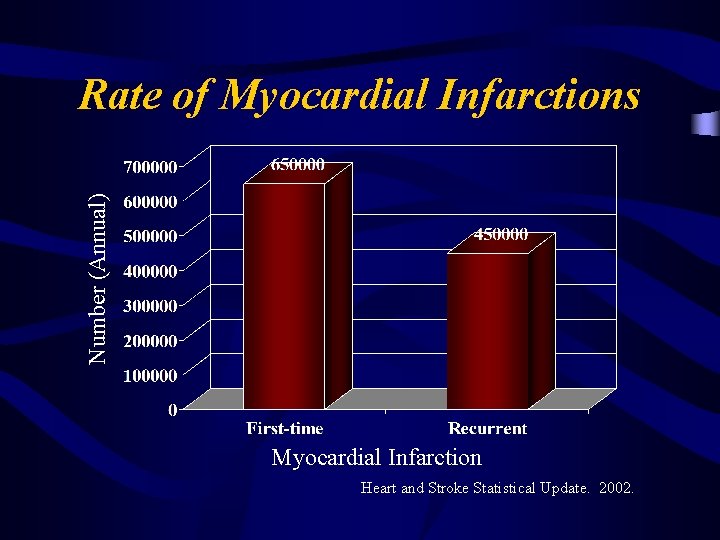
Number (Annual) Rate of Myocardial Infarctions Myocardial Infarction Heart and Stroke Statistical Update. 2002.
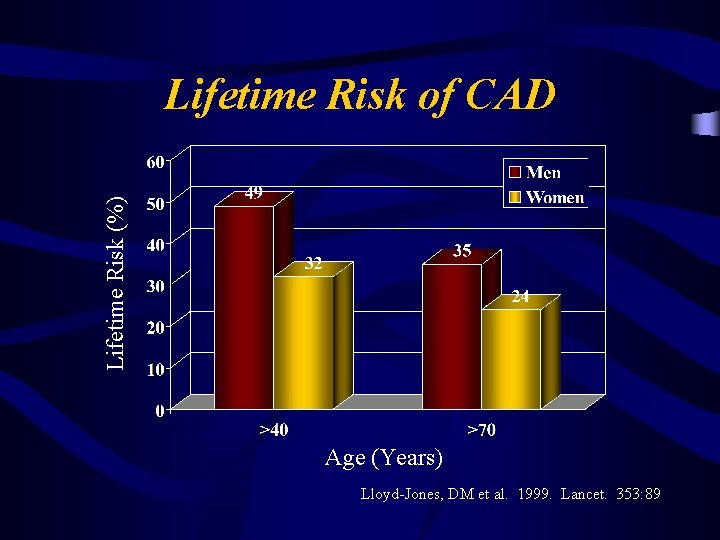
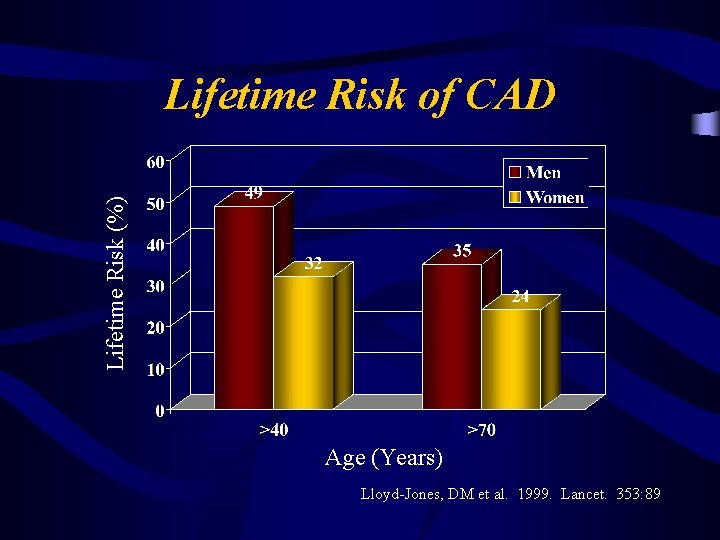
Lifetime Risk (%) Lifetime Risk of CAD Age (Years) Lloyd-Jones, DM et al. 1999. Lancet. 353: 89
Growing Prevalence of CAD v Larger pool Ø Population v is growing older Greater Risks Ø Increasing incidence of Obesity Diabetes Metabolic Syndrome Hypertension
Who Are at Risk? How Can We Identify Them?

The Framingham Score for Risk Prediction Risk: Low Intermediate High <10% 10 -20% >20% Greenland Gaziano, NEJM, 2003
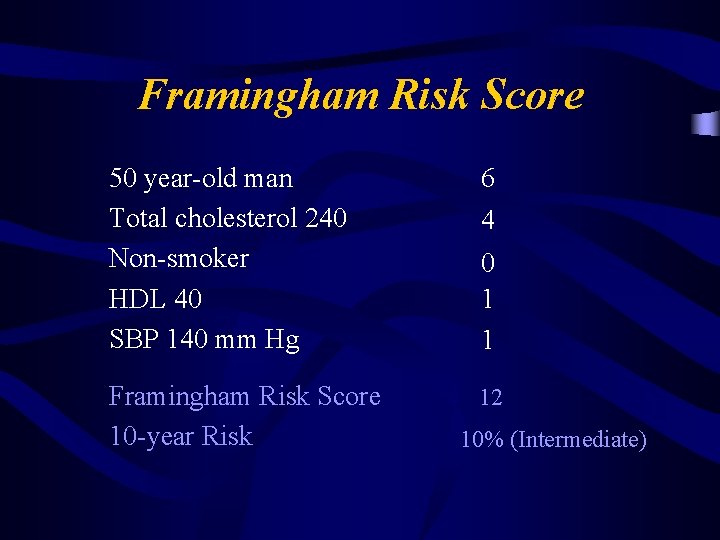
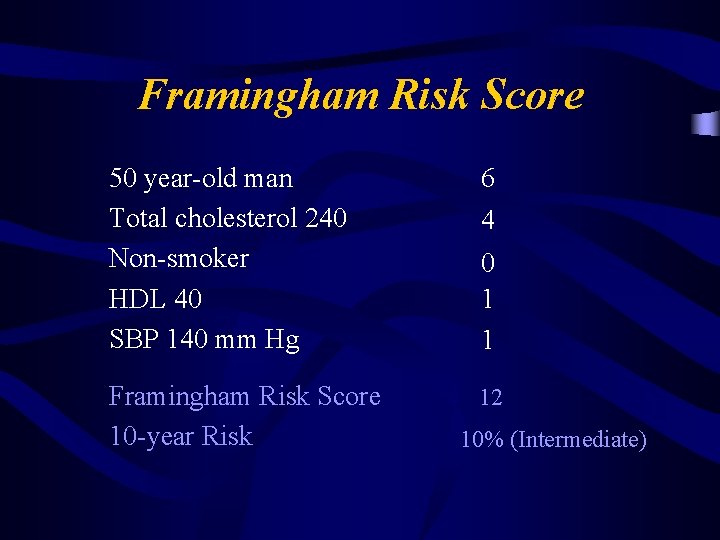
Framingham Risk Score 50 year-old man Total cholesterol 240 Non-smoker HDL 40 SBP 140 mm Hg 6 4 Framingham Risk Score 10 -year Risk 12 0 1 1 10% (Intermediate)
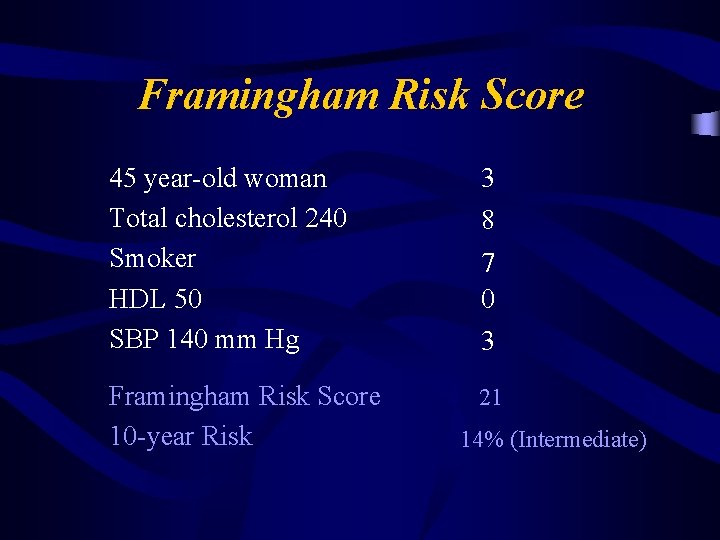
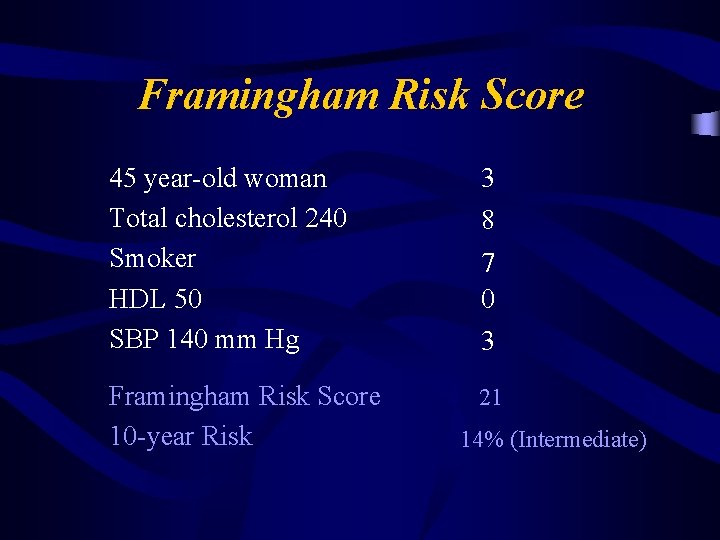
Framingham Risk Score 45 year-old woman Total cholesterol 240 Smoker HDL 50 SBP 140 mm Hg 3 8 Framingham Risk Score 10 -year Risk 21 7 0 3 14% (Intermediate)
Limitations of the Framingham Risk Score v Family v CRP History of Premature CAD Levels v Metabolic Syndrome
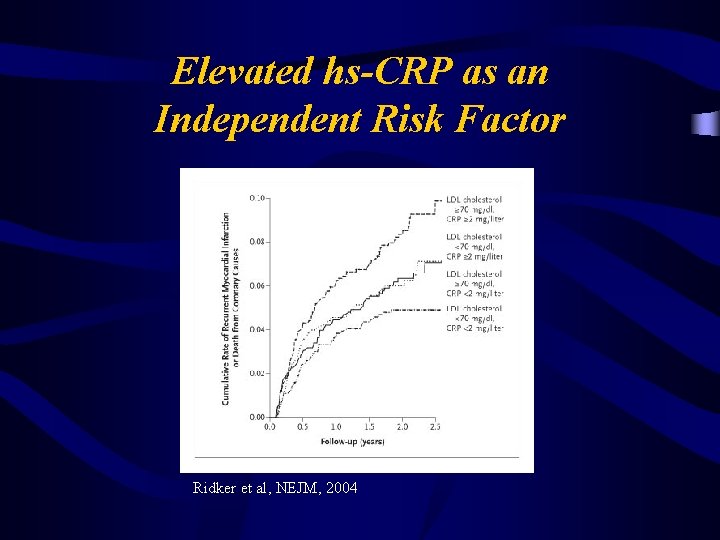
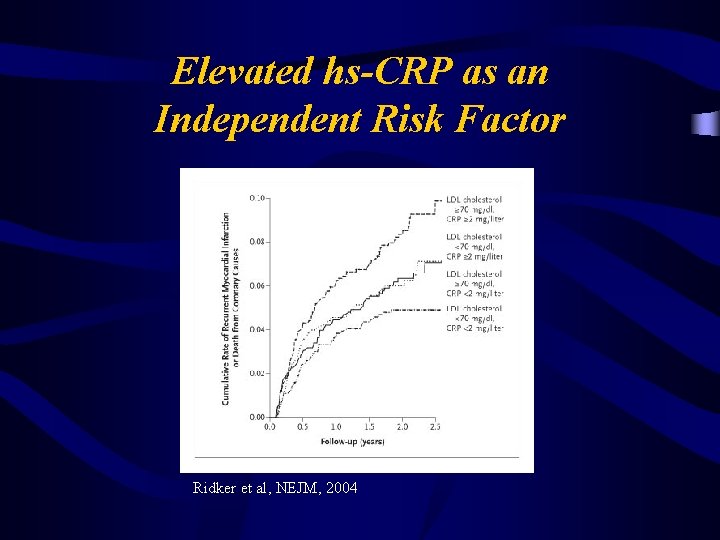
Elevated hs-CRP as an Independent Risk Factor Ridker et al, NEJM, 2004

Mortality Rates in Adults with Metabolic Syndrome NHANES II: 1976 -80 Follow-up Study 13 years average follow-up. Source: Circulation 2004; 110: 1245 -50.
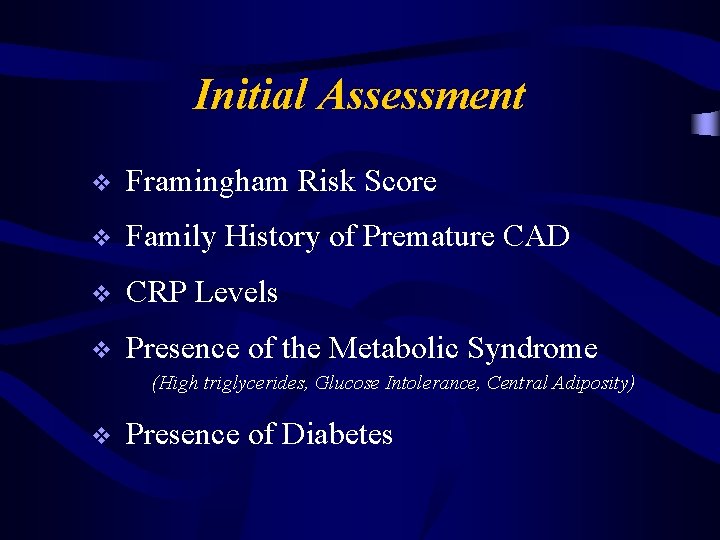
Initial Assessment v Framingham Risk Score v Family History of Premature CAD v CRP Levels v Presence of the Metabolic Syndrome (High triglycerides, Glucose Intolerance, Central Adiposity) v Presence of Diabetes
Now What? “Fear of God” Modify Risk Factors Further Risk Stratify
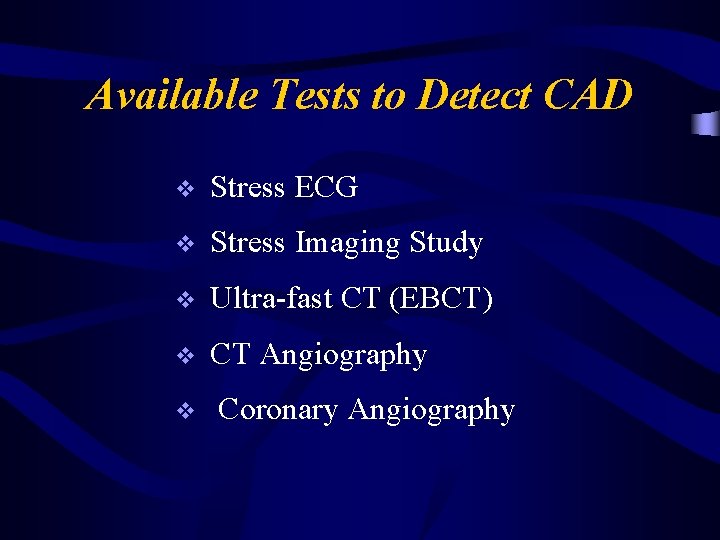
Available Tests to Detect CAD v Stress ECG v Stress Imaging Study v Ultra-fast CT (EBCT) v CT Angiography v Coronary Angiography
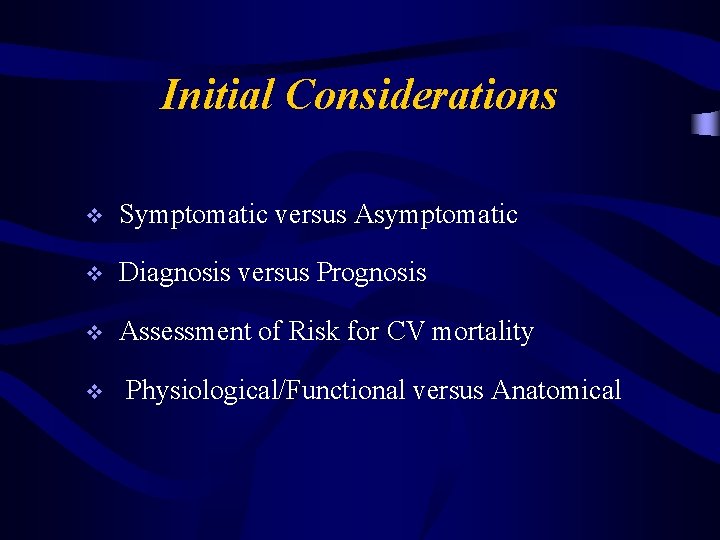
Initial Considerations v Symptomatic versus Asymptomatic v Diagnosis versus Prognosis v Assessment of Risk for CV mortality v Physiological/Functional versus Anatomical
Patients with Symptoms
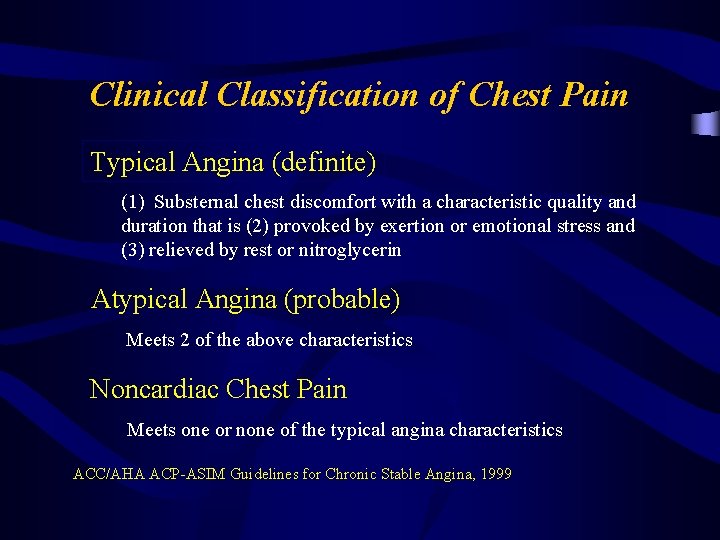
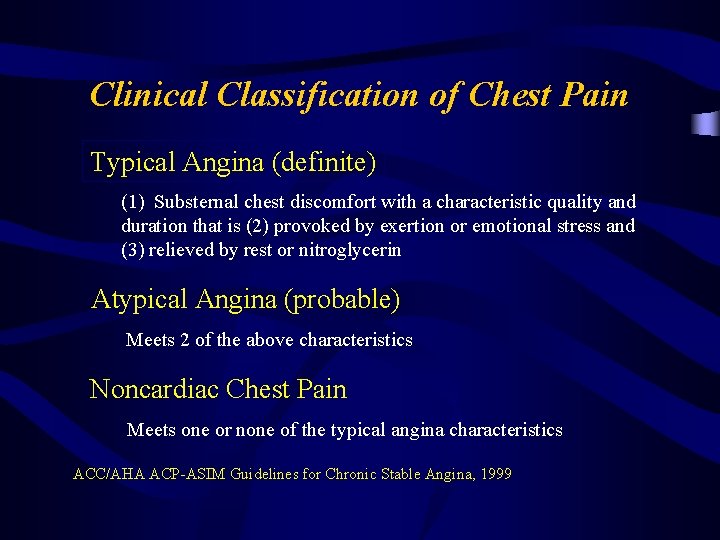
Clinical Classification of Chest Pain Typical Angina (definite) (1) Substernal chest discomfort with a characteristic quality and duration that is (2) provoked by exertion or emotional stress and (3) relieved by rest or nitroglycerin Atypical Angina (probable) Meets 2 of the above characteristics Noncardiac Chest Pain Meets one or none of the typical angina characteristics ACC/AHA ACP-ASIM Guidelines for Chronic Stable Angina, 1999
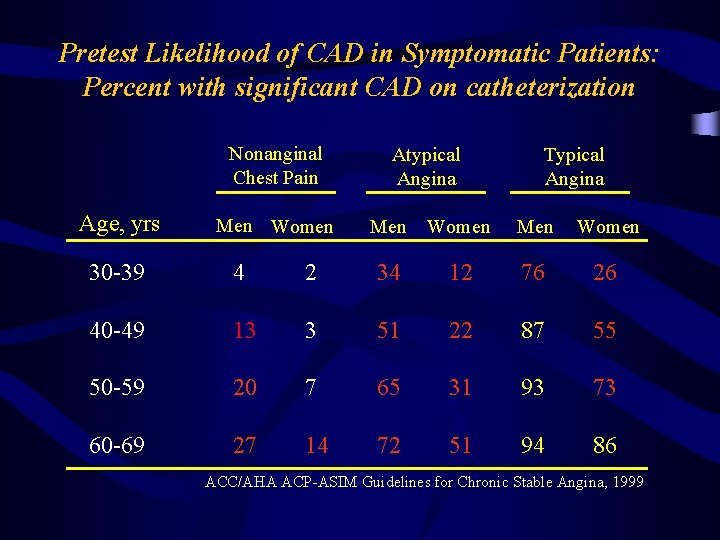
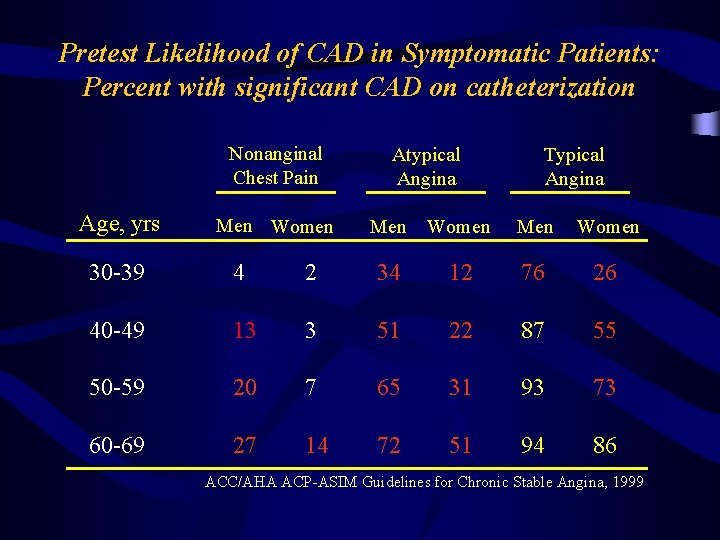
Pretest Likelihood of CAD in Symptomatic Patients: Percent with significant CAD on catheterization Nonanginal Chest Pain Age, yrs Men Women Atypical Angina Typical Angina Men Women 30 -39 4 2 34 12 76 26 40 -49 13 3 51 22 87 55 50 -59 20 7 65 31 93 73 60 -69 27 14 72 51 94 86 ACC/AHA ACP-ASIM Guidelines for Chronic Stable Angina, 1999

Kaplan-Meier Survival in Risk Stratified Patients Shaw, et al, AJC, 2000
Exercise Testing
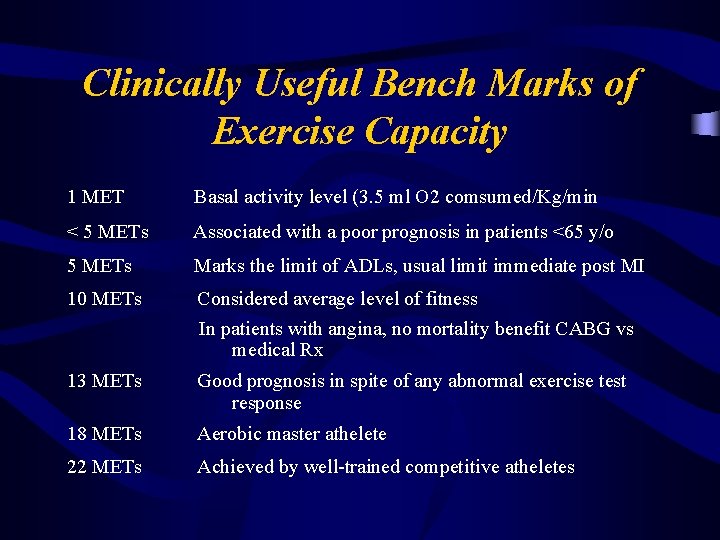
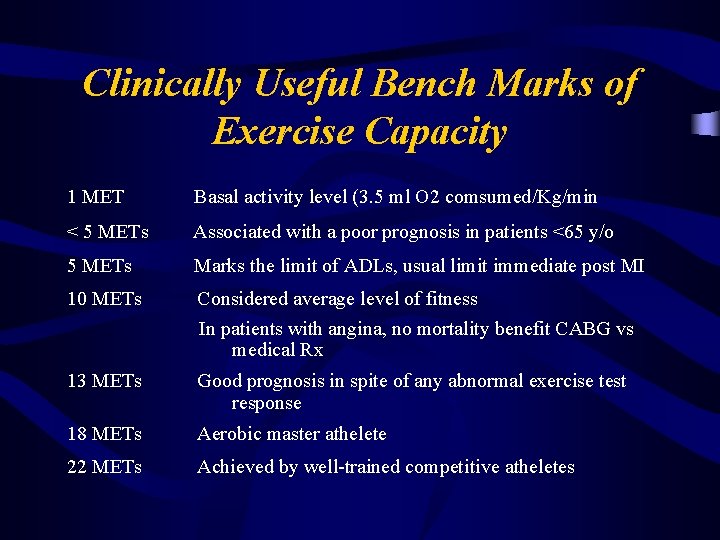
Clinically Useful Bench Marks of Exercise Capacity 1 MET Basal activity level (3. 5 ml O 2 comsumed/Kg/min < 5 METs Associated with a poor prognosis in patients <65 y/o 5 METs Marks the limit of ADLs, usual limit immediate post MI 10 METs Considered average level of fitness In patients with angina, no mortality benefit CABG vs medical Rx 13 METs Good prognosis in spite of any abnormal exercise test response 18 METs Aerobic master athelete 22 METs Achieved by well-trained competitive atheletes

4 -year Mortality Rates (%) Four-year Mortality Rates with Abnormal ETT: Effects of Exercise Capacity Weiner, et al, JACC, 1984

Exercise Parameters Associated with Advanced CAD or Poor Prognosis 1. Duration of ETT <6. 5 METS (<5 METS for women) 2. Exercise HR <120 bpm off b-blockers 3. Ischemic ST segment change at HR <120 bpm or <6. 5 METS 4. ST segment depression >2 mm, especially in multiple leads 5. ST segment depression for >6 min in recovery 6. Decrease in BP during exercise
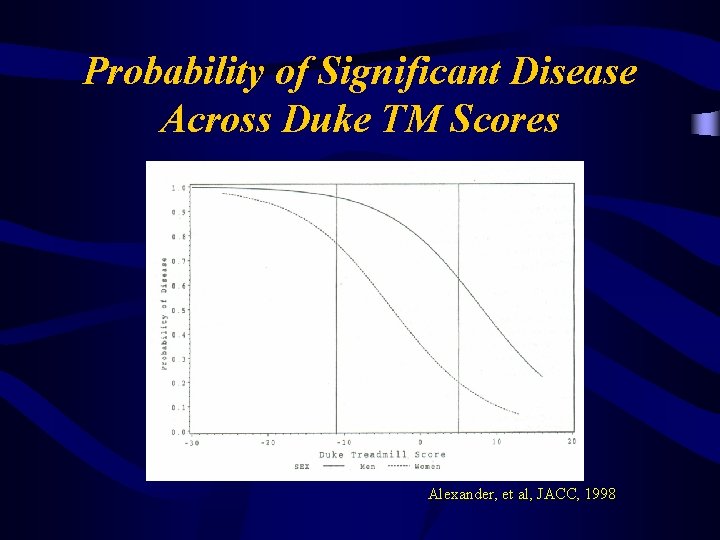
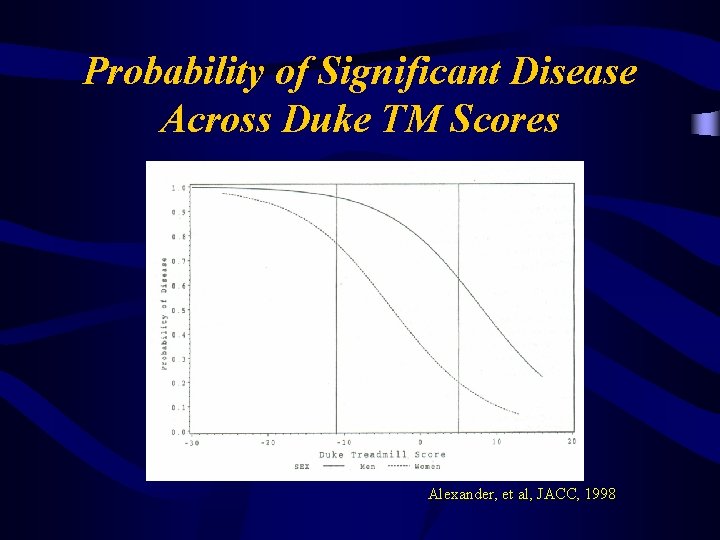
Probability of Significant Disease Across Duke TM Scores Alexander, et al, JACC, 1998
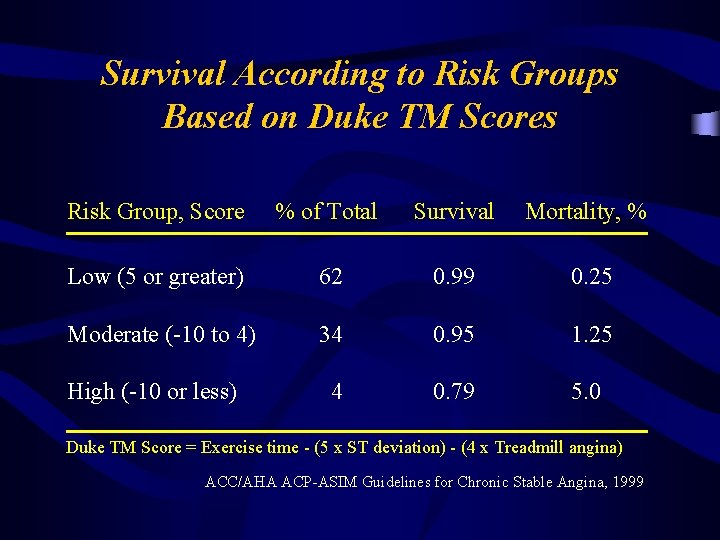
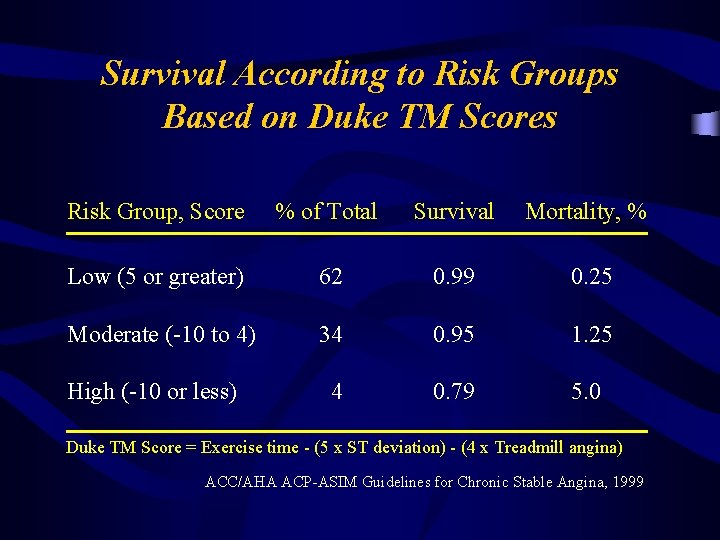
Survival According to Risk Groups Based on Duke TM Scores Risk Group, Score % of Total Survival Mortality, % Low (5 or greater) 62 0. 99 0. 25 Moderate (-10 to 4) 34 0. 95 1. 25 4 0. 79 5. 0 High (-10 or less) Duke TM Score = Exercise time - (5 x ST deviation) - (4 x Treadmill angina) ACC/AHA ACP-ASIM Guidelines for Chronic Stable Angina, 1999
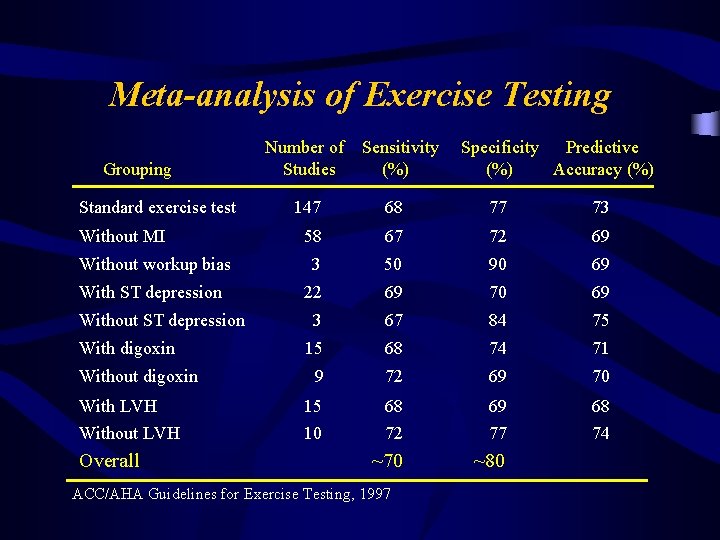
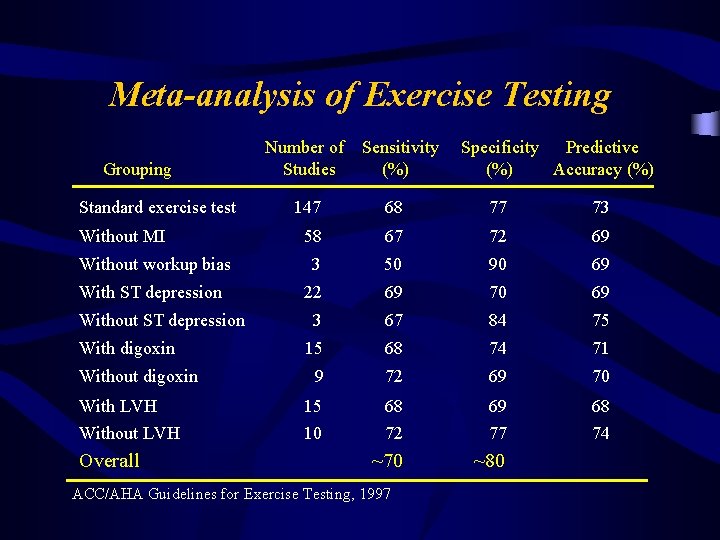
Meta-analysis of Exercise Testing Grouping Standard exercise test Number of Studies Sensitivity (%) Specificity Predictive (%) Accuracy (%) 147 68 77 73 58 67 72 69 Without workup bias 3 50 90 69 With ST depression 22 69 70 69 3 67 84 75 15 68 74 71 9 72 69 70 15 10 68 72 69 77 68 74 ~70 ~80 Without MI Without ST depression With digoxin Without digoxin With LVH Without LVH Overall ACC/AHA Guidelines for Exercise Testing, 1997
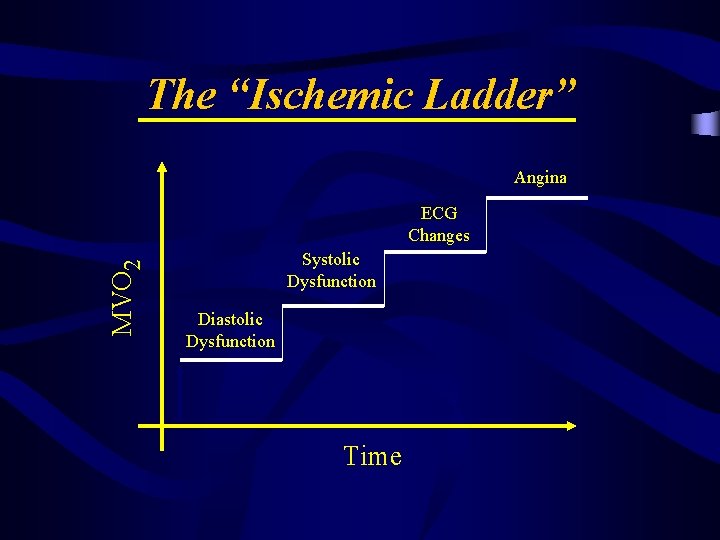
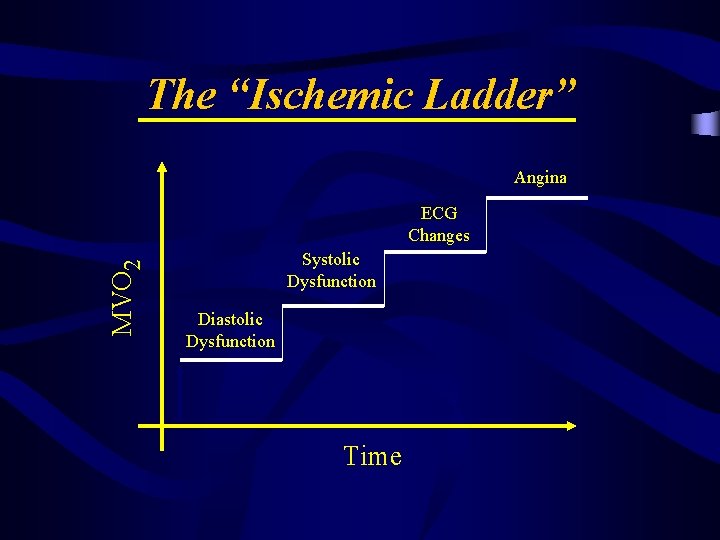
The “Ischemic Ladder” Angina MVO 2 ECG Changes Systolic Dysfunction Diastolic Dysfunction Time
Stress Imaging

Stress Imaging Studies Stress Modalities v v Exercise Dobutamine Adenosine (Persantine) Imaging Modalities v v Echocardiography Perfusion Imaging – – v Nuclear Scan Thallium Scan Sestamibi Scan Hybrid Scan MRI

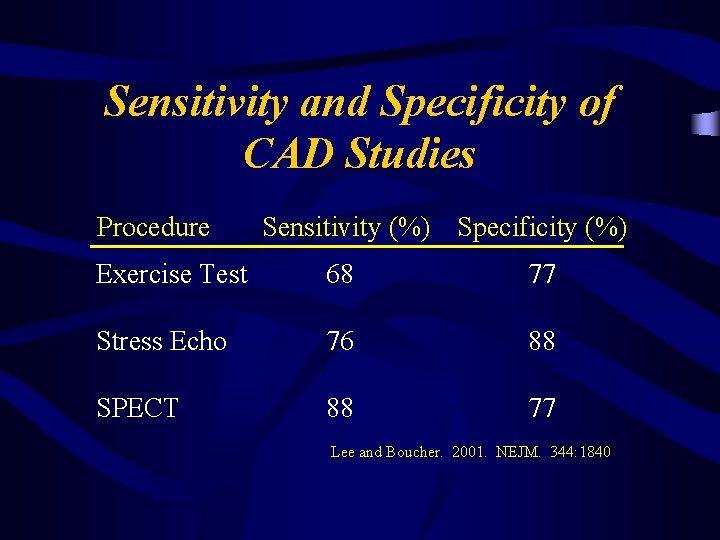
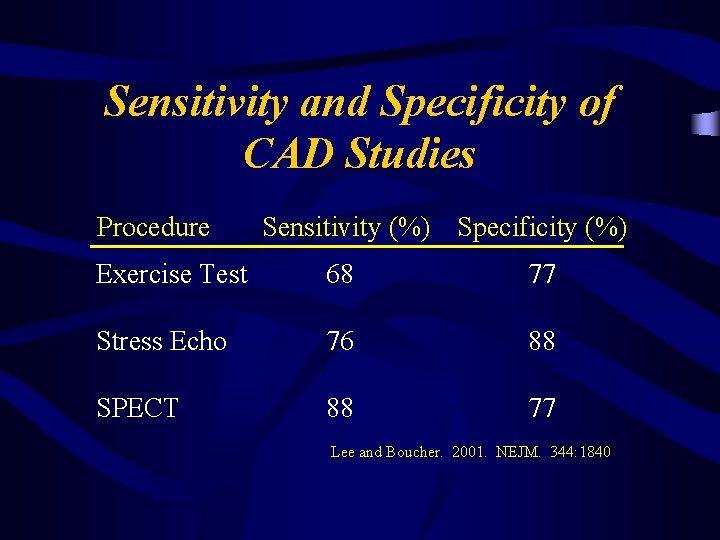
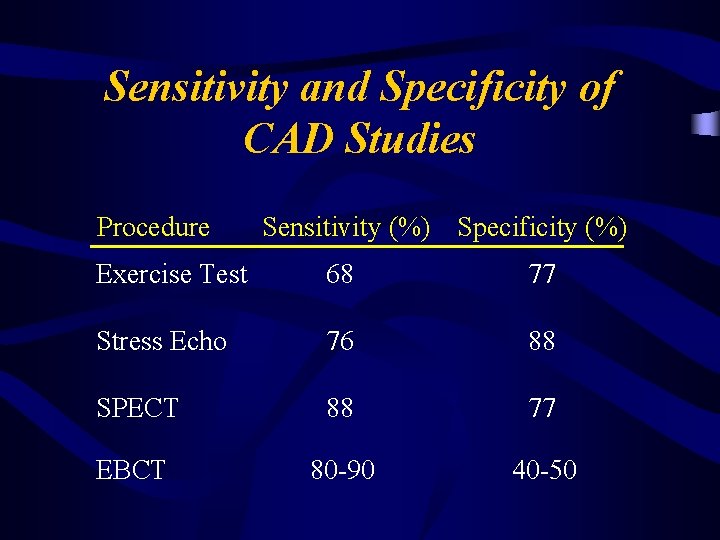
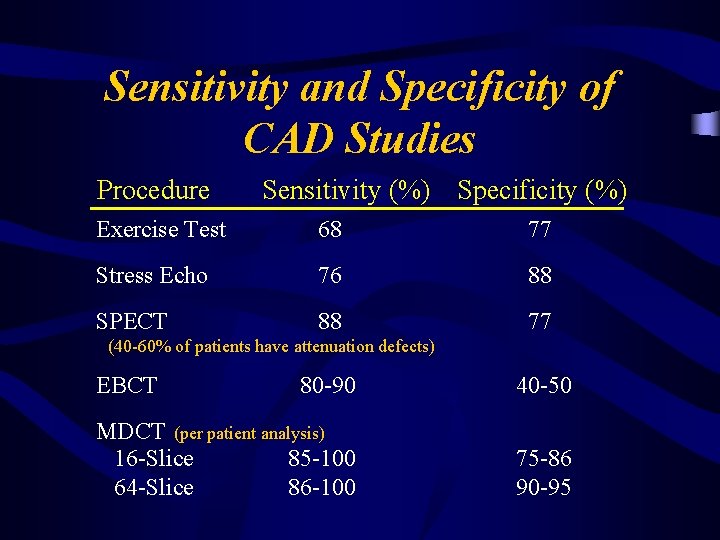
Sensitivity and Specificity of CAD Studies Procedure Sensitivity (%) Specificity (%) Exercise Test 68 77 Stress Echo 76 88 SPECT 88 77 Lee and Boucher. 2001. NEJM. 344: 1840

Advantages of Stress Echocardiography 1. Higher specificity 2. Versatility: more extensive evaluation of cardiac anatomy and function 3. Greater convenience/efficacy/availability 4. Lower cost
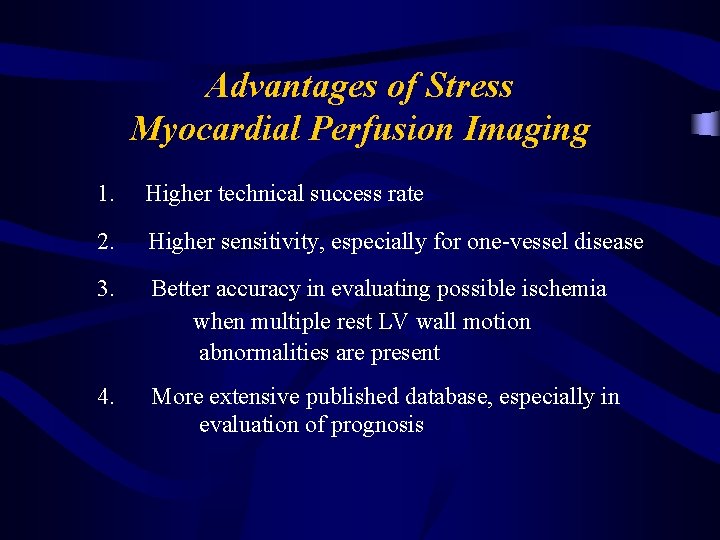
Advantages of Stress Myocardial Perfusion Imaging 1. Higher technical success rate 2. Higher sensitivity, especially for one-vessel disease 3. Better accuracy in evaluating possible ischemia when multiple rest LV wall motion abnormalities are present 4. More extensive published database, especially in evaluation of prognosis

Patients without Symptoms High Grade Stenoses Diabetics Non-flow Limiting Disease
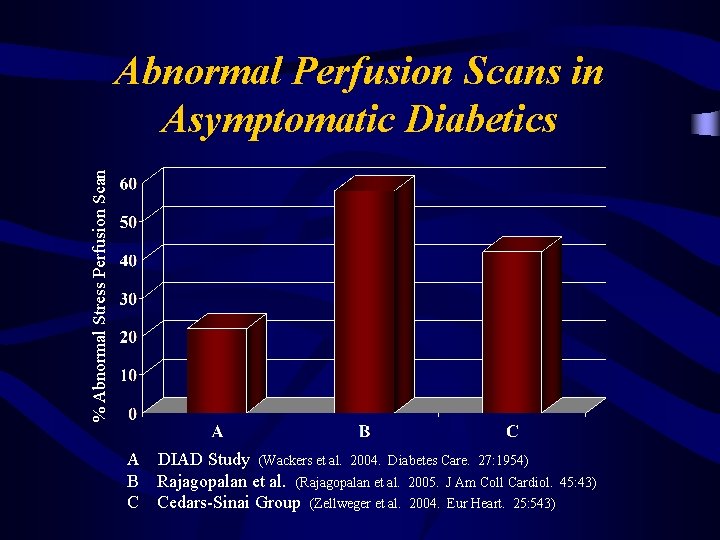
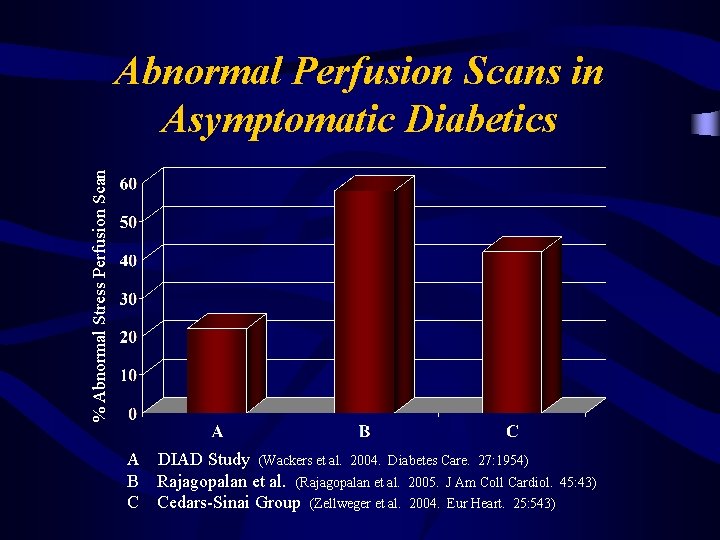
% Abnormal Stress Perfusion Scan Abnormal Perfusion Scans in Asymptomatic Diabetics A DIAD Study (Wackers et al. 2004. Diabetes Care. 27: 1954) B Rajagopalan et al. (Rajagopalan et al. 2005. J Am Coll Cardiol. 45: 43) C Cedars-Sinai Group (Zellweger et al. 2004. Eur Heart. 25: 543)

Yield of High-Risk Scans in Asymtomatic Diabetics Subgroup High-risk Scans Q waves on ECG 43% Abnormal ECG 26% Peripheral Vascular Disease 28% LDL >100 mg/dl 20% Two or more risk factors 17% Rajagopalan et al. 2005. J Am Coll Cardiol. 45: 43
Screening of CAD: ADA Recommendations In asymptomatic diabetic patients with: v v v Abnormal resting ECG (MI or ischemia) Peripheral vascular disease Two or more additional CAD risk factors
Patients without Symptoms Mild CAD Not Detectable by Stress Testing
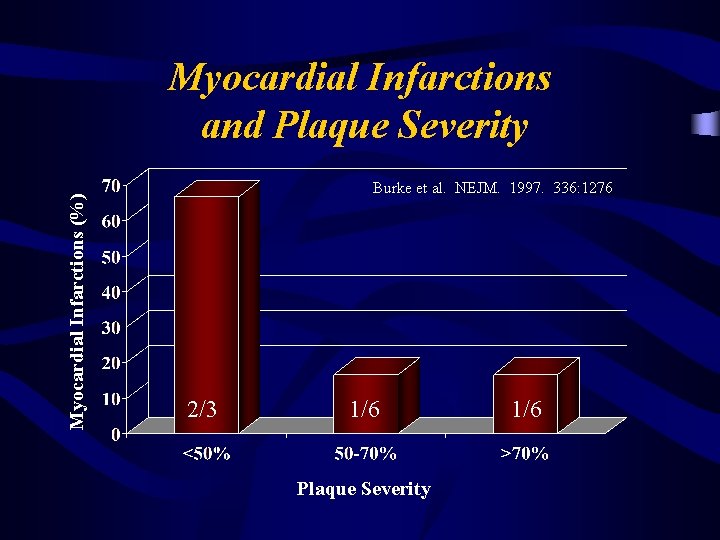
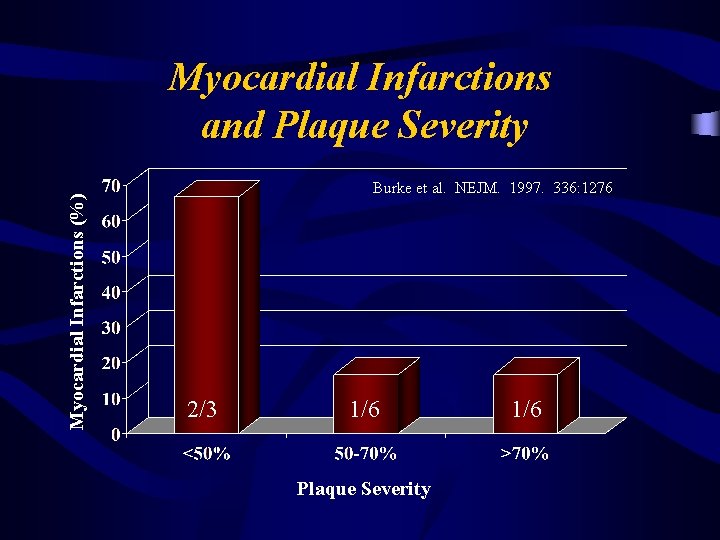
Myocardial Infarctions (%) Myocardial Infarctions and Plaque Severity Burke et al. NEJM. 1997. 336: 1276 2/3 1/6 Plaque Severity 1/6
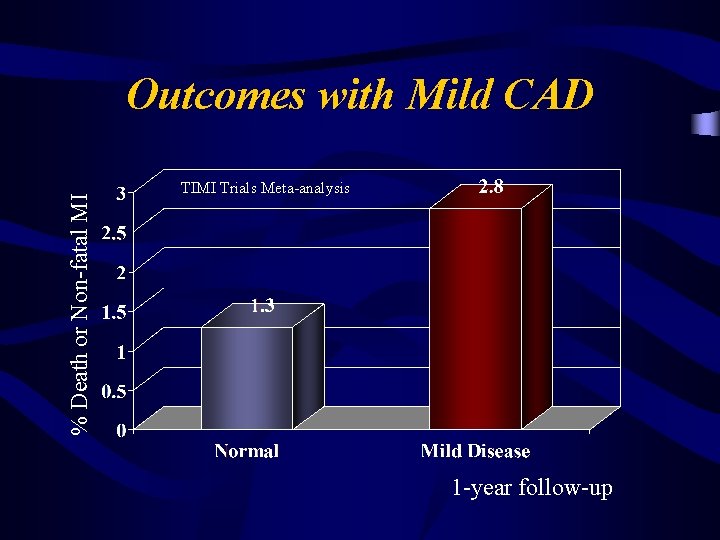
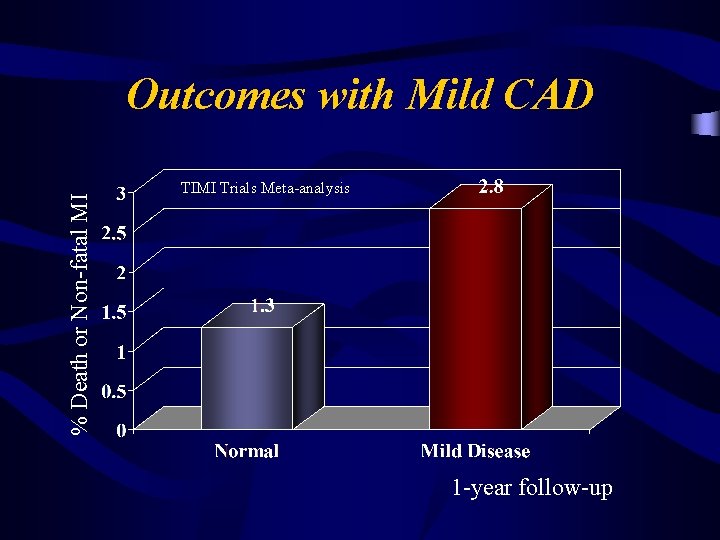
% Death or Non-fatal MI Outcomes with Mild CAD TIMI Trials Meta-analysis 1 -year follow-up
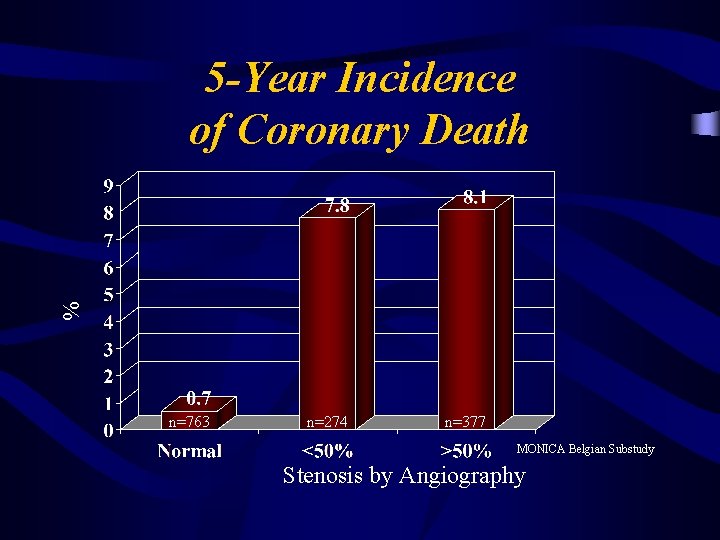
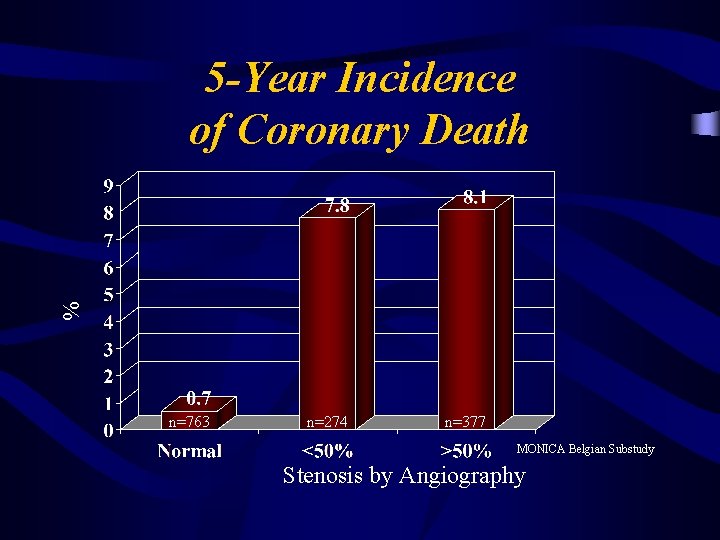
% 5 -Year Incidence of Coronary Death n=763 n=274 n=377 MONICA Belgian Substudy Stenosis by Angiography
Available Tests to Detect CAD v Stress ECG v Stress Imaging Study v Ultra-fast CT (EBCT) v CT Angiography v Coronary Angiography
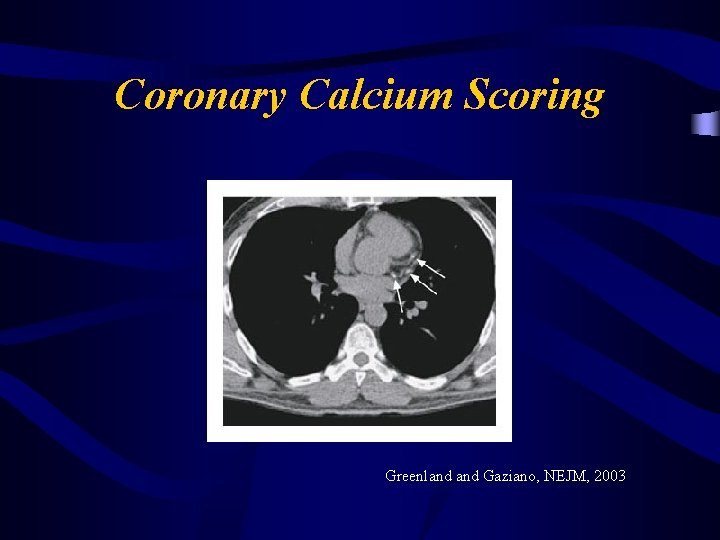
Coronary Calcium Scoring Greenland Gaziano, NEJM, 2003
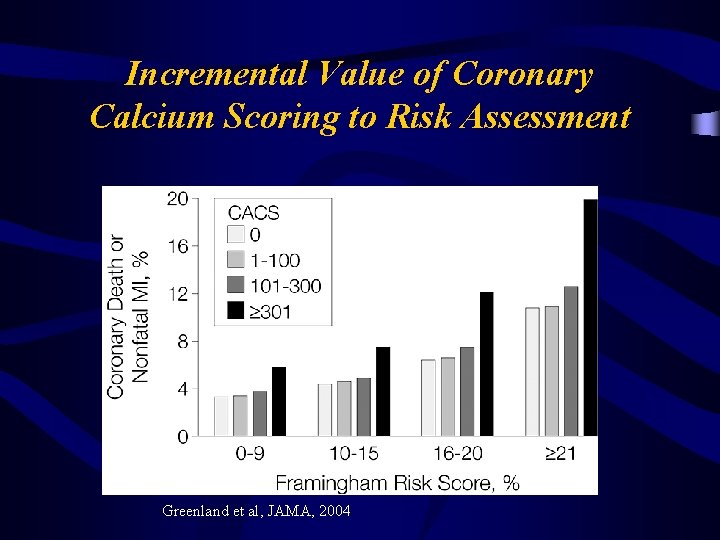
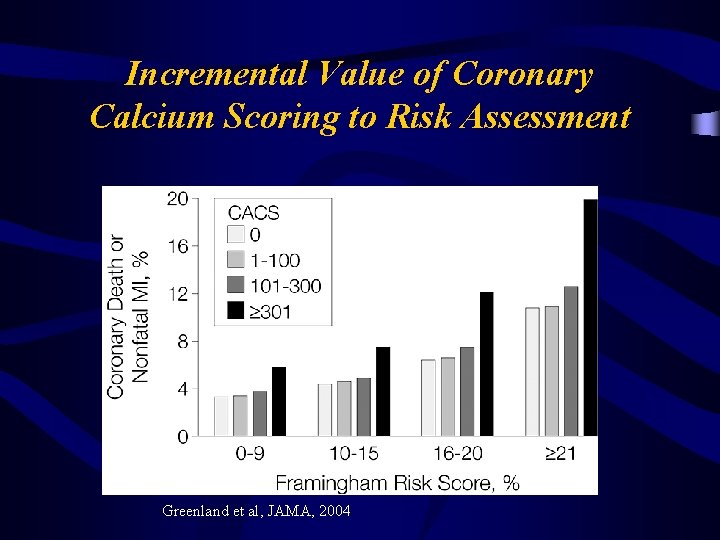
Incremental Value of Coronary Calcium Scoring to Risk Assessment Greenland et al, JAMA, 2004
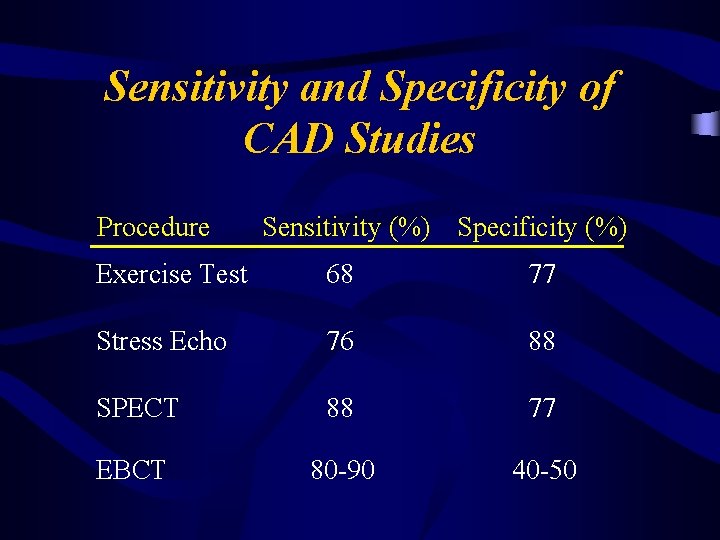
Sensitivity and Specificity of CAD Studies Procedure Sensitivity (%) Specificity (%) Exercise Test 68 77 Stress Echo 76 88 SPECT 88 77 EBCT 80 -90 40 -50

“Treating the Herd” Population versus Individual Risk
Multi-Detector Computer Tomography (MDCT)
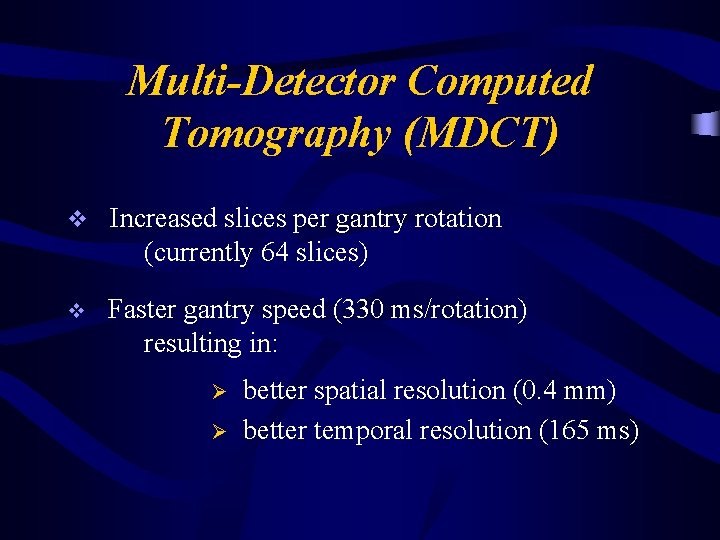
Multi-Detector Computed Tomography (MDCT) v Increased slices per gantry rotation (currently 64 slices) v Faster gantry speed (330 ms/rotation) resulting in: Ø Ø better spatial resolution (0. 4 mm) better temporal resolution (165 ms)
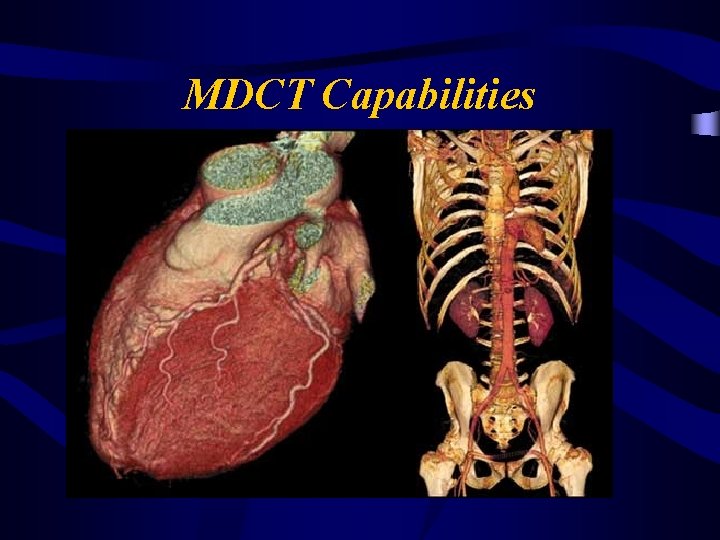
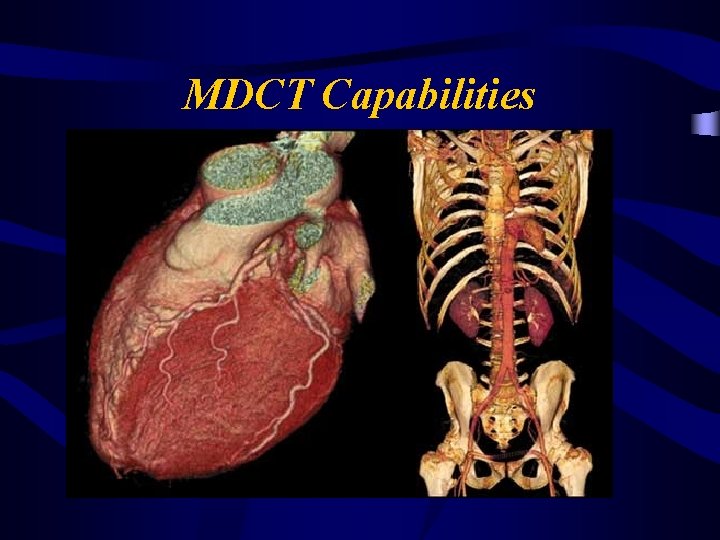
MDCT Capabilities
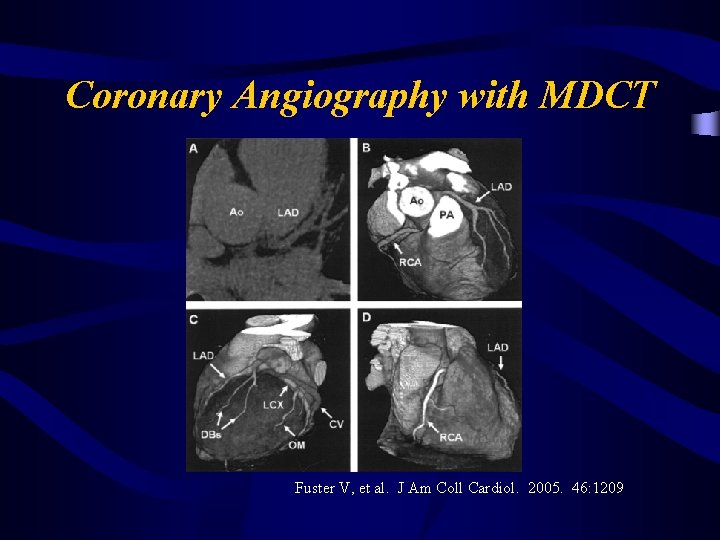
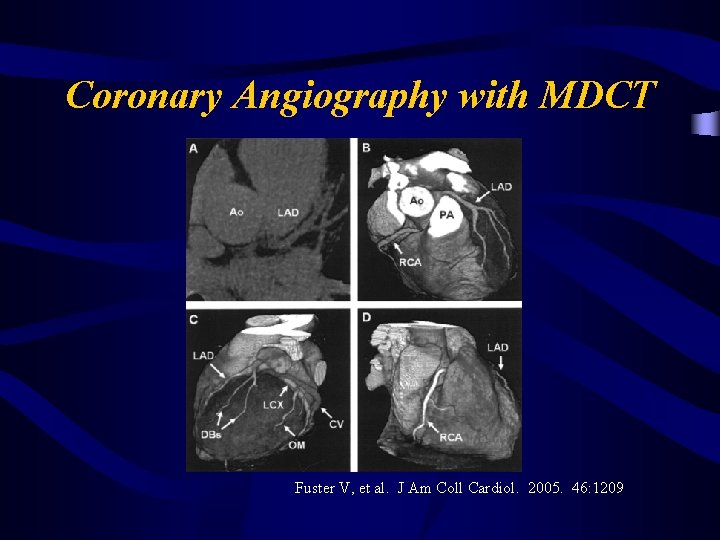
Coronary Angiography with MDCT Fuster V, et al. J Am Coll Cardiol. 2005. 46: 1209
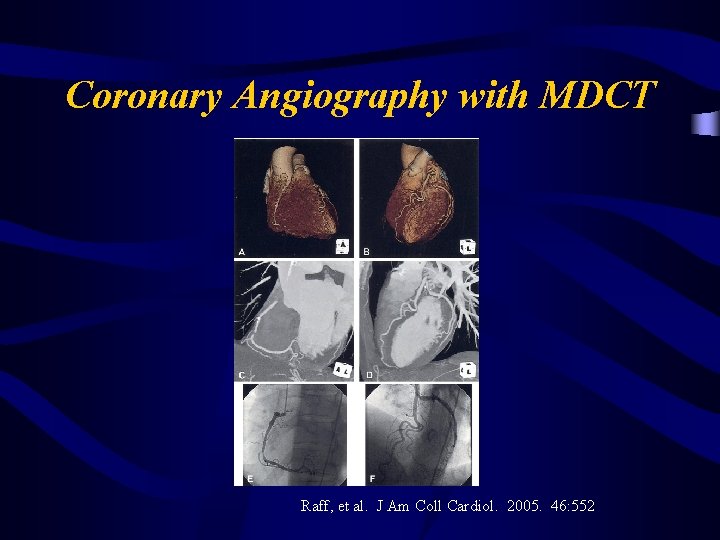
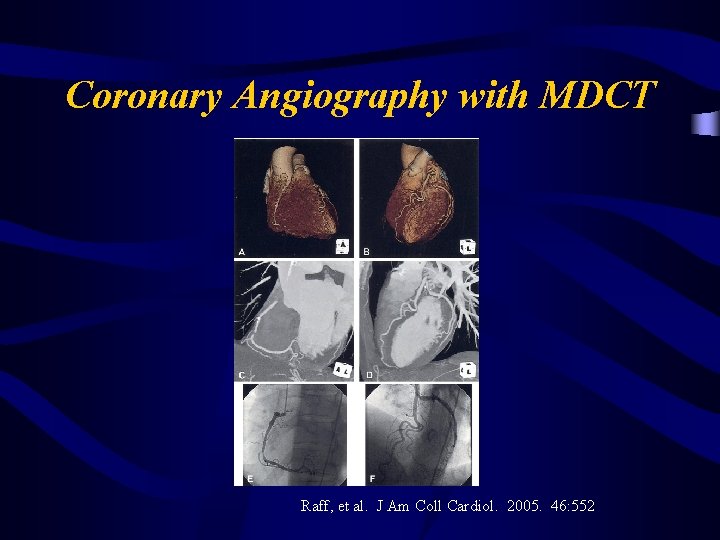
Coronary Angiography with MDCT Raff, et al. J Am Coll Cardiol. 2005. 46: 552
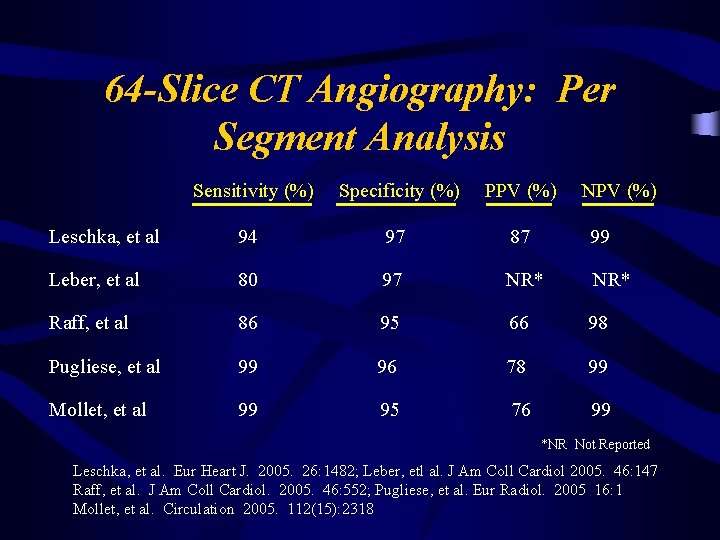
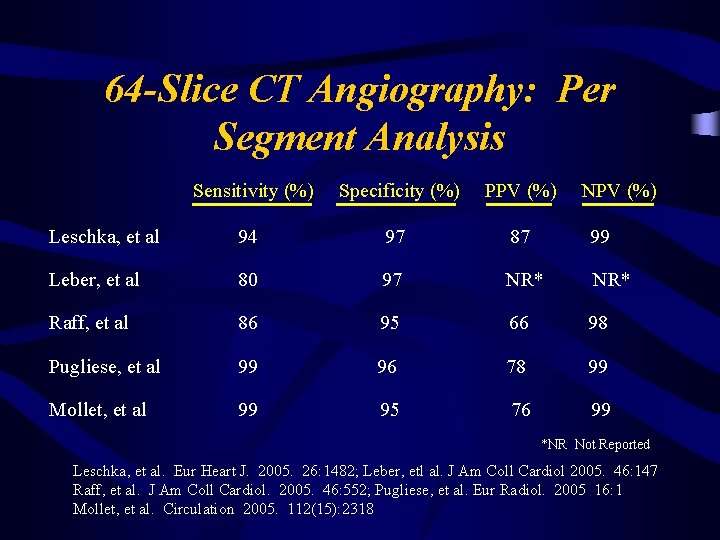
64 -Slice CT Angiography: Per Segment Analysis Sensitivity (%) Specificity (%) PPV (%) NPV (%) Leschka, et al 94 97 87 99 Leber, et al 80 97 NR* Raff, et al 86 95 66 98 Pugliese, et al 99 96 78 99 Mollet, et al 99 95 76 99 *NR Not Reported Leschka, et al. Eur Heart J. 2005. 26: 1482; Leber, etl al. J Am Coll Cardiol 2005. 46: 147 Raff, et al. J Am Coll Cardiol. 2005. 46: 552; Pugliese, et al. Eur Radiol. 2005 16: 1 Mollet, et al. Circulation 2005. 112(15): 2318
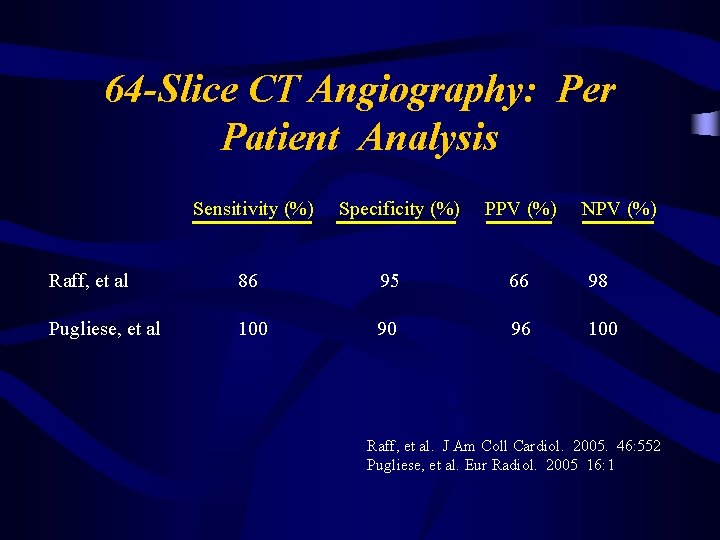
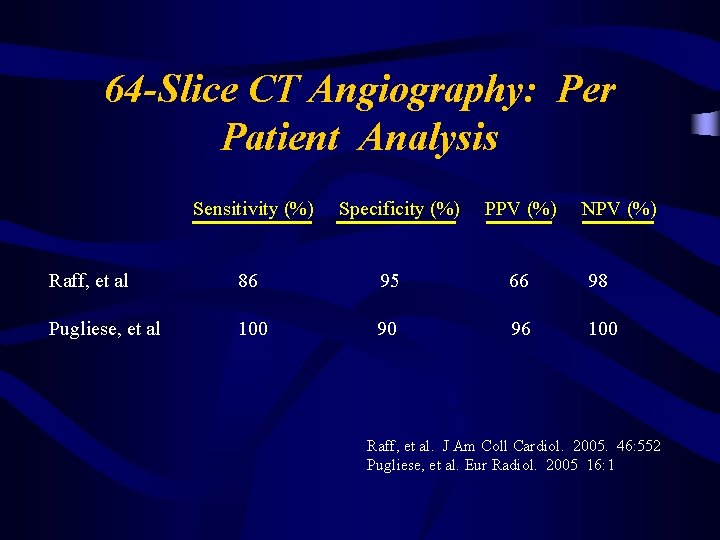
64 -Slice CT Angiography: Per Patient Analysis Sensitivity (%) Specificity (%) PPV (%) NPV (%) Raff, et al 86 95 66 98 Pugliese, et al 100 90 96 100 Raff, et al. J Am Coll Cardiol. 2005. 46: 552 Pugliese, et al. Eur Radiol. 2005 16: 1
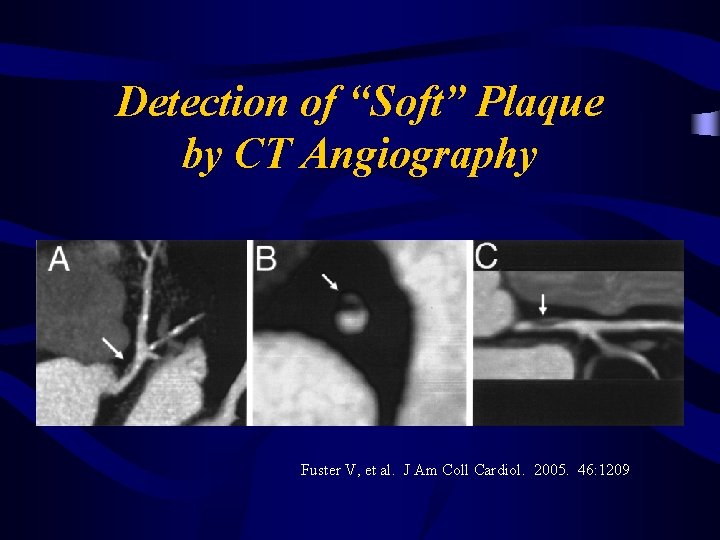
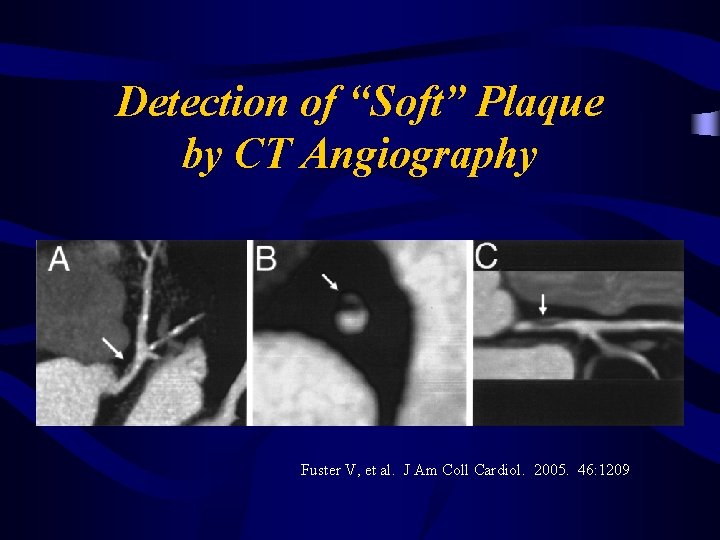
Detection of “Soft” Plaque by CT Angiography Fuster V, et al. J Am Coll Cardiol. 2005. 46: 1209
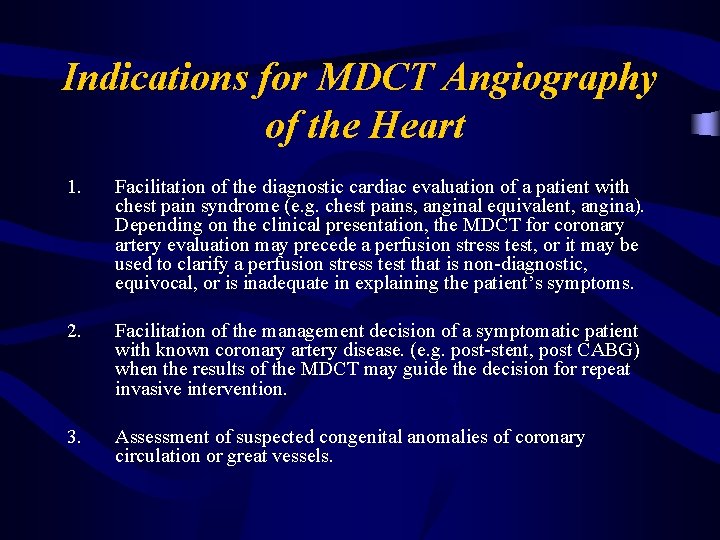
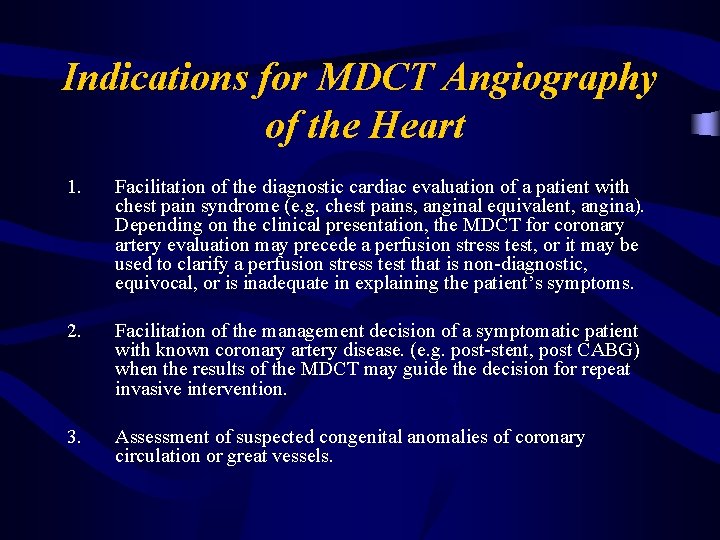
Indications for MDCT Angiography of the Heart 1. Facilitation of the diagnostic cardiac evaluation of a patient with chest pain syndrome (e. g. chest pains, anginal equivalent, angina). Depending on the clinical presentation, the MDCT for coronary artery evaluation may precede a perfusion stress test, or it may be used to clarify a perfusion stress test that is non-diagnostic, equivocal, or is inadequate in explaining the patient’s symptoms. 2. Facilitation of the management decision of a symptomatic patient with known coronary artery disease. (e. g. post-stent, post CABG) when the results of the MDCT may guide the decision for repeat invasive intervention. 3. Assessment of suspected congenital anomalies of coronary circulation or great vessels.
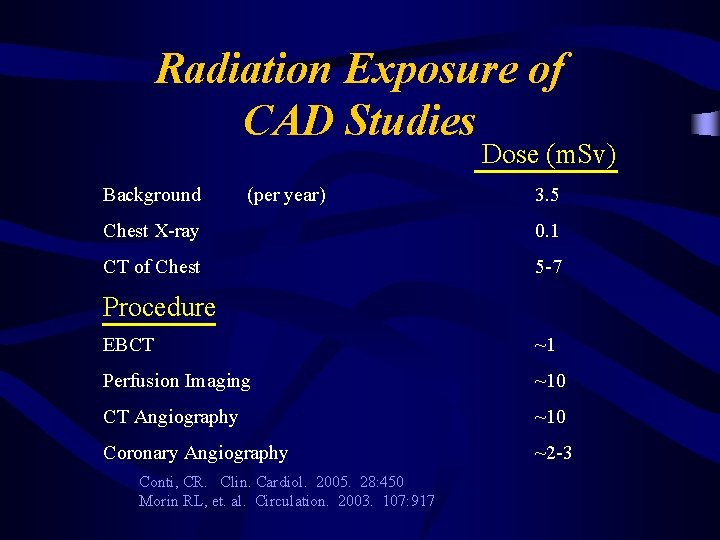
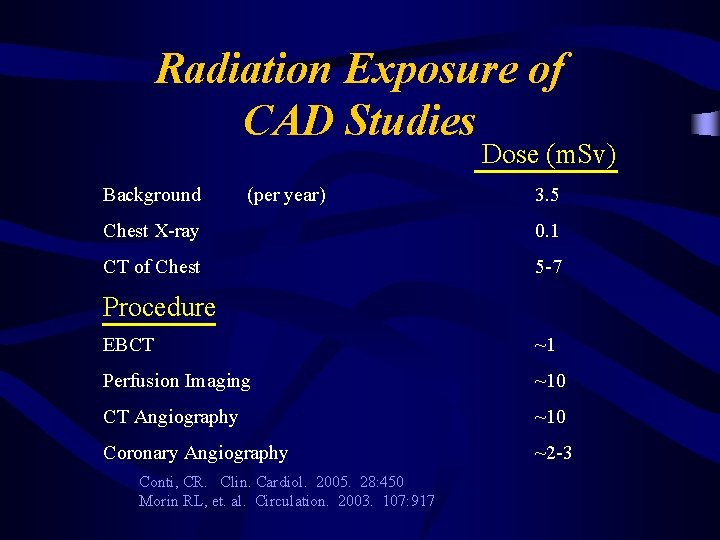
Radiation Exposure of CAD Studies Dose (m. Sv) Background (per year) 3. 5 Chest X-ray 0. 1 CT of Chest 5 -7 Procedure EBCT ~1 Perfusion Imaging ~10 CT Angiography ~10 Coronary Angiography ~2 -3 Conti, CR. Clin. Cardiol. 2005. 28: 450 Morin RL, et. al. Circulation. 2003. 107: 917
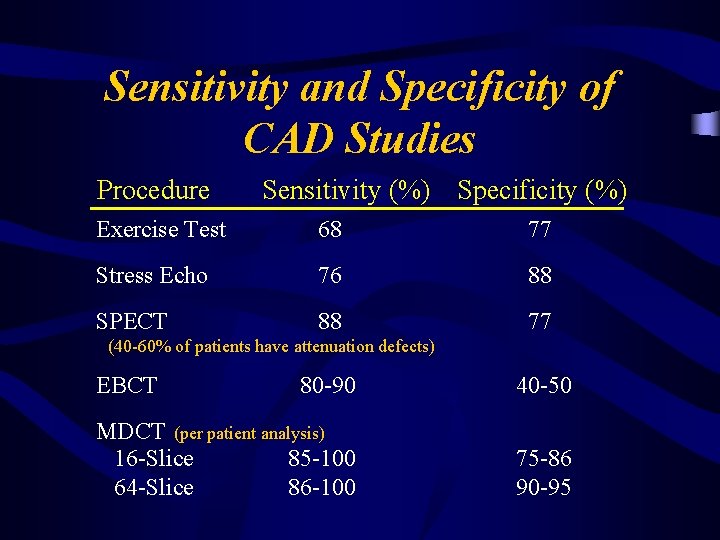
Sensitivity and Specificity of CAD Studies Procedure Sensitivity (%) Specificity (%) Exercise Test 68 77 Stress Echo 76 88 SPECT 88 77 (40 -60% of patients have attenuation defects) EBCT 80 -90 40 -50 MDCT (per patient analysis) 16 -Slice 85 -100 64 -Slice 86 -100 75 -86 90 -95
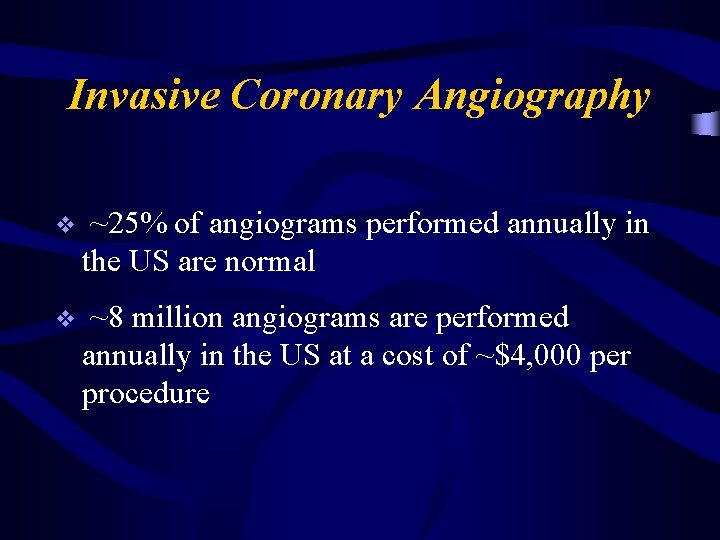
Invasive Coronary Angiography v ~25% of angiograms performed annually in the US are normal v ~8 million angiograms are performed annually in the US at a cost of ~$4, 000 per procedure

Invasive Coronary Angiography v Therefore, there are ~2 million angiograms performed annually on patients with normal coronary arteries v These procedures expose patients to the inherent risks of invasive coronary angiography at a cost of ~ $4 billion per year

Summary v The incidence and prevalence of CAD is growing due to aging of the population and to increases in risk factors. v Global clinical assessment, CRP levels, and calcium scoring may help to further stratify individual risks.
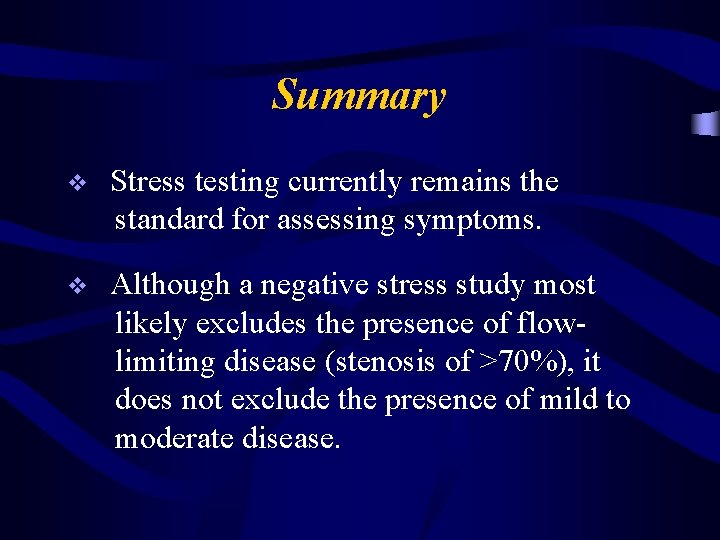
Summary v Stress testing currently remains the standard for assessing symptoms. v Although a negative stress study most likely excludes the presence of flowlimiting disease (stenosis of >70%), it does not exclude the presence of mild to moderate disease.

Summary v Mild to moderate disease still confers an increase in coronary deaths and infarctions. v Invasive coronary arteriography has been the only method of identifying patients with mild to moderate disease up to now.

Summary v CT angiography will allow for the noninvasive identification of at-risk patients as having (or not having) underlying coronary atherosclerosis.
Summary v Exercise Test – Probable more than we do v Stress Echocardiogram – Lower pre-test probablility population – Valvular or other structural heart disease
Summary v Stress Perfusion Scan – Higher pre-test probability population v Cardiac MRI – When above unhelpful and expertise is available
Summary v Ultra-fast CT (EBCT) – No role in symptomatic patients v CT Angiography – Will play larger role with ability to image coronaries (Triple Rule Out) v Coronary Angiography – When stress testing is potentially dangerous